Abstract
Multiple myeloma is a plasma cell skeletal malignancy. While therapeutic agents such as bortezomib and lenalidomide have significantly improved overall survival, the disease is currently incurable with the emergence of drug resistance limiting the efficacy of chemotherapeutic strategies. Failure to cure the disease is in part due to the underlying genetic heterogeneity of the cancer. Myeloma progression is critically dependent on the surrounding microenvironment. Defining the interactions between myeloma cells and the more genetically stable hematopoietic and mesenchymal components of the bone microenvironment is critical for the development of new therapeutic targets. In this review, we discuss recent advances in our understanding of how microenvironmental elements contribute to myeloma progression and therapeutically, how those elements can or are currently being targeted in a bid to eradicate the disease.
Introduction
Multiple myeloma is a clonal expansion of malignant plasma cells within the bone marrow. Malignant transformation of plasma cells often begins with the chromosomal translocation, into the IgG loci. Secondary mutations, then lead to the development of clonal variants with KRAS mutations, MYC up regulation and the activation of NFκb pathways [1]. Clinically, the current consensus regarding a diagnosis of myeloma is made based upon low levels of hemoglobin (≤10.5 g/dL), increased levels of circulating calcium (≥12mg/dL), immunoglobulin in the urine and the presence of areas of bone destruction [2]. Cancer-induced bone disease is associated with significant morbidity as a result of pain, pathological fractures and hypercalcemia [3]. Worldwide, approximately 115,000 patients are diagnosed with myeloma per year. The median survival time is 3 – 4 years subsequent to diagnosis and approximately, 80,000 patients succumb to the disease each year [4].
Although currently incurable, the recent discovery of novel therapeutics has significantly improved overall survival for patients diagnosed with symptomatic myeloma. The current standard of care for patients with various stages of myeloma includes the following approaches that are divided based on newly diagnosed versus refractory disease. For patients under the age of 70 years old, without comorbidities, high-dose chemotherapy followed by autologous stem cell transplantation (HDT-ASCT) is a first line treatment strategy for newly diagnosed myeloma. A major advance has been the introduction of novel agents including immunomodulatory drugs (thalidomine and lenalidomide), and proteasome inhibitors (bortezomib), increasing the rates of remission [5]. In those individuals not eligible for stem cell transplantation, the combination of melphalan/prednisone/thalidomide or bortezomib is a standard treatment strategy. Additionally, the majority of patients receive a bisphosphonate (e.g. Zometa) that significantly reduces bone pain and the risk of skeletal related events (e.g. hypercalcemia, fracture and spinal cord compression) [6].
Relapsed, or refectory disease is defined as individuals that fail to respond to salvage therapy, or undergo disease progression rapidly following initial therapy. As expected, refractory disease is often more aggressive in nature and resistant to standard of care therapies and consequently, a different treatment strategy is required [7]. National Comprehensive Cancer Network (NCCN) guidelines indicate the use of new agents pomalidomide (an analogue of thalidomine and lenalidomide) and carfilzomib (a second generation proteasome inhibitor) for use in relapsed patients who have failed bortezomib or lenalidomide based therapies [8].
Reports from ongoing clinical trials are also encouraging in regards to extending progression free and overall survival for myeloma patients (Table 1). However, the majority of these clinical trials still focus primarily on treatment of the malignant myeloma cells. Given that myeloma is highly susceptible to genetic mutation, this leads to increased probability of drug resistant clones that will emerge following therapeutic intervention [9]. Despite the numerous mutations associated with myeloma, the progression of the disease is often dependent on interactions with the surrounding bone microenvironment [10]. The paradigm for myeloma-bone interaction has been described as the “vicious cycle” wherein myeloma cells suppress bone-forming osteoblasts and promote the formation of bone-resorbing osteoclasts. The bone matrix is rich in factors such as transforming growth factor beta (TGFβ) that upon release feed back on the myeloma cells to promote disease progression [11]. Targeting the stromal cells driving the vicious cycle represent a logical therapeutic opportunity. In this regard, bisphosphonates, which target osteoclasts have been shown to significantly reduce the risk of myeloma induced pathological fracture and in subsets of myeloma patients can extend overall survival [12, 13]. Now, emerging studies have begun to define important contributions from other cell types in the bone marrow microenvironment. The bone marrow microenvironment is a natural reservoir for hematopoietic cell progenitors. Hemangioblasts give rise to endothelial and hematopoietic stem cells (HSCs). Angiogenesis and the vascularization of the myeloma-bone microenvironment has long been associated with the progression of the disease and the contribution of endothelial cells and the factors regulating the process has been extensively reviewed [14– 16]. Here, we will examine the contributions of HSC derived hematopoietic and mesenchymal cells in contributing to myeloma progression and discuss potential therapeutics that could significantly impact disease progression and extend overall survival for these patients.
Table 1.
Currently, there are approximately 178 interventional clinical trials targeting multiple myeloma in the United States alone. Here, a selection of trials is illustrated to demonstrate the diverse approaches being used to treat the disease.
| MECHANISM OF ACTION | PHASE | TRIAL NUMBER | |||
|---|---|---|---|---|---|
| COMBINATION TRIALS | Bortezomib + Lenalidomide + Dexamethasone |
Proteasome Inhibitor; Anti-tumor/ Anti-bone resorptive Thalidomide derivative; Anti-tumor/Anti-angiogenesis/IMiD Corticosteroid; Anti-inflammatory |
Phase III | NCT01863550 | |
| Carfilzomib + Pomalidomide + Dexamethasone |
2nd Gen. Proteasome Inhibitor; Anti-tumor 2nd Gen. Thalidomide Derivative; Anti-tumor/Anti-angiogenesis/IMiD Corticosteroid; Anti-inflammatory |
Phase II/I | NCT0166794 NCT01464034 |
||
| Pomalidomide + Dexamethasone + Clarithromycin |
2nd Gen. Thalidomide Derivative; Anti-tumor/Anti-angiogenesis/IMiD Corticosteroid; Anti-inflammatory Antibiotic; Anti-tumor (Autophagy and RNA polymerase inhibitor) |
Phase II | NCT01745588 | ||
| Carfilzomib +Lenalidomide +Dexamethasone |
2nd Gen. Proteasome Inhibitor; Anti-tumor Thalidomide derivative; Anti-tumor/Anti-angiogenesis/IMiD Corticosteroid; Anti-inflammatory |
Phase II |
NCT01863550 NCT01816971 |
||
| NOVEL TARGETED REAGENTS | 1 | Elotuzumab Daratumumab |
CS1 inhibitor; Anti-tumor, targets CS1 expressing myeloma cells CD38 inhibitor; Anti-tumor, promotes myeloma apoptosis. NK cell activation |
Phase II Phase II/III Phase I Phase III |
NCT01668719 NCT02419118 NCT02252263 NCT02076009 |
| 2 | Panobinostat | Hydroxamic acid; Anti-tumor (Cell cycle arrest) Anti-angiogenic | Phase I/II Phase I |
NCT01549431 NCT01301807 |
|
| 3 | Oprozomib Ixazomib |
2nd Gen. Epoxyketone Proteasome Inhibitor; Anti-tumor 2nd Gen. Oral Proteasome Inhibitor; Anti-tumor |
Phase II Phase I Phase III Phase III |
NCT01881789 NCT02072863 NCT01564537 NCT01850524 |
|
| 4 | Dasatinib Trametinib GSK2141795 Dinaciclib |
SRC Tyrosine Kinase Inhibitor; Anti-tumor, inhibits proliferation MEK inhibitor; Anti-tumor, inhibits proliferation Akt inhibitor; Anti-tumor, inhibits proliferation, promotes apoptosis CDK inhibitor; Anti-tumor: Inhibits cell cycle, and induces apoptosis. |
Phase I/II Phase I/II Phase II Phase II Phase II Phase I |
NCT01609816 NCT01643603 NCT01989598 NCT02140840 NCT01989598 NCT01711528 |
|
| 5 | Pembrolizumab Nivolumab Ipilimumab CAR-T Lirilumab |
PD-1 inhibitor; T-cell activation PD-1 inhibitor; T-cell activation CTLA-4 inhibitor; T-cell activation Modified T-cells to target myeloma specific antigens KIR inhibitor; NK cell activation |
Phase I Phase I/II Phase I Phase I/II Phase I Phase I Phase I/II |
NCT02036502 NCT02289222 NCT01592370 NCT01822509 NCT00060372 NCT02215967 NCT01886976 |
|
| 6 | ALT-803 Silituximab |
IL-15R agonist; NK and CD8+ T-cell activation. IL-6 neutralizing antibody; Prevents IL-6 utilization by myeloma |
Phase I/II Phase I/II Phase II |
NCT01885897 NCT02099539 NCT01484275 |
|
Novel targeted reagents are divided into 1. Targeted antibody based therapies, 2. Histone deacetylase inhibitors, 3. Kinase inhibitors, 4. Immunotherapies and 5, Cytokine targeted therapies. Information obtained from the National Institutes of Health (www.clinicaltrials.gov).
The impact of hematopoietic derived cells on myeloma progression
The bone marrow microenvironment is rich in HSCs and, HSC derived myeloid and lymphoid cells that form the cellular components of blood, have been identified as playing causal but in some cases protective roles in the progression of the disease.
Myeloid Derived cells in myeloma-bone microenvironment
Hematopoietic stem cells can differentiate into myeloid cells including osteoclasts, myeloid derived suppressor cells (MDSCs), macrophages, dendritic cells, neutrophils, megakaryocytes and mast cells that play roles in innate and adaptive immunity.
Osteoclasts
Bone destruction is a hallmark of myeloma and is mediated by osteoclasts [11]. Osteoclasts are generated by the fusion of myeloid/monocytic precursor cells in response to potent osteoclastogenic factors such as receptor activator of nuclear kappa B ligand (RANKL) and interleukins (ILs) [17]. Further, heightened AKT activity in bone marrow monocytes from myeloma patients can lead to elevated expression of the RANK receptor on osteoclast precursor cells. These data suggest that in the bone marrow of patients, osteoclast precursor cells are primed for RANKL mediated osteogenesis [18]. Myeloma cells also directly promote osteoclast formation via the endogenous expression of RANKL, tumor necrosis factor alpha (TNFα) and macrophage inflammatory protein 1alpha (MIP1α) [19–23]. In addition, myeloma cells further enhance osteoclastogenesis by down regulating expression of the RANKL decoy receptor, osteoprotegerin (OPG), produced by osteoblasts and endothelial cells [24, 25]. Once generated, osteoclasts form a resorptive seal on the mineralized bone matrix surface and degrade the bone by secreting hydrochloric acid and acidophilic collagenases such as cathepsin K [26]. It has been hypothesized that myeloma cells may also induce bone destruction directly, forming “osteoclast-like” cells capable of bone resorption at least in vitro [27, 28]. Intriguingly, 30% of the osteoclast nuclei in myeloma patients were identified to contain transcriptionally active chromosomes of myeloma cells origin, suggesting that myeloma cells may fuse with normal osteoclasts and potentially, influence their functionality [29]. As expected, the formation of osteolytic lesions occurs in sites adjacent to myeloma cells and resorption of the bone matrix results in the release of sequestered growth factors such as TGFβ and insulin like growth factor-I (IGF-I) that in turn promote myeloma survival and growth [30]. Osteoclasts can also directly stimulate myeloma proliferation [31]. Cell-cell contact between myeloma cells and osteoclasts, increased cell growth and survival, partially due to an interleukin-6 (IL-6) and osteopontin mediated mechanism [32]. Bisphosphonates and monoclonal antibodies to RANKL are commonly used approaches to limiting osteoclast activity [33, 34]. Surprisingly, given the role of the osteoclast in supporting myeloma growth, inhibition of osteoclast formation/function with RANKL blocking antibodies or bisphosphonates does not extend overall survival with the exception of some subset groups [12, 35]. However, the therapies do significantly delay skeletal related events such as pathological fracture and therefore importantly, reduce disease-associated morbidity [6, 36].
