Abstract
The treatment of renal cell carcinoma (RCC) has changed greatly over the past 15 years. Progress in the surgical management of the primary tumor and increased understanding of the molecular biology and genomics of the disease have led to the development of new therapeutic agents. The management of the primary tumor has changed owing to the realization that clean margins around the primary lesion are sufficient to prevent local recurrence, as well as the development of more sophisticated tools and techniques that increase the safety of partial nephrectomy. The management of advanced disease has altered even more dramatically as a result of new agents that target the tumor vasculature or that attenuate the activation of intracellular oncogenic pathways. This review summarizes data from prospective randomized phase III studies on the surgical management and systemic treatment of RCC, and provides an up to date summary of the histology, genomics, staging, and prognosis of RCC. It describes the management of the primary tumor and offers an overview of systemic agents that form the mainstay of treatment for advanced disease. The review concludes with an introduction to the exciting new class of immunomodulatory agents that are currently in clinical trials and may form the basis of a new therapeutic approach for patients with advanced RCC.
Sources and selection criteria
We searched PubMed from 1995 to 2014 using the keywords “renal cell carcinoma”, “RCC”, “histology”, “partial nephrectomy”, “sorafenib”, “sunitinib”, “pazopanib”, “bevacizumab”, “axitinib”, “temsirolimus”, and “everolimus”. References were prioritized to include prospective randomized phase III trials, followed by prospective randomized phase II trials. Selected retrospective peer reviewed studies were included if no prospective data were available on the topic. Material from abstracts was not included.
Introduction
The investigation and management of renal cell carcinoma (RCC) has undergone an unprecedented period of change. This is largely due to advances in genomics and biological discoveries that can be successfully targeted to benefit patients. Pivotal to these advances was the recognition of mutations of the von Hippel-Lindau gene, and resultant stabilization of the hypoxia response pathway as a major driver of clear cell type RCC.1 2 Numerous new therapies are emerging or available based on this discovery, and new concepts regarding disease management to avoid overtreatment or toxicity are being considered. The pace of new findings continues unabated, making regular, comprehensive updates essential both to stay current with the evolving literature and standards, and to be poised and ready to adapt to the coming changes as this field continues to advance.
Incidence and prevalence
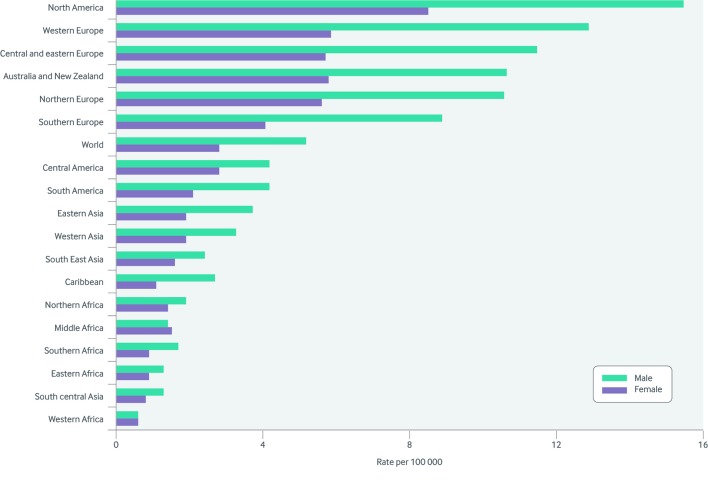
Worldwide, RCC is the ninth most common cancer, with about 337 860 new cases diagnosed in 2012.3 In 2013, cancers of the kidney and renal pelvis were estimated to occur in 65 150 patients in the United States, resulting in 13 680 deaths.4 In the World Health Organization Europe region, an estimated 121 629 new cases of RCC occurred in 2012, of which 75 676 affected men. The incidence of RCC varies geographically (figs 1 and 2), with the highest incidence in developed countries.5 The reason for the higher incidence in developed countries and in men is not clear. Genomic, occupational, and other environmental exposures such as smoking have been implicated. With the increased use of abdominal imaging for screening and diagnostic purpose, incidental renal masses and RCCs are being discovered more often. In a recent review of 3001 patients without symptoms being imaged for computed tomography colonography, 14% of patients harbored a renal mass greater than 1 cm in size.6
Fig 1 Incidence of renal cell carcinoma in different geographical regions. Adapted with permission from Cancer Research UK5
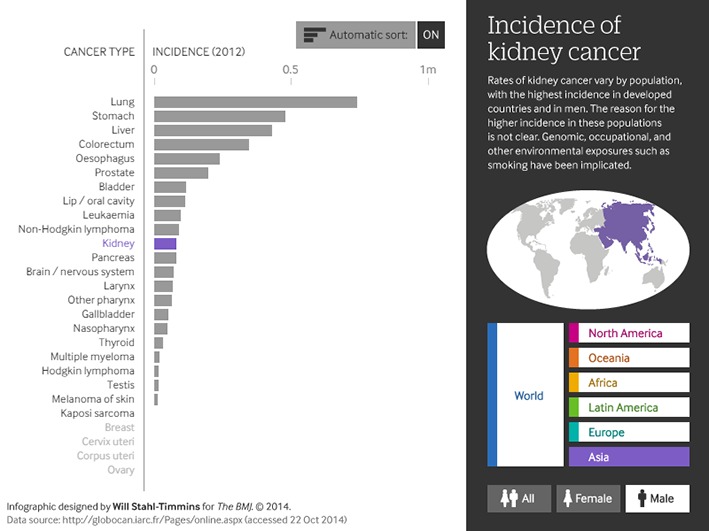
Fig 2 Which continent has the highest incidence of kidney cancer? Use our interactive tool to find out how cancer incidence varies by population. See www.bmj.com/content/349/bmj.g4797/infographic
Classification of RCC
In the past decade it has become clear that not all RCCs are related. It is no longer appropriate to lump these diseases together in clinical trials or in the consciousness of practising oncologists and urologists. This section will briefly define the diseases that fall under this umbrella and the implications for surgical and medical management. It will also provide a brief overview of their genetic features.
RCC and other diseases arising in the kidney
We deliberately avoid the term “subtype,” which refers to a subordinate grouping within a general classification. Rather, we will refer to these cancers as the independent entities that they are.7 We will describe clear cell, papillary, and chromophobe renal cell carcinomas and will briefly review several rare cancers that are also found in the kidney (collecting duct carcinoma, renal medullary carcinoma, and urothelial carcinomas). Several benign lesions of the kidney will also be discussed because they may mimic RCC or complicate its management. Detailed descriptions of the histologic diagnosis of these cancers can be found elsewhere,8 along with recently updated grading recommendations.9
Clear cell RCC
These cancers make up about 70% of all cancers of the kidney.10 Histologically, they are defined by clear cytoplasm, with nested clusters of cells surrounded by a dense endothelial network.
Papillary RCC
This is the second most common tumor. Two subtypes of papillary renal cell cancer have been recognized—papillary type 1 and papillary type 2.11 Diagnosis is mostly based on features of papillary architecture. Cells typically display a basophilic cytoplasm, and the presence of foamy histiocytes is characteristic.
Chromophobe RCC
These tumor cells have a largely empty cytoplasm, typically have characteristic perinuclear clearing, and often feature a low mitotic rate.12 In general, these tumors have the lowest risk of developing metastases.
Rare tumors of the nephron and collecting system
Each of these tumor types occurs in less than 5% of cases. Renal cell carcinomas are thought to be derived from the tubules, with regional variance in the site of origin. However, tumors also arise from the cells and tissues that make up the renal medulla and collecting system. These tumors—collecting duct carcinoma, renal medullary carcinoma, and urothelial carcinoma—are highly distinct disease entities that bear little resemblance to RCCs. No strict standards of care exist for their management.
Premalignant and benign lesions arising in the kidney
Finally, various non-neoplastic conditions in the kidney give rise to masses that can share radiographic findings with renal cancers. These include angiomyolipomas—sarcomatous change lesions that can grow to a large size and can cause spontaneous hemorrhage. In addition, oncocytomas, which have low malignant potential, share many cytological and biological features with chromophobe-type renal cell carcinoma and can complicate the diagnosis on biopsy specimens.
Key mutations and genomic features of renal derived carcinomas
Clear cell RCC
This cancer has recently been defined in The Cancer Genome Atlas.13 The genetic feature most closely associated with this cancer is loss or mutation of the von Hippel-Lindau (VHL) tumor suppressor gene. Germline mutations cause the eponymous VHL syndrome.14 VHL mutation or loss is identified in 60-90% of sporadic cases. The loss of this protein results in stabilization of the family of hypoxia inducible factors—protein transcriptional activators of genes that are involved in mediating the hypoxia response. This in turn transactivates genes involved in angiogenesis, cell migration, and metabolism.
In addition to this common genetic event, other events closely associated with RCC include mutations, with loss of heterozygosity, in a large group of chromatin remodeling genes. The most commonly inactivated genes include PBRM1, BAP1, and SETD2, although mutations in a variety of additional histone modifiers (KDM5a, ARID1a, and UTX) are also seen.15 16 17 18
The impact of these mutations on the outcomes and biological properties of these cancers is only now being identified,19 20 21 with recent evidence pointing to an association between SETD2 mutations and changes in chromatin packaging. Finally, mutations in genes associated with mTOR pathway signaling (PIK3CA, PTEN, and MTOR) have also been identified in a substantial proportion of tumors.
