Abstract
Human Toll-like receptors (TLRs) are a family of transmembrane receptors, which play a key role in both innate and adaptive immune responses. Beside of recognizing specific molecular patterns that associated with different types of pathogens, TLRs may also detect a number of self-proteins and endogenous nucleic acids. Activating TLRs lead to the heightened expression of various inflammatory genes, which have a protective role against infection. Data rising predominantly from human patients and animal models of autoimmune disease indicate that, inappropriate triggering of TLR pathways by exogenous or endogenous ligands may cause the initiation and/or perpetuation of autoimmune reactions and tissue damage. Given their important role in infectious and non-infectious disease process, TLRs and its signaling pathways emerge as appealing targets for therapeutics. In this review, we demonstrate how TLRs pathways could be involved in autoimmune disorders and their therapeutic application.
Keywords: Toll-like receptor, Immune response, Autoimmune disease, Therapeutic application
Introduction
Overview on TLRs
The innate immune system, an organism’s first line of defense against invading pathogens, consists of different molecules and cells that work in conjunction with the adaptive immune system to maintain physiological homeostasis of the host and to protect it against potentially pathogenic organisms.1 Recognition of a wide range of molecular structures that presents in different microorganisms is dependent on a diverse set of germ line encoded receptors, termed pattern recognition receptors (PRRs).2 These receptors are expressed by a variety type of cells — especially the innate immune system cells, such as dendritic cells (DCs) and macrophages — and they act to sense danger or damage signals. The PRR ligands comprise conserved microbial structures, named pathogen-associated molecular patterns (PAMPs), such as viral and bacterial nucleic acids, lipopolysaccharide (LPS) and flagellin. In addition, PRRs can sense damage-associated molecular patterns (DAMPs, endogenous danger signals from dead and dying cells), such as saturated fatty acids and amyloid β.3 Toll-like receptors (TLRs), the best characterized PRRs, were first reported in humans in 1998.3,4 These receptors are a family of type I transmembrane glycoproteins comprised of an extracellular domain with leucine-rich repeat (LRR) motifs, and a Toll/interleukin-1 receptor (IL-1R) -interacting (TIR) domain with at least 11 members in human and 13 in mouse, which leads to intracellular signaling and play an important role in both innate and acquired immune responses.5-7 Each TLR is able to recognize a particular molecular pattern. For example, TLR2, 4, 5, 6 and 11 bind to bacterial membrane-associated molecules such as LPS, lipoprotein and peptidoglycan whereas TLR3, 7, 8 and 9 sense viral and bacterial or endogenous nucleic acids, including ssRNA, dsRNA, and unmethylated cytosine phosphate guanine (CpG) -containing DNA (Table 1). Also, TLRs can be classified based on their localization in the cell so that TLR1, 2, 4, 5 and 6 are expressed on the cell membrane, whereas TLR3, 7, 8 and 9 are localized mainly in the endosomal compartment.8 Triggering of TLRs upon ligand binding results in signaling events that lead to the expression of some immune response genes, including inflammatory cytokines, stimulatory immune cytokines, chemokines, and costimulatory molecules (Figure 1), which augment the killing of pathogens and initiates the process of developing acquired immunity.4
Table 1. Toll-like receptors and their ligands, adaptor usage, and cytokine production .
| TLR | Cellular location | Exogenous ligands | Endogenous ligands | Signal adaptor | Production | References |
| TLR1 | Cell surface | Bacteria: triacyl-lipopeptides | Unknown | MyD88 | Proinflammatory cytokines | 3,9-12 |
| TLR2 | Cell surface | Bacteria: peptidoglycan, lipoproteins, LTA Fungi: zymosan |
HSP60, HSP70; Gp96 fragments) hyaluronic acid (ECM HMGB1, versican and |
MyD88/ TIRAP | Proinflammatory cytokines | 3,10-16 |
| TLR3 | Endosomal Compartment |
Viruses: dsRNA | mRNA | TRIF | Proinflammatory cytokines, type I IFNs | 3,10-12,17 |
| TLR4 | Cell surface | Bacteria: LPS Viruses: RSV fusion protein Fungi: mannan Protozoa: Glycoinositolphospholipids |
HSP22, HSP 60, HSP70, HSP72, Gp96, HMGB1, oxidized phospholipids heparin sulfate, fibronectin, tenascin-C, b-defensin 2, versican, hyaluronic acid, |
MyD88/ TIRAP/ TRAM/ TRIF |
Proinflammatory cytokines, type I IFNs | 3,10-12,14,16,18 |
| TLR5 | Cell surface | Bacteria: flagellin | Unknown | MyD88 | Proinflammatory cytokines | 3,10-12,19 |
| TLR7 | Endosomal Compartment |
Viruses: ssRNA | ssRNA (immune complex) | MyD88 | Proinflammatory cytokines, type I IFNs | 3,10-12,20 |
| TLR8 | Endosomal Compartment |
Viruses: ssRNA | ssRNA (immune complex) | MyD88 | Proinflammatory cytokines, type I IFNs | 3,10-12,21 |
| TLR9 | Endosomal compartment |
Bacteria: CpG DNA Viruses: CpG DNA Protozoa: CpG DNA, haemozoin |
Chromatin IgG complex | MyD88 | Proinflammatory cytokines, type I IFNs | 3,10-12,22 |
| TLR11 | Endosomal compartment |
Protozoa: profilin-like molecule (a protein from Toxoplasmosis gondii) | Unknown | MyD88 | Proinflammatory cytokines | 3,10-12,23 |
| TLR13 | Endosomal compartment |
Bacteria: 23S rRNA | Unknown | MyD88 | Proinflammatory cytokines | 3,10-12,17 |
Abbreviations: LTA, lipoteichoic acid; ECM, extracellular matrix; IFN, interferon; dsRNA, double-stranded RNA; LPS, lipopolysaccharide; RSV, respiratory syncytial virus; HSP, heat-shock protein; Gp96, glycoprotein 96; HMGB1, high-mobility group box 1; MyD88, Myeloid differentiation primary response protein 88; TIRAP, Toll/IL-1 receptor-domain-containing adaptor protein; TRAM, TRIF-related adaptor molecule; dsRNA, Double-stranded RNA; TRIF, Toll/IL-1 receptor-domain-containing adaptor protein inducing INF-α; ssRNA, Single stranded RNA; CpG, unmethylated cytosine-guanosine.
Figure 1.
