Abstract
Escherichia coli O104:H4-associated hemolytic uremic syndrome (HUS) is characterized by Shiga toxin-induced vascular damage. As indicated by recent studies, dysregulation of the angiopoietin (Angpt)/Tie2 ligand receptor system may be crucial for endothelial dysfunction in HUS. Early Angpt-2 levels quantified in 48 adult HUS patients were predictive for a complicated clinical course, in particular for need of hemodialysis and mechanical ventilation as well as occurrence of seizures. In vitro challenge of human umbilical vein endothelial cells with patients' sera indicated an injurious mediator role of Angpt-2 opening future perspectives for mitigating endothelial activation in HUS.
1. Introduction
Hemolytic uremic syndrome (HUS) is characterized by acute hemolytic anemia, thrombotic microangiopathy, and kidney injury often caused by intestinal infections with Shiga-like toxin-producing E. coli (STEC-HUS). STEC-HUS is a medical emergency with a mortality rate of 4% [1]. A significant proportion of patients suffer from complications such as bloody diarrhea, neurological symptoms up to generalized seizures, and acute kidney injury (AKI) or need for renal replacement therapy (RRT) [1]. Many patients with STEC-HUS show spontaneous remission and complete recovery within a few weeks. However, in some patients the disease progresses rapidly requiring best supportive treatment, intensive care, and interventional therapy. Definition of relevant prognostic parameters for early identification of high-risk patients remains a challenge for treating physicians. Instruments of risk evaluation such as prognostic biomarkers remain highly desirable.
Global endothelial damage of the microvasculature and subsequent organ failure is pathophysiological hallmark of STEC-HUS [2]. Some pathological details remain unidentified, while Shiga toxins are known to alter expression of chemokines, chemokine receptors, and molecules of cell adhesion, thereby increasing leucocyte recruitment [3]. In addition, platelets [4] and neutrophil granulocytes [5] are activated. Endothelial reactions include an increased release of tissue-factor [6] and activation of several pathways [7]. Concerning endothelial activation, we also focused on a potential involvement of angiopoietins.
Angiopoietin-1 (Angpt-1) and Angpt-2 are antagonistic ligands of the endothelial tyrosine kinase Tie2. The Angpt/Tie2 ligand receptor system is a nonredundant gatekeeper of endothelial activation and controls the endothelial phenotype during angiogenesis and inflammation. Angpt-1 is continuously released by pericytes and maintains endothelial quiescence. In contrast, Angpt-2 competitively inhibits binding of Angpt-1 to Tie2 and thereby disrupts protective Angpt-1 signalling, causing loss of vessel integrity, vascular leakage, and expression of inflammatory genes [8]. In a recent study published, the dysregulation of the Angpt/Tie2 system was associated with a diagnosis of STEC-HUS in children [9]. However, clinical and prognostic impact of this phenomenon still remains elusive, and no data is available assessing the role of circulating angiopoietins in adult STEC-HUS patients.
On a single centre basis, we analyzed Angpt-2 plasma levels in adult STEC-HUS patients during the largest reported outbreak of Escherichia coli O104:H4 in northern Germany from May till July 2011 [10, 11]. We aimed to determine early predictive factors for complications and outcome.
2. Materials and Methods
2.1. Patients and Study Design
Forty-eight patients with STEC-HUS treated in Hannover Medical School during the outbreak in 2011 were included in this study after obtaining written informed consents from the patients or their legal representatives. The study was performed in accordance with the declaration of Helsinki and approved by the Institutional Review Board at Hannover Medical School (number 1123-2011).
STEC-HUS was diagnosed when patients had EHEC and/or Shiga toxin-2 positive stools or history of bloody diarrhoea between May and July 2011 and fulfilled all of the following three criteria: (1) platelet count below 150/nL, (2) haemolytic anaemia with haemoglobin below the lower limit of normal, and (3) kidney injury as indicated by an increase of urea or creatinine [12]. All of the above patients fulfilled these criteria.