Papillary RCC
Much less is known about this tumor type. Two familial syndromes are associated with increased risk of papillary-type renal cell carcinoma. Mutations in the MET proto-oncogene predispose people to multifocal papillary type I RCC.22 In addition, the syndrome of hereditary leiomyomatosis and renal cell carcinoma (HLRCC)—caused by mutations in the fumarate hydratase (FH) gene—carries a risk for familial type II papillary RCC.23
Although sporadic tumors in this disease group often fall into the papillary types I and II histological groups, it is not clear that they carry the same mutations as their hereditary counterparts. The results of large scale genomic profiling studies will be available soon.
Chromophobe RCC
Most of these tumors harbor chromosomal losses, including losses of whole chromosomes 1, 2, 6, 10, 13, 17, and 21,24 although the effect of these massive losses of DNA content remain uncertain. Except for mutations in PTEN, located at 10q23, and TP53, located at 17p13, few other mutations in tumor suppressor genes have been identified in chromophobe RCC. The familial syndrome of chromophobe tumors is linked to Birt-Hogg-Dube syndrome,25 which is caused by germline mutations in the folliculin gene, FLCN.26
Rare tumours
These include unclassified tumors, which may be misclassified cases of the RCC subtypes described above, as well as collecting duct carcinoma, urothelial tumors (a variant of transitional cell carcinoma), and renal medullary carcinoma. Renal medullary carcinoma is found exclusively in patients with a hemoglobinopathy, most commonly sickle cell trait, and is characterized by loss of expression of the chromatin regulatory gene SNF5/INI-1.27 Very little information has been isolated from the genome to enable a better understanding of the pathophysiology of these tumors.
Staging and prognosis of RCC
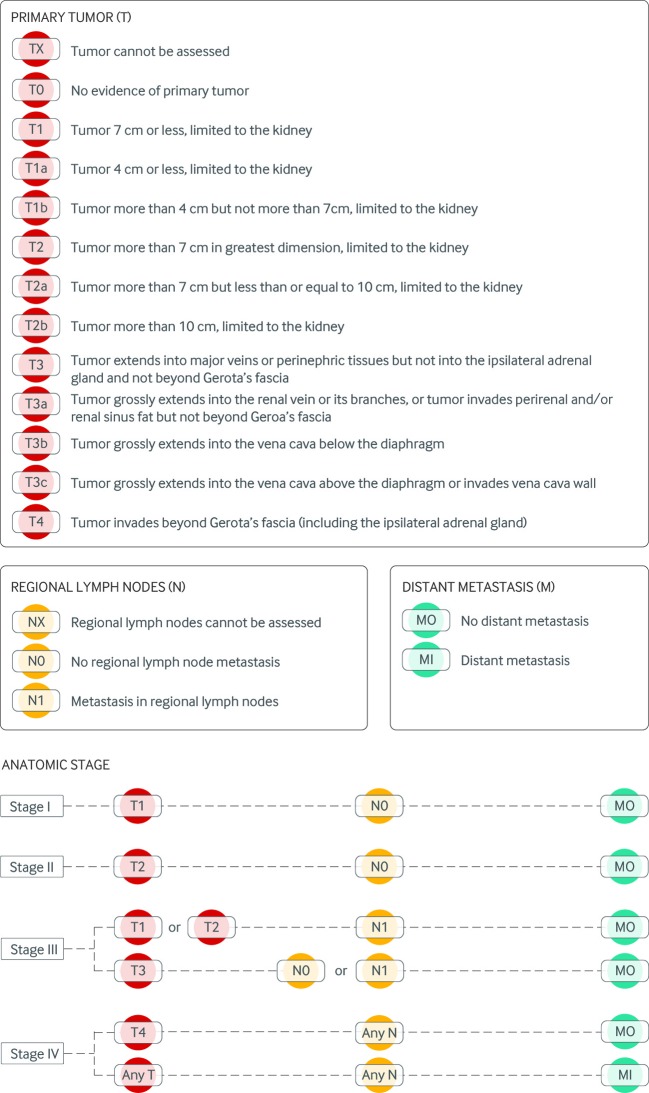
The most commonly used staging system for RCC is the American Joint Committee on Cancer (AJCC) tumor node metastasis (TNM) system (fig 3). This system was last revised in 2010 and contains three components: T indicates the size of the primary tumor and extent of invasion; N describes the status of metastasis to regional lymph nodes; and M indicates whether there is distant metastasis.28 Numbers or letters appearing after T, N, and M subcategorize the size of the tumor or extent of disease.
Fig 3 Tumor node metastasis (TNM) staging for renal cell carcinoma (2010 version)
TNM information is combined to assign an overall anatomic stage of I-IV, which correlates with prognosis. Patients with stage I RCC have a five year disease specific survival of about 80-95%; patients with stage II RCC have a five year disease specific survival of around 80%.29 In patients with stages I-II RCC, tumor invasion of the urinary collecting system is associated with significantly worse prognosis—five year survival is only about 60% compared with over 90% in those without invasion.30 For patients with stage III RCC, five year survival is about 60%.29 During the cytokine era, from the late 1980s to 2006, patients with stage IV RCC had a five year disease specific survival of less than 10%, with a median overall survival of 10-15 months.31 32 33 However, with the development of targeted agents, the median overall survival in patients with stage IV RCC has been extended beyond two years.34
Management of localized disease
About three quarters of people with RCC present with localized disease, and definitive local treatment remains the gold standard for managing patients with no evidence of distant metastasis.35 The incidence of small (<4 cm) renal masses has risen and the question of how to manage these lesions is now a daily dilemma for urologists.36 This has led to new considerations and conversations about management strategies that incorporate biopsy or surveillance of lower risk lesions.37 38 39
Nephrectomy (partial v radical) and laparoscopy
Partial or radical nephrectomy remains the gold standard for the management of renal masses. The selection of tumors for partial nephrectomy has long been dictated by the anatomic location of the tumor, tumor stage, or other features that limit the potential for a complete tumor resection. Randomized clinical trials have examined the potential for nephron sparing approaches to preserve kidney function and reduce the long term morbidity associated with having a solitary kidney.40 In the final analysis of these results, the intention to treat analysis showed 10 year overall survival of 81.1% for radical nephrectomy and 75.7% for nephron sparing surgery. With a hazard ratio of 1.50 (95% confidence interval 1.03 to 2.16), the test for non-inferiority was not significant (P=0.77) but the test for superiority was significant (P=0.03), favoring radical nephrectomy. However, in patients with RCC who met all of the histopathological and clinical eligibility criteria, the difference was less pronounced (hazard ratio 1.43 and 1.34, respectively) and the superiority test was no longer significant (P=0.07 and P=0.17, respectively). Only 12 of 117 deaths were the result of RCC (four radical nephrectomy and eight partial nephrectomy), and 21 patients progressed (nine after radical nephrectomy and 12 after nephron sparing surgery.41 Results favored partial nephrectomy for preservation of renal function.42 Therefore, recently published guidelines recommend partial nephrectomy, when anatomically feasible, or radical nephrectomy when appropriate.35
Laparoscopic procedures have emerged because they provide improved postoperative recovery for patients and greater surgical operative field visibility for surgeons. Various studies have compared standard laparoscopy with robotic laparoscopy and have shown that laparoscopic partial nephrectomy is associated with an increased rate of conversion to radical nephrectomy when compared with robotic techniques (11.5% v 1%; P<0.001) and a greater decrease in estimated glomerular filtration rate (−16.0% v − 12.6%; P=0.03). No significant differences were seen with respect to warm ischemia time, estimated blood loss, transfusion rate, or postoperative complication.43 Cost comparison models currently favor the non-robotic standard laparoscopic approach.44
Ablative approaches
Ablative therapies have seen an increase in use and acceptance for a variety of reasons. A comprehensive review of each technology is not possible and can be found elsewhere.45 46 47 48 49 50 51 Renal masses can be managed with definitive radiofrequency ablation, including new microwave ablation, cryoablation, and stereotactic radiation. The effect on the tumor is unclear because evidence of viable tumor cells has been found on post-ablation histological examination, even when radiographically the tumor appears to be fully ablated. No randomized studies have compared ablative therapies with nephrectomy or directly compared the ablative options themselves. However, owing to the limited invasiveness of ablative techniques, they have an important role in managing small renal masses in patients whose comorbidities or other factors preclude surgical intervention.
The controversy of mandatory node dissection
In most other cancers, it is standard practice to assess local lymph nodes for evidence of disease spread, with sentinel lymph node analysis or extensive nodal dissection being essential for accurate staging of disease. However, although draining nodes in the retroperitoneum are commonly affected in advanced stages of disease, the routine collection of clinically uninvolved nodes is not standard practice across leading institutions. The European Organisation for Research and Treatment of Cancer (EORTC) investigated this in a randomized phase III trial, which found cancer in about 4% of resected nodes, and no difference in morbidity or long term outcomes with lymph node resection.52 53 54 Patients must continue to be considered on a case by case basis, and the resection of apparently involved nodes remains an important part of the care of patients with resectable locally advanced disease.
Risk factors for progression
Several clinical algorithms have been evaluated and validated for predicting the risk of developing recurrence after definitive local treatment. One of the first is the still widely used Leibovich prognostic score, which incorporates tumor size, stage, grade, histologic necrosis, and regional lymph node status in an algorithm designed to assess risk for developing metastatic disease.55 Other models include the Mayo clinic stage, size, grade, and necrosis (SSiGN) model56 57; the University of California, Los Angeles integrated staging system (UISS), which quantifies stage, tumor grade, and performance status58 59; and other preoperative clinical risk algorithms.60 61 A recent review of algorithms compared these tools.62
Although many biological and genetic features of renal cell carcinoma have recently been identified, none has yet been prospectively validated as risk factors. As our knowledge about these gene mutations, gene expression patterns, and protein expression patterns develops, it will be essential to integrate them into currently used clinical algorithms.
