Abstract
Objective
Nectin-4 is a member of the Nectin family of four Ca+-independent immunoglobulin-like cell adhesion molecules and implicated in cell adhesion, movement, proliferation, differentiation, polarization, and survival. The aberrant expression of Nectin-4 has been found in a variety of tumors; however, its expression in hepatocellular carcinoma (HCC) is still poorly understood. This study was to investigate the expression of Nectin-4 and its clinical significance in the patients with HCC.
Methods
The expression of Nectin-4 was assessed at mRNA and protein levels by quantitative reverse transcription polymerase chain reaction (qRT-PCR) and Western blotting assays in 20 HCC specimens and adjacent non-tumor live tissues. Furthermore, the clinical significance of Nectin-4 in 87 cases of HCC was confirmed by immunohistochemistry.
Results
The mRNA and protein levels of Nectin-4 were higher in HCC tumor tissues than in the matched non-tumor tissues. Nectin-4 was located in the cytoplasm of tumor cells and over-expressed in 67.82% (59/87) HCC tissues by immunohistochemical staining. Positive Nectin-4 expression was significantly correlated with tumor size (P=0.029), status of metastasis (P=0.023), vascular invasion (P=0.018) and tumor-node-metastasis stage (P=0.003). In addition, Kaplan–Meier survival analysis indicated that positive Nectin-4 expression was associated with worse recurrence-free survival (RFS) and overall survival (OS) (P=0.006 and P=0.005, respectively). In multivariate analysis, Nectin-4 was an independent prognostic factor for RFS and OS in the patients with HCC.
Conclusion
Nectin-4 is upregulated in HCC and may be a novel prognostic biomarker for the patients after surgical resection.
Keywords: Nectin-4, hepatocellular carcinoma, prognostic marker, RT-PCR, Western blot, immunohistochemistry
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common malignancy worldwide and its mortality rate ranks the third among all tumor-associated disease.1 At present, the most effective therapies for the patients with HCC are surgical resection and liver transplantation, but most patients are inoperable due to the late diagnosis.2 Even after surgical removal, the long-term prognosis for most patients with HCC remains unsatisfactory because of its high rate of recurrence.3,4 Therefore, searching new applicable biological biomarkers for HCC is urgently needed to predict prognosis and improve therapeutic efficacy.
Nectin is a family of four Ca+-independent immunoglobulin-like cell adhesion molecules (Nectin-1 to 4), which contribute to cell–cell adhesion in a homotypic or heterotypic manner and mediate several cellular behaviors, such as movement, proliferation, differentiation, polarization, survival, and the entry of viruses.5–10 All Nectins share similar domain structure: an extracellular region with three immunoglobulin-like domains, a single transmembrane region, and a short cytoplasmic tail domain.6,11 Nectins, localized normally to the adherens junctions, are components of E-cadherin junctions in epidermal cells and are connected to the actin cytoskeleton through the afadin scaffold molecule.12–14 While the other three Nectins are widely expressed in normal adult tissues, Nectin-4 expression is originally restricted in the embryo and placenta.5,10 Recently, several researchers found that Nectin-4 was over-expressed in human breast cancer,15,16 ovarian cancer,17 lung cancer,18 pancreatic adenocarcinoma,19 and colon carcinoma.20 However, the expression patterns and clinical significance of Nectin-4 in HCC have not been determined.
In this study, we measured the levels of Nectin-4 mRNA and protein in HCC tumor tissue and adjacent non-tumor liver tissue by quantitative reverse transcription polymerase chain reaction (qRT-PCR) and Western blotting. In addition, we also used immunohistochemistry to evaluate the expression of Nectin-4 in HCC tissues and to investigate its association with clinicopathological features as well as patient survival.
Materials and methods
Patients and tissue samples
This study was approved by the Human Research Ethics Committee of Anhui Medical University, and the written informed consent was obtained from all of the patients. A total of 20 pairs of snap-frozen HCC tumor tissues and adjacent non-tumor liver tissues (2 cm away from tumor margin) used for qRT-PCR and Western blotting were collected from the Affiliated Provincial Hospital of Anhui Medical University (Hefei, People’s Republic of China). In addition, 87 pairs of paraffin-embedded HCC samples and non-tumor liver tissues were collected between June 2006 and April 2010 for immunohistochemistry. None of the patients received anti-tumor therapy before surgery. These patients comprised 66 males and 21 females with a mean age of 53 years (range: 21–78 years). Hepatic function was assessed using the Child–Pugh grade. Tumor size was defined in its maximum dimension. Tumor differentiation was classified according to the Edmondson grading system.21 The pathological tumor stage was evaluated according to the sixth edition of the tumor-node-metastasis (TNM) classification of the International Union Against Cancer. The main clinicopathological parameters of the patients were shown in Table 1. The complete follow-up data were collected from all patients. Median follow-up was 23 months (range: 2–60 months). Recurrence-free survival (RFS) time was the interval between surgical operation and first confirmed recurrence. Overall Survival (OS) was the time from the date of surgery to death or last observation.