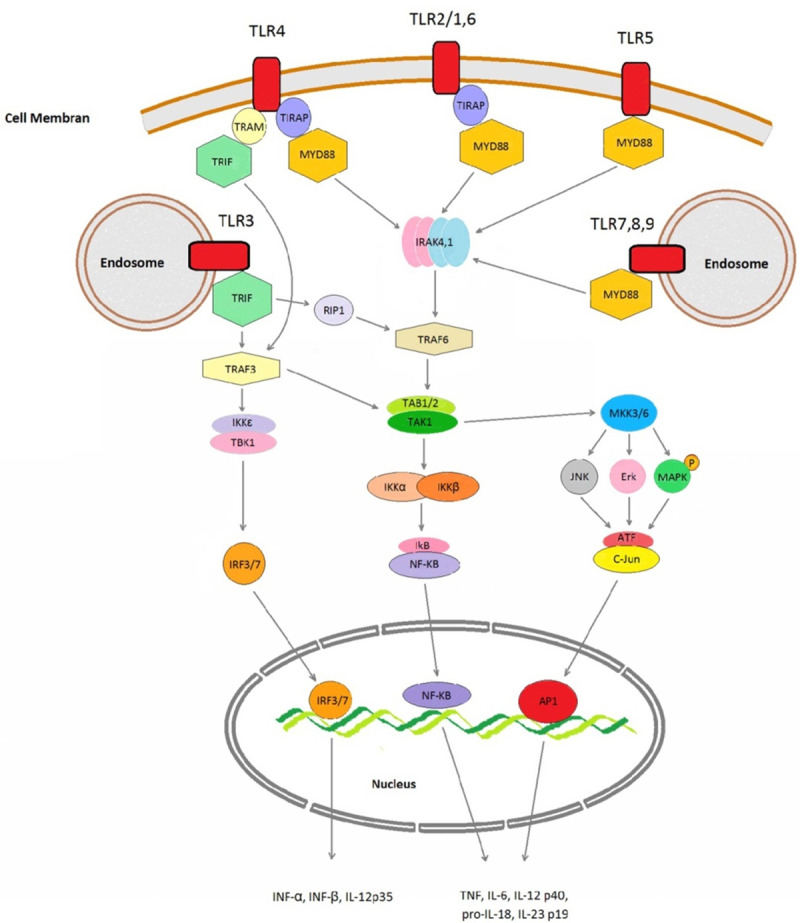
Overview of the Toll-like receptor signaling pathway
When TLRs are stimulated by their ligands, they recruit downstream adaptor molecules, such as myeloid Toll/interleukin (IL) -1 receptor (TIR) -domain-containing adaptor-inducing interferon-β (TRIF), TRIF-related adaptor molecule (TRAM) and differentiation primary-response protein 88 (MyD88) which trigger other downstream molecules leading to the activation of signaling cascades that converge at the nuclear factor-kB (NF-kB), interferon (IFN) response factors (IRFs) and mitogen-activated protein (MAP) kinases. These transcription factors induce the transcription of some proinflammatory agents, such as interleukin (IL) -6, IL-12, IL-23, and tumor necrosis factor α (TNF-α). The production and secretion of these molecules counters the threat posed by microbes and helps activate other immunological components. AP1, activator protein 1; ATF, activating transcription factor; ERK, extracellular signal-regulated kinase; IKK, inhibitor of kappa light polypeptide gene enhancer in B-cell kinase; IRAK, IL-1 receptor-associated kinase; JNK, c-Jun N-terminal kinase; MKK, MAPK kinase; RIP1, receptor interacting protein 1; TAB, transforming growth factor-b-activated kinase 1/MAP3K7- binding protein; TAK, transforming growth factor-activated kinase; TRAF, tumor necrosis factor receptor-associated factor.
TLRs and autoimmunity
Autoimmunity is emerged by several coincident mechanisms that relate to the presence of auto-reactive immune cell subsets and loss of immunological tolerance.10 Loss of tolerance during central and peripheral differentiation of the adaptive immune response may lead to uncontrolled activation of self-reactive B and T cells which induce autoimmunity assisted by the cells of the innate immunity. TLR expression has been found in various types of immune cells, including T cells, B cells, different subsets of dendritic cells, monocytes, macrophages, neutrophils, eosinophils, mast cells, and epithelial cells (Table 2).8,11,19,24 TLR signaling plays an essential role in the activation of the adaptive immune system by inducing the production of pro-inflammatory cytokines and up-regulating costimulatory molecules of antigen presenting cells (APCs).7 Considering the role of TLRs as a critical link between the innate and the adaptive immune responses, the idea has created that continuous activation or dysregulation of TLR signaling might contribute to the pathogenesis of autoimmunity.25,26
Table 2. The expression pattern of Toll-like receptors (TLRs) on different immune cells .