2.2. Blood Sampling and Quantification of Circulating Angpt-1 and Angpt-2
EDTA plasma samples for quantification of Angpt-1 and Angpt-2 were obtained for each patient on different time points (admission and day three after admission or referral to our tertiary care hospital), immediately centrifuged, divided into aliquots, and stored at −80°C. Plasma Angpt-1 and Angpt-2 were measured as described previously [13]. Plasma samples of controls were also anticoagulated with EDTA.
2.3. Endothelial Cell Culture
Passage 5 human umbilical vein endothelial cells (HUVECs) (Lonza, Basel, Switzerland) were cultured, treated, and blotted as described previously in detail [14].
In order to perform fluorescent immunocytochemistry HUVECs were grown to confluence on glass coverslips, fixed, permeabilized, and stained with an anti-VE-cadherin antibody and with phalloidin to visualize F-actin as described previously [15]. These experiments were each time done in duplication and the results were reproducible (data not shown).
Endothelial cells were incubated with EBM-2 containing 5% fetal bovine serum (FBS) to grow to a confluent monolayer. When the experiment was started the tissue culture medium was changed to EBM-2 containing 5% of patients' plasma.
2.4. Measurements of Tie2
Tie2 and phosphoTie2 (pTie2) were measured as described previously [16, 17]. Shortly, antibodies against pTie2 (Y992) (R&D systems, Minneapolis, MN) and Tie2 (C-20) (Santa Cruz Biotechnology, Heidelberg, Germany) were used. For immunoblotting, equal amounts of lysed protein were resolved on 0% polyacrylamide gel and transferred to polyvinylidene fluoride (PVDF) membranes (Merck Millipore, Darmstadt, Germany). Membranes were blocked for 1 hour at room temperature in 3% bovine serum albumin (BSA). All washing steps were carried out in TBST (20 mM Tris, 150 mM NaCl, and 0.1% Tween 20 (Merck)). Afterwards, membranes were incubated with anti-phosphotyrosine antibody (R&D systems) or anti-Tie2 antibody (Santa Cruz). Proteins were visualized by secondary antibodies conjugated to horseradish peroxidase (HRP) (Santa Cruz) and by enhanced chemiluminescence. An exemplary blot from HUVEC lysates stimulated plasma from our patients is shown in Supplemental Figure 1 in Supplementary Material available online at http://dx.doi.org/10.1155/2015/670248.
2.5. Statistical Analysis
Continuous variables are expressed as medians with corresponding 25th and 75th percentiles (Interquartile Range (IQR)) and compared by using the Mann-Whitney rank sum test. Correlations between variables were assessed by Spearman's correlation test or linear regression. Data analysis and figure preparation were performed using GraphPad Prism (GraphPad Prism Software Inc., San Diego, California, USA).
3. Results
3.1. Patients' Characteristics
Our STEC-HUS cohort contained 48 patients (73% female) with a median age of 45 (27–57) years. None had a history of chronic kidney disease. All patients developed haemolysis, thrombocytopenia, and moderate to severe inflammation (Table 1). Median admission creatinine was 259.5 (163–342) μmol/L and 43 patients (89.6%) suffered acute kidney injury (AKI) AKIN I or higher.
Table 1.
Characteristics, chemistry values, and clinical symptoms in 48 patients with STEC-HUS mediated by Escherichia coli O104:H4.
