Abstract
Diabetes mellitus is a group of metabolic diseases involving carbohydrate, lipid, and protein metabolism. It is characterized by persistent hyperglycemia which results from defects in insulin secretion, or action or both. Diabetes mellitus has been known since antiquity. Descriptions have been found in the Egyptian papyri, in ancient Indian and Chinese medical literature, as well as, in the work of ancient Greek and Arab physicians. In the 2nd century AD Aretaeus of Cappadocia provided the first accurate description of diabetes, coining the term diabetes, while in 17th century Thomas Willis added the term mellitus to the disease, in an attempt to describe the extremely sweet taste of the urine. The important work of the 19th century French physiologist Claude Bernard, on the glycogenic action of the liver, paved the way for further progress in the study of the disease. In 1889, Oskar Minkowski and Joseph von Mering performed their famous experiment of removing the pancreas from a dog and producing severe and fatal diabetes. In 1921, Frederick Banting and Charles Best extended Minkowski’s and Mering’s experiment. They isolated insulin from pancreatic islets and administrated to patients suffering from type 1 diabetes, saving thus the lives of millions and inaugurating a new era in diabetes treatment.
Keywords: History of endocrinology, Metabolic disorder, Diabetes mellitus, Aretaeus of Cappadocia, Insulin
Core tip: Diabetes mellitus has been known since antiquity and despite therapeutic advances it still remains an incurable chronic disease. In our historical article, we attempt to provide the most important steps in the history of diabetes mellitus from antiquity till nowadays. The contribution of leading medical figures such as Aretaeus of Cappadocia, Thomas Willis, Claude Bernard, Oskar Minkowski, Joseph von Mering, Frederick Banting and Charles Best is mentioned, in an attempt to highlight the development of our current knowledge in diabetes mellitus.
INTRODUCTION
Diabetes mellitus is a group of metabolic diseases involving carbohydrate, lipid, and protein metabolism. It is characterized by persistent hyperglycemia, as a result of defects in insulin secretion, insulin action or a combination of both, defective secretion and incorrect action. There are two main types of diabetes mellitus: Type 1 (insulin-dependent), and type 2 (non-insulin-dependent). Type 1 diabetes results by the autoimmune destruction of the β-cells of the pancreatic islets and type 2 diabetes is caused from impaired insulin secretion and resistance to the action of insulin[1].Current epidemiological data reveal that 9% of adults, 18 years of age and older, has diabetes mellitus while it was estimated that in 2012, 1.5 million people died due to the disease. According to the World Health Organization, diabetes will be the 7th leading cause of death in 2030[2-4].
The disease has a long history reaching back into antiquity. However, during that period, due to a poor knowledge of anatomy, pathophysiology and lack of diagnostic tools, the disease remained extremely perplexing to physicians.
Nevertheless, physicians in antiquity observed the distinctive features of diabetes and proposed several therapeutic approaches. In Ebers papyrus, dated back to 1500 BC, we may find passages describing patients who suffer from excessive thirst, copious urination and they are treated by plants’ extracts. However, according to the Egyptian endocrinologist, historian of medicine and translator of the Ebers papyrus Paul Ghalioungui (1908-1987), the description of a probable diabetes, in Ebers, is regarded as unsatisfactory and probably wrong. In Kahun papyrus (c. 2000 BC) there is just the title of a recipe for the “Treatment of a thirsty woman”, but the text is missing[5]. So, we may assume that ancient Egyptians could not recognize behind the symptoms of specific disease entity such as diabetes.
Around the 5th century BC, the famous Indian surgeon Sushruta, in his work Samhita, identified diabetes, by using the term madhumeha (honey-like urine) and pointed out not only the sweet taste of the urine but also its sticky feeling to the touch and its ability to attract the ants (!). Sushruta further mention that diabetes affects primarily the rich castes and is related to the excessive food consumption as the rice, cereals and sweets[6].