Table 1.
Correlation between clinicopathological variables and Nectin-4 expression in HCC
| Variables | Total | Nectin-4 protein expression
|
χ2 | P-value | |
|---|---|---|---|---|---|
| Negative | Positive | ||||
| Sex | |||||
| Male | 66 | 19 | 47 | 1.445 | 0.229 |
| Female | 21 | 9 | 12 | ||
| Age (years) | |||||
| ≤50 | 36 | 13 | 23 | 0.434 | 0.510 |
| >50 | 51 | 15 | 36 | ||
| HBsAg status | |||||
| Negative | 25 | 10 | 15 | 0.982 | 0.322 |
| Positive | 62 | 18 | 44 | ||
| Liver cirrhosis | |||||
| Absent | 14 | 6 | 8 | 0.871 | 0.351 |
| Present | 73 | 22 | 51 | ||
| Child–Pugh grade | |||||
| A | 68 | 21 | 47 | 0.242 | 0.623 |
| B | 19 | 7 | 12 | ||
| AFP (ng/mL) | |||||
| ≤20 | 32 | 10 | 22 | 0.020 | 0.887 |
| >20 | 55 | 18 | 37 | ||
| Tumor size (cm) | |||||
| ≤5 | 33 | 6 | 27 | 4.776 | 0.029 |
| >5 | 54 | 22 | 32 | ||
| Status of metastasis | |||||
| Absent | 58 | 14 | 44 | 5.161 | 0.023 |
| Present | 29 | 14 | 15 | ||
| Tumor capsula | |||||
| Complete | 43 | 16 | 27 | 0.984 | 0.321 |
| None | 44 | 12 | 32 | ||
| Vascular invasion | |||||
| Absent | 43 | 19 | 24 | 5.612 | 0.018 |
| Present | 44 | 9 | 35 | ||
| Edmondson grade | |||||
| I–II | 45 | 17 | 28 | 1.336 | 0.248 |
| III–IV | 42 | 11 | 31 | ||
| TNM stage | |||||
| I–II | 52 | 23 | 29 | 8.595 | 0.003 |
| III–IV | 35 | 5 | 30 | ||
Abbreviations: AFP, α-fetoprotein; HBsAg, hepatitis B surface antigen; HCC, hepatocellular carcinoma; TNM, tumor-node-metastasis.
qRT-PCR analysis
The total RNA from frozen HCC tumor and adjacent non-tumor tissues was extracted using TRIzol reagent (Thermo Fisher Scientific, Waltham, MA, USA) according to the manufacturer’s instructions. cDNA was synthesized from 1 μg of total RNA using the RevertAid First Strand cDNA Synthesis Kit (Thermo Fisher Scientific). Messenger RNA (mRNA) expression of Nectin-4 was performed using SYBR green-based RT-PCR on a PikoReal Real-Time PCR System (Thermo Fisher Scientific). The cycling conditions were as follows: an initial denaturation step of 95°C for 3 minutes, followed by 40 amplification cycles involving denaturation at 95°C for 10 seconds, annealing at 60°C for 60 seconds, and elongation at 72°C for 60 seconds. The Nectin-4 primer sequences were (forward) 5′-CAAAATCTGTGGCACATTGG-3′ and (reverse) 5′-GCTGACATGGCAGACGTAGA-3′. β-Actin (forward 5′-GGGAAATCGTGCGTGACATTAAGG-3′ and reverse 5′-CAGGAAGGAAGGCTGGAAGAGTG-3′) was used as an internal control. The Nectin-4 mRNA expression between samples was evaluated using the 2−∆∆Ct method.22
Western blot analysis
The tissue samples were lysed with radioimmunoprecipitation assay (RIPA) lysis buffer with phenylmethylsulfonyl fluoride (Beyotime Institute of Biotechnology, Shanghai, People’s Republic of China) 1 mm at 4°C for 30 minutes, followed by centrifugation at 12,000 rpm for 10 minutes at 4°C, and protein concentration were measured using the BCA protein assay (Thermo Fisher Scientific). Equal amounts of protein from sample were separated on 10% sodium dodecyl sulfate polyacrylamide gel electrophoresis gels and transferred onto polyvinylidene fluoride membranes (PVDF membrane, EMD Millipore, Billerica, MA, USA) in an ice-water environment. The membranes were blocked with blocking buffer (0.05% Tween 20-phosphate-buffered saline [PBS] with 5% non-fat milk) for 2 hours at room temperature and then incubated overnight at 4°C with rabbit primary antibodies against human Nectin-4 (1:1,000 dilution, Abcam, Cambridge, MA, USA) and the internal control human β-actin (Zhongshan Golden Bridge Biotechnology Inc, Beijing, People’s Republic of China). The blot was washed three times with 0.05% Tween 20-PBS, then the membranes were incubated with anti-rabbit secondary antibodies conjugated with horseradish peroxidase (1:60,000) for 2 hours at 37°C. Immunoreactive bands of protein were visualized using the enhanced chemiluminescence kit (ECL; Pierce Biotechnology, Rockford, IL, USA). Finally, the densities of the bands were quantified with a computerized densitometer (ImageJ Launcher, Broken Symmetry Software, Bethesda, MD, USA). Equivalent protein loading and transfer efficiency were verified by staining for β-actin.
