Abstract
Rotator cuff tears (RCT) are prevalent in older individuals and may compound age-associated functional declines. Our purpose was to determine whether self-report measures of perceived functional ability are valid for older patients with RCT. Twenty five subjects participated (12M/13F; age=63.9±3.0 years); 13 with RCT and 12 controls (CON). Participants completed self-report measures of shoulder function (SST, ASES, WORC) and health-related quality of life (SF-36). Isometric joint moment and range of motion (ROM) were measured at the shoulder. Relationships among functional self-reports, and between these measures and joint moment and ROM were assessed; group differences for total and subcategory scores were evaluated. There were significant correlations among self-reports (rs=0.62–0.71, p≤0.02). For RCT subjects, ASES was associated with all joint moments except adduction (p≤0.02); SST, ASES, and WORC were associated with abduction and external rotation ROM (p≤0.04). For RCT subjects, SST and WORC were associated with SF-36 physical function subcategory scores (p≤0.05). The RCT group scored worse than CON on all functional self-reports (p<0.01) and WORC and ASES subcategories (p<0.01). In conclusion, SST, ASES, and WORC demonstrate utility and discriminant validity for older individuals by distinguishing those with RCT, but this work suggests prioritizing ASES given its stronger association with functional group strength.
Clinical Trials Registration Number: NCT#01459536
Keywords: self report, aged, rotator cuff, upper extremity, activities of daily living, strength, range of motion
1. Introduction
As the United States population grows older (National Institute on Aging, 2007), it is important to understand the functional implications of common musculoskeletal conditions that may impact older individuals’ ability to maintain independence. Rotator cuff tears (RCT) are a common musculoskeletal injury affecting older adults (Yamaguchi et al., 2006), with a prevalence of 26% for individuals aged 60–69 years, 46% for 70–79 years, and 50% for 80+ years (Yamamoto et al., 2010). Sarcopenia and decreased strength occur in healthy aging (Clark and Manini, 2010; Janssen et al., 2002), and may play a role in an individual’s ability to successfully perform activities of daily living (ADLs) (Katz et al., 1963). However, the physiological changes (muscle atrophy, decreased strength) associated with RCT may further diminish one’s ability to perform ADLs (Lin et al., 2008).
Self-report instruments have been developed to evaluate overall health and function of the shoulder and rotator cuff (Amstutz et al., 1981; Brophy et al., 2005; Constant and Murley, 1987; Heald et al., 1997; Hudak et al., 1996; Kirkley et al., 2003; Lippitt et al., 1993; Patel et al., 2007; Richards et al., 1994; Smith et al., 2012; Wright and Baumgarten, 2010). These measures assess a patient’s self-perceived functional status and can aid clinicians in the diagnosis and treatment decision-making process. Best practice suggests administration of several different self-report measures to obtain a broad assessment of the patient’s physical health and functional status (Smith et al., 2012; Wright and Baumgarten, 2010). Further, a more general health-related quality of life instrument, like the RAND 36-Item Short Form Health Survey (SF-36) (RAND; Stewart et al., 1992), should be acquired (Wright and Baumgarten, 2010) because it allows clinicians to examine unanticipated effects (Beaton and Richards, 1996; Patel et al., 2007) of a disease or treatment on physical function, which can be affected by both physical (e.g. reduced strength) and mental (e.g. depressed mood) aspects of a patient’s health (Patel et al., 2007).
Existing self-report instruments have been developed for and are traditionally used in younger cohorts (Hegedus et al., 2014). These instruments have not been specifically validated in a cohort of older adults, for whom ADL tasks are of utmost importance. Self-report instruments of shoulder function often query patients on tasks which have little or no relevance to older individuals (e.g. ability to throw a ball) and it is unclear if they are able to effectively discriminate between older adults with and without RCT (Hegedus et al., 2014). Understanding which, if any, existing self-report instruments of shoulder function are useful for clinicians treating an increasingly large number of older adults will allow clinicians to select appropriate self-report measures for their patients.
The purpose of this work was to evaluate the Simple Shoulder Test (SST) (Lippitt et al., 1993), the American Shoulder and Elbow Surgeons Shoulder Outcome Survey (ASES) (Richards et al., 1994), and the Western Ontario Rotator Cuff Index (WORC) (Kirkley et al., 2003) self-report instruments in a sample of older individuals with and without a RCT. We examined whether these self-report measures of shoulder function 1) were related to one another and with the SF-36 in this older cohort; 2) could distinguish between older adults with and without a RCT; and 3) were related to physical symptoms associated with RCT. We hypothesized that self-reported measures of shoulder function 1) would be associated with one another and with the SF-36; 2) could distinguish between older adults with and without a RCT; and 3) would be positively correlated with physical symptoms of RCT.
2. Methods
2.1 Study participants
We recruited 25 subjects; 13 with a RCT (6M/7F) and 12 healthy age- and gender-matched asymptomatic controls (CON) (6M/6F) (Table 1). All subjects provided written informed consent in accordance with the Wake Forest University Health Sciences Institutional Review Board, which approved this study. Patients with RCT were recruited from our institution’s orthopaedic clinic. Inclusion criteria included having at least a major thickness (>50% tendon thickness) supraspinatus tear, confirmed with magnetic resonance imaging. Patients were excluded if they had any prior shoulder surgery, concomitant pathology (e.g. severe osteoarthritis), or neurologic disorder. Asymptomatic control subjects with no history of shoulder pain or injury were recruited from the local community. They were further evaluated for a rotator cuff tear with a lateral Jobe’s test (Gillooly et al., 2010) (positive likelihood ratio=7.36) in which subjects abducted their arms to 90° in the scapular plane and maintained neutral shoulder rotation as manual resistance was applied.
Table 1.
Participant demographics. R = rotator cuff tear patient; C = control subject; F = female; M = male; N/A = not applicable.