| Variable | Admission | Day 3 |
|---|---|---|
| Demographics | ||
| Number of patients (n, %) | 48 (100) | |
| Age (years, median (IQR)) | 45 (27–57) | |
| Female sex (n, %) | 35 (72.9) | |
| Positive test for Shiga toxin or EHEC (n, %) | 45 (93.8) | |
| Onset of diarrhea (median (IQR)) | 2 (1–4) | |
| Medical history (n, %) | ||
| Arterial hypertension | 11 (22.9) | |
| Diabetes mellitus | 2 (4.2) | |
| Coronary heart disease | 2 (4.2) | |
| Chronic kidney disease | 0 (0) | |
| Laboratory data (median (IQR)) | ||
| Creatinine (μmol/L) | 202 (120–335) | 264.5 (184.8–344) |
| eGFR (mL/min/1.73 m2) | 26 (15–51.5) | 20 (13–33) |
| LDH (U/L) | 1018 (749–1429) | 886 (651–1142.3) |
| Platelets (/nL) | 46 (32–64) | 52 (23–72) |
| Hemoglobin (g/dL) | 11.2 (9.8–12.4) | 9.2 (8.3–10.4) |
| Angiopoietin-1 [ng/mL] | 1.5 (0.7–2.1) | 1.36 (0.95–2.29) |
| Angiopoietin-2 [ng/mL] | 2.4 (2–3.2) | 2.6 (1.8–3.28) |
| Clinical data (n, %) | ||
| Complicated course | 32 (66.7) | |
| Need of RRT | 32 (66.7) | |
| Seizures | 10 (20.8) | |
| Need of mechanical ventilation | 9 (18.8) | |
3.2. Angiopoietin Levels
Compared to healthy control patients, we found significantly lower plasma levels of Angpt-1 in STEC-HUS patients (1.36 [0.95–2.29] versus 2.5 [1.5–3.4] ng/mL, p < 0.05) as well as significantly elevated Angpt-2 (2.6 [1.8–3.28] ng/mL versus 1.39 [0.91–1.64], p < 0.0001, resp.) on day 3 after admission.
3.3. Association of Angiopoietins with a Complicated Clinical Course of STEC-HUS
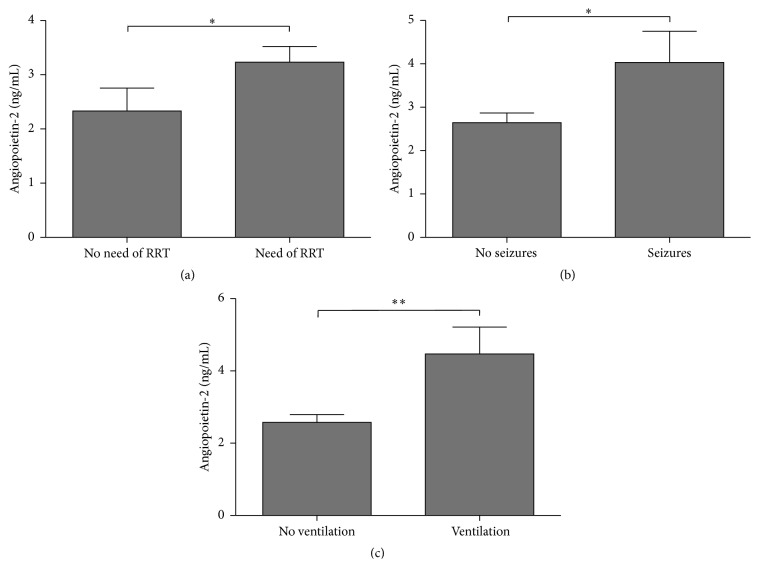
Focusing on STEC-HUS patients, we compared Angpt-1 and Angpt-2 levels within subcollectives following different outcome parameters. In particular, early plasma levels of angiopoietins were then compared between patients being either more severely or less afflicted by clinical symptoms and complications during the course. 32 patients required RRT (66.7%) a median of 5 (3–7.3) days after admission. Angpt-2 levels were significantly higher in patients requiring RRT compared to those without (2.9 [2.1–3.8] ng/mL versus 1.8 [1.2–2.8] ng/mL, p < 0.05) (Figure 1(a)). Angpt-2 levels on day three after admission discriminated between patients requiring RRT and those who did not with an area under the receiver operating characteristic curve (ROC) of 0.73 (95% confidence interval, 0.567–0.888; p = 0.01) (data not shown). Even on day of admission, Angpt-2 levels were associated with patients requiring RRT compared to those without (2.7 [2.2–3.6] ng/mL versus 1.9 [1.3–2.2] ng/mL, p < 0.001) (data not shown).
Figure 1.
Association of Angpt-2 levels on day three after admission with clinical complications. Boxplots showing associations between Angpt-2 levels and clinical outcomes ((a) need of RRT, (b) occurrence of seizures, and (c) need of mechanical ventilation); ∗ p < 0.05 and ∗∗ p < 0.01.
