Abstract
Male circumcision (MC) reduces the risk of HIV and other sexually transmitted infections (STIs), including human papillomavirus (HPV) and herpes simplex virus type 2 (HSV-2), and is recommended as an important component of a comprehensive package of HIV prevention interventions. While computer modeling has demonstrated that substantial reductions in HIV could be achieved with rapid scale-up of MC services in sub-Saharan Africa, scale-up has lagged due to scarcity of trained providers coupled with relative technical difficulty of recommended surgical MC techniques. Simplified techniques, such as devices, have the potential to allow for a more rapid roll-out of MC. One such device is the Shang Ring, a novel disposable MC device that eliminates the need for suturing and has been on the Chinese market since 2005. Results from Chinese studies have demonstrated that the Shang Ring is both safe and easy to use. Since 2008, a series of studies using the Shang Ring for adult MC have been carried out in Kenya, Uganda and Zambia, according to guidelines established by World Health Organization (WHO) for clinical evaluation of new devices for adult MC. These include a proof of concept study, a study of delayed removal of the Shang Ring, two studies comparing Shang Ring circumcision to conventional surgical approaches, and a large field trial to evaluate safety of Shang Ring circumcision during routine service delivery. Results from these studies demonstrate that the Shang Ring has an excellent safety profile and that Shang Ring circumcision is relatively easy to teach and learn, making Shang Ring MC an appealing technique for use in sub-Saharan Africa where doctors are in short supply and non-physician providers such as nurses and clinical officers are playing a major role in providing MC through task shifting. Shang Ring MC and device removals were uneventfully performed by trained nurses and clinical officers, who preferred the Shang Ring to conventional surgical techniques. Adverse event rates were similar to those observed with conventional surgical circumcision and were managed with, at most, minor interventions, resolving with no long-term sequale. Perhaps one of the biggest advantages of the Shang Ring is the relatively short 3-6 minutes procedure time. Importantly, men also preferred the Shang Ring compared to conventional circumcision and satisfaction with cosmetic appearance of their circumcised penis was very high. The vast majority of participants in studies in Africa as well as China have reported few problems and little disruption to daily life while wearing the device. The Shang Ring holds great promise as an innovative technology that has the potential to facilitate the safe and effective scale-up of circumcision services in settings where MC is not widely used and where the burden of HIV-disease is high.
Keywords: HIV prevention, male circumcision (MC), Shang Ring
Introduction
According to the most recent estimates, approximately 35.3 million people are living with HIV worldwide, with 2.3 million new infections having occurred around the world in 2012 (1), which has seriously affected public health priorities worldwide. Sub-Saharan Africa—the region hit hardest by the pandemic—accounted for 70% of all new HIV infections in 2012 (1). Other STIs, while generally less life threatening, also cause substantial morbidity and in fact outnumber HIV infection in terms of incidence and prevalence. For example, in 2008, there were an estimated 499 million new cases of curable STIs (Chlamydia trachomatis, Neisseria gonorrhoeae, syphilis, and Trichomonas vaginalis) in adults between 15 and 49 years old (2).
MC reduces HIV infection
Male circumcision (MC) is the only HIV prevention method that has been shown in clinical studies to consistently reduce the risk of HIV transmission (3,4). Three large randomized controlled trials (RCT) conducted in Kenya, Uganda and South Africa by independent research groups—together encompassing nearly 10,000 men—demonstrated that MC dramatically reduces the risk of men acquiring HIV by approximately 60% during penovaginal intercourse (5-9). Long-term follow-up data from Uganda have shown that the reductions in HIV acquisition due to MC are sustained for at least 5 years (10); similar data from Kenya have shown protection persists for at least 4.5 years (11). On a population level, roll-out of adult MC services in the Orange Farm region of South Africa has been shown to have led to significant reductions in HIV incidence among circumcised men (12).
MC reduces other STIs, including human papillomavirus (HPV) and herpes simplex virus type 2 (HSV-2)
MC also provides protection against transmission of other STIs, making men less susceptible to acquiring or transmitting genital ulcer disease, trichomonas and gonorrhea (8,13-16). Data also show that MC provides significant protection against both HPV and HSV-2, reducing the risk of infection by about one-third for both viruses (13,17-19), in addition to reducing the risk of cervical cancer in female sex partners of circumcised men (20-22).
The current strategies and policies of WHO and UNAIDS
The World Health Organization (WHO) and the Joint United Nations Programme on HIV/AIDS (UNAIDS) strongly recommend that countries with low rates of MC, high HIV prevalence, and generalized predominantly heterosexual HIV epidemics consider scaling-up MC as one important component of a comprehensive package of HIV prevention interventions (23). Following these recommendations, thirteen priority countries in eastern and southern Africa have established national MC programs including completion of a situational analysis; identification of prominent national champion to promote and support MC for HIV prevention; appointment of a dedicated focal person within the national government to coordinate MC activities; development of appropriate national strategies, policies and guidelines; and establishment of quality MC services (24).
Computer modeling has demonstrated that substantial reductions in HIV incidence and prevalence could be achieved with rapid scale-up of MC services in countries with generalized epidemics (25-28). Models have estimated that over 20 million adult MCs must be performed between 2011 and 2015 in order to achieve 80% coverage in the 13 high priority countries in sub-Saharan Africa. Additionally, over 8 million additional adult male circumcisions would need to be performed between 2016 and 2025 to maintain the 80% coverage beyond that time (29).
The current challenges for MC programs in Africa
Various issues have delayed the rapid scale-up of MC services in priority countries in sub-Saharan Africa, including the scarcity of trained providers coupled with relative technical difficulty of MC, need for suturing, risk of bleeding, and time required to complete the techniques recommended by WHO and UNAIDS. Task shifting to mid-level providers (e.g., clinical officers and nurses) is being employed to increase access to MC services in many of the priority countries, addressing some of the human resource constraints to scale-up (24). The recommended surgical approaches typically require 20-40 minutes with suturing (30-32). Simplified techniques for MC, such as devices, have the potential to allow for a more rapid roll-out of MC (33).