Myeloid derived suppressor cells
In healthy individuals, a small number of immature myeloid cells (IMCs) are present in the bone marrow. IMCs are capable of differentiating into macrophages, dendritic cells and granulocytes. However, in response to tumor-derived factors such as vascular endothelial growth factor (VEGF), granulocyte macrophage colony stimulating factor (GM-CSF) and IL-6, differentiation is blocked, leading to the rapid expansion and accumulation of immature MDSCs, that can make the tumor microenvironment immune-privileged by inhibiting the cytotoxic effects of T-cells and contribute to cancer progression and metastasis [37, 38]. In mice, MDSC can broadly be defined as monocytic (CD11b+GR-1+Ly6C+) and granulocytic (CD11b+GR-1+Ly6G+) MDSC, with both populations differing in their mechanisms of T-cell suppression. Human MDSCs are less defined with CD11b+ CD33+HLA-DRlow/− commonly used as a marker [39]. Analysis of immunocompetent mouse models of myeloma has revealed an expansion of MDSC in the bone marrow, with monocytic MDSC found to be the predominant population [40, 41]. In addition to their immunomodulatory effects, MDSCs also can also differentiate into other cell types depending on the presence of signaling cues in the cancer microenvironment. For example, MDSCs isolated from the bone marrow of the 5TGM1 syngeneic murine myeloma model were found to have a greater propensity to differentiate into osteoclasts than immature myeloid cells, both in vitro and in vivo with studies in breast cancer demonstrating the incorporation of MDCSs into the endothelium during angiogenesis [42, 43].
MDSCs represent an exciting area for therapeutic intervention with strategies focusing on depletion, inhibition of expansion, limiting T-Cell suppression or stimulating differentiation [38]. Direct targeting of MDSCs is also possible with antibodies that target growth factors such as GM-CSF, macrophage colony-stimulating factor 1 receptor (CSF1R), VEGF and chemokines such as c-x-c chemokine receptor 4 (CXCR4) and chemokine (CC motif) ligand 2 (CCL2) that prevent MDSC expansion and mobilization in pre-clinical studies [44]. The cytotoxic drug 5-Fluorouracil has also been demonstrated to deplete MDSC. Treatment of a mouse myeloma model with 5-fluorouracil significantly inhibited MDSC populations, and decreased tumor burden [45]. Additionally, phosphodiesterase-5 inhibitors have been demonstrated to down-regulate MDSC immunosuppressive pathways, restoring T-cell antitumor activity in vivo. Treatment of PBMCs isolated from myeloma patients with the phosphodiesterase inhibitor, Sildenafil, restored CD4+ T-cell proliferation [46]. Phosphodiesterase-5 inhibition has also been shown to restore responsiveness to lenalidomide in patients with refractory myeloma with possible mechanisms of immune activation noted [47]. This study indicates that MDSCs protect myeloma cells and that MDSC elimination may render the disease susceptible to immune and chemotherapy based treatments.
Macrophages
Macrophages have long been implicated in the progression and metastasis of several solid cancers [48]. Macrophage polarization into a spectrum of phenotypes is dictated by cytokines and growth factors present in the tumor microenvironment. The “anti-tumor” phenotype is characterized by the expression of TNF-α, interleukin-1 (IL-1) and interleukin-12 (IL-12) and has noted protective effects while the “pro-tumor” phenotype, characterized by interleukin-10 (IL-10) production can contribute to the progression of the disease by stimulating proliferation, angiogenesis, suppressing the immune system, protecting against chemotherapy induced apoptosis [49, 50]. In myeloma, blood-derived monocytes are recruited to the bone marrow by myeloma derived c-x-c motif chemokine 12 (CXCL12) and undergo maturation to a pro-tumor macrophage phenotype in response to tumor-derived IL-10 [51]. Subsequently, the pro-tumor/M2 generated macrophages enhance myeloma cell proliferation and survival by secreting high levels of IL-6 and IL-10 [52–54]. Myeloma induced macrophages may also play roles in drug resistance to chemotherapeutic agents and in promoting angiogenesis [55–57].
Tumor associated macrophages (TAMS) are a subset of the M2 phenotype and can promote myeloma survival through mechanisms including immunosuppression and chemotherapy resistance [58]. Targeting these tumor-promoting cells may not only lead to new therapeutic strategies but may enhance currently used therapeutic agents. Repolarizing TAMs to an “anti-tumor” phenotype or their depletion with CSF1R based therapies are important immunotherapeutic strategies under investigation [59, 60]. Alternatively, TAMS can be directly targeted. For example, anti-CD40 agonists and targeted monoclonal antibodies have been demonstrated to activate antigen presenting cells, in particular macrophages, with enhanced anti-tumor effects achieved with co-administration of Toll Like Receptor-9 agonist, CpG [61]. This strategy was recently applied to a mouse model of refractory myeloma, resulting a significant increase in overall survival following the use of an anti-CD40 mAB [62]. Preventing monocyte recruitment is also possible by targeting chemokines including the CXCR4/CXCL12 axis [51].
Dendritic Cells
Dendritic cells are antigen presenting cells that link innate and adaptive immunity by regulating T-cell behavior. In humans, dendritic cells can be functionally and phenotypically categorized into myeloid dendritic cells and plasmoid dendritic cells. Plasmoid dendritic cells play a role in the regulation and differentiation of normal B-cells [63]. Myeloma patients have noted dysfunctional plasmoid dendritic cells with impaired T-cell stimulatory abilities compared to healthy controls reported [64]. The number of plasmoid dendritic cells is significantly increased in the bone marrow of myeloma patients compared to healthy individuals, with only a modest increase in peripheral blood [65]. One such mechanism of immune tolerance is a result of reduced dendritic cell maturation and antigen presentation, mediated in part by IL-6 [66]. Additionally, dendritic cells may directly influence myeloma growth, with co-culture of dendritic cells increasing clonogenicity of myeloma cells in vitro. Many studies have demonstrated the value of autologous transplantation of dendritic cells as a vaccination or as a means of immune system augmentation for cancer treatment. Direct targeting of cancer associated dendritic cells may also be a potentially impactful treatment. For example, inhibition of RANKL and A Proliferation-Inducing Ligand (APRIL) pathways prevented dendritic cell enhancement of clonogenicity [67]. Plasmoid dendritic cells were demonstrated to confer resistance to bortezomib, increasing the IC50 of myeloma cells in vitro by up regulating proteasome activity [65]. Dendritic cells may also directly contribute to myeloma-induced osteolysis by differentiating into osteoclasts [68]. Induction of osteoclastogenesis in dendritic cells is believed to be induced by interleukin-17A in myeloma patients, with levels significantly elevated in the bone marrow and plasma compared to healthy individuals [69].
Other myeloid cell lineages are also being investigated in regards to their role in the myeloma progression. For example, neutrophils isolated from myeloma patients were found to have a reduced phagocytic ability, and inhibit T cell function. These data suggest that neutrophils may contribute to immune suppression in myeloma patients [70]. Megakarocytes and eosinophils are known to be involved in the survival of normal plasma cells, with their ability to promote myeloma cell survival in early stages of growth due to the production of IL-6 and APRIL [71]. Mast cells are another cellular component of myeloma and can contribute to neovascularization by directly incorporating into the vasculature [72]. Mast cell density is associated with increased vascular density, and myeloma proliferation, indicating that mast cells directly promote myeloma progression [73]. Therapies that focus on these myeloid cells types could therefore potentially be used for myeloma treatments.
Lymphoid Derived cells in myeloma-bone microenvironment
Originating in the bone marrow from a common progenitor, lymphoid cells include B-cells, NK cells and T-cells. Following differentiation, lymphoid cells enter circulation and migrate to the Thymus (T-cells), and lymphoid organs (NK and B-cells) where they can control adaptive immunity.
T-Cells
T-cells play a pivotal role in systemic immunity and are delineated from other leukocytes by the expression of T cells receptors (TCR). Developing in the thymus from hematopoietic stem cells, T-cells have distinct functions both in immunity, and in cancer. T-cells can be broadly categorized into cytotoxic T-cells (CD8+) killing infected and transformed cells, helper T cells (CD4+) playing a role in the adaptive immune system, and regulatory T-cells (CD4+CD25+) mediating immunosuppression and tolerance. In addition to their roles in regulating the immune system, T-cells can also impact normal bone homeostasis and osteolytic and inflammatory bone diseases such as rheumatoid arthritis [74]. In normal bone remodeling, activated CD8+/CD4+ T-cells express RANKL directly stimulating osteoclastogenesis in the absence of osteoblasts. In contrast, production of interferon gamma (IFN-γ) can inhibit T-cell mediated osteolysis [75, 76].
CD4+CD25+FOXP3+ regulatory T-cells (Tregs) are essential for maintaining peripheral T-cell homeostasis and self-tolerance by inhibiting CD4+T cells, CD8+T cells, dendritic cells, macrophages, B cells and NK cells. Tregs can be found in the thymus and the bone marrow of healthy individuals is rich in this cell type [77]. In solid tumors Tregs play critical roles in immune evasion and making the tumor microenvironment an immune privileged site. The picture in myeloma is not as clear. Studies have defined higher levels of circulating Tregs in patients with asymptomatic and symptomatic myeloma compared to healthy control individuals that could suppress naïve T-cell (CD4+CD25− T-cells) proliferation and activation by secreting factors including TGFβ and IL-10 [78–80]. Further, elevated levels of Tregs were associated with a decrease in overall survival and progression free survival compared to myeloma patients with lower Treg numbers [81, 82]. Interestingly, analysis of myeloma patient bone marrow revealed the Tregs numbers to match that of healthy individuals, indicating myeloma cells do not recruit Tregs to the bone marrow and that other immune cells may be responsible for disease related immune tolerance. However, given the functionality of Tregs in the bone marrow, therapeutic targeting of these cells may yet prove an alternative means with which to target myeloma and augment existing therapies [83].
Recently, a regulatory subset of CD8+ T-cells has been identified in myeloma patients, with the ability to suppress CD4+ T-cell proliferation via the secretion of IFN-γ [84]. The clinical role of this subset of T-cells is currently unknown, although they are believed to contribute to immune suppression in myeloma. While myeloma patients have functional cytotoxic CD8+ T-cells, myeloma cells escape the immune system resulting in their expansion within the bone marrow. This is a result of impaired plasma cell recognition, due to alterations in antigen presentation machinery on the transformed plasma cells [85, 86]. One such mechanism of escape includes the expression of carcinoembryonic antigen-related cell adhesion molecule-6 (CEACAM-6) on the plasma cells surface. Binding and cross linking of cytotoxic T-cells to the CEACAM-6 receptor inhibits T-cell activation and response to malignant plasma cells [87].
T-cell targeted therapies are currently providing exciting results in clinical trials in solid cancers and in hematological malignancies such as multiple myeloma. In addition to clinical trials (NCT02215967, NCT00881920 and NCT01886976) focusing on modulating T-cells to display chimeric antigen receptors (CAR T-cells) that allow for the specific targeting of myeloma; novel therapies are also being implemented that make myeloma cells more “visible” to the immune system [62]. The cytotoxic activity of T-cells in the immune microenvironment can be suppressed by the activation of a number of receptors expressed on the T-cell including Programmed Cell Death-1 receptor (PD-1) and cytotoxic T-Lymphocyte-associated protein 4 (CTLA-4). Therefore, myeloma cells expressing PD-1 ligand (PD-L1) can promote immune tolerance [88]. PD-L1 is highly expressed by myeloma cells and its expression can be induced via interaction with the surrounding bone marrow stroma [88, 89]. Notably, PD-1 expression is also enhanced on T-cells isolated from myeloma patients [90]. Culture of myeloma cells with CD4+ T-cells resulted in the generation of Tregs with immune suppressive activities, highly expressing PD-1 [91]. The immunomodulatory mechanistic effects of lenalidomide in activating NK and cytotoxic T-cells may be in part explained by reduced PD-1 and PD-L1 expression in T-cells and myeloma cells respectively [92]. Pre-clinical studies using anti-PD-L1 antibodies or PD-1 deficient mice have shown significant suppression of myeloma growth, and have provided solid rationale for a number of ongoing clinical trials [93–95]. Both PD-1/PD-L1 antibodies are currently under investigation as a single agent (NCT01375842) or in combination with other agents including Lenalidomide (NCT02077959), and with myeloma vaccines (e.g. NCT01067287). PD-1 inhibition is also been investigated in combination with other T-cell co-inhibitor molecules such as cytotoxic T-lymphocyte-associate protein 4 (CTLA-4) (NCT01592370).
B-Cells
B-cell development results in the formation of terminally differentiated, antibody producing plasma cells [96]. Myeloma is a B-cell malignancy, and individuals with myeloma have a reduced level of normal immunoglobulin (serum IgM ∼1.9mg/ml), associated with the suppression of B-cell differentiation that may be explained by an arrest in B-cell maturation [97]. Symptomatic myeloma patients have lower numbers of B-cells compared to age matched controls. In particular, memory B-cells were reduced, with an increased reduction in myeloma patients compared to individuals with early stage disease. This reduction in memory cells was associated with a reduction in antibodies, and memory recall, resulting in increased infection and a reduced response to vaccinations [98]. A number of therapies directed towards B-cell antigens are currently under investigation to directly target myeloma cells, including antibodies towards B-cell maturation antigen (BCMA) and vaccines targeting CD138 [99, 100]. Targeting these cell surface markers, and others, is the focus of ongoing clinical trials (NCT02064387) (NCT01718899).