| TLR | Expression on immune cells | References |
| TLR1 | Most cell types including DCs and B cells | 8 |
| TLR2 | PMLs, DCs, monocytes and T cells | 13,14,27 |
| TLR3 | DCs, NK cells and T cells | 17,28 |
| TLR4 | Macrophages, DCs and T cells | 17,18,28 |
| TLR5 | Monocytes, DCs, NK cells and T cells | 17,19 |
| TLR6 | High expression in B cells and DCs; low in monocytes and NK cells | 17,29 |
| TLR7 | B cells, DCs, monocytes and T cells | 20,28 |
| TLR8 | Monocytes, DCs; low in NK and T cells | 21,22 |
| TLR9 | DCs, B cells, PMLs, macrophages, NK cells and microglial cells | 8,22 |
| TLR10 | B cells; low in DCs | 28,30 |
DC, dendritic cell; NK, natural killer; PML, peripheral mononuclear leukocytes
Role of TLRs on B cells function in autoimmunity
Systemic autoimmune diseases are frequently associated with the production of autoantibodies that react with nuclear or cytosolic cellular components. These autoantibodies have an important role in the immunopathogenesis of various autoimmune diseases.31 A key finding which brought the logical link between the TLRs that recognize nucleic acids and the production of antibodies (Abs) that recognizes nucleic acids involved studies on AM14 transgenic mice. The B cells of these mice express specific Abs for self-IgG, also known as rheumatoid factor.32 In this study, anti-nucleosomal IgG was mixed well with cell lysates to induce B cell proliferation in transgenic B cells.33 Furthermore, this stimulation was DNase sensitive and depends on MyD88, and TLR9 inhibitory oligonucleotides could abrogate the response of the auto-reactive B cells. These observations provided the first report of a synergistic effect between a DNA-binding TLR and a BCR that binds and internalizes DNA-containing complexes. More support of the role of DNA as a stimulus of auto-reactive B cells was shown by using transgenic 3H9 B cells that have a specific BCR for DNA.34 With this system, CpG-associated proliferation was also sensitive to TLR-inhibiting oligonucleotides, confirming the idea that combined signals via TLRs and the BCR provide a mechanism to activate auto-reactive B cells.31 Using an animal model of autoimmunity making by an anti-DNA BCR transgene and homozygous deficiency of the FcγR IIB, an inhibitory receptor, it was shown that isotype switching of auto-reactive B cells to the IgG2a and 2b subclasses requires TLR9 and MyD88 signaling; accordingly, deficiency in TLR9 or MyD88 resulted in reduced pathology and mortality in this model.35 As well, B cells containing the Y-linked autoimmune accelerator (Yaa), a genetic modifier, have an intrinsic tendency toward the production of more pathogenic anti-nucleolar autoantibodies. Analysis of the Yaa locus showed a duplication of the TLR7 gene.36 Also, the importance of TLR7 role as a coreceptor to activate auto-reactive B cells are more supported by a study using a BCR knockin mouse with specificity for a number of nuclear antigens. Breakage of tolerance and autoantibody production in this mouse was largely dependent on TLR7.37 Finally, by analyzing chimeric mice, where deficiency in TLR9 is restricted to the B cell lineage, suggests that TLR9 promotes the activation and differentiation of anti-DNA plasmablasts in murine lupus via a B cell-intrinsic mechanism.38,39 Also, TLR4 signaling directs peripheral B cells to rapidly locate within the lymph nodes (LNs) and the splenic white pulp. So, it probably does by enhancing chemokine receptor expression, increasing the expression of L-selectin molecules, and biasing the signaling pathway toward heightened responsiveness. The TLR4-activated cells predominantly reside in the center of the LN follicle where they can directly interact with each other. If an LN follicle contains a germinal center, exposure to a TLR4 ligand will promote the entrance of stimulated B cells into the dark zone. Signals from TLR response provide a mechanism that augments the polyclonal expansion of the B cells which happens after exposure to infectious agents and during the course of autoimmune disorders.40 In humans, the peripheral dendritic cells (pDCs) expressing TLR-9 recognize bacterial and viral nucleic acids. So, the activation of pDCs through TLR-9 leads to production and release of type I IFN (IFN-α, IFN-β) which enhance humoral immunity. In fact, IFN-α enables B cells to undergo isotype-switching and mature into antibody-secreting cells.41 Also, TLR-9 stimulation with CpG_oligodeoxynucleotide (ODN) induces naive B cell maturation into memory cells, as demonstrated by the AID mRNA expression, induction of CD27 and IgG production. On the other hand, IFN-α produced by pDCs amplifies the inductive effect of CpG-ODN on naive B cells activation and on Ig production through a mechanism involving TLR-9/MyD88-dependent signaling (by an up-regulation of MyD88 expression). Thus, TLR-9 signaling plays a direct role on naive B cells, comprising Ig production with a possible risk for autoimmunity, and an indirect role on pDCs, comprising IFN-α production, which boost IgM production, further amplifies the susceptibility to autoimmune disorders.42
Role of TLRs on T cells function in autoimmunity
Researches showed that T helper 17 (TH17) and TH1 cells or IL 17+ IFNγ+ CD4+ T cells may have pathogenic roles in chronic inflammatory and autoimmune diseases. Before the discovery of TH17 cells, it was believed that TH1 cells were the primary pathogenic cell population in T cell-mediated autoimmune disorders. However, mice deficient in IFNγ or IL 12 were found to have enhanced susceptibility to collagen-induced arthritis (CIA) and experimental autoimmune encephalomyelitis (EAE).43-45 It was subsequently shown that IL 17–/– mice have a reduced susceptibility to EAE,46 and that EAE can be induced in naive mice following the transfer of myelin-specific TH17 cells that are isolated from mice with EAE and expanded in vitro using IL 23.47 It has also been reported that the transfer of auto-reactive TH1 cells into naive recipients induced experimental autoimmune uveitis (EAU) in this group, and this was not inhibited by treatment with specific anti-IL-17 antibodies.48 Finally, CD4+ T cells that express both IL 17 and IFNγ have been found in the gut of patients with Crohn’s disease.49 It is well established that TLR signaling in innate immune cells can indirectly promote T cell differentiation and proliferation through DC maturation and regulatory cytokine production. TLR3, TLR4 or TLR9 ligands induce MyD88 dependent production of cytokines from DCs that promotes the differentiation of TH17 cells.50 Moreover, the TLR4 ligand LPS promotes IL 17 production by antigen-specific memory T cells in mice through the induction of IL 1 and IL 23 production by DCs.51 T cells also express TLRs, and evidence is showing that TLR signaling in T cells can promote the cytokine production or regulate their function.3
Role of TLRs in regulatory T cells function in autoimmunity
