Abstract
Interstitial cystitis/painful bladder syndrome (IC/PBS) is a chronic debilitating condition that is characterised by suprapubic pain and urinary symptoms such as urgency, nocturia and urinary frequency. The prevalence of the condition is increasing due to more inclusive diagnostic criteria. Herein, we review the evolving epidemiology of IC/PBS and investigate health seeking behaviour for the condition through Internet search activity. Study selection was performed in accordance with PRISMA. In addition, global search trends for the terms ‘Interstitial Cystitis’ and ‘Painful Bladder Syndrome’ from 2005 to 2015 were also evaluated using the ‘Google Trends’ search application. The mean search activity per month was recorded and mean activity at annual intervals calculated. Regional search activity by country and city was also measured. Prevalence rates for IC/PBS vary according to diagnostic criteria and range from 2% to 17.3% among the general population. Increased prevalence is associated with female gender and females with one first-degree relative affected. There has been an increase in global mean search activity for IC/PBS on an annual basis since 2005. The greatest increase in search activity was in USA, Canada, United Kingdom, Australia, Ireland and India respectively. The top five cities for search activity for IC/PBS were in the USA. As diagnostic criteria for IC/PBS continues to become more inclusive it is likely that the prevalence will continue to increase. This is particularly true for the USA and Canada as these regions have demonstrated the greatest increase in Internet search activity for IC/ PBS.
Keywords: Interstitial cystitis (IC), painful bladder syndrome (PBS), interstitial cystitis/painful bladder syndrome (IC/PBS)
Introduction
Interstitial cystitis/painful bladder syndrome (IC/PBS) is a chronic debilitating condition that is defined by pelvic/suprapubic pain and urinary storage symptoms such as urgency, nocturia and urinary frequency (1). Historically, with strict diagnostic criteria, IC/PBS was diagnosed infrequently with an overall global prevalence of approximately 0.1% (2). More recently, the prevalence of the condition has increased to at least 2% among females due to broader and more inclusive diagnostic criteria (3,4). Diagnosis for IC/PBS is often difficult and delayed as its presentation is similar to a number of other urological and gynaecological conditions (5,6). An improved understanding of the pathophysiology of the condition among physicians has led to increasing numbers of patients being diagnosed with IC/PBS. Clinicians should familiarise themselves with its evolving epidemiology, increasing prevalence and appropriate evidence based treatment options to maximise treatment outcomes early in the course of the disease.
Public awareness on the presenting symptoms and signs of IC/PBS has increased due to the availability of informative medical information available on Internet websites and through healthcare campaigns (7). The Internet provides a convenient medium for patients with various medical conditions to gather relevant information in private (7). The primary objective of this narrative review was to assess the evolving epidemiology and increasing prevalence of IC/PBS. We also aimed to investigate the global demographics of IC/PBS by evaluating health seeking behaviour through Internet search activity.
Literature review
A literature search was undertaken using the Medline and EMBASE databases and the Cochrane Central Register of Controlled Trials for studies that investigated the prevalence of IC/PBS. The title and abstract of citations and full texts of potentially eligible trials were obtained and study selection was performed in accordance with PRISMA. The following terms were entered into the search algorithm to identify peer-reviewed articles that investigated the prevalence for IC/PBS: “interstitial cystitis” and “painful bladder syndrome” or “interstitial cystitis/painful bladder syndrome”. Studies on adult and paediatric patients published in English between January 1915 and April 2015 were included. A manual search of the bibliographies of retrieved studies was also conducted. If a patient group was reported twice, the most recent publication was chosen. The latest search was performed on April 19th 2015. Two authors (N.D. and S.G.) independently examined the title and abstract of citations and the full texts of potentially eligible articles were obtained and analysed in detail. In addition, published guidelines from the European Association of Urology (EAU) and American Urological Association (AUA) were included in the literature search process (8,9).
A total of 112 studies published between 1938 and 2015 were retrieved, of which 29 were considered suitable based on clinical relevance and content. The evolving epidemiology for IC/PBS was investigated with particular emphasis on global prevalence.