NK-Cell
Natural killer cells (NKs) can identify cancer cells in the absence of major histocompatibility complex (MHC) presentation. NK activity negatively correlates with disease progression in myeloma patients [101]. Agents such as bortezomib, and lenalidomide have been in part, shown to function by enhancing NK anti-tumor activity towards myeloma cells [102, 103]. Many therapeutic strategies to enhance NK-cell activity are currently under investigation. PD-1 has been demonstrated to be expressed by NK cells isolated from myeloma patients, but not from healthy individuals. Inhibition of PD-1 was found to enhance NK cell response to myeloma cells in vitro [104]. Further, administration of NK cells in a mouse xenograft model of myeloma, significantly reduced tumor burden [105]. Clinical trials are currently underway investigating the transplantation of NK cells to myeloma patients (NCT01040026.) Expansion, and activation of human NK cells ex vivo has been demonstrated in the presence of human leukocyte antigen (HLA) deficient cell line K562 genetically modified to express an activated T-Cell ligand (41BBL) and interleukin-15 (IL-15.) Safe auto- or allo-transplant of educated NK cells has been demonstrated in patients [106]. Similarly to T-cells, CAR-NK cells are also under investigation for the treatment of myeloma, with CS1 as a potential therapeutic target [107].
Taken together, our increased understanding of how the innate and adaptive arms of the immune system contribute to, or protect against, myeloma progression has revealed many new therapeutic approaches that are being translated to the clinical setting.
Mesenchymal derived cells play crucial roles in myeloma progression (MSC)
Mesenchymal stem cells (MSCs) give rise to bone, cartilage, adipose, muscle and dermal tissues. The bone marrow is rich in MSCs and roles for MSCs and their derivatives; namely, osteoblasts, adipocytes and chondrocytes have been shown to play novel roles in myeloma progression.
MSCs
In primary solid cancers, MSCs have been shown to differentiate into cancer-associated fibroblasts (CAFs) that can contribute to disease progression [108]. Given that bone is rich in MSCs, this intriguing cell population and its role in myeloma progression has been under extensive investigation. Myeloma cell interaction with bone marrow stromal MSCs promotes the secretion of cytokines (eg. IL-6, and VEGF), chemokines (eg. macrophage inflammatory protein (MIP-1)) and the expression of adhesion molecules (eg. integrins) [109]. IL-6 is a key cytokine in the progression of the disease, and is secreted by both myeloma and bone marrow stromal cells [110]. Originally identified as a regulator of normal B-cell differentiation, it has been shown to promote myeloma cell proliferation and protect cells from apoptosis [111]. Cell-cell contact between BMSC and myeloma cells is also essential for the development chemotherapeutic drug resistance in myeloma patients [112]. The expression and activation of adhesion molecules are essential for mediating these cellular interactions. Integrins, including VLA-4 (α4β1) facilitate binding of myeloma cells to stromal cells via vascular cell adhesion molecule-1 (VCAM-1), and to the extracellular matrix components such as fibronectin [113]. Growth factors such as TNF-α can up-regulate VLA-4 expression in myeloma cells, enhancing homing and adhesion to fibronectin and stromal cells [114]. CD138, a cell surface marker commonly used to identify myeloma cells, is a proteoglycan responsible for binding to extracellular matrix proteins, as well as regulating integrin activity [115]. Cell-Cell adhesion modulates pathways in both the myeloma and stromal components, which is ultimately sufficient to mediate a multi-drug resistant phenotype commonly referred to as cell adhesion mediated drug resistance (CAM-DR). Data suggest that CAM-DR results in a failure to eradicate minimal residual disease following delivery of standard of care agents and may contribute to the emergence of acquired drug resistance in myeloma [112, 116, 117]. Although MSCs from healthy and myeloma patients are capable of inducing resistance in vitro, myeloma derived MSCs could inhibit the effects of bortezomib on cell growth to a greater extent [118]. One mechanism by which myeloma cells become resistant is by increased expression of the apoptosis suppressor protein survivin by cell contact [119]. In addition to enhancing myeloma resistance to chemotherapy, IL-6 can also directly stimulate osteoclast formation and RANKL production in stromal cells [120]. Similarly, myeloma derived IL-1β is also known to stimulate osteoclastogenesis by increasing expression of adhesion molecules and paracrine secretion of IL-6 [121]. Further, myeloma cells produce chemokine MIP-1α, stimulating osteoclast formation and adhesion to BMSC by enhancing cytokine production (eg. IL-6, VEGF) [122].
Because of their pluripotency MSCs can also play a role in the myeloma bone microenvironment by differentiating into a number of cell types. Differential gene expression analysis revealed genes such as IL-6 and Dickopf-1 (DKK-1) are up regulated in myeloma derived MSCs compared to healthy controls [109]. Further, MSCs isolated from myeloma patients have a reduced ability to differentiate into osteoblasts, with the down-regulation of osteogenic genes such as Wnt1 and Wnt2 implicated. Myeloma derived factors such as the Wnt antagonist, DKK-1, can also limit the differentiation of MSCs into osteoblasts. MSCs isolated from the bone marrow stroma of myeloma patients also produce notably higher endogenous levels of DKK-1 [123]. MSCs have immunomodulatory roles that affect the proliferation and function of T-cells both in vivo and in vitro. MSC isolated from myeloma patients expressed high levels of TGFβ, IL-6, interleukin-3 (IL-3), TNF-α and RANKL, and decreased expression of FAS-L and TGFβ compared to those from healthy individuals. T-cells from normal individuals were capable of stimulating osteoblastic differentiation, with this ability reduced in those from myeloma patients or cultured with myeloma-MSC [124, 125].
It is important to note that MSCs in some contexts can have protective roles in tumor progression. For example, intra-tibial injections of myeloma naïve MSCs were demonstrated to delay disease due to increased bone formation and reduced myeloma growth [126]. The inhibitory effect of MSCs on myeloma growth, are partially explained by Fas-L induced apoptosis [127]. Fas-L expression is significantly decreased in myeloma-derived MSC, potentially explaining conflicting observations in MSC focused studies [126]. Nevertheless, these studies open up the question of modulating MSCs, or transplantation of normal MSC to treat myeloma, however understanding the mechanisms by which MSC inhibit myeloma may provide a safer therapeutic strategy. Given our knowledge regarding MSC derived IL-6 for example, therapies generated either against the cytokine directly or the IL-6 receptor/pathway would be logical choices for the design of targeted therapies. Siltuximab is a monoclonal against IL-6 and is well tolerated in patients (NCT01484275)[128]. However, transplant ineligible patients that underwent Siltuximab treatment in combination with velcade, melphalan and prednisone (VMP) did not demonstrate improved complete response rates compared to the VMP arm alone [129]. Since IL-6 is involved in early myeloma-stroma interactions and survival, it is possible that application of the IL-6 therapy at earlier stages of the disease may prove more beneficial. In this regard, Siltuximab is currently under investigation in patients with asymptomatic disease (NCT01484275.)
Novel molecules are also being investigated that can potentially block the interaction between MSCs and stromal cells and the extracellular matrix. One such example is HYD1; this short peptide has been demonstrated to bind adhesion molecules CD44 and VLA-4 [130]. HYD1 treatment prevented myeloma cells adhesion to fibronectin, and reversed adhesion mediated drug resistance in a co-culture with bone marrow stromal cells. In addition, HYD1 induced necrosis in myeloma cell lines in vitro. Tumor burden was significantly reduced with HYD1 treatment in vivo, making HYD1 an attractive therapeutic agent [131].
Osteoblasts/osteocytes
Osteoblast mediated bone formation/mineralization is severely restricted in myeloma patients. The factors involved in osteoblast suppression have been widely described, with the Wnt pathway and myeloma-derived factors, such as IL-3 implicated [132]. Many therapeutic agents are currently under investigation to stimulate bone formation or block agonists in myeloma patients. These include but are not limited to potent osteogenic factors such as Wnt, and DKK-1, fibroblast growth factor 23 (FGF23) and heparanse [52, 133, 134]. The DKK-1 inhibitor BHQ880, increases osteoblast number and trabecular bone volume in an in vivo myeloma model [135]. In clinical trials BHQ880 showed a trend towards increased bone mineral density when used in combination with a bisphosphonate for the treatment of relapsed myeloma [136]. Other Phase I/II clinical trials examining the efficacy of BHQ880 have been completed with reports from those trials pending (NCT01302886, NCT00741377 and NCT01337752).
A recent study demonstrated that quiescent myeloma cells are primarily located in the osteoblastic niche in a dormant stem like state compared to those isolated from the vascular niche [137]. Emerging data, suggests that these dormant cells are protected from chemotherapy, leading to repopulation of the tumor and ultimately, patient relapse [138]. In some instances, osteoblasts can inhibit the growth of myeloma cells and induce apoptosis in part explaining why osteoblast activity is so suppressed in patients with myeloma [139]. Similarly, the majority of patient derived osteoblasts were found to inhibit myeloma growth in co-culture and reciprocally, myeloma suppression of osteoblast activity correlated with the degree of skeletal disease [139, 140]. Mechanistically, osteoblasts appear to suppress myeloma growth via the production of decorin, a small leucine-rich proteoglycan known to be unregulated in differentiating osteoblasts and a sink for TGFβ. Osteoblast-derived, or recombinant decorin, upregulated cell-cycle regulator p21, and induced myeloma cell apoptosis [141]. Levels of decorin were shown to be significantly decreased in the bone marrow of myeloma patients compared to that of healthy individuals [142].
During the bone remodeling process, osteoblasts are embedded into the bone matrix where they terminally differentiate into mechanosensing osteocytes. There is increasing evidence that osteocytes regulate bone remodeling, stimulating osteoclast formation and inhibiting osteoblasts by secretion of sclerostin. Osteocytes have also been identified as a major source of RANKL [143]. To date, the role of osteocytes in myeloma is relatively unknown. Transcriptional analysis of osteocytes isolated from myeloma patients revealed changes in the expression of approximately 1800 genes, compared to healthy controls. These data indicate that myeloma cells may influence osteocyte function [144]. Analysis of myeloma patient biopsies revealed a significant decrease in the number of osteocytes, compared to healthy individuals. The reduction in osteocyte number was equated to increased apoptosis [145]. Osteocyte apoptosis can drive osteoclast recruitment and formation by as yet undefined mechanisms. The use of fluorescently labeled bisphosphonate analogue has also revealed uptake in the osteocytic lacunae indicating potential additional sites of action [146]. In vitro studies, have suggested bisphosphonates may protect osteocytes from apoptosis at low concentrations, suggesting that bisphosphonates may have anti-apoptotic effects on osteocytes in vivo [147]. Trials are currently underway exploring the factors that control this intriguing cell type in myeloma patients (NCT02212262).
Adipocytes
Adipocytes are responsible for fat storage in the body make up a large component of bone marrow, with the number of adipocytes increasing with age. In the setting of healthy bone, the adipokines; leptin and adiponectin, have been shown to promote osteoblast differentiation, proliferation, and mineralization, but prevent osteoclastogenesis [148]. These adipokines also drive the growth of solid tumors, such as prostate cancer, however their role in hematological cancers is not as widely understood [149]. The culture of myeloma cell lines with adipocyte conditioned media, revealed soluble factors could promote myeloma cell proliferation, migration while inhibiting apoptosis potentially via leptin [150]. Additionally, adipocytes secrete significant amounts of IL-6 [151]. By secreting heparanase, myeloma cells can also promote MSC to adipocyte differentiation, thereby suppressing bone formation by limiting the number of stem cells that can commit to the osteoblast/osteogenic program [134].
Increasing evidence now indicates a link between obesity and myeloma incidence [152]. In fact, leptin levels were found to be increased in the serum of non-obese myeloma patients, with concentration correlating with disease progression [153]. Further, adiponectin has been associated with a reduction in myeloma cell survival due to the suppression of lipogenesis [154, 155]. Pre-clinical studies also support a role for adipokines in the progression of the disease. The 5TGM1 mouse model grows in syngeneic C57BL/KaLwRij mice, but not in the closely related C57BL/6 mouse strain. A recent study, demonstrated that when C57BL/6 were fed a high fat diet, the 5TGM1 cells were now able to grow in the bone marrow and induce osteolysis indicating a key role for adipocytes/adipokines in myeloma [156]. Interestingly, although myeloma incidence is higher in obese patients, the disease takes longer to progress with higher overall survival rates noted [157]. Although much of the data suggests adipocytes promote myeloma, this study indicates that further investigation is required before we can begin to consider adipocytes and adipokines as therapeutic targets.