Adjuvant therapy
Unfortunately, no adjuvant therapies have been proved to have a significant benefit in RCC. Randomized trials of cytokine immunotherapies showed no benefit.63 64 65 Several adjuvant studies examining the emerging classes of vascular endothelial growth factor (VEGF) receptor and mTOR inhibitor therapies are under way or have completed accrual, and results will be available soon (NCT01120249; NCT00326898; NCT00492258; NCT00375674; NCT01235962).
Similarly, neoadjuvant therapy has not been rigorously examined in prospective studies. Several smaller studies of agents that target the VEGF pathway have consistently shown a modest response in the primary tumor, and that these agents do not, in general, increase perioperative surgical morbidity compared with surgery without neoadjuvant therapy.66 67 68 69 A significantly increased risk of wound complications was seen with bevacizumab, probably because of its long half life.66 Preoperative therapy is currently used to shrink borderline or unresectable tumors when it is a safe option for patients with biopsy confirmed clear cell histology. Effects on the risk of recurrence or other outcomes are not known.
Management of metastatic disease
The treatment of metastatic RCC has changed greatly over the past 15 years. Established practice is to perform cytoreductive nephrectomy before starting systemic drugs in most patients.70 71 72 This is followed by treatment with a chosen combination of eight US Food and Drug Administration approved agents, which include immunotherapeutic drugs, antiangiogenic agents, and mTOR inhibitors. Data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program point to an increase in overall survival for patients with metastatic RCC who were diagnosed after 2005.70 Median survival among patients receiving cytoreductive nephrectomy increased with the introduction of targeted therapy (19 v 13 months), while median survival among patients not receiving cytoreductive nephrectomy increased only slightly (4 v 3 months).70 Nevertheless, even with treatment, in most people the disease progresses and is the cause of their death. Better treatments are clearly needed.
Cytoreductive nephrectomy
In the US, about 17% of patients diagnosed with de novo RCC present with metastatic disease.4 Two randomized phase III studies published in 2001 showed an improvement in survival for patients with metastatic RCC who underwent cytoreductive nephrectomy before treatment with interferon alfa.71 72 A review of SEER data showed that the proportion of patients who underwent cytoreductive nephrectomy gradually increased from 1993 to 2004, from 29% to 39%, then dropped slightly to 34% in 2010.70 A prospective randomized study assessing the effect of cytoreductive nephrectomy in patients treated with sunitinib was still accruing patients at the time of writing (NCT00930033).
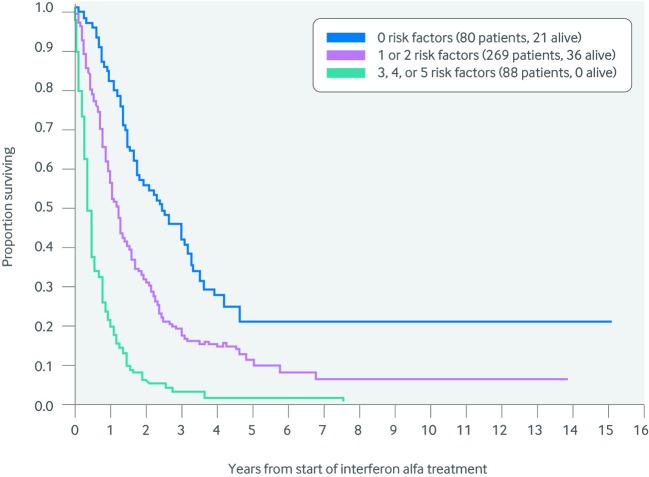
Prognostic algorithms for patients with metastatic disease
A retrospective analysis at the Memorial Sloan Kettering Cancer Center (MSKCC) assessed 670 patients with metastatic RCC who received immunotherapy. A prognostic algorithm was then developed by performing a multivariable analysis of a series of clinical and laboratory parameters.73 Five independent adverse features were ultimately included in the algorithm (fig 4):
Fig 4 Memorial Sloan Kettering risk criteria. The algorithm includes five factors: hemoglobin below the lower limit of normal, Karnofsky performance status of less than 80, less than one year from diagnosis to start of systemic therapy, corrected calcium above the upper limit of normal, and lactate dehydrogenase more than 1.5 times the upper limit of normal. Patients with a good risk have no risk factors; intermediate risk patients have one or two; and poor risk patients have three or more factors73
Karnofsky performance status of less than or equal to two
Less than one year between diagnosis and first systemic treatment
Hypercalcemia
Anemia
Lactate dehydrogenase more than one and a half times the upper limit of normal.
Patients with none of the five negative features had a median survival of 30 months, whereas those with three or more had a median survival of 4.8 months. A few years later, a similar analysis was performed on 645 patients who subsequently received molecularly targeted therapy, and a six component algorithm was derived.74 As in the MSKCC algorithm, it contained performance status, anemia, hypercalcemia and time from diagnosis to treatment, but instead of lactate dehydrogenase it included thrombocytosis and leucocytosis. This algorithm also separated patients into prognostically distinct categories.
Currently available systemic drugs
Three major categories of systemic drugs are currently being used to treat metastatic RCC: cytokines, drugs that target the VEGF pathway, and mTOR inhibitors.
Cytokines
High dose interleukin 2 (IL-2) was approved by the FDA in 1992. Approval was based on a series of phase II studies describing the outcome of 250 patients treated with 600 000-720 000 IU per kg given intravenously every eight hours for a maximum of 14 doses per cycle.75 Patients showed an overall response rate (sum of partial and complete response rates) of 15% and a complete response rate of 5%. Most complete responses achieved with high dose IL-2 were durable, which provided the main impetus for FDA approval. Because of the rigors of receiving high dose IL-2, the patient population was highly selected—patients had excellent performance status, robust lung and cardiac function, and an age of less than 70 years. Two prospective randomized phase III studies published in 2003 and 2005 confirmed the complete response rate, but also found a 1% death rate from treatment related toxicity.76 77 The first randomized trial found a higher response rate and complete response rate with high dose IL-2 (21% and 7%) than with low dose IL-2 (13% (P=0.048) and 4%), but no difference in overall survival, probably because the trial was not powered to assess the subset of the study population with a complete response.76
Similarly, in the second randomized trial,77 the response rate was 23.2% for high dose IL-2 versus 9.9% for subcutaneous IL-2 plus interferon (P=0.018). No difference in overall survival was seen between arms. Efforts to identify predictive biomarkers for response to high dose IL-2 have so far been unsuccessful, and no published prospective reports provide guidance on how to select patients who may benefit from this treatment.
Interferon alfa was the mainstay of treatment for patients with metastatic RCC until the advent of targeted therapies, with two randomized prospective phase III studies showing a modest survival advantage for patients who received interferon compared with placebo.78 79 Interferon was clearly inferior to most of the newer agents in terms of progression-free survival (PFS) measures and was poorly tolerated. This led to interferon being phased out as a treatment for patients with metastatic RCC except in combination with bevacizumab.
Drugs that target the VEGF pathway
The discovery of the VHL mutation in patients with VHL disease,1 followed by the finding that somatic VHL mutations occur in most sporadic clear cell RCCs,80 led to the development of agents that target circulating VEGF and VEGF receptors.
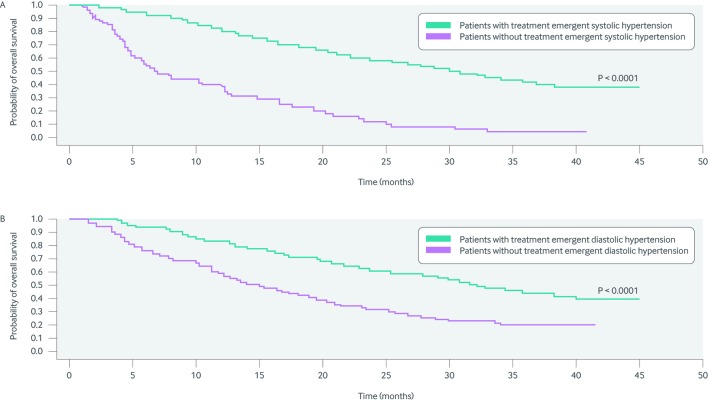
Five agents have been approved by the FDA for the treatment of metastatic RCC,81 82 83 84 85 86 including the intravenously administered VEGF inactivating antibody bevacizumab, and the orally bioavailable small molecule VEGF receptor inhibitors sorafenib, sunitinib, pazopanib, and axitinib. These agents vary in the number of addition tyrosine kinases that they target and the avidity with which they bind and inactivate the VEGF receptor (fig 5).87 These agents are thought to target the tumor endothelium and to have minimal effect on the tumor cells.88 A striking finding in patients treated with these agents is the association between treatment emergent or antecedent hypertension and improved patient survival.89 Figure 6 summarizes the differences in overall survival in patients who experienced treatment emergent hypertension versus those who did not. The biological drivers of this phenomenon have not been elucidated, but the findings raised important questions about the value of dose intensity for agents that target the VEGF pathway. As described in the axitinib section below, recent data suggest that increasing the dose beyond a certain threshold improves overall response rate but not PFS, and neither does it result in a higher complete response rate.90
Fig 5 Kinome profile for axitinib, pazopanib, sunitinib, and sorafenib. The branches represent the known human kinases. Red circles represent targets for the various agents and the size of the circle indicates the inhibitory potency of the kinase (circle sizes are inversely proportional to fold selectivity ratios). Axitinib is an example of a highly specific kinase inhibitor, whereas sunitinib has a considerably broader range of action. Darker red dots provide contrast where overlapping dots are present. Adapted, with permission, from McTigue and colleagues87
Fig 6 Overall survival in patients who developed (A) treatment emergent systolic hypertension (>140 mm Hg) and (B) treatment emergent diastolic hypertension while receiving sunitinib. Those who developed hypertension had significantly better overall survival than those who did not. Adapted, with permission, from Rini et al91
The table provides an overview of the major prospective clinical trials that have defined current practice in the treatment of metastatic RCC. Sorafenib increased PFS to 5.5 months versus 2.8 months for placebo in a prospective, phase III study of patients who were previously treated with cytokines.81 Sorafenib was FDA approved for the treatment of advanced RCC in December 2005. Unfortunately, when tested in a phase II randomized study, PFS was 5.7 months for sorafenib compared with 5.6 months for interferon.92 Sorafenib has therefore been relegated to second and subsequent lines of treatment for most patients.
