Abstract
Recent scientific evidence demonstrates that many young men commonly resist condom use with their female sex partners and that both alcohol intoxication and a history of sexual aggression may increase the risk of condom use resistance (CUR). Using a community sample of heterosexual male non-problem drinkers with elevated sexual risk (N=311), this alcohol administration study examined the direct and indirect effects of intoxication and sexual aggression history on men's CUR intentions through a sexual risk analogue. State impulsivity, CUR-related attitudes, and CUR-related self-efficacy were assessed as mediators. Results demonstrated that alcohol intoxication directly increased CUR intentions, and sexual aggression history both directly and indirectly increased CUR intentions. These findings highlight the importance of addressing both alcohol use and sexual aggression in risky sex prevention programs, as well as indicate the continued worth of research regarding the intersection of men's alcohol use, sexual aggression, and sexual risk behaviors, especially CUR.
Keywords: condom use resistance, alcohol, sexual aggression, impulsivity
Incidence rates of sexually transmitted infections (STIs) continue to pose important public health concerns for young adults, with half of all new STIs occurring in individuals aged 15 - 24 (1). National estimates indicate that young men aged 20 - 24 have the highest rates of chlamydia, syphilis, and gonorrhea as compared to all other men, and these rates continue to rise (2). Consistent and correct condom usage could reduce STI transmission rates; however, the majority of young adults report that they do not use condoms consistently even with casual sexual partners (3). Further, recent research has demonstrated that active resistance of condom use is commonplace in young adult samples of men who have sex with women (4). The present study builds upon previous examinations of young men's condom use resistance (CUR) by investigating both distal and proximal predictors of CUR likelihood.
Condom Use Resistance
Studies indicate that men typically have more control than their female partners over whether or not a condom is correctly used (5, 6), suggesting that men also have the ability to avoid or resist condom use should they desire to not use a condom. CUR refers to attempts to engage in unprotected sexual intercourse with a partner who wants to use a condom (4). Previous research has identified several tactics that young men report employing to resist condom use with their female partners. These CUR tactics vary widely and include such behaviors as reassuring the partner that STI transmission risk is low, using emotional or relational reasons for forgoing condom use, and lying to or deceiving the partner about sexual risks (4, 5, 7). In one study, Davis, Stappenbeck et al. (2014) reported that almost 80% of young male non-problem drinkers who have sex with women indicated having successfully used one or more of these CUR tactics since the age of 14. Research from other investigators has also demonstrated that resistance to using condoms is quite common (8), and qualitative data indicate that young men perceive CUR to be normative and “just part of the game” when engaging in sexual interactions with casual female sex partners (9).
Proximal and Distal CUR Risk Factors
Socio-cognitive factors
Despite the apparent frequency and acceptance of CUR in some samples, relatively few studies have investigated potential CUR risk factors. Indeed, researchers have called for continued research into the predictors of CUR in order to augment our general understanding of condom negotiation (10). Socio-cognitive models successfully used to explain condom use intentions, such as the Theory of Planned Behavior (11, 12) have also been successfully applied to the prediction of CUR intentions (Author Citation masked for review). In that study, distal attitudes about CUR (e.g., whether CUR is viewed as positive or negative) and self-efficacy regarding CUR were significant positive predictors of CUR intentions. Although the study demonstrated the applicability of TPB constructs to the prediction of intentions to engage in CUR behavior, these constructs were measured generally and not within the context of a specific sexual situation. That is, participants were asked about their CUR attitudes, self-efficacy, and intentions regarding CUR behavior in the next three months. In the present study, we extend these findings by utilizing more proximal and specific measures of CUR attitudes and self-efficacy assessed through a sexual risk analogue paradigm.
Alcohol intoxication
The above-referenced study by Author and colleagues (under review) also demonstrated that alcohol intoxication may serve as a risk factor for engaging in CUR. Using an alcohol administration paradigm, participants completed TPB measures related to CUR (e.g., attitudes, self-efficacy, and intentions) both before and after consuming alcohol. Results indicated that alcohol intoxication increased participants' positive attitudes toward CUR, self-efficacy regarding CUR, and intentions to engage in CUR with a casual sex partner in the next three months. Alcohol's acute effects on TPB constructs related to CUR are commensurate with other literature demonstrating that acute alcohol intoxication can increase unprotected sex intentions (13).
State Impulsivity
One mechanism through which alcohol may exert its proximal influence on sexual risk behaviors, including CUR, is through its effects on in-the-moment or state impulsivity. Although impulsivity has been inconsistently defined, it is largely viewed as a multi-dimensional construct that involves “the tendency to engage in inappropriate or maladaptive behaviors” due to impaired behavior inhibition or decision-making processes (14). While often thought of as a trait, impulsivity may also fluctuate in brief, state-dependent ways (14, 15). Researchers have demonstrated that alcohol intoxication can increase impulsive behavior on a variety of tasks (e.g., delay discounting) that measure different facets of impulsivity, including response inhibition and consequence insensitivity (16). Although trait impulsivity has been positively related to irregular condom use in young men (17), as well as greater use of CUR tactics (4), the effects of state impulsivity on CUR has not been examined. Because alcohol intoxication can temporarily increase impulsivity, and because greater impulsivity has been related to greater engagement in CUR, in the present study we examined state impulsivity as a potential mediator of alcohol's effect on CUR intentions.
Sexual aggression history
The first examinations of CUR risk factors focused specifically on the use of coercive or forceful tactics to avoid condom use. For example, Abbey and colleagues (18) asked male participants how justified they would feel in using a variety of coercive tactics to have unprotected sex with a woman even though she desired to use a condom. Men who reported the distal risk factor of a history of sexual assault perpetration reported feeling significantly more justified in using coercive CUR tactics than men without a perpetration history. Other studies have also found a positive association between a history of sexual violence and forcing unprotected sex (19, 20); however, there has been little examination of the role of sexual aggression background as a predictor of non-forceful CUR tactics. The present study addresses this knowledge gap by examining the direct relationship between sexual aggression history and CUR intentions. Moreover, because sexual aggression perpetration is associated with greater impulsivity (21–24), we also examined state impulsivity as a potential mediator of the direct association between sexual aggression history and CUR intentions.