Collectively, these data illustrate how mesenchymal derived cells can play pivotal roles in myeloma growth and therapy resistance and that targeting the mesenchymal arm of the myeloma-bone microenvironment can be of significant benefit for patients.
Targeting early microenvironmental changes to prevent symptomatic myeloma
The therapeutic strategies discussed above are largely geared toward tackling active symptomatic myeloma disease or the cells of the established myeloma-tumor microenvironment. Earlier intervention may ultimately have a more profound impact on overall survival. In the majority of patients, myeloma is preceded by precursor stages known as monoclonal gammopathy of undetermined significance (MGUS) and smoldering myeloma (SMM)[2]. These stages are typically categorized by serum immunoglobulin levels (MGUS <30g/l, SMM >30g/l). The median time of progression to overt myeloma varies greatly from 2 to 10 years, with a rate of progression of MGUS to myeloma at 0.5–1.5% per year. The risk of progression from SMM is significantly greater, with approximately 10% of patients progressing to overt disease within the first 5 years [158]. Currently, patients diagnosed with MGUS or SMM are simply monitored until the onset of symptomatic disease. The reasons for delaying therapeutic intervention include drug toxicity, as well of the risk of developing drug resistance. However, it is recognized that that there are sub-groups of patients within these categories that are at “higher risk” of progression but their identification remains a challenge. A number of markers including soluble free light chain (FLC) ratios (normal ratio for κ/λ is 0.26–1.65), and clonal bone marrow plasma cell percentage (>60% defined as myeloma) have been identified [159]. Recent data suggests that defining systemic factors capable of modulating the bone microenvironment may provide insight into the identification of those patients at high risk. Although this MGUS stage does not present with osteolytic lesions, patients are more susceptible to fracture as a result of systemic osteoporosis [160]. These findings suggest that even during MGUS, malignant plasma cells are modulating the skeletal microenvironment. The concept of the “pre-metastatic niche” has been described in a number of solid tumors; therefore one may speculate that myeloma can prepare new bone sites for arrival and colonization [161]. Understanding myeloma colonization mechanisms could limit the systemic nature of the disease [162]. For example, myeloma interactions with MSCs via VLA-4/VCAM-1 promotes the colonization of the disease in the bone marrow and results in increased osteoclastogenesis via IL-6 production [163, 164]. In addition, VLA-4/VCAM-1 interaction has been shown to be important for the homing of myeloma cells to the bone marrow [165]. Emerging studies are also beginning to elucidate roles for exosomes. Exosomes have come to light as key mediators of cell-cell communication, particularly in modulating the pre-metastatic microenvironment to be ready for future metastatic seeding. These nanometer vesicles (50–150nm) of endocytic origin have been shown to transfer proteins, lipids, RNAs, and even DNA between cell types. Released by a variety of cells, proteomic profiling has revealed exosomal content to be cell type specific [166]. Recent data, has implicated myeloma derived exosomes in disease progression by promoting angiogenesis, osteoclastogenesis and mediating drug resistance [162, 167–169]. Further exploration of these cellular and molecular mechanisms could allow for therapeutic intervention to prevent systemic bone microenvironmental changes the development of symptomatic disease or at the very least identify patients that are at a high-risk of progression.
Concluding remarks
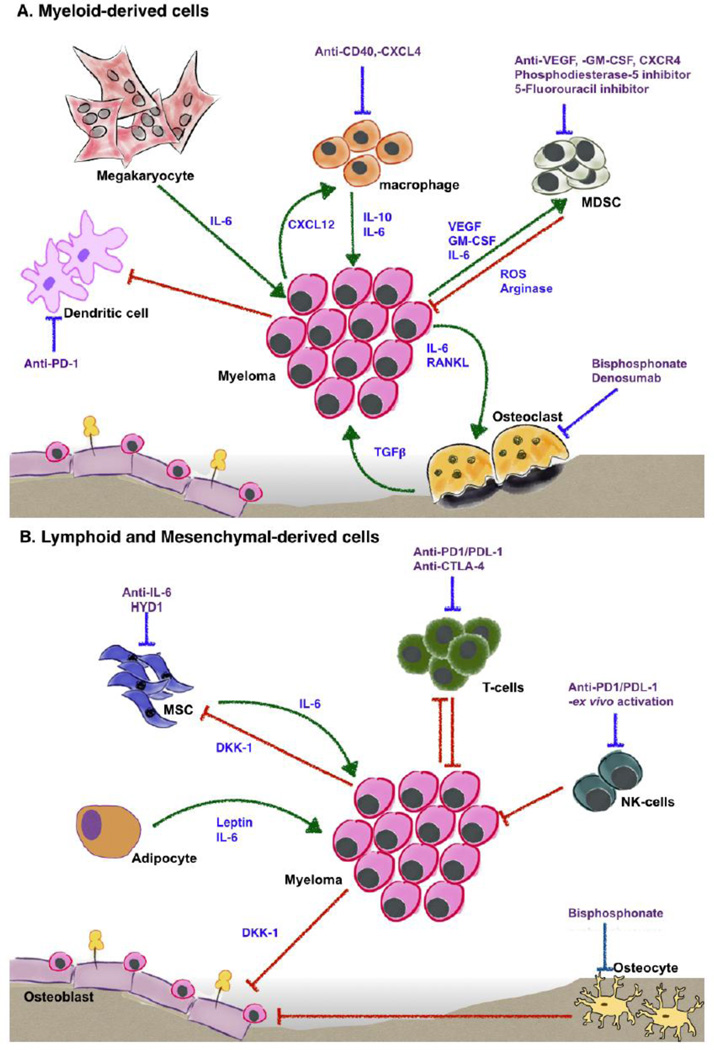
The recent discovery of novel therapeutics such as proteasome inhibitors (bortezomib, and carfilzomib) and lenolidomide has significantly enhanced our ability to treat symptomatic multiple myeloma and extend patient overall survival. The optimal use of these agents, alone or in combination with other novel therapies is the focus of many ongoing clinical trials that no doubt will increase complete response and overall survival rates. However, the genetic heterogeneity underlying myeloma pathogenesis indicates that the emergence of refractory disease is but a matter of time. The surrounding microenvironment of myeloma is critical for the progression of the disease and given its relative genetic stability, presents a logical area for the development of targeted therapies. Clinical trials designed to target immune and stromal components of the microenvironment are ongoing and, in combination with myeloma targeted therapies should get us closer to our ultimate objective of curing the disease (Fig. 1).
Figure 1.
The multiple myeloma bone microenvironment. Our understanding of the “vicious cycle” between myeloma cells, osteoclasts and osteoblasts, can now been updated to include the contribution of other cells in the microenvironment including those of a myeloid (A) and lymphoid/mesenchymal stem cell (B) lineage.
As new treatment strategies come online and begin to impact overall survival, one challenge on the horizon may be how to deal with extramedullary multiple myeloma. In advanced disease stages, myeloma cells can become independent of the bone microenvironment leading to the presentation of soft tissue plasmacytomas. Postmortem studies have revealed that approximately 70% of myeloma patients have extramedullary disease at autopsy [170, 171]. Extramedullary myeloma most frequently occurs at local sites, arising from bone involvement (eg. vertebrae) although plasmacytomas can occur in organs such as the skin, liver and central nervous system [172]. Extramedullary disease is associated with a significant reduction in progression-free, and overall survival [173]. It is too premature to determine whether the incidence of extramedullary disease is increasing with the advent of new therapies but, it is possible that longer overall survival may allow for extramedullary disease to develop. If so, then understanding how myeloma extravasates from the skeletal tissue and occupies soft tissue may be an important area of research in the future.
In conclusion, while multiple myeloma currently remains an incurable disease, there is much optimism moving forward, based on ongoing clinical trials, that meaningful increases in complete response and overall survival rates can be achieved. Future advances in our understanding of the molecular mechanisms driving multiple myeloma and importantly, how the surrounding bone microenvironment controls disease evolution and progression, will surely increase the number of therapeutic options available to the hematology oncologist to eradicate the disease.
Acknowledgements
This work was supported in part by R21CA191981 (CCL & LH).
References
- 1.Mahindra A, Hideshima T, Anderson KC. Multiple myeloma: biology of the disease. Blood Rev. 2010;(24 Suppl 1):S5–S11. doi: 10.1016/S0268-960X(10)70003-5. [DOI] [PubMed] [Google Scholar]
- 2.Ghobrial IM, Landgren O. How I treat smoldering multiple myeloma. Blood. 2014;124:3380–3388. doi: 10.1182/blood-2014-08-551549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edwards CM, Zhuang J, Mundy GR. The pathogenesis of the bone disease of multiple myeloma. Bone. 2008;42:1007–1013. doi: 10.1016/j.bone.2008.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferlay JSI, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr. [Google Scholar]
- 5.Rosen CJ, Ackert-Bicknell C, Rodriguez JP, Pino AM. Marrow fat and the bone microenvironment: developmental, functional, and pathological implications. Crit Rev Eukaryot Gene Expr. 2009;19:109–124. doi: 10.1615/critreveukargeneexpr.v19.i2.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berenson JR, Lichtenstein A, Porter L, Dimopoulos MA, Bordoni R, George S, Lipton A, Keller A, Ballester O, Kovacs M, et al. Long-term pamidronate treatment of advanced multiple myeloma patients reduces skeletal events. Myeloma Aredia Study Group. J Clin Oncol. 1998;16:593–602. doi: 10.1200/JCO.1998.16.2.593. [DOI] [PubMed] [Google Scholar]
- 7.Richardson P, Mitsiades C, Schlossman R, Ghobrial I, Hideshima T, Chauhan D, Munshi N, Anderson K. The treatment of relapsed and refractory multiple myeloma. Hematology Am Soc Hematol Educ Program. 2007:317–323. doi: 10.1182/asheducation-2007.1.317. [DOI] [PubMed] [Google Scholar]
- 8.Anderson KC. Multiple myeloma: new uses for available agents, excitement for the future. J Natl Compr Canc Netw. 2015;13:694–696. doi: 10.6004/jnccn.2015.0206. [DOI] [PubMed] [Google Scholar]
- 9.Abdi J, Chen G, Chang H. Drug resistance in multiple myeloma: latest findings and new concepts on molecular mechanisms. Oncotarget. 2013;4:2186–2207. doi: 10.18632/oncotarget.1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roodman GD. Targeting the bone microenvironment in multiple myeloma. J Bone Miner Metab. 2010;28:244–250. doi: 10.1007/s00774-009-0154-7. [DOI] [PubMed] [Google Scholar]
- 11.Galson DL, Silbermann R, Roodman GD. Mechanisms of multiple myeloma bone disease. Bonekey Rep. 2012;1:135. doi: 10.1038/bonekey.2012.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCloskey EV, Dunn JA, Kanis JA, MacLennan IC, Drayson MT. Long-term follow-up of a prospective, double-blind, placebo-controlled randomized trial of clodronate in multiple myeloma. Br J Haematol. 2001;113:1035–1043. doi: 10.1046/j.1365-2141.2001.02851.x. [DOI] [PubMed] [Google Scholar]
- 13.Croucher PI, De Hendrik R, Perry MJ, Hijzen A, Shipman CM, Lippitt J, Green J, Van Marck E, Van Camp B, Vanderkerken K. Zoledronic acid treatment of 5T2MM-bearing mice inhibits the development of myeloma bone disease: evidence for decreased osteolysis, tumor burden and angiogenesis, and increased survival. J Bone Miner Res. 2003;18:482–492. doi: 10.1359/jbmr.2003.18.3.482. [DOI] [PubMed] [Google Scholar]
- 14.Ribatti D, Vacca A. The role of inflammatory cells in angiogenesis in multiple myeloma. Adv Exp Med Biol. 2014;816:361–376. doi: 10.1007/978-3-0348-0837-8_14. [DOI] [PubMed] [Google Scholar]
- 15.Ribatti D, Basile A, Ruggieri S, Vacca A. Bone marrow vascular niche and the control of angiogenesis in multiple myeloma. Front Biosci (Landmark Ed) 2014;19:304–311. doi: 10.2741/4209. [DOI] [PubMed] [Google Scholar]
- 16.De Bruyne E, Menu R, Van Valckenborgh E, De Raeve H, Van Camp B, Van Riet I, Vanderkerken K. Myeloma cells and their interaction with the bone marrow endothelial cells. Curr Immunol Rev. 2007;3(1):41–55. [Google Scholar]
- 17.Henriksen K, Karsdal MA, Martin TJ. Osteoclast-derived coupling factors in bone remodeling. Calcif Tissue Int. 2014;94:88–97. doi: 10.1007/s00223-013-9741-7. [DOI] [PubMed] [Google Scholar]
