Abstract
The adherence to and invasion of the human epithelial cell line A549 by group B streptococcus (GBS) serotype VIII strains were compared with those of serotype III strains by a conventional method and the dynamic in vitro attachment and invasion system. Twenty GBS strains, including nine vaginal isolates and one invasive isolate each of serotypes III and VIII, were used in the conventional attachment and invasion assay. Adherence to and invasion of A549 cells by serotype VIII GBS strains were significantly greater (P < 0.0001) than those by serotype III strains for both the invasive strain and vaginal isolates. Cytokine production by A549 cells following stimulation with GBS serotypes III and VIII or their purified capsular polysaccharides (CPS) was measured. Serotype III strains stimulated significantly greater tumor necrosis factor alpha (TNF-α) (P < 0.0001) and interleukin-10 (IL-10) (P < 0.05) production than did serotype VIII strains. IL-8 production in response to serotype VIII was significantly higher (P < 0.001) than that in response to serotype III. TNF-α, IL-8, and IL-10 production was greater in A549 cells infected with GBS than in the untreated control cells. TNF-α production was significantly greater (P < 0.005) after stimulation with purified GBS serotype III CPS than after stimulation with serotype VIII CPS, a result similar to that after stimulation with whole GBS. IL-12 production by A549 cells was observed only in response to infection with GBS serotype III, resulting in the possibility of a greater TH1 response in serotype III GBS. These results suggest differences in immune responses to infection with GBS serotypes III and VIII.
Group B streptococci (GBS), or Streptococcus agalactiae, are a component of the normal flora colonizing the respiratory, gastrointestinal, and urologic tracts of humans. They are important pathogens that cause neonatal pneumonia, sepsis, and meningitis associated with high morbidity and mortality (8, 42).
GBS are classified according to the presence of type-specific capsular polysaccharides (CPS), of which nine have been identified. GBS disease in the United States is caused primarily by types Ia, Ib, II, III, and V (12). Strains of serotypes IV, VI, VII, and VIII have rarely been isolated from patients in the United States (24, 36). However, in many regions of the world, the serotypes that cause GBS infections are not restricted to those most prevalent in the United States (48). Several studies revealed the prevalence of GBS serotypes VI and VIII among pregnant women in Japan (13, 21, 30, 48). Of particular interest is the fact that GBS serotype VIII, the serotype most frequently isolated from colonized women in Japan, is rarely associated with neonatal disease. Ongoing monitoring of the distribution of GBS serotypes is important for charting changes in serotype prevalence and for determining the components of an effective GBS vaccine. The differences in serotype distribution among various populations also may reflect differences in pathogenesis among the serotypes. We hypothesized that such differences between one of the dominant U.S. serotypes (serotype III) and one of the dominant Japanese serotypes (serotype VIII) might be present.
Adherence of bacteria and their invasion into host tissue is mediated through a complex series of events that involve changes in surface constituents (40). We examined adherence to and invasion of GBS serotype III and VIII strains into cultured A549 epithelial cells, using both a conventional method (41) and the dynamic in vitro attachment and invasion system (DIVAS) (16, 25).
Innate proinflammatory responses to GBS infection that may contribute to respiratory pathology include the synthesis and release of cytokines, prostaglandins, and nitric oxide (20, 22, 26). Cytokines are also important mediators in host defenses against bacterial and viral infections (18). Cytokines are secreted proteins that function in intracellular signaling during inflammatory and immune processes (18). In general, proinflammatory cytokines, such as tumor necrosis factor alpha (TNF-α), interleukin-1α (IL-1α), IL-1β, IL-6, IL-8, and IL-12, function as part of a cascade that orchestrates the recruitment and activation of inflammatory cells and the induction of effectors (18, 44). TNF-α and IL-8 are produced by a variety of host cells upon exposure of the cells to a range of unrelated microbial components (7). IL-10 is produced by a variety of cells, including CD4+ T cells, B cells, and macrophages. IL-10 possesses several characteristics and is a potent down-modulator of immune response (10, 35, 49, 50). IL-12 is an integral immune regulator which promotes TH1 response while suppressing TH2 response (34). The low frequency of infection with serotype VIII might be associated with the ability of these strains to provoke the production of these cytokines. To address this possibility, we examined the cytokine response of human lung epithelial cells following stimulation with GBS serotypes III and VIII.
MATERIALS AND METHODS
Bacterial strains.
We used to 20 strains of GBS, 10 of serotype III and 10 of serotype VIII, in these studies. Serotype III strain M781 was originally isolated from a newborn with meningitis (49). An invasive strain of serotype VIII, NKMC1998, was kindly provided by Kousaku Matsubara (Department of Pediatrics, Nishi-Kobe Medical Center, Kobe, Japan) (30). Vaginal isolates of serotype III strains (SMU001, SMU007, SMU016, SMU019, SMU056, SMU072, SMU075, SMU080, and SMU097) and vaginal isolates of serotype VIII strains (SMU003, SMU012, SMU014, SMU022, SMU029, SMU037, SMU044, SMU076, and SMU089) were obtained from cultures of vaginal samples from pregnant Japanese women, as described previously (21).
Cell line.
The A549 cell line (ATCC CCL-185) was derived from a human lung carcinoma; it has many of the characteristics of type II alveolar epithelial cells, including surfactant production in culture, and has been used in our laboratory for invasion experiments (16). A549 cells were maintained in RPMI 1640 culture medium (GIBCO, Invitrogen, Grand Island, N.Y.) with 1% l-glutamine and 10% fetal bovine serum (GIBCO, Invitrogen) without antibiotics. The medium was replaced 1 day before the experiment. A549 cells suspended in 0.5 ml of RPMI 1640 with 10% fetal bovine serum were seeded into each well of 24-well culture plates and incubated for 4 days at 37°C with 5% CO2. By the beginning of the assay, the cell number had increased to approximately 1.5 × 106 cells per well. Cell viability was determined by 0.4% trypan blue exclusion and hemocytometer counts.