The Shang Ring circumcision device
The Shang Ring (Wu Hu SNNDA Medical Treatment Appliance Technology Co., LTD., Wu Hu City, China), a novel disposable MC device invented by Mr. Jianzhong Shang in China, has been on the Chinese market since 2005. It is commercially available in China in 32 sizes, ranging from 9-42 mm in diameter, for use with neonates to adults. The Shang Ring consists of two parts, an inner ring and an outer ring (Figure 1). The inner ring has a shallow groove on its outer surface that is lined by a silicone band which confers a non-bioreactive surface against which the outer ring sandwiches the foreskin. The outer ring consists of two halves that are hinged together at one end. The outer ring is closed securely via a ratchet style closure. Hemostasis provided by the locking rings minimizes bleeding and removes the need for sutures.
Figure 1.
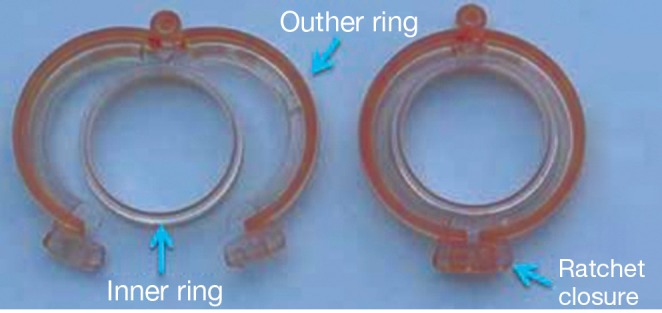
The Shang Ring male is a sterile, single use, disposable male circumcision device that consists of two concentric plastic rings, the inner of which is lined by a silicone pad. The outer ring consists of two halves that are hinged together at one end with a ratchet closure. Hemostasis is realized by the pressure applied by the interlocking rings which minimizes bleeding and eliminates the need for sutures.
The Shang Ring has been safely used for MC in more than 600,000 males in China since 2005. Over 3,000 men have participated in clinical studies in China and Africa between 2007 and 2013. The device has a CE mark, which allows the Shang Ring to be sold and used in the European Union, has received clearance by the U.S. Food and Drug Administration for sale and use in the United States, and is currently under consideration for prequalification by WHO (34).
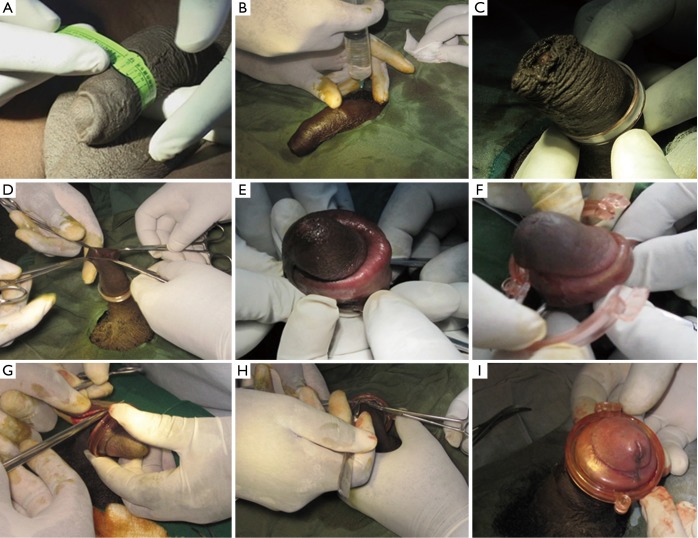
Details of use of the Shang Ring for adult MC, which have been reported elsewhere, are summarized below and shown in Figures 2 and 3 (35,36). The appropriate Shang Ring size is determined before the surgical scrub, using a special measuring tape (Figure 2A). Following a standard surgical scrub and administration of local anesthesia (Figure 2B), the inner ring is placed on the penis at the level of the coronal sulcus (Figure 2C,D). The foreskin is then everted over the inner ring (Figure 2E). The outer ring is secured over the inner ring sandwiching the foreskin in-between the two rings (Figure 2F). Excess foreskin is excised using surgical scissors (Figure 2G), and 8 to 10 nicks are made on the incision using a scalpel blade (Figure 2H,I). These slits are necessary to allow the skin to expand as healing occurs. The ring is removed seven days after circumcision.
Figure 2.
The Shang Ring circumcision procedure: (A) measure the penis to determine which size device to use; (B) administer local anesthesia after preparing the site with antiseptic; (C) place the inner ring onto the penis at the level of the coronal sulcus; (D) grasp the edges of the foreskin with clamps; (E) flip the foreskin over the inner ring; (F) place the out ring over the inner ring, with the foreskin in-between; (G) cut the foreskin on the underside of the device using scissors; (H) make 8-10 slices in the foreskin on the underside of the ring using a scalpel blade. These slits are necessary to allow the skin to spread as healing occurs and to allow for ‘expansion’ of the scab during an erection; (I) the completed procedure. The device remains in place for seven days.