- 18.Cao H, Zhu K, Qiu L, Li S, Niu H, Hao M, Yang S, Zhao Z, Lai Y, Anderson JL, et al. Critical role of AKT protein in myeloma-induced osteoclast formation and osteolysis. J Biol Chem. 2013;288:30399–30410. doi: 10.1074/jbc.M113.469973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raisz LG, Luben RA, Mundy GR, Dietrich JW, Horton JE, Trummel CL. Effect of osteoclast activating factor from human leukocytes on bone metabolism. J Clin Invest. 1975;56:408–413. doi: 10.1172/JCI108106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pearse RN, Sordillo EM, Yaccoby S, Wong BR, Liau DF, Colman N, Michaeli J, Epstein J, Choi Y. Multiple myeloma disrupts the TRANCE/ osteoprotegerin cytokine axis to trigger bone destruction and promote tumor progression. Proc Natl Acad Sci U S A. 2001;98:11581–11586. doi: 10.1073/pnas.201394498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han JH, Choi SJ, Kurihara N, Koide M, Oba Y, Roodman GD. Macrophage inflammatory protein-1alpha is an osteoclastogenic factor in myeloma that is independent of receptor activator of nuclear factor kappaB ligand. Blood. 2001;97:3349–3353. doi: 10.1182/blood.v97.11.3349. [DOI] [PubMed] [Google Scholar]
- 22.Farrugia AN, Atkins GJ, To LB, Pan B, Horvath N, Kostakis P, Findlay DM, Bardy P, Zannettino AC. Receptor activator of nuclear factor-kappaB ligand expression by human myeloma cells mediates osteoclast formation in vitro and correlates with bone destruction in vivo. Cancer Res. 2003;63:5438–5445. [PubMed] [Google Scholar]
- 23.Heider U, Langelotz C, Jakob C, Zavrski I, Fleissner C, Eucker J, Possinger K, Hofbauer LC, Sezer O. Expression of receptor activator of nuclear factor kappaB ligand on bone marrow plasma cells correlates with osteolytic bone disease in patients with multiple myeloma. Clin Cancer Res. 2003;9:1436–1440. [PubMed] [Google Scholar]
- 24.Giuliani N, Bataille R, Mancini C, Lazzaretti M, Barille S. Myeloma cells induce imbalance in the osteoprotegerin/osteoprotegerin ligand system in the human bone marrow environment. Blood. 2001;98:3527–3533. doi: 10.1182/blood.v98.13.3527. [DOI] [PubMed] [Google Scholar]
- 25.Seidel C, Hjertner Ø, Abildgaard N, Heickendorff L, Hjorth M, Westin J, Nielsen JL, Hjorth-Hansen H, Waage A, Sundan A, et al. Serum osteoprotegerin levels are reduced in patients with multiple myeloma with lytic bone disease. Blood. 2001;98:2269–2271. doi: 10.1182/blood.v98.7.2269. [DOI] [PubMed] [Google Scholar]
- 26.Crockett JC, Rogers MJ, Coxon FP, Hocking LJ, Helfrich MH. Bone remodelling at a glance. J Cell Sci. 2011;124:991–998. doi: 10.1242/jcs.063032. [DOI] [PubMed] [Google Scholar]
- 27.McDonald DF, Schofield BH, Prezioso EM, Adams VL, Frondoza CA, Trivedi SM, Craig C, Humphrey RL. Direct bone resorbing activity of murine myeloma cells. Cancer Lett. 1983;19:119–124. doi: 10.1016/0304-3835(83)90145-3. [DOI] [PubMed] [Google Scholar]
- 28.Calvani N, Cafforio P, Silvestris F, Dammacco F. Functional osteoclast-like transformation of cultured human myeloma cell lines. Br J Haematol. 2005;130:926–938. doi: 10.1111/j.1365-2141.2005.05710.x. [DOI] [PubMed] [Google Scholar]
- 29.Andersen TL, Boissy P, Sondergaard TE, Kupisiewicz K, Plesner T, Rasmussen T, Haaber J, Kolvraa S, Delaisse JM. Osteoclast nuclei of myeloma patients show chromosome translocations specific for the myeloma cell clone: a new type of cancer-host partnership? J Pathol. 2007;211:10–17. doi: 10.1002/path.2078. [DOI] [PubMed] [Google Scholar]
- 30.Lentzsch S, Ehrlich LA, Roodman GD. Pathophysiology of multiple myeloma bone disease. Hematol Oncol Clin North Am. 2007;21:1035–49. doi: 10.1016/j.hoc.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 31.Yaccoby S, Pearse RN, Johnson CL, Barlogie B, Choi Y, Epstein J. Myeloma interacts with the bone marrow microenvironment to induce osteoclastogenesis and is dependent on osteoclast activity. Br J Haematol. 2002;116:278–290. doi: 10.1046/j.1365-2141.2002.03257.x. [DOI] [PubMed] [Google Scholar]
- 32.Abe M, Hiura K, Wilde J, Shioyasono A, Moriyama K, Hashimoto T, Kido S, Oshima T, Shibata H, Ozaki S, et al. Osteoclasts enhance myeloma cell growth and survival via cell-cell contact: a vicious cycle between bone destruction and myeloma expansion. Blood. 2004;104:2484–2491. doi: 10.1182/blood-2003-11-3839. [DOI] [PubMed] [Google Scholar]
- 33.Rogers MJ. From molds and macrophages to mevalonate: a decade of progress in understanding the molecular mode of action of bisphosphonates. Calcif Tissue Int. 2004;75:451–461. doi: 10.1007/s00223-004-0024-1. [DOI] [PubMed] [Google Scholar]
- 34.Lipton A, Fizazi K, Stopeck AT, Henry DH, Brown JE, Yardley DA, Richardson GE, Siena S, Maroto P, Clemens M, et al. Superiority of denosumab to zoledronic acid for prevention of skeletal-related events: a combined analysis of 3 pivotal, randomised, phase 3 trials. Eur J Cancer. 2012;48:3082–3092. doi: 10.1016/j.ejca.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 35.Henry DH, Costa L, Goldwasser F, Hirsh V, Hungria V, Prausova J, Scagliotti GV, Sleeboom H, Spencer A, Vadhan-Raj S, et al. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol. 2011;29:1125–1132. doi: 10.1200/JCO.2010.31.3304. [DOI] [PubMed] [Google Scholar]
- 36.Henry D, Vadhan-Raj S, Hirsh V, von Moos R, Hungria V, Costa L, Woll PJ, Scagliotti G, Smith G, Feng A, et al. Delaying skeletal-related events in a randomized phase 3 study of denosumab versus zoledronic acid in patients with advanced cancer: an analysis of data from patients with solid tumors. Support Care Cancer. 2014;22:679–687. doi: 10.1007/s00520-013-2022-1. [DOI] [PubMed] [Google Scholar]
- 37.Chioda M, Peranzoni E, Desantis G, Papalini F, Falisi E, Solito S, Samantha S, Mandruzzato S, Bronte V. Myeloid cell diversification and complexity: an old concept with new turns in oncology. Cancer Metastasis Rev. 2011;30:27–43. doi: 10.1007/s10555-011-9268-1. [DOI] [PubMed] [Google Scholar]
- 38.Gabrilovich DI, Ostrand-Rosenberg S, Bronte V. Coordinated regulation of myeloid cells by tumours. Nat Rev Immunol. 2012;12:253–268. doi: 10.1038/nri3175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Solito S, Marigo I, Pinton L, Damuzzo V, Mandruzzato S, Bronte V. Myeloid-derived suppressor cell heterogeneity in human cancers. Ann N Y Acad Sci. 2014;1319:47–65. doi: 10.1111/nyas.12469. [DOI] [PubMed] [Google Scholar]
- 40.Van Valckenborgh E, Schouppe E, Movahedi K, De Bruyne E, Menu E, De Baetselier P, Vanderkerken K, Van Ginderachter JA. Multiple myeloma induces the immunosuppressive capacity of distinct myeloid-derived suppressor cell subpopulations in the bone marrow. Leukemia. 2012;26:2424–2428. doi: 10.1038/leu.2012.113. [DOI] [PubMed] [Google Scholar]
- 41.Ramachandran IR, Martner A, Pisklakova A, Condamine T, Chase T, Vogl T, Roth J, Gabrilovich D, Nefedova Y. Myeloid-derived suppressor cells regulate growth of multiple myeloma by inhibiting T cells in bone marrow. J Immunol. 2013;190:3815–3823. doi: 10.4049/jimmunol.1203373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhuang J, Zhang J, Lwin ST, Edwards JR, Edwards CM, Mundy GR, Yang X. Osteoclasts in multiple myeloma are derived from Gr-1+CD11b+myeloid-derived suppressor cells. PLoS One. 2012;7:e48871. doi: 10.1371/journal.pone.0048871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang L, DeBusk LM, Fukuda K, Fingleton B, Green-Jarvis B, Shyr Y, Matrisian LM, Carbone DP, Lin PC. Expansion of myeloid immune suppressor Gr+CD11b+ cells in tumor-bearing host directly promotes tumor angiogenesis. Cancer Cell. 2004;6:409–421. doi: 10.1016/j.ccr.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 44.Talmadge JE, Gabrilovich DI. History of myeloid-derived suppressor cells. Nat Rev Cancer. 2013;13:739–752. doi: 10.1038/nrc3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peinado H, Lavotshkin S, Lyden D. The secreted factors responsible for pre-metastatic niche formation: old sayings and new thoughts. Semin Cancer Biol. 2011;21:139–146. doi: 10.1016/j.semcancer.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 46.Serafini P, Meckel K, Kelso M, Noonan K, Califano J, Koch W, Dolcetti L, Bronte V, Borrello I. Phosphodiesterase-5 inhibition augments endogenous antitumor immunity by reducing myeloid-derived suppressor cell function. J Exp Med. 2006;203:2691–2702. doi: 10.1084/jem.20061104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Noonan KA, Ghosh N, Rudraraju L, Bui M, Borrello I. Targeting immune suppression with PDE5 inhibition in end-stage multiple myeloma. Cancer Immunol Res. 2014;2:725–731. doi: 10.1158/2326-6066.CIR-13-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ruffell B, Affara NI, Coussens LM. Differential macrophage programming in the tumor microenvironment. Trends Immunol. 2012;33:119–126. doi: 10.1016/j.it.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Biswas SK, Gangi L, Paul S, Schioppa T, Saccani A, Sironi M, Bottazzi B, Doni A, Vincenzo B, Pasqualini F, et al. A distinct and unique transcriptional program expressed by tumor-associated macrophages (defective NF-kappaB and enhanced IRF-3/STAT1 activation) Blood. 2006;107:2112–2122. doi: 10.1182/blood-2005-01-0428. [DOI] [PubMed] [Google Scholar]
- 50.Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25:677–686. doi: 10.1016/j.it.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 51.Beider K, Bitner H, Leiba M, Gutwein O, Koren-Michowitz M, Ostrovsky O, Abraham M, Wald H, Galun E, Peled A, et al. Multiple myeloma cells recruit tumor-supportive macrophages through the CXCR4/CXCL12 axis and promote their polarization toward the M2 phenotype. Oncotarget. 2014;5:11283–11296. doi: 10.18632/oncotarget.2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim J, Denu RA, Dollar BA, Escalante LE, Kuether JP, Callander NS, Asimakopoulos F, Hematti P. Macrophages and mesenchymal stromal cells support survival and proliferation of multiple myeloma cells. Br J Haematol. 2012;158:336–346. doi: 10.1111/j.1365-2141.2012.09154.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gu ZJ, Costes V, Lu ZY, Zhang XG, Pitard V, Moreau JF, Bataille R, Wijdenes J, Rossi JF, Klein B. Interleukin-10 is a growth factor for human myeloma cells by induction of an oncostatin M autocrine loop. Blood. 1996;88:3972–3986. [PubMed] [Google Scholar]
- 54.Alexandrakis MG, Goulidaki N, Pappa CA, Boula A, Psarakis F, Neonakis I, Tsirakis G. Interleukin-10 Induces Both Plasma Cell Proliferation and Angiogenesis in Multiple Myeloma. Pathol Oncol Res. 2015;21(4):929–34. doi: 10.1007/s12253-015-9921-z. [DOI] [PubMed] [Google Scholar]
- 55.Zheng Y, Cai Z, Wang S, Zhang X, Qian J, Hong S, Li H, Wang M, Yang J, Yi Q. Macrophages are an abundant component of myeloma microenvironment and protect myeloma cells from chemotherapy drug-induced apoptosis. Blood. 2009;114:3625–3628. doi: 10.1182/blood-2009-05-220285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scavelli C, Nico B, Cirulli T, Ria R, Di Pietro G, Mangieri D, Bacigalupo A, Mangialardi G, Coluccia AM, Caravita T, et al. Vasculogenic mimicry by bone marrow macrophages in patients with multiple myeloma. Oncogene. 2008;27:663–674. doi: 10.1038/sj.onc.1210691. [DOI] [PubMed] [Google Scholar]