Invasion and adherence assays.
The attachment and invasion assays were done essentially as described by Rubens et al. (41), and DIVAS was performed as described previously (16), with the modifications indicated below. For the conventional assays, GBS were grown to an optical density at 650 nm (OD650) of 0.3 to 0.5 in Todd-Hewitt broth (THB) (Becton Dickinson and Co., Sparks, Md.) and inoculated onto A549 monolayers for 2 h in each well of 24-well plates at 1.5 × 106 CFU/well to achieve a multiplicity of infection of 1:1. The infected monolayers were then washed three times with phosphate-buffered saline (PBS) (ICN Biochemicals, Aurora, Ohio); 1 ml of fresh RPMI 1640 medium with 10% fetal bovine serum, 5 μg of penicillin G (Sigma-Aldrich, St. Louis, Mo.) per ml, and 100 μg of gentamicin (Sigma-Aldrich) per ml was added to each well, and plates were incubated in a CO2 incubator for 2 h. Monolayers were rinsed five times with PBS, and A549 cells were detached by addition of 0.2 ml of trypsin-EDTA (GIBCO, Invitrogen), lysed by addition of 0.8 ml of 0.025% Triton X-100 (LabChem, Pittsburgh, Pa.), transferred quantitatively to microtubes, and mixed on a Vortex mixer for 1 min. Appropriately diluted aliquots in 0.025% Triton X-100 were plated on tryptic soy-5% sheep blood agar plates. The plates were incubated at 37°C overnight, and the number of GBS CFU recovered per well was determined. Each test was done in quadruplicate.
Bacterial adherence was determined as follows. GBS grown in THB to mid-log phase (OD650 of 0.3 to 0.5) were inoculated at 1.5 × 106 CFU/well onto A549 monolayers for 2 h in each well of 24-well plates. The infected monolayers were then washed five times with PBS, detached from the wells with 0.2 ml of trypsin-EDTA, lysed with 0.8 ml of 0.025% Triton X-100, transferred quantitatively to microtubes, and vortexed vigorously for 1 min. Aliquots diluted in 0.025% Triton X-100 were plated on tryptic soy-5% sheep blood agar plates. The plates were incubated at 37°C overnight, and GBS CFU were counted. The number of attached GBS was calculated as total (attached and invaded) CFU minus invaded CFU. Each test was done in quadruplicate, and the number of CFU recovered per well was determined.
DIVAS.
DIVAS was developed to study microbe-host cell interactions with bacteria held at steady-state growth in a chemostat under defined environmental and nutritional conditions (16, 25). Bacteria held at the steady state of growth are perfused slowly over an established monolayer of tissue culture cells as described below. In brief, a 1-liter chemostat vessel (Applikon, Foster City, Calif.) with a working volume of 0.5 liter was used to grow GBS in chemically defined medium with glucose limitation at a mass doubling time (td) of 1.8 h (fast growth). The temperature (37°C), pH (pH 7.3), and mixing rate (400 rpm) were maintained at constant levels throughout the experiments. Levels of dissolved oxygen (DO2) were monitored with a polarographic DO2 probe and controlled by the addition of a mixture of compressed nitrogen and oxygen. All growth parameters (pH, temperature, mixing rate, media inflow rate, and DO2) were computer controlled with a BioController (model ADI 1030; Applikon).
Attachment and invasion experiments were performed with A549 respiratory epithelial cells grown in 60-mm-diameter culture dishes. Confluent cells were washed twice with 3.0 ml of PBS prior to use in DIVAS. GBS from the chemostat were perfused over the A549 cells by using a plate holder apparatus with inlet and outlet ports to allow for perfusion of bacteria (25). The apparatus was placed on a rotary shaker at 20 rpm in a 37°C incubator, and perfusion of GBS proceeded for 2 h, after which the plates were disconnected from the outflow line of the chemostat. Cell monolayers were washed with PBS, extracellular GBS were killed with antibiotics, eukaryotic cells were disrupted, and internalized GBS were quantified by standard plate counts as described previously (16, 25).
SMU007 (serotype III) and SMU029 (serotype VIII) GBS were used for DIVAS assay. Invasion and adherence with DIVAS were performed with GBS held at a td of 1.8 h and 12% DO2, conditions that result in high levels of invasion (16). Cytokine assays were also performed twice on filtered outflow supernatant fluid samples obtained at 0, 1, and 2 h after GBS passed over the A549 cell monolayer.
Induction of cytokines from human lung epithelial cells.
The following GBS strains were used in the experiments involving cytokine production by human A549 lung epithelial cells: serotype III M781, SMU007, SMU016, SMU001, SMU056, and SMU019 and serotype VIII NKMC1998, SMU014, SMU037, SMU029, SMU003, and SMU044.
Sampling method for cytokine assays.
GBS were grown to an OD650 of 0.3 to 0.5 in THB. GBS were inoculated at 1.5 × 106 CFU/well onto A549 monolayers in each well of 24-well plates at an MOI of 1:1. The supernatant fluid was removed after 2 h of contact with the bacteria. The supernatant fluids were clarified by centrifugation and were filtered (0.22-μm-pore-size filter) for clarification.
Cytokine assay.
Cytokines secreted into the culture supernatant were detected with enzyme-linked immunosorbent assays. Human TNF-α or human TNF-α US (ultrasensitive), human IL-8/NAP-1, human IL-10 or human IL-10 US, and human IL-12 US immunoassay kits (all from BioSource International, Camarillo, Calif.) were used to detect TNF-α, IL-8, IL-10, and IL-12, respectively. The quantitative limits of detection were 15.6 to 1,000, 0.5 to 32, 15.6 to 1,000, 7.8 to 500, 0.78 to 50, and 1.56 to 100 pg/ml for the TNF-α, TNF-α US, IL-8/NAP-1, IL-10, IL-10 US, and IL-12 US kits, respectively. All assays were conducted according to the manufacture's instructions in duplicate.