Studies of molecularly targeted agents for renal cell carcinoma*
| Drug | Previous treatment | Comparator | Study size | Primary endpoint | PFS (months)† | Met primary endpoint? |
|---|---|---|---|---|---|---|
| Sorafenib83 | Cytokines | Placebo | 903 | PFS | 5.5/2.8 | Yes |
| Sorafenib92 | None | Interferon | 189 | PFS‡ | 5.7/5.6 | No |
| Sunitinib86 | None | Interferon | 750 | PFS | 11.0/5.0 | Yes |
| Pazopanib87 | Cytokines or none | Placebo | 415 | PFS | 9.2/4.2 | Yes |
| Pazopanib93 | None | Sunitinib | 1110 | PFS§ | 8.4/9.5 | Yes |
| Axitinib88 | TKIs or cytokines | Sorafenib | 723 | PFS | 6.7/4.7 | Yes |
| Axitinib94 | None | Sorafenib | 288 | PFS | 10.1/6.5 | No |
| Bevacizumab and interferon95 | None | Interferon | 732 | PFS | 8.5/5.2 | Yes |
| Bevacizumab and interferon84 | None | Interferon + placebo | 649 | PFS | 10.2/5.4 | Yes |
| Temsirolimus96 | None; poor risk patients | Interferon | 626 | OS | 10.9/7.3 | Yes |
| Temsirolimus97 | Sunitinib | Sorafenib | 512 | PFS | 4.2/3.9 | No |
| Everolimus85 | Sorafenib or sunitinib | Placebo | 410 | PFS | 4.0/1.9 | Yes |
*OS=overall survival; PFS=progression-free survival; TKI=tyrosine kinase inhibitor.
†Treatment/comparator.
‡Randomized phase II trial.
§Non-inferiority design.
Sunitinib was approved by the FDA in January 2006 for the treatment of advanced RCC on the basis of a trial of 750 patients who were randomized to sunitinib or interferon. PFS was 11.0 months in patients treated with sunitinib versus 5.0 months in those treated with interferon (hazard ratio 0.42, 0.32 to 0.54; P<0.001).84 Sunitinib is currently a commonly used first line treatment for metastatic RCC. A recent retrospective review of an alternate two week on/one week off schedule versus the standard four week on/two weeks off schedule suggested that the alternate schedule improved tolerability.98
Pazopanib was approved by the FDA in October 2009 for the treatment of advanced RCC on the basis of a prospective phase III study that randomized 415 patients with metastatic RCC to pazopanib or placebo. Patients included those who were pretreated with cytokine and those who were not.85 PFS was 9.2 months for pazopanib treated patients versus 4.2 months for the placebo group (0.46, 0.34 to 0.62; P<0.0001). In the treatment naive subgroup, PFS was 11.1 months for patients who received pazopanib versus 2.8 months for the placebo group (0.40, 0.27 to 0.60; P<0.0001).
A subsequent trial of 1110 patients compared pazopanib with sunitinib as first line drugs, using a non-inferiority statistical design.93 Pazopanib was non-inferior to sunitinib (1.05, 0.90 to 1.22). Median PFS was 8.4 months with pazopanib (8.3 to 10.9) and 9.5 months with sunitinib (8.3 to 11.1), and 11 of 14 quality of life measures favored pazopanib over sunitinib.
Axitinib was approved by the FDA in January 2012 for patients with treatment refractory RCC. Approval was based on a prospective phase III study that randomized 723 previously treated patients with metastatic RCC to axitinib or sorafenib.86 Overall PFS for axitinib was 6.7 months versus 4.7 months for sorafenib (0.665, 0.544 to 0.812; one sided P<0.0001). PFS for patients who progressed on sunitinib was 4.8 months for axitinib treated patients and 3.4 months for sorafenib treated patients (0.741, 0.573.4; one sided P=0.0107.
Subsequently, a prospective randomized phase II study with 202 patients tested the hypothesis that axitinib dose escalation would improve outcomes in treatment naive patients.99 The study concluded that dose escalation improved the overall response rate but did not alter PFS. To formally test the efficacy of axitinib as a first line drug, a phase III study randomized 192 previously untreated patients with metastatic RCC to receive axitinib and 96 patients to receive sorafenib.94 PFS for axitinib was 10.1 months (7.2 to 12.1) versus 6.5 months (4.7 to 8.3) for sorafenib, with a stratified hazard ratio of 0.77 (0.56 to 1.05). This study failed to demonstrate the superiority of axitinib over sorafenib because of the unexpected performance of sorafenib, and because the study had an inadequate sample size.
The combination of bevacizumab plus interferon was approved by the FDA in 2009 on the basis of two prospective randomized phase III trials.82 95 In both studies this combination showed a superior PFS when compared with interferon monotherapy or interferon plus placebo. In the first study (732 patients), median PFS was 8.5 months in patients receiving bevacizumab plus interferon (7.5 to 9.7) versus 5.2 months (3.1 to 5.6) in those receiving interferon monotherapy (log rank P<0.0001). The adjusted hazard ratio was 0.71 (0.61 to 0.83; P<0.0001). In the second study, 649 patients with treatment naive metastatic RCC were randomized to bevacizumab plus interferon or placebo plus interferon. Median PFS was significantly longer in the bevacizumab plus interferon group than in the control group (10.2 v 5.4 months; hazard ratio 0.63, 0.52 to 0.75; P=0.0001). No phase III prospective studies to test the efficacy of bevacizumab monotherapy have been published or are planned.
Although PFS endpoints were met in many of these studies, overall survival was not significantly longer in the experimental arms of any of them.100 101 102 103 104 This has been explained by the fact that crossover to an experimental arm or to an equivalent agent was possible in many of the patients. Where crossover was not possible and no second line drug was available, a clear survival advantage was reported in patients treated with sunitinib compared with those who received interferon.100
mTOR inhibitors
The second major class of molecularly targeted agents used to treat metastatic RCC targets mTOR, a serine-threonine protein kinase within the family of phosphatidylinositol-3 kinase (PI3K) related kinases. Mutations in the PI3K pathway upstream of mTOR and in mTOR itself occur in RCC,105 suggesting that this pathway is important for renal carcinogenesis. Both agents bind to the prolyl isomerase FKBP12, and this complex in turn inhibits mTOR activity.
Temsirolimus was approved by the FDA for the treatment of advanced RCC in 2007, on the basis of a prospective phase III study that randomized 626 patients with metastatic RCC and at least three poor risk features (the five MSKCC factors plus metastasis in more than one organ) to temsirolimus, an attenuated dose of temsirolimus plus interferon, or interferon monotherapy.96 These patients were different from those in previously described studies in that 20% of patients had non-clear cell histology, and only two thirds had undergone cytoreductive nephrectomy. This trial also used overall survival as a primary endpoint. Overall survival for patients treated with temsirolimus was 10.9 months versus 7.3 months for the interferon monotherapy arm (0.73, 0.58 to 0.92; P=0.008). Temsirolimus is currently used mainly in poor risk patients as a first line drug.
In a recent study that tested the utility of temsirolimus in patients who had not responded to sunitinib,97 512 patients were randomized between temsirolimus and sorafenib, with a primary PFS endpoint. No significant difference was seen for PFS (stratified hazard ratio 0.87, 0.71 to 1.07; two sided P=0.19) or overall response rate. Median PFS was 4.3 and 3.9 months in the temsirolimus and sorafenib arms, respectively. Surprisingly, overall survival was significantly longer in the sorafenib treated group than in the temsirolimus treated group (16.6 v 12.3 months; 1.31, 1.05 to 1.63; two sided P=0.01). Reasons for this difference were not immediately apparent, but this result dampened enthusiasm for temsirolimus as a treatment for patients who do not respond to VEGF receptor inhibitors.
Everolimus was approved by the FDA in 2009 for the treatment of patients who progressed on sorafenib, sunitinib, or both. The approval was based on a phase III study that randomized 410 patients who had previously not responded to antiangiogenic therapy to everolimus or placebo.83 PFS was 4.0 months for everolimus treated patients versus 1.9 months for the placebo group (0.30, 0.22 to 0.40; P<0.0001). Everolimus is commonly used as a second line or third line drug. Currently, no data support the use of everolimus as a first line drug.