Immunohistochemical analysis
Tissue sections (2 μm thick) were deparaffinized with xylene, rehydrated, washed in PBS, and then retrieved by Tris-ethylenediaminetetraacetic acid (EDTA) buffer (pH 9.0) in the microwave antigen retrieval for 20 minutes. Endogenous peroxidase activity was blocked by 0.3% hydrogen peroxide for 10 minutes. Sections were incubated in goat serum at room temperature for 30 minutes to reduce non-specific binding. Next, sections were incubated with rabbit antihuman Nectin-4 antibody (1:1,500 dilution, Abcam) at 4°C overnight. After three washings in PBS, the sections were incubated with horseradish peroxidase-conjugated secondary antibody (Zhongshan Golden Bridge Biotechnology Inc) for 30 minutes. Being washed again, immunoreactivity was visualized using the diaminobenzidine and counterstained with hematoxylin. The primary antibody was replaced by PBS for negative control.
The evaluation of immunostaining of Nectin-4 protein was made blinded by two independent pathologists simultaneously. Based on a previously reported method,19 Nectin-4 staining was assessed as follows: scored as follows: negative (<5% positive cells, score 0); weak staining (5%–29%, score 1); moderate staining (30%–59%, score 2) and strong staining (over 60%, score 3). For statistical analysis, the data were binarized to create two groups, in which all positive scores (+1, +2, and +3) were grouped together and compared with the negatively scored tissues.
Statistical analysis
All statistical calculations were performed using the statistical package SPSS 16.0 (SPSS, Inc., Chicago, IL, USA). Continuous data were expressed as mean ± standard deviation (SD). Significant differences in the level of Nectin-4 expression using the independent Student’s t-test. Categorical variables were assessed using the χ2 test. The Kaplan–Meier method and the log-rank test were employed to determine the survival analysis. The Cox proportional hazards model was used to perform univariate and multivariate regression analyses of potential prognostic factors. Values of P<0.05 were considered to be statistically significant.
Results
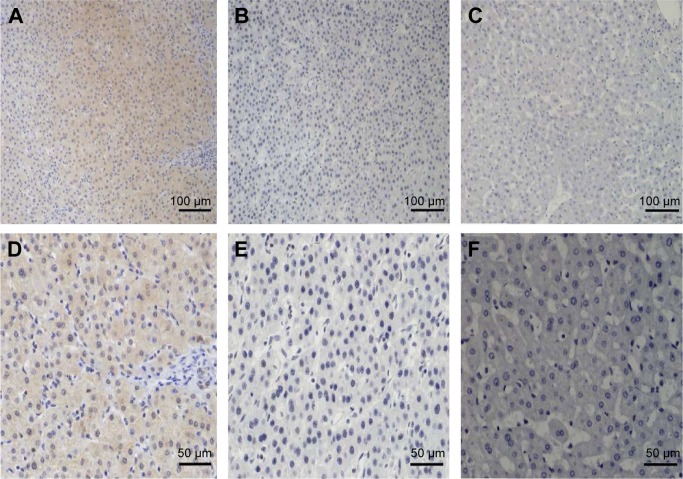
Expression of Nectin-4 mRNA in HCC tissues
To explore the expression of Nectin-4 in HCC, we first assessed the mRNA levels of Nectin-4 in a cohort of 20 patients with HCC with paired adjacent non-tumorous tissue by qRT-PCR. The data showed that the median Nectin-4 mRNA expression was significantly upregulated in tumor tissues compared to the adjacent non-tumor tissues (3.79±1.44 vs 2.15±0.81, P<0.05), and the positive rate was 70.0% (14/20) in tumor tissues (Figure 1).
Figure 1.
The expression of Nectin-4 mRNA in HCC tissues by qRT-PCR.
Notes: The mRNA expression level of Nectin-4 in 20 pairs of HCCs (filled squares) and adjacent non-tumorous tissues (filled circles) was examined by quantitative real-time PCR (qRT-PCR), **P<0.01.
Abbreviations: HCC, hepatocellular carcinoma; PCR, polymerase chain reaction; ANT, adjacent non-tumorous tissues; T, tumorous tissues.
