Abstract
Purpose of review
To propose a prevention of mother-to-child transmission (PMTCT) care continuum that defines the programmatic steps necessary to provide HIV care to the HIV-infected pregnant woman and her infant during the risk period for HIV transmission.
Recent findings
There are several complexities of PMTCT care that should be considered in the care continuum including the evolution in the population of women entering PMTCT care, various models of PMTCT service delivery and patterns of PMTCT care, and the critical step of transfer of women’s HIV care from PMTCT programs to adult HIV clinics.
Summary
We propose a re-conceptualized PMTCT care continuum that accounts for the complexities of PMTCT care. We also propose a combined outcome for pregnant women and their infants across an interlinked PMTCT continuum to measure both maternal and child health outcomes.
Keywords: HIV, PMTCT (prevention of mother-to-child transmission), vertical transmission
Introduction
Over the past decade, the scale-up of prevention of mother-to-child transmission (PMTCT) services in resource-limited settings has been remarkable with substantial increases in coverage rates of HIV testing and receipt of antiretroviral drugs among pregnant and breastfeeding women (1). As a result of these efforts, between 2009 and 2013 globally there was an estimated 40% reduction in vertical transmission of HIV (2). Nonetheless, there were 240,000 new infections among children in low- and middle-income countries in 2013, and more than 20 countries globally that have perinatal rates above 30% (2).
In 2013, WHO Guidelines recommended triple antiretroviral therapy (ART) for all HIV-infected pregnant and breastfeeding women, regardless of the woman’s CD4+ cell count, referred to as the Option B+ approach (3). The goal of Option B+ is to increase ART coverage during pregnancy and breastfeeding, ensure that all ART eligible women initiate treatment, and further reduce vertical transmission. This approach has streamlined the PMTCT care continuum, avoiding the need for laboratory assessment for ART eligibility and simplifying antiretroviral options to triple drug therapy for all pregnant women rather than tailoring antiretroviral options based on the woman’s HIV disease stage.
Most high-prevalence countries such as South Africa, Uganda, and Zambia are adopting Option B+ nationally. Malawi was the first country to introduce Option B+ in late 2011 and quickly demonstrated enormous success in expanding ART access across the country and dramatically increasing the number of HIV-infected pregnant women starting ART. In the first quarter of implementation, there was a 748% increase in the number of HIV-infected pregnant women who started lifelong treatment. By the third quarter of 2012, pregnant women comprised 35% of all adults initiated on ART in the country (4).
While Option B+ appears to have improved the number of pregnant women initiating ART, the progress of PMTCT programs towards eliminating vertical HIV transmission and achieving desired health outcomes for HIV-infected women and their infants is dependent on many steps beyond just initiation of ART. Suboptimal retention in PMTCT care continues to threaten efforts to prevent new pediatric infections. In a study conducted in Malawi, attrition of pregnant women in 540 health facilities providing Option B+ was 17% within six months of ART initiation, with five-fold higher risk of attrition (adjusted odds ratio 5.0, 95% CI 4.2–6.1) among women starting ART during pregnancy as compared to women with advanced disease initiating treatment for their own health (5).
The PMTCT care continuum is a framework of essential steps that are needed for both the pregnant woman and her infant in order to achieve the desired outcome of HIV-free survival as well as optimal retention, adherence and viral load suppression among the HIV-infected woman. In this paper, we propose a PMTCT care continuum that consists of two interlinked continua of care—one for the HIV-infected woman and one for her child—and discuss complexities in effective engagement of women and infants in and across each step of the continua that must be addressed to optimize maternal and child health outcomes.
The PMTCT Care Continuum
PMTCT care involves two persons—the pregnant woman and her infant—motivating the need for two interlinked PMTCT continua, one focusing on maternal care and the other highlighting key steps across the child’s continuum of care.
Maternal PMTCT Continuum
Identification of HIV infection in pregnant women is a critical step in the prevention of MTCT. As noted in Figure 1, HIV testing is the first step in the maternal PMTCT continuum. All pregnant women should be provided opt-out HIV testing during antenatal care, with repeat testing at delivery of those who test negative and repeat testing of negative women with each additional pregnancy (6). In a review of 44 studies from 15 countries in sub-Saharan Africa, HIV-testing uptake at antenatal care (ANC) was 94% (CI 95% 92–95%) for opt-out testing as compared to 58% (95% CI 40–75%) with an opt-in approach (7). The adoption of routine provider-initiated HIV testing and counseling within ANC has facilitated progress towards universal testing among pregnant women (8). It is also important to note that pregnancy and the post-partum period are times of high risk for HIV acquisition which confer significantly increased risk of MTCT as well (9). Therefore, detection of HIV should be prioritized through repeat testing at delivery and during breastfeeding in high HIV prevalence settings (10–12).
Figure 1.