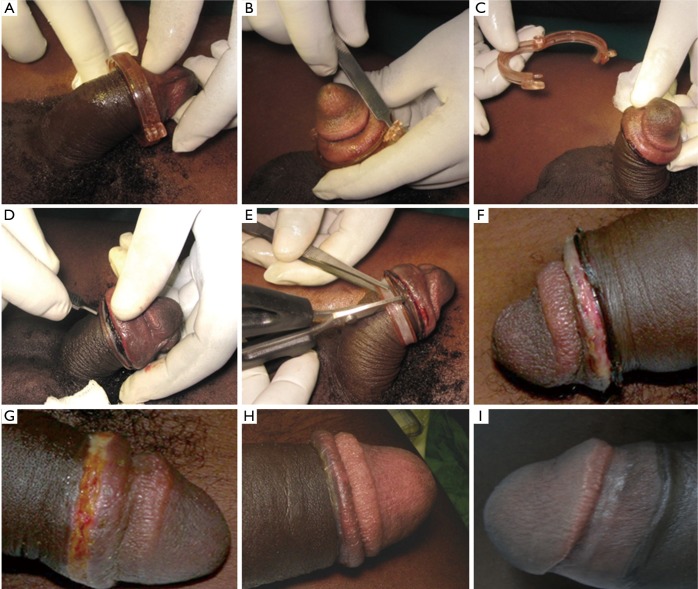
Figure 3.
Removal of the Shang Ring and healing of the penis: (A) seven days after the procedure; (B) open the outer ring; (C) remove the outer ring; (D) carefully pull back the inner ring from the wound edge; (E) cut the inner ring in two places with the special scissors and remove; (F) after ring has been removed on day 7 post-circumcision; (G) day 14 post-circumcision showing normal healing; (H) day 28 post-circumcision showing normal healing; (I) completely healed at day 42 post-circumcision.
Removal involves breaking the ratchet closure of the outer ring using the Shang Ring opener and removing it (Figure 3B,C), carefully pulling the inner ring back from the edge of the wound (Figure 3D), and cutting the inner ring at the 3 and 9 o’clock positions using blunt end scissors (Figure 3E). The wound should be covered with a bandage, and men instructed to remove the bandage after 24 hours, keeping the wound clean and dry thereafter.
Shang Ring clinical studies in China
Results from Chinese studies have demonstrated that the Shang Ring is both safe and easy to use. The first report of the Shang Ring in the literature was from a study conducted by Peng et al. who reported low rates of complication among 1,200 Shang Ring circumcisions (37). Similarly low complication rates were seen in a series of 328 men circumcised with the Shang Ring in another Chinese study by Cheng et al. (38). A third study by Li et al. conducted in China comparing Shang Ring circumcision with the dorsal slit technique found significantly fewer complications, lower pain levels during and after the procedure, and higher participant satisfaction among participants circumcised with the Shang Ring (30). Average Shang Ring circumcision times (excluding administration of local anesthesia), were reported in the Chinese studies to be between 3-5 minutes with patient satisfaction rates over 98% (30,37,38).
Shang Ring clinical studies in Africa
Since 2008, a series of studies using the Shang Ring for adult MC have been carried out in Africa (Table 1), according to guidelines established by WHO for clinical evaluation of new devices for adult MC (44). These guidelines outline a series of studies that include: (I) a case series to provide preliminary information on ease of use and device performance; (II) a randomized study comparing the device to WHO-recommended conventional MC methods; and (III) a field trail that is a non-comparative study of the device under more usual service delivery conditions.
Table 1. Shang Ring clinical studies in Africa (34).
| Study [type of study] | Location | Number and type of participants | Type of provider |
|---|---|---|---|
| Safety Study in Kenya [case series] (39) | Homa Bay District Hospital, Kenya | 40 healthy HIV-negative men | Physicians and nurses experienced in conventional surgical circumcision and trained in China to conduct Shang Ring circumcisions |
| Spontaneous detachment Study in Kenya [comparative trial] (40) | Homa Bay District Hospital, Kenya | 50 healthy HIV-negative men | Physicians and nurses experienced in conventional surgical circumcision and trained in China to conduct Shang Ring circumcisions |
| Randomized comparison with Conventional Surgical Circumcision in Kenya and Zambia [comparative trial] (41) | Homa Bay District Hospital, Homa Bay Kenya and University Teaching Hospital, Lusaka, Zambia | 400 healthy HIV-negative men (200 allocated to Shang Ring circumcision and 200 to conventional surgical circumcision) | Physicians, nurses and clinical officers experienced in conventional surgical circumcision and trained in China to conduct Shang Ring circumcisions |
| Field studies in Kenya and Zambia [field studies] (42) | Seven sites in Homa Bay, Kenya and three sites in Lusaka, Zambia | 1,211 healthy HIV-negative and HIV positive men | Physicians, nurses and clinical officers experienced in conventional surgical circumcision who were either trained in China or trained locally by those trained in China to conduct Shang Ring circumcisions |
| Acceptability and safety in Uganda [field study] (43) | Rakai Health Sciences Programme, Rakai District, Uganda | 621 health HIV-negative men (508 chose Shang Ring circumcision and 113 chose conventional surgical circumcision) | Clinical officers experienced in conventional surgical circumcision and trained in Kenya to conduct Shang Ring circumcisions |
Adapted from, WHO Technical Advisory Group on Innovations in Male Circumcision: Evaluation of Two Adult Devices. Meeting report. Geneva, Switzerland 2013. (Table 4, page 26. http://apps.who.int/iris/bitstream/10665/85269/1/9789241505635_eng.pdf). Reproduced with permission from the publisher.
Proof of concept study
The first use of the Shang Ring outside of China was a proof of concept study conducted in 2009 assessing the safety, preliminary efficacy, and acceptability of the Shang Ring in Kenya (39). HIV-negative men aged 18 to 54 years seeking MC at the Homa Bay District Hospital in Kenya were recruited for the study. Circumcisions were performed by a physician or nurse working with another physician or nurse as an assistant; all had received training on the Shang Ring technique and postsurgical management in China. Study participants were asked to return for follow-up on days 2, 7, 9, 14, 21, 28, 35, and 42 after circumcision. Pain was assessed at various time points using a visual analog scale (VAS) (0, no pain; 10, worst possible).