A median of 10.5 days after admission, 10 patients (20.8%) developed neurological complications ranging from mild cognitive disorder to generalized seizures. Again, early Angpt-2 on day three was significantly increased in those patients with seizures during the course compared to those without (3.1 [2.5–5.7] ng/mL versus 2.4 [1.7–3.1] ng/mL, p < 0.05) (Figure 1(b)). The corresponding ROC curve showed an area under the curve (AUC) of 0.71 (95% CI, 0.547–0.882, p = 0.04) (data not shown).
Mechanical ventilation was needed in 9 patients (18.8%). Angpt-2 on day three after admission was higher in patients requiring mechanical ventilation compared to those without (3.8 [2.7–5.9] ng/mL versus 2.3 [1.7–3.1] ng/mL, p < 0.001) (Figure 1(c)). The AUC of the corresponding ROC curves was 0.80 (95% CI, 0.652–0.952, p = 0.005) (data not shown).
Angpt-2 levels on admission did not correlate with occurrence of seizures and need of mechanical ventilation (data not shown). Angpt-2 levels on admission did not correlate with occurrence of seizures and need of mechanical ventilation (data not shown). On admission and day three, neither Angpt-1 nor the Angpt-2/Angpt-1 ratio was associated with need of RRT, mechanical ventilation, or occurrence of seizures (data not shown).
3.4. Disruption of Endothelial Integrity In Vitro Might Be Induced by Angpt-2
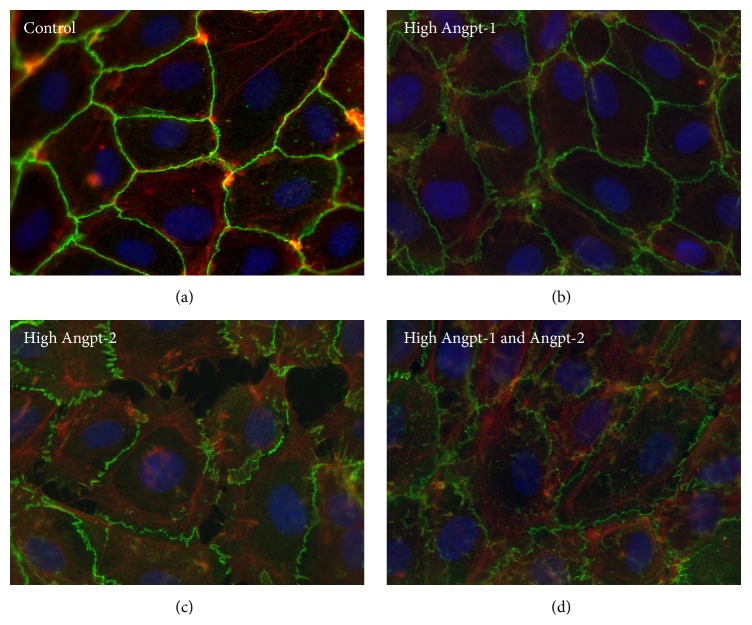
Parikh et al. have previously shown that, in sepsis, excess Angpt-2 diminishes Tie2 activation, which leads to paracellular gap formation driven by actin-myosin-based contraction of the cytoskeleton. Addition of Angpt-1 reverses this process [18]. To explore a potential mediator role of Angpt-1 and Angpt-2 we challenged endothelial cells with patients' plasma. We chose plasma from patients with high Angpt-2 levels (Angpt-2: 13.6 and 15.6 ng/mL) and challenged ECs to test the effect of higher Angpt-2 levels on the endothelial phenotype. Fluorescent immunocytochemistry for F-actin, a structural protein of the cytoskeleton, and VE-cadherin, a main constituent of endothelial adherens junctions, were performed. ECs treated with controls' plasma did not affect the confluent, adjacent cell monolayer with cortical actin architecture and the typical cell border localization of VE-cadherin. The same quiescent phenotype was observed using plasma from those HUS patients with a particularly high Angpt-1 concentration (Angpt-1: 15.5 and 17.2 ng/mL) (Figure 2). However, patients' plasma with a high Angpt-2 (Angpt-2: 13.6 and 15.6 ng/mL) disrupted the endothelial architecture, as depicted by increased actin stress fibers (ASF) and distinct endothelial gap formation. We then performed an experiment to test the effect of plasma with high Angpt-1 and Angpt-2 levels on the endothelial integrity. Exposure of patient's plasma with both high Angpt-1 and Angpt-2 levels (Angpt-1: 12.1 and 10.1 ng/mL, Angpt-2: 9.3 and 12.9 ng/mL, resp.) completely abolished the formation of ASF and interendothelial gaps.