| Subject | Age | Height (cm) | Body Mass (kg) | Dominant Arm | Injured Arm |
|---|---|---|---|---|---|
| RF01 | 64 | 162.6 | 58.5 | Right | Right |
| RF02 | 65 | 165.1 | 83.9 | Right | Right |
| RF03 | 65 | 149.9 | 53.5 | Right | Left |
| RF04 | 63 | 160 | 73.5 | Right | Right |
| RF05 | 60 | 180.3 | 122.5 | Right | Right |
| RF06 | 75 | 162.6 | 55.3 | Right | Right |
| RF07 | 65 | 162.6 | 65.8 | Right | Left |
| RM01 | 64 | 175.3 | 73 | Right | Left |
| RM02 | 61 | 167.6 | 83.9 | Right | Left |
| RM03 | 64 | 177.8 | 108 | Left | Left |
| RM04 | 64 | 182.9 | 88.5 | Right | Left |
| RM05 | 62 | 177.8 | 95.3 | Left | Left |
| RM06 | 66 | 168.9 | 87.1 | Right | Left |
|
| |||||
| CF01 | 64 | 152.4 | 74.8 | Left | N/A |
| CF02 | 63 | 172.7 | 54.4 | Right | N/A |
| CF03 | 67 | 172.7 | 70.8 | Right | N/A |
| CF04 | 65 | 162.6 | 65.8 | Right | N/A |
| CF05 | 60 | 157.5 | 79.4 | Right | N/A |
| CF06 | 64 | 160 | 60.3 | Right | N/A |
| CM01 | 64 | 172.7 | 70.3 | Right | N/A |
| CM02 | 61 | 177.8 | 99.8 | Right | N/A |
| CM03 | 64 | 182.9 | 86.2 | Right | N/A |
| CM04 | 62 | 172.7 | 73.5 | Right | N/A |
| CM05 | 61 | 175.3 | 70.3 | Right | N/A |
| CM06 | 66 | 182.9 | 83.9 | Right | N/A |
|
| |||||
| Rotator cuff tear mean±SD | 64.5±3.6 | 168.7±9.6 | 80.7±20.5 | ||
| Control mean±SD | 63.4±2.1 | 170.2±9.9 | 74.1±12.1 | ||
2.2 Self-report questionnaires
To reduce treatment effect, data were collected from each RCT participant at baseline. Each subject completed three self-report instruments of shoulder function, including 2 region-specific measures (SST, ASES) and a disease-specific measure (WORC), and one self-report measure of health-related quality of life (SF-36). These instruments were chosen because previous studies report that each has demonstrated validity in younger cohorts (Brazier et al., 1992; Godfrey et al., 2007; Kirkley et al., 2003; Michener et al., 2002; Schmidt et al., 2014), they spanned a broad range of subcategories (Table 2), and they did not require any assistance from a physician.
Table 2.
Characteristics of the SST, ASES, WORC, and SF-36. ICF classifications were reported in Roe et al., 2013.
| Questionnaire | Type | Number of Questions | Format of questions | Categories assessed | ICF Classifications |
|---|---|---|---|---|---|
| SST | Shoulder- specific self- report measure of function | 12 | Yes/No |
|
|
| ASES | Shoulder- specific self- report measure of function | 12 | Visual analog scale; Ordinal scale |
|
|
| WORC | Rotator cuff- specific self- report measure of function | 21 | Visual analog scale |
|
|
| SF-36 | Health-related quality of life | 36 | Likert scale |
|
|
2.3 Strength assessments
We collected measures of maximal voluntary isometric joint moment and active, pain-free range of motion (ROM) at the shoulder. These parameters are reduced in RCT patients (McCabe et al., 2005). Strength and ROM were measured <1 week from completion of the self-report instruments. Joint moments were assessed for the 3 shoulder degrees of freedom using a Biodex dynamometer (Biodex Medical Systems, Shirley, NY) (Table 3). For all tests, subjects were seated with the torso restrained. Standardized verbal encouragement was given to motivate maximal performance. Three 5sec trials were collected with 60sec of rest between trials and 2min of rest between tests. The maximum moment maintained for at least 0.5sec was determined with a custom Matlab (Rev. 2012b, The MathWorks, Natick, MA) program (Holzbaur et al., 2007). The maximum moment achieved across all trials for each functional group was considered the maximum moment variable for analyses.
Table 3.
Testing postures used to assess maximal voluntary isometric joint moment and active, pain-free range of motion.
| Isometric joint moment | ||
|---|---|---|
| Abduction/Adduction | Flexion/Extension | Internal/External Rotation |
| Humerus abducted 30° in the coronal plane Elbow braced in extension Wrist braced in neutral |
Humerus forward flexed 30° in the sagittal plane Elbow braced in extension Wrist braced in 90° pronation |
Humerus abducted 30° in the coronal plane Elbow flexed 90°, restrained with an elastic bandage wrap Wrist braced in neutral |
| Active, pain-free range of motion | ||
|---|---|---|
| Abduction | Flexion/Extension | Internal/External Rotation |
| Humerus in neutral in the sagittal plane Elbow fully extended Wrist in neutral |
Humerus in neutral in the sagittal plane Elbow fully extended Wrist in neutral |
Humerus abducted 30° in the coronal plane Elbow flexed 90° Wrist in neutral |
2.4 Range of motion assessments
Active, pain-free ROM was measured using a goniometer with subjects standing. Subjects were instructed to move their arm in each direction as far as they could without any pain and not bend the torso. Measurements were taken for abduction, flexion/extension, and internal/external rotation (Table 3).
2.4 Statistical analysis
Descriptive statistics were used to summarize participant demographics (Table 1). To test the first hypothesis, the relationships between self-reported functional ability and health-related quality of life were evaluated. Partial Spearman correlations controlling for group were used to evaluate relationships between SST, ASES, and WORC scores and the SF-36 physical function and pain subcategory scores, since previous studies report that these categories are consistently lower for patients with musculoskeletal injuries (Picavet and Hoeymans, 2004). No total score is calculated for the SF-36 (Patel et al., 2007). Sensitivity analyses were repeated using only the RCT group to determine the consistency of estimated effects within the group.
To test the second hypothesis, we used one-way ANOVA to determine whether self-report measures could distinguish between individuals with and without a RCT. Differences between groups were tested for each self-report measure and subcategory score for ASES, WORC, and SF-36. SST only evaluates functional ability, so no subgroup analyses were performed.
To evaluate the third hypothesis, we used partial Spearman correlations controlling for group to separately evaluate associations between self-report scores and joint moment and ROM measurements for subjects in the RCT and CON groups. Sensitivity analyses were repeated to determine the consistency of estimated effects within the RCT group. All statistical analyses were performed using SAS software (version 9.3, Cary, NC), with significance set at p≤0.05. No Type I error corrections were made due to the exploratory nature of these analyses.
3. Results
3.1 Relationships among self-report questionnaires
Associations among SST, ASES, and WORC were significant for analyses with all subjects (all p<0.01) and with the RCT group only (all p≤0.02) (Table 4; Supplement 1). There were also significant correlations between self-report measures of shoulder function and the SF-36. The SF-36 physical function score was correlated with SST (p<0.01) and WORC (p=0.04) scores for analyses including all subjects. For the RCT group only, SST (p=0.04) and WORC (p=0.05) were significantly correlated with the physical function score while ASES was not (p=0.22). There was only a significant association between the ASES and SF-36 pain category when all subjects were evaluated (p=0.01). No correlations were significant when evaluating only the RCT group.
Table 4.