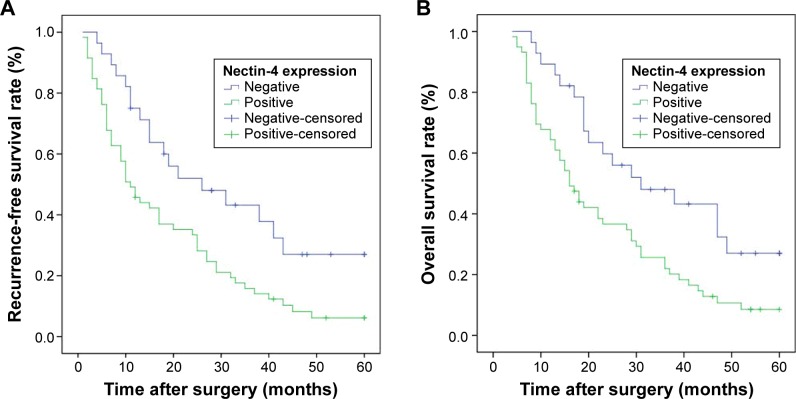
Expression of Nectin-4 protein in HCC tissues
To confirm Nectin-4 expression at the protein levels, the same 20 samples were measured by Western blot. The Nectin-4 protein was overexpressed in the HCC tissues (1.02±0.41), but was negative or low in adjacent non-tumor tissues (0.72±0.33) (P<0.05). Consistent with the present qRT-PCR results, the positive rate of Nectin-4 expression was observed in 65.0% (13/20) of tumor samples (P<0.05; Figure 2).
Figure 2.
The expression of Nectin-4 in tissues from HCC tumorous and adjacent non-tumorous tissues was analyzed by Western blotting.
Notes: (A) Representative images of Nectin-4 protein expression in paired HCC tumorous tissues (T) and the matched adjacent non-tumorous tissues (ANT) from five patients. The protein expression Nectin-4 was normalized to β-actin. (B) All the paired HCC tissues (filled squares) and the matched adjacent non-tumorous tissues (filled circles) from 20 patients; *P<0.05.
Abbreviation: HCC, hepatocellular carcinoma.
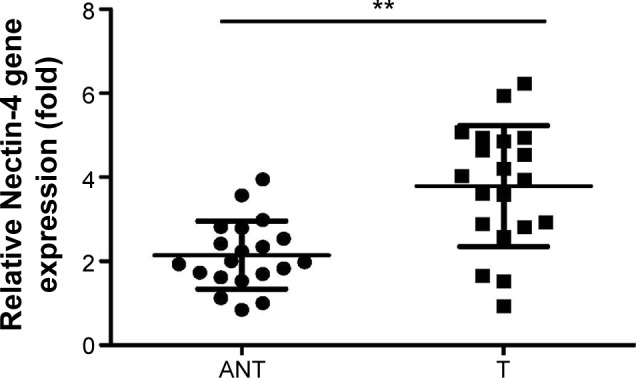
Nectin-4 expression in HCC and its relations to the clinicopathological features
The expression of Nectin-4 in 87 specimens with HCC was further investigated by immunohistochemical analysis. In adjacent non-tumor liver tissues, Nectin-4 protein staining was absent or only present in few cells. The expression of Nectin-4 was localized in the cytoplasm of tumor cells. The rate of Nectin-4 protein expression was 67.82% (59/87) in tumor tissues HCC. Representative images of immunohistochemistry are shown in Figure 3. The high Nectin-4 expression was significantly correlated with larger tumor size (P=0.029), status of metastasis (P=0.023), vascular invasion (P=0.018), and higher TNM stage (P=0.003). However, no significant associations were found between Nectin-4 expression and other clinical features, including sex, age, HbsAg status, liver cirrhosis, Child–Pugh grade, serum AFP, tumor capsula, and Edmondson grade (Table 1).
Figure 3.
Immunostaining of Nectin-4 in HCC tissues and adjacent non-tumor live tissues.
Notes: (A and D) high expression of Nectin-4 in HCC tissue cells; (B and E) negative expression of Nectin-4 in HCC tissue cells; (C and F) negative expression of Nectin-4 in adjacent non-tumor live tissue; original magnification was 200 for A–C and 400 for D–F.
Abbreviation: HCC, hepatocellular carcinoma.
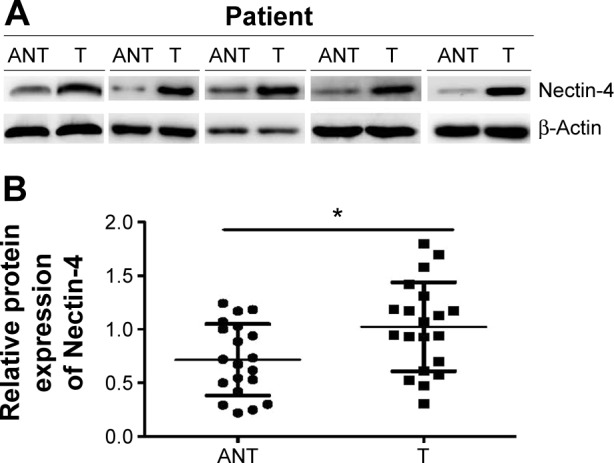
Relationship between Nectin-4 expression and prognosis
Kaplan–Meier curve (Figure 4) analysis by the log-rank test was performed to estimate the relationship between Nectin-4 expression and patient survival. The patients whose tumor scored positive for Nectin-4 expression had shorter RFS and OS than those that scored negative for Nectin-4 expression. The median RFS was 17.73 months (95% confidence interval [CI] 7.255–14.745) for patients whose tumors were Nectin-4 positive compared to 25.79 months (95% CI 8.125–43.875) for patients whose tumors were Nectin-4 negative (P=0.006). Likewise, the median OS was 21.92 months (95% CI 12.271–19.729) for patients with positive Nectin-4 expression, which was significantly shorter than 31.32 months (95% CI 11.681–50.319) in patients whose tumors were negative of Nectin-4 (P=0.005).