Effect of stimulation with GBS CPS on TNF-α production.
TNF-α production by A549 cells stimulated with serotype III and VIII GBS CPS at 2, 5, and 10 μg/ml was investigated. GBS serotype III and serotype VIII CPS were purified as previously described (47, 48). Each test was done in triplicate, and cytokine assays were conducted twice in duplicate. Because of the potential for the presence of trace amounts of endotoxin in the purified CPS, each CPS was exposed to polymyxin B (2, 5, and 10 μg/ml) (Sigma-Aldrich) at stimulation. Each test was done in quadruplicate, and cytokine assays were conducted twice in duplicate.
Statistical analyses.
The significance of GBS invasion for two different variables was determined by the unpaired t test with the Welch correction. These analyses were performed with Instat version 3.0a (GraphPad, San Diego, Calif.). P values of <0.05 were considered significant.
RESULTS
Adherence and invasion.
Adherence to and invasion into A549 cells by serotype VIII GBS was significantly higher than those by serotype III GBS (Table 1) both for the invasive isolate (P < 0.0001) and for vaginal isolates (P < 0.0001). For serotype VIII, a significant difference (P < 0.005) between the invasion into A549 cells by invasive isolate NKMC1998 and vaginal isolates was seen, whereas for serotype III, no significant difference (P > 0.05) between invasive and vaginal isolates was noted. For both serotypes, there was no significant difference (P > 0.05) in the adherence of invasive and vaginal isolates to A549 cells.
TABLE 1.
Adherence to and invasion into A549 cells by serotypes III and VIII of GBSa
| Serotype and strain | Source of isolate | Adherence
|
Invasion
|
||
|---|---|---|---|---|---|
| Mean log10 CFU ± SD | %b | Mean log10 CFU ± SD | %c | ||
| III | |||||
| M781 | Invasive | 4.040 ± 0.071 | 0.80 | 3.792 ± 0.069 | 0.42 |
| SMU097 | Vaginal | 4.040 ± 0.071 | 0.80 | 3.720 ± 0.165 | 0.37 |
| SMU001 | Vaginal | 4.061 ± 0.062 | 0.84 | 3.775 ± 0.060 | 0.40 |
| SMU075 | Vaginal | 4.095 ± 0.060 | 0.87 | 3.812 ± 0.149 | 0.45 |
| SMU080 | Vaginal | 4.083 ± 0.092 | 0.85 | 3.690 ± 0.188 | 0.35 |
| SMU056 | Vaginal | 4.092 ± 0.073 | 0.84 | 3.758 ± 0.149 | 0.40 |
| SMU007 | Vaginal | 4.140 ± 0.124 | 0.95 | 3.762 ± 0.137 | 0.40 |
| SMU016 | Vaginal | 4.144 ± 0.051 | 0.93 | 3.823 ± 0.087 | 0.45 |
| SMU072 | Vaginal | 4.118 ± 0.072 | 0.88 | 3.746 ± 0.127 | 0.38 |
| Vaginal isolate mean | 4.097 ± 0.072 | 0.87 | 3.768 ± 0.125 | 0.41 | |
| Total mean | 4.092 ± 0.072 | 0.86 | 3.770 ± 0.119 | 0.41 | |
| VIII | |||||
| NKMC1998 | Invasive | 4.473 ± 0.025 | 1.98 | 4.183 ± 0.028 | 1.02 |
| SMU029 | Vaginal | 4.406 ± 0.017 | 1.72 | 4.049 ± 0.067 | 0.78 |
| SMU089 | Vaginal | 4.439 ± 0.020 | 1.83 | 4.041 ± 0.052 | 0.77 |
| SMU044 | Vaginal | 4.355 ± 0.047 | 1.52 | 4.012 ± 0.020 | 0.72 |
| SMU014 | Vaginal | 4.439 ± 0.016 | 1.83 | 4.074 ± 0.086 | 0.82 |
| SMU003 | Vaginal | 4.406 ± 0.073 | 1.63 | 4.012 ± 0.020 | 0.72 |
| SMU037 | Vaginal | 4.466 ± 0.115 | 2.00 | 4.023 ± 0.022 | 0.73 |
| SMU012 | Vaginal | 4.370 ± 0.113 | 1.60 | 4.073 ± 0.095 | 0.84 |
| SMU022 | Vaginal | 4.390 ± 0.095 | 1.67 | 4.088 ± 0.100 | 0.83 |
| SMU076 | Vaginal | 4.426 ± 0.040 | 1.78 | 4.102 ± 0.119 | 0.87 |
| Vaginal mean | 4.411 ± 0.060 | 1.73 | 4.053 ± 0.065 | 0.79 | |
| Total mean | 4.417 ± 0.056 | 1.76 | 4.066 ± 0.061 | 0.81 | |
Adherence to and invasion into A549 cells were significantly, higher for serotype VIII GBS strains than for serotype III strains, both for the invasive strain and for vaginal strains (P < 0.0001 and P < 0.0001 for CFU of invasive and vaginal strains, respectively). There was a significant difference between invasion into A549 cells by invasive strain NKMC1998 and by vaginal strains of serotype VIII (P < 0.005), but there was no significant difference between invasion by invasive and vaginal strains for serotype III (P > 0.05).
Number of adherent CFU/number of CFU in inoculum.
Number of intracellular CFU/number of CFU in inoculum.