Spearman correlations (rs), corresponding p-values, and lower and upper limits of the 95% confidence interval (CI) for all subjects and rotator cuff tear subjects for SST, ASES, WORC, and SF-36 pain and physical function categories.
| All subjects (N=25) | Rotator cuff tear subjects (N=13) | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| SST | ASES | WORC | SST | ASES | WORC | |
|
| ||||||
| ASES | rs=0.71 (p<0.01)* CI=0.42, 0.86 |
- | - | rs=0.71 (p=0.01)* CI=0.23, 0.90 |
- | - |
|
| ||||||
| WORC | rs=−0.62 (p<0.01)* CI=-0.82, −0.28 |
rs=−0.70 (p<0.01)* CI=−0.86, −0.40 |
- | rs=−0.66 (p=0.02)* CI=−0.88, −0.14 |
rs=−0.63 (p=0.02)* CI=−0.87, −0.09 |
- |
|
| ||||||
| SF-36 Pain | rs=0.31 (p=0.14) CI=−0.11, 0.63 |
rs=0.51 (p=0.01)* CI=0.13, 0.76 |
rs=−0.29 (p=0.18) CI=−0.61, 0.14 |
rs=0.11 (p=0.71) CI=−0.47, 0.62 |
rs=0.47 (p=0.11) CI=−0.13, 0.80 |
rs=−0.02 (p=0.94) CI=−0.57, 0.54 |
|
| ||||||
| SF-36 Physical Function | rs=0.62 (p<0.01)* CI=0.28, 0.82 |
rs=0.40 (p=0.05) CI=−0.01, 0.69 |
rs=−0.42 (p=0.04)* CI=−0.70, −0.01 |
rs=0.59 (p=0.04)* CI=0.03, 0.85 |
rs=0.37 (p=0.22) CI=−0.24, 0.76 |
rs=−0.56 (p=0.05)* CI=−0.84, 0.01 |
indicates statistical significance.
3.2 Self-report questionnaire scores between subject groups
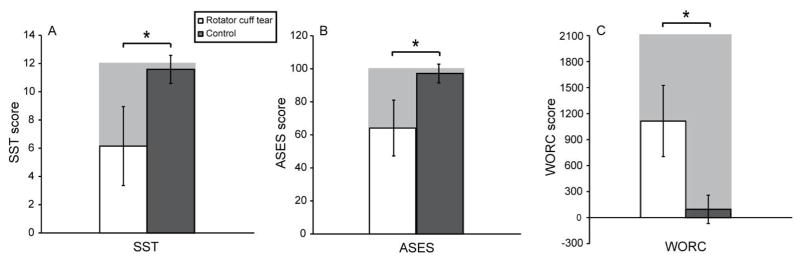
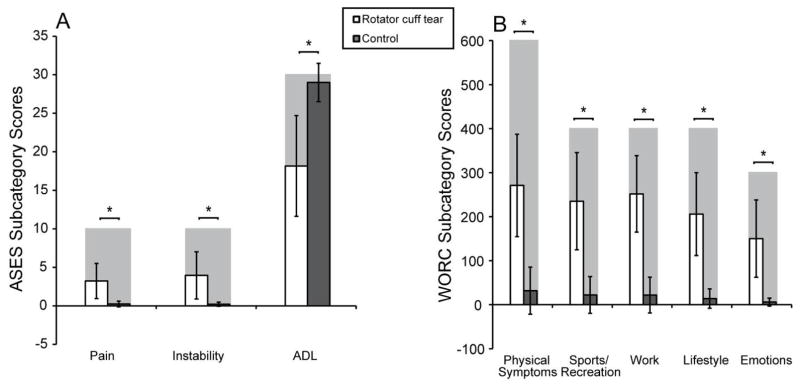
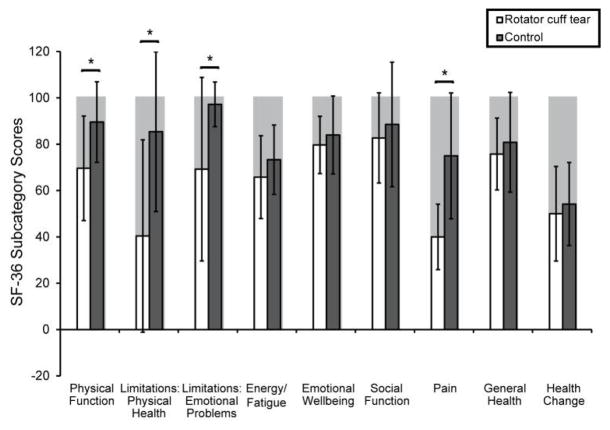
There were significant differences between RCT and CON groups for all self-report measures of shoulder function (all p<0.01, Figure 1). Further analysis of ASES and WORC subcategories showed that RCT participants had significantly worse scores than CON (p<0.01) (Figure 2). Likewise, the RCT group had worse scores than CON on the SF-36 sub-scales for physical function (p=0.02), limitations due to physical health (p=0.01), limitations due to emotional problems (p=0.03), and pain (p<0.01) (Figure 3).
Figure 1.
Mean±SD self-report measures of shoulder function for rotator cuff tear (white) and control (gray) groups. Maximum scores indicating best (SST, ASES) or worst (WORC) outcome are indicated by gray bars in the background. Rotator cuff tear group had worse scores than controls for (A) SST (p<0.01); (B) ASES (p<0.01); and (C) WORC (p<0.01). * indicates statistical significance. Note: standard deviations from this cohort are reported; it is not possible to obtain a score larger than what is indicated by the shaded gray bars in the background.
Figure 2.
Mean±SD for ASES and WORC subcategories for rotator cuff tear (white) and control (gray) groups. Shaded bars in background indicate the best (ASES: ADL) or worst (ASES: pain, instability; WORC: all categories) score. (A) Rotator cuff tear group had significantly worse ASES category scores for pain (p<0.01), instability (p<0.01), and ADL (p<0.01); (B) Rotator cuff tear group had significantly worse scores on all WORC categories (all p<0.01); * indicates statistical significance. Note: standard deviations from this cohort are reported; it is not possible to obtain a score larger than what is indicated by the shaded gray bars in the background.
Figure 3.
Mean±SD for each subcategory score for the SF-36 for rotator cuff tear (white) and control (gray) groups. Shaded bars in background indicate the best score. The rotator cuff tear group had worse scores on all categories than controls, with significantly worse scores on the physical function (p=0.02), limitations due to physical health (p=0.01), limitations due to emotional problems (p=0.03), and pain categories (p<0.01). Note: standard deviations from this cohort are reported; it is not possible to obtain a score larger than what is indicated by the shaded gray bars in the background.
3.3 Relationships between self-report questionnaires and physical symptoms
Significant positive correlations were seen between ASES and SST instruments and abduction, flexion, and internal and external rotation joint moments (all p≤0.05, Table 5; Supplement 2) when all subjects were evaluated. ASES (p=0.01) was also associated with extension joint moment. Evaluating only RCT subjects, we saw significant correlations between ASES and all strength measures except adduction (p≤0.02), and between SST and abduction (p=0.04) and flexion (p=0.01) joint moments.
Table 5.