Forty men were recruited all of whom successfully underwent Shang Ring circumcision. Four participants (10%) required a small (mean 8 mm) slit in the foreskin to allow for eversion of the foreskin due to phimosis. Mean Shang Ring circumcision procedure time, excluding administration of local anesthesia, was 4.8 minutes (SD ±2.0). Men reported minimal disruption to their lives with the Shang Ring in place, and none requested early ring removal. Erections with the ring in place were well tolerated by study participants; mean pain score 3.5 (SD ±2.3). Shang Rings were removed on day 7 without major problems, with a mean removal time of 3.9 minutes (SD ±2.6). The mean pain score during Shang Ring removal was 4.9 (SD ±2.5), although this decreased to 2.2 (SD ±1.8) once the removal was completed.
There were no moderate or severe adverse events, although there were three minor cutaneous injuries of the skin of the penis; similar injuries had not been reported in China. Mean time from circumcision to complete healing was 28.9 days. All participants reported at the 42-day post-circumcision interview that they were very satisfied, happy with the appearance of their circumcised penis, and would recommend Shang Ring circumcision to others. These results showed that the Shang Ring was safe for further study in Africa.
Study of delayed removal of the Shang Ring
A small RCT was conducted in Kenya to explore what would happen if men did not return for Shang Ring removal and determine if the Shang Ring would spontaneously detach if removal was delayed beyond the current label instructions of seven days (40). Fifty HIV-negative men seeking MC at the Homa Bay District Hospital were randomly assigned to device removal at 7, 14 or 21 days after Shang Ring circumcision. Scheduled follow-up visits were at 7, 14, 21, 28, and 42 days after circumcision, as well as 2 days after Shang Ring removal. Clinical outcome measures included adverse events, degree of detachment, and time to complete healing.
Shang Ring circumcisions in all 50 men were successfully completed without complications. Nine (18.0%) men required a small slit (median 15 mm) in the foreskin to facilitate eversion of the foreskin over the inner ring. Complete detachment of the Shang Ring occurred in 22 men (66.7% of those wearing the ring >7 days); most (81.8%, 18/22) of these complete detachments occurred between 10 and 16 days after circumcision. In some men experiencing complete detachment, the ring fell off the penis, while in others it slid back towards the base of the penis and was removed by a provider at follow-up. Among men still wearing the device on the day of planned removal, the cumulative probability of at least partial detachment was 26.0%, 94.1%, and 100.0% on days 7, 14, and 21, respectively. Cumulative probabilities of complete spontaneous detachment were 0.0%, 56.1%, and 93.7% at 7, 14, and 21 days, respectively.
A total of seven men in 14- and 21-day groups requested early ring removal due to pain/discomfort from the partially detached ring contacting the healing wound. Rings were removed as requested and healing proceeded normally. There were six moderate AEs including three that were pain related (one postoperatively and two approximately one week after circumcision) and three wound disruptions. Four of the six AEs were among the men who requested early ring removal. Although not considered moderate or severe AEs, there were nine instances of the minor cutaneous injuries to the penile shaft similar to what was seen in the proof of concept study noted above. Based on the location of the injuries and the experiences of the circumcision providers, study investigators hypothesized that these injuries occurred when a small fold of skin from the penis was trapped between the inner and outer rings as the outer ring was closed during the circumcision procedure.
No significant differences (P=0.86) in cumulative probability of compete healing were seen by randomization group. Overall, the cumulative probability of complete healing by 42 days was 94.5%. There were no problems with healing and excellent cosmetic results among the 46 men in which complete wound healing was observed, irrespective of presence of an AE, day device was removed, occurrence of spontaneous detachment, or request for early removal.
Studies comparing Shang Ring and conventional circumcision
Two studies conducted in Africa have compared Shang Ring circumcision to conventional surgical approaches (41,43).
RCT in Kenya and Zambia
An RCT enrolled HIV-negative men 18 to 54 years old who were seeking MC in Homa Bay, Kenya, and Lusaka, Zambia (41). Men were randomized to Shang Ring or conventional circumcision (forceps-guided method in Kenya and dorsal slit method in Zambia). Shang Rings were removed at the 7-day visit. Outcomes measures included: (I) safety (e.g., adverse events rates, time to complete wound healing by clinical assessment); (II) pain and acceptability among study participants (e.g., post-operative pain using a VAS, participant acceptability); and (III) ease of use and provider preferences (e.g., duration of surgery, surgical difficulties, provider preferences).
A total of 400 men were enrolled and randomized, 200 at each site with 197 and 201 contributed to the Shang Ring and conventional surgery analyses, respectively. Over 80% of the procedures in both arms were performed by nurses or clinical officers. Results are summarized in Table 2.
Table 2. Summary of results of a randomized controlled trial of the Shang Ring vs. conventional male circumcision in Kenya and Zambia (41).
| Shang Ring circumcision | Conventional circumcision | |
|---|---|---|
| Adverse events (moderate and severe) | 15/197 (7.6%) | 10/201 (5.0%) |
| Mean ± SD day to healed* | 44.1±12.6 | 38.9±12.6 |
| Pain with erection during first 7 days after circumcision (mean ± SD)*; (0, none; 10, worst possible) | 3.5±1.9 | 2.3±1.7 |
| “Very satisfied” with cosmetic appearance 60 days post-circumcision* | 182/197 (92.4%) | 152/201 (75.6%) |
| Mean ± SD duration of procedure (excluding anesthesia administration)** | 7.0±1.9 | 20.7±6.0 |
*, P<0.001; **, P<0.0001.