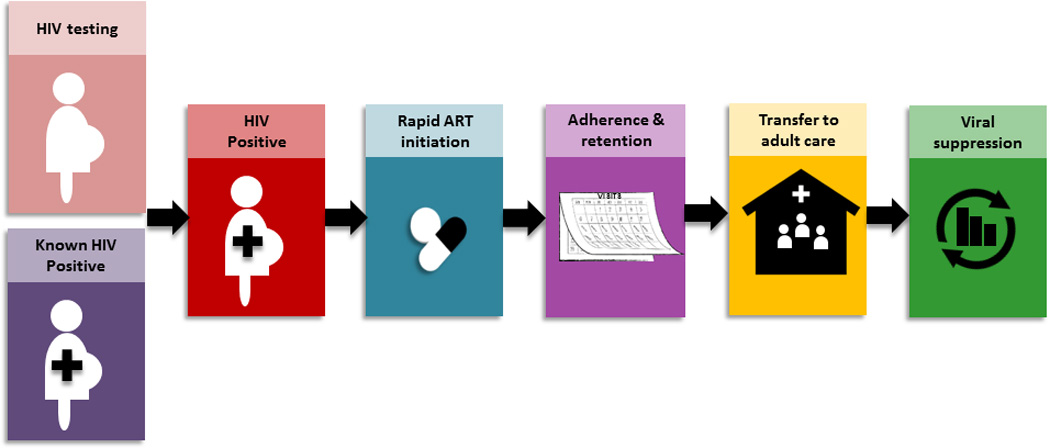
PMTCT and HIV Care Continuum: Pregnant Women
The second step in the continuum is prompt ART initiation among HIV-infected pregnant women as soon as possible after HIV diagnosis and as early as possible in the course of pregnancy. Studies have shown that longer duration of ART use by the woman during pregnancy is correlated with a reduced risk of transmission to the infant (13–15). Over the past several years there have been changes in the models of care for ART delivery to HIV-infected pregnant women. The training of nurses and other non-physician cadres to prescribe ART in the ANC setting, in contrast to referring ART eligible pregnant women to adult HIV clinics to initiate treatment, has expedited ART initiation and been associated with reduced loss to follow-up among pregnant women. A study conducted in South Africa reported that integration of ART into ANC was associated with increases in the proportion of eligible pregnant women starting ART and shorter time to start ART, with 82% of women initiating ART at their first ANC visit (16). The third step in the continuum involves retention of women in PMTCT care and support of adherence to ART throughout the course of the pregnancy and breastfeeding periods. Retention in care is critical for management of ART side-effects and treatment failure, prevention of opportunistic infections, and in some settings receipt of reproductive health services. Adherence to ART during pregnancy and breastfeeding is essential for prevention of MTCT, as maternal viral load is the primary determinant of risk of the infant acquiring HIV infection (17). The fourth step in the continuum involves the woman’s transfer of HIV care from PMTCT services, generally provided in ANC clinics, to adult HIV care and treatment, which is often located in a different clinic location in order to ensure that the women continue to receive lifelong HIV care. Depending on how services are organized in specific settings, transfer of care can take place during pregnancy, after delivery, or after cessation of breastfeeding when perinatal transmission risk ends (Figure 2). The ultimate step in the maternal continuum is maintenance of lifelong viral suppression, which is critical for long-term health of the mother and only achieved through adherence to treatment and retention in care.
Figure 2.
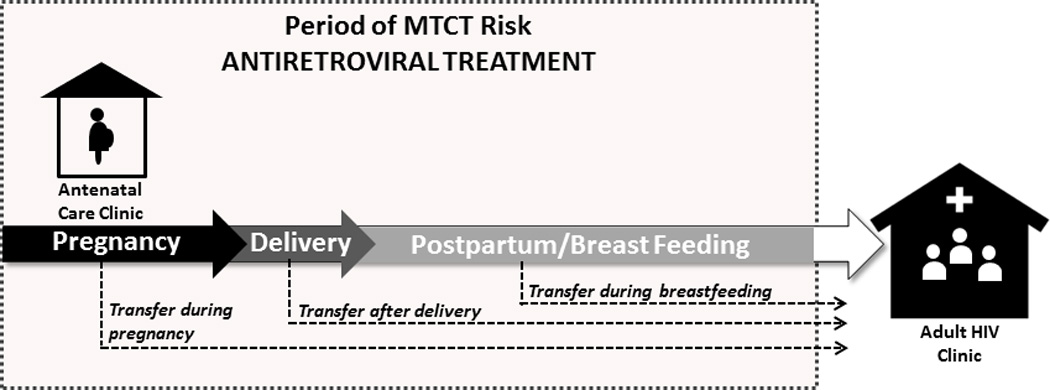
Timeline for transfer from antenatal care to adult HIV care for antiretroviral treatment during period of risk for vertical HIV transmission
While often not recognized as a component of the PMTCT care continuum, pregnant women who test HIV-negative should be provided with HIV prevention services, which are generally available at clinic locations outside of the maternal-child health setting. Services include partner testing, condom use, and repeat HIV testing.