Spearman correlations (rs), corresponding p-values, and lower and upper limits of the 95% confidence interval (CI) for comparisons between SST, ASES, and WORC total scores and abduction, adduction, flexion, extension, internal rotation, and external rotation joint moment (Nm).
| All subjects (N=25)
|
||||||
|---|---|---|---|---|---|---|
| Abduction joint moment | Adduction joint moment | Flexion joint moment | Extension joint moment | Internal rotation joint moment | External rotation joint moment | |
|
| ||||||
| SST | rs=0.44 (p=0.03)* CI=0.03, 0.71 |
rs=0.38 (p=0.07) CI=−0.04, 0.67 |
rs=0.53 (p=0.01)* CI=0.15, 0.76 |
rs=0.38 (p=0.06) CI=−0.03, 0.68 |
rs=0.41 (p=0.05)* CI=−0.00, 0.69 |
rs=0.56 (p<0.01)* CI=0.18, 0.78 |
|
| ||||||
| ASES | rs=0.43 (p=0.04)* CI=0.02, 0.70 |
rs=0.35 (p=0.09) CI=−0.06, 0.66 |
rs=0.45 (p=0.03)* CI=0.04, 0.72 |
rs=0.52 (p=0.01)* CI=0.14, 0.76 |
rs=0.42 (p=0.04)* CI=0.01, 0.70 |
rs=0.52 (p=0.01)* CI=0.14, 0.76 |
|
| ||||||
| WORC | rs=−0.18 (p=0.41) CI=−0.54, 0.25 |
rs=−0.15 (p=0.47) CI=−0.52, 0.27 |
rs=−0.26 (p=0.22) CI=−0.60, 0.17 |
rs=−0.26 (p=0.23) CI=−0.59, 0.17 |
rs=−0.14 (p=0.51) CI=−0.51, 0.28 |
rs=−0.29 (p=0.17) CI=−0.61, 0.14 |
| Rotator cuff tear subjects (N=13)
|
||||||
|---|---|---|---|---|---|---|
| Abduction joint moment | Adduction joint moment | Flexion joint moment | Extension joint moment | Internal rotation joint moment | External rotation joint moment | |
|
| ||||||
| SST | rs=0.58 (p=0.04)* CI=0.01, 0.85 |
rs=0.08 (p=0.79) CI=−0.50, 0.60 |
rs=0.67 (p=0.01)* CI=0.16, 0.89 |
rs=0.40 (p=0.17) CI=−0.21, 0.77 |
rs=0.49 (p=0.09) CI=−0.10, 0.81 |
rs=0.43 (p=0.14) CI=−0.18, 0.79 |
|
| ||||||
| ASES | rs=0.63 (p=0.02)* CI=0.10, 0.87 |
rs=0.30 (p=0.32) CI=−0.31, 0.73 |
rs=0.72 (p=0.01)* CI=0.25, 0.90 |
rs=0.74 (p<0.01)* CI=0.29, 0.91 |
rs=0.68 (p=0.01)* CI=0.17, 0.89 |
rs=0.62 (p=0.02)* CI=0.08, 0.87 |
|
| ||||||
| WORC | rs=−0.17 (p=0.59) CI=−0.65, 0.43 |
rs=−0.01 (p=0.99) CI=−0.55, 0.55 |
rs=−0.42 (p=0.15) CI=−0.78, 0.18 |
rs=−0.23 (p=0.45) CI=−0.69, 0.38 |
rs=−0.15 (p=0.63) CI=−0.64, 0.44 |
rs=−0.16 (p=0.60) CI=−0.65, 0.43 |
indicates statistical significance.
With regard to ROM (Table 6; Supplement 3), for analyses evaluating all subjects, the ASES was associated with abduction (p=0.04), flexion (p=0.01), and internal rotation (p=0.05) ROM, SST was associated with abduction (p=0.01) and internal rotation (p=0.01) ROM, and WORC was associated with abduction (p=0.02) ROM. Analyses with the RCT group only demonstrated significant correlations between SST, ASES, and WORC scores and abduction and external rotation ROM (all p≤0.04). SST and ASES scores were also associated with flexion ROM (p≤0.01).
Table 6.
Spearman correlations (rs), corresponding p-values, and lower and upper limits of the 95% confidence interval (CI) for comparisons between SST, ASES, and WORC total scores and abduction, flexion, extension, internal rotation, and external rotation range of motion (ROM) (degrees).
| All subjects (N=25)
|
|||||
|---|---|---|---|---|---|
| Abduction ROM | Flexion ROM | Extension ROM | Internal rotation ROM | External rotation ROM | |
|
| |||||
| SST | rs=0.53 (p=0.01)* CI=0.15, 0.77 |
rs=0.36 (p=0.08) CI=−0.06, 0.66 |
rs=0.18 (p=0.40) CI=−0.25, 0.54 |
rs=0.53 (p=0.01)* CI=0.15, 0.77 |
rs=0.34 (p=0.10) CI=−0.08, 0.65 |
|
| |||||
| ASES | rs=0.43 (p=0.04)* CI=0.02, 0.71 |
rs=0.51 (p=0.01)* CI=0.13, 0.75 |
rs=0.08 (p=0.70) CI=−0.33, 0.47 |
rs=0.41 (p=0.05)* CI=−0.00, 0.69 |
rs=0.32 (p=0.13) CI=−0.11, 0.63 |
|
| |||||
| WORC | rs=−0.45 (p=0.02)* CI=−0.72, −0.06 |
rs=−0.21 (p=0.33) CI=−0.56, 0.22 |
rs=0.26 (p=0.22) CI=−0.17, 0.60 |
rs=−0.39 (p=0.06) CI=−0.68, 0.02 |
rs=−0.34 (p=0.10) CI=−0.65, 0.08 |
| Rotator cuff tear subjects (N=13)
|
|||||
|---|---|---|---|---|---|
| Abduction ROM | Flexion ROM | Extension ROM | Internal rotation ROM | External rotation ROM | |
|
| |||||
| SST | rs=0.84 (p<0.01)* CI=0.52, 0.95 |
rs=0.66 (p=0.01)* CI=0.15, 0.88 |
rs=−0.00 (p=0.99) CI=−0.55, 0.55 |
rs=0.34 (p=0.25) CI=−0.27, 0.74 |
rs=0.79 (p<0.01)* CI=0.39, 0.93 |
|
| |||||
| ASES | rs=0.82 (p<0.01)* CI=0.46, 0.94 |
rs=0.81 (p<0.01)* CI=0.44, 0.94 |
rs=−0.06 (p=0.84) CI=−0.59, 0.51 |
rs=0.13 (p=0.67) CI=−0.46, 0.63 |
rs=0.58 (p=0.04)* CI=0.02, 0.85 |
|
| |||||
| WORC | rs=−0.72 (p=0.01)* CI=−0.90, −0.25 |
rs=−0.39 (p=0.19) CI=−0.77, 0.22 |
rs=0.40 (p=0.17) CI=−0.21, 0.77 |
rs=−0.34 (p=0.25) CI=−0.75, 0.27 |
rs=−0.68 (p=0.01)* CI=−0.89, −0.18 |
indicates statistical significance.