Regulatory CD4+ CD25+ T (Treg) cells with the ability to suppress host immune responses against self- or non-self antigens have significant roles in the processes of autoimmunity. Interestingly, new evidence proposes that TLR signaling may directly or indirectly regulate the immunosuppressive function of CD4+ CD25+ Treg cells in immune responses. TLR signaling may shift the balance between CD4+ T-helper cells and Treg cells, and finally influence the outcome of the immune response.11 The effect of TLR signaling on Treg cells suppression experiments indicated that TLR ligands such as LPS and unmethylated CpG DNA motifs (which bind TLR4 and TLR9, respectively) allowed T cells to proliferate even in the presence of Tregs. It is now supposed that CpG-DNA can directly costimulate T-cell proliferation and also can make T cells resistant to Treg suppression in a MyD88-dependent manner.52,53 Ligation of TLR2 has been reported to confer resistance to suppression of Treg, in part by increasing IL-2 production.54 In the other hand, following the extension of TLR2-driven proliferation, Treg suppression appeared to be enhanced.27 Also ligation of flagellin to TLR5 has been shown to increase Treg suppressive capacity.19 In contrast, triggering of TLR8 with nucleic acid ligands has been shown to directly impair Treg function.21 Thus, Treg suppression can be either boosted or attenuated by distinct TLR ligands.55
Role of TLRs in the pathogenesis of autoimmune diseases
Systemic lupus erythematosus (SLE)
Increasingly, data from both murine and human studies have implicated TLR activation in the pathogenesis of SLE. SLE is a systemic autoimmune disease characterized by the production of autoantibodies.56 The patient sera contain endogenous ligands for TLRs, particularly the nucleic acid binding TLRs including TLR7, TLR8 and TLR9.57,58 In patients with SLE, auto-reactive cells are producing large quantities of autoantibodies against self-nuclear antigens which make immune complexes with self-nucleic acids and present in SLE serum. Since self-RNA and self-DNA in the form of protein complexes can act as TLR7 and TLR9 ligands, stimulation of TLRs is suggested as an additional signal contributing to activate and/or modulation of the aberrant adaptive immune response. Data from researches on mouse models suggest a pathogenic role for TLR7 signaling and a protective role for TLR9 signaling in the pathogenesis of SLE.59
Rheumatoid arthritis (RA)
RA is a chronic inflammatory autoimmune disease characterized by the progressive and irreversible destruction of joints.60 Some of the endogenous TLR ligands can be found in arthritic joints. Recently it was shown that RNA released from necrotic synovial fluid cells of RA patients can activate TLR3 on RA synovial fibroblasts.61 The presence of endogenous TLR4 ligands such as fibronectin fragments and heat-shock proteins (HSPs) has also been demonstrated in rheumatoid synovium,62-64 and it has been reported that rheumatoid synovial fibroblast–like cells synthesize extra domain A (ED-A) –containing fibronectin.65 In addition, serum and synovial fluid of RA patients can activate a TLR4–expressing ovary cell line of Chinese hamster, suggesting the presence of TLR4–activating substances in RA serum and joints.25,66
Multiple Sclerosis (MS)
MS is an autoimmune disease in which central nervous system (CNS) lesions result from the perivascular immune cell infiltration associated with damage to myelin, oligodendrocytes and neurons. In MS, leukocytes such as monocytes, DCs, NK cells, B cells and CD4+ CD8+ T cells, migrate to the CNS and cause myelin destruction, axon damage and neuronal cell death.67-69 Ligation of TLR2 and TLR4 of DCs with endogenous ligands such as high mobility group box 1 (HMGB1) induces the production of IL1, IL6 and IL12 that stimulate the differentiation of naive T cells into Th1 and Th17 cells, which secrete INFγ and IL17 respectively. INFγ/IL17-producing T cells facilitate leukocyte migration through the blood-brain barrier and contribute to CNS damage.70
Experimental autoimmune encephalomyelitis (EAE)
EAE is a family of models of autoimmune CNS damage induced by the immunization of experimental animals with CNS components (either an extract, purified protein or a peptide), usually in the presence of an adjuvant,71 which in turn promote pathogenic auto-reactive T cell responses. Studies showed that mice deficient in the adaptor protein MyD88 is resistant to EAE, which associated with decreased IL 6 and IL 23 production by DCs and decreased IFNγ and IL 17 production by T cells.72,73 This suggests that innate immune responses that are initiated through TLR or IL 1R signaling are required for the induction of experimental autoimmunity. Mice with a lymphoid cell-specific TLR2 deficiency is less susceptible to EAE and have reduced Th17 responses compared with wild-type controls.74 Also, it has been reported that parenteral injection of polyinosinic–polycytidylic acid (poly I: C), a TLR3 ligand, suppressed relapsing–remitting EAE.75 Collectively, these findings indicate that TLR and IL 1R signaling is crucial for the induction of EAE. Moreover, depending on the stage of the disease, some TLRs (including TLR2 and TLR9) may have pro-inflammatory functions, whereas others (such as TLR3 and TLR9) may also have a regulatory role in the EAE process.3
TLRs as drug targets for autoimmunity
Since the bulk of the data suggests that the TLR pathway plays a key role in autoimmune disease pathogenesis, targeting TLRs and their signaling pathways may provide an effective therapeutic approach for certain autoimmune diseases. Since there are several proteins involved in TLR signaling, there are various targets that may be utilized for potential drugs (Table 3).
Table 3. Toll-like receptor targeting drugs .
| Drug | Mechanism of function | References |
| IRS 661 | Block signaling via TLR-7 and inhibit the production of IFN-α by human plasmacytoid dendritic cells (pDC) | 2,76-81 |
| Nucleic acid-binding polymers | Recognize ssRNA, dsRNA or hypomethylated DNA, inhibit nucleic acid-mediated activation of TLRs | 4 |
| High molecular weight hyaluronan (HA900) | Up-regulated suppressor of cytokine signaling 3 (SOCS3) expression and down-regulated pleiotrophin expression | 82 |
| 9-benzyl-8-hydroxy-2-(2-methoxyethoxy) adenine | Induced hypo-responsiveness or tolerance to TLR7 | 83 |
| Vitamin D3 | Down-regulate TLR2 and TLR4 expression on monocytes | 84 |
| Chloroquine and related compounds | TLR7/8/9 antagonists, inhibits signaling through these TLRs | 77,85-87 |
| ST2825 | A heptapeptide analog specifically designed to inhibit MyD88 dimerization, interfere with the recruitment of IRAK1 and IRAK4 by MyD88, resulting in the inhibition of IL-1β-mediated activation of NF-κB and IL-6. Suppressed B cell proliferation and differentiation into plasma | 88 |
| Compound 4a | Interfere with the interaction between MyD88 and IL-1R at the TIR domains | 89 |
| RO0884 | Dual inhibitor of IRAK1 and IRAK4, block pro-inflammatory cytokine production | 90 |
Synthetic oligo deoxynucleotides with immunoregulatory sequences (IRS)
Conclusion
TLR molecules and their downstream signaling pathways play a critical role in activating innate and adaptive immune cells. Their specific role in modulating immunity also interferes with the mechanisms that maintain tolerance in the host. Thus, aberrantly expressed or activated of TLRs can contribute to the loss of tolerance by multiple mechanisms. Given that this pathway is important in several autoimmune diseases, this axis constitutes an attractive target for therapeutic intervention.
Ethical Issues
Not applicable.
Conflict of Interest
The authors report no conflicts of interest.