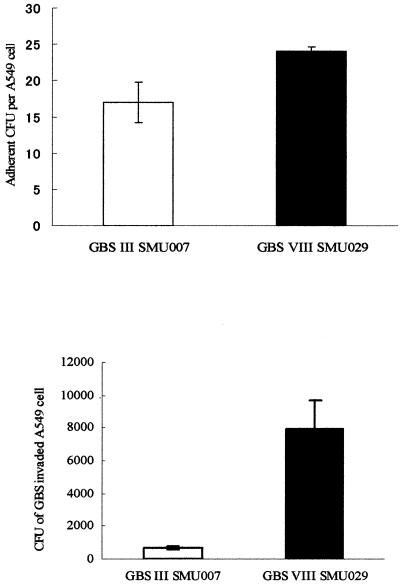
To determine the invasiveness of GBS held at a steady state of growth and perfused over A549 cells, we performed DIVAS with two selected strains of GBS: serotype III SMU007 and serotype VIII SMU029. A mean (± standard deviation) of 17 ± 2.8 GBS serotype III SMU007 cells adhered per A549 cell, compared with 24 ± 0.7 GBS serotype VIII SMU029 cells (P < 0.05) (Fig. 1).
FIG. 1.
Adherence of GBS to (top) and invasion of GBS into (bottom) A549 cells during fast growth (td of 1.8 h) with 12% DO2 in DIVAS. Error bars indicate standard deviations.
GBS serotype VIII SMU029 grown in continuous culture invaded A549 cells more readily than did GBS serotype III SMU007 (Fig. 1). The CFU of GBS serotypes III and VIII grown at a td of 1.8 h with 12% DO2 that invaded A549 cells were 672 ± 56 and 7,900 ± 1,800, respectively (P < 0.0001).
Cytokine production.
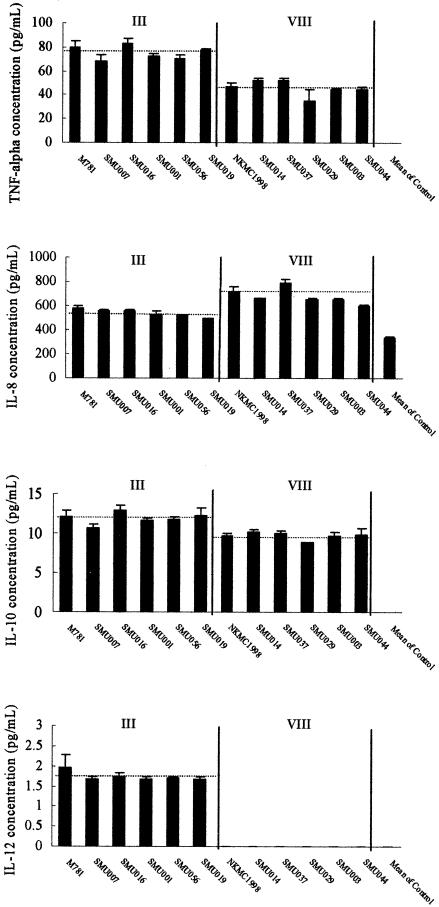
Secretion of TNF-α, IL-8, and IL-10 by A549 cells in response to GBS infection was significantly increased compared with secretion by the untreated control group. There was a significant difference between TNF-α production by serotypes III and VIII for both invasive and vaginal isolates (P < 0.0001 and P < 0.0001 for invasive and vaginal isolates, respectively) (Fig. 2). There was a significant difference in IL-8 production between serotypes III and VIII for both invasive and vaginal isolates (P < 0.001 and P < 0.001 for invasive and vaginal isolates, respectively) (Fig. 2). IL-10 production by A549 cells was similar to that of TNF-α. There was a significant difference in IL-10 production in response to serotypes III and VIII for both invasive (P < 0.05) and vaginal (P < 0.01) isolates (Fig. 2). IL-12 production by A549 cells in response to GBS infection was observed for serotype III, while it was not observed for serotype VIII (Fig. 2).
FIG. 2.
TNF-α, IL-8, IL-10, and IL-12 production by A549 cells after 2 h of stimulation with GBS serotype III and serotype VIII strains. The dotted line shows the average of each cytokine value. The means of TNF-α production following stimulation with serotypes III and VIII are 75.1 and 46.1 pg/ml, respectively. The means of IL-8 production for serotypes III and VIII are 541.2 and 677.4 pg/ml, respectively. The means of IL-10 production for serotypes III and VIII are 11.9 and 9.7 pg/ml, respectively. The mean of IL-12 production for serotype III is 1.74 pg/ml. Error bars indicate standard deviations.
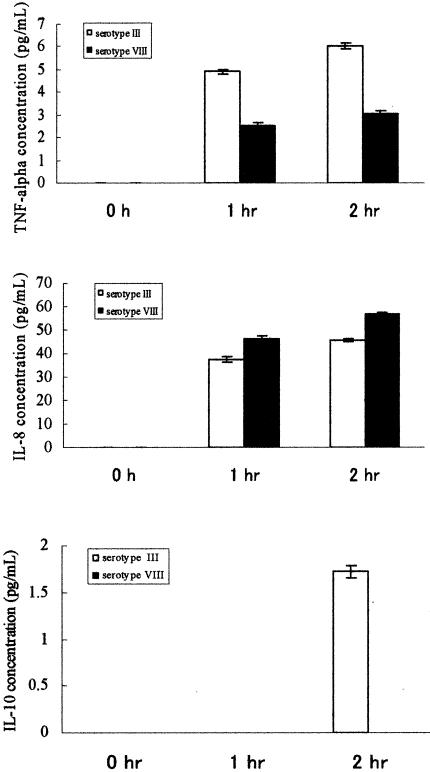
Since the flow of chemically defined medium in the DIVAS assay is continuous, cytokines do not accumulate but are diluted in this open-flow system over time; thus, the level of cytokine production was relatively low in all samples. Nevertheless, TNF-α production in response to serotypes III and VIII differed significantly (P < 0.0001 and P < 0.0001 at 1 and 2 h, respectively) (Fig. 3). Also, there was a significant difference in IL-8 production in response to serotypes III and VIII (P < 0.0005 and P < 0.0001 at 1 and 2 h, respectively) (Fig. 3). On the other hand, IL-10 production could be detected only for serotype III GBS at 2 h and was below the detection limit for serotype VIII (Fig. 3).