4. Discussion
We evaluated the SST, ASES, and WORC in a cohort of older subjects with and without a RCT, an age group for which there has not been specific validation of these instruments. We found that these instruments can distinguish between groups in this older cohort, with RCT subjects reporting worse total and subcategory scores on the self-report measures of shoulder function. Significant correlations were seen between self-report measures of shoulder function and the SF-36 and these instruments were also associated with physical symptoms of a RCT.
4.1 Associations between self-report questionnaires
The pain and physical function categories of the SF-36 captured the reduced function assessed with the SST, ASES, and WORC instruments, confirming part of our first hypothesis. These results are consistent with previous studies reporting associations between the SF-36 and musculoskeletal injuries (Gartsman et al., 1998; Patel et al., 2007; Picavet and Hoeymans, 2004; Smith et al., 2000), where pain and physical function category scores were consistently lower (Picavet and Hoeymans, 2004). Patients with RCT have previously demonstrated reductions in SF-36 sub-scores (Smith et al., 2000). However, when we analyzed only the RCT group, there were no significant associations between pain and self-reported shoulder function, which is contrary to reports where associations were observed from subjects with lower extremity arthritis and joint replacement (Stratford and Kennedy, 2006; Terwee et al., 2006). In our study, 10 of the 13 RCT subjects scored a 40 out of a possible 100 on the SF-36 pain category. The pain category score is determined by the average of only 2 questions. It is possible that the SF-36 does not include enough pain-associated questions to discriminate among patients experiencing some level of pain, or that pain is a greater determinant of self-reported function in the lower limb than in the upper limb (Patel et al., 2007; Terwee et al., 2006). The SF-36 is a validated measure that demonstrated utility in the cohort evaluated in this study, as well as in prior rotator cuff tear participants (Gartsman et al., 1998), but it should not be relied on exclusively (Gartsman et al., 1998; Patel et al., 2007; Shapiro et al., 1996). Use of a disease-specific measure in addition to the SF-36 provides more specific information and clinically-relevant functional limitations (Gartsman et al., 1998; Patel et al., 2007; Shapiro et al., 1996; Wright and Baumgarten, 2010).
The ASES, SST, and WORC instruments are intended to assess how a shoulder injury may change physical function. When we evaluated all subjects together, we saw moderate-to-strong relationships among SST, ASES, and WORC scores, and moderate associations between these measures and SF-36 physical function score, using the interpretation described by Taylor (1990), in which 0.36≤r≤0.67 is considered a moderate correlation and 0.68≤r≤1.0 is a strong correlation. Results of this study support the notion that region- and disease-specific measures have stronger correlations with one another than with health-related quality of life measures, like the SF-36, because they are intended to evaluate functional ability (Beaton and Richards, 1996). Similarly, the results of analyses for the RCT group demonstrated stronger correlations among SST, ASES, and WORC, than those correlations between the shoulder self-report instruments and the SF-36 physical function category. This may be a consequence of the SF-36 focusing more on lower limb function than upper limb function (Patel et al., 2007), thus being less sensitive to functional changes experienced by individuals with a RCT. Beaton and Richards (1996) and Michener et al. (2002) reported high correlations between ASES scores and the SF-36 physical function score in studies on younger cohorts, but we did not identify significant correlations for this older cohort. Godfrey et al. (2007) did not find a significant association between SST and the physical function component of the SF-12 for a sub-analysis of 14 patients aged >60 with a rotator cuff injury. However, consistent with our results, they reported a significant relationship among SST and ASES. Associations between ASES and WORC scores (Holtby and Razmjou, 2005; Razmjou et al., 2006) and between SST and WORC scores (Getahun et al., 2000) have also been reported for cohorts including younger subjects. The significant correlations found in this study among SST, ASES, and WORC suggest that these assessments of perceived shoulder function perform as expected in this older cohort and confirm our first hypothesis.
4.2 Self-report questionnaires between subject groups
The SST, ASES, and WORC each successfully distinguished between RCT and CON groups, confirming our second hypothesis. Additionally, the subcategories of the ASES and WORC and those categories of the SF-36 relating to pain and function were able to distinguish between groups. The higher levels of pain and lower levels of function reported by the RCT group were captured by the ASES and SF-36 instruments. These results were expected for the RCT group because pain is the primary symptom in those who seek treatment (Itoi, 2013). However, it is not clear whether pain is the primary contributor to reduced function or a concurrent symptom. Some suggest that patients consider pain and function together (Roddey et al., 2000) and pain may contribute to strength or movement deficits (Hermans et al., 2013; Stratford and Kennedy, 2006). Further, bursal sided partial-thickness tears may be more painful for patients (Fukuda, 2000). Additional work is needed to elucidate the causative role of pain in functional ability for this group.
4.3 Self-report questionnaires and physical symptoms
Confirming the third hypothesis, the results of this study support the use of SST and ASES for assessment of shoulder function in older individuals based on their correlations with strength. However, within the RCT group, ASES performed better than SST. The ASES was the only questionnaire consistently associated with strength for upper limb functional groups when all subjects or only the RCT group were evaluated. This may indicate that the ASES can be used as a proxy measurement for strength-associated function for this age group. Therefore, in accordance with previous reports from recent reviews (Hegedus et al., 2014; Roe et al., 2013; Schmidt et al., 2014), we recommend use of ASES, particularly if resources are limited. Age-associated strength loss can have functional implications (Clark and Manini, 2010). Previous work has shown that isometric strength is a significant predictor of functional strength in older adults (Daly et al., 2013). Others have suggested that when strength falls below a minimum threshold, disability may occur (Rantanen, 2003). However, more work is needed to determine how the ASES is correlated to specific functional tasks requiring strength. The ASES and SST may be better than the WORC at distinguishing functional strength among RCT patients due to their significant associations with clinically-meaningful ROM measures. Our results for analyses with the RCT group corroborate previous work describing associations between flexion and abduction ROM and self-reported function for younger patients following rotator cuff repair (Gore et al., 1986). While range of motion is an easily measured physical attribute which is reduced following a rotator cuff tear (Bytomski and Black, 2006; McCabe et al., 2005), it is important to consider that many ADLs require motion in two or more degrees of freedom (e.g. hair combing requires abduction and external rotation) (Magermans et al., 2005). Likewise, ROM during functional tasks may differ from planar ROM measures because of the joint posture during task performance (Magermans et al., 2005). Some suggest that diminished motion may be the result of patients altering the ways in which they used their upper extremity or as a result of the aging process in the absence of any pathology (Gore et al., 1986).