Figure 2.
Fluorescent immunocytochemistry microscopy images showing immunofluorescence staining for F-actin (red) and VE-cadherin (green) performed on 100% confluent P5 HMVECs. Cells were treated with 5% prefiltered human EDTA plasma. EDTA plasma samples were collected from healthy controls (a), patients with high Angpt-1 (Angpt-1: 15.5 and 17.2 ng/mL) (b), high Angpt-2 (Angpt-2: 13.6 and 15.6 ng/mL) (c), and both high Angpt-1 and Angpt-2 (Angpt-1: 12.1 and 10.1 ng/mL, Angpt-2: 9.3 and 12.9 ng/mL, resp.) (d).
3.5. Phosphorylation of the Tie2 Receptor In Vitro
Ligation of Angpt-1 to Tie2 leads to its tyrosine phosphorylation, whereas Angpt-2 can antagonize Tie2 activation. To test whether or not gap formation is consistent with degree of Tie2 phosphorylation, we immunoblotted EC lysates for pTie2 after having been challenged with the Angpt-1 and Angpt-2 plasma constellations mentioned. The Angpt-1/Angpt-2 ratio was significantly associated with the phosphorylated Tie2/total Tie2 ratio (pTie2/tTie2) (r 2 = 0.27, p = 0.02) (Figure 3) indicating that these circulating molecules were indeed biologically active and that they target their canonical common receptor as a pathophysiological feature of HUS-associated endothelial dysfunction.
Figure 3.
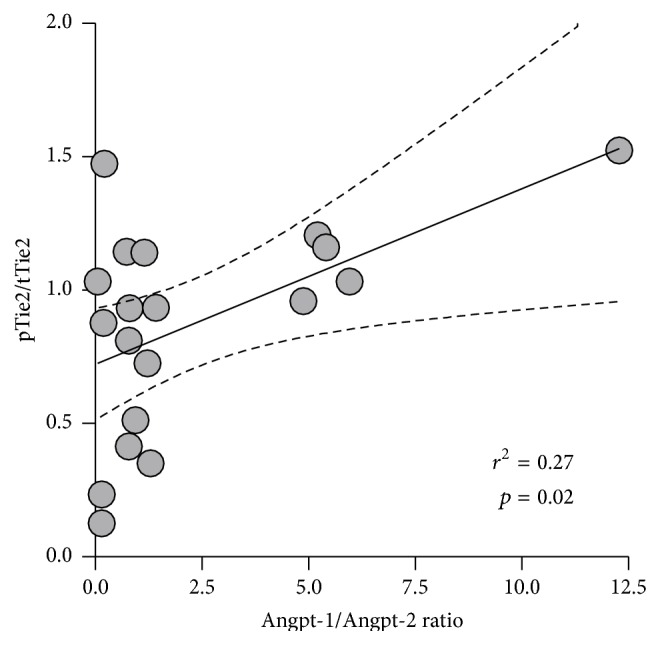
Linear regression shows the correlation between the Angpt-1/Angpt-2 ratio and the phosphorylated Tie2/total Tie2 ratio (pTie2/tTie2).
4. Discussion
Although STEC-HUS is categorized as a thrombotic microangiopathy, the incidences of thrombotic events or embolism were rare in the German outbreak 2011 [19]. Renal impairment seems to be also provoked by direct acute tubular damage even when thrombotic events are foreclosed by choice of mouse models [20]. In addition, the contribution of microvascular damage to clinical symptoms in STEC-HUS was indicated by prolonged T2 relaxation times in quantitative MRI scans of patients with neurological complications [21]. For the purpose of investigating mechanisms of endothelial damage and dysfunction in our patients, we correlated angiopoietin levels with outcome parameters.