- 57.Chen H, Campbell RA, Chang Y, Li M, Wang CS, Li J, Sanchez E, Share M, Steinberg J, Berenson A, et al. Pleiotrophin produced by multiple myeloma induces transdifferentiation of monocytes into vascular endothelial cells: a novel mechanism of tumor-induced vasculogenesis. Blood. 2009;113:1992–2002. doi: 10.1182/blood-2008-02-133751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Berardi S, Ria R, Reale A, De Luisi A, Catacchio I, Moschetta M, Vacca A. Multiple myeloma macrophages: pivotal players in the tumor microenvironment. J Oncol 2013 Article ID 183602. 2013 doi: 10.1155/2013/183602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cook J, Hagemann T. Tumour-associated macrophages and cancer. Curr Opin Pharmacol. 2013;13:595–601. doi: 10.1016/j.coph.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 60.Ries CH, Hoves S, Cannarile MA, Rüttinger D. CSF-1/CSF-1R targeting agents in clinical development for cancer therapy. Curr Opin Pharmacol. 2015;23:45–51. doi: 10.1016/j.coph.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 61.Rakhmilevich AL, Alderson KL, Sondel PM. T-cell-independent antitumor effects of CD40 ligation. Int Rev Immunol. 2012;31:267–278. doi: 10.3109/08830185.2012.698337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jensen JL, Rakhmilevich A, Heninger E, Broman AT, Hope C, Phan F, Miyamoto S, Maroulakou I, Callander N, Hematti P, et al. Tumoricidal Effects of Macrophage-Activating Immunotherapy in a Murine Model of Relapsed/Refractory Multiple Myeloma. Cancer Immunol Res. 2015;3(8):881–90. doi: 10.1158/2326-6066.CIR-15-0025-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jego G, Pascual V, Palucka AK, Banchereau J. Dendritic cells control B cell growth and differentiation. Curr Dir Autoimmun. 2005;8:124–139. doi: 10.1159/000082101. [DOI] [PubMed] [Google Scholar]
- 64.Brown RD, Pope B, Murray A, Esdale W, Sze DM, Gibson J, Ho PJ, Hart D, Joshua D. Dendritic cells from patients with myeloma are numerically normal but functionally defective as they fail to up-regulate CD80 (B7-1) expression after huCD40LT stimulation because of inhibition by transforming growth factor-beta1 and interleukin-10. Blood. 2001;98:2992–2998. doi: 10.1182/blood.v98.10.2992. [DOI] [PubMed] [Google Scholar]
- 65.Chauhan D, Singh AV, Brahmandam M, Carrasco R, Bandi M, Hideshima T, Bianchi G, Podar K, Tai YT, Mitsiades C, et al. Functional interaction of plasmacytoid dendritic cells with multiple myeloma cells: a therapeutic target. Cancer Cell. 2009;16:309–323. doi: 10.1016/j.ccr.2009.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ratta M, Fagnoni F, Curti A, Vescovini R, Sansoni P, Oliviero B, Fogli M, Ferri E, Della Cuna GR, Tura S, et al. Dendritic cells are functionally defective in multiple myeloma: the role of interleukin-6. Blood. 2002;100:230–237. doi: 10.1182/blood.v100.1.230. [DOI] [PubMed] [Google Scholar]
- 67.Kukreja A, Hutchinson A, Dhodapkar K, Mazumder A, Vesole D, Angitapalli R, Jagannath S, Dhodapkar MV. Enhancement of clonogenicity of human multiple myeloma by dendritic cells. J Exp Med. 2006;203:1859–1865. doi: 10.1084/jem.20052136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tucci M, Ciavarella S, Strippoli S, Brunetti O, Dammacco F, Silvestris F. Immature dendritic cells from patients with multiple myeloma are prone to osteoclast differentiation in vitro. Exp Hematol. 2011;39:773–83. doi: 10.1016/j.exphem.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 69.Tucci M, Stucci S, Savonarola A, Ciavarella S, Cafforio P, Dammacco F, Silvestris F. Immature dendritic cells in multiple myeloma are prone to osteoclast-like differentiation through interleukin-17A stimulation. Br J Haematol. 2013;161:821–831. doi: 10.1111/bjh.12333. [DOI] [PubMed] [Google Scholar]
- 70.Parrinello N, Conticello C, Cavalli M, La Fauci A, Rizzo G, La Cava P, Chiarenza A, Tibullo D, Giallongo C, Palumbo GA, et al. Neutrophils Of Multiple Myeloma Are Dysfunctional and Immunosuppressive. Blood. 2013;122:3138–3138. [Google Scholar]
- 71.Wong D, Winter O, Hartig C, Siebels S, Szyska M, Tiburzy B, Meng L, Kulkarni U, Fähnrich A, Bommert K, et al. Eosinophils and megakaryocytes support the early growth of murine MOPC315 myeloma cells in their bone marrow niches. PLoS One. 2014;9:e109018. doi: 10.1371/journal.pone.0109018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nico B, Mangieri D, Crivellato E, Vacca A, Ribatti D. Mast cells contribute to vasculogenic mimicry in multiple myeloma. Stem Cells Dev. 2008;17:19–22. doi: 10.1089/scd.2007.0132. [DOI] [PubMed] [Google Scholar]
- 73.Pappa CA, Tsirakis G, Stavroulaki E, Kokonozaki M, Xekalou A, Konsolas I, Alexandrakis MG. Mast cells influence the proliferation rate of myeloma plasma cells. Cancer Invest. 2015;33:137–141. doi: 10.3109/07357907.2015.1008639. [DOI] [PubMed] [Google Scholar]
- 74.D’Amico L, Roato I. Cross-talk between T cells and osteoclasts in bone resorption. Bonekey Rep. 2012;1:82. doi: 10.1038/bonekey.2012.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kong YY, Feige U, Sarosi I, Bolon B, Tafuri A, Morony S, Capparelli C, Li J, Elliott R, McCabe S, et al. Activated T cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprotegerin ligand. Nature. 1999;402:304–309. doi: 10.1038/46303. [DOI] [PubMed] [Google Scholar]
- 76.Cook LM, Shay G, Aruajo A, Lynch CC. Integrating new discoveries into the “vicious cycle” paradigm of prostate to bone metastases. Cancer Metastasis Rev. 2014;33(2–3):511–25. doi: 10.1007/s10555-014-9494-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zou L, Barnett B, Safah H, Larussa VF, Evdemon-Hogan M, Mottram P, Wei S, David O, Curiel TJ, Zou W. Bone marrow is a reservoir for CD4+CD25+ regulatory T cells that traffic through CXCL12/CXCR4 signals. Cancer Res. 2004;64:8451–8455. doi: 10.1158/0008-5472.CAN-04-1987. [DOI] [PubMed] [Google Scholar]
- 78.Beyer M, Schultze JL. Regulatory T cells: major players in the tumor microenvironment. Curr Pharm Des. 2009;15:1879–1892. doi: 10.2174/138161209788453211. [DOI] [PubMed] [Google Scholar]
- 79.Beyer M, Kochanek M, Giese T, Endl E, Weihrauch MR, Knolle PA, Classen S, Schultze JL. In vivo peripheral expansion of naive CD4+CD25high FoxP3+ regulatory T cells in patients with multiple myeloma. Blood. 2006;107:3940–3949. doi: 10.1182/blood-2005-09-3671. [DOI] [PubMed] [Google Scholar]
- 80.Prabhala RH, Neri P, Bae JE, Tassone P, Shammas MA, Allam CK, Daley JF, Chauhan D, Blanchard E, Thatte HS, et al. Dysfunctional T regulatory cells in multiple myeloma. Blood. 2006;107:301–304. doi: 10.1182/blood-2005-08-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Giannopoulos K, Kaminska W, Hus I, Dmoszynska A. The frequency of T regulatory cells modulates the survival of multiple myeloma patients: detailed characterisation of immune status in multiple myeloma. Br J Cancer. 2012;106:546–552. doi: 10.1038/bjc.2011.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bryant C, Suen H, Brown R, Yang S, Favaloro J, Aklilu E, Gibson J, Ho PJ, Iland H, Fromm P, et al. Long-term survival in multiple myeloma is associated with a distinct immunological profile, which includes proliferative cytotoxic T-cell clones and a favourable Treg/Th17 balance. Blood Cancer J. 2013;3:e148. doi: 10.1038/bcj.2013.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Foglietta M, Castella B, Mariani S, Coscia M, Godio L, Ferracini R, Ruggeri M, Muccio V, Omedé P, Palumbo A, et al. The bone marrow of myeloma patients is steadily inhabited by a normal-sized pool of functional regulatory T cells irrespectiveof the disease status. Haematologica. 2014;99:1605–1610. doi: 10.3324/haematol.2014.105866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Muthu Raja KR, Kubiczkova L, Rihova L, Piskacek M, Vsianska P, Hezova R, Pour L, Hajek R. Functionally suppressive CD8 T regulatory cells are increased in patients with multiple myeloma: a cause for immune impairment. PLoS One. 2012;7:e49446. doi: 10.1371/journal.pone.0049446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Moss P, Gillespie G, Frodsham P, Bell J, Reyburn H. Clonal populations of CD4+ and CD8+ T cells in patients with multiple myeloma and paraproteinemia. Blood. 1996;87:3297–3306. [PubMed] [Google Scholar]
- 86.Racanelli V, Leone P, Frassanito MA, Brunetti C, Perosa F, Ferrone S, Dammacco F. Alterations in the antigen processing-presenting machinery of transformed plasma cells are associated with reduced recognition by CD8+ T cells and characterize the progression of MGUS to multiple myeloma. Blood. 2010;115:1185–1193. doi: 10.1182/blood-2009-06-228676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Witzens-Harig M, Hose D, Junger S, Pfirschke C, Khandelwal N, Umansky L, Seckinger A, Conrad H, Brackertz B, Reme T, et al. Tumor cells in multiple myeloma patients inhibit myeloma-reactive T cells through carcinoembryonic antigen-related cell adhesion molecule-6. Blood. 2013;121:4493–4503. doi: 10.1182/blood-2012-05-429415. [DOI] [PubMed] [Google Scholar]
- 88.Liu J, Hamrouni A, Wolowiec D, Coiteux V, Kuliczkowski K, Hetuin D, Saudemont A, Quesnel B. Plasma cells from multiple myeloma patients express B7-H1 (PD-L1) and increase expression after stimulation with IFN-{gamma} and TLR ligands via a MyD88-, TRAF6-, and MEK-dependent pathway. Blood. 2007;110:296–304. doi: 10.1182/blood-2006-10-051482. [DOI] [PubMed] [Google Scholar]
- 89.Yousef S, Marvin J, Steinbach M, Langemo A, Kovacsovics T, Binder M, Kröger N, Luetkens T, Atanackovic D. Immunomodulatory molecule PD-L1 is expressed on malignant plasma cells and myeloma-propagating pre-plasma cells in the bone marrow of multiple myeloma patients. Blood Cancer J. 2015;5:e285. doi: 10.1038/bcj.2015.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rosenblatt J, Glotzbecker B, Mills H, Vasir B, Tzachanis D, Levine JD, Joyce RM, Wellenstein K, Keefe W, Schickler M, et al. PD-1 blockade by CT-011, anti-PD-1 antibody, enhances ex vivo T-cell responses to autologous dendritic cell/myeloma fusion vaccine. J Immunother. 2011;34:409–418. doi: 10.1097/CJI.0b013e31821ca6ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Feyler S, Scott GB, Parrish C, Jarmin S, Evans P, Short M, McKinley K, Selby PJ, Cook G. Tumour cell generation of inducible regulatory T-cells in multiple myeloma is contact-dependent and antigen-presenting cell-independent. PLoS One. 2012;7:e35981. doi: 10.1371/journal.pone.0035981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Luptakova K, Rosenblatt J, Glotzbecker B, Mills H, Stroopinsky D, Kufe T, Vasir B, Arnason J, Tzachanis D, Zwicker JI, et al. Lenalidomide enhances anti-myeloma cellular immunity. Cancer Immunol Immunother. 2013;62:39–49. doi: 10.1007/s00262-012-1308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Iwai Y, Ishida M, Tanaka Y, Okazaki T, Honjo T, Minato N. Involvement of PD-L1 on tumor cells in the escape from host immune system and tumor immunotherapy by PD-L1 blockade. Proc Natl Acad Sci U S A. 2002;99:12293–12297. doi: 10.1073/pnas.192461099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kearl TJ, Jing W, Gershan JA, Johnson BD. Programmed death receptor-1/programmed death receptor ligand-1 blockade after transient lymphodepletion to treat myeloma. J Immunol. 2013;190:5620–5628. doi: 10.4049/jimmunol.1202005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hallett WH, Jing W, Drobyski WR, Johnson BD. Immunosuppressive effects of multiple myeloma are overcome by PD-L1 blockade. Biol Blood Marrow Transplant. 2011;17:1133–1145. doi: 10.1016/j.bbmt.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 96.Shapiro-Shelef M, Calame K. Plasma cell differentiation and multiple myeloma. Curr Opin Immunol. 2004;16:226–234. doi: 10.1016/j.coi.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 97.Pilarski LM, Ruether BA, Mant MJ. Abnormal function of B lymphocytes from peripheral blood of multiple myeloma patients. Lack of correlation between the number of cells potentially able to secrete immunoglobulin M and serum immunoglobulin M levels. J Clin Invest. 1985;75:2024–2029. doi: 10.1172/JCI111921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Carmichael J, Carter CR, Parrish C, Kallmeyer C, Feyler S, Wood PM, Cook G. Reduced Circulating Memory B-Cells Account for Humoral Immune Defects in Multiple Myeloma, Associated with Infective Risk and Poor Vaccination Responses. Blood. 2014;124:3393–3393. [Google Scholar]