Shang Ring procedures took significantly less time compared to conventional circumcisions (approximately 7 vs. 21 minutes). There were no significant problems reported during the circumcisions, although one man randomized to the Shang Ring group underwent a forceps-guided MC because he had an unusually thick foreskin, thought to be due to scarring following a previous STI, which prevented closure of the outer ring. As in previous Shang Ring studies, some men undergoing a Shang Ring MC required a small cut in the foreskin in order to facilitate eversion of the foreskin over the inner ring (40/197, 20.3%; mean length of cut =11.4 mm).
There were six cases of cutaneous pinches noted in the Shang Ring group; all were mild and healed uneventfully. Prior to the start of the RCT, circumcision providers were advised on how to reduce the likelihood of occurrence of cutaneous pinches by carefully checking the skin on the shaft of the penis to ensure that no extraneous wrinkled shaft skin was pinched or trapped between the rings when the outer ring was closed.
Adverse event rates were similar between the two groups, with 24 moderate AEs and one severe AE. The severe AE was a case of pain during the MC that occurred in the Shang Ring group. The other AEs included wound dehiscence, hematoma, post-procedure pain, swelling, and an anesthetic complication. All were treated and resolved without problems. Median time to complete wound healing was 43.0 days in both groups, although conventional circumcisions healed on average 5.2 (95% CI: 2.68, 7.76) days sooner (P<0.001).
Pain scores were similar between the two groups at most time points, however the mean score for pain experienced with erections during the seven days after circumcision was significantly higher in the Shang Ring group. At 60 days post-circumcision, significantly more men in the Shang Ring group said they were “very satisfied” with the cosmetic appearance of their circumcision compared to the conventional surgery group. All of the circumcision providers said they preferred the Shang Ring over conventional circumcision, reporting that they found the former “much easier” to perform.
Comparative study in Uganda
HIV-negative men 18 years and older seeking MC in Rakai, Uganda were provided detailed information on the Shang Ring and dorsal site methods of MC (43). Those interested in participating in the study were asked to choose their preferred procedure. Circumcisions were conducted by clinical officers trained in the Shang Ring technique in Kenya. Participants returned for follow-up at 7 and 28 days post-circumcision (Shang Rings were removed at the 7-day visit).
A total of 621 men were enrolled in the study, with the majority (508/621, 81.8%) choosing the Shang Ring over the dorsal slit procedure (113/621, 18.2%). Reasons men gave for choosing the Shang Ring included shorter procedure time and the belief that it was safer and would be a less painful procedure. Men who chose dorsal slit circumcision did so because it was the standard procedure, they believed it was safer, and it did not require a removal procedure. In four cases (4/508, 0.8%) the Shang Ring procedure failed, and the circumcision needed to be completed with sutures; the ring slipped off after the foreskin was removed in three cases and there was damage to the foreskin after the Shang Ring had been placed in the other case. All of the device failures occurred early in the study and were attributed by study investigators to provider inexperience.
The two self-selected groups were comparable, with no significant differences in socio-demographic variables or self-reported behaviors between the men receiving Shang Ring and dorsal slit circumcisions. Results were similar to those from the randomized study described above. Shang Ring circumcisions took approximately 1/3 the time of conventional ones (mean ± SD =6.1 minutes ±2.7 vs. 17.7 minutes ±7.3). There was no difference in the rate of moderate and severe adverse events between the groups; 5/500 (1.0%) in the Shang Ring group vs. 1/117 (0.9%) in the dorsal slit group. AEs included post-operative pain, bleeding, infection, wound dehiscence, and insufficient skin removal. Significantly (P<0.001) more men in the dorsal slit group (111/113, 100%) demonstrated complete wound healing at four weeks follow-up compared to the Shang Ring group (408/486, 84.0%). There was no difference between the two groups in the proportion of men reporting they were satisfied or very satisfied with the circumcision procedure they chose or the cosmetic outcome of their circumcision.
Field study of Shang Ring circumcision in Kenya and Zambia
Results of a yet unpublished field study on use of the Shang Ring for adult MC in Kenya and Zambia were reviewed by the WHO Technical Advisory Group on Innovations in Male Circumcision in January, 2013 and presented at the 7th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention in June/July, 2013 (34,42). The primary objective of the study was to evaluate the safety of Shang Ring circumcision during routine service delivery, with outcomes including adverse events rates and device-related incidents. Secondary objectives included evaluating client acceptability (e.g., pain after Shang Ring circumcision, effect of Shang Ring circumcision on normal activities, satisfaction with Shang Ring circumcision) and provider preferences (e.g., provider experiences with the device and preferences for circumcision technique).
The non-comparative prospective field study was conducted at eight sites in Kenya and three in Zambia among men 18-54 years old seeking MC. The study sites included hospitals and health centers, as well as some outreach sites such as schools. The sites covered the spectrum from well-equipped health care facilities, to basic health facilities, to places that were not health facilities at all. Shang Rings were removed 7 days after circumcision and men were asked to return for one additional follow-up visit between 35 and 42 days post-circumcision.
Among the 1,211 men who were screened, 48 were not enrolled, including five that were considered unsuitable for Shang Ring circumcision because of foreskin abnormalities. The procedure-related AE rate was 1.6% (18/1149). Two adverse events were considered severe, one instance of post-operative pain and one of wound dehiscence. The remaining 16 AEs were moderate, mostly cases of wound dehiscence. All AEs were managed conservatively to resolution without problems.
The Shang Ring was well accepted by study participants. For example, pain associated with the device caused little disruption in sleep or work, and pain with erections when the device was in place was moderate and well tolerated by most men. At the 35-42 days follow-up visit, most men reported being very satisfied with the circumcision and nearly all said they would recommend the Shang Ring to others.