4.4 Importance of physical performance measures
Patient function is approximated clinically before and after treatment through the use of self-report measures of function (Hegedus et al., 2014; Jette et al., 2009; Prince et al., 2008). While self-report instruments query patients regarding their perceived functional ability, physical performance measures require patients to perform specific tasks. Inclusion of a physical performance measure is recommended (Kennedy et al., 2002); self-reported measures and physical performance measures are frequently not well correlated because they assess different aspects of function, but together these measures provide a more comprehensive patient assessment (Hegedus et al., 2014; Kennedy et al., 2002; Prince et al., 2008). While a robust physical performance measure is currently lacking for this older adult clinical population, the FIT-HaNSA (MacDermid et al., 2007) has been suggested (Hegedus et al., 2014). However, more work is needed to determine a physical performance measure applicable to an older population with RCT (Hegedus et al., 2014).
4.4 Limitations
Limitations of this study include that a small cohort was evaluated; however, even with this sample we identified significant correlations and differences between groups. Our study was cross-sectional in design. Longitudinal studies are needed to establish test-retest reliability, responsiveness, and further validation for these self-report measures for an older population. Further work is needed to expand these results to include participants older than age 70 years. Asymptomatic subjects were used as a control group in this study. Although these individuals were screened with a modified Jobe’s test, no diagnostic imaging was performed, so it is possible that some subjects may have had an asymptomatic RCT. With the high prevalence of asymptomatic tears in the older adult population (Yamamoto et al., 2011), it is important that future studies also consider these patients. We did not explore whether SST, ASES, and WORC are sensitive to tear severity or different shoulder impairments in older individuals, but future studies should examine this.
4.5 Conclusions
We evaluated the SST, ASES, and WORC in a cohort of older adults with and without RCT. While each of the self-report measures of shoulder function distinguished between older patients with and without RCT, the SST and ASES performed better than the WORC. This finding is likely because the SST and ASES focus more on physical function and ADLs, which are more relevant to older individuals. Within the RCT group, ASES was significantly correlated with most measurements of strength and ROM, suggesting that it may be a better instrument to use for patients with a known RCT. While additional validation is needed for these instruments in an older adult cohort, we recommend use of the ASES in this population.
Supplementary Material
Acknowledgments
We would like to acknowledge the financial support received from the National Institute on Aging of the National Institutes of Health (#F31AG040921 (MEV)), the Wake Forest University Claude D. Pepper Older Americans Independence Center (#P30AG021332), and the National Science Foundation (#1405246 (KRS)), which allowed us to conduct this work. The design, collection, analysis, interpretation of data, and decision to submit the manuscript for publication is solely that of the authors.
Biographies

Meghan Vidt is a Postdoctoral Fellow in the Department of Kinesiology at the University of Waterloo. She received her BS in Biomedical Engineering from North Carolina State University in 2006 and her PhD in 2014 from the Virginia Tech – Wake Forest School of Biomedical Engineering and Sciences. Her current research interests include upper limb biomechanics, shoulder injury, rotator cuff tear, aging, musculoskeletal imaging, computational modeling, and human factors and ergonomics.

Anthony Santago II is currently a research assistant in the Department of Mechanical Engineering at North Carolina State University. He received his BS in Mechanical Engineering from North Carolina State University in 2008. His graduate work was in Biomedical Engineering within the Virginia Tech – Wake Forest School of Biomedical Engineering and Sciences, where he received his MS in 2010 and PhD in 2015. His research interests include aging, rotator cuff tears, materials testing, musculoskeletal imaging, and computational modeling.
Eric Hegedus is the founding Chair of the Doctor of Physical Therapy Department at High Point University. He received his BSBA from Bucknell University in 1985. In 1991 and 1998, he received his MPT and DPT degrees, respectively, from Slippery Rock University. He received his MHSc degree in Clinical Research from Duke University in 2006. His research and clinical interests include physical therapy of active patients of all ages, particularly in the orthopedic and sports settings. Academic interests also include collaborative, interdisciplinary research with clinical applications, lecturing at the national and international level, and teaching evidence-based examination and treatment for patients with shoulder pathology.

Anthony Marsh is a Professor in the Department of Health and Exercise Science at Wake Forest University. He received both his B.P.E. (Hons) degree in Exercise Science in 1986 and his M.Ed. degree in Exercise Science in 1989 from the University of Western Australia. In 1995 he received his PhD from Arizona State University in Exercise Science with a concentration in Biomechanics. His research interests include examination of the role of muscle strength, power, and balance in gait, physical function, and disability in older adults, methods to assess physical activity, physical function, and disability, and intervention strategies to improve physical function and reduce disability in older adults with chronic disease.

Christopher Tuohy is an Assistant Professor in Orthopaedics at Wake Forest Baptist Medical Center. He received his BS from the University of North Carolina Chapel Hill in 1993 and his MD from Wake Forest University in 2001. In 2002 he completed a General Surgery Internship at Albert Einstein Medical Center and completed his Residency in Orthopaedic Surgery in 2006 while at Albert Einstein Medical Center. He completed a Fellowship in Hand and Microvascular Surgery at Vanderbilt University School of Medicine in 2007 and a Shoulder and Elbow Fellowship at Thomas Jefferson University in 2008. He is certified by the American Board of Orthopaedic Surgery in Orthopaedic Surgery as well as in the Subspecialty in the Surgery of the Hand. Research and clinical interests include shoulder replacement, arthroscopy of the shoulder, elbow, and wrist, rotator cuff and shoulder instability, orthopaedics, and hand surgery.
Gary Poehling is a Professor of Orthopaedics at Wake Forest Baptist Medical Center. He completed his BS at Marquette University in 1964 and his MD at the Medical College of Wisconsin in 1968. Following his degree, he completed an Internship in Surgery at Duke University Hospital in 1969. He also completed four residencies, including a Residency in Surgery at Duke University Hospital in 1970, Residency in Orthopaedic Surgery at Duke University Hospital in 1974, Residency in Orthopaedic Surgery at Lenox Baker Childrens Hospital in 1975 and a Residency in Orthopaedic Surgery at Duke University Hospital in 1976. He is board certified by the American Board of Orthopaedic Surgery. Research and clinical interests include peripheral nerve repair, lower extremity trauma, arthroscopy of the shoulder, elbow, wrist, and knee, adolescent sports medicine, robotic partial knee resurfacing, arthroscipic surgery, orthopaedics, hand surgery, and sports medicine.
Michael Freehill is an assistant professor of orthopaedic surgery at Wake Forest University in Winstom-Salem, North Carolina. He received his bachelor’s degree in Chemistry from the University of San Diego. He was a member of the baseball team while in college and played at every level of the minor leagues with the California Angels and the Texas Rangers. After retiring from baseball, Dr. Freehill received his medical doctorate from Tulane University in New Orleans and performed his orthopaedic residency at Johns Hopkins University Hospital in Baltimore. As a Chief resident, Dr. Freehill received the Johns Hopkins University Department of Orthopaedic Surgery Resident Researcher Award. Secondary to his interest in the shoulder, he decided to pursue both a sports and shoulder fellowship. His sports medicine fellowship was completed at Stanford University followed by a shoulder fellowship at Harvard University, which also included time in France. Throughout residency and to date he has been involved in both coverage and research with the Baltimore Orioles organization and continues to study the overhead athlete. Dr. Freehill also acts as a team physician to the Wake Forest baseball team, the Winston-Salem Dash minor league baseball team, and Winston-Salem State University athletics.