Infant PMTCT Continuum
The first step in the infant PMTCT continuum is initiation of antiretroviral (ARV) prophylaxis within hours of birth (Figure 3). WHO guidelines recommend 6–12 weeks of daily ARVs for all HIV-exposed infants independent of maternal ART regimen (3). The second step is virologic testing, early infant diagnosis, which should be done at 6 weeks of age to determine if the exposed infant is HIV-infected. Virologic testing, with HIV RNA, DNA or total nucleic acid, can be utilized to detect the HIV virus and distinguish HIV exposure, as evidenced by presence of maternal HIV antibodies which cross the placenta, from HIV infection. Based on the result of the virologic test, the continuum for infants varies. Infants determined to have a positive virologic test must be transferred to pediatric HIV care and treatment services, where ART is promptly initiated in order to prevent the early morbidity and mortality of untreated HIV infection in infants (18). Infants must then be retained in HIV care where they can be monitored for growth, development and treatment side-effects, and receive prophylaxis for opportunistic infections and support for optimal ART adherence. The final step in the continuum for HIV-infected infants and children is viral load suppression and retention in lifelong care, similar to their mothers.
Figure 3.
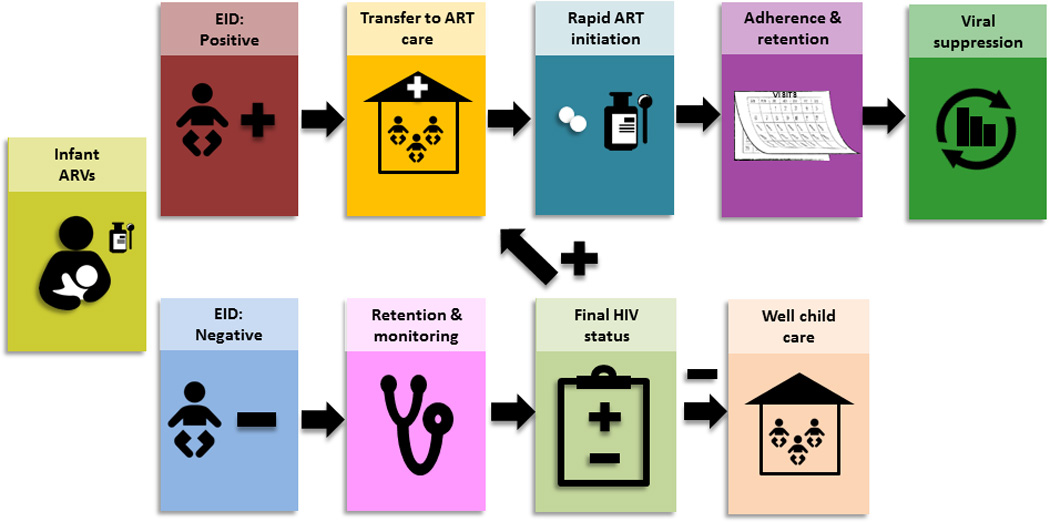
PMTCT and HIV Care Continuum: Infants
For infants who have a negative virologic test at 6 weeks, it is critical that they remain in care until 18 months of age or until after weaning, whichever is later, when final HIV status can be assessed. These infants need to be monitored for growth and development and for evidence of HIV disease, and then retested for infection, typically by HIV antibody testing. Infants found to be infected must be rapidly linked to pediatric HIV care and treatment services and initiated on ART while those who test negative are linked to routine well-child pediatric care. The ultimate endpoint for the uninfected infants is HIV-free survival, typically measured at 18–24 months after birth.
Complexities of the PMTCT Care Continuum
The proposed interlinked PMTCT continuum acknowledges several complexities in PMTCT care which have not previously been featured, including: 1) the evolution of the population of women entering PMTCT care; 2) various models of PMTCT service delivery and patterns of PMTCT care; and 3) the need for a new step in the PMTCT continuum accounting for the transfer of the woman’s HIV care from PMTCT programs to adult HIV care and treatment services. We also propose consideration of a combined final outcome for the woman and the child across an interlinked PMTCT continuum.
The evolution of the population of women entering PMTCT care
The traditional PMTCT care continuum begins with testing of pregnant women during antenatal care. However, the scale-up of HIV services over the past decade has resulted in more women who are already known to be HIV infected and engaged in HIV care who become pregnant. Such women are referred to PMTCT programs for antenatal care and initiation of ART for prevention of vertical transmission, if not already receiving it for their own health. As these women were already in HIV care prior to the pregnancy, the decision as to where they will continue to receive HIV care and treatment during pregnancy and postnatally during breastfeeding will depend on how services are organized—options may include follow-up in the adult HIV clinic, the ANC clinic or a PMTCT clinic. Figure 4 shows HIV and treatment status among 46,989 pregnant HIV positive women entering PMTCT services, October 2013-March 2015, at sites supported by ICAP at Columbia University in four countries in Sub Saharan Africa (Democratic Republic of Congo, Mozambique, Ethiopia, Cote d’Ivoire). At entry into ANC care, 31% of all HIV-infected women were already known to be HIV positive and 24% were receiving ART.