From our data, we conclude that angiopoietins and Tie2 receptor alterations contribute to the early stage of STEC-HUS. It appears capable of indicating the severity of potential initial endothelial damage and thereby also a prognostic value for the onset of further complications. Affliction of endothelial integrity might be more important than thrombotic events, lightening a new aspect on this disease.
The endothelial integrity is supported by high Angpt-1 levels and impaired by elevated Angpt-2. Endothelial cells exposed to plasma with low Angpt-2 and high Angpt-1 levels showed intact cell-cell contacts and a cortical configuration of the cytoskeleton whereas exposure to high Angpt-2 without elevated Angpt-1 levels induced severe gap formation. In particular, the contribution of Angpt-2 is emphasized in our results, predicting the requirement of RRT and mechanical ventilation as well as occurrence of seizures at an early stage of the disease. As a Weibel-Palade body-stored protein, Angpt-2 can be rapidly released upon various stimuli including cytokines, thrombin, hypoxia, activated leucocytes, and platelets [22]. In children with E. coli O157:H7 mediated STEC-HUS early dysregulation of angiopoietins has been described recently [9]. During the pre-HUS phase, children exhibit prothrombotic coagulation abnormalities with evidence of early vascular injury preceding HUS with renal injury [23]. However, triggering factors inducing Angpt-2 release are still largely unknown, and clinical and prognostic impact of Angpt-2 plasma levels in STEC-HUS patients have been missing so far. A possible confounder of endothelial barrier disruption could be the presence of EDTA. By analogous confrontation of samples from patients and controls with EDTA, EDTA specific effects should be minimized from the observed differences.
Plasma levels of Angpt-1 showed no significant correlation with severity of affliction in our patients. Due to the sudden initiation of our study during the German outbreak 2011, Angpt-1 measurements could not be performed widely enough and thereby present a limitation to our study. As being expressed more constitutively by pericytes and vascular smooth muscle cells [22, 24], the adaption to a rapid increase of Angpt-2 is likely following delayed to clinical complications. Whether or not the administration of Angpt-1 to individuals afflicted by STEC-HUS could protect from endothelial, renal, or neurological impairment could be a valuable target of future studies. Other studies underlining diagnostic and prognostic potential of circulating Angpt-1 and Angpt-2 in various infectious diseases like malaria and/or sepsis with and without multiorgan dysfunction syndrome (MODS) [13, 18, 25, 26] indicate that detailed investigations of prognostic and therapeutic options for angiopoietins and the Tie2 receptor are worth considering intensely.
Our conclusions are that E. coli O104:H4 induced STEC-HUS is likely to be associated with early elevations of Angpt-2 and disruption of endothelial integrity. Early elevated plasma levels supply a valuable approach for prognostic parameters in patients. As STEC-HUS remains a rare disease predominantly affecting children, we encourage monitoring Angpt-2 levels for risk assessment.
In addition, we want to promote the concept of larger, prospective multicenter studies needed to confirm the reliability of prognostic values and possibilities of therapeutic intervention in the Angpt/Tie2 pathway.
Supplementary Material
Supportive Figure 1: Western blot from HUVEC lysates stimulated with plasma of STEC-HUS patients (lo = low Angpt-1/-2 concentration, hi = high Angpt-1/-2 concentration). The sample with high Angpt-2 and low Angpt-1 (left column) shows a low pTie2 / tTie2 ratio. In contrast, the sample with low Angpt-2 and high Angpt-1 (right column) shows a higher pTie2 / tTie2 ratio.
Acknowledgment
The authors are indebted to their colleagues at Medical School Hannover for intensive support in recruiting and monitoring the patients participating in this study.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors' Contribution
Alexander Lukasz and Jan Beneke contributed equally to the paper and are both considered first authors.