FIG. 3.
TNF-α, IL-8, and IL-10 production by A549 cells in DIVAS following stimulation with GBS serotype III and VIII strains. Error bars indicate standard deviations.
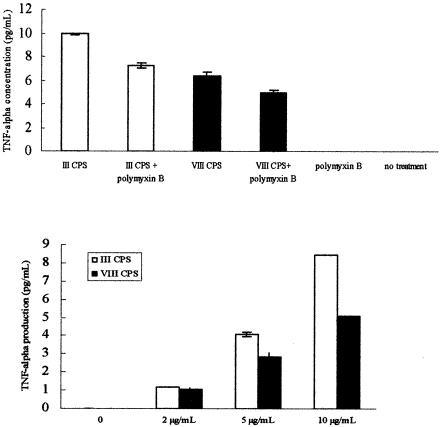
Effect of stimulation with GBS CPS on TNF-α production.
TNF-α production by A549 cells increased in a dose-dependent manner with both serotypes after stimulation with CPS (Fig. 4). There was a significant difference in TNF-α production in response to CPS of serotypes III and VIII at all concentrations tested (P < 0.005, P < 0.0001, and P < 0.0001 at CPS concentrations of 2, 5, and 10 μg/ml, respectively) (Fig. 4). TNF-α production by A549 cells was inhibited by only 26.2% (serotype III CPS) and 21.5% (serotype VIII CPS) following stimulation of A549 cells by CPS with polymyxin B. TNF-α production by A549 cells differed significantly (P < 0.0005) following stimulation by either serotype III CPS or serotype VIII CPS.
FIG. 4.
TNF-α production by A549 cells after stimulation by GBS serotype III and VIII CPS. (Top panel) Induction of TNF-α by purified CPS with and without addition of polymyxin B. (Bottom panel) THF-α production as a function of CPS concentration. Error bars indicate standard deviations.
DISCUSSION
Since the early 1980s, GBS strains of serotypes VI and VIII have been prevalent in Japan among isolates colonizing pregnant women, with serotype VIII accounting for 25 to 36% of all isolates (21, 30). Despite this high carriage rate, the frequency of early-onset disease due to serotype VIII among Japanese neonates is low (14). In Japan, a nationwide surveillance of early-onset neonatal GBS infection conducted from 1983 to 1997 found that the most frequent serotypes among 224 strains examined were serotype III (38.4%), serotype Ia (17.0%), serotype Ib (8.5%), serotype VI (8.5%), serotype II (6.7%), and serotype VIII (4.9% [11 cases]) (14). Recent studies have shown that women colonized with GBS serotypes Ia, Ib, II, III, and V had significantly higher concentrations of IgG specific for the CPS of the colonizing serotype in serum compared with women not colonized with GBS (2, 4, 11). We hypothesized that a difference in the host response to serotype III and VIII strains may account for this disparity and that this difference may be associated with their ability to invade host cells. The results of our in vitro study support the hypothesis that serotype VIII strains are more invasive than strains of serotype III. Factors that may account for differences between these two serotypes are numerous and may involve fine structural features of the CPS or expression of surface proteins associated with attachment and invasion (31).
Significant differences in attachment and invasion of serotype VIII strains and serotype III strains were independent of the assay (conventional or DIVAS) used. Of the two vaginal isolates tested in DIVAS, higher numbers of GBS serotype VIII than of GBS serotype III attached to and invaded A549 cells, a surprising finding because the number of cells of serotype III strain M781 (an invasive isolate) that invaded A549 cells under the same growth conditions was high (23,000 ± 9,050 CFU invaded/dish) (A. Johri and L.C. Paoletti, unpublished data). The difference in invasiveness between an invasive and a colonizing GBS may be due to the difference in expression of factors specifically involved with the invasion process or to differences in metabolism and nutrient requirements. An understanding of mechanisms responsible for these differences awaits further experimentation.
Host immune factors have an obvious and important role in disease progression. Matsubara et al. reported that women colonized with serotype VIII had significantly higher titers of serum antibodies to serotype VIII CPS than did women who were not colonized (29). It is possible that entry into epithelial cells might enhance the antibody response to GBS, possibly through better antigen processing, thus diminishing the rate of invasive infection caused by serotype VIII GBS compared with the rate of colonization by this serotype. We have hypothesized that in some circumstances, entry into epithelial cells may serve as a host defense mechanism, since GBS do not to replicate intracellularly (41) and may be expelled from the host as the epithelial cells are shed. Increased systemic concentrations of proinflammatory cytokines, including TNF-α, have been correlated with septic shock and mortality (6, 46). The ability of GBS to induce proinflammatory cytokines has been documented for human leukocytes (45, 47) and in rodent infection models (23, 28). In those models, TNF-α plays a central role in mediating mortality (28, 45). We found that the production of TNF-α by A549 cells following stimulation with serotype III GBS was significantly higher than that following stimulation with serotype VIII, although adherence to and invasion of A549 cells were lower for serotype III than for serotype VIII. Therefore, TNF-α expression may be associated with the major virulence factor (i.e., CPS antigen) of GBS and may account for the greater virulence of serotype III strains. The fact that production of IL-12 was observed in response to serotype III and not for serotype VIII infection might lead to more antibody production for women colonized by serotype VIII. The elucidation of cellular mechanisms involved in GBS-induced cytokine production may also be important for the development of effective therapeutic strategies (27). These data are consistent with the hypothesis that greater invasion by GBS serotype VIII and lower TNF-α production tend to drive a TH2 response, resulting in higher levels of protective antibody.