Diagnosis of IC/PBS
Historical perspective
In 1915 Guy Hunner described an initial case series of eight females presenting with frequency, urgency, nocturia and suprapubic pain at the AUA (10). This group of patients had been followed for 17 years and had visible bleeding areas on the wall of the urinary bladder at cystoscopy. Afterwards, the pseudonym “Hunner’s ulcer” was coined to describe this “pathognomonic” finding for IC/PBS. It is now widely believed that this description was a misnomer as early cystoscopies gave a poorly lit view of the urinary bladder and the “ulcers” were most likely due to petechial haemorrhages. At the time Hunner postulated that IC/PBS resulted from persistent bacterial infection secondary to chronic disorders such as disseminated tuberculosis (TB). In subsequent decades, until TB of the urinary tract became rare, causes of IC/PBS were always assessed to out-rule TB infection as a differential diagnosis.
In 1949, Hand reported on 223 patients that were sub-classified into three different grades of IC/PBS depending on the severity with grade 3 representing a small-capacity scarred urinary bladder (11). In 1977 Walsh described a pan-mural cystitis and “glomerulations” that corresponded with the petechial haemorrhages described by Hand (12). The following year Messing and Stamey averted attention from the pathognomonic Hunner’s ulcer and focused on more representative cystoscopic findings (13). They described symptoms and glomerulations at the time of bladder distension in their diagnostic criteria. Although the definitions described by Walsh, Messing and Stamey are considered practical for the urologist; they are not patient friendly and may only be relevant for more severe cases of IC/PBS.
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
In 1999, NIDDK standardised the diagnostic criteria for IC/PBS based on cystoscopic and cystometric findings (14). Interestingly, the panel comprised of physicians and not urologists. Minimum criteria for age, duration of symptoms, degree of frequency and nocturia were also required. Initially, these criteria were not meant to define the disease but were developed to ensure that groups of patients included in basic and clinical research studies were comparable. However, it is widely accepted that the NIDDK “research definition” quickly became a modern day definition for IC/PBS. Using these rigid diagnostic criteria it was demonstrated that up to 60% of patients with IC/PBS are not diagnosed and this led to concerns that many patients suffering from this syndrome might be misdiagnosed (13).
Contemporary diagnostic algorithms
The European Society for the Study of IC/PBS has described more inclusive diagnostic criteria for IC/PBS (15). Their criteria are predominantly based on the following clinical symptoms:
Pelvic pain >6 months duration;
Pressure/discomfort accompanied by at least one other urinary symptom such as urgency or frequency;
Furthermore, conditions with similar presenting symptoms should be excluded with appropriate investigations before a diagnosis is made. A thorough history is important for patients presenting with pelvic discomfort, urinary frequency and urgency. Typically, patients with IC/PBS present with pain on bladder filling that is relieved upon voiding (15).
The updated 2011 AUA guidelines also describe more inclusive criteria for the diagnosis of IC/PBS with the aim of improving early diagnosis and treatment (8). Their definition for IC/BPS is an unpleasant sensation (pain, pressure), perceived to be related to the urinary bladder, and associated with lower urinary tract symptoms of more than 6 weeks duration in the absence of infection or other identifiable causes (8). This relatively short duration of symptoms was selected to allow early treatment to be commenced in these patients. The EAU 2008 proposals describe more rigid and stricter diagnostic criteria (15). Their diagnostic algorithm places more emphasis on investigations such as cystoscopy, hydrodistension with bladder volume measurement and bladder biopsy to assess for pathological features that demonstrate inflammatory infiltrates and granulation tissue (15). During the hydrodistension stellate scars can occasionally be visualised during the first fill with glomerulations and bleeding more frequently visible during the second fill. Ulcerating lesions are associated with more severe disease. Panmural cystitis with scarring and reduced anatomical capacity reflects end stage disease.
Prevalence
Due to the aforementioned variations in diagnostic criteria of IC/PBS, epidemiological studies demonstrate varying statistics on prevalence. Earlier studies suggested that females are 9 times more likely to be diagnosed with IC/PBS compared to males. Female gender was the only definitive risk factor for developing IC/PBS. However, in a managed care population the female to male ratio decreases to 5:1 which suggests that the condition may be under diagnosed among males (16). Clemens et al. demonstrated prevalence ranges from 52-500/100,000 in females compared to 8-41/100,000 in males (16). They suggest that the condition is significantly under diagnosed as the prevalence of IC/PBS symptoms was 30- to 50-fold higher in women and 60- to 100-fold higher in men than the prevalence of a coded physician diagnosis of IC in the same population. The prevalence increases to 1,431/100,000 for females with first-degree relatives IC/PBS which suggests a hereditary component (17).