References
- 1.Kielstein J. T., Beutel G., Fleig S., et al. Best supportive care and therapeutic plasma exchange with or without eculizumab in Shiga-toxin-producing E. coli O104:H4 induced haemolytic-uraemic syndrome: an analysis of the German STEC-HUS registry. Nephrology Dialysis Transplantation. 2012;27(10):3807–3815. doi: 10.1093/ndt/gfs394. [DOI] [PubMed] [Google Scholar]
- 2.Barbour T., Johnson S., Cohney S., Hughes P. Thrombotic microangiopathy and associated renal disorders. Nephrology Dialysis Transplantation. 2012;27(7):2673–2685. doi: 10.1093/ndt/gfs279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noris M., Mescia F., Remuzzi G. STEC-HUS, atypical HUS and TTP are all diseases of complement activation. Nature Reviews Nephrology. 2012;8(11):622–633. doi: 10.1038/nrneph.2012.195. [DOI] [PubMed] [Google Scholar]
- 4.Karpman D., Papadopoulou D., Nilsson K., Sjögren A.-C., Carl Mikaelsson S. L. Platelet activation by Shiga toxin and circulatory factors as a pathogenetic mechanism in the hemolytic uremic syndrome. Blood. 2001;97(10):3100–3108. doi: 10.1182/blood.v97.10.3100. [DOI] [PubMed] [Google Scholar]
- 5.van Setten P. A., Monnens L. A. H., Verstraten R. G. G., van den Heuvel L. P. W. J., van Hinsbergh V. W. M. Effects of verocytotoxin-1 on nonadherent human monocytes: binding characteristics, protein synthesis, and induction of cytokine release. Blood. 1996;88(1):174–183. [PubMed] [Google Scholar]
- 6.Nestoridi E., Tsukurov O., Kushak R. I., Ingelfinger J. R., Grabowski E. F. Shiga toxin enhances functional tissue factor on human glomerular endothelial cells: implications for the pathophysiology of hemolytic uremic syndrome. Journal of Thrombosis and Haemostasis. 2005;3(4):752–762. doi: 10.1111/j.1538-7836.2005.01205.x. [DOI] [PubMed] [Google Scholar]
- 7.Karch H., Friedrich A. W., Gerber A., Zimmerhackl L. B., Schmidt M. A., Bielaszewska M. New aspects in the pathogenesis of enteropathic hemolytic uremic syndrome. Seminars in Thrombosis and Hemostasis. 2006;32(2):105–112. doi: 10.1055/s-2006-939766. [DOI] [PubMed] [Google Scholar]
- 8.van Meurs M., Kümpers P., Ligtenberg J. J. M., Meertens J. H. J. M., Molema G., Zijlstra J. G. Bench-to-bedside review: angiopoietin signalling in critical illness—a future target? Critical Care. 2009;13, article 207 doi: 10.1186/cc7153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Page A. V., Tarr P. I., Watkins S. L., et al. Dysregulation of angiopoietin 1 and 2 in Escherichia coli O157:H7 infection and the hemolytic-uremic syndrome. The Journal of Infectious Diseases. 2013;208(6):929–933. doi: 10.1093/infdis/jit268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frank C., Werber D., Cramer J. P., et al. Epidemic profile of Shiga-toxin-producing Escherichia coli O104:H4 outbreak in Germany. The New England Journal of Medicine. 2011;365(19):1771–1780. doi: 10.1056/nejmoa1106483. [DOI] [PubMed] [Google Scholar]
- 11.Rohde H., Qin J., Cui Y., et al. Open-source genomic analysis of Shiga-toxin-producing E. coli O104:H4. The New England Journal of Medicine. 2011;365(8):718–724. doi: 10.1056/nejmoa1107643. [DOI] [PubMed] [Google Scholar]
- 12.Menne J., Nitschke M., Stingele R., et al. Validation of treatment strategies for enterohaemorrhagic Escherichia coli O104:H4 induced haemolytic uraemic syndrome: case-control study. The British Medical Journal. 2012;345(7869) doi: 10.1136/bmj.e4565.e4565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lukasz A., Hellpap J., Horn R., et al. Circulating angiopoietin-1 and angiopoietin-2 in critically ill patients: development and clinical application of two new immunoassays. Critical Care. 2008;12, article R94 doi: 10.1186/cc6966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clajus C., Lukasz A., David S., et al. Angiopoietin-2 is a potential mediator of endothelial barrier dysfunction following cardiopulmonary bypass. Cytokine. 