Emerging treatments and concepts in RCC
Immune checkpoint blocking agents
Recently, monoclonal antibodies against immune checkpoint blockade molecules including CTLA-4 (cytotoxic T lymphocyte antigen 4) and PD-1 (programmed cell death 1) have been shown to have clinical activity against several cancers, including RCC. For T cells to be activated for tumor cell killing, two sets of stimulating signals must be present. The first activating signal is provided by interaction between the T cell receptor and antigen bound to the major histocompatibility complex (MHC). The second signal is mediated by interaction between a T cell costimulatory molecule CD28 and its ligands, the B7 proteins.106
CTLA-4 is expressed by activated CD4 and CD8 T cells. It is a homolog of the T cell costimulator CD28 but has a higher binding affinity for CD28 ligands. Upon T cell activation, signaling pathways lead to production of CTLA-4, which is then mobilized from intracellular vesicles to the cell surface, where it outcompetes CD28 for binding to B7 proteins. Binding of CTLA-4 to B7 proteins interrupts CD28 costimulatory signals and thereby limits T cell responses.106 107
Owing to the negative regulatory effects of CTLA-4 on T cell responses, it was hypothesized that blockade of CTLA-4 signaling would potentiate immune responses against tumor cells. The first antibody to block CTLA-4 (ipilimumab) was tested for the treatment of metastatic RCC in the phase II clinical trial MDX010-11 but showed only modest activity.108
Similar to CTLA-4, PD-1 also negatively regulates T cells. It exerts this effect by binding to two ligands, PD-L1 and PD-L2, which are expressed on several cells, including antigen presenting cells and tumor cells. A recent phase I clinical trial with an anti-PD1 antibody (BMS-936558) showed an 18-28% objective response rate in patients with advanced non-small cell lung cancer, RCC, and melanoma.109 Among patients with metastatic RCC in this trial, there was a 27% clinical response rate, with most responses lasting more than a year.
Another almost concurrent phase I trial with an anti-PD-L1 antibody found an objective response rate of 6-17% in patients with advanced non-small cell lung cancer, melanoma, and RCC.110 Among patients with metastatic RCC in this trial, there was a 12% response rate, and 41% of patients whose disease stabilized remained stable for at least six months.
A phase III clinical trial of anti-PD1 in patients with metastatic RCC is ongoing. Combinations of anti-CTLA-4 and agents that target the VEGF pathway are also being investigated. However, despite their promising efficacy, immune checkpoint blocking agents have associated toxicities, known as immune related adverse events, including colitis, hepatitis, and hypopituitarism. Understanding the mechanisms and management of these adverse events will be an important aspect of effective use of these agents.
Other targeted agents
Newer agents that target the VEGF pathway, PI3K pathway, and mTOR pathway are in development. Recently, the FDA rejected a newer VEGF receptor inhibitor, tivozanib, because phase III data showed that it did not significantly improve median overall survival, although it did significantly prolong median PFS, when compared with sorafenib in patients with advanced RCC.111 Cabozantinib, a tyrosine kinase inhibitor of VEGF, the cellular receptor KIT, and MET, was tested in a phase II trial and showed a 28% overall response rate and 52% stable disease rate, with a median PFS of 14.7 months.112 A phase III clinical trial (NCT01865747) is currently evaluating the efficacy of cabozantinib versus everolimus in patients with metastatic RCC whose disease progressed after treatment with at least one tyrosine kinase inhibitor. A phase III clinical trial of dovitinib, an inhibitor of fibroblast growth factor, in addition to a VEGF receptor inhibitor, failed to show a superiority of this combination versus sorafenib in terms of PFS.113
Similarly, several newer PI3K and mTOR inhibitors are also being developed for RCC. Among these, AZD8055 has been reported to have promising activity in preclinical studies,114 and phase I clinical trials are now complete.115 To build on the success of individual PI3K inhibitors and mTOR inhibitors, a dual inhibitor of PI3K and mTOR (NVP-BEZ235) has been developed. Preclinical studies indicated that NVP-BEZ235 had better in vitro antiproliferative effects than rapamycin.116 Currently, NVP-BEZ235 is being tested on RCC in phase I-II clinical trials (NCT01453595).
Genomic heterogeneity and impact on treatment
Owing to its prevalence, clear cell RCC is the most genetically well studied subtype of RCC. A recent analysis of data from the Cancer Genome Atlas (TCGA)—which included comprehensive integrated analyses of somatic alterations as well as analysis of DNA methylation profiles, RNA expression profiles, and protein expression profiles—has illustrated the genomic heterogeneity of clear cell RCC.13
Firstly, these analyses confirmed previously identified major genetic changes that underlie clear cell RCC, including mutations in genes that control cellular oxygen sensing (such as VHL) and the maintenance of chromatin states (such as PBRM1, BAP1, and SETD2), as well as genes in the mTOR pathway (PIK3CA and MTOR).105 In addition, hypermethylation of promoter DNA was associated with higher stages and grades of clear cell RCC.
Furthermore, clear cell RCC can be separated into different prognostic groups on the basis of gene expression, DNA methylation, and protein expression profiles. Aggressive cancers with worse survival show gene expression changes that favor a metabolic shift toward fatty acid synthesis (Warburg-like phenotype). For example, reduced expression of the Krebs cycle gene AMP activated kinase (AMPK) and increased expression of the pentose phosphate pathway gene acetyl-CoA carboxylase (ACC) is associated with worse survival. In addition, decreased methylation of the MIR21 gene promoter correlated with increased expression of the microR-21 gene, which downregulates the tumor suppressor gene PTEN, and is associated with worse survival. By contrast, better survival is associated with decreased methylation of the tumor suppressor gene GRB10 (growth factor receptor bound protein 10) gene promoter and increased expression of the GRB10 protein, which is a negative regulator of PI3K.
Collectively, these data suggest that key genes involved in DNA methylation, chromatin structure, and cellular metabolism may serve not only as potential prognostic markers but also as potential therapeutic targets for clear cell RCC. In addition, these observations define a great deal of genomic variety across tumors. A recent study that examined the intratumoral heterogeneity of clear cell RCC identified substantial differences in mutations from different sites within a single primary tumor, as well as a distinct mutational profile for metastatic lesions. The mutations identified also showed evidence of convergent evolution.117 Further studies will be needed to translate these findings into clinical settings.
Guidelines
European Association of Urology guidance can be found at: www.uroweb.org/gls/pdf/10_Renal_Cell_Carcinoma_LR.pdf
The National Comprehensive Cancer Network provides regularly updated cancer treatment guidelines and maintains a set of guidelines for renal cell carcinoma, which can be accessed at: www.nccn.org/professionals/physician_gls/f_guidelines.asp
Conclusion
RCC is an important and increasing public health threat in the developed world. Substantial progress has been made in the management of localized disease, with nephron sparing approaches emerging in the past 15 years. For patients with metastatic disease, cytoreductive nephrectomy is still considered a reasonable approach in those who subsequently receive contemporary systemic drugs. The most commonly used agents to treat metastatic RCC are drugs that inhibit VEGF receptors, such as sunitinib and pazopanib, and those that inhibit mTOR, such as everolimus and temsirolimus. Unfortunately, most patients ultimately progress on treatment and die of their disease.
The new class of checkpoint blocking antibodies that target the PD-1 and the CTLA-4 receptors may provide profound and durable responses in a subset of patients. Ongoing work will help define the utility of these agents in the treatment of RCC, and will enable us to identify those most likely to benefit. Similar efforts are under way to identify the determinants of response and resistance to antiangiogenic drugs, and to design the next generation of agents, which will target factors that engender resistance to established agents.
Future research questions
What are the key genomic features that define a lethal renal cell carcinoma?
Does a risk adapted strategy for follow-up affect the natural course of disease?
How does resistance to antiangiogenic therapy develop and how can we overcome this resistance?
Which patients are most likely to benefit from checkpoint blocking antibodies and other classes of biological agents?
How can we rationally target drivers of non-clear cell renal cell carcinoma?
Contributors: All three authors helped with data gathering, analysis, and synthesis as well as the writing, review and final approval of the manuscript. EJ is guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare the following interests. EJ: consultant for Aveo, Bayer, GSK, Novartis, and Pfizer; clinical research support from BMS, GSK, Novartis, Pfizer, and Onyx; laboratory research support from Exelixis. WKR: consultant for Aveo (uncompensated), clinical research support from GSK and Seattle Genetics. ); WKR’s husband was funded for a research sabbatical by Novartis pharmaceuticals. JJG: none.
Provenance and peer review: Commissioned; externally peer reviewed.
Cite this as: BMJ 2014;349:g4797
References
- 1.Latif F, Tory K, Gnarra J, Yao M, Duh FM, Orcutt ML, et al. Identification of the von Hippel-Lindau disease tumour suppressor gene. Science 1993;260:1317-20. [DOI] [PubMed] [Google Scholar]
- 2.Kaelin WG Jr. The von Hippel-Lindau tumour suppressor protein: O2 sensing and cancer. Nat Rev Cancer 2008;8:865-73. [DOI] [PubMed] [Google Scholar]
- 3.International Agency for Research on Cancer. GLOBOCAN. Kidney—estimated incidence, all ages: both sexes. 2012 http://globocan.iarc.fr/old/summary_table_site-html.asp?selection=10210&title=Kidney&sex=0&type=0&window=1&africa=1&america=2&asia=3&europe=4&oceania=5&build=6&sort=0&submit=%C2%A0Execute%C2%A0.
- 4.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin 2013;63:11-30. [DOI] [PubMed] [Google Scholar]
- 5.Cancer Research UK. Kidney cancer incidence statistics. 2013. www.cancerresearchuk.org/cancer-info/cancerstats/types/kidney/incidence/#source17.