In ancient China, Chang Chung-Ching (ca. 160-ca. 219), referred to as “the Chinese Hippocrates”, described polyuria, polydipsia and loss of weight as symptoms of a specific disease, while in 7th century AD Chen Chuan recorded the sweet urine in diabetes mellitus and named the disease Hsiao kho ping mentioning its characteristic symptoms: intense thirst, copious drinking and large amounts of urine which is tasted sweet. In an attempt to treat that disease his colleague Li Hsuan proposed the abstinence from wine, salt and sex[6].
From the 8th century onwards, physicians observed the tendency of diabetic patients to develop skin infections as furuncles, rodent ulcers and troubles of the eyesight. In 11th century AD, the celebrated Arabo-islamic physician Avicenna (980-1037) in his textbook El-Kanun (Canon of Medicine) described diabetes and mentioned gangrene and sexual dysfunction as its complication. Years later, the medieval scholar Moises Maimonides (1138-1204) described in detail diabetes, including the symptoms of acidosis[6].
Ancient Egyptians, Indians, Chinese and Arabs tried to describe the clinical signs and symptoms of diabetes mellitus. However, few are the main protagonists in the history of diabetes mellitus who contributed significantly, not only to its diagnosis and treatment but also to the development of our current notions on the disease, paving the way for further study and establishing a new medical sub specialty, diabetology.
ARETAEUS OF CAPPADOCIA (2nd CENTURY AD) AND THE FIRST ACCURATE DESCRIPTION OF DIABETES
Aretaeus, surnamed the Cappadocian, is probably the greatest physician of the Greco-Roman antiquity after Hippocrates, and at least equal of Galen. He was born in Cappadocia, a region in eastern Asia Minor, studied medicine in Alexandria and practiced in Rome probably during the 2nd century AD. Areataeus’ medical practice was based on the principals of the Pneumatic school believing not only in the vital role of pneuma (air) but embracing also the theory of the four humors (heat, coldness, moisture, dryness). In his two treatises, De causis et signis morborum acutorum et diuturnorum (on the causes and symptoms of acute and chronic diseases) and De curatione morborum acutorum et diuturnorum (on the cure of acute and chronic diseases), written in Ionic dialect, Aretaeus impresses us by the vividness and the simplicity of his descriptions. Among others he described, in an accurate way for his time, leprosy, asthma, pneumonia cancer, tetanus, hysteria, epilepsy, gout[7,8] (Figure 1).
Figure 1.
The distinguished physician Aretaeus of Cappadocia. (Source: Wellcome Library, London).
Before Aretaeus, ancient Greek medical authors such as Rufus of Ephesus (c. 1st century AD) and Galen (130-c.201) were mentioning that diabetes was provoking excessive thirst, polyuria, emaciation of the human body, leading sometimes to death. The symptom of polyuria gives the idea to Galen, who according to his own writings he has seen the disease only twice, to name diabetes diarrhea urinoma (diarrhea of the urine). Later, the term diabetes was introduced into medical nomenclature by Aretaeus. It arises from the Greek verb διαβαινω (diabaino) which means I pass through and diabetes, the condition that the fluid runs through.
In the following passage of Areateus’ work, we may admire the clinical presentation and interpretation of diabetes: “Diabetes is a wonderful affection, not very frequent among men… The course is the common one, namely, the kidneys and the bladder; for the patients never stop making water, but the flow is incessant, …. The nature of the disease, then, is chronic, and it takes a long period to form; but the patient is short-lived, if the constitution of the disease be completely established; for the melting is rapid, the death speedy. Moreover, life is disgusting and painful; thirst; excessive drinking, which, however, is disproportionate to the large quantity of urine, for more urine is passed; and one cannot stop them either from drinking or making water. Or if for a time they abstain from drinking, their mouth becomes parched and their body dry; they are affected with nausea, restlessness, and a burning thirst; and at no distant term they expire. Thirst, as if scorched up with fire... But if it increase still more, the heat is small indeed, but pungent, and seated in the intestines; the abdomen shriveled, veins protuberant, general emaciation, when the quantity of urine and the thirst have already increased; and when, at the same time, the sensation appears at the extremity of the member, the patients immediately make water”. For the treatment of the disease he proposes the consumption of cereals, milk and wine, the topical application of cataplasms and the administration of Theriac, the famous cure all remedy of antiquity[7,8].