Figure 4.
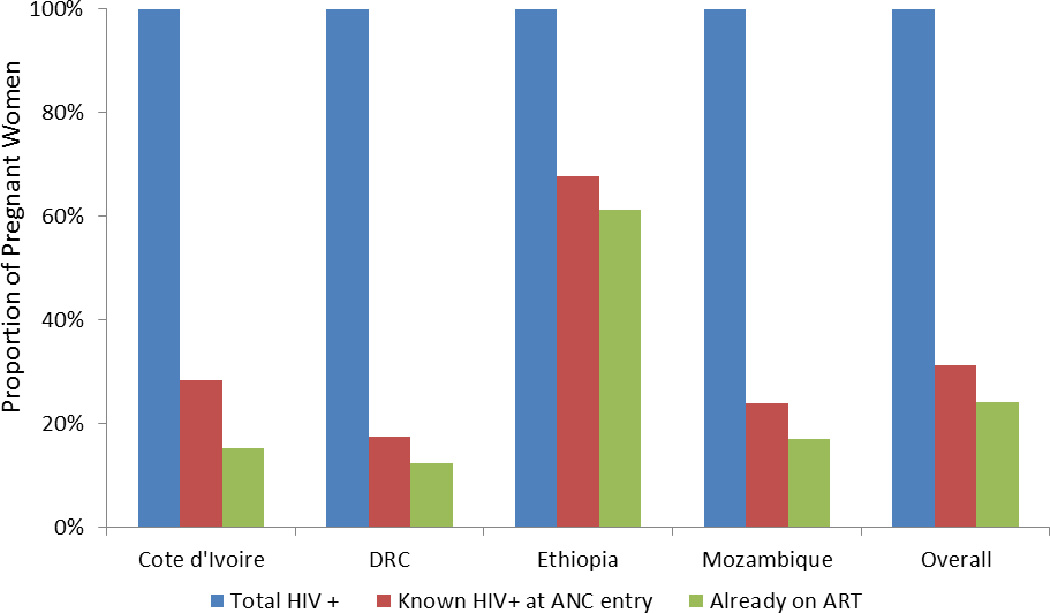
Percent of all pregnant women entering ANC who were known positive at entry and who were already on ART: N =46,989, October 2013-March 2015
Variation in PMTCT Models and Patterns of Care
One key challenge in providing pregnant HIV-infected women and their infants with care is that each step in the continuum may be situated in a different physical location. This differs from adult HIV care in which the majority of steps (i.e., enrollment in HIV care, assessment for HIV eligibility, ART initiation, and follow-up care) occur in the same clinical context. Variations in location of care delivery have led to a diversity of PMTCT models of care. A study in Kenya found that an integrated model of ANC and HIV care within an ANC clinic setting, as compared to non-integrated care in which PMTCT services are provided in an ANC setting but women are referred for HIV care at HIV clinics, was associated with increased enrollment in HIV care, a shorter time to enrollment in HIV care, and a higher proportion of women who initiated ART (19). Van Lettow et al. describe several PMTCT Option B+ “models of care” in Malawi which include: 1) all PMTCT care including ART provided in the ANC clinic, 2) women initiating ART in the ANC clinic with referral to the adult HIV clinic for ongoing ART throughout pregnancy, 3) women referred from the ANC clinic to the adult HIV clinic for ART initiation and follow-up throughout pregnancy, and 4) women initiating ART in an ANC or an adult HIV clinic with referral to another HIV clinic for ongoing ART throughout pregnancy (20). However, these models focus primarily on the antenatal period with less attention given to the postpartum period, an equally important period when adherence to ART and retention in care are critical for the woman as well as for prevention of HIV transmission during breastfeeding (21).
A second complexity in PMTCT care is the fact that pregnant women may migrate to their home communities seeking support from their families during delivery and the post-partum period. Some may return back with their infants and continue care at their primary clinics, while others may choose to continue care elsewhere or leave their infants with family members. These often time-limited periods of migration are difficult to document within the PMTCT care continuum. Using the lexicon of the adult HIV care continuum, such gaps in care among women who leave and return to HIV care are referred to as a “side door” (22). HIV programs should strengthen counseling among women who wish to migrate during the MTCT risk period in order to avoid treatment interruptions, rebound viremia, and health threats to both the woman and her baby. Should the woman choose to transfer HIV care during pregnancy, robust communication between staff members in the various clinics, including documentation of necessary information, must occur to ensure women receive ongoing PMTCT care and to minimize misclassification of losses to care.