- 6.O’Connor SD, Pickhardt PJ, Kim DH, Oliva MR, Silverman SG. Incidental finding of renal masses at unenhanced CT: prevalence and analysis of features for guiding management. AJR Am J Roentgenol 2011;197:139-45. [DOI] [PubMed] [Google Scholar]
- 7.Linehan WM, Srinivasan R, Garcia JA. Non-clear cell renal cancer: disease-based management and opportunities for targeted therapeutic approaches. Semin Oncol 2013;40:511-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Algaba F, Akaza H, Lopez-Beltran A, Martignoni G, Moch H, Montironi R, et al. Current pathology keys of renal cell carcinoma. Eur Urol 2011;60:634-43. [DOI] [PubMed] [Google Scholar]
- 9.Delahunt B, Cheville JC, Martignoni G, Humphrey PA, Magi-Galluzzi C, McKenney J, et al. The International Society of Urological Pathology (ISUP) grading system for renal cell carcinoma and other prognostic parameters. Am J Surg Pathol 2013;37:1490-504. [DOI] [PubMed] [Google Scholar]
- 10.American Cancer Society. Cancer facts & figures. 2013. www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf.
- 11.Klatte T, Pantuck AJ, Said JW, Seligson DB, Rao NP, LaRochelle JC, et al. Cytogenetic and molecular tumor profiling for type 1 and type 2 papillary renal cell carcinoma. Clin Cancer Res 2009;15:1162-9. [DOI] [PubMed] [Google Scholar]
- 12.Yamazaki K, Sakamoto M, Ohta T, Kanai Y, Ohki M, Hirohashi S. Overexpression of KIT in chromophobe renal cell carcinoma. Oncogene 2003;22:847-52. [DOI] [PubMed] [Google Scholar]
- 13.Comprehensive molecular characterization of clear cell renal cell carcinoma. Nature 2013;499:43-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaelin WG. Von Hippel-Lindau disease. Annu Rev Pathol 2007;2:145-73. [DOI] [PubMed] [Google Scholar]
- 15.Jonasch E, Futreal PA, Davis IJ, Bailey ST, Kim WY, Brugarolas J, et al. State of the science: an update on renal cell carcinoma. Mol Cancer Res 2012;10:859-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Varela I, Tarpey P, Raine K, Huang D, Ong CK, Stephens P, et al. Exome sequencing identifies frequent mutation of the SWI/SNF complex gene PBRM1 in renal carcinoma. Nature 2011;469:539-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dalgliesh GL, Furge K, Greenman C, Chen L, Bignell G, Butler A, et al. Systematic sequencing of renal carcinoma reveals inactivation of histone modifying genes. Nature 2010;463:360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pena-Llopis S, Vega-Rubin-de-Celis S, Liao A, Leng N, Pavia-Jimenez A, Wang S, et al. BAP1 loss defines a new class of renal cell carcinoma. Nat Genet 2012;44:751-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hakimi AA, Ostrovnaya I, Reva B, Schultz N, Chen YB, Gonen M, et al. Adverse outcomes in clear cell renal cell carcinoma with mutations of 3p21 epigenetic regulators BAP1 and SETD2: a report by MSKCC and the KIRC TCGA research network. Clin Cancer Res 2013;19:3259-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gossage L, Murtaza M, Slatter AF, Lichtenstein CP, Warren A, Haynes B, et al. Clinical and pathological impact of VHL, PBRM1, BAP1, SETD2, KDM6A, and JARID1c in clear cell renal cell carcinoma. Genes Chromosomes Cancer 2014;53:38-51. [DOI] [PubMed] [Google Scholar]
- 21.Kapur P, Pena-Llopis S, Christie A, Zhrebker L, Pavia-Jimenez A, Rathmell WK, et al. Effects on survival of BAP1 and PBRM1 mutations in sporadic clear-cell renal-cell carcinoma: a retrospective analysis with independent validation. Lancet Oncol 2013;14:159-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schmidt L, Duh FM, Chen F, Kishida T, Glenn G, Choyke P, et al. Germline and somatic mutations in the tyrosine kinase domain of the MET proto-oncogene in papillary renal carcinomas. Nat Genet 1997;16:68-73. [DOI] [PubMed] [Google Scholar]
- 23.Toro JR, Nickerson ML, Wei MH, Warren MB, Glenn GM, Turner ML, et al. Mutations in the fumarate hydratase gene cause hereditary leiomyomatosis and renal cell cancer in families in North America. Am J Hum Genet 2003;73:95-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Speicher MR, Schoell B, du Manoir S, Schrock E, Ried T, Cremer T, et al. Specific loss of chromosomes 1, 2, 6, 10, 13, 17, and 21 in chromophobe renal cell carcinomas revealed by comparative genomic hybridization. Am J Pathol 1994;145:356-64. [PMC free article] [PubMed] [Google Scholar]
- 25.Perdeaux E, Solly J. Birt-Hogg-Dube syndrome. JAMA 2013;309:1460. [DOI] [PubMed] [Google Scholar]
- 26.Schmidt LS, Nickerson ML, Warren MB, Glenn GM, Toro JR, Merino MJ, et al. Germline BHD-mutation spectrum and phenotype analysis of a large cohort of families with Birt-Hogg-Dube syndrome. Am J Hum Genet 2005;76:1023-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu Q, Galli S, Srinivasan R, Linehan WM, Tsokos M, Merino MJ. Renal medullary carcinoma: molecular, immunohistochemistry, and morphologic correlation. Am J Surg Pathol 2013;37:368-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Edge S, Bird DR, Compton CC, Fritz AG, Greene, FL, Trotti A, eds. Kidney. In: American Joint Committee on Cancer Staging manual. 7th ed. Springer, 2010.
- 29.Elmore JM, Kadesky KT, Koeneman KS, Sagalowsky AI. Reassessment of the 1997 TNM classification system for renal cell carcinoma. Cancer 2003;98:2329-34. [DOI] [PubMed] [Google Scholar]
- 30.Verhoest G, Avakian R, Bensalah K, Thuret R, Ficarra V, Artibani W, et al. Urinary collecting system invasion is an independent prognostic factor of organ confined renal cell carcinoma. J Urol 2009;182:854-9. [DOI] [PubMed] [Google Scholar]
- 31.Motzer RJ, Bander NH, Nanus DM. Renal-cell carcinoma. N Engl J Med 1996;335:865-75. [DOI] [PubMed] [Google Scholar]
- 32.Motzer RJ, Mazumdar M, Bacik J, Berg W, Amsterdam A, Ferrara J. Survival and prognostic stratification of 670 patients with advanced renal cell carcinoma. J Clin Oncol 1999;17:2530-40. [DOI] [PubMed] [Google Scholar]
- 33.Mekhail TM, Abou-Jawde RM, Boumerhi G, Malhi S, Wood L, Elson P, et al. Validation and extension of the Memorial Sloan-Kettering prognostic factors model for survival in patients with previously untreated metastatic renal cell carcinoma. J Clin Oncol 2005;23:832-41. [DOI] [PubMed] [Google Scholar]
- 34.Gore ME, Larkin JM. Challenges and opportunities for converting renal cell carcinoma into a chronic disease with targeted therapies. Br J Cancer 2011;104:399-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Campbell SC, Novick AC, Belldegrun A, Blute ML, Chow GK, Derweesh IH, et al. Guideline for management of the clinical T1 renal mass. J Urol 2009;182:1271-9. [DOI] [PubMed] [Google Scholar]
- 36.Chow WH, Devesa SS, Warren JL, Fraumeni JF Jr. Rising incidence of renal cell cancer in the United States. JAMA 1999;281:1628-31. [DOI] [PubMed] [Google Scholar]
- 37.Stakhovskyi O, Yap SA, Leveridge M, Lawrentschuk N, Jewett MA. Small renal mass: what the urologist needs to know for treatment planning and assessment of treatment results. AJR Am J Roentgenol 2011;196:1267-73. [DOI] [PubMed] [Google Scholar]
- 38.Volpe A, Cadeddu JA, Cestari A, Gill IS, Jewett MA, Joniau S, et al. Contemporary management of small renal masses. Eur Urol 2011;60:501-15. [DOI] [PubMed] [Google Scholar]
- 39.Leveridge MJ, Finelli A, Kachura JR, Evans A, Chung H, Shiff DA, et al. Outcomes of small renal mass needle core biopsy, nondiagnostic percutaneous biopsy, and the role of repeat biopsy. Eur Urol 2011;60:578-84. [DOI] [PubMed] [Google Scholar]
- 40.Van Poppel H, Da Pozzo L, Albrecht W, Matveev V, Bono A, Borkowski A, et al. A prospective randomized EORTC intergroup phase 3 study comparing the complications of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol 2007;51:1606-15. [DOI] [PubMed] [Google Scholar]
- 41.Van Poppel H, Da Pozzo L, Albrecht W, Matveev V, Bono A, Borkowski A, et al. A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol 2011;59:543-52. [DOI] [PubMed] [Google Scholar]
- 42.Scosyrev E, Messing EM, Sylvester R, Campbell S, Van Poppel H. Renal function after nephron-sparing surgery versus radical nephrectomy: results from EORTC randomized trial 30904. Eur Urol 2014;65:372-7. [DOI] [PubMed] [Google Scholar]
- 43.Long JA, Yakoubi R, Lee B, Guillotreau J, Autorino R, Laydner H, et al. Robotic versus laparoscopic partial nephrectomy for complex tumors: comparison of perioperative outcomes. Eur Urol 2012;61:1257-62. [DOI] [PubMed] [Google Scholar]
- 44.Mir SA, Cadeddu JA, Sleeper JP, Lotan Y. Cost comparison of robotic, laparoscopic, and open partial nephrectomy. J Endourol 2011;25:447-53. [DOI] [PubMed] [Google Scholar]
- 45.Haddad RL, Patel MI, Vladica P, Kassouf W, Bladou F, Anidjar M. Percutaneous radiofrequency ablation of small renal tumors using CT-guidance: a review and its current role. Urol J 2012. l;9:629-38. [PubMed]