However, it remains unknown how Aretaeus made such a precise description of a relatively rare disease during that period, just by observation.
THOMAS WILLIS (1621-1675) AND THE TERM “MELLITUS”
The English anatomist and physician Thomas Willis, is considered one of the greatest physicians in 17th century. He lived in a period that England was in political and religious turmoil and he needed to interrupt several times his studies. Willis studied classics and then medicine at Oxford where he was appointed Professor of Natural Philosophy to the highly prestigious Sedleian chair. During his career, he wrote several books and articles on medicine and his work on the anatomy of the brain and nervous system, based on his own dissections, remains very celebrated. Willis provided the description of the autonomic nervous system, the spinal cord, the vasculature at the base of the brain (circle of Willis) and the cranial nerves, including the accessory nerve (Willis’ nerve)[9].
Willis, as physician, belonged to the Iatrochemical School of medicine which believed that chemistry was the basis of human function. Concerning diabetes, in his Pharmaceutice rationalis, Willis devoted a chapter to the “pissing evil”. He commented on the sweetness of the urine in diabetic patients, coining also the term mellitus[10]. It was actually a rediscovery, as in the 7th century BC the Indian physician Sushruta mentioned the sweet urine of the disease but this work apparently was unknown to Willis. So, he was the first European medical writer who mentioned the sweet taste of the urine in diabetes mellitus. It seems that he saw several cases of diabetes mellitus and he believed that it was due to an affection of the blood rather of the kidneys. He attributed it to the eating habits and psychological status “an ill manner of living and chiefly an assiduous and immoderate drinking of cider, beer and sharp wines; sometimes sadness, long grief”. He recognized also diabetic neuropathy in the sufferers describing it as “stinging and other…frequent contractions or convulsion, twinging of the tendons and muscles and other disturbances”[9-11].
Concerning the sweet taste of the urine, he reported a case of “a certain noble earl” who suddenly “became much inclined to excessive pissing… in the space of twenty-four hours, he voided almost a gallon and a half of limpid, clear, and wonderful sweet water, that tasted as if it has been mixed with honey”. Therapeutically he considered beneficial for the disease a “thickening and moderately cooling diet and cordials” and he mentioned that slimy vegetables, rice, white starch may improve patient’s status. He also suggested a milk drink which was distilled with cypress tops and egg whites, two powders (a mixture of gum arabic and gum dragant), rhubarb and cinnamon. Following Willis’ therapeutic advices, patient’s condition improved in a month but immediately after his recovery, he returned to his past dietary habits[9].
However Willis could not explain “why the urine is wonderfully sweet like sugar or honey”. The explanation was given 100 years later, by another English physician, Matthew Dobson (1732-1784) of Liverpool, who experimentally demonstrated the presence of sugar in urine. He actually boiled urine to dryness and noticed that the residue, a crystalline material, had the taste of brown sugar[11].
CLAUDE BERNARD’S (1813-1878) BRILLIANT DISCOVERY ON THE GLYCOGENIC ACTION OF THE LIVER
Born to a poor family in Beaujolais region, south of France, Claude Bernard at the age of 19 was apprenticed to an apothecary. His passion for the theatre led him to write two plays La Rose du Rhône and Arthur de Bretagne but soon after arriving to Paris, he was discouraged by the literary critic and politician Saint-Marc Girardin (1801-1873) who counseled him to enroll in medicine. In Medical School of Paris, Bernard was not considered a brilliant student and unwilling to practice medicine, he was appointed assistant to the Professor of Physiology and pioneer of experimental physiology François Magendie (1783-1855). However, Bernard’s research career was very successful. In 1854, he became member of the Academy of Sciences and later on he succeeded Magendie to the chair of experimental physiology at the College de France. The Emperor Napoleon III admired him so much that created two laboratories for him and made him a Senator. Among Bernard’s several discoveries we may cite: the vasomotor innervation, the principle of physiological determinism, the concept of internal secretion, the concept of milieu intérieur or internal environment (meaning the interstitial fluid, and its physiological capacity to ensure protective stability for the tissues and organs), the nature and function of curare, carbon monoxide and other poisons (Figure 2). Unfortunately, the only way to understand and discover all these phenomena, promoting our knowledge to physiology, was through animals’ vivisections. This was the reason for his wife to divorce him and join with his children the antivivisection movement, campaigning actively on the issue[12].