Figure 4.
Kaplan–Meier survival analysis of Nectin-4 expression in 87 HCC patients.
Notes: (A) positive expression of Nectin-4 was associated with worse recurrence-free survival (RFS) rate compared with negative expression (P=0.006). (B) Positive expression of Nectin-4 was associated with unfavorable overall survival (OS) rate compared with negative expression (P=0.005).
Abbreviation: HCC, hepatocellular carcinoma.
In order to estimate the prognostic factors of patients with HCC after surgical operation, univariate and multivariate analysis were performed for RFS and OS. In univariate analyses, both RFS and OS were correlated significantly with the status of metastasis, Edmondson grade, vascular invasion, TNM stage, as well as Nectin-4 expression. In addition, RFS was related to the tumor size and capsula status (Table 2). No significant correlations of either RFS or OS with the other clinicopathological variables were found (P>0.05). After elimination of the non-significant factors, the Cox regression multivariable analysis indicated that only positive Nectin-4 expression, status of metastasis, vascular invasion, and TNM stage were independent prognostic factors for both RFS and OS in HCC, and tumor size for RFS (Table 3).
Table 2.
Univariate analysis of factors associated with RFS and OS
| Variables | RFS
|
OS
|
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| Sex (female vs male) | 1.141 | 0.662–1.966 | 0.635 | 1.208 | 0.691–2.111 | 0.507 |
| Age (years) (≤50 vs >50) | 0.800 | 0.498–1.283 | 0.354 | 0.860 | 0.534–1.386 | 0.537 |
| HBsAg (negative vs positive) | 1.570 | 0.933–2.643 | 0.089 | 1.476 | 0.875–2.490 | 0.144 |
| Liver cirrhosis (absent vs present) | 0.884 | 0.484–1.614 | 0.688 | 0.848 | 0.464–1.551 | 0.593 |
| Child–Pugh grade (A vs B) | 0.175 | 0.360–1.204 | 0.658 | 0.695 | 0.379–1.273 | 0.238 |
| AFP (ng/mL) (≤20 vs >20) | 1.548 | 0.943–2.542 | 0.084 | 1.550 | 0.939–2.559 | 0.087 |
| Tumor size (cm) (≤5.0 vs >5.0) | 1.653 | 1.015–2.694 | 0.044 | 1.635 | 0.996–2.684 | 0.052 |
| Status of metastasis (absent vs present) | 1.746 | 1.076–2.832 | 0.024 | 1.770 | 1.086–2.884 | 0.022 |
| Tumor capsula (none vs complete) | 1.688 | 1.058–2.693 | 0.028 | 1.559 | 0.973–2.501 | 0.065 |
| Edmondson grade (I–II vs III–IV) | 1.810 | 1.132–2.895 | 0.013 | 1.800 | 1.118–2.897 | 0.016 |
| Vascular invasion (present vs absent) | 3.221 | 1.948–5.327 | 0.000 | 3.027 | 1.828–5.011 | 0.000 |
| TNM stage (I–II vs III–IV) | 3.154 | 1.907–5.214 | 0.000 | 2.942 | 1.789–4.839 | 0.000 |
| Nectin-4 expression (negative vs positive) | 2.054 | 1.202–3.507 | 0.008 | 2.085 | 1.216–3.574 | 0.008 |
Abbreviations: AFP, α-fetoprotein; CI, confidence interval; HBsAg, hepatitis B surface antigen; HR, hazard ratio; OS, overall survival; RFS, recurrence-free survival; TNM, tumor-node-metastasis.
Table 3.