Transfer of maternal HIV care from PMTCT to adult HIV services
Typically, the PMTCT care continuum has focused on the steps involved in determining the final HIV status of the exposed infant and only included steps in the mother’s pathway of care as related to that outcome (23–25). The continuum must be expanded to include the transfer of the mother’s HIV care from PMTCT services to adult HIV care and treatment as this step is essential for optimal health outcomes of the mother and for prevention of HIV transmission during future pregnancies and to her sexual partners. Depending on an HIV program’s model of care, transfer can happen early (if ART is administered in the ART clinic during pregnancy), after delivery (if ART is integrated into antenatal care services), or at end of MTCT risk period/after weaning (if ART is integrated with infant postnatal follow-up) (Figure 2).
Currently, there are no guidelines for the timing or criteria for transfer, and generally no monitoring tools for measuring this step in either PMTCT or HIV programs (21). Moreover, there are large programmatic differences between PMTCT and adult HIV clinics which pose challenges for successful transfer. These include differences in clinic locations (ANC versus adult HIV clinics), staffing, clinic patient volume, waiting times, and support and peer services (26). Few studies have included this important transfer step (23, 27) which has gained more importance as increasing numbers of pregnant women initiate ART with Option B+ and thus must continue lifelong treatment.
Consideration of a combined outcome for the PMTCT care continuum
Traditionally, PMTCT program outcomes include an estimate of early vertical transmission, the number of new pediatric infections detected with early infant diagnosis, in addition to process measures for earlier steps in the continuum such as number of pregnant women tested and number who initiated ART (6, 28). A limitation of using the number of infants infected as the key outcome of the PMTCT care continuum is that it does not take into account the women and infants who are lost from the continuum prior to getting virologic testing at 6 weeks. Such losses to follow-up may be due to pregnancy-related mortality, stillbirths, miscarriages, newborn and infant mortality, as well as mother/baby disengagement from care (29). Another limitation of this endpoint is that it only acknowledges the early outcome for the infant, while failing to account for ongoing HIV transmission risk to the child during breastfeeding. Furthermore, the focus on the child does not take into account the outcome of the HIV-infected woman. In many countries with high HIV prevalence, maternal mortality remains high (30) with HIV infection being associated with a six-fold increased risk of maternal mortality (31).
To respond to the need for a more comprehensive indicator, we propose an ambitious combined PMTCT outcome which includes both HIV-free survival for the infant and sustained viral load suppression for the mother. HIV-free survival is an outcome commonly used in PMTCT research and is defined as a child being alive and HIV-free at the time of final HIV testing (typically at 18 or 24 months) (32, 33). A combined outcome that is also relevant to the long-term health of the mother raises the bar for PMTCT programs with “no partial credit” given for achievement of only one endpoint either for the woman or the child (34). The advantage of such a combined outcome is that it promotes a systems perspective, highlights the context of pregnancy which is a transient event in a chronic lifelong disease, and uses a maternal-child health approach by underscoring the impact of PMTCT programs on achievement of future maternal and child health outcomes (34, 35). Furthermore it underscores global efforts to eliminate new pediatric HIV infections and reach the ambitious new 90.90.90 targets set by UNAIDS (36, 37). Finally, a combined outcome shifts attention from counting infections to measuring survival and would indicate that PMTCT programs are implementing all of the services required to achieve optimal outcomes for both women and infants. In order to operationalize the measurement of this outcome, HIV programs as well as funders will need to embrace this approach and to establish systems to collect information to derive this combined indicator.
Conclusions
While PMTCT programs have made impressive strides in decreasing the number of HIV-infected children globally, there is still vast need for continued improvement in PMTCT program performance in order to achieve an AIDS-free generation. To further optimize PMTCT care, we propose a reconceptualization of the PMTCT care continuum to include two interlinked continua—one for the HIV-infected mother and one for her infant. We also propose a combined outcome across the continuum of maternal viral load suppression plus HIV-free infant survival which emphasizes the desired impact of PMTCT programs on maternal and child health long-term outcomes.
Key bullet point summary.
This paper presents a PMTCT care continuum that defines the programmatic steps necessary to provide HIV care to the HIV-infected pregnant woman and her infant during the risk period for HIV transmission.
The proposed PMTCT care continuum addresses several complexities of PMTCT care including the evolution in the population of women entering PMTCT care, various models of PMTCT service delivery and patterns of PMTCT care, and the critical step of transfer of women’s HIV care from PMTCT programs to adult HIV clinics.
A combined outcome across the continuum of maternal viral load suppression plus HIV-free infant survival is encouraged and emphasizes the desired impact of PMTCT programs on maternal and child health long-term outcomes.
Acknowledgements
none
Financial support and sponsorship: WES acknowledges funding support for the HIV Prevention Trials Network through National Institute of Health UM1 AI068619-08.
Footnotes
Conflicts of interest: The authors have not conflicts of interest to declare.
All authors have no funding support to report.