References
- 1.Kulkarni R, Behboudi S, Sharif S. Insights into the role of Toll-like receptors in modulation of T cell responses. Cell Tissue Res. 2011;343(1):141–52. doi: 10.1007/s00441-010-1017-1. [DOI] [PubMed] [Google Scholar]
- 2.Barrat FJ, Coffman RL. Development of TLR inhibitors for the treatment of autoimmune diseases. Immunol Rev. 2008;223:271–83. doi: 10.1111/j.1600-065x.2008.00630.x. [DOI] [PubMed] [Google Scholar]
- 3.Mills KH. TLR-dependent T cell activation in autoimmunity. Nat Rev Immunol. 2011;11(12):807–22. doi: 10.1038/nri3095. [DOI] [PubMed] [Google Scholar]
- 4.Lee J, Sohn JW, Zhang Y, Leong KW, Pisetsky D, Sullenger BA. Nucleic acid-binding polymers as anti-inflammatory agents. Proc Natl Acad Sci U S A. 2011;108(34):14055–60. doi: 10.1073/pnas.1105777108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Booth J, Wilson H, Jimbo S, Mutwiri G. Modulation of B cell responses by Toll-like receptors. Cell Tissue Res. 2011;343(1):131–40. doi: 10.1007/s00441-010-1031-3. [DOI] [PubMed] [Google Scholar]
- 6.Skivka LM, Pozur VV. Responses with participation of toll-like receptors in protective immunity and in pathologic states. Ukr Biokhim Zh. 2008;80(3):5–20. [PubMed] [Google Scholar]
- 7.Li M, Zhou Y, Feng G, Su SB. The critical role of Toll-like receptor signaling pathways in the induction and progression of autoimmune diseases. Curr Mol Med. 2009;9(3):365–74. doi: 10.2174/156652409787847137. [DOI] [PubMed] [Google Scholar]
- 8.Kawai T, Akira S. TLR signaling. Semin Immunol. 2007;19(1):24–32. doi: 10.1016/j.smim.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 9.Berglova I, Krejsek J, Kolackova M, Slezak R. B cell toll-like receptors with respect to the pathogenesis of Sjogren's syndrome. Acta Medica (Hradec Kralove) 2011;54(2):51–7. doi: 10.14712/18059694.2016.18. [DOI] [PubMed] [Google Scholar]
- 10.Anders HJ, Zecher D, Pawar RD, Patole PS. Molecular mechanisms of autoimmunity triggered by microbial infection. Arthritis Res Ther. 2005;7(5):215–24. doi: 10.1186/ar1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu G, Zhao Y. Toll-like receptors and immune regulation: their direct and indirect modulation on regulatory CD4+ CD25+ T cells. Immunology. 2007;122(2):149–56. doi: 10.1111/j.1365-2567.2007.02651.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anwar MA, Basith S, Choi S. Negative regulatory approaches to the attenuation of Toll-like receptor signaling. Exp Mol Med. 2013;45:e11. doi: 10.1038/emm.2013.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel M, Xu D, Kewin P, Choo-Kang B, Mcsharry C, Thomson NC. et al. TLR2 agonist ameliorates established allergic airway inflammation by promoting Th1 response and not via regulatory T cells. J Immunol. 2005;174(12):7558–63. doi: 10.4049/jimmunol.174.12.7558. [DOI] [PubMed] [Google Scholar]
- 14.Murphy TJ, Ni Choileain N, Zang Y, Mannick JA, Lederer JA. CD4+CD25+ regulatory T cells control innate immune reactivity after injury. J Immunol. 2005;174(5):2957–63. doi: 10.4049/jimmunol.174.5.2957. [DOI] [PubMed] [Google Scholar]
- 15.Liew FY, Xu D, Brint EK, O'neill LA. Negative regulation of toll-like receptor-mediated immune responses. Nat Rev Immunol. 2005;5(6):446–58. doi: 10.1038/nri1630. [DOI] [PubMed] [Google Scholar]
- 16.Oganesyan G, Saha SK, Guo B, He JQ, Shahangian A, Zarnegar B. et al. Critical role of TRAF3 in the Toll-like receptor-dependent and -independent antiviral response. Nature. 2006;439(7073):208–11. doi: 10.1038/nature04374. [DOI] [PubMed] [Google Scholar]
- 17.Bellocchio S, Moretti S, Perruccio K, Fallarino F, Bozza S, Montagnoli C. et al. TLRs govern neutrophil activity in aspergillosis. J Immunol. 2004;173(12):7406–15. doi: 10.4049/jimmunol.173.12.7406. [DOI] [PubMed] [Google Scholar]
- 18.Fitzgerald KA, McWhirter SM, Faia KL, Rowe DC, Latz E, Golenbock DT. et al. Ikkepsilon and tbk1 are essential components of the irf3 signaling pathway. Nat Immunol. 2003;4(5):491–6. doi: 10.1038/ni921. [DOI] [PubMed] [Google Scholar]
- 19.Crellin NK, Garcia RV, Hadisfar O, Allan SE, Steiner TS, Levings MK. Human CD4+ T cells express TLR5 and its ligand flagellin enhances the suppressive capacity and expression of FOXP3 in CD4+CD25+ T regulatory cells. J Immunol. 2005;175(12):8051–9. doi: 10.4049/jimmunol.175.12.8051. [DOI] [PubMed] [Google Scholar]
- 20.Lee J, Wu CC, Lee KJ, Chuang TH, Katakura K, Liu YT. et al. Activation of anti-hepatitis C virus responses via Toll-like receptor 7. Proc Natl Acad Sci U S A. 2006;103(6):1828–33. doi: 10.1073/pnas.0510801103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peng G, Guo Z, Kiniwa Y, Voo KS, Peng W, Fu T. et al. Toll-like receptor 8-mediated reversal of CD4+ regulatory T cell function. Science. 2005;309(5739):1380–4. doi: 10.1126/science.1113401. [DOI] [PubMed] [Google Scholar]
- 22.Sun CM, Deriaud E, Leclerc C, Lo-Man R. Upon TLR9 Signaling, CD5+ B Cells Control the IL-12-Dependent Th1-Priming Capacity of Neonatal DCs. Immunity. 2005;22(4):467–77. doi: 10.1016/j.immuni.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 23.Wang RF, Peng G, Wang HY. Regulatory T cells and Toll-like receptors in tumor immunity. Semin Immunol. 2006;18(2):136–42. doi: 10.1016/j.smim.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 24.Mazzoni A, Segal DM. Controlling the Toll road to dendritic cell polarization. J Leukocyte Biol. 2004;75(5):721–30. doi: 10.1189/jlb.1003482. [DOI] [PubMed] [Google Scholar]