- 99.Oden F, Marino SF, Brand J, Scheu S, Kriegel C, Olal D, Takvorian A, Westermann J, Yilmaz B, Hinz M, et al. Potent anti-tumor response by targeting B cell maturation antigen (BCMA) in a mouse model of multiple myeloma. Mol Oncol. 2015;9(7):1348–58. doi: 10.1016/j.molonc.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bae J, Tai YT, Anderson KC, Munshi NC. Novel epitope evoking CD138 antigen-specific cytotoxic T lymphocytes targeting multiple myeloma and other plasma cell disorders. Br J Haematol. 2011;155:349–361. doi: 10.1111/j.1365-2141.2011.08850.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jurisic V, Srdic T, Konjevic G, Markovic O, Colovic M. Clinical stage-depending decrease of NK cell activity in multiple myeloma patients. Med Oncol. 2007;24:312–317. doi: 10.1007/s12032-007-0007-y. [DOI] [PubMed] [Google Scholar]
- 102.Shi J, Tricot GJ, Garg TK, Malaviarachchi PA, Szmania SM, Kellum RE, Storrie B, Mulder A, Shaughnessy JD, Barlogie B, et al. Bortezomib down-regulates the cell-surface expression of HLA class I and enhances natural killer cell-mediated lysis of myeloma. Blood. 2008;111:1309–1317. doi: 10.1182/blood-2007-03-078535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Davies FE, Raje N, Hideshima T, Lentzsch S, Young G, Tai YT, Lin B, Podar K, Gupta D, Chauhan D, et al. Thalidomide and immunomodulatory derivatives augment natural killer cell cytotoxicity in multiple myeloma. Blood. 2001;98:210–216. doi: 10.1182/blood.v98.1.210. [DOI] [PubMed] [Google Scholar]
- 104.Benson DM, Bakan CE, Mishra A, Hofmeister CC, Efebera Y, Becknell B, Baiocchi RA, Zhang J, Yu J, Smith MK, et al. The PD-1/PD-L1 axis modulates the natural killer cell versus multiple myeloma effect: a therapeutic target for CT-011, a novel monoclonal anti-PD-1 antibody. Blood. 2010;116:2286–2294. doi: 10.1182/blood-2010-02-271874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Swift BE, Williams BA, Kosaka Y, Wang XH, Medin JA, Viswanathan S, Martinez-Lopez J, Keating A. Natural killer cell lines preferentially kill clonogenic multiple myeloma cells and decrease myeloma engraftment in a bioluminescent xenograft mouse model. Haematologica. 2012;97:1020–1028. doi: 10.3324/haematol.2011.054254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Szmania S, Lapteva N, Garg T, Greenway A, Lingo J, Nair B, Stone K, Woods E, Khan J, Stivers J, et al. Ex vivo-expanded natural killer cells demonstrate robust proliferation in vivo in high-risk relapsed multiple myeloma patients. J Immunother. 2015;38:24–36. doi: 10.1097/CJI.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chu J, Deng Y, Benson DM, He S, Hughes T, Zhang J, Peng Y, Mao H, Yi L, Ghoshal K, et al. CS1-specific chimeric antigen receptor (CAR)-engineered natural killer cells enhance in vitro and in vivo antitumor activity against human multiple myeloma. Leukemia. 2014;28:917–927. doi: 10.1038/leu.2013.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Xing F, Saidou J, Watabe K. Cancer associated fibroblasts (CAFs) in tumor microenvironment. Front Biosci (Landmark Ed) 2010;15:166–179. doi: 10.2741/3613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Reagan MR, Ghobrial IM. Multiple myeloma mesenchymal stem cells: characterization, origin, and tumor-promoting effects. Clin Cancer Res. 2012;18:342–349. doi: 10.1158/1078-0432.CCR-11-2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lauta VM. Interleukin-6 and the network of several cytokines in multiple myeloma: an overview of clinical and experimental data. Cytokine. 2001;16:79–86. doi: 10.1006/cyto.2001.0982. [DOI] [PubMed] [Google Scholar]
- 111.Yoshizaki K, Nakagawa T, Fukunaga K, Tseng LT, Yamamura Y, Kishimoto T. Isolation and characterization of B cell differentiation factor (BCDF) secreted from a human B lymphoblastoid cell line. J Immunol. 1984;132:2948–2954. [PubMed] [Google Scholar]
- 112.Meads MB, Hazlehurst LA, Dalton WS. The bone marrow microenvironment as a tumor sanctuary and contributor to drug resistance. Clin Cancer Res. 2008;14:2519–2526. doi: 10.1158/1078-0432.CCR-07-2223. [DOI] [PubMed] [Google Scholar]
- 113.Katz BZ. Adhesion molecules--The lifelines of multiple myeloma cells. Semin Cancer Biol. 2010;20:186–195. doi: 10.1016/j.semcancer.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 114.Hideshima T, Chauhan D, Schlossman R, Richardson P, Anderson KC. The role of tumor necrosis factor alpha in the pathophysiology of human multiple myeloma: therapeutic applications. Oncogene. 2001;20:4519–4527. doi: 10.1038/sj.onc.1204623. [DOI] [PubMed] [Google Scholar]
- 115.Morgan MR, Humphries MJ, Bass MD. Synergistic control of cell adhesion by integrins and syndecans. Nat Rev Mol Cell Biol. 2007;8:957–969. doi: 10.1038/nrm2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Damiano JS, Cress AE, Hazlehurst LA, Shtil AA, Dalton WS. Cell adhesion mediated drug resistance (CAM-DR): role of integrins and resistance to apoptosis in human myeloma cell lines. Blood. 1999;93:1658–1667. [PMC free article] [PubMed] [Google Scholar]
- 117.Mitsiades CS, McMillin DW, Klippel S, Hideshima T, Chauhan D, Richardson PG, Munshi NC, Anderson KC. The role of the bone marrow microenvironment in the pathophysiology of myeloma and its significance in the development of more effective therapies. Hematol Oncol Clin North Am. 2007;21:1007–34. doi: 10.1016/j.hoc.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 118.Hao M, Zhang L, An G, Meng H, Han Y, Xie Z, Xu Y, Li C, Yu Z, Chang H, et al. Bone marrow stromal cells protect myeloma cells from bortezomib induced apoptosis by suppressing microRNA-15a expression. Leuk Lymphoma. 2011;52:1787–1794. doi: 10.3109/10428194.2011.576791. [DOI] [PubMed] [Google Scholar]
- 119.Wang X, Zhang Z, Yao C. Survivin is upregulated in myeloma cell lines cocultured with mesenchymal stem cells. Leuk Res. 2010;34:1325–1329. doi: 10.1016/j.leukres.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 120.Roodman GD. Treatment strategies for bone disease. Bone Marrow Transplant. 2007;40:1139–1146. doi: 10.1038/sj.bmt.1705802. [DOI] [PubMed] [Google Scholar]
- 121.Sati HI, Greaves M, Apperley JF, Russell RG, Croucher PI. Expression of interleukin-1beta and tumour necrosis factor-alpha in plasma cells from patients with multiple myeloma. Br J Haematol. 1999;104:350–357. doi: 10.1046/j.1365-2141.1999.01193.x. [DOI] [PubMed] [Google Scholar]
- 122.Oyajobi BO, Mundy GR. Receptor activator of NF-kappaB ligand, macrophage inflammatory protein-1alpha, and the proteasome: novel therapeutic targets in myeloma. Cancer. 2003;97:813–817. doi: 10.1002/cncr.11133. [DOI] [PubMed] [Google Scholar]
- 123.Garderet L, Mazurier C, Chapel A, Ernou I, Boutin L, Holy X, Gorin NC, Lopez M, Doucet C, Lataillade JJ. Mesenchymal stem cell abnormalities in patients with multiple myeloma. Leuk Lymphoma. 2007;48:2032–2041. doi: 10.1080/10428190701593644. [DOI] [PubMed] [Google Scholar]
- 124.Li B, Fu J, Chen P, Zhuang W. Impairment in immunomodulatory function of mesenchymal stem cells from multiple myeloma patients. Arch Med Res. 2010;41:623–633. doi: 10.1016/j.arcmed.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 125.Di Nicola M, Carlo-Stella C, Magni M, Milanesi M, Longoni PD, Matteucci P, Grisanti S, Gianni AM. Human bone marrow stromal cells suppress T-lymphocyte proliferation induced by cellular or nonspecific mitogenic stimuli. Blood. 2002;99:3838–3843. doi: 10.1182/blood.v99.10.3838. [DOI] [PubMed] [Google Scholar]
- 126.Li X, Ling W, Khan S, Yaccoby S. Therapeutic effects of intrabone and systemic mesenchymal stem cell cytotherapy on myeloma bone disease and tumor growth. J Bone Miner Res. 2012;27:1635–1648. doi: 10.1002/jbmr.1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Atsuta I, Liu S, Miura Y, Akiyama K, Chen C, An Y, Shi S, Chen FM. Mesenchymal stem cells inhibit multiple myeloma cells via the Fas/Fas ligand pathway. Stem Cell Res Ther. 2013;4:111. doi: 10.1186/scrt322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kurzrock R, Voorhees PM, Casper C, Furman RR, Fayad L, Lonial S, Borghaei H, Jagannath S, Sokol L, Usmani SZ, et al. A phase I, open-label study of siltuximab, an anti-IL-6 monoclonal antibody, in patients with B-cell non-Hodgkin lymphoma, multiple myeloma, or Castleman disease. Clin Cancer Res. 2013;19:3659–3670. doi: 10.1158/1078-0432.CCR-12-3349. [DOI] [PubMed] [Google Scholar]
- 129.San-Miguel J, Bladé J, Shpilberg O, Grosicki S, Maloisel F, Min CK, Polo Zarzuela M, Robak T, Prasad SV, Tee Goh Y, et al. Phase 2 randomized study of bortezomib-melphalan-prednisone with or without siltuximab (anti-IL-6) in multiple myeloma. Blood. 2014;123:4136–4142. doi: 10.1182/blood-2013-12-546374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nair RR, Gebhard AW, Emmons MF, Hazlehurst LA. Emerging strategies for targeting cell adhesion in multiple myeloma. Adv Pharmacol. 2012;65:143–189. doi: 10.1016/B978-0-12-397927-8.00006-3. [DOI] [PubMed] [Google Scholar]
- 131.Nair RR, Emmons MF, Cress AE, Argilagos RF, Lam K, Kerr WT, Wang HG, Dalton WS, Hazlehurst LA. HYD1-induced increase in reactive oxygen species leads to autophagy and necrotic cell death in multiple myeloma cells. Mol Cancer Ther. 2009;8:2441–2451. doi: 10.1158/1535-7163.MCT-09-0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Roodman GD. Osteoblast function in myeloma. Bone. 2011;48:135–140. doi: 10.1016/j.bone.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 133.Fukumoto S. FGF23-FGF Receptor/Klotho Pathway as a New Drug Target for Disorders of Bone and Mineral Metabolism. Calcif Tissue Int. 2015 doi: 10.1007/s00223-015-0029-y. [DOI] [PubMed] [Google Scholar]