- 46.Siva S, Pham D, Gill S, Corcoran NM, Foroudi F. A systematic review of stereotactic radiotherapy ablation for primary renal cell carcinoma. BJU Int 2012;110:E737-43. [DOI] [PubMed] [Google Scholar]
- 47.Dib RE, Touma NJ, Kapoor A. Review of the efficacy and safety of radiofrequency ablation for the treatment of small renal masses. Can Urol Assoc J 2009;3:143-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hines-Peralta A, Goldberg SN. Review of radiofrequency ablation for renal cell carcinoma. Clin Cancer Res 2004;10(18 Pt 2):6328S-34S. [DOI] [PubMed] [Google Scholar]
- 49.Johnson DB, Solomon SB, Su LM, Matsumoto ED, Kavoussi LR, Nakada SY, et al. Defining the complications of cryoablation and radiofrequency ablation of small renal tumors: a multi-institutional review. J Urol 2004;172:874-7. [DOI] [PubMed] [Google Scholar]
- 50.Rehman J, Landman J, Lee D, Venkatesh R, Bostwick DG, Sundaram C, et al. Needle-based ablation of renal parenchyma using microwave, cryoablation, impedance- and temperature-based monopolar and bipolar radiofrequency, and liquid and gel chemoablation: laboratory studies and review of the literature. J Endourol 2004;18:83-104. [DOI] [PubMed] [Google Scholar]
- 51.Murphy DP, Gill IS. Energy-based renal tumor ablation: a review. Semin Urol Oncol 2001;19:133-40. [PubMed] [Google Scholar]
- 52.Ljungberg B. Words of wisdom. Re: Radical nephrectomy with and without lymph-node dissection: final results of european organization for research and treatment of cancer (EORTC) randomized phase 3 trial 30881. Eur Urol 2009;55:1486-7. [DOI] [PubMed] [Google Scholar]
- 53.Blom JH, van Poppel H, Marechal JM, Jacqmin D, Schroder FH, de Prijck L, et al. Radical nephrectomy with and without lymph-node dissection: final results of European Organization for Research and Treatment of Cancer (EORTC) randomized phase 3 trial 30881. Eur Urol 2009;55:28-34. [DOI] [PubMed] [Google Scholar]
- 54.Blom JH, van Poppel H, Marechal JM, Jacqmin D, Sylvester R, Schroder FH, et al. Radical nephrectomy with and without lymph node dissection: preliminary results of the EORTC randomized phase III protocol 30881. EORTC Genitourinary Group. Eur Urol 1999;36:570-5. [DOI] [PubMed] [Google Scholar]
- 55.Leibovich BC, Blute ML, Cheville JC, Lohse CM, Frank I, Kwon ED, et al. Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: a stratification tool for prospective clinical trials. Cancer 2003;97:1663-71. [DOI] [PubMed] [Google Scholar]
- 56.Ficarra V, Martignoni G, Lohse C, Novara G, Pea M, Cavalleri S, et al. External validation of the Mayo Clinic stage, size, grade and necrosis (SSIGN) score to predict cancer specific survival using a European series of conventional renal cell carcinoma. J Urol 2006;175:1235-9. [DOI] [PubMed] [Google Scholar]
- 57.Frank I, Blute ML, Cheville JC, Lohse CM, Weaver AL, Zincke H. An outcome prediction model for patients with clear cell renal cell carcinoma treated with radical nephrectomy based on tumor stage, size, grade and necrosis: the SSIGN score. J Urol 2002;168:2395-400. [DOI] [PubMed] [Google Scholar]
- 58.Han KR, Bleumer I, Pantuck AJ, Kim HL, Dorey FJ, Janzen NK, et al. Validation of an integrated staging system toward improved prognostication of patients with localized renal cell carcinoma in an international population. J Urol 2003;170(6 Pt 1):2221-4. [DOI] [PubMed] [Google Scholar]
- 59.Zisman A, Pantuck AJ, Dorey F, Said JW, Shvarts O, Quintana D, et al. Improved prognostication of renal cell carcinoma using an integrated staging system. J Clin Oncol 2001;19:1649-57. [DOI] [PubMed] [Google Scholar]
- 60.Raj GV, Thompson RH, Leibovich BC, Blute ML, Russo P, Kattan MW. Preoperative nomogram predicting 12-year probability of metastatic renal cancer. J Urol 2008;179:2146-51; discussion 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sorbellini M, Kattan MW, Snyder ME, Reuter V, Motzer R, Goetzl M, et al. A postoperative prognostic nomogram predicting recurrence for patients with conventional clear cell renal cell carcinoma. J Urol 2005;173:48-51. [DOI] [PubMed] [Google Scholar]
- 62.Lane BR, Kattan MW. Prognostic models and algorithms in renal cell carcinoma. Urol Clin North Am 2008;35:613-25; vii. [DOI] [PubMed] [Google Scholar]
- 63.Aitchison M, Bray CA, Van Poppel H, Sylvester R, Graham J, Innes C, et al. Adjuvant 5-flurouracil, alpha-interferon and interleukin-2 versus observation in patients at high risk of recurrence after nephrectomy for renal cell carcinoma: results of a phase iii randomised European Organisation for Research and Treatment of Cancer (Genito-Urinary Cancers Group)/National Cancer Research Institute trial. Eur J Cancer 2014;50:70-7. [DOI] [PubMed] [Google Scholar]
- 64.Scherr AJ, Lima JP, Sasse EC, Lima CS, Sasse AD. Adjuvant therapy for locally advanced renal cell cancer: a systematic review with meta-analysis. BMC Cancer 2011;11:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Clark JI, Atkins MB, Urba WJ, Creech S, Figlin RA, Dutcher JP, et al. Adjuvant high-dose bolus interleukin-2 for patients with high-risk renal cell carcinoma: a cytokine working group randomized trial. J Clin Oncol 2003;21:3133-40. [DOI] [PubMed] [Google Scholar]
- 66.Jonasch E, Wood CG, Matin SF, Tu SM, Pagliaro LC, Corn PG, et al. Phase II presurgical feasibility study of bevacizumab in untreated patients with metastatic renal cell carcinoma. J Clin Oncol 2009;27:4076-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cowey CL, Amin C, Pruthi RS, Wallen EM, Nielsen ME, Grigson G, et al. Neoadjuvant clinical trial with sorafenib for patients with stage II or higher renal cell carcinoma. J Clin Oncol 2010;28:1502-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.68Rini BI, Garcia J, Elson P, Wood L, Shah S, Stephenson A, et al. The effect of sunitinib on primary renal cell carcinoma and facilitation of subsequent surgery. J Urol 2012;187:1548-54. [DOI] [PubMed] [Google Scholar]
- 69.Thomas AA, Rini BI, Lane BR, Garcia J, Dreicer R, Klein EA, et al. Response of the primary tumor to neoadjuvant sunitinib in patients with advanced renal cell carcinoma. J Urol 2009;181:518-23; discussion 23. [DOI] [PubMed] [Google Scholar]
- 70.Conti SL, Thomas IC, Hagedorn JC, Chung BI, Chertow GM, Wagner TH, et al. Utilization of cytoreductive nephrectomy and patient survival in the targeted therapy era. Int J Cancer 2014;134:2245-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Flanigan RC, Salmon SE, Blumenstein BA, Bearman SI, Roy V, McGrath PC, et al. Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J Med 2001;345:1655-9. [DOI] [PubMed] [Google Scholar]
- 72.Mickisch GH, Garin A, van Poppel H, de Prijck L, Sylvester R. Radical nephrectomy plus interferon-alfa-based immunotherapy compared with interferon alfa alone in metastatic renal-cell carcinoma: a randomised trial. Lancet 2001;358:966-70. [DOI] [PubMed] [Google Scholar]
- 73.Motzer RJ, Bacik J, Murphy BA, Russo P, Mazumdar M. Interferon-alfa as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinoma. J Clin Oncol 2002;20:289-96. [DOI] [PubMed] [Google Scholar]
- 74.Heng DY, Xie W, Regan MM, Warren MA, Golshayan AR, Sahi C, et al. Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol 2009;27:5794-9. [DOI] [PubMed] [Google Scholar]
- 75.Fyfe G, Fisher RI, Rosenberg SA, Sznol M, Parkinson DR, Louie AC. Results of treatment of 255 patients with metastatic renal cell carcinoma who received high-dose recombinant interleukin-2 therapy. J Clin Oncol 1995;13:688-96. [DOI] [PubMed] [Google Scholar]
- 76.Yang J, Sherry RM, Steinberg SM, Topalian SL, Schwarzentruber DJ, Hwu P, et al. Randomized study of high-dose and low-dose interleukin-2 in patients with metastatic renal cancer. J Clin Oncol 2003;21:3127-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.McDermott DF, Regan MM, Clark JI, Flaherty LE, Weiss GR, Logan TF, et al. Randomized phase III trial of high-dose interleukin-2 versus subcutaneous interleukin-2 and interferon in patients with metastatic renal cell carcinoma. J Clin Oncol 2005;23:133-41. [DOI] [PubMed] [Google Scholar]
- 78.Pyrhonen S, Salminen E, Ruutu M, Lehtonen T, Nurmi M, Tammela T, et al. Prospective randomized trial of interferon alfa-2a plus vinblastine versus vinblastine alone in patients with advanced renal cell cancer. J Clin Oncol 1999;17:2859-67. [DOI] [PubMed] [Google Scholar]
- 79.Interferon-alpha and survival in metastatic renal carcinoma: early results of a randomised controlled trial. Medical Research Council Renal Cancer Collaborators [see comments]. Lancet 1999;353:14-7. [PubMed] [Google Scholar]