Study Overview and Hypotheses
The present study used alcohol administration methods and a sexual risk analogue to examine the direct and indirect effects of alcohol intoxication and sexual aggression history on men's CUR intentions. Utilizing a path analysis framework, the hypothesized model (see Figure 1) proposed that intoxicated men would report greater CUR intentions than sober men (Hypothesis 1) and that more severe histories of sexual aggression perpetration would be associated with greater CUR intentions (Hypothesis 2). We also expected that alcohol intoxication (Hypothesis 3) and sexual aggression history severity (Hypothesis 4) would each predict stronger feelings of impulsivity during the sexual risk analogue. Greater feelings of impulsivity were expected to predict greater CUR intentions directly (Hypothesis 5) as well as indirectly through increases in CUR attitudes (Hypothesis 6) and CUR self-efficacy (Hypothesis 7).
Figure 1.
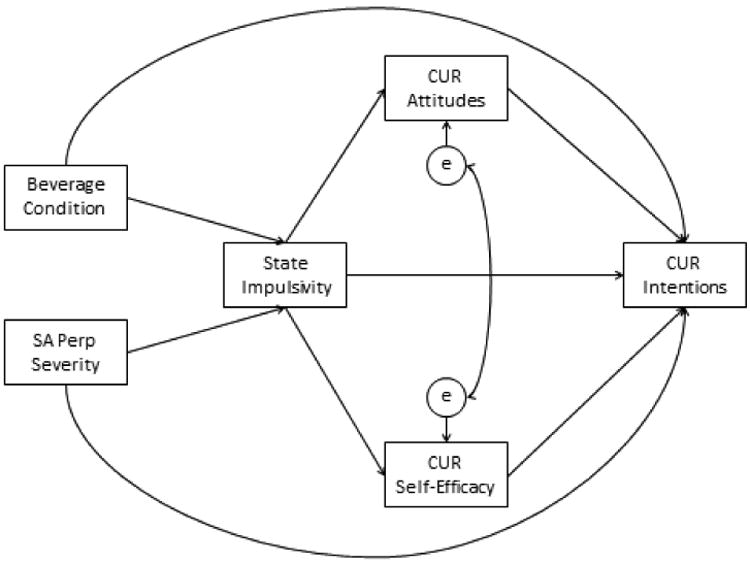
Hypothesized Model.
Note. SA Perp Severity = Sexual Aggression Perpetration Severity. CUR = Condom Use Resistance. All paths were hypothesized to have a positive association.
Method
Participants
We recruited 321 single male non-problem drinkers through print (e.g., newspaper and fliers) and online advertisements placed in locations and media outlets targeted to younger audiences. Advertisements solicited single male drinkers of all ethnicities, aged 21 to 30, to participate in a study of male-female social interactions. Interested men called the laboratory and male research assistants (RA) described the study and screened the callers for eligibility. Inclusion criteria included: 1) being a man between 21 and 30 years old; 2) being interested in sexual activity with women; 3) having at least one experience of vaginal or anal intercourse without a condom in the past year; and 4) being a non-problem drinker. Due to the requirements of the alcohol administration laboratory protocols in the experimental phase of the study, callers were excluded on the basis of: a) being under the legal drinking age; b) having medical conditions or taking prescription medications that were contraindicated with alcohol use; and/or c) having a history of negative reactions to alcohol or problem drinking (25).
The average age of participants was 25.5 (SD=3.5). The majority of the sample self-identified as Caucasian (76.4%); 7.8% self-identified as African American/Black; 8.1% identified as Asian/Pacific Islander; 6.5% as Hispanic/Latino; 0.7% as Native American; and 15.8% as multiracial or other. This was a predominantly well-educated sample with the majority of participants (82.1%) reporting at least some college education, and 33.8% reporting full- or part-time student status. Full- or part-time employment status was reported by 49.7%. The majority of participants (71.6%) reported a yearly income of $40,999 or below (47.6%, $20,999 or below).
Procedures
All study procedures and materials were approved by the University Human Subjects Division. Eligible and interested participants were scheduled for a laboratory session and informed of the following previsit requirements: a) not driving to the laboratory; b) not consuming a caloric beverage or food within 3 hours before the appointment; c) not consuming alcohol or using recreational or over-the-counter drugs within 24 hours before their appointment; and d) bringing a photographic form of identification.
Upon participants' arrival, a male RA checked compliance with previsit requirements. Participants were also given an alcohol breath test to ensure that their blood alcohol content (BAC) was 0.0%. Participants were escorted to a private office where they were guided through the process of informed consent. The RA then left them alone in a private room to complete a series of demographic and background measures on the computer.
Experimental procedures
Following the background measures, participants were randomly assigned to one of four beverage conditions: a) an alcohol dose (.41 ml ethanol per pound of body weight) intended to yield a peak BAC of 0.04%; b) an alcohol dose (.82 ml ethanol per pound of body weight) intended to yield a peak BAC of 0.08%; c) a control condition in which participants were given no alcohol and were informed as such; and d) a placebo condition in which participants were told they would be receiving the .04% dose, but in actuality received no alcohol (26). Alcoholic beverages consisted of one part 100-proof vodka to three parts orange juice.
Procedures for the placebo manipulation followed those recommended by Rohsenow and Marlatt (27). Beverages for the placebo condition contained flattened tonic water in place of vodka. The cups for the placebo condition were misted with vodka near the rim of the cup and had a squirt of vodka and lime added to the beverage to increase the fidelity of the placebo manipulation. Placebo participants who inquired about their BAC were given false feedback (told their BAC was 0.025% and rising) to enhance the manipulation. Participants were instructed to pace their beverage consumption evenly over 9 minutes. Control participants consumed a volume of orange juice that was equivalent to the total volume of beverage that they would have received in the alcohol condition to which they were yoked (explained below).