- 25.Abdollahi-Roodsaz S, Joosten LA, Roelofs MF, Radstake TR, Matera G, Popa C. et al. Inhibition of Toll-like receptor 4 breaks the inflammatory loop in autoimmune destructive arthritis. Arthritis Rheum. 2007;56(9):2957–67. doi: 10.1002/art.22848. [DOI] [PubMed] [Google Scholar]
- 26.Fischer M, Ehlers M. Toll-like receptors in autoimmunity. Ann N Y Acad Sci. 2008;1143(1):21–34. doi: 10.1196/annals.1443.012. [DOI] [PubMed] [Google Scholar]
- 27.Sutmuller RP, Den Brok MH, Kramer M, Bennink EJ, Toonen LW, Kullberg BJ. et al. Toll-like receptor 2 controls expansion and function of regulatory T cells. J Clin Invest. 2006;116(2):485–94. doi: 10.1172/jci25439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nishiya T, Kajita E, Miwa S, Defranco AL. TLR3 and TLR7 are targeted to the same intracellular compartments by distinct regulatory elements. J Biol Chem. 2005;280(44):37107–17. doi: 10.1074/jbc.m504951200. [DOI] [PubMed] [Google Scholar]
- 29.Wang RF. Regulatory T cells and toll-like receptors in cancer therapy. Cancer Res. 2006;66(10):4987–90. doi: 10.1158/0008-5472.can-05-4676. [DOI] [PubMed] [Google Scholar]
- 30.Houot R, Perrot I, Garcia E, Durand I, Lebecque S. Human CD4+CD25high regulatory T cells modulate myeloid but not plasmacytoid dendritic cells activation. J Immunol. 2006;176(9):5293–8. doi: 10.4049/jimmunol.176.9.5293. [DOI] [PubMed] [Google Scholar]
- 31.Green NM, Marshak-Rothstein A. Toll-like receptor driven B cell activation in the induction of systemic autoimmunity. Semin Immunol. 2011;23(2):106–12. doi: 10.1016/j.smim.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leadbetter EA, Rifkin IR, Hohlbaum AM, Beaudette BC, Shlomchik MJ, Marshak-Rothstein A. Chromatin-IgG complexes activate B cells by dual engagement of IgM and Toll-like receptors. Nature. 2002;416(6881):603–7. doi: 10.1038/416603a. [DOI] [PubMed] [Google Scholar]
- 33.Deane JA, Bolland S. Nucleic acid-sensing TLRs as modifiers of autoimmunity. J Immunol. 2006;177(10):6573–8. doi: 10.4049/jimmunol.177.10.6573. [DOI] [PubMed] [Google Scholar]
- 34.Fields ML, Metzgar MH, Hondowicz BD, Kang SA, Alexander ST, Hazard KD. et al. Exogenous and endogenous TLR ligands activate anti-chromatin and polyreactive B cells. J Immunol. 2006;176(11):6491–502. doi: 10.4049/jimmunol.176.11.6491. [DOI] [PubMed] [Google Scholar]
- 35.Ehlers M, Fukuyama H, McGaha TL, Aderem A, Ravetch JV. TLR9/MyD88 signaling is required for class switching to pathogenic IgG2a and 2b autoantibodies in SLE. J Exp Med. 2006;203(3):553–61. doi: 10.1084/jem.20052438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pisitkun P, Deane JA, Difilippantonio MJ, Tarasenko T, Satterthwaite AB, Bolland S. Autoreactive B cell responses to RNA-related antigens due to TLR7 gene duplication. Science. 2006;312(5780):1669–72. doi: 10.1126/science.1124978. [DOI] [PubMed] [Google Scholar]
- 37.Berland R, Fernandez L, Kari E, Han JH, Lomakin I, Akira S. et al. Toll-like receptor 7-dependent loss of B cell tolerance in pathogenic autoantibody knockin mice. Immunity. 2006;25(3):429–40. doi: 10.1016/j.immuni.2006.07.014. [DOI] [PubMed] [Google Scholar]
- 38.Christensen SR, Shlomchik MJ. Regulation of lupus-related autoantibody production and clinical disease by Toll-like receptors. Semin Immunol. 2007;19(1):11–23. doi: 10.1016/j.smim.2006.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meyer-Bahlburg A, Rawlings DJ. B cell autonomous TLR signaling and autoimmunity. Autoimmun Rev. 2008;7(4):313–6. doi: 10.1016/j.autrev.2007.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hwang IY, Park C, Harrison K, Kehrl JH. TLR4 signaling augments B lymphocyte migration and overcomes the restriction that limits access to germinal center dark zones. J Exp Med. 2009;206(12):2641–57. doi: 10.1084/jem.20091982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Le Bon A, Schiavoni G, D'agostino G, Gresser I, Belardelli F, Tough DF. Type i interferons potently enhance humoral immunity and can promote isotype switching by stimulating dendritic cells in vivo. Immunity. 2001;14(4):461–70. doi: 10.1016/s1074-7613(01)00126-1. [DOI] [PubMed] [Google Scholar]
- 42.Giordani L, Sanchez M, Libri I, Quaranta MG, Mattioli B, Viora M. Ifn-alpha amplifies human naive b cell tlr-9-mediated activation and ig production. J Leukoc Biol. 2009;86(2):261–71. doi: 10.1189/jlb.0908560. [DOI] [PubMed] [Google Scholar]
- 43.Cua DJ, Sherlock J, Chen Y, Murphy CA, Joyce B, Seymour B. et al. Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature. 2003;421(6924):744–8. doi: 10.1038/nature01355. [DOI] [PubMed] [Google Scholar]
- 44.Vermeire K, Heremans H, Vandeputte M, Huang S, Billiau A, Matthys P. Accelerated collagen-induced arthritis in IFN-gamma receptor-deficient mice. J Immunol. 1997;158(11):5507–13. [PubMed] [Google Scholar]
- 45.Krakowski M, Owens T. Interferon-γ confers resistance to experimental allergic encephalomyelitis. Eur J Immunol. 1996;26(7):1641–6. doi: 10.1002/eji.1830260735. [DOI] [PubMed] [Google Scholar]
- 46.Komiyama Y, Nakae S, Matsuki T, Nambu A, Ishigame H, Kakuta S. et al. IL-17 plays an important role in the development of experimental autoimmune encephalomyelitis. J Immunol. 2006;177(1):566–73. doi: 10.4049/jimmunol.177.1.566. [DOI] [PubMed] [Google Scholar]