IL-8 is a potent neutrophil chemotactic stimulus (33) that further acts to up-regulate the expression of adhesion molecules on the neutrophil surface (5), to promote their transendothelial migration (15), and to stimulate an oxidative burst and release of lysosomal enzymes (37). An elevated level of circulating IL-8 is a strong predictor of bacterial infection (9), and marked increases in levels of IL-8 have been detected in sputum, bronchoalveolar lavage fluid, and uterine endometrial lavage fluid from patients with various infectious diseases (32, 39, 43). IL-8 is also the major neutrophil chemoattractant produced by lung epithelial cells after experimental infection (19). In the present study, we found that GBS induced IL-8 release from A549 lung epithelial cells in a cell surface adhesion-, cell invasion-, and time-dependent fashion (data not shown). The greater amount of IL-8 may lead to recruitment of more inflammatory cells, which may lead to the more rapid elimination of GBS serotype VIII strains.
It is interesting that we detected IL-10 as well as TNF-α and IL-8 production by A549 cells cultured in the presence of GBS. IL-10 has been shown to inhibit the production of many proinflammatory cytokines, including IL-1, IL-6, TNF-α, IL-8, granulocyte-monocyte colony-stimulating factor, and granulocyte colony-stimulating factor; to down-regulate activity by macrophages/monocytes and polymorphonuclear cells (1, 3, 38); and to inhibit leukocyte chemotaxis (17). The presence of IL-10 may represent a cellular response to the increasing levels of TNF-α, since this has been described as an autoregulatory mechanism to decrease the production of TNF-α.
Production of TNF-α was significantly greater after stimulation by serotype III CPS than after stimulation by serotype VIII CPS, a result similar to that for stimulation by whole bacteria. This indicates that production of TNF-α is also dependent on bacterial surface components such as CPS.
It is clear that serotype III isolates provoke a more robust inflammatory response while at the same time potentiating the down-regulation of the immune response via IL-10. The diminished IL-10 response and the absence of an IL-12 response to serotype VIII GBS may result in a more robust production of protective antibody via a TH2 route. Continued research into the differences in the pathogenesis of different strains of the nine GBS serotypes and between colonizing and invasive isolates will provide a more complete understanding of factors important for GBS pathogenesis. Future studies will address the possibility of a predominant TH2 response with concomitant antibody production in women colonized with serotype VIII GBS.
Acknowledgments
We thank Vilas Patwardhan for technical assistance during the DIVAS assay and Kousaku Matsubara for providing the invasive strain of serotype VIII GBS.
This work supported in part by a grant to Hiroshige Mikamo from the Ministry of Education, Culture, Sports, Science and Technology of the Japanese Government; by NIH grants AI38424 and AI053191; and by NIAID contract AI-75326.
The contents of this publication do not necessarily reflect the views or policies of the Department of Health and Human Services, nor does the mention of trade names, commercial products, or organizations imply endorsements by the U.S. Government.
Editor: V. J. DiRita
REFERENCES
- 1.Bogdan, C., Y. Vodovotz, and C. Nathan. 1991. Macrophage deactivation by interleukin-10. J. Exp. Med. 174:1549-1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell, J. R., S. L. Hillier, M. A. Krohn, P. Ferrieri, D. F. Zaleznik, and C. J. Baker. 2000. Group B streptococcal colonization and serotype-specific immunity in pregnant women at delivery. Obstet. Gynecol. 96:498-503. [DOI] [PubMed] [Google Scholar]
- 3.Cassatella, M. A., L. Meda, S. Bonora, M. Ceska, and G. Coinstantin. 1993. Interleukin 10 (IL-10) inhibits the release of proinflammatory cytokines from human polymorphonuclear leukocytes. Evidence for an autocrine role of tumor necrosis factor and IL-1 beta in mediating the production of IL-8 triggered by lipopolysaccharide. J. Exp. Med. 178:2207-2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davies, H. D., C. Adair, A. McGeer, M. Doreen, S. Robertson, M. Mucenski, L. Kowalsky, G. Tyrell, and C. J. Baker. 2001. Antibodies to capsular polysaccharide of group B Streptococcus in pregnant Canadian women: relationship to colonization status and infection in the neonate. J. Infect. Dis. 184:285-291. [DOI] [PubMed] [Google Scholar]
- 5.Detmers, P. A., S. K. Lo, E. Olsen-Egbert, A. Walz, M. Baggiolini, and Z. A. Cohn. 1990. Neutrophil-activating protein 1/interleukin-8 stimulates the binding activity of the leukocyte adhesion receptor XD11b/CD18 on human neutrophils. J. Exp. Med. 171:1155-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dinarello, C. A. 1991. The proinflammatory cytokines interleukin 1 and tumor necrosis factor and treatment of the septic shock syndrome. J. Infect. Dis. 163:1177-1184. [DOI] [PubMed] [Google Scholar]