Alcohol intoxication limb (either ascending or descending levels of intoxication) has been shown to differentially affect cognitive and behavioral performance (e.g., 28). Thus we ensured that the sexual risk analogue and related assessments were completed on the ascending limb or at peak by testing participant BAC every 4 minutes until they reached a criterion BAC of ≥ 0.02% for participants in the 0.04% alcohol condition and ≥ 0.05% for the participants in the 0.08% condition. At this point, the participants began reading the sexual risk analogue (described below). A yoked control design was used to reduce error variance in time between beverage consumption and experimental manipulation (29, 30). In this design, each participant assigned to either a control or placebo condition was yoked to a prior alcohol participant and was conducted through the experiment at the same time intervals as the alcohol participant to whom he had been yoked. Half of the control participants were yoked to low-dose alcohol participants; half were yoked to high-dose participants. Placebo condition participants were yoked only to alcohol participants in the 0.04% condition. Participants in the low dose condition had a mean BAC of .037% just prior to reading the sexual risk analogue, and their respective mean BAC after the completion of the dependent measures was .039%. Participants in the high dose condition had a mean BAC of .061% just prior to reading the sexual risk analogue, and their respective mean BAC after the completion of the dependent measures was .073%.
Sexual risk analogue
After reaching the criterion BAC, participants read a sexually explicit scenario of approximately 1,600 words that was at a 5th grade reading level. The story was generated by members of the research team and was pilot tested and modified in response to pilot participant feedback. The story was written in the second person, and participants were instructed to project themselves into the story as the protagonist at their current level of intoxication. In the story, the protagonist interacts with “Erica,” an attractive woman with whom he has previously had sex twice with inconsistent condom use. Erica has invited the protagonist to her apartment to watch a movie. While at Erica's apartment, the protagonist is offered either soda or a mixed drink of soda and alcohol, consistent with the beverage condition. Erica and the protagonist progress from kissing to removing their clothes. The protagonist and Erica realize that neither one of them has a condom, and the story pauses for assessment of dependent measures (Break 1). After completion of Break 1 dependent measures, the story continues with Erica and the protagonist continuing sexual activities, including genital fondling but not intercourse. During this section, the sexual risk analogue contained a risk rationale manipulation. Because previous research indicates that condom requests that are based on pregnancy risks rather than the risk of STIs are perceived as more acceptable, more persuasive, and less evocative of trust issues for the recipient of the request (31), participants were randomly assigned to read a story in which Erica states that while she wants to have sex with the protagonist, she is also concerned about either 1) the risks of pregnancy or 2) the risk of sexually transmitted infections (STIs). The story then pauses again for assessment of dependent measures (Break 2). The story continues with the female character again requesting condom use due to either pregnancy or STI concerns and includes a third assessment of dependent measures not included in these analyses. Participants reported that the scenario represented a realistic situation (“I feel that the scenario depicted a realistic situation that might happen to me”; 1= not at all; 7=very much; M = 5.84; SD = 1.56) and that they could easily project themselves into the scenario [“I found it easy to project myself into the scenario (i.e., imagine the scenario was happening to me)”; 1 = not at all; 7 = very much; M = 5.96; SD = 1.43].
Manipulation checks
Two manipulation checks were used to ensure the placebo manipulation was successful. Near the conclusion of the study, participants were asked how many drinks they had consumed and what their highest level of intoxication was on a scale from 1 (not at all intoxicated) to 7 (extremely intoxicated). If a participant indicated “0” drinks and an intoxication level of “1,” he was considered a placebo manipulation failure.
One item was administered to assess the risk rationale story manipulation. Participants were asked to select if the female character wanted to use condoms due to concerns about pregnancy or concerns about STIs. If a participant did not choose the correct answer for his assigned condition, he was considered a story condition manipulation failure.
Detoxing and debriefing
After completing the dependent measures, participants were debriefed, and paid $15 per hour. Participants who received alcohol were not debriefed or released until their BAC dropped to .03% or below. No additional manipulation failures were detected in the debriefing process.
Measures
Sexual aggression experiences
A modified version of the Sexual Experiences Survey (SES; 32) was used to assess prior perpetration of sexual aggression and/or coercion that occurred since the age of 14. Perpetration of unwanted sexual contact (fondling, kissing), attempted nonconsensual intercourse, completed nonconsensual intercourse, and other nonconsensual penetrative or oral sex were assessed for each of five different tactics: (1) overwhelming the woman with continual arguments or pressure; (2) telling her lies; (3) making her feel guilty or getting angry; (4) taking advantage of the woman when she was passed out or too intoxicated to consent; and (5) using or threatening to use physical force. Participants indicated the number of times that they did each of these combinations ranging from 0 (never) to 5 (5 or more times). A modified severity scoring method was utilized to include event frequency, severity of tactic used, and varied combinations of assault outcomes, yielding a possible maximum score of 63 (33). This scoring method accounts for multiple perpetrations through multiple tactics, thus allowing for a more comprehensive reflection of the perpetration severity of this sample (33).1
State impulsivity
State impulsivity was assessed at the second break in the story through a 5-item scale (α =.86) assessing various impulsive feelings “at this point in the story” (e.g., “impulsive”, “reckless”, “daring”) using 1 (not at all) to 7 (extremely) scales.
Condom use resistance tactics
Theory of Planned Behavior (TPB) components related to attitudes, self-efficacy, and intention to engage in condom use resistance (CUR) with Erica were all assessed at the second break in the scenario after Erica directly requested that they use a condom during intercourse. Three subscales were assessed: CUR Attitudes (5 items; α =.91), CUR Self-efficacy (3 items; α =.91), and CUR Intentions (14 items, α =.91). The CUR Attitudes and Self-efficacy scales were developed for the current study based on the extensive TPB literature (11, 34), while the CUR Intentions scale was developed from previous research on CUR tactics (4, 9). To assess CUR Attitudes, participants were given the stem “Having sex with Erica without a condom would be,” and then asked to indicate how bad vs. good, awful vs. nice, harmful vs. helpful, foolish vs. wise, and unpleasant vs. pleasant that behavior would be on 7-point scales ranging from -3 to 3. To assess CUR Self-Efficacy, participants responded to three items addressing their confidence in their ability to engage in unprotected sexual intercourse with Erica (e.g., “I have the ability to have sex with Erica without a condom if I want to”) on 7-point scales from 1 (strongly disagree) to 7 (strongly agree). CUR Intentions were measured with 14 items asking participants to rate their likelihood of employing different condom use resistance tactics to engage in unprotected sexual intercourse with Erica on scales ranging from 1 (very unlikely) to 7 (very likely). Sample items include “At this point in the situation, how likely are you to reassure Erica that you are ‘clean’ so that she will have sex without a condom” and “At this point in the situation, how likely are you to promise to have a relationship with Erica so she will have sex with you without a condom”. Items were averaged for each of the CUR scales.