Figure 2.
Portrait of the French physiologist Claude Bernard. (Source: Wellcome Library, London).
Bernard’s contribution in the study of metabolism and diabetes remains leading. In 19th century, scientists hypothesized on the role of pancreas in the physiopathology of diabetes as they found in the post-mortem examination of the diseased, atrophic or stone filled pancreases. However, as they believed that pancreas was an exocrine organ, they interpreted these post-mortem findings as a chance phenomenon. During that period the French experimental physiologist, Claude Bernard decided to test this hypothesis[1,12].
At the beginning, he falsely believed that “diabetes was a nervous affection of the lungs”. However, during an experiment, he injected grape sugar into the jugular vein of a dog, extracting at the same time blood from the carotid artery. This blood contained a large amount of sugar and he realized that glucose was not destroyed in the lungs, because blood must pass by these organs in order to move from the jugular vein to the carotid artery. He was then fed dogs on a carbohydrate-rich diet, the blood from the hepatic veins and vena cava contained sugar which was not destroyed in the liver and was also present in heart ventricles, so the theory of lungs’ role in diabetes was rejected. In further experiments, Bernard proved that animal blood contains sugar even if it is not supplied by food. Testing the theory that sugar absorbed from food was destroyed when it was passing through tissues, Bernard put dogs in carbohydrate diet and killed them immediately after feeding. To his surprise he observed large amounts of sugar in hepatic veins. The same observation was done in the control group, animals that were fed only by meat. He then moved to the analysis of liver tissue samples and in every liver he examined he found large quantities of glucose which was missing from other organs. He concluded that liver was storing a water insoluble starchy substance that he named glycogen which was converted into sugar or glucose and secreted into the blood. He assumed that it was an excess of this secretion that caused diabetes[13,14].
Moving toward, Bernard demonstrated the connection between the central nervous system and diabetes. Using a needle, he stimulated the floor of the fourth brain ventricle and produced temporary “artificial diabetes” which lasted less than one day. He named this procedure piqûre diabétique and linked for the first time glucose homeostasis and the brain to the pathogenesis of diabetes[15] (Figure 3).
Figure 3.
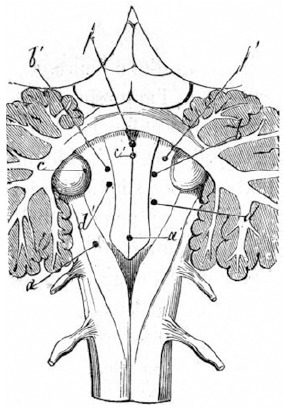
Sites of punctures of 4th ventricle from Bernard’s book «Leçons sur la Physiologie et la Pathologie du Système Nerveux», 1858. (Source: Wellcome Library, London).
The work of Claude Bernard on glycogenic action of the liver illuminated the pathway of gluconeogenesis and promoted the study of diabetes.
OSKAR MINKOWSKI (1858-1931) AND JOSEPH VON MERING (1849-1908): THE DISCOVERY OF “PANCREATIC DIABETES”
A turning point in the history of diabetes mellitus took place in 1889 after the experiments of Minkowski and von Mering.
In 1886, three years before their first meeting, von Mering discovered that phlorizin, a glucoside, could cause transient glucuresis. In 1889, while von Mering was working in Hoppe Seyler’s Institute at the University of Strasbourg, Minkowski, assistant at that time to the German leading authority on diabetes Professor Bernard Naunyn (1839-1925), he visited the Institute to look at some chemical books of the library. They met accidentally and talked about Lipanin, an oil containing free fatty acids and von Mering used to administrate to patients suffering from digestive disturbances. Minkowski was not in favor of Lipanin intake and then their conversation turned on whether the pancreas had a role in digestion and absorption of fats. As a result of the discussion, the two men decided the same evening to perform a pancreatectomy in a dog in Naunyn’s laboratory. The animal remained alive and was closely observed by Minkowski, as von Mering left urgently to Colmar because of a family issue. Soon after the operation, the dog developed polyuria. Minkowski examined the urine and found that it contained 12% sugar. Initially Minkowski believed that the dog developed diabetes due to the fact that von Mering had treated it for a long time with phlorizin. So he repeated the pancreatectomy in three more dogs which had no sugar in their urine previous to operation and all of them developed glycosuria[13,16].