The prevalence of IC/PBS was as high as 2.6% in a cross-sectional study in Boston. Inclusion criteria included self-reported pain associated with bladder filling and relieved by urination present for at least 3 months (18). In another USA study, Ibrahim et al. also investigated the prevalence rates of self-reported IC/PBS, IC/PBS-like symptoms and pelvic pain among 823 female controls in the community (19). Prevalence rates of 3.7% and 4.4% and 17.3% respectively were recorded (19).
IC/PBS is typically diagnosed in midlife but patients’ history may extend back to childhood. Investigations such as cystoscopy, hydrodistension and biopsy are used for diagnosing IC/PBS in paediatric patients as eliciting clinical symptoms can be difficult and unreliable (20). The prevalence of IC/PBS in the paediatric population is not known as the NIDDK criteria excludes IC/PBS in patients <18 years of age (14). However, retrospective data demonstrates that up to 25% of adults with IC/PBS report persistence of their symptoms since they were children (20).
During clinical work-up, the O’Leary-Sant interstitial cystitis questionnaire contributes to the diagnostic process as it objectively defines the extent and duration of pelvic pain as well as urinary urgency and frequency (21,22). Clinical examination is essential to exclude urogynaecological pathologies such as urethral diverticulae, vulvitis and vaginitis. Patients with IC/PBS are typically tender at the bladder base (6). Readily available dipstick urinalysis can exclude active urinary tract infection. Irritative voiding symptoms should be treated with suspicion in the context of non-visible or visible haematuria as a bladder neoplasm should be ruled out with a cystoscopic examination during the initial investigatory process.
Measuring Internet search activity
To investigate health seeking behaviour and global interest for IC/PBS data, analysis was performed using the established “Google Trends” search application. Global search trends for the terms “interstitial cystitis” and “painful bladder syndrome” from 2005 to 2015 were evaluated. Google trends is a “search-volume” tool that provides information on Internet searches that generate a significant volume of results (23). Data is normalised to a reference population and scaled from 0-100%. Peak search activity over a given period is graded as 100% and activity at all other time periods is presented relative to that peak (24). The mean search activity per month was recorded and mean activity at annual intervals calculated. Regional search activity and related search trends were also measured. Values for annual activity were plotted on an “XY scatter plot”.
Figure 1 illustrates the global annual mean search activity for “IC/PBS” since 2005. There has been an increase in global mean search activity for IC/PBS on an annual basis since the beginning of 2005. The greatest increase in mean search activity was in USA, Canada, United Kingdom, Australia, Ireland and India respectively (Figure 2). These findings indicate a large increase in health seeking behaviour for IC/PBS in these countries. The top five cities for search activity for IC/PBS were in the USA and are demonstrated in Figure 3. The top five related/associated search terms are demonstrated in Figure 4.
Figure 1.
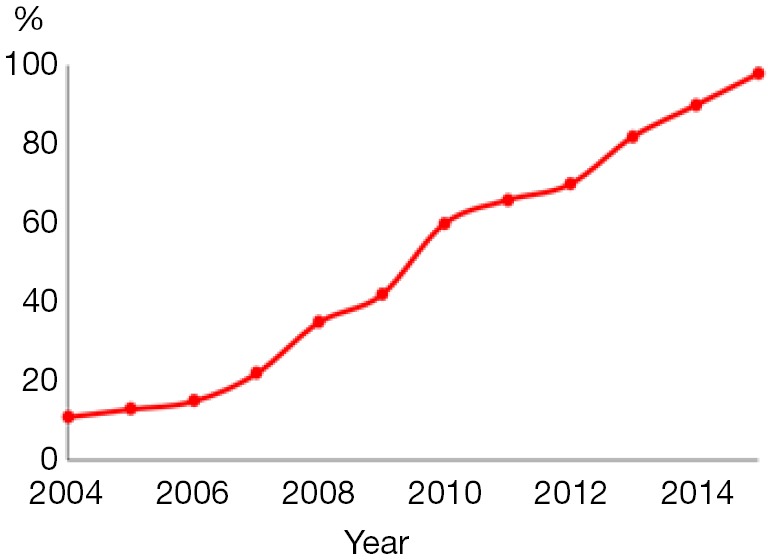
Scatter plot demonstrating mean global Internet search activity for IC/PBS between January 2005 and April 2015. There has been an increase on an annual basis for internet search activity. IC/PBS, interstitial cystitis/painful bladder syndrome.