- 47.Langrish CL, Chen Y, Blumenschein WM, Mattson J, Basham B, Sedgwick JD. et al. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J Exp Med. 2005;201(2):233–40. doi: 10.1084/jem.20041257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Luger D, Silver PB, Tang J, Cua D, Chen Z, Iwakura Y. et al. Either a Th17 or a Th1 effector response can drive autoimmunity: conditions of disease induction affect dominant effector category. J Exp Med. 2008;205(4):799–810. doi: 10.1084/jem.20071258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Annunziato F, Cosmi L, Santarlasci V, Maggi L, Liotta F, Mazzinghi B. et al. Phenotypic and functional features of human Th17 cells. J Exp Med. 2007;204(8):1849–61. doi: 10.1084/jem.20070663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Veldhoen M, Hocking RJ, Atkins CJ, Locksley RM, Stockinger B. TGFbeta in the context of an inflammatory cytokine milieu supports de novo differentiation of IL-17-producing T cells. Immunity. 2006;24(2):179–89. doi: 10.1016/j.immuni.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 51.Higgins SC, Jarnicki AG, Lavelle EC, Mills KH. TLR4 mediates vaccine-induced protective cellular immunity to Bordetella pertussis: role of IL-17-producing T cells. J Immunol. 2006;177(11):7980–9. doi: 10.4049/jimmunol.177.11.7980. [DOI] [PubMed] [Google Scholar]
- 52.Gelman AE, Larosa DF, Zhang J, Walsh PT, Choi Y, Sunyer JO. et al. The adaptor molecule MyD88 activates PI-3 kinase signaling in CD4+ T cells and enables CpG oligodeoxynucleotide-mediated costimulation. Immunity. 2006;25(5):783–93. doi: 10.1016/j.immuni.2006.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Larosa DF, Gelman AE, Rahman AH, Zhang J, Turka LA, Walsh PT. CpG DNA inhibits CD4+CD25+ Treg suppression through direct MyD88-dependent costimulation of effector CD4+ T cells. Immunol Lett. 2007;108(2):183–8. doi: 10.1016/j.imlet.2006.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu H, Komai-Koma M, Xu D, Liew FY. Toll-like receptor 2 signaling modulates the functions of CD4+ CD25+ regulatory T cells. Proc Natl Acad Sci U S A. 2006;103(18):7048–53. doi: 10.1073/pnas.0601554103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Walker LS. Regulatory T cells overturned: the effectors fight back. Immunology. 2009;126(4):466–74. doi: 10.1111/j.1365-2567.2009.03053.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Groom JR, Fletcher CA, Walters SN, Grey ST, Watt SV, Sweet MJ. et al. BAFF and MyD88 signals promote a lupuslike disease independent of T cells. J Exp Med. 2007;204(8):1959–71. doi: 10.1084/jem.20062567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lafyatis R, York M. Innate immunity and inflammation in systemic sclerosis. Curr Opin Rheumatol. 2009;21(6):617–22. doi: 10.1097/bor.0b013e32832fd69e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Marshak-Rothstein A. Toll-like receptors in systemic autoimmune disease. Nat Rev Immunol. 2006;6(11):823–35. doi: 10.1038/nri1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Celhar T, Magalhaes R, Fairhurst AM. TLR7 and TLR9 in SLE: when sensing self goes wrong. Immunol Res. 2012;53(1-3):58–77. doi: 10.1007/s12026-012-8270-1. [DOI] [PubMed] [Google Scholar]
- 60.Maciejewska Rodrigues H, Jungel A, Gay RE, Gay S. Innate immunity, epigenetics and autoimmunity in rheumatoid arthritis. Mol Immunol. 2009;47(1):12–8. doi: 10.1016/j.molimm.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 61.Brentano F, Schorr O, Gay RE, Gay S, Kyburz D. RNA released from necrotic synovial fluid cells activates rheumatoid arthritis synovial fibroblasts via Toll-like receptor 3. Arthritis Rheum. 2005;52(9):2656–65. doi: 10.1002/art.21273. [DOI] [PubMed] [Google Scholar]
- 62.Scott DL, Delamere JP, Walton KW. The distribution of fibronectin in the pannus in rheumatoid arthritis. Br J Exp Pathol. 1981;62(4):362–8. [PMC free article] [PubMed] [Google Scholar]
- 63.Walle TK, Vartio T, Helve T, Virtanen I, Kurki P. Cellular fibronectin in rheumatoid synovium and synovial fluid: a possible factor contributing to lymphocytic infiltration. Scand J Immunol. 1990;31(4):535–40. doi: 10.1111/j.1365-3083.1990.tb02802.x. [DOI] [PubMed] [Google Scholar]
- 64.Roelofs MF, Boelens WC, Joosten LA, Abdollahi-Roodsaz S, Geurts J, Wunderink LU. et al. Identification of small heat shock protein B8 (HSP22) as a novel TLR4 ligand and potential involvement in the pathogenesis of rheumatoid arthritis. J Immunol. 2006;176(11):7021–7. doi: 10.4049/jimmunol.176.11.7021. [DOI] [PubMed] [Google Scholar]
- 65.Hino K, Shiozawa S, Kuroki Y, Ishikawa H, Shiozawa K, Sekiguchi K. et al. EDA-containing fibronectin is synthesized from rheumatoid synovial fibroblast-like cells. Arthritis Rheum. 1995;38(5):678–83. doi: 10.1002/art.1780380516. [DOI] [PubMed] [Google Scholar]
- 66.Roelofs MF, Joosten LA, Abdollahi-Roodsaz S, Van Lieshout AW, Sprong T, Van Den Hoogen FH. et al. The expression of toll-like receptors 3 and 7 in rheumatoid arthritis synovium is increased and costimulation of toll-like receptors 3, 4, and 7/8 results in synergistic cytokine production by dendritic cells. Arthritis Rheum. 2005;52(8):2313–22. doi: 10.1002/art.21278. [DOI] [PubMed] [Google Scholar]
- 67.Toneatto S, Finco O, Van Der Putten H, Abrignani S, Annunziata P. Evidence of blood-brain barrier alteration and activation in HIV-1 gp120 transgenic mice. AIDS. 1999;13(17):2343–8. doi: 10.1097/00002030-199912030-00005. [DOI] [PubMed] [Google Scholar]
- 68.Deng C, Radu C, Diab A, Tsen MF, Hussain R, Cowdery JS. et al. IL-1 receptor-associated kinase 1 regulates susceptibility to organ-specific autoimmunity. J Immunol. 2003;170(6):2833–42. doi: 10.4049/jimmunol.170.6.2833. [DOI] [PubMed] [Google Scholar]