Furthermore Minkowski implanted a small portion of pancreas subcutaneously, in depancreatized dogs, and observed that hyperglycemia was prevented until the implant was removed or had spontaneously degenerated[13].
Minkowski and von Mering experiment demonstrated that pancreas was a gland of internal secretion important for the maintenance of glucose homeostasis. They also paved the way for Banting and Best to conduct their experiments and to meet with success.
FREDERICK BANTING (1891-1941), CHARLES BEST (1899-1978), JAMES BERTRAM COLLIP (1892-1965) AND JOHN MACLEOD (1876-1935): THE DISCOVERY OF INSULIN
In 1923 the Nobel Prize in Medicine was awarded to Frederick Banting and John MacLeod for the discovery of insulin. It was actually a story of success that provoked a great scientific conflict.
Frederick Banting was a young Canadian surgeon, who was admitted into the laboratory of the eminent biochemist, interested in diabetes, Professor John Macleod, at the University of Toronto[13]. In 1920, Moses Barron, physician in Minnesota, published an article on “The relation of the islets of Langerhans to diabetes, with special reference to cases of pancreatic lithiasis[17] which was mentioning that the continuation of experiments of Minkowski and von Mering could lead to the discovery of a substance capable to control diabetes. Influenced by this article, Banting focused on the study of diabetes[13]. During that period the distinguished English physiologist Ernest Starling (1886-1927) was mentioning: “We don’t know yet how the pancreas affects sugar production or utilization in the same animal. It is generally assumed that it secretes into the bloodstream a hormone which may pass to the tissues and enable them to utilize sugar or pass to the liver and inhibit the sugar production of this organ… but we have been unable to imitate the action of the pancreas still in vascular connection with the body, by injection or administration of the extracts of this organ”[18].
On 16 May 1921, Banting started to collaborate with Charles Best, a young medical student. Experimenting in dogs they initially ligate the pancreatic ducts, achieving atrophy of the exocrine region and almost ten weeks later they removed dog’s degenerated pancreas. They crushed the atrophied pancreatic glands in a cool mortar and froze it in salt water. Then the mass was ground down and added to 100 mL of physiological salt. Afterwards, they administrated 5 mL of this extract intravenously to a depangreatized dog. Within 2 h its blood sugar had considerably dropped. They repeated several times the experiment with other diabetic dogs, gaining similar results and they experimented also with fetal calf pancreas using different ways of administration such as subcutaneous and rectal[19,20] (Figure 4).
Figure 4.
The Nobel laureate Frederick Banting in his laboratory with a dog. (Source: Wellcome Library, London).
At the end of 1921 the skilled chemist James Collip joined the team and developed a better extraction and purification technique. Obtained substance was initially named by the team insletin and later on by MacLeod insulin[13].
The next step was to test insulin in humans. So on 11 January 1922, insulin was administrated to Leonard Thompson a 14-year-old boy treated for diabetes in Toronto Hospital[13]. It’s worth mentioning that after the introduction of Apollinaire Bouchardat’s (1806-1886) pioneering dietary treatment for diabetes, physicians repeated in several generations of diabetics his motto: “mangez le moins possible” (eat as little as possible)[21,22]. Thomson was also following a strict fasting diet proposed by Frederick Madison Allen (1879-1964) and he was in critical state. He received 15 mL of insulin, injected in his buttock but he developed abscesses at the injection site and became even sicker. Collip further improved the quality of insulin and on January 23, Thompson received a second injection. The results were excellent. His blood glucose from 520 mg/dL fell to 120 mg/dL in 24 h and urinary ketones disappeared. Thompson continued the treatment with insulin and lived another 13 years. He died of pneumonia at 27 years old[13]. Similar is the story of Elizabeth Hughes Gossett (1907-1981). Daughter of the United States politician Charles Evans Hughes, Elisabeth was diagnosed with diabetes at age 11. Initially she was also treated by Allen and in August 1922 began the use of insulin. She survived, graduated from College, got married, had three children and died suddenly of a heart attack at 74 years old[23].