Data Analytic Strategy
Path analysis was conducted with MPlus 6 (35) using maximum likelihood estimation with robust standard errors. We used the cutoff criteria for fit indices suggested by West, Taylor, and Wu (36) to conclude acceptable model fit: non-significant chi-squared statistic, SRMR < .08, TLI > .95, CFI > .95, and RMSEA < .06. We also examined modification indices to determine whether adding additional paths consistent with previous research and theory would improve model fit. All possible indirect pathways from alcohol to CUR intentions and from sexual aggression perpetration severity to CUR intentions were examined. We obtained bias-corrected bootstrap confidence intervals for the indirect effects using 1,000 bootstrap draws.
Results
Preliminary Analyses
Two subjects withdrew from the study prior to completion, and four failed experimental manipulation checks (two failed the beverage manipulation check; two failed the story condition manipulation check). Two participants responded “no answer” to the majority of study items, and two men were removed from the modeling analysis for having missing data on the sexual aggression (SA) perpetration variable, leaving a final sample of 311.
One-way ANOVAs revealed no significant differences across any of the variables in the model between the control and placebo conditions, nor did we find significant differences between the low dose and high dose conditions on any of the variables in the model (all p's > .69). Thus, we combined the control and placebo conditions (coded -1 = received no alcohol) and the low and high dose alcohol conditions (coded 1 = received alcohol). We also conducted a series of one-way ANOVAs with the scenario risk rationale condition (pregnancy excuse, STI excuse) predicting each of the process (state impulsivity, CUR attitudes, CUR self-efficacy) and outcome (CUR intentions) variables in the model, which revealed no significant associations (all p's > .23). To consider interactive effects with the other predictors in the model (beverage condition and SA perpetration history), we also conducted preliminary regression analyses (PROCESS model 3; 37) with the predictors risk rationale condition (coded: -1 = pregnancy excuse, 1 = STI excuse), beverage condition (coded as described above), SA perpetration history (centered), and all 2 and 3-way interactions as predictors of each variable in the model. The analyses revealed no main or interactive effects involving risk rationale condition, thus the scenario risk rationale condition was not included as a predictor in the model. The two-way interaction of beverage condition and SA perpetration history was also not significant, and thus was not included in the model (all p's > .06).
Table 1 contains means, standard deviations, and correlations for all variables in the model (Figure 1). The pattern of bivariate associations was consistent with the hypothesized model with the exception that alcohol condition was not associated with state impulsivity. Additionally, all variables met the distributional assumptions of normality reasonably well (no skew statistics greater than +/-1.96; 38) with the exception of CUR intentions. Thus, we conducted a natural log transform on this variable, which successfully reduced the skew.
Table 1. Correlations and Descriptive Statistics.
| 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|
| 1. Alc | -- | |||||
| 2. SA Perpetration Severity | .04 | -- | ||||
| 3. State Impulsivity | .07 | .19*** | -- | |||
| 4. CUR Attitudes | -.01 | .14* | .32*** | -- | ||
| 5. CUR Self-Efficacy | .06 | .17** | .29*** | .28*** | -- | |
| 6. CUR Intentions | .15** | .30*** | .53*** | .53*** | -- | |
|
| ||||||
| Actual Range | -- | 0-36 | 1-7 | -3-3 | 1-7 | 1-7 |
| Mean | -- | 6.67 | 3.66 | -.43 | 4.23 | 2.61 |
| SD | -- | 8.27 | 1.58 | 1.36 | 1.73 | 1.27 |
Note: Alc = beverage condition (coded -1 = no alc, 1 = alc). SA = sexual aggression. CUR = Condom Use Resistance. CUR intentions was natural log transformed to reduce skew; non-transformed range, mean, and standard deviation are presented to aid in interpretability.
p < .05,
p ≤ .01,
p ≤ .001.
Model Fit
The hypothesized model fit the data well and the modification indices did not suggest the addition of other paths, χ2(4) = 6.84, p = .14; SRMR = .03, TLI = .96, CFI = .99, RMSEA (90% CI) = .05 (.00, .11). As shown in Figure 2, all of the hypothesized direct associations (Hypotheses 1, 2, and 4-7) were significant and positive with the exception that beverage condition was not associated with state impulsivity (Hypothesis 3). The variables included in the model accounted for 4% of the variance in state impulsivity (R2 = .04, p = .06), 10% of the variance in CUR attitudes (R2 = .10, p < .01), 8% of the variance in CUR self-efficacy (R2 = .08, p < .01), and 50% of the variance in CUR intentions (R2 = .50, p < .001).
Figure 2.
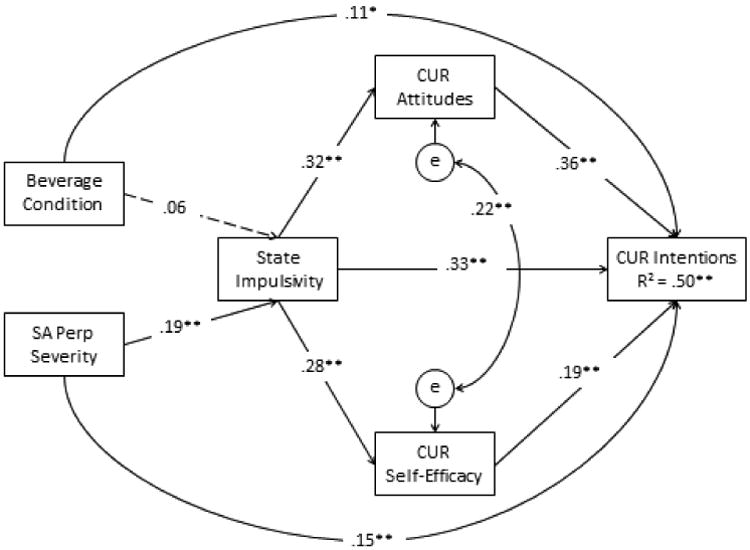
Final Path Model.