Multivariate analysis of factors associated with RFS and OS
| Variables | RFS
|
OS
|
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| Tumor size (cm) (≤5.0 vs >5.0) | 1.994 | 1.182–3.367 | 0.010 | |||
| Status of metastasis (absent vs present) | 2.343 | 1.370–4.006 | 0.002 | 2.471 | 1.462–4.177 | 0.001 |
| Tumor capsula (complete vs none) | 1.568 | 0.943–2.605 | 0.083 | |||
| Edmondson grade (I–II vs III–IV) | 1.328 | 0.787–2.239 | 0.288 | 1.138 | 0.675–1.918 | 0.628 |
| Vascular invasion (present vs absent) | 2.539 | 1.339–4.815 | 0.004 | 2.276 | 1.202–4.308 | 0.012 |
| TNM stage (I–II vs III–IV) | 2.098 | 1.135–3.880 | 0.018 | 1.924 | 1.027–3.605 | 0.041 |
| Nectin-4 expression (negative vs positive) | 2.731 | 1.490–5.005 | 0.001 | 2.258 | 1.271–4.009 | 0.005 |
Abbreviations: CI, confidence interval; HR, hazard ratio; OS, overall survival; RFS, recurrence-free survival; TNM, tumor-node-metastasis.
Discussion
Nectin-4, known as the poliovirus receptor-related 4 (PVRL4), is a member of the Nectin family that belongs to cell adhesion molecules.23 Recently, Nectin-4 has been found to play a pivotal role in regulating adherence functions of epithelial cells in ectodermal organogenesis.5,10 In mouse normal tissues, the Nectin-4 is detected in skin, hair follicles, and cultured keratinocytes, and its expression become lower with the increasing of the keratinization.24 In humans, Brancati et al25 found that abnormal Nectin-4 expression was implicated in ectodermal dysplasia-syndactyly syndrome and lost its adhesive capacity in patient’s keratinocytes.
As an embryonic protein, the Nectin-4 has been reported to be a tumor-associated antigen in breast, lung, ovarian, colon, and pancreatic cancers.15–20 Fabre-Lafay et al15 reported that positive expression of Nectin-4 was 61% in ductal breast carcinoma and 6% in lobular type, and was closely related to tumor histological type. In another report, Athanassiadou et al16 found that a similar proportion of Nectin-4 positive expression was 63.5% in all breast carcinoma, but positive expression of Nectin-4 did not reveal any difference in all tumor histological types. Furthermore, their immunohistochemical analysis showed that the high expression of Nectin-4 was strongly associated with larger tumor size, increased tumor grade, increased lymph nodes infiltration and worse survival. In ovarian cancer, Derycke et al17 found that the Nectin-4 positive expression was 48.6% of all tumor tissues, and had a greater percentage in the low-grade tumors, but did not relate to RFS and OS. Meanwhile, Takano et al18 found that the expression of Nectin-4 was strongly associated with poor prognosis in non-small cell lung cancer, and its expression increased the formation of lamellipodia and the invasion ability of tumor cell through the activation of small GTPase Rac1, and further using small interfering RNAs against Nectin-4 could suppress its expression and tumor cell proliferation. In pancreatic cancer, Izumi et al19 found that high expression of Nectin-4 was related to larger tumor size, but did not to the patients’ prognosis.
Based on earlier studies, we first assessed the expression of Nectin-4 in HCC tissues at the mRNA and protein levels in paired frozen HCC tissue samples. Our results showed that the expression of Nectin-4 was significantly higher in HCC tissues than their matched adjacent non-tumor tissues. Moreover, through immunohistochemical staining, we found that the increased expression of Nectin-4 was related to numerous unfavorable characteristics of HCC, including larger tumor size, status of metastasis, vascular invasion, and advanced TNM stage. In this study, patients with high expression of Nectin-4 had a significantly shorter RFS and OS than those with low Nectin-4 expression by Kaplan–Meier analysis. Furthermore, multivariate analysis indicated that Nectin-4 was an independent prognostic factor for patients with HCC after surgical operation. Hence, the current findings suggest that Nectin-4 may play a crucial role in tumorigenesis and progression of HCC.
It is possible that Nectin-4 may have effect on the tumor malignant behaviors of HCC via interaction of nectin-afadin complex, which could activate the phosphoinositide 3-kinase (PI3K)–AKT signaling pathway, and eventually lead to cell survival enhancement and apoptosis resistance.26 Loss of afadin induces cell proliferation, invasion, and migration, and is associated with poor prognosis in breast, colon, and endometrial cancers.27–30 Furthermore, phosphorylation of afadin by the PI3K-AKT pathway plays a key role in controlling increasing cell migration in breast cancer.31 As previously reported, the PI3K–AKT pathway was involved in promoting tumor cell growth, proliferation and resistance to drug in HCC.32,33 Derycke et al17 found that Nectin-4 increased the survival of drug resistance spheroids of ovarian cancer cells. In colon cancer, Das et al20 demonstrated that increased expression of Nectin-4 was observed in 5-fluorouracil(FU)-resistant and 5-FU-exposed cells, and the significant increase in the tumor cell proliferation, migration, colony-formation and resistant to 5-FU were noted in 5-FU-resistant cells, but reverse was found after silencing of Nectin-4. Additionally, their results showed that Nectin-4 could deregulate afadin, which result in upregulation of the AKT–NF-κB pathway in colon cancer cells. Given the association between Nectin-4 expression and HCC, therefore, the underlying mechanism between the Nectin-4 expression and the AKT–NF-κB pathway in HCC might be exist and is worthy of further research.