- 7.Doran, K. S., J. C. W. Chang, V. M. Benoit, L. Eckmann, and V. Nizet. 2002. Group B streptococcal β-hemolysin/cytolysin promotes invasion of human lung epithelial cells and release of interleukin-8. J. Infect. Dis. 185:196-203. [DOI] [PubMed] [Google Scholar]
- 8.Faro, S. 1981. Group B beta-hemolytic streptococci and puerperal infections. Am. J. Obstet. Gynecol. 139:686-689. [DOI] [PubMed] [Google Scholar]
- 9.Franz, A. R., G. Steinbach, M. Kron, and F. Pohlandt. 1999. Reduction of unnecessary antibiotic therapy in newborn infants using interleukin-8 and C-reactive protein as markers of bacterial infections. Pediatrics 104:447-453. [DOI] [PubMed] [Google Scholar]
- 10.Gibson, F. C., III, A. O. Tzianabos, and A. B. Onderdonk. 1996. The capsular polysaccharide complex of Bacteroides fragilis induces cytokine production from human and murine phagocytic cells. Infect. Immun. 64:1065-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gray, B. M., D. G. Pritchard, and H. C. Dillon, Jr. 1985. Seroepidemiological studies of group B Streptococcus type II. J. Infect. Dis. 151:1073-1080. [DOI] [PubMed] [Google Scholar]
- 12.Harrison, L. H., D. M. Dwyer, and J. A. Johnson. 1995. Emergence of serotype V group B streptococcal infection among infants and adults. J. Infect. Dis. 171:513. [DOI] [PubMed] [Google Scholar]
- 13.Hoshina, K. 1997. Minimization of the number of pregnant women to be treated with preventive procedure against GBS infection by means of antibody measure. Acta Paediatr. Jpn. 39:546-549. [DOI] [PubMed] [Google Scholar]
- 14.Hoshina, K., Y. Suzuki, H. Nishida, K. Kaneko, S. Matsuda, M. Kobayashi, and N. Kadoi. 2002. Trend of neonatal group B streptococcal infection during the last 15 years. Pediatr. Int. 44:641-646. [DOI] [PubMed] [Google Scholar]
- 15.Huber, A. R., S. L. Kunkel, R. F. Todd III, and S. J. Weiss. 1991. Regulation of transendothelial neutrophil migration by endogenous interleukin-8. Science 254:99-102. [DOI] [PubMed] [Google Scholar]
- 16.Johri, A. K., J. Padilla, G. Malin, and L. C. Paoletti. 2003. Oxygen regulates invasiveness and virulence of group B Streptococcus. Infect. Immun. 71:6707-6711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kasama, T., R. M. Strieter, N. W. Lukacs, P. M. Lincoln, M. D. Burdick, and S. L. Kunkel. 1995. Interleukin-10 expression and chemokine regulation during the evolution of the murine type II collagen-induced arthritis. J. Clin. Investig. 95:2868-2876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kelley, J. 1990. Cytokines of the lung. Am. Rev. Respir. Dis. 141:765-788. [DOI] [PubMed] [Google Scholar]
- 19.Kunkel, S. L., T. Standiford, K. Kasahara, and R. M. Strieter. 1991. Interleukin-8 (IL-8): the major neutrophil chemotactic factor in the lung. Exp. Lung Res. 17:17-23. [DOI] [PubMed] [Google Scholar]
- 20.Kwak, D. J., N. H. Augustine, W. G. Borges, J. L. Joyner, W. F. Green, and H. R. Hill. 2000. Intracellular and extracellular cytokine production by human mixed mononuclear cells in response to group B streptococci. Infect. Immun. 68:320-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lachenauer, C. S., D. L. Kasper, J. Shimada, Y. Ichiman, H. Ohtsuka, M. Kaku, L. C. Paoletti, P. Ferrieri, and L. C. Madoff. 1999. Serotypes VI and VIII predominate among group B streptococci isolated from pregnant Japanese women. J. Infect. Dis. 179:1030-1033. [DOI] [PubMed] [Google Scholar]
- 22.Leib, S. L., Y. S. Kim, S. M. Black, J. H. Tureen, and M. G. Tauber. 1998. Inducible nitric oxide synthase and the effect of aminoguanadine in experimental neonatal meningitis. J. Infect. Dis. 177:692-700. [DOI] [PubMed] [Google Scholar]
- 23.Levy, O., R. M. Jean-Jacques, C. Cywes, R. B. Sisson, K. A. Zarember, P. J. Godowski, J. L. Christianson, H. Guttormsen, M. C. Carroll, A. Nicholson-Weller, and M. R. Wessels. 2003. Critical role of the complement system in group B Streptococcus-induced tumor necrosis factor alpha release. Infect. Immun. 71:6344-6353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lin, F. Y., J. D. Clemens, P. H. Azimi, J. A. Regan, L. E. Weisman, J. B. Philips III, G. G. Rhoads, P. Clark, R. A. Brenner, and P. Ferrieri. 1998. Capsular polysaccharide types of group B streptococcal isolates from neonates with early-onset systemic infection. J. Infect. Dis. 177:790-792. [DOI] [PubMed] [Google Scholar]
- 25.Malin, G., and L. C. Paoletti. 2001. Use of a dynamic in vitro attachment and invasion system (DIVAS) to determine influence of growth rate on invasion of respiratory epithelial cells by group B Streptococcus. Proc. Natl. Acad. Sci. USA 98:13335-13340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maloney, C. G., S. D. Thompson, H. R. Hill, J. F. Bohnsack, T. M. McIntyre, and G. A. Zimmerman. 2000. Induction of cyclooxygenase-2 by human monocytes exposed to group B streptococci. J. Leukoc. Biol. 67:615-621. [DOI] [PubMed] [Google Scholar]
- 27.Mancuso, G., A. Midiri, C. Beninati, G. Piraino, A. Valenti, G. Nicocia, D. Teti, J. Cook, and G. Teti. 2002. Mitogen-activated protein kinases and NF-κB are involved in TNF-α responses to group B streptococci. J. Immunol. 169:1401-1409. [DOI] [PubMed] [Google Scholar]