Most procedures were performed by nurses or clinical officers, with some of the providers in both countries being women. While there were a small number of men who refused to be circumcised by a female provider, this was not a significant barrier. Most (70%) of the circumcisions were performed at sites that had no previous experience with the Shang Ring. The providers at those sites were trained locally by the providers who had participated in the previous Shang Ring studies in Kenya and Zambia and had originally been trained in China. Providers reported that the Shang Ring was easy to use and that there were no problems during the circumcision procedures and few during the removals. In 12 men there were minor problems during removal, primarily pain or difficulty pulling the inner ring away from the scab. Most providers said they preferred using the Shang Ring compared to conventional circumcision surgery because Shang Ring circumcision was faster and easier to perform, with better cosmetic results.
Discussion
Results from the studies conducted to date in Africa demonstrate that the Shang Ring has an excellent safety profile, supporting results of Shang Ring use in China and indicating that the Shang Ring could facilitate rapid roll-out of MC for HIV prevention in Africa. Potential advantages and disadvantages of the Shang Ring are shown in Table 3. The African experience shows that the Shang Ring is easily used by trained non-physicians, which would facilitate task shifting, and is strongly preferred by providers and well-liked by men who have participated in the studies. The vast majority of participants in studies in Africa as well as China have reported few problems and little disruption to daily life while wearing the device. The significantly shorter procedure time for Shang Ring circumcision would allow for many more procedures to be done in a given time frame compared to conventional MC techniques.
Table 3. Potential advantages & disadvantages of the Shang Ring.
| Potential advantages |
| Simple design that makes the device easy to use |
| Single use and disposable |
| Device sized commercially available for all ages, newborn to adults |
| Easy to train providers and easy for providers to learn the technique |
| Minimally invasive & essentially no bleeding |
| Short procedure time |
| Does not require cautery or suturing for wound closure |
| Excellent cosmetic results |
| Design decreases risk of serious surgical errors |
| Well-liked by men and preferred by providers over conventional MC techniques |
| Potential disadvantages |
| Multiple device sizes must be kept in stock |
| Ring stays on for seven days |
| Removal visit required |
| Healing is delayed compared to conventional MC |
MC, male circumcision.
Measures of safety such as AE rates and pain scores were found to be similar between the Shang Ring and conventional techniques, although healing has been shown to be slower with Shang Ring circumcision compared to conventional techniques in the comparative studies in Africa and China (30,41,43). The clinical significance of healing prolonged by 3-5 days following Shang Ring circumcision relative to conventional methods however is unclear. Healing following MC with the PrePex device is also slower than with conventional techniques (34,45). This difference in healing times is not surprising given that healing following Shang Ring or PrePex circumcision is by secondary intention, which is slower than the primary intention healing associated with conventional circumcision.
Results of the field study conducted in Kenya and Zambia demonstrate that Shang Ring circumcisions can be safely provided in routine service delivery settings. No unexpected adverse events or problems were seen with roll-out to sites that did not have prior experience using the device with inexperienced non-physician providers who were trained locally.
Relatively few device-related problems were seen during Shang Ring circumcision or removal procedures. In the studies in Kenya and Zambia, there were few men where it was not possible to use the device because of foreskin abnormalities (e.g., excessively thick foreskin). The few failures of device placement seen in Uganda were attributed to inexperience of the MC providers but may also suggest that surgical back up is needed as services are rolled out in case the circumcision cannot be completed with the device or complications need to be addressed. Clearly, careful hands-on surgical training is critical if Shang Ring MC is to be conducted safely. One recent study demonstrates this point; inadequate Shang Ring surgical training and a lack of experience and understanding of wound healing following Shang Ring MC appears to have led to longer procedure times and higher complication rates than reported in other studies, along with potential misclassification of normal healing as complications (46,47).
The need for a small slit in the foreskin to facilitate use of the device in up to 20% of cases was seen in the African studies (39-41), although it was not unexpected given it was also reported in China (30,37,38) and with other adult MC devices (32,48,49). It should be considered a normal part of the procedure in cases where the foreskin is too tight to allow for eversion over the inner ring. It is not a problem given that the penis is anesthetized.
The fact that current Shang Ring label instructions include a follow-up removal visit may be considered a disadvantage by some. However, the WHO/UNAIDS MC guidelines do recommend a one week follow-up visit after conventional circumcision (50), and most Ministry of Health guidelines recommend that men return for at least one follow-up visit after circumcision as well (51-53). This visit can also be used for health education and giving men HIV prevention messages, including reminders that MC does not provide 100% protection against acquisition of HIV. Concerns about men not returning for Shang Ring removal may also be unfounded. In the study exploring removal at different times after Shang Ring MC, data showed that the device will eventually detach on its own, without significant problems if removal is delayed beyond seven days where men do not return on time or perhaps do not return at all for removal (40). Although some men in 14- and 21-day groups requested early removal due to pain and discomfort, over 75% of the men in the delayed removal groups had complete detachment without seeking early removal. Implementation research is needed to determine if allowing the Shang Ring to fall off on its own is a viable service delivery strategy on a larger scale.