Conclusion
This study demonstrated that Nectin-4 was overexpressed in HCC. High level of Nectin-4 expression in HCC samples was associated with poor prognosis and was an independent prognostic marker for patients with HCC after surgical resection. Therefore, the present results showed that Nectin-4 may be a new prognostic biomarker for HCC and may provide a novel therapeutic target for treating this disease.
Acknowledgments
This work was supported by the Anhui Provincial Natural Science Foundation (No 1408085MKL71) and Anhui science and technology platform construction plan (No 1206c0805035). We are grateful to two pathologists Ke Chen and Hangcheng Zhou for their excellent professional support.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Carr BI. Hepatocellular carcinoma: current management and future trends. Gastroenterology. 2004;127(5 Suppl 1):S218–S224. doi: 10.1053/j.gastro.2004.09.036. [DOI] [PubMed] [Google Scholar]
- 3.Fan ST, Mau Lo C, Poon RT, et al. Continuous improvement of survival outcomes of resection of hepatocellular carcinoma: a 20-year experience. Ann Surg. 2011;253(4):745–758. doi: 10.1097/SLA.0b013e3182111195. [DOI] [PubMed] [Google Scholar]
- 4.Mazzaferro V, Llovet JM, Miceli R, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10(1):35–43. doi: 10.1016/S1470-2045(08)70284-5. [DOI] [PubMed] [Google Scholar]
- 5.Reymond N, Fabre S, Lecocq E, Adelaïde J, Dubreuil P, Lopez M. Nectin4/PRR4, a new afadin-associated member of the nectin family that trans-interacts with nectin1/PRR1 through V domain interaction. J Biol Chem. 2001;276(46):43205–43215. doi: 10.1074/jbc.M103810200. [DOI] [PubMed] [Google Scholar]
- 6.Yasumi M, Shimizu K, Honda T, Takeuchi M, Takai Y. Role of each immunoglobulin-like loop of nectin for its cell-cell adhesion activity. Biochem Biophys Res Commun. 2003;302(1):61–66. doi: 10.1016/s0006-291x(03)00106-2. [DOI] [PubMed] [Google Scholar]
- 7.Nakanishi H, Takai Y. Roles of nectins in cell adhesion, migration and polarization. Biol Chem. 2004;385(10):885–892. doi: 10.1515/BC.2004.116. [DOI] [PubMed] [Google Scholar]
- 8.Takai Y, Miyoshi J, Ikeda W, Ogita H. Nectins and nectin-like molecules: roles in contact inhibition of cell movement and proliferation. Nat Rev Mol Cell Biol. 2008;9(8):603–615. doi: 10.1038/nrm2457. [DOI] [PubMed] [Google Scholar]
- 9.Sakisaka T, Ikeda W, Ogita H, Fujita N, Takai Y. The roles of nectins in cell adhesions: cooperation with other cell adhesion molecules and growth factor receptors. Curr Opin Cell Biol. 2007;19(5):593–602. doi: 10.1016/j.ceb.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Fabre S, Reymond N, Cocchi F, et al. Prominent role of the Ig-like V domain in trans-interactions of nectins. Nectin 3 and nectin 4 bind to the predicted C-C′-C″-D beta-strands of the nectin1 V domain. J Biol Chem. 2002;277(30):27006–27013. doi: 10.1074/jbc.M203228200. [DOI] [PubMed] [Google Scholar]
- 11.Sakisaka T, Takai Y. Biology and pathology of nectins and nectin-like molecules. Curr Opin Cell Biol. 2004;16(5):513–521. doi: 10.1016/j.ceb.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 12.Takahashi K, Nakanishi H, Miyahara M, et al. Nectin/PRR: an immunoglobulin-like cell adhesion molecule recruited to cadherin-based adherens junctions through interaction with Afadin, a PDZ domain-containing protein. J Cell Biol. 1999;145(3):539–549. doi: 10.1083/jcb.145.3.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reymond N, Borg J-P, Lecocq E, et al. Human nectin3/PRR3: a novel member of the PVR/PRR/nectin family that interacts with afadin. Gene. 2000;255:347–355. doi: 10.1016/s0378-1119(00)00316-4. [DOI] [PubMed] [Google Scholar]
- 14.Takai Y, Ikeda W, Ogita H, Rikitake Y. The immunoglobulin-like cell adhesion molecule nectin and its associated protein afadin. Annu Rev Cell Dev Biol. 2008;24:309–342. doi: 10.1146/annurev.cellbio.24.110707.175339. [DOI] [PubMed] [Google Scholar]
- 15.Fabre-Lafay S, Monville F, Garrido-Urbani S, et al. Nectin-4 is a new histological and serological tumor associated marker for breast cancer. BMC Cancer. 2007;7:73. doi: 10.1186/1471-2407-7-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Athanassiadou AM, Patsouris E, Tsipis A, Gonidi M, Athanassiadou P. The significance of Survivin and Nectin-4 expression in the prognosis of breast carcinoma. Folia Histochem Cytobiol. 2011;49(1):26–33. doi: 10.5603/fhc.2011.0005. [DOI] [PubMed] [Google Scholar]