Note. SA Perp Severity = Sexual Aggression Perpetration Severity. CUR = Condom Use Resistance. Dotted line indicates the non-significant hypothesized path. *p < .01. **p < .001.
Indirect Effects
Refer to Table 2 for the indirect effects. Unexpectedly, all indirect paths from beverage condition to CUR intentions were not significant indicating that the effect of beverage condition on CUR intentions was direct only. However, consistent with predictions, all indirect paths from SA perpetration severity to CUR intentions were significant and positive indicating that SA perpetration severity had both direct and indirect effects on CUR intentions. Specifically, SA perpetration severity predicted higher levels of state impulsivity, which in turn predicted increased CUR intentions directly or via either CUR attitudes or CUR self-efficacy.
Table 2. Indirect Effects from Alcohol and Sexual Aggression to CUR Intentions.
| Indirect Paths | Unstandardized Estimate | 95% C.I. |
|---|---|---|
| Alc total effects | .07** | .024, .118 |
| Alc total indirect effects | .015 | -.012, .042 |
| Alc specific indirect effects | ||
| Alc to State impulsivity | .010 | -.008, .028 |
| Alc to State impulsivity to CUR attitudes | .003 | -.003, .010 |
| Alc to State impulsivity to CUR self-efficacy | .002 | -.001, .005 |
| SA perp severity total effects | .014*** | .010, .019 |
| SA perp severity total indirect effects | .005*** | .002, .009 |
| SA perp severity specific indirect effects | ||
| SA perp severity to State impulsivity | .004** | .001, .006 |
| SA perp severity to State impulsivity to CUR attitudes | .001** | .000, .002 |
| SA perp severity to State impulsivity to CUR self-efficacy | .001* | .000, .001 |
Note: C.I. = confidence interval. Alc = beverage condition (coded -1 no alc, 1 = alc). SA perp severity = Sexual Aggression Perpetration Severity. CUR = Condom Use Resistance. CUR intentions variable was natural log transformed to reduce skew.
p < .05,
p < .01,
p ≤ .001.
Discussion
Our findings indicate that men's intentions to resist condom use with a casual female sex partner are predicted by both distal and proximal risk factors. Specifically, 50% of the variance in CUR intentions was predicted in our final model. In support of our hypotheses, sexual aggression perpetration severity history predicted greater intentions to engage in CUR directly and indirectly via impulsivity and social-cognitive factors. Hypotheses regarding alcohol intoxication's role as a proximal risk factor were partially supported. Overall, results suggest that alcohol intoxication and sexual aggression history may increase CUR through different pathways. These findings expand the current literature by assessing the influence of distal and proximal predictors on men's CUR through a sexual risk analogue paradigm as well as through rigorous alcohol administration methods.
Consistent with hypotheses and previous research (Author Citation), alcohol directly increased men's intentions to resist using a condom with a female partner who requested condom use. This finding is consistent with other research regarding the direct effects of acute alcohol intoxication on sexual risk behaviors, such as intentions to have sex with a casual partner (39) and condom use intentions (13). Other studies (e.g., 40, 41) have suggested that acute alcohol intoxication may increase sexual risk likelihood through increased cognitive impairment, particularly through a phenomenon known as “alcohol myopia.” Alcohol myopia theory contends that the cognitive impairment effects of alcohol shifts individuals' attention away from more distant inhibiting cues (such as STI transmission risk) towards more salient impelling cues (such as sexual arousal), thereby shifting the decisional balance in favor of greater risk taking (42). Although alcohol's direct effect on increased CUR intentions is consistent with this theory, we did not directly assess alcohol myopia processes. Future work in this area could directly examine this potential mechanism of alcohol's effects on CUR. Moreover, because alcohol intoxication predicted increased intentions to engage in CUR, sexual risk reduction efforts should not only include a focus on CUR but should also address the role of alcohol in these risky sexual behaviors.
Consistent with other studies of alcohol's effects on sexual risk behaviors (e.g., 43), preliminary analyses revealed no significant placebo effects. Additionally, preliminary analyses did not demonstrate significant differences between the low (target BAC .04%) and high (target BAC .08%) alcohol dose conditions, suggesting that CUR intentions do not linearly increase as alcohol dosage increases. That noted, in the real world many individuals typically drink to higher intoxication levels than can be ethically achieved in an alcohol administration laboratory study; thus, future research could utilize reports of men's actual real-world drinking and CUR behavior to assess if alcohol dosage effects are detectable at higher levels of consumption. However, our findings do suggest that programs addressing CUR-related risk factors may not need to focus their content on dosage effects for typically moderate drinkers (i.e., BAC between .04% and .08%). Additionally, preliminary analyses did not demonstrate significant differences between the placebo and no alcohol conditions indicating that expectancy set did not influence CUR intentions in this study. However, we did not directly assess participants' alcohol expectancies regarding CUR. Future investigations should assess the potential influence of CUR-related alcohol expectancies on alcohol-involved CUR in order to determine if alcohol expectancies could serve as a useful intervention target regarding men's CUR.
Although we proposed that alcohol intoxication would indirectly increase CUR intentions through its effects on state impulsivity, our analyses did not support this hypothesis. Although previous research has demonstrated acute intoxication effects on proximal measures of impulsivity (e.g., 16), most of these studies involved behavioral measures of impulsivity rather than self-report measures of impulsive feelings. Moreover, studies examining the relationship of impulsivity to condom use and CUR have focused on self-reported trait impulsivity rather than self-reported state impulsivity. Future studies could continue to explore the role of impulsivity in men's CUR intentions by assessing state impulsivity through behavioral measures, as well as examining the potential moderating effects of trait impulsivity on alcohol intoxication.