- 80.Nickerson ML, Jaeger E, Shi Y, Durocher JA, Mahurkar S, Zaridze D, et al. Improved identification of von Hippel-Lindau gene alterations in clear cell renal tumors. Clin Cancer Res 2008;14:4726-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med 2007;356:125-34. [DOI] [PubMed] [Google Scholar]
- 82.Escudier B, Pluzanska A, Koralewski P, Ravaud A, Bracarda S, Szczylik C, et al. Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: a randomised, double-blind phase III trial. Lancet 2007;370:2103-11. [DOI] [PubMed] [Google Scholar]
- 83.Motzer RJ, Escudier B, Oudard S, Hutson TE, Porta C, Bracarda S, et al. Efficacy of everolimus in advanced renal cell carcinoma: a double-blind, randomised, placebo-controlled phase III trial. Lancet 2008;372:449-56. [DOI] [PubMed] [Google Scholar]
- 84.Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 2007;356:115-24. [DOI] [PubMed] [Google Scholar]
- 85.Sternberg CN, Davis ID, Mardiak J, Szczylik C, Lee E, Wagstaff J, et al. Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol 2010;28:1061-8. [DOI] [PubMed] [Google Scholar]
- 86.Rini BI, Escudier B, Tomczak P, Kaprin A, Szczylik C, Hutson TE, et al. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet 2012;378:1931-9. [DOI] [PubMed] [Google Scholar]
- 87.McTigue M, Murray BW, Chen JH, Deng YL, Solowiej J, Kania RS. Molecular conformations, interactions, and properties associated with drug efficiency and clinical performance among VEGFR TK inhibitors. Proc Natl Acad Sci U S A 2012;109:18281-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Huang D, Ding Y, Li Y, Luo WM, Zhang ZF, Snider J, et al. Sunitinib acts primarily on tumor endothelium rather than tumor cells to inhibit the growth of renal cell carcinoma. Cancer Res 2010;70:1053-62. [DOI] [PubMed] [Google Scholar]
- 89.Rini BI, Cohen DP, Lu DR, Chen I, Hariharan S, Gore ME, et al. Hypertension as a biomarker of efficacy in patients with metastatic renal cell carcinoma treated with sunitinib. J Natl Cancer Inst 2011;103:763-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rini BI, Melichar B, Ueda T, Grunwald V, Fishman MN, Arranz JA, et al. Axitinib with or without dose titration for first-line metastatic renal-cell carcinoma: a randomised double-blind phase 2 trial. Lancet Oncol 2013;14: 1233-42. [DOI] [PMC free article] [PubMed]
- 91.Rini BI, Cohen DP, Lu DR, Chen I, Hariharan S, Gore ME, et al. Hypertension as a biomarker of efficacy in patients with metastatic renal cell carcinoma treated with sunitinib. J Natl Cancer Inst 2011;103:763-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Escudier B, Szczylik C, Hutson TE, Demkow T, Staehler M, Rolland F, et al. Randomized phase II trial of first-line treatment with sorafenib versus interferon alfa-2a in patients with metastatic renal cell carcinoma. J Clin Oncol 2009;27:1280-9. [DOI] [PubMed] [Google Scholar]
- 93.Motzer RJ, Hutson TE, Cella D, Reeves J, Hawkins R, Guo J, et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N Engl J Med 2013;369:722-31. [DOI] [PubMed] [Google Scholar]
- 94.Hutson TE, Lesovoy V, Al-Shukri S, Stus VP, Lipatov ON, Bair AH, et al. Axitinib versus sorafenib as first-line therapy in patients with metastatic renal-cell carcinoma: a randomised open-label phase 3 trial. Lancet Oncol 2013;14:1287-94. [DOI] [PubMed] [Google Scholar]
- 95.Rini BI, Halabi S, Rosenberg JE, Stadler WM, Vaena DA, Ou SS, et al. Bevacizumab plus interferon alfa compared with interferon alfa monotherapy in patients with metastatic renal cell carcinoma: CALGB 90206. J Clin Oncol 2008;26:5422-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hudes G, Carducci M, Tomczak P, Dutcher J, Figlin R, Kapoor A, et al. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med 2007;356:2271-81. [DOI] [PubMed] [Google Scholar]
- 97.Hutson TE, Escudier B, Esteban E, Bjarnason GA, Lim HY, Pittman KB, et al. Randomized phase iii trial of temsirolimus versus sorafenib as second-line therapy after sunitinib in patients with metastatic renal cell carcinoma. J Clin Oncol 2013; published online 2 Dec. [DOI] [PMC free article] [PubMed]
- 98.Atkinson BJ, Kalra S, Wang X, Bathala T, Corn P, Tannir NM, et al. Clinical outcomes for patients with metastatic renal cell carcinoma treated with alternative sunitinib schedules. J Urol 2014;191:611-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rini BI, Melichar B, Ueda T, Grunwald V, Fishman MN, Arranz JA, et al. Axitinib with or without dose titration for first-line metastatic renal-cell carcinoma: a randomised double-blind phase 2 trial. Lancet Oncol 2013;14:1233-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Oudard S, et al. Overall survival and updated results for sunitinib compared with interferon alfa in patients with metastatic renal cell carcinoma. J Clin Oncol 2009;27:3584-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Escudier B, Bellmunt J, Negrier S, Bajetta E, Melichar B, Bracarda S, et al. Phase III trial of bevacizumab plus interferon alfa-2a in patients with metastatic renal cell carcinoma (AVOREN): final analysis of overall survival. J Clin Oncol 2010;28:2144-50. [DOI] [PubMed] [Google Scholar]
- 102.Motzer RJ, Escudier B, Oudard S, Hutson TE, Porta C, Bracarda S, et al. Phase 3 trial of everolimus for metastatic renal cell carcinoma: final results and analysis of prognostic factors. Cancer 2010;116:4256-65. [DOI] [PubMed] [Google Scholar]
- 103.Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Staehler M, et al. Sorafenib for treatment of renal cell carcinoma: final efficacy and safety results of the phase III treatment approaches in renal cancer global evaluation trial. J Clin Oncol 2009;27:3312-8. [DOI] [PubMed] [Google Scholar]
- 104.Motzer RJ, Escudier B, Tomczak P, Hutson TE, Michaelson MD, Negrier S, et al. Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol 2013;14:552-62. [DOI] [PubMed] [Google Scholar]
- 105.Cancer Genome Atlas Research Network. Comprehensive molecular characterization of clear cell renal cell carcinoma. Nature 2013;499:43-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sharma P, Wagner K, Wolchok JD, Allison JP. Novel cancer immunotherapy agents with survival benefit: recent successes and next steps. Nat Rev Cancer 2011;11:805-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Peggs KS, Quezada SA, Allison JP. Cancer immunotherapy: co-stimulatory agonists and co-inhibitory antagonists. Clin Exp Immunol 2009;157:9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yang JC, Hughes M, Kammula U, Royal R, Sherry RM, Topalian SL, et al. Ipilimumab (anti-CTLA4 antibody) causes regression of metastatic renal cell cancer associated with enteritis and hypophysitis. J Immunother 2007;30:825-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 2012;366:2443-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med 2012;366:2455-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Motzer RJ, Nosov D, Eisen T, Bondarenko I, Lesovoy V, Lipatov O, et al. Tivozanib versus sorafenib as initial targeted therapy for patients with metastatic renal cell carcinoma: results from a phase III trial. J Clin Oncol 2013;31:3791-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Choueiri TK, Pal SK, McDermott DF, Ramies DA, Morrissey S, Lee Y, et al. Efficacy of cabozantinib (XL184) in patients with metastatic, refractory renal cell carcinoma (RCC). J Clin Oncol 2012;30(suppl): abstr 4504.
- 113.Motzer RJ, Porta C, Vogelzang NJ, Sternberg CN, Szczylik C, Zolnierek J, et al. Dovitinib versus sorafenib for third-line targeted treatment of patients with metastatic renal cell carcinoma: an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:286-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chresta CM, Davies BR, Hickson I, Harding T, Cosulich S, Critchlow SE, et al. AZD8055 is a potent, selective, and orally bioavailable ATP-competitive mammalian target of rapamycin kinase inhibitor with in vitro and in vivo antitumor activity. Cancer Res 2010;70:288-98. [DOI] [PubMed] [Google Scholar]
- 115.Asahina H, Nokihara H, Yamamoto N, Yamada Y, Tamura Y, Honda K, et al. Safety and tolerability of AZD8055 in Japanese patients with advanced solid tumors; a dose-finding phase I study. Invest New Drugs 2013;31:677-84. [DOI] [PubMed] [Google Scholar]
- 116.Cho DC, Cohen MB, Panka DJ, Collins M, Ghebremichael M, Atkins MB, et al. The efficacy of the novel dual PI3-kinase/mTOR inhibitor NVP-BEZ235 compared with rapamycin in renal cell carcinoma. Clin Cancer Res 2010;16:3628-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gerlinger M, Rowan AJ, Horswell S, Larkin J, Endesfelder D, Gronroos E, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med 2012;366:883-92. [DOI] [PMC free article] [PubMed] [Google Scholar]