Michael Miller is a Professor in the Department of Biostatistical Sciences at Wake Forest School of Medicine. He received his BA in mathematics from the College of Wooster in 1983, his MS in Biostatistics from the University of Cincinnati in 1985, and his PhD in Biostatistics from the University of Michigan in 1988. His statistical research interests include development of methods for analysis of clustered discrete observations and accounting for missing outcomes. Collaborative interests encompass the fields of aging, cognition and learning, diabetes, fitness and physical activity, neurosciences and behavior, and statistics and mathematics.
Katherine Saul is an Associate Professor in the Department of Mechanical and Aerospace Engineering at North Carolina State University. She received her Sc.B. in Engineering from Brown University in 2000 and both her MS and PhD degrees in Mechanical Engineering from Stanford University in 2002 and 2005, respectively. Her research interests include upper limb biomechanics, dynamics and neural control of the musculoskeletal system, orthopaedic rehabilitation, computational dynamic simulation of movement, and musculoskeletal imaging.
Footnotes
Conflict of Interest
MTF serves as a consultant for Smith and Nephew, although no financial remuneration was received related to the information from this study. CJT has an ownership interest in a medical device used for measuring tension in rotator cuff tendon repairs with research applications, however, development and testing of this device is outside the scope of the work presented in this manuscript. None of the other authors have any conflicts of interest to disclose related to the content of this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981 Mar-Apr;(155):7–20. [PubMed] [Google Scholar]
- Beaton DE, Richards RR. Measuring function of the shoulder. A cross-sectional comparison of five questionnaires. J Bone Joint Surg Am. 1996;78(6):882–90. doi: 10.2106/00004623-199606000-00011. [DOI] [PubMed] [Google Scholar]
- Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305(6846):160–4. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brophy RH, Beauvais RL, Jones EC, Cordasco FA, Marx RG. Measurement of shoulder activity level. Clin Orthop Relat Res. 2005 Oct;(439):101–8. doi: 10.1097/01.blo.0000173255.85016.1f. [DOI] [PubMed] [Google Scholar]
- Bytomski JR, Black D. Conservative treatment of rotator cuff injuries. J Surg Orthop Adv. 2006;15(3):126–31. [PubMed] [Google Scholar]
- Clark BC, Manini TM. Functional consequences of sarcopenia and dynapenia in the elderly. Curr Opin Clin Nutr Metab Care. 2010;13(3):271–6. doi: 10.1097/MCO.0b013e328337819e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987 Jan;(214):160–4. [PubMed] [Google Scholar]
- Daly M, Vidt ME, Eggebeen JD, Simpson WG, Miller ME, Marsh AP, et al. Upper extremity muscle volumes and functional strength after resistance training in older adults. J Aging Phys Act. 2013;21(2):186–207. doi: 10.1123/japa.21.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuda H. Partial-thickness rotator cuff tears: a modern view on Codman’s classic. J Shoulder Elbow Surg. 2000;9(2):163–8. [PubMed] [Google Scholar]
- Gartsman GM, Brinker MR, Khan M. Early effectiveness of arthroscopic repair for full- thickness tears of the rotator cuff: an outcome analysis. J Bone Joint Surg Am. 1998;80(1):33–40. [PubMed] [Google Scholar]
- Getahun TY, MacDermid JC, Patterson SD. Concurrent validity of patient rating scales in assessment of outcome after rotator cuff repair. J Musculoskelet Res. 2000;4(2):119–27. [Google Scholar]
- Gillooly JJ, Chidambaram R, Mok D. The lateral Jobe test: A more reliable method of diagnosing rotator cuff tears. Int J Shoulder Surg. 2010;4(2):41–3. doi: 10.4103/0973-6042.70822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher M. Reliability, validity, and responsiveness of the simple shoulder test: psychometric properties by age and injury type. J Shoulder Elbow Surg. 2007;16(3):260–7. doi: 10.1016/j.jse.2006.07.003. [DOI] [PubMed] [Google Scholar]
- Gore DR, Murray MP, Sepic SB, Gardner GM. Shoulder-muscle strength and range of motion following surgical repair of full-thickness rotator-cuff tears. J Bone Joint Surg Am. 1986;68(2):266–72. [PubMed] [Google Scholar]
- Heald SL, Riddle DL, Lamb RL. The shoulder pain and disability index: the construct validity and responsiveness of a region-specific disability measure. Phys Ther. 1997;77(10):1079–89. doi: 10.1093/ptj/77.10.1079. [DOI] [PubMed] [Google Scholar]
- Hegedus EJ, Vidt ME, Tarara DT. The best combination of physical performance and self- report measures to capture function in three patient groups. Phys Ther Rev. 2014;19(3):196–203. [Google Scholar]
- Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel DL, Bierma-Zeinstra SMA. Does this patient with shoulder pain have rotator cuff disease? The rational clinical examination systematic review. JAMA. 2013;310(8):837–47. doi: 10.1001/jama.2013.276187. [DOI] [PubMed] [Google Scholar]
- Holtby R, Razmjou H. Measurement properties of the Western Ontario rotator cuff outcome measure: a preliminary report. J Shoulder Elbow Surg. 2005;14(5):506–10. doi: 10.1016/j.jse.2005.02.017. [DOI] [PubMed] [Google Scholar]
- Holzbaur KR, Delp SL, Gold GE, Murray WM. Moment-generating capacity of upper limb muscles in healthy adults. J Biomech. 2007;40(11):2442–9. doi: 10.1016/j.jbiomech.2006.11.013. [DOI] [PubMed] [Google Scholar]
- Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–8. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Itoi E. Rotator cuff tear: physical examination and conservative treatment. J Orthop Sci. 2013;18(2):197–204. doi: 10.1007/s00776-012-0345-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50:889–96. doi: 10.1046/j.1532-5415.2002.50216.x. [DOI] [PubMed] [Google Scholar]
- Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of Standardized Outcome Measures in Physical Therapist Practice: Perceptions and Applications. Physical Therapy. 2009;89(2):125–35. doi: 10.2522/ptj.20080234. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of Illness in the Aged. The Index of Adl: A Standardized Measure of Biological and Psychosocial Function. JAMA. 1963;185(Sep 21):914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kennedy D, Stratford PW, Pagura SM, Walsh M, Woodhouse LJ. Comparison of gender and group differences in self-report and physical performance measures in total hip and knee arthroplasty candidates. J Arthroplasty. 2002;17(1):70–7. doi: 10.1054/arth.2002.29324. [DOI] [PubMed] [Google Scholar]
- Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: The Western Ontario Rotator Cuff Index. Clin J Sport Med. 2003;13(2):84–92. doi: 10.1097/00042752-200303000-00004. [DOI] [PubMed] [Google Scholar]
- Lin JC, Weintraub N, Aragaki DR. Nonsurgical treatment for rotator cuff injury in the elderly. J Am Med Dir Assoc. 2008;9(9):626–32. doi: 10.1016/j.jamda.2008.05.003. [DOI] [PubMed] [Google Scholar]
- Lippitt S, Harryman D, II, Matsen F., III . A Practical Tool for Evaluating Function: The Simple Shoulder Test. In: Matsen F III, Fu F, Hawkins R, editors. The Shoulder: A Balance of Mobility and Stability. Rosemont, IL: The American Academy of Orthopaedic Surgeons; 1993. pp. 545–59. [Google Scholar]
- MacDermid JC, Ghobrial M, Quirion KB, St-Amour M, Tsui T, Humphreys D, et al. Validation of a new test that assesses functional performance of the upper extremity and neck (FIT-HaNSA) in patients with shoulder pathology. BMC Musculoskelet Disord. 2007;8:42. doi: 10.1186/1471-2474-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magermans DJ, Chadwick EK, Veeger HE, van der Helm FC. Requirements for upper extremity motions during activities of daily living. Clin Biomech (Bristol, Avon) 2005;20(6):591–9. doi: 10.1016/j.clinbiomech.2005.02.006. [DOI] [PubMed] [Google Scholar]
- McCabe RA, Nicholas SJ, Montgomery KD, Finneran JJ, McHugh MP. The effect of rotator cuff tear size on shoulder strength and range of motion. J Orthop Sports Phys Ther. 2005;35(3):130–5. doi: 10.2519/jospt.2005.35.3.130. [DOI] [PubMed] [Google Scholar]
- Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587–94. doi: 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- National Institute on Aging NIH. Why Population Aging Matters: A Global Perspective. U.S. Department of Health and Human Services, U.S. Department of State; 2007. [Google Scholar]
- Patel AA, Donegan D, Albert T. The 36-item short form. J Am Acad Orthop Surg. 2007;15(2):126–34. doi: 10.5435/00124635-200702000-00007. [DOI] [PubMed] [Google Scholar]
- Picavet HS, Hoeymans N. Health related quality of life in multiple musculoskeletal diseases: SF-36 and EQ-5D in the DMC3 study. Ann Rheum Dis. 2004;63(6):723–9. doi: 10.1136/ard.2003.010769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phy. 2008:5. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RAND. Medical Outcomes Study: 36-Item Short Form Survey Instrument. Santa Monica, CA: RAND Health; [Google Scholar]
- Rantanen T. Muscle strength, disability and mortality. Scand J Med Sci Sports. 2003;13(1):3–8. doi: 10.1034/j.1600-0838.2003.00298.x. [DOI] [PubMed] [Google Scholar]
- Razmjou H, Bean A, van Osnabrugge V, MacDermid JC, Holtby R. Cross-sectional and longitudinal construct validity of two rotator cuff disease-specific outcome measures. BMC Musculoskelet Disord. 2006;7:26. doi: 10.1186/1471-2474-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347–52. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- Roddey TS, Olson SL, Cook KF, Gartsman GM, Hanten W. Comparison of the University of California-Los Angeles Shoulder Scale and the Simple Shoulder Test with the shoulder pain and disability index: single-administration reliability and validity. Phys Ther. 2000;80(8):759–68. [PubMed] [Google Scholar]
- Roe Y, Soberg HL, Bautz-Holter E, Ostensjo S. A systematic review of measures of shoulder pain and functioning using the International classification of functioning, disability and health (ICF) BMC Musculoskelet Disord. 2013;14:73. doi: 10.1186/1471-2474-14-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt S, Ferrer M, Gonzalez M, Gonzalez N, Valderas JM, Alonso J, et al. Evaluation of shoulder-specific patient-reported outcome measures: a systematic and standardized comparison of available evidence. J Shoulder Elbow Surg. 2014;23(3):434. doi: 10.1016/j.jse.2013.09.029. [DOI] [PubMed] [Google Scholar]
- Shapiro ET, Richmond JC, Rockett SE, McGrath MM, Donaldson WR. The use of a generic, patient-based health assessment (SF-36) for evaluation of patients with anterior cruciate ligament injuries. Am J Sports Med. 1996;24(2):196–200. doi: 10.1177/036354659602400214. [DOI] [PubMed] [Google Scholar]
- Smith KL, Harryman DT, 2nd, Antoniou J, Campbell B, Sidles JA, Matsen FA., 3rd A prospective, multipractice study of shoulder function and health status in patients with documented rotator cuff tears. J Shoulder Elbow Surg. 2000;9(5):395–402. doi: 10.1067/mse.2000.108962. [DOI] [PubMed] [Google Scholar]
- Smith MV, Calfee RP, Baumgarten KM, Brophy RH, Wright RW. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94(3):277–85. doi: 10.2106/JBJS.J.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart A, Shebourne C, Hays R. Summary and discussion of MOS measures. In: Stewart AL, Ware J, editors. Measuring functioning and well-being: the Medical Outcomes Study approach. Durham, NC: Duke University Press; 1992. pp. 345–71. [Google Scholar]
- Stratford PW, Kennedy DM. Performance measures were necessary to obtain a complete picture of osteoarthritic patients. J Clin Epidemiol. 2006;59(2):160–7. doi: 10.1016/j.jclinepi.2005.07.012. [DOI] [PubMed] [Google Scholar]
- Taylor R. Interpretation of the correlation coefficient: a basic review. J Diagn Med Sonog. 1990;6(1):35–9. [Google Scholar]
- Terwee CB, van der Slikke RM, van Lummel RC, Benink RJ, Meijers WG, de Vet HC. Self-reported physical functioning was more influenced by pain than performance-based physical functioning in knee-osteoarthritis patients. J Clin Epidemiol. 2006;59(7):724–31. doi: 10.1016/j.jclinepi.2005.11.019. [DOI] [PubMed] [Google Scholar]
- Wright RW, Baumgarten KM. Shoulder outcomes measures. J Am Acad Orthop Surg. 2010;18(7):436–44. doi: 10.5435/00124635-201007000-00006. [DOI] [PubMed] [Google Scholar]
- Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease - A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699–704. doi: 10.2106/JBJS.E.00835. [DOI] [PubMed] [Google Scholar]
- Yamamoto A, Takagishi K, Kobayashi T, Shitara H, Osawa T. Factors involved in the presence of symptoms associated with rotator cuff tears: a comparison of asymptomatic and symptomatic rotator cuff tears in the general population. J Shoulder Elbow Surg. 2011;20(7):1133–7. doi: 10.1016/j.jse.2011.01.011. [DOI] [PubMed] [Google Scholar]
- Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–20. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.