Men's sexual aggression perpetration severity both directly and indirectly predicted greater CUR intentions. The findings support the growing literature regarding the connections between men's aggressive behaviors and sexual risk (44, 45) as well as advance the field by demonstrating that sexual aggression perpetration severity is related to non-forceful CUR intentions in addition to forceful or coercive condom non-use (18). Because more severe perpetrators had greater CUR intentions, sexual risk prevention and intervention efforts could increase their impact by targeting their efforts towards men who report a history of sexual aggression perpetration. Moreover, our final model suggests potential intervention targets that could be useful for tailoring CUR-related interventions towards sexually aggressive men. For example, men with more severe sexual aggression histories reported greater in-the-moment feelings of impulsivity, which directly predicted greater CUR intentions. Teaching men to cope with these feelings through effective emotion regulation strategies could be a useful intervention strategy for reducing their resistance of condom use (17). More favorable CUR attitudes also predicted greater CUR intentions, indicating that intervention efforts focused on changing CUR-related attitudes by emphasizing the negative effects of CUR could be efficacious. Finally, CUR self-efficacy was also related to greater CUR intentions. While prevention efforts often focus on strengthening self-efficacy regarding sexually protective behaviors such as condom use (e.g., 46, 47), it may also be important for some individuals to decrease their self-efficacy regarding sexually risky behaviors. Interventions that seek to decrease men's CUR self-efficacy could simultaneously attempt to augment their self-efficacy regarding their ability to have protected sex that is pleasurable for both partners (48).
When considering these results as a whole, it is interesting that alcohol intoxication and sexual aggression history were both associated with stronger CUR intentions, yet through different pathways. Both variables were directly linked to greater CUR intentions; however, only sexual aggression history predicted the hypothesized mediators. Moreover, preliminary analyses indicated that alcohol intoxication did not moderate perpetration history's associations with CUR-related variables even though similar moderation effects have been found in studies in which sexual assault intentions are the measured outcome (49). Future research could explore these differences. For example, only perpetration history predicted state impulsivity. Because impulsivity is a multidimensional construct that can be assessed in multiple ways (14-16), it will be important to investigate whether the facet of impulsivity being assessed (e.g., response inhibition, trait/state impulsivity) and the method through which it is assessed (e.g., go/no go tasks, questionnaires) yield similar patterns of findings for alcohol intoxication and sexual aggression history. Because our results suggest that alcohol intoxication and sexual aggression background influence CUR outcomes in different ways and perhaps through different mechanisms, examinations of other possible moderators and mediators of these relationships may be informative. Moreover, the research on CUR is in relatively early stages; thus, continued research that delineates its key predictors and explores how CUR behavior may be similarly or differentially impacted by intervention and prevention strategies targeting these predictors and their underlying mechanisms is warranted.
Finally, although we experimentally manipulated the female partner's reason for desiring condom use (i.e., pregnancy or STI concerns), preliminary analyses indicated that this manipulation had no significant effects on model variables and was thus not included as a predictor. While some previous research suggests that condom use requests based on pregnancy concerns are more favorably received than those based on STI concerns (31), other research suggests a great deal of variability in young men regarding the importance of using condoms for these two reasons. In one focus group study (9), some men reported that avoiding STIs is their primary reason for condom use, while others reported that minimizing pregnancy risks is the main benefit of condom use. Perhaps individual differences in participants' a priori attitudes about the importance of using condoms relative to STI and pregnancy concerns obfuscated the effect of this manipulation. Future research could examine how men's pre-existing beliefs about the reasons to use condoms influence their sexual decision making in the moment and whether their partner's reasons for wanting to use a condom are more influential when other factors (e.g., relationship type) or variables (e.g., emotional responses) are considered.
Limitations and conclusions
One limitation of this study concerns the use of alcohol administration methods coupled with a sexual risk analogue. Although rigorous experimental methods such as these enable researchers to assess causal relationships, they can often lack ecological validity. Alcohol administration protocols are limited in their ability to utilize extremely high alcohol doses (i.e., above .10%), thus it is unknown if these findings would extend to situations involving greater alcohol consumption. Regarding the sexual risk analogue, participants reported that our sexual risk analogue was realistic and that they could easily project themselves into the depicted situation; however, there may have been important situational elements predictive of men's CUR that were not included in present analogue. Moreover, our measure of impulsivity only captured one of the several dimensions of impulsivity. Future research could address these limitations and complement the present findings by assessing other impulsivity constructs (e.g., response inhibition, trait impulsivity) as well as surveying men about their real-world CUR behaviors in order to include varied alcohol consumption amounts and patterns as well as other situational factors that may play a role in men's CUR.
Finally, our sample consisted of young men who have sex with women, are non-problem drinkers, and do not use condoms consistently. Given their alcohol consumption and irregular condom use, findings from this sample may not extend to men who consume alcohol in different patterns (e.g., lighter drinkers, problem drinkers) or to men who use condoms consistently. Future research could explore the distal and proximal predictors of CUR in other samples of men, particularly those who drink more heavily given alcohol's direct effect on CUR intentions in this study. Moreover, very little is known about CUR by men who have sex with men making this another important sample to investigate in future work.
Overall, the results of this study indicate that in casual sexual relationships, a man's history of sexual aggression and current intoxication may increase the likelihood of condom use resistance which could result in a greater degree of sexual risk. These findings underscore the relevance and importance of addressing alcohol and sexual aggression experiences in sexual risk prevention and intervention programs. The current study also extended the TPB and demonstrated that CUR attitudes and self-efficacy were important proximal predictors of men's CUR intentions. CUR attitudes and self-efficacy also served as a pathway by which men's history of sexual aggression increased CUR intentions, suggesting that these constructs could be targeted in intervention efforts aimed at reducing men's CUR behavior. Although additional research is needed, the current study contributes to the growing literature on young men's CUR and indicates that consideration of both distal and proximal CUR predictors may enhance the effectiveness of empirically-based sexual risk prevention and intervention efforts.
Acknowledgments
This research was supported by a grant to the first author from the National Institute of Alcohol Abuse and Alcoholism (R01-AA017608).