The pioneering work of Banting and Best saved millions of lives and diabetics started to live a normal life. Lilly Pharmaceutical Company collaborated with the two scientists and in 1923 introduced Iletin, the world’s first commercially available insulin product[13].
However in 1923 the Nobel Committee decided to award Banting and MacLeod for insulin’s discovery. Banting became furious as he believed that he should share the prize with Best instead of MacLeod and he decided to share with Best his cash award. In his turn, MacLeod shared also his award with Collip[13].
Another black spot in the history of insulin discovery was also the discovery of pancreatin, an extract of bovine pancreas discovered by the Romanian Professor of Physiology Nicolae Constantin Paulescu (1869-1931) in 1916, published a few years later because of the war in 1921 and patented in April 1922. Even if Paulescu was the first to provide a detailed demonstration of the antidiabetic and antiketogenic effect of a pancreatic extract, pancreatine was not used in humans and passed over silently[24].
A crucial step in the history of diabetes has been completed. Over the next years insulin purification methods improved and new insulin formulations were developed such as Protamine–zinc insulin, a long-acting insulin in 1930s, neutral protamine Hagedorn in 1940s and Lente series in 1950s[13].
CONCLUSION
For more than 3000 years physicians quested the causes and treatment of diabetes mellitus (Figure 5). However, an important progress has been made over the last two centuries thanks to the development of chemistry, physics and pharmacology. Over the next years scientists continued to make significant discoveries: The structure of insulin was delineated in 1955 by the Nobel laureate Fred Sanger (1918-2013); in 1967 proinsulin was discovered by Donald Steiner (1930-2014) and with his colleagues he produced the radioimmunoassay for C-peptide which is used today to measure endogenous insulin production; in the same year, the first pancreas transplant in a human was performed by William Kelly, Richard Lillehei (1927-1981) and colleagues at the University of Minnesota; in 1972 the U100 insulin was introduced to promote better accuracy in administration; ten years later, in 1982, recombinant human insulin became available and in early 1990’s insulin pen delivery devices become popular following by the discoveries of short (1996) and long (2001) acting insulin analogues[1].
Figure 5.
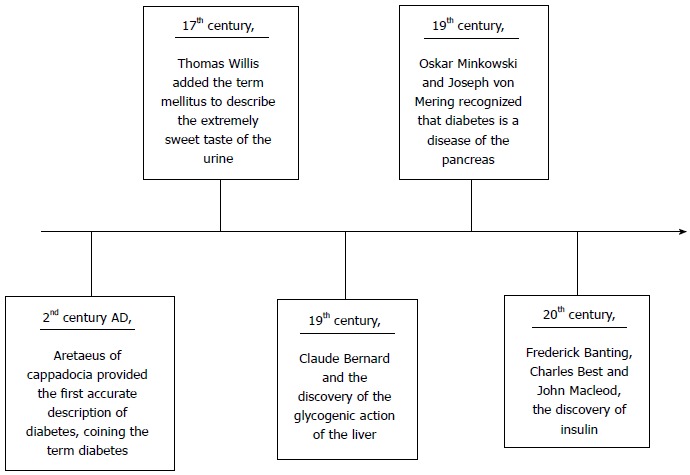
Timeline table presenting the main contributors in the history of diabetes mellitus.
Since biotechnology helps medicine to progress, nobody knows what the future will bring. We are sure of just one thing: History of diabetes is being still written.