- 69.Waldner H, Collins M, Kuchroo VK. Activation of antigen-presenting cells by microbial products breaks self tolerance and induces autoimmune disease. J Clin Invest. 2004;113(7):990–7. doi: 10.1172/JCI19388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Miranda-Hernandez S, Baxter AG. Role of toll-like receptors in multiple sclerosis. Am J Clin Exp Immunol. 2013;2(1):75–93. [PMC free article] [PubMed] [Google Scholar]
- 71.Baxter AG. The origin and application of experimental autoimmune encephalomyelitis. Nat Rev Immunol. 2007;7(11):904–12. doi: 10.1038/nri2190. [DOI] [PubMed] [Google Scholar]
- 72.Prinz M, Garbe F, Schmidt H, Mildner A, Gutcher I, Wolter K. et al. Innate immunity mediated by TLR9 modulates pathogenicity in an animal model of multiple sclerosis. J Clin Invest. 2006;116(2):456–64. doi: 10.1172/jci26078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Marta M, Andersson A, Isaksson M, Kampe O, Lobell A. Unexpected regulatory roles of TLR4 and TLR9 in experimental autoimmune encephalomyelitis. Eur J Immunol. 2008;38(2):565–75. doi: 10.1002/eji.200737187. [DOI] [PubMed] [Google Scholar]
- 74.Reynolds JM, Pappu BP, Peng J, Martinez GJ, Zhang Y, Chung Y. et al. Toll-like receptor 2 signaling in CD4(+) T lymphocytes promotes T helper 17 responses and regulates the pathogenesis of autoimmune disease. Immunity. 2010;32(5):692–702. doi: 10.1016/j.immuni.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Touil T, Fitzgerald D, Zhang GX, Rostami A, Gran B. Cutting Edge: TLR3 stimulation suppresses experimental autoimmune encephalomyelitis by inducing endogenous IFN-beta. J Immunol. 2006;177(11):7505–9. doi: 10.4049/jimmunol.177.11.7505. [DOI] [PubMed] [Google Scholar]
- 76.Pawar RD, Ramanjaneyulu A, Kulkarni OP, Lech M, Segerer S, Anders HJ. Inhibition of Toll-like receptor-7 (TLR-7) or TLR-7 plus TLR-9 attenuates glomerulonephritis and lung injury in experimental lupus. J Am Soc Nephrol. 2007;18(6):1721–31. doi: 10.1681/asn.2006101162. [DOI] [PubMed] [Google Scholar]
- 77.Sun S, Rao NL, Venable J, Thurmond R, Karlsson L. TLR7/9 antagonists as therapeutics for immune-mediated inflammatory disorders. Inflamm Allergy Drug Targets. 2007;6(4):223–35. doi: 10.2174/187152807783334300. [DOI] [PubMed] [Google Scholar]
- 78.Sibilia J. Novel concepts and treatments for autoimmune disease: ten focal points. Joint Bone Spine. 2004;71(6):511–7. doi: 10.1016/j.jbspin.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 79.Horton CG, Pan ZJ, Farris AD. Targeting Toll-like receptors for treatment of SLE. Mediators Inflamm. 2010;2010:1–9. doi: 10.1155/2010/498980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhu J, Mohan C. Toll-like receptor signaling pathways--therapeutic opportunities. Mediators Inflamm. 2010;2010:1–7. doi: 10.1155/2010/781235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tse K, Horner AA. Update on toll-like receptor-directed therapies for human disease. Ann Rheum Dis. 2007;66 Suppl 3:iii77–80. doi: 10.1136/ard.2007.078998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Asari A, Kanemitsu T, Kurihara H. Oral administration of high molecular weight hyaluronan (900 kDa) controls immune system via Toll-like receptor 4 in the intestinal epithelium. J Biol Chem. 2010;285(32):24751–8. doi: 10.1074/jbc.m110.104950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hayashi T, Gray CS, Chan M, Tawatao RI, Ronacher L, Mcgargill MA. et al. Prevention of autoimmune disease by induction of tolerance to Toll-like receptor 7. Proc Natl Acad Sci U S A. 2009;106(8):2764–9. doi: 10.1073/pnas.0813037106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Du T, Zhou ZG, You S, Huang G, Lin J, Yang L. et al. Modulation of monocyte hyperresponsiveness to TLR ligands by 1,25-dihydroxy-vitamin D3 from LADA and T2DM. Diabetes Res Clin Pract. 2009;83(2):208–14. doi: 10.1016/j.diabres.2008.09.046. [DOI] [PubMed] [Google Scholar]
- 85.Rutz M, Metzger J, Gellert T, Luppa P, Lipford GB, Wagner H. et al. Toll-like receptor 9 binds single-stranded CpG-DNA in a sequence- and pH-dependent manner. Eur J Immunol. 2004;34(9):2541–50. doi: 10.1002/eji.200425218. [DOI] [PubMed] [Google Scholar]
- 86.Krieg AM, Vollmer J. Toll-like receptors 7, 8, and 9: linking innate immunity to autoimmunity. Immunol Rev. 2007;220:251–69. doi: 10.1111/j.1600-065x.2007.00572.x. [DOI] [PubMed] [Google Scholar]
- 87.Papadimitraki ED, Bertsias GK, Boumpas DT. Toll like receptors and autoimmunity: a critical appraisal. J Autoimmun. 2007;29(4):310–8. doi: 10.1016/j.jaut.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 88.Loiarro M, Capolunghi F, Fanto N, Gallo G, Campo S, Arseni B. et al. Pivotal Advance: Inhibition of MyD88 dimerization and recruitment of IRAK1 and IRAK4 by a novel peptidomimetic compound. J Leukoc Biol. 2007;82(4):801–10. doi: 10.1189/jlb.1206746. [DOI] [PubMed] [Google Scholar]
- 89.Bartfai T, Behrens MM, Gaidarova S, Pemberton J, Shivanyuk A, Rebek J Jr. A low molecular weight mimic of the Toll/IL-1 receptor/resistance domain inhibits IL-1 receptor-mediated responses. Proc Natl Acad Sci U S A. 2003;100(13):7971–6. doi: 10.1073/pnas.0932746100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Song KW, Talamas FX, Suttmann RT, Olson PS, Barnett JW, Lee SW. et al. The kinase activities of interleukin-1 receptor associated kinase (IRAK)-1 and 4 are redundant in the control of inflammatory cytokine expression in human cells. Mol Immunol. 2009;46(7):1458–66. doi: 10.1016/j.molimm.2008.12.012. [DOI] [PubMed] [Google Scholar]