Footnotes
Author Note: Portions of this paper were presented at The NIAAA Workshop to Consider Next Steps in HIV Prevention Intervention Development, National Institute on Alcohol Abuse and Alcoholism, Bethesda, MD (February 2014).
Analyses were also conducted using the traditional coding scheme of “most severe assault perpetrated.” The pattern of results did not differ between the two SES scoring methods.
References
- 1.Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MCB, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013 Mar;40(3):187–93. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Atlanta: U.S. Department of Health and Human Services; 2014. 2013 Sexually Transmitted Diseases Surveillance [Internet] cited 2015 Jan 14. Available from: http://www.cdc.gov/std/stats13/default.htm. [Google Scholar]
- 3.Reece M, Herbenick D, Schick V, Sanders SA, Dodge B, Fortenberry JD. Condom use rates in a national probability sample of males and females ages 14 to 94 in the United States. J Sex Med. 2010 Oct;7(Suppl 5):266–76. doi: 10.1111/j.1743-6109.2010.02017.x. [DOI] [PubMed] [Google Scholar]
- 4.Davis KC, Stappenbeck CA, Norris J, George WH, Jacques-Tiura AJ, Schraufnagel TJ, et al. Young men's condom use resistance tactics: a latent profile analysis. J Sex Res. 2014;51(4):454–65. doi: 10.1080/00224499.2013.776660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bowleg L, Lucas KJ, Tschann JM. “The ball was always in his court”: An exploratory analysis of relationship scripts, sexual scripts, and condom use among African American women. Psychol Women Q. 2004;28(1):70–82. [Google Scholar]
- 6.Kennedy SB, Nolen S, Applewhite J, Waiter E. Urban African-American males' perceptions of condom use, gender and power, and HIV/STD prevention program. J Natl Med Assoc. 2007 Dec;99(12):1395–401. [PMC free article] [PubMed] [Google Scholar]
- 7.Teitelman AM, Tennille J, Bohinski JM, Jemmott LS, Jemmott JBI. Unwanted unprotected sex: Condom coercion by male partners and self-silencing of condom negotiation among adolescent girls. Adv Nurs Sci. 2011 Jul;34(3):243–59. doi: 10.1097/ANS.0b013e31822723a3. [DOI] [PubMed] [Google Scholar]
- 8.Measor L. Condom use: A culture of resistance. Sex Educ. 2006 Nov;6(4):393–402. [Google Scholar]
- 9.Davis KC, Schraufnagel TJ, Kajumulo KF, Gilmore AK, Norris J, George WH. A qualitative examination of men's condom use attitudes and resistance: “It”s just part of the game'. Arch Sex Behav. 2014 Apr;43(3):631–43. doi: 10.1007/s10508-013-0150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peasant C, Parra GR, Okwumabua TM. Condom Negotiation: Findings and Future Directions. J Sex Res. 2015;52(4):470–483. doi: 10.1080/00224499.2013.868861. [DOI] [PubMed] [Google Scholar]
- 11.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991 Dec;50(2):179–211. [Google Scholar]
- 12.Albarracín D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: a meta-analysis. Psychol Bull. 2001 Jan;127(1):142–61. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: systematic review and meta-analysis of experimental studies. Addict Abingdon Engl. 2012 Jan;107(1):51–9. doi: 10.1111/j.1360-0443.2011.03621.x. [DOI] [PubMed] [Google Scholar]
- 14.De Wit H. Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addict Biol. 2009 Jan;14(1):22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wingrove J, Bond AJ. Impulsivity: A state as well as trait variable. Does mood awareness explain low correlations between trait and behavioural measures of impulsivity? Personal Individ Differ. 1997 Mar;22(3):333–9. [Google Scholar]
- 16.Dougherty DM, Marsh-Richard DM, Hatzis ES, Nouvion SO, Mathias CW. A test of alcohol dose effects on multiple behavioral measures of impulsivity. Drug Alcohol Depend. 2008 Jul;96(1-2):111–20. doi: 10.1016/j.drugalcdep.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Derefinko KJ, Peters JR, Eisenlohr-Moul TA, Walsh EC, Adams ZW, Lynam DR. Relations between trait impulsivity, behavioral impulsivity, physiological arousal, and risky sexual behavior among young men. Arch Sex Behav. 2014 Aug;43(6):1149–58. doi: 10.1007/s10508-014-0327-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abbey A, Parkhill MR, Jacques-Tiura AJ, Saenz C. Alcohol's role in men's use of coercion to obtain unprotected sex. Subst Use Misuse. 2009;44(9-10):1329–48. doi: 10.1080/10826080902961419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Purdie MP, Abbey A, Jacques-Tiura AJ. Perpetrators of Intimate Partner Sexual Violence: Are There Unique Characteristics Associated With Making Partners Have Sex Without a Condom? Violence Women. 2010 Oct 1;16(10):1086–97. doi: 10.1177/1077801210382859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raj A, Santana MC, La Marche A, Amaro H, Cranston K, Silverman JG. Perpetration of intimate partner violence associated with sexual risk behaviors among young adult men. Am J Public Health. 2006 Oct;96(10):1873–8. doi: 10.2105/AJPH.2005.081554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lisak D, Roth S. Motivational factors in nonincarcerated sexually aggressive men. J Pers Soc Psychol. 1988 Nov;55(5):795–802. doi: 10.1037//0022-3514.55.5.795. [DOI] [PubMed] [Google Scholar]
- 22.Petty GM, Dawson B. Sexual aggression in normal men: Incidence, beliefs, and personality characteristics. Personal Individ Differ. 1989;10(3):355–62. [Google Scholar]
- 23.Spence JT, Losoff M, Robbins AS. Sexually aggressive tactics in dating relationships: Personality and attitudinal correlates. J Soc Clin Psychol. 1991;10(3):289–304. Fal. [Google Scholar]