Conclusions
Shang Ring circumcision is relatively easy to teach and learn, making Shang Ring MC an appealing technique for use in Sub-Saharan Africa where doctors are in short supply and non-physician providers such as nurses and clinical officers are playing a major role in providing MC through task shifting. Through a series of recent studies in Africa, Shang Ring MC and device removals were shown to be uneventfully performed by trained non-physician providers, including nurses and clinical officers, who preferred the Shang Ring to conventional surgical techniques. Perhaps one of the biggest advantages of Shang Ring circumcision is the relatively short 3-6 minutes procedure time. Importantly, men also preferred the Shang Ring compared to conventional circumcision, and satisfaction with cosmetic appearance of their circumcised penis was very high. The Shang Ring holds great promise as an innovative technology that has the potential to facilitate the safe and effective scale-up of circumcision services in settings where MC is not widely used and where the burden of HIV-disease is high.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva, Switzerland. 2013. Available online: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf
- 2.WHO. Global incidence and prevalence of selected curable sexually transmitted infections – 2008. Geneva, Switzerland. 2012. Available online: http://apps.who.int/iris/bitstream/10665/75181/1/9789241503839_eng.pdf
- 3.Padian NS, Buve A, Balkus J, et al. Biomedical interventions to prevent HIV infection: evidence, challenges, and way forward. Lancet 2008;372:585-99. [DOI] [PubMed] [Google Scholar]
- 4.Potts M, Halperin DT, Kirby D, et al. Public health. Reassessing HIV prevention. Science 2008;320:749-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Auvert B, Taljaard D, Lagarde E, et al. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med 2005;2:e298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 2007;369:643-56. [DOI] [PubMed] [Google Scholar]
- 7.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet 2007;369:657-66. [DOI] [PubMed] [Google Scholar]
- 8.Marrazzo JM, Cates W. Interventions to prevent sexually transmitted infections, including HIV infection. Clin Infect Dis 2011;53 Suppl 3:S64-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss HA, Halperin D, Bailey RC, et al. Male circumcision for HIV prevention: from evidence to action? AIDS 2008;22:567-74. [DOI] [PubMed] [Google Scholar]
- 10.Gray R, Kigozi G, Kong X, et al. The effectiveness of male circumcision for HIV prevention and effects on risk behaviors in a posttrial follow-up study. AIDS 2012;26:609-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bailey RC, Moses S, Parker CB, et al. The protective effect of adult male circumcision against HIV acquisition is sustained for at least 54 months: results from the Kisumu, Kenya trial. XVIII International AIDS Conference; Vienna, 2010. [Google Scholar]
- 12.Lissouba P, Taljaard D, Rech D, et al. Adult male circumcision as an intervention against HIV: an operational study of uptake in a South African community (ANRS 12126). BMC Infect Dis 2011;11:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Auvert B, Sobngwi-Tambekou J, Cutler E, et al. Effect of male circumcision on the prevalence of high-risk human papillomavirus in young men: results of a randomized controlled trial conducted in Orange Farm, South Africa. J Infect Dis 2009;199:14-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gray RH, Kigozi G, Serwadda D, et al. The effects of male circumcision on female partners’ genital tract symptoms and vaginal infections in a randomized trial in Rakai, Uganda. Am J Obstet Gynecol 2009;200:42.e1-7. [DOI] [PMC free article] [PubMed]
- 15.Halperin DT, Bailey RC. Male circumcision and HIV infection: 10 years and counting. Lancet 1999;354:1813-5. [DOI] [PubMed] [Google Scholar]
- 16.Nasio JM, Nagelkerke NJ, Mwatha A, et al. Genital ulcer disease among STD clinic attenders in Nairobi: association with HIV-1 and circumcision status. Int J STD AIDS 1996;7:410-4. [DOI] [PubMed] [Google Scholar]
- 17.Backes DM, Bleeker MC, Meijer CJ, et al. Male circumcision is associated with a lower prevalence of human papillomavirus-associated penile lesions among Kenyan men. Int J Cancer 2012;130:1888-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Serwadda D, Wawer MJ, Makumbi F, et al. Circumcision of HIV-infected men: effects on high-risk human papillomavirus infections in a randomized trial in Rakai, Uganda. J Infect Dis 2010;201:1463-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson LE, Gravitt P, Tobian AA, et al. Male circumcision reduces penile high-risk human papillomavirus viral load in a randomised clinical trial in Rakai, Uganda. Sex Transm Infect 2013;89:262-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Albero G, Castellsague X, Giuliano AR, et al. Male circumcision and genital human papillomavirus: a systematic review and meta-analysis. Sex Transm Dis 2012;39:104-13. [DOI] [PubMed] [Google Scholar]
- 21.Davis MA, Gray RH, Grabowski MK, et al. Male circumcision decreases high-risk human papillomavirus viral load in female partners: a randomized trial in Rakai, Uganda. Int J Cancer 2013;133:1247-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wawer MJ, Tobian AA, Kigozi G, et al. Effect of circumcision of HIV-negative men on transmission of human papillomavirus to HIV-negative women: a randomised trial in Rakai, Uganda. Lancet 2011;377:209-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.WHO/UNAIDS Technical Consultation. New Data on Male Circumcision and HIV Prevention: Policy and Programme Implications. Geneva, Switzerland: WHO, 2007. Available online: http://libdoc.who.int/publications/2007/9789241595988_eng.pdf
- 24.WHO/UNAIDS. Progress in scale-up of male circumcision for HIV prevention in Eastern and Southern Africa: Focus on service delivery. Geneva, Switzerland: WHO; 2011. Available online: http://whqlibdoc.who.int/publications/2011/9789241502511_eng.pdf