- 28.Mancuso, G., F. Tomasello, C. von Hunolstein, G. Orefici, and G. Teti. 1994. Induction of tumor necrosis factor alpha by the group- and type-specific polysaccharides from type III group B streptococci. Infect. Immun. 62:2748-2753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matsubara, K., K. Katayama, K. Baba, H. Nigami, H. Harigawa, and M. Sugiyama. 2002. Seroepidemiologic studies of serotype VIII group B Streptococcus in Japan. J. Infect. Dis. 186:855-858. [DOI] [PubMed] [Google Scholar]
- 30.Matsubara, K., M. Sugiyama, K. Hoshina, H. Mikamo, and K. Baba. 2000. Early onset neonatal sepsis caused by serotype VIII group B streptococci. Pediatr. Infect. Dis. J. 19:359-360. [DOI] [PubMed] [Google Scholar]
- 31.Michon, F., E. Katzenellenbogen, D. L. Kasper, and H. L. Jennings. 1987. Structure of the complex group-specific polysaccharide of group B Streptococcus. Biochemistry 26:476-486. [DOI] [PubMed] [Google Scholar]
- 32.Mikamo, H., K. Kawazoe, Y. Sato, and T. Tamaya. 1998. Effects of long-term/low dose clarithromycin on neutrophil count and interleukin-8 level in pyometra. Chemotherapy 44:50-54. [DOI] [PubMed] [Google Scholar]
- 33.Murphy, P. M. 1997. Neutrophil receptors for interleukin-8 and related CXC chemokines. Semin. Hematol. 34:311-318. [PubMed] [Google Scholar]
- 34.O'Garra, A. 1998. Cytokines induce the development of functionally heterogeneous T helper cell subsets. Immunity 8:275-283. [DOI] [PubMed] [Google Scholar]
- 35.O'Garra, A., R. Chang, N. Go, R. Hasting, G. Haughton, and M. Howard. 1992. Ly-1 B (B-1) cells are the main source of B cell-derived interleukin 10. Eur. J. Immunol. 22:711-717. [DOI] [PubMed] [Google Scholar]
- 36.Paoletti, L. J., J. Bradford, and L. C. Paoletti. 1999. A serotype VIII strain among colonizing group B streptococcal isolates in Boston, Massachusetts. J. Clin. Microbiol. 37:3759-3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peveri, P., A. Walz, B. Dewald, and M. Baggiolini. 1988. A novel neutrophil-activating factor produced by human mononuclear phagocytes. J. Exp. Med. 167:1547-1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Puliti, M., C. von Hunolstein, C. Verwaerde, F. Bistoni, G. Orefici, and L. Tissi. 2002. Regulatory role of interleukin-10 in experimental group B streptococcal arthritis. Infect. Immun. 70:2862-2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rodriguez, J. L., C. G. Miller, L. E. DeForge, L. Kelty, C. J. Shanley, R. H. Bartlett, and D. G. Remick. 1992. Local production of interleukin-8 is associated with nosocomial pneumonia. J. Trauma 33:74-81. [DOI] [PubMed] [Google Scholar]
- 40.Rubens, C. E., H. V. Raff, J. C. Jackson, E. Y. Chi, J. Bielitzki, and S. Hillier. 1991. Pathophysiology and histopathology of group B streptococcal sepsis in Macaca nemestrina primates induced after intraamniotic inoculation: evidence for bacterial cellular invasion. J. Infect. Dis. 164:320-330. [DOI] [PubMed] [Google Scholar]
- 41.Rubens, C. E., S. Smith, M. Hulse, E. Y. Chi, and G. Belle. 1992. Respiratory epithelial cell invasion by group B streptococci. Infect. Immun. 60:5157-5163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schuchat, A., and J. D. Wenger. 1994. Epidemiology of group B streptococcal disease. Risk factors, prevention strategy, and vaccine development. Epidemiol. Rev. 16:374-402. [DOI] [PubMed] [Google Scholar]
- 43.Standiford, T. J., S. L. Kunkel, M. J. Greenberger, L. L. Laichalk, and R. M. Strieter. 1996. Expression and regulation of chemokines in bacterial pneumonia. J. Leukoc. Biol. 59:24-28. [DOI] [PubMed] [Google Scholar]
- 44.Teti, G., G. Mancuso, and F. Tomasello. 1993. Cytokine appearance and effects of anti-tumor necrosis factor alpha antibodies in a neonatal rat model of group B streptococcal infection. Infect. Immun. 61:227-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vallejo, J., C. J. Baker, and M. Edwards. 1996. Role of the bacterial cell wall and capsule in induction of tumor necrosis factor alpha by type III group B streptococci. Infect. Immun. 64:5042-5046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Verhoef, J., and E. Mattsson. 1995. The role of cytokine in Gram-positive bacterial shock. Trends Microbiol. 3:136-140. [DOI] [PubMed] [Google Scholar]
- 47.von Hunolstein, C., A. Totolian, G. Alfarone, G. Mancuso, V. Cusumano, G. Teti, and G. Orefici. 1997. Soluble antigens from group B streptococci induce cytokine production in human blood cultures. Infect. Immun. 65:4017-4021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Walsh, J. A., and S. Hutchins. 1989. Group B streptococcal disease: its importance in the developing world and prospect for prevention with vaccines. Pediatr. Infect. Dis. J. 8:271-277. [PubMed] [Google Scholar]
- 49.Wessels, M. R., L. C. Paoletti, D. L. Kasper, J. L. DiFabio, F. Michon, and H. J. Jennings. 1990. Immunogenicity in animals of a polysaccharide-protein conjugate vaccine against type III group B Streptococcus. J. Clin. Invest. 86:1428-1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yassl, H., R. De Waal Malefyt, M. G. Roncarolo, J. S. Abrams, R. Lahesmaa, H. Spits, and J. E. de Vries. 1992. Interleukin 10 is produced by subsets of human CD4+ T-cell clones and peripheral blood T-cells. J. Immunol. 149:2378-2384. [PubMed] [Google Scholar]