- 24.Kingree JB, Thompson M. A comparison of risk factors for alcohol-involved and alcohol-uninvolved sexual aggression. J Int Viol. 2015;30(9):1478–1492. doi: 10.1177/0886260514540806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pokorny AD, Miller BA, Kaplan HB. The brief MAST: A shortened version of the Michigan Alcoholism Screening Test. Am J Psychiatry. 1972 Sep;129(3):342–5. doi: 10.1176/ajp.129.3.342. [DOI] [PubMed] [Google Scholar]
- 26.Friel PN, Logan BK, O'Malley D, Baer JS. Development of dosing guidelines for reaching selected target breath alcohol concentrations. J of Stud Alc. 1999;60(4):555–565. doi: 10.15288/jsa.1999.60.555. [DOI] [PubMed] [Google Scholar]
- 27.Rohsenow DJ, Marlatt GA. The balanced placebo design: methodological considerations. Addict Behav. 1981;6(2):107–22. doi: 10.1016/0306-4603(81)90003-4. [DOI] [PubMed] [Google Scholar]
- 28.Pihl RO, Paylan SS, Gentes-Hawn A, Hoaken PNS. Alcohol affects executive cognitive functioning differentially on the ascending versus descending limb of the blood alcohol concentration curve. Alcohol Clin Exp Res. 2003 May;27(5):773–9. doi: 10.1097/01.ALC.0000065434.92204.A1. [DOI] [PubMed] [Google Scholar]
- 29.Giancola PR, Zeichner A. The biphasic effects of alcohol on human physical aggression. J Abnorm Psychol. 1997 Nov;106(4):598–607. doi: 10.1037//0021-843x.106.4.598. [DOI] [PubMed] [Google Scholar]
- 30.Schacht RL, Stoner SA, George WH, Norris J. Idiographically determined versus standard absorption periods in alcohol administration studies. Alcohol Clin Exp Res. 2010 May;34(5):925–7. doi: 10.1111/j.1530-0277.2010.01165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bird ST, Harvey SM, Beckman LJ, Johnson CH. Getting your partner to use condoms: Interviews with men and women at risk of HIV/STDs. J Sex Res. 2001 Aug;38(3):233–40. [Google Scholar]
- 32.Abbey A, Parkhill MR, Koss MP. The effects of frame of reference on responses to questions about sexual assault victimization and perpetration. Psychol Women Q. 2005 Dec;29(4):364–73. doi: 10.1111/j.1471-6402.2005.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davis KC, Gilmore AK, Stappenbeck CA, Balsan MJ, George WH, Norris J. How to score the Sexual Experiences Survey? A comparison of nine methods. Psychol Violence. 2014 Oct;4(4):445–61. doi: 10.1037/a0037494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ajzen I. Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. J Appl Soc Psychol. 2002 Apr;32(4):665–83. [Google Scholar]
- 35.Muthén, Muthén . Mplus users guide. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- 36.West SG, Taylor AB, Wu W. Model fit and model selection in structural equation modeling. In: Hoyle RH, editor. Handbook of structural equation modeling. New York, NY, US: Guilford Press; 2012. pp. 209–31. [Google Scholar]
- 37.Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper] 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf.
- 38.Tabachnick BG, Fidell LS. Using Multivariate Statistics. Pearson. 2007:980. [Google Scholar]
- 39.Cho YH, Span SA. The effect of alcohol on sexual risk-taking among young men and women. Addict Behav. 2010 Aug;35(8):779–85. doi: 10.1016/j.addbeh.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 40.Davis KC, Hendershot CS, George WH, Norris J, Heiman JR. Alcohol's effects on sexual decision making: an integration of alcohol myopia and individual differences. J Stud Alcohol Drugs. 2007 Nov;68(6):843–51. doi: 10.15288/jsad.2007.68.843. [DOI] [PubMed] [Google Scholar]
- 41.MacDonald TK, Fong GT, Zanna MP, Martineau AM. Alcohol myopia and condom use: can alcohol intoxication be associated with more prudent behavior? J Pers Soc Psychol. 2000 Apr;78(4):605–19. doi: 10.1037//0022-3514.78.4.605. [DOI] [PubMed] [Google Scholar]
- 42.Steele CM, Josephs RA. Alcohol myopia. Its prized and dangerous effects. Am Psychol. 1990 Aug;45(8):921–33. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- 43.Purdie MP, Norris J, Davis KC, Zawacki T, Morrison DM, George WH, et al. The effects of acute alcohol intoxication, partner risk level, and general intention to have unprotected sex on women's sexual decision making with a new partner. Exp Clin Psychopharmacol. 2011 Oct;19(5):378–88. doi: 10.1037/a0024792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frye V, Ompad D, Chan C, Koblin B, Galea S, Vlahov D. Intimate partner violence perpetration and condom use-related factors: associations with heterosexual men's consistent condom use. AIDS Behav. 2011 Jan;15(1):153–62. doi: 10.1007/s10461-009-9659-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peterson ZD, Janssen E, Heiman JR. The association between sexual aggression and HIV risk behavior in heterosexual men. J Interpers Violence. 2010 Mar;25(3):538–56. doi: 10.1177/0886260509334414. [DOI] [PubMed] [Google Scholar]
- 46.Bandura A. Adolescent development from agentic perspective. In: Pajares F, Urdan TC, editors. Self-efficacy beliefs of adolescents. Greenwich, Conn.: IAP - Information Age Pub.; 2006. pp. 1–43. [Google Scholar]
- 47.Schwarzer R, Luszczynska A. Self-efficacy, adolescents' risk-taking behaviors, and health. In: Pajares F, Urdan TC, editors. Self-efficacy beliefs of adolescents. Greenwich, Conn.: IAP - Information Age Pub.; 2006. pp. 1–43. [Google Scholar]
- 48.Scott-Sheldon LAJ, Johnson BT. Eroticizing creates safer sex: a research synthesis. J Prim Prev. 2006 Nov;27(6):619–40. doi: 10.1007/s10935-006-0059-3. [DOI] [PubMed] [Google Scholar]
- 49.Abbey A, Wegner R, Woerner J, Pegram SE, Pierce J. Review of survey and experimental research that examined the relationship between alcohol consumption and men's sexual aggression perpetration. Trauma, Violence, & Abuse. 2014;15(4):265–282. doi: 10.1177/1524838014521031. [DOI] [PMC free article] [PubMed] [Google Scholar]