Figure 2.
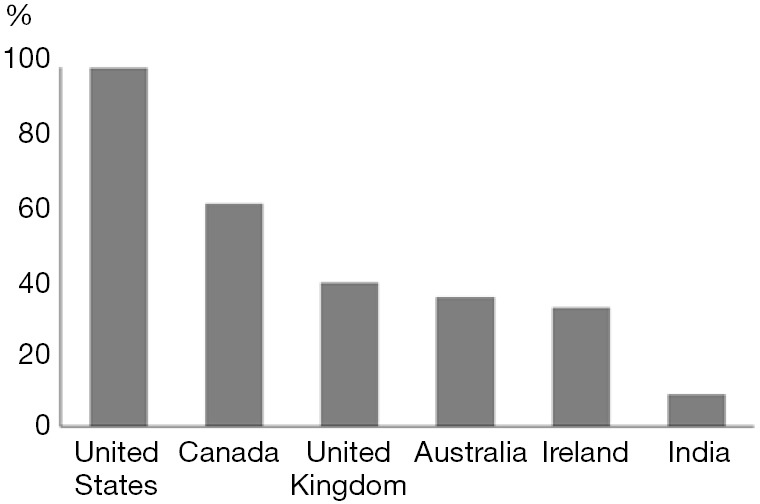
Regional interest over time for Internet search activity for IC/PBS. The top six countries using Internet searches for IC/PBS are represented. IC/PBS, interstitial cystitis/painful bladder syndrome.
Figure 3.
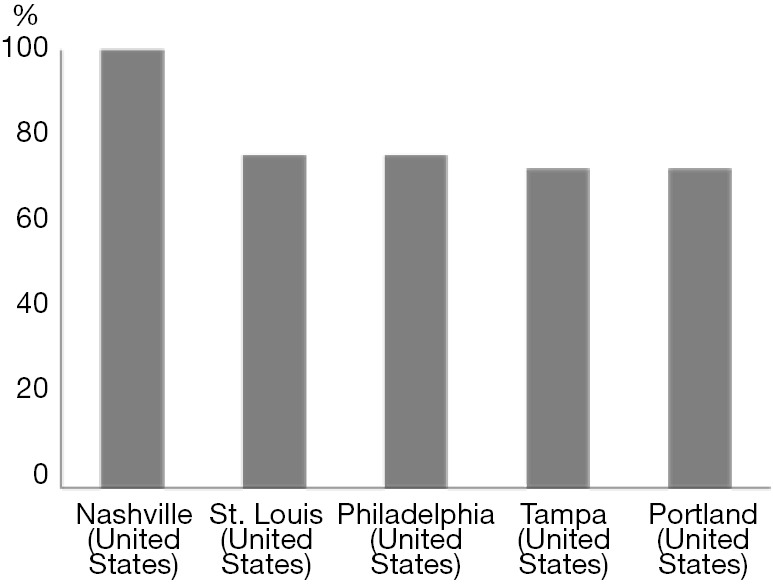
Top five cities using Internet searches for IC/PBS. All five cities are in the USA. IC/PBS, interstitial cystitis/painful bladder syndrome.
Figure 4.
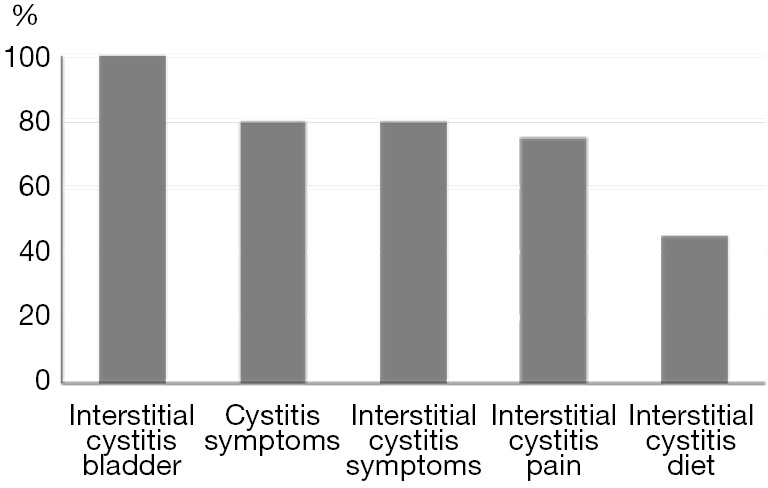
The top five related Internet searches for IC/PBS. IC/PBS, interstitial cystitis/painful bladder syndrome.