- 134.Ruan J, Trotter TN, Nan L, Luo R, Javed A, Sanderson RD, Suva LJ, Yang Y. Heparanase inhibits osteoblastogenesis and shifts bone marrow progenitor cell fate in myeloma bone disease. Bone. 2013;57:10–17. doi: 10.1016/j.bone.2013.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Fulciniti M, Tassone P, Hideshima T, Vallet S, Nanjappa P, Ettenberg SA, Shen Z, Patel N, Tai YT, Chauhan D, et al. Anti-DKK1 mAb (BHQ880) as a potential therapeutic agent for multiple myeloma. Blood. 2009;114:371–379. doi: 10.1182/blood-2008-11-191577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Iyer SP, Beck JT, Stewart AK, Shah J, Kelly KR, Isaacs R, Bilic S, Sen S, Munshi NC. A Phase IB multicentre dose-determination study of BHQ880 in combination with anti-myeloma therapy and zoledronic acid in patients with relapsed or refractory multiple myeloma and prior skeletal-related events. Br J Haematol. 2014;167:366–375. doi: 10.1111/bjh.13056. [DOI] [PubMed] [Google Scholar]
- 137.Chen Z, Orlowski RZ, Wang M, Kwak L, McCarty N. Osteoblastic niche supports the growth of quiescent multiple myeloma cells. Blood. 2014;123:2204–2208. doi: 10.1182/blood-2013-07-517136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.McDonald M, Lawson M, Kovacic N, Terry R, Khoo WH, Down J, Pettitt J, Quinn J, Pettit A, Phan T, Croucher P. Bone cells control myeloma cell dormancy and activation in the skeleton. IBMS BoneKEy. 2015;13:673. [Google Scholar]
- 139.Takeuchi K, Abe M, Hiasa M, Oda A, Amou H, Kido S, Harada T, Tanaka O, Miki H, Nakamura S, et al. Tgf-Beta inhibition restores terminal osteoblast differentiation to suppress myeloma growth. PLoS One. 2010;5:e9870. doi: 10.1371/journal.pone.0009870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yaccoby S, Wezeman MJ, Zangari M, Walker R, Cottler-Fox M, Gaddy D, Ling W, Saha R, Barlogie B, Tricot G, et al. Inhibitory effects of osteoblasts and increased bone formation on myeloma in novel culture systems and a myelomatous mouse model. Haematologica. 2006;91:192–199. [PMC free article] [PubMed] [Google Scholar]
- 141.Li X, Pennisi A, Yaccoby S. Role of decorin in the antimyeloma effects of osteoblasts. Blood. 2008;112:159–168. doi: 10.1182/blood-2007-11-124164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kristensen IB, Pedersen L, Ro TB, Christensen JH, Lyng MB, Rasmussen LM, Ditzel HJ, Borset M, Abildgaard N. Decorin is down-regulated in multiple myeloma and MGUS bone marrow plasma and inhibits HGF-induced myeloma plasma cell viability and migration. Eur J Haematol. 2013;91:196–200. doi: 10.1111/ejh.12125. [DOI] [PubMed] [Google Scholar]
- 143.Kramer I, Halleux C, Keller H, Pegurri M, Gooi JH, Weber PB, Feng JQ, Bonewald LF, Kneissel M. Osteocyte Wnt/beta-catenin signaling is required for normal bone homeostasis. Mol Cell Biol. 2010;30:3071–3085. doi: 10.1128/MCB.01428-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Eisenberger S, Ackermann K, Voggenreiter G, Sultmann H, Kasperk C, Pyerin W. Metastases and multiple myeloma generate distinct transcriptional footprints in osteocytes in vivo. J Pathol. 2008;214:617–626. doi: 10.1002/path.2322. [DOI] [PubMed] [Google Scholar]
- 145.Giuliani N, Ferretti M, Bolzoni M, Storti P, Lazzaretti M, Dalla Palma B, Bonomini S, Martella E, Agnelli L, Neri A, et al. Increased osteocyte death in multiple myeloma patients: role in myeloma-induced osteoclast formation. Leukemia. 2012;26:1391–1401. doi: 10.1038/leu.2011.381. [DOI] [PubMed] [Google Scholar]
- 146.Roelofs AJ, Coxon FP, Ebetino FH, Lundy MW, Henneman ZJ, Nancollas GH, Sun S, Blazewska KM, Bala JL, Kashemirov BA, et al. Fluorescent risedronate analogues reveal bisphosphonate uptake by bone marrow monocytes and localization around osteocytes in vivo. J Bone Miner Res. 2010;25:606–616. doi: 10.1359/jbmr.091009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Plotkin LI, Weinstein RS, Parfitt AM, Roberson PK, Manolagas SC, Bellido T. Prevention of osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin. J Clin Invest. 1999;104:1363–1374. doi: 10.1172/JCI6800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Liu Y, Song CY, Wu SS, Liang QH, Yuan LQ, Liao EY. Novel adipokines and bone metabolism. Int J Endocrinol 2013 Article ID 895045. 2013 doi: 10.1155/2013/895045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Nieman KM, Romero IL, Van Houten B, Lengyel E. Adipose tissue and adipocytes support tumorigenesis and metastasis. Biochim Biophys Acta. 2013;1831:1533–1541. doi: 10.1016/j.bbalip.2013.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Caers J, Deleu S, Belaid Z, De Raeve H, Van Valckenborgh E, De Bruyne E, Defresne MP, Van Riet I, Van Camp B, Vanderkerken K. Neighboring adipocytes participate in the bone marrow microenvironment of multiple myeloma cells. Leukemia. 2007;21:1580–1584. doi: 10.1038/sj.leu.2404658. [DOI] [PubMed] [Google Scholar]
- 151.Vicennati V, Vottero A, Friedman C, Papanicolaou DA. Hormonal regulation of interleukin-6 production in human adipocytes. Int J Obes Relat Metab Disord. 2002;26:905–911. doi: 10.1038/sj.ijo.0802035. [DOI] [PubMed] [Google Scholar]
- 152.Carson KR, Bates ML, Tomasson MH. The skinny on obesity and plasma cell myeloma: a review of the literature. Bone Marrow Transplant. 2014;49:1009–1015. doi: 10.1038/bmt.2014.71. [DOI] [PubMed] [Google Scholar]
- 153.Esheba NE, Shahba A, El Shora O. Assessment of leptin and resistin levels in non-obese multiple myeloma patients and their relation with Ig level and disease stage. J Egypt Natl Canc Inst. 2014;26:61–66. doi: 10.1016/j.jnci.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 154.Medina EA, Oberheu K, Polusani SR, Ortega V, Velagaleti GV, Oyajobi BO. PKA/AMPK signaling in relation to adiponectin’s antiproliferative effect on multiple myeloma cells. Leukemia. 2014;28:2080–2089. doi: 10.1038/leu.2014.112. [DOI] [PubMed] [Google Scholar]
- 155.Fowler JA, Lwin ST, Drake MT, Edwards JR, Kyle RA, Mundy GR, Edwards CM. Host-derived adiponectin is tumor-suppressive and a novel therapeutic target for multiple myeloma and the associated bone disease. Blood. 2011;118:5872–5882. doi: 10.1182/blood-2011-01-330407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Lwin ST, Olechnowicz SW, Fowler JA, Edwards CM. Diet-induced obesity promotes a myeloma-like condition in vivo. Leukemia. 2015;29:507–510. doi: 10.1038/leu.2014.295. [DOI] [PubMed] [Google Scholar]
- 157.Beason TS, Chang SH, Sanfilippo KM, Luo S, Colditz GA, Vij R, Tomasson MH, Dipersio JF, Stockerl-Goldstein K, Ganti A, et al. Influence of body mass index on survival in veterans with multiple myeloma. Oncologist. 2013;18:1074–1079. doi: 10.1634/theoncologist.2013-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Rajkumar SV, Landgren O, Mateos MV. Smoldering multiple myeloma. Blood. 2015;125(20):3069–75. doi: 10.1182/blood-2014-09-568899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Mateos MV, San Miguel JF. Smoldering multiple myeloma: when to observe and when to treat. Am Soc Clin Oncol Educ Book. 2015;35:e484–e492. doi: 10.14694/EdBook_AM.2015.35.e484. [DOI] [PubMed] [Google Scholar]
- 160.Kristinsson SY, Tang M, Pfeiffer RM, Björkholm M, Blimark C, Mellqvist UH, Wahlin A, Turesson I, Landgren O. Monoclonal gammopathy of undetermined significance and risk of skeletal fractures: a population-based study. Blood. 2010;116:2651–2655. doi: 10.1182/blood-2010-04-282848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Psaila B, Lyden D. The metastatic niche: adapting the foreign soil. Nat Rev Cancer. 2009;9:285–293. doi: 10.1038/nrc2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ghobrial IM. Myeloma as a model for the process of metastasis: implications for therapy. Blood. 2012;120:20–30. doi: 10.1182/blood-2012-01-379024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Uchiyama H, Barut BA, Mohrbacher AF, Chauhan D, Anderson KC. Adhesion of human myeloma-derived cell lines to bone marrow stromal cells stimulates interleukin-6 secretion. Blood. 1993;82:3712–3720. [PubMed] [Google Scholar]
- 164.Michigami T, Shimizu N, Williams PJ, Niewolna M, Dallas SL, Mundy GR, Yoneda Cell-cell contact between marrow stromal cells and myeloma cells via VCAM-1 and alpha(4)beta(1)-integrin enhances production of osteoclast-stimulating activity. Blood. 2000;96:1953–1960. [PubMed] [Google Scholar]
- 165.Teoh G, Anderson KC. Interaction of tumor and host cells with adhesion and extracellular matrix molecules in the development of multiple myeloma. Hematol Oncol Clin North Am. 1997;11:27–42. doi: 10.1016/s0889-8588(05)70413-5. [DOI] [PubMed] [Google Scholar]
- 166.Pant S, Hilton H, Burczynski ME. The multifaceted exosome: biogenesis, role in normal and aberrant cellular function, and frontiers for pharmacological and biomarker opportunities. Biochem Pharmacol. 2012;83:1484–1494. doi: 10.1016/j.bcp.2011.12.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Raimondi L, De Luca A, Amodio N, Manno M, Raccosta S, Taverna S, Bellavia D, Naselli F, Fontana S, Schillaci O, et al. Involvement of multiple myeloma cell-derived exosomes in osteoclast differentiation. Oncotarget. 2015;6(15):13772–89. doi: 10.18632/oncotarget.3830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Roccaro AM, Sacco A, Maiso P, Azab AK, Tai YT, Reagan M, Azab F, Flores LM, Campigotto F, Weller E, et al. BM mesenchymal stromal cell-derived exosomes facilitate multiple myeloma progression. J Clin Invest. 2013;123:1542–1555. doi: 10.1172/JCI66517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Wang J, Hendrix A, Hernot S, Lemaire M, De Bruyne E, Van Valckenborgh E, Lahoutte T, De Wever O, Vanderkerken K, Menu E. Bone marrow stromal cell-derived exosomes as communicators in drug resistance in multiple myeloma cells. Blood. 2014;124:555–566. doi: 10.1182/blood-2014-03-562439. [DOI] [PubMed] [Google Scholar]
- 170.Varettoni M, Corso A, Pica G, Mangiacavalli S, Pascutto C, Lazzarino M. Incidence, presenting features and outcome of extramedullary disease in multiple myeloma: a longitudinal study on 1003 consecutive patients. Ann Oncol. 2010;21:325–330. doi: 10.1093/annonc/mdp329. [DOI] [PubMed] [Google Scholar]
- 171.Blade J, Fernandez de Larrea C, Rosinol L. Extramedullary disease in multiple myeloma in the era of novel agents. Br J Haematol. 2015;169(6):843–50. doi: 10.1111/bjh.13384. [DOI] [PubMed] [Google Scholar]
- 172.Bladé J, Fernández de Larrea C, Rosiñol L, Cibeira MT, Jiménez R, Powles R. Soft-tissue plasmacytomas in multiple myeloma: incidence, mechanisms of extramedullary spread, and treatment approach. J Clin Oncol. 2011;29:3805–3812. doi: 10.1200/JCO.2011.34.9290. [DOI] [PubMed] [Google Scholar]
- 173.Usmani SZ, Heuck C, Mitchell A, Szymonifka J, Nair B, Hoering A, Alsayed Y, Waheed S, Haider S, Restrepo A, et al. Extramedullary disease portends poor prognosis in multiple myeloma and is over-represented in high-risk disease even in the era of novel agents. Haematologica. 2012;97:1761–1767. doi: 10.3324/haematol.2012.065698. [DOI] [PMC free article] [PubMed] [Google Scholar]