2012;60(2):352–359. doi: 10.1016/j.cyto.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.David S., Mukherjee A., Ghosh C. C., et al. Angiopoietin-2 may contribute to multiple organ dysfunction and death in sepsis. Critical Care Medicine. 2012;40(11):3034–3041. doi: 10.1097/CCM.0b013e31825fdc31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.David S., Ghosh C. C., Kümpers P., et al. Effects of a synthetic PEG-ylated Tie-2 agonist peptide on endotoxemic lung injury and mortality. American Journal of Physiology—Lung Cellular and Molecular Physiology. 2011;300(6):L851–L862. doi: 10.1152/ajplung.00459.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghosh C. C., Mukherjee A., David S., et al. Impaired function of the Tie-2 receptor contributes to vascular leakage and lethality in anthrax. Proceedings of the National Academy of Sciences of the United States of America. 2012;109:10024–10029. doi: 10.1073/pnas.1120755109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parikh S. M., Mammoto T., Schultz A., et al. Excess circulating angiopoietin-2 may contribute to pulmonary vascular leak in sepsis in humans. PLoS Medicine. 2006;3(3, article e46) doi: 10.1371/journal.pmed.0030046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Menne J., Beneke J. Clincial and laboratory consequences of platelet transfusion in Shigatoxin-mediated Hemolytic Uremic Syndrome. Personal Communication, 2015. [DOI] [PubMed]
- 20.Porubsky S., Federico G., Müthing J., et al. Direct acute tubular damage contributes to Shigatoxin-mediated kidney failure. The Journal of Pathology. 2014;234(1):120–133. doi: 10.1002/path.4388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weissenborn K., Bültmann E., Donnerstag F., et al. Quantitative MRI shows cerebral microstructural damage in hemolytic-uremic syndrome patients with severe neurological symptoms but no changes in conventional MRI. Neuroradiology. 2013;55(7):819–825. doi: 10.1007/s00234-013-1176-3. [DOI] [PubMed] [Google Scholar]
- 22.Fiedler U., Scharpfenecker M., Koidl S., et al. The Tie-2 ligand angiopoietin-2 is stored in and rapidly released upon stimulation from endothelial cell Weibel-Palade bodies. Blood. 2004;103(11):4150–4156. doi: 10.1182/blood-2003-10-3685. [DOI] [PubMed] [Google Scholar]
- 23.Chandler W. L., Jelacic S., Boster D. R., et al. Prothrombotic coagulation abnormalities preceding the hemolytic-uremic syndrome. The New England Journal of Medicine. 2002;346(1):23–32. doi: 10.1056/nejmoa011033. [DOI] [PubMed] [Google Scholar]
- 24.Wakui S., Yokoo K., Muto T., et al. Localization of Ang-1, -2, Tie-2, and VEGF expression at endothelial-pericyte interdigitation in rat angiogenesis. Laboratory Investigation. 2006;86(11):1172–1184. doi: 10.1038/labinvest.3700476. [DOI] [PubMed] [Google Scholar]
- 25.Lovegrove F. E., Tangpukdee N., Opoka R. O., et al. Serum angiopoietin-1 and -2 levels discriminate cerebral malaria from uncomplicated malaria and predict clinical outcome in African children. PLoS ONE. 2009;4(3) doi: 10.1371/journal.pone.0004912.e4912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Page A. V., Liles W. C. Biomarkers of endothelial activation/dysfunction in infectious diseases. Virulence. 2013;4(6):507–516. doi: 10.4161/viru.24530. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supportive Figure 1: Western blot from HUVEC lysates stimulated with plasma of STEC-HUS patients (lo = low Angpt-1/-2 concentration, hi = high Angpt-1/-2 concentration). The sample with high Angpt-2 and low Angpt-1 (left column) shows a low pTie2 / tTie2 ratio. In contrast, the sample with low Angpt-2 and high Angpt-1 (right column) shows a higher pTie2 / tTie2 ratio.