References
*Of importance
- 1.UNAIDS. The Gap Report. Geneva, Switzerland: WHO; 2014. [Google Scholar]
- 2.Unicef. Children, adolescents and AIDS: 2014 statistical update. New York, NY: Unicef; 2014. [Google Scholar]
- 3.WHO. Consolidated Guidelinese on The Use of Antiretroviral Drugs for Treating and Preventing HIV Infection. Geneva: WHO; 2013. [PubMed] [Google Scholar]
- 4.Centers for Disease C, Prevention. Impact of an Innovative Approach to Prevent Mother-to-Child Transmission of HIV - Malawi, July 2011-September 2012. MMWR Morb Mortal Wkly Rep. 2013;62:148–151. [PMC free article] [PubMed] [Google Scholar]
- 5. Tenthani L, Haas AD, Tweya H, Jahn A, van Oosterhout JJ, Chimbwandira F, et al. Retention in care under universal antiretroviral therapy for HIV-infected pregnant and breastfeeding women ('Option B+') in Malawi. AIDS. 2014;28(4):589–598. doi: 10.1097/QAD.0000000000000143. This is a retrostpective study of retention among HIV-infected pregnant and breastfeeding women in Option B+ PMTCT programs in Malawi which reported 17% of women were lost to follow-up 6 months after ART initiation. Additionally, women who started ART during pregnancy were five times more likely than women who started ART in advanced WHO stage or CD4 cell count less than 350 cells/uL to never return after their initial HIV care visit. Facility level data from 540 facilities with 21,939 women in addition to individual-level data from 11534 women at 19 large facilities was included.
- 6.UNICEF, UNAIDS, WHO. Towards Universal Access: Scaling up HIV services forwomen and children in the health sector--Progress Report 2011. Geneva: WHO; 2010. [Google Scholar]
- 7.Wettstein C, Mugglin C, Egger M, Blaser N, Vizcaya LS, Estill J, et al. Missed opportunities to prevent mother-to-child-transmission: systematic review and meta-analysis. AIDS. 2012;26(18):2361–2373. doi: 10.1097/QAD.0b013e328359ab0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hensen B, Baggaley R, Wong VJ, Grabbe KL, Shaffer N, Lo YR, et al. Universal voluntary HIV testing in antenatal care settings: a review of the contribution of provider-initiated testing & counselling. Trop Med Int Health. 2012;17(1):59–70. doi: 10.1111/j.1365-3156.2011.02893.x. [DOI] [PubMed] [Google Scholar]
- 9. Dinh TH, Delaney KP, Goga A, Jackson D, Lombard C, Woldesenbet S, et al. Impact of Maternal HIV Seroconversion during Pregnancy on Early Mother to Child Transmission of HIV (MTCT) Measured at 4–8 Weeks Postpartum in South Africa 2011–2012: A National Population-Based Evaluation. PLoS One. 2015;10(5):e0125525. doi: 10.1371/journal.pone.0125525. A prospective study in South Africa of 9802 mother-infant pairs with infants aged 4–8 weeks from 578 health facilities reported a nationally weighted estimate of 3.3% of HIV-seroconversion during pregnancy (95% CI 2.8–3.8%). Median time of seroconversion was 32.8 weeks gestation. Early MTCT was 10.7% for HIV-seroconversion during pregnancy (6.2%-16.8%) vs. 2.2% (1.7%-2.8%) for mothers with known HIV-positive status. THis study shows that HIV-seroconversion during pregnancy contributes significantly to early MTCT.
- 10.Drake AL, Wagner A, Richardson B, John-Stewart G. Incident HIV during pregnancy and postpartum and risk of mother-to-child HIV transmission: a systematic review and meta-analysis. PLoS Med. 2014;11(2):e1001608. doi: 10.1371/journal.pmed.1001608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moodley D, Esterhuizen T, Reddy L, Moodley P, Singh B, Ngaleka L, et al. Incident HIV infection in pregnant and lactating women and its effect on mother-to-child transmission in South Africa. J Infect Dis. 2011;203(9):1231–1234. doi: 10.1093/infdis/jir017. [DOI] [PubMed] [Google Scholar]
- 12.Birkhead GS, Pulver WP, Warren BL, Hackel S, Rodriguez D, Smith L. Acquiring human immunodeficiency virus during pregnancy and mother-to-child transmission in New York: 2002–2006. Obstetrics and gynecology. 2010;115(6):1247–1255. doi: 10.1097/AOG.0b013e3181e00955. [DOI] [PubMed] [Google Scholar]
- 13. Townsend CL, Byrne L, Cortina-Borja M, Thorne C, de Ruiter A, Lyall H, et al. Earlier initiation of ART and further decline in mother-to-child HIV transmission rates, 2000–2011. AIDS. 2014;28(7):1049–1057. doi: 10.1097/QAD.0000000000000212. A study conducted in the UK and Ireland using population-based surveillance data showing that the rate of MTCT declined from 2.1% in 2000–2001 to 0.46% in 2010–2011, which was primarily attributable to earlier ART initiation during pregnancy.