The Internet is a useful tool for patients to gather information on medical conditions and over 80% of all Internet users in the USA use this application to access health information (25). Globally, the internet has become widely available and recent studies have used search engines to investigate and monitor public interest for urological conditions such as erectile dysfunction (7), urinary tract calculi (26) and urinary tract infections (27). Monitoring health seeking behaviour in the form of queries to online search engines has previously been reported (24). The originally developed the Google Insights for Search Application was initially used to track influenza-like illness in different populations for vaccine purposes (28). Afterwards, the software was used to investigate potential outbreaks for salmonella and Dengue fever (29). Such reports demonstrate the effectiveness of the Internet for gathering accurate international data on health seeking behaviour among the general public.
Future perspectives and conclusions
IC/PBS is increasing in prevalence globally due to broader diagnostic criteria and patients are using online technologies to gather information on the condition, particularly in the developed world. Due to readily available nature of the Internet, there appears to be a trend for patients to seek self-help. Herein, we demonstrated a global increase in overall Internet search activity for IC/PBS since 2005. As diagnostic criteria continue to broaden and become more inclusive it is likely that the prevalence of IC/PBS will continue to increase. Therefore, urologists are likely to be referred more patients with symptoms that are consistent with modernised IC/PBS diagnostic criteria. This is particularly true for the USA and Canada as these regions demonstrate the greatest increase in regional interest over time for Internet search activity for IC/PBS.
The broadened diagnostic criteria and increased prevalence by inclusion of patients hitherto can be considered positive. From the patients’ viewpoint, they have a diagnostic label for their troublesome symptomatology. From a scientific viewpoint, it facilitates research on a much larger patient cohort. Paradoxically, it could be speculated that research will ultimately lead to subdivision into categories of IC/PBS, or even into different diseases.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Davis NF, Brady CM, Creagh T. Interstitial cystitis/painful bladder syndrome: epidemiology, pathophysiology and evidence-based treatment options. Eur J Obstet Gynecol Reprod Biol 2014;175:30-7. [DOI] [PubMed] [Google Scholar]
- 2.Jones CA, Nyberg L. Epidemiology of interstitial cystitis. Urology 1997;49:2-9. [DOI] [PubMed] [Google Scholar]
- 3.Payne CK, Joyce GF, Wise M, et al. Interstitial cystitis and painful bladder syndrome. J Urol 2007;177:2042-9. [DOI] [PubMed] [Google Scholar]
- 4.Konkle KS, Berry SH, Elliott MN, et al. Comparison of an interstitial cystitis/bladder pain syndrome clinical cohort with symptomatic community women from the RAND Interstitial Cystitis Epidemiology study. J Urol 2012;187:508-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vij M, Srikrishna S, Cardozo L. Interstitial cystitis: diagnosis and management. Eur J Obstet Gynecol Reprod Biol 2012;161:1-7. [DOI] [PubMed] [Google Scholar]
- 6.Dell JR, Mokrzycki ML, Jayne CJ. Differentiating interstitial cystitis from similar conditions commonly seen in gynecologic practice. Eur J Obstet Gynecol Reprod Biol 2009;144:105-9. [DOI] [PubMed] [Google Scholar]
- 7.Davis NF, Smyth LG, Flood HD. Detecting internet activity for erectile dysfunction using search engine query data in the Republic of Ireland. BJU Int 2012;110:E939-42. [DOI] [PubMed] [Google Scholar]
- 8.Hanno PM, Burks DA, Clemens JQ, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol 2011;185:2162-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Engeler DS, Baranowski AP, Dinis-Oliveira P, et al. The 2013 EAU guidelines on chronic pelvic pain: is management of chronic pelvic pain a habit, a philosophy, or a science? 10 years of development. Eur Urol 2013;64:431-9. [DOI] [PubMed] [Google Scholar]