- 25.UNAIDS/WHO/SACEMA Expert Group on Modelling the Impact and Cost of Male Circumcision for HIV Prevention . Male circumcision for HIV prevention in high HIV prevalence settings: what can mathematical modelling contribute to informed decision making? PLoS Med 2009;6:e1000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hallett TB, Singh K, Smith JA, et al. Understanding the impact of male circumcision interventions on the spread of HIV in southern Africa. PLoS One 2008;3:e2212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nagelkerke NJ, Moses S, de Vlas SJ, et al. Modelling the public health impact of male circumcision for HIV prevention in high prevalence areas in Africa. BMC Infect Dis 2007;7:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.White RG, Glynn JR, Orroth KK, et al. Male circumcision for HIV prevention in sub-Saharan Africa: who, what and when? AIDS 2008;22:1841-50. [DOI] [PubMed] [Google Scholar]
- 29.Njeuhmeli E, Forsythe S, Reed J, et al. Voluntary medical male circumcision: modeling the impact and cost of expanding male circumcision for HIV prevention in eastern and southern Africa. PLoS Med 2011;8:e1001132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li HN, Xu J, Qu LM. Shang Ring circumcision versus conventional surgical procedures: comparison of clinical effectiveness. Zhonghua Nan Ke Xue 2010;16:325-7. [PubMed] [Google Scholar]
- 31.Krieger JN, Bailey RC, Opeya JC, et al. Adult male circumcision outcomes: experience in a developing country setting. Urol Int 2007;78:235-40. [DOI] [PubMed] [Google Scholar]
- 32.Decastro B, Gurski J, Peterson A. Adult template circumcision: a prospective, randomized, patient-blinded, comparative study evaluating the safety and efficacy of a novel circumcision device. Urology 2010;76:810-4. [DOI] [PubMed] [Google Scholar]
- 33.Auvert B, Marseille E, Korenromp EL, et al. Estimating the resources needed and savings anticipated from roll-out of adult male circumcision in Sub-Saharan Africa. PLoS One 2008;3:e2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO Technical Advisory Group on Innovations in Male Circumcision: Evaluation of Two Adult Devices. Meeting report. Geneva, Switzerland 2013. Available online: http://apps.who.int/iris/bitstream/10665/85269/1/9789241505635_eng.pdf
- 35.Masson P, Li PS, Barone MA, et al. The ShangRing device for simplified adult circumcision. Nat Rev Urol 2010;7:638-42. [DOI] [PubMed] [Google Scholar]
- 36.Cheng Y, Li PS. eds. Male circumcision using the Shang Ring. Beijing, China: People’s Medical Publishing House, 2012. [Google Scholar]
- 37.Peng YF, Cheng Y, Wang GY, et al. Clinical application of a new device for minimally invasive circumcision. Asian J Androl 2008;10:447-54. [DOI] [PubMed] [Google Scholar]
- 38.Cheng Y, Peng YF, Liu YD, et al. A recommendable standard protocol of adult male circumcision with the Chinese Shang Ring: outcomes of 328 cases in China. Zhonghua Nan Ke Xue 2009;15:584-92. [PubMed] [Google Scholar]
- 39.Barone MA, Ndede F, Li PS, et al. The Shang Ring device for adult male circumcision: a proof of concept study in Kenya. J Acquir Immune Defic Syndr 2011;57:e7-12. [DOI] [PubMed] [Google Scholar]
- 40.Barone MA, Awori QD, Li PS, et al. Randomized trial of the Shang Ring for adult male circumcision with removal at one to three weeks: delayed removal leads to detachment. J Acquir Immune Defic Syndr 2012;60:e82-9. [DOI] [PubMed] [Google Scholar]
- 41.Sokal DC, Li PS, Zulu R, et al. Randomized controlled trial of the shang ring versus conventional surgical techniques for adult male circumcision: safety and acceptability. J Acquir Immune Defic Syndr 2014;65:447-55. [DOI] [PubMed] [Google Scholar]
- 42.Barone MA LP, Zulu R, Awori QD, et al. A Field Study of Male Circumcision Using the Shang Ring, a Minimally-Invasive Disposable Device, in Routine Clinical Settings in Kenya and Zambia. 7th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention; Kuala Lumpur, Malaysia, 2013. [Google Scholar]
- 43.Kigozi G, Musoke R, Watya S, et al. The acceptability and safety of the Shang Ring for adult male circumcision in Rakai, Uganda. J Acquir Immune Defic Syndr 2013;63:617-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.WHO. Framework for Clinical Evaluation of Devices for Adult Male Circumcision. Geneva, Switzerland 2011. Available online: http://apps.who.int/iris/bitstream/10665/75954/1/9789241504355_eng.pdf
- 45.Mutabazi V, Kaplan SA, Rwamasirabo E, et al. HIV prevention: male circumcision comparison between a nonsurgical device to a surgical technique in resource-limited settings: a prospective, randomized, nonmasked trial. J Acquir Immune Defic Syndr 2012;61:49-55. [DOI] [PubMed] [Google Scholar]
- 46.Kanyago S, Riding DM, Mutakooha E, et al. Shang Ring versus forceps-guided adult male circumcision: a randomized, controlled effectiveness study in southwestern Uganda. J Acquir Immune Defic Syndr 2013;64:130-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee R, Osterberg EC, Li PS, et al. Proper surgical training and grading of complications for Shang Ring circumcision are necessary. J Acquir Immune Defic Syndr 2013;64:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lagarde E, Taljaard D, Puren A, et al. High rate of adverse events following circumcision of young male adults with the Tara KLamp technique: a randomised trial in South Africa. S Afr Med J 2009;99:163-9. [PubMed] [Google Scholar]
- 49.Senel FM, Demirelli M, Pekcan H. Mass circumcision with a novel plastic clamp technique. Urology 2011;78:174-9. [DOI] [PubMed] [Google Scholar]
- 50.WHO, UNAIDS, JHPIEGO Manual for Male Circumcision under Local Anesthesia. Version 3.1. Geneva, Switzerland: WHO 2009. Available online: http://www.who.int/hiv/pub/malecircumcision/who_mc_local_anaesthesia.pdf
- 51.Xaba S. eds. Country Update, Zimbabwe. Scaling-up Male Circumcision Programmes in the Eastern and Southern Africa Region: Country Update Meeting; Arusha, Tanzania, 2010. [Google Scholar]
- 52.Lissouba P, Taljaard D, Rech D, et al. A model for the roll-out of comprehensive adult male circumcision services in African low-income settings of high HIV incidence: the ANRS 12126 Bophelo Pele Project. PLoS Med 2010;7:e1000309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kenya Ministry of Public Health & Sanitation. Kenya National Strategy for Voluntary Medical Male Circumcision. Nairobi, Kenya, 2009. Available online: http://nascop.or.ke/library/VMMC/VMMC%20Strategy.pdf