- 14.Read PJ, Mandalia S, Khan P, Harrisson U, Naftalin C, Gilleece Y, et al. When should HAART be initiated in pregnancy to achieve an undetectable HIV viral load by delivery? AIDS. 2012;26(9):1095–1103. doi: 10.1097/QAD.0b013e3283536a6c. [DOI] [PubMed] [Google Scholar]
- 15.European Collaborative S. Patel D, Cortina-Borja M, Thorne C, Newell ML. Time to undetectable viral load after highly active antiretroviral therapy initiation among HIV-infected pregnant women. Clin Infect Dis. 2007;44(12):1647–1656. doi: 10.1086/518284. [DOI] [PubMed] [Google Scholar]
- 16. Myer L, Phillips T, Manuelli V, McIntyre J, Bekker LG, Abrams EJ. Evolution of antiretroviral therapy services for HIV-infected pregnant women in Cape Town, South Africa. J Acquir Immune Defic Syndr. 2015 doi: 10.1097/QAI.0000000000000584. A retrospective cohort analysis of sequential cohorts of HIV-infected pregnant women receving PMTCT in South Africa examining the impact of changes in PMTCT models of service delivery on ART uptake. The authors reported that integration of ART into ANC services was associated with decreased time to ART initiation, with 82% of the women starting ART on the day of the first ANC visit.
- 17.Garcia PM, Kalish LA, Pitt J, Minkoff H, Quinn TC, Burchett SK, et al. Maternal levels of plasma human immunodeficiency virus type 1 RNA and the risk of perinatal transmission. Women and Infants Transmission Study Group. N Engl J Med. 1999;341(6):394–402. doi: 10.1056/NEJM199908053410602. [DOI] [PubMed] [Google Scholar]
- 18.Violari A, Cotton MF, Gibb DM, Babiker AG, Steyn J, Madhi SA, et al. Early antiretroviral therapy and mortality among HIV-infected infants. N Engl J Med. 2008;359(21):2233–2244. doi: 10.1056/NEJMoa0800971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Turan JM, Onono M, Steinfeld RL, Shade SB, Owuor K, Washington S, et al. Effects of antenatal care and HIV treatment integration on elements of the PMTCT cascade: Results from the SHAIP cluster-randomized controlled trial in Kenya. J Acquir Immune Defic Syndr. 2015 doi: 10.1097/QAI.0000000000000678. This study compared integrated HIV and ANC care within the ANC setting (6 clinics, 569 women) with non-integrated care in which PMTCT services were provided in the ANC settin but women were referred to HIV care at the HIV clinic within the same facility (6 clinics 603 women) in rural Kenya on PMTCT outcomes. The clinics randomzied to integrated care, as compared to non-integrated care, had higher enrollment in HIV care (OR 3.94, 95% CI 1.14–13.63), shorter median time to enrollment (0 versus 8 days, HR 2.20, 95% CI 1.62–3.01), and a higher proportion of eligible women initiated ART (40% versus 17%, OR 3.22, 95% CI 1.81–5.72). Additionally, infant testing was more common in the integrated clinics (25% versus 18%, not stastically different).
- 20. van Lettow M, Bedell R, Mayuni I, Mateyu G, Landes M, Chan AK, et al. Towards elimination of mother-to-child transmission of HIV: performance of different models of care for initiating lifelong antiretroviral therapy for pregnant women in Malawi (Option B+) J Int AIDS Soc. 2014;17:18994. doi: 10.7448/IAS.17.1.18994. A study of 141 health facilities providing various models of care for Option B+ which illustrates large variation in how Option B+ has been integrated into routine service delivery.
- 21.Psaros C, Remmert JE, Bangsberg DR, Safren SA, Smit JA. Adherence to HIV care after pregnancy among women in sub-Saharan Africa: falling off the cliff of the treatment cascade. Curr HIV/AIDS Rep. 2015;12(1):1–5. doi: 10.1007/s11904-014-0252-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hallett TB, Eaton JW. A side door into care cascade for HIV-infected patients? J Acquir Immune Defic Syndr. 2013;63(Suppl 2):S228–S232. doi: 10.1097/QAI.0b013e318298721b. [DOI] [PubMed] [Google Scholar]
- 23.Ferguson L, Grant AD, Watson-Jones D, Kahawita T, Ong'ech JO, Ross DA. Linking women who test HIV-positive in pregnancy-related services to long-term HIV care and treatment services: a systematic review. Trop Med Int Health. 2012;17(5):564–580. doi: 10.1111/j.1365-3156.2012.02958.x. [DOI] [PubMed] [Google Scholar]
- 24.Stringer EM, Ekouevi DK, Coetzee D, Tih PM, Creek TL, Stinson K, et al. Coverage of nevirapine-based services to prevent mother-to-child HIV transmission in 4 African countries. JAMA. 2010;304(3):293–302. doi: 10.1001/jama.2010.990. [DOI] [PubMed] [Google Scholar]
- 25.Marcos Y, Phelps BR, Bachman G. Community strategies that improve care and retention along the prevention of mother-to-child transmission of HIV cascade: a review. J Int AIDS Soc. 2012;15(Suppl 2):17394. doi: 10.7448/IAS.15.4.17394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Phillips T, McNairy M, Zerbe A, Myer L, Abrams EJ. Postpartum transfer of care among HIV-infected women who initiated antiretroviral therapy during pregnancy: a cohort study. [Manuscript] 2015 doi: 10.1097/QAI.0000000000000771. In press. A prospective cohort study of postpartum HIV-infected women, initiatied on ART during pregnancy under Option A approach, in South Africa reporting 74–91% had successfully transferred their HIV care from an integrated ANC/ART clinic to a general ART clinic.