Footnotes
Conflict-of-interest statement: There is no conflict of interest associated with any of the senior author or other coauthors contributed their efforts in this manuscript.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: August 13, 2015
First decision: September 17, 2015
Article in press: December 18, 2015
P- Reviewer: Charoenphandhu N, Hssan M, Masaki T, Tarantino G S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
References
- 1.Kahn CR, Weir GC, editors . Joslin’s diabetes mellitus, 14th ed. Philadelphia: Lippincott; 2005. [Google Scholar]
- 2.Geneva: World Health Organization, 2012. Philadelphia: Lippincott; [Google Scholar]
- 3.World Health Organization. Global health estimates: Deaths by cause, age, sex and country, 2000-2012. Geneva: World Health Organization; 2014. [Google Scholar]
- 4.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghalioungui P. The Ebers papyrus: A new English translation, commentaries and glossaries. Cairo: Academy of Scientific Research and Technology; 1987. [Google Scholar]
- 6.Peumery JJ. Histoire illustrée du diabète. De l’Antiquité à nos jours. Paris: Les Éditions Roger Dacosta; 1987. [Google Scholar]
- 7.Laios K, Karamanou M, Saridaki Z, Androutsos G. Aretaeus of Cappadocia and the first description of diabetes. Hormones (Athens) 2012;11:109–113. doi: 10.1007/BF03401545. [DOI] [PubMed] [Google Scholar]
- 8.Adams F The extant works of Aretaeus the Cappadocian. London: Sydenham Society, 1856 [Google Scholar]
- 9.Furdell EL. Fatal Thirst. Diabetes in Britain until Insulin. Leiden: Brill; 2009. pp. 81–92. [Google Scholar]
- 10.Willis T Opera Omnia. Coloniae: Sumptibus Gasparis Storti, 1694: 460. Leiden: Brill; [Google Scholar]
- 11.Williamson RT. English Physicians of the past. Newcastle: Andrew Reid and Company; 1923. pp. 47–52. [Google Scholar]
- 12.Grmek M. Le Legs de Claude Bernard. Paris: Fayard; 1997. [Google Scholar]
- 13.von Engelhardt D, editor . Diabetes: Its medical and cultural history. Berlin: Springer-Verlag; 1989. pp. 306–319, 350-358, 411-426. [Google Scholar]
- 14.Bernard C Du suc pancréatique et de son rôle dans les phénomènes de la digestion. C R Soc Acad Sci (Paris) 1850; 1: 99-119. Berlin: Springer-Verlag; [Google Scholar]
- 15.Grmek M. Examen critique de la genèse d’une grande découverte: La piqûre diabétique de Claude Bernard. Clio med. 1965;1:341–350. [Google Scholar]
- 16.von Mering J, Minkowski O. Diabetes mellitus nach Pankreas extirpation. Arch f exper Path u Pharmakol. 1889;26:371. [Google Scholar]
- 17.Barron M. The relation of the Islets of Langerhans to Diabetes. Surg Gynecol Obstet. 1920;31:437–448. [Google Scholar]
- 18.Medvei VC. The History of Clinical Endocrinology: A Comprehensive Account of Endocrinology from Earliest Times to the Present Day. New York: Parthenon; 1993. p. 253. [Google Scholar]
- 19.Banting FG, Best CH, Collip JB, Cambell WR, Fletcher AA, Macleod JJR, Noble EC. The Effect Produced on Diabetes by Extractions of Pancreas. Transact Ass Amer Physicians. 1922;37:337. [Google Scholar]
- 20.Banting FG, Best CH, Macleod JJR. The internal secretion of the pancreas. Am J Physiol. 1922;59:479. [Google Scholar]
- 21.Karamanou M, Koutsilieris M, Laios K, Marineli F, Androutsos G. Apollinaire Bouchardat (1806-1886): founder of modern Diabetology. Hormones (Athens) 2014;13:296–300. doi: 10.1007/BF03401345. [DOI] [PubMed] [Google Scholar]
- 22.Bouchardat A De la glycosurie ou diabète sucré. Son traitement hygiénique. Paris: Baillière, 1875 [Google Scholar]
- 23.Cooper T, Ainsberg A. Breakthrough: Elizabeth Hughes, the Discovery of Insulin, and the Making of a Medical Miracle. New York: St Martin’s Press; 2010. [Google Scholar]
- 24.Angelescu C, Nicolae C. Paulescu: Omul şi opera sa medicală. Bucuresti: Vremea; 2009. [Google Scholar]