- 17.Derycke MS, Pambuccian SE, Gilks CB, et al. Nectin 4 overexpression in ovarian cancer tissues and serum: potential role as a serum biomarker. Am J Clin Pathol. 2010;134(5):835–845. doi: 10.1309/AJCPGXK0FR4MHIHB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Takano A, Ishikawa N, Nishino R, et al. Identification of nectin-4 oncoprotein as a diagnostic and therapeutic target for lung cancer. Cancer Res. 2009;69(16):6694–6703. doi: 10.1158/0008-5472.CAN-09-0016. [DOI] [PubMed] [Google Scholar]
- 19.Izumi H, Hirabayashi K, Nakamura N, Nakagohri T. Nectin expression in pancreatic adenocarcinoma: nectin-3 is associated with a poor prognosis. Surg Today. 2015;45(4):487–494. doi: 10.1007/s00595-015-1126-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Das D, Satapathy SR, Siddharth S, Nayak A, Kundu CN. NECTIN-4 increased the 5-FU resistance in colon cancer cells by inducing the PI3K-AKT cascade. Cancer Chemother Pharmacol. 2015;76(3):471–479. doi: 10.1007/s00280-015-2794-8. [DOI] [PubMed] [Google Scholar]
- 21.Edmondson HA, Steiner PE. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer. 1954;7(3):462–503. doi: 10.1002/1097-0142(195405)7:3<462::aid-cncr2820070308>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 22.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25(4):402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 23.Samanta D, Almo SC. Nectin family of cell-adhesion molecules: structural and molecular aspects of function and specificity. Cell Mol Life Sci. 2015;72(4):645–658. doi: 10.1007/s00018-014-1763-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Okabe N, Ozaki-Kuroda K, Nakanishi H, Shimizu K, Takai Y. Expression patterns of nectins and afadin during epithelial remodeling in the mouse embryo. Dev Dyn. 2004;230(1):174–186. doi: 10.1002/dvdy.20033. [DOI] [PubMed] [Google Scholar]
- 25.Brancati F, Fortugno P, Bottillo I, et al. Mutations in PVRL4, encoding cell adhesion molecule nectin-4, cause ectodermal dysplasia-syndactyly syndrome. Am J Hum Genet. 2010;87(2):265–473. doi: 10.1016/j.ajhg.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kanzaki N, Ogita H, Komura H, et al. Involvement of the nectin-afadin complex in PDGF-induced cell survival. J Cell Sci. 2008;121(Pt 12):2008–2017. doi: 10.1242/jcs.024620. [DOI] [PubMed] [Google Scholar]
- 27.Letessier A, Garrido-Urbani S, Ginestier C, et al. Correlated break at PARK2/FRA6E and loss of AF-6/Afadin protein expression are associated with poor outcome in breast cancer. Oncogene. 2007;26(2):298–307. doi: 10.1038/sj.onc.1209772. [DOI] [PubMed] [Google Scholar]
- 28.Fournier G, Cabaud O, Josselin E, et al. Lossof AF6/afadin, a marker of poor outcome in breast cancer, induces cell migration, invasiveness and tumor growth. Oncogene. 2011;30(36):3862–3874. doi: 10.1038/onc.2011.106. [DOI] [PubMed] [Google Scholar]
- 29.Sun TT, Wang Y, Cheng H, et al. Disrupted interaction between CFTR and AF-6/afadin aggravates malignant phenotypes of colon cancer. Biochim Biophys Acta. 2013;1843(3):618–628. doi: 10.1016/j.bbamcr.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 30.Yamamoto T, Mori T, Sawada M, et al. Loss of AF-6/afadin induces cell invasion, suppresses the formation of glandular structures and might be a predictive marker of resistance to chemotherapy in endometrial cancer. BMC Cancer. 2015;15:275. doi: 10.1186/s12885-015-1286-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elloul S, Kedrin D, Knoblauch NW, Beck AH, Toker A. The adherens junction protein afadin is an AKT substrate that regulates breast cancer cell migration. Mol Cancer Res. 2014;12(3):464–476. doi: 10.1158/1541-7786.MCR-13-0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou Q, Lui VW, Yeo W. Targeting the PI3K/Akt/mTOR pathway in hepatocellular carcinoma. Future Oncol. 2011;7(10):1149–1167. doi: 10.2217/fon.11.95. [DOI] [PubMed] [Google Scholar]
- 33.Brown KK, Toker A. The phosphoinositide 3-kinase pathway and therapy resistance in cancer. F1000Prime Rep. 2015;7:13. doi: 10.12703/P7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]