- 27.Watson-Jones D, Balira R, Ross DA, Weiss HA, Mabey D. Missed opportunities: poor linkage into ongoing care for HIV-positive pregnant women in Mwanza, Tanzania. PLoS One. 2012;7(7):e40091. doi: 10.1371/journal.pone.0040091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rawizza HE, Chang CA, Chaplin B, Ahmed IA, Meloni ST, Oyebode T, et al. Loss to Follow-Up within the Prevention of Mother-to-Child Transmission Care Cascade in a Large ART Program in Nigeria. Curr HIV Res. 2015;13(3):201–209. doi: 10.2174/1570162x1303150506183256. This retrospective cohort study reports PMTCT outcomes among 31,504 women who received PMTCT services in 31 clinical sites in Nigeria from 2004 to 2014. A total of 66% of women completed the entire cascade of services. The largest loss of women (21%) in the cascade occurred prior to delivery. A further loss of 16% of women occurred prior to the first infant visit. Among the 20,202 (53%) infants with available HIV DNA PCR results, the rate of HIV transmission for infants whose mothers received any antental and/or delivery care was 2.8% versus 20.0% if their mothers received none.
- 29. Kim MH, Ahmed S, Hosseinipour MC, Giordano TP, Chiao EY, Yu X, et al. Implementation and operational research: the impact of option B+ on the antenatal PMTCT cascade in Lilongwe, Malawi. J Acquir Immune Defic Syndr. 2015;68(5):e77–e83. doi: 10.1097/QAI.0000000000000517. A pre-post study comparing acheivement of steps in the PMTCT care cascade before and after adoption of Option B+ in Malawi. Enrollment of HIV-infected women into a PMTCT program and retention of women through delivery were higher after implementation of Option B+, as was time to ART initiation.
- 30.WHO, UNICEF, UNFPA, The World Bank, United Nations Population Division. Trends in Maternal Morality: 1990 to 2013. Geneva: 2014. [Google Scholar]
- 31.Black V, Brooke S, Chersich MF. Effect of human immunodeficiency virus treatment on maternal mortality at a tertiary center in South Africa: a 5-year audit. Obstetrics and gynecology. 2009;114(2 Pt 1):292–299. doi: 10.1097/AOG.0b013e3181af33e6. [DOI] [PubMed] [Google Scholar]
- 32.Kuhn L, Aldrovandi GM, Sinkala M, Kankasa C, Semrau K, Mwiya M, et al. Effects of early, abrupt weaning on HIV-free survival of children in Zambia. N Engl J Med. 2008;359(2):130–141. doi: 10.1056/NEJMoa073788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taha TE, Li Q, Hoover DR, Mipando L, Nkanaunena K, Thigpen MC, et al. Postexposure prophylaxis of breastfeeding HIV-exposed infants with antiretroviral drugs to age 14 weeks: updated efficacy results of the PEPI-Malawi trial. J Acquir Immune Defic Syndr. 2011;57(4):319–325. doi: 10.1097/QAI.0b013e318217877a. [DOI] [PubMed] [Google Scholar]
- 34.McNairy ML, El-Sadr WM. The HIV care continuum: no partial credit given. AIDS. 2012;26(14):1735–1738. doi: 10.1097/QAD.0b013e328355d67b. [DOI] [PubMed] [Google Scholar]
- 35.Nolan T, Berwick DM. All-or-none measurement raises the bar on performance. JAMA. 2006;295(10):1168–1170. doi: 10.1001/jama.295.10.1168. [DOI] [PubMed] [Google Scholar]
- 36.UNAIDS. Countdown to Zero: global plan towards the elimination of new HIV infections among children by 2015 and keeping their mothers alive, 2011–2015. Geneva: UNAIDS; 2011. p. 48. [Google Scholar]
- 37.UNAIDS. 90-90-90 An Ambitious treatment target to help end the AIDS epidemic. Geneva: UNAIDS; 2014. http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf. [Google Scholar]