- 10.Hunner GL. A Rare Type of Bladder Ulcer in Women; Report of Cases. Boston Med Surg J 1915;172:660-4. [Google Scholar]
- 11.Hand JR. Interstitial cystitis; report of 223 cases, 204 women and 19 men. Portland Clin Bull 1949;3:41-7. [PubMed] [Google Scholar]
- 12.Walsh A. Interstitial cystitis. Observations on diagnosis and on treatment with anti-inflammatory drugs, particularly benzydamine. Eur Urol 1977;3:216-7. [PubMed] [Google Scholar]
- 13.Messing EM, Stamey TA. Interstitial cystitis: early diagnosis, pathology, and treatment. Urology 1978;12:381-92. [DOI] [PubMed] [Google Scholar]
- 14.Hanno PM, Landis JR, Matthews-Cook Y, et al. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health Interstitial Cystitis Database study. J Urol 1999;161:553-7. [DOI] [PubMed] [Google Scholar]
- 15.van de Merwe JP, Nordling J, Bouchelouche P, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol 2008;53:60-7. [DOI] [PubMed] [Google Scholar]
- 16.Clemens JQ, Meenan RT, Rosetti MC, et al. Prevalence and incidence of interstitial cystitis in a managed care population. J Urol 2005;173:98-102; discussion 102. [DOI] [PubMed] [Google Scholar]
- 17.Warren JW, Jackson TL, Langenberg P, et al. Prevalence of interstitial cystitis in first-degree relatives of patients with interstitial cystitis. Urology 2004;63:17-21. [DOI] [PubMed] [Google Scholar]
- 18.Hall SA, Link CL, Pulliam SJ, et al. The relationship of common medical conditions and medication use with symptoms of painful bladder syndrome: results from the Boston area community health survey. J Urol 2008;180:593-8. [DOI] [PubMed] [Google Scholar]
- 19.Ibrahim IA, Diokno AC, Killinger KA, et al. Prevalence of self-reported interstitial cystitis (IC) and interstitial-cystitis-like symptoms among adult women in the community. Int Urol Nephrol 2007;39:489-95. [DOI] [PubMed] [Google Scholar]
- 20.Peters KM, Killinger KA, Ibrahim IA. Childhood symptoms and events in women with interstitial cystitis/painful bladder syndrome. Urology 2009;73:258-62. [DOI] [PubMed] [Google Scholar]
- 21.Kushner L, Moldwin RM. Efficiency of questionnaires used to screen for interstitial cystitis. J Urol 2006;176:587-92. [DOI] [PubMed] [Google Scholar]
- 22.Berry SH, Elliott MN, Suttorp M, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol 2011;186:540-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davis NF, Breslin N, Creagh T. Using Google Trends to assess global interest in 'Dysport®' for the treatment of overactive bladder. Urology 2013;82:1189. [DOI] [PubMed] [Google Scholar]
- 24.Glynn RW, Kelly JC, Coffey N, et al. The effect of breast cancer awareness month on internet search activity--a comparison with awareness campaigns for lung and prostate cancer. BMC Cancer 2011;11:442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hay J, Coups EJ, Ford J, et al. Exposure to mass media health information, skin cancer beliefs, and sun protection behaviors in a United States probability sample. J Am Acad Dermatol 2009;61:783-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Willard SD, Nguyen MM. Internet search trends analysis tools can provide real-time data on kidney stone disease in the United States. Urology 2013;81:37-42. [DOI] [PubMed] [Google Scholar]
- 27.Rossignol L, Pelat C, Lambert B, et al. A method to assess seasonality of urinary tract infections based on medication sales and google trends. PLoS One 2013;8:e76020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ginsberg J, Mohebbi MH, Patel RS, et al. Detecting influenza epidemics using search engine query data. Nature 2009;457:1012-4. [DOI] [PubMed] [Google Scholar]
- 29.Althouse BM, Ng YY, Cummings DA. Prediction of dengue incidence using search query surveillance. PLoS Negl Trop Dis 2011;5:e1258. [DOI] [PMC free article] [PubMed] [Google Scholar]


