Abstract
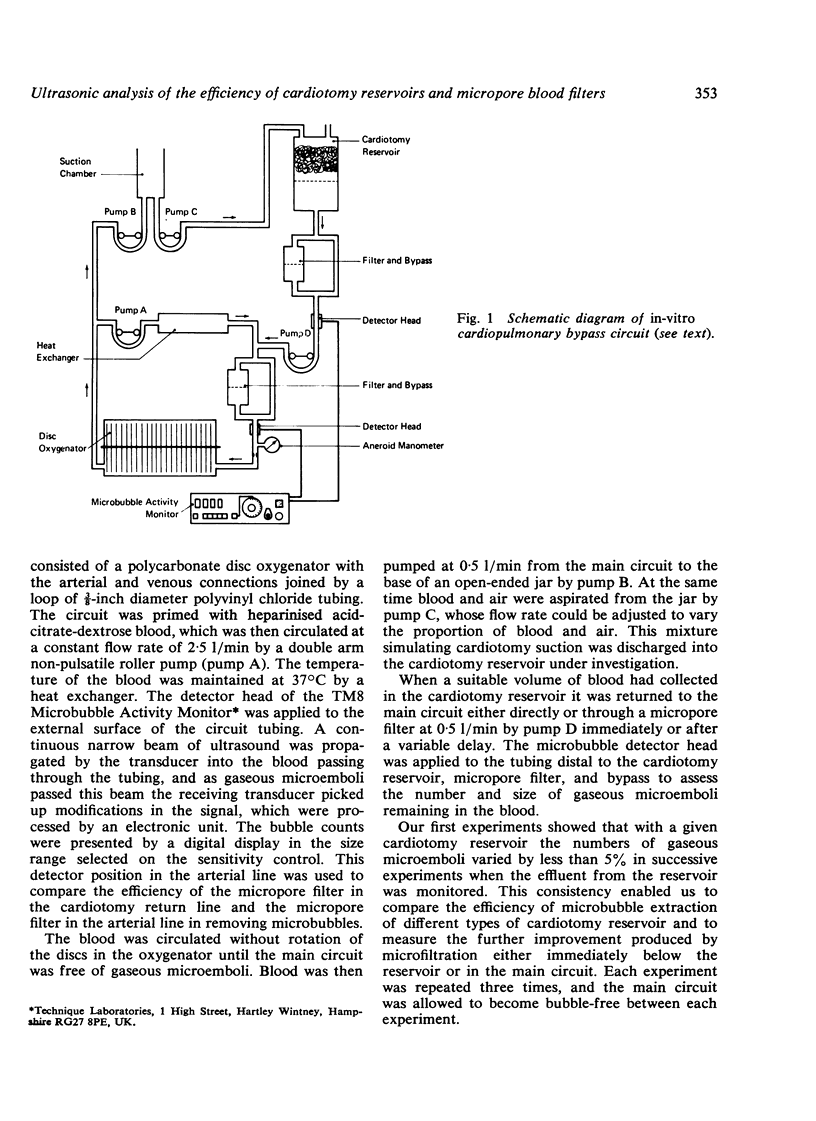
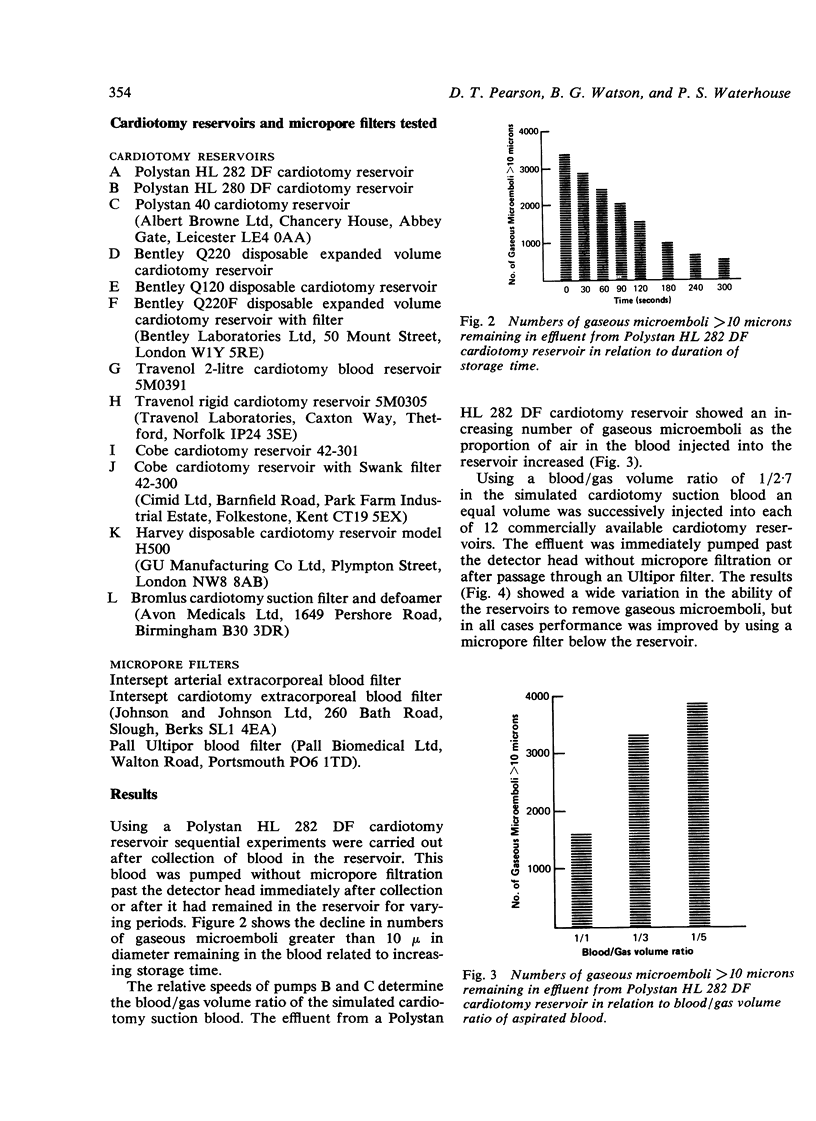
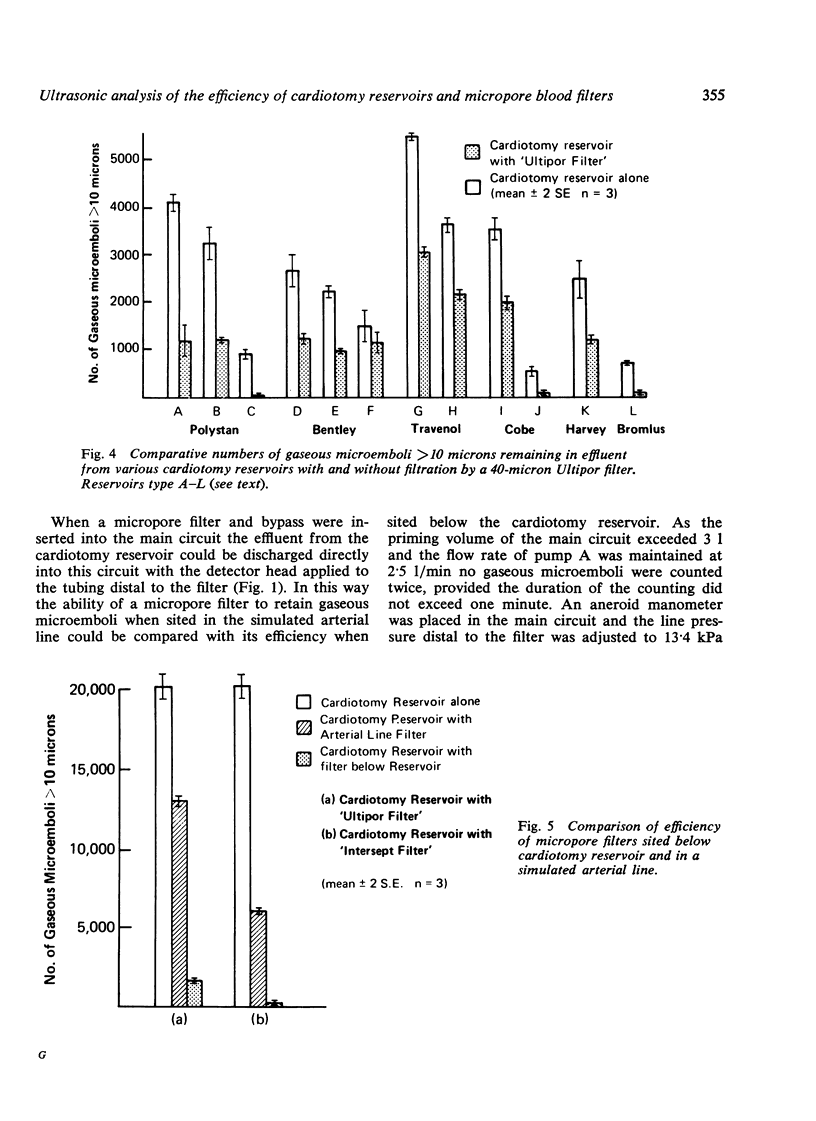
The ability of 12 commercially available cardiotomy reservoirs to remove bubbles from aspirated blood was investigated by means of a simulated cardiopulmonary bypass circuit and an ultrasonic microbubble detector. Performance varied considerably. The number of gaseous microemboli remaining after passage of blood through the reservoir was reduced by (a) holding the blood in the reservoir, (b) reducing the volume of air mixed with the aspirated blood, and (c) using a reservoir that did not induce turbulence and that contained integral micropore filtration material. Further micropore filtration of the blood after passage through the cardiotomy reservoir was beneficial, and significantly more bubbles were extracted when the microfilter was sited below the reservoir than when it was placed in the arterial line.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aberg T., Kihlgren M. Cerebral protection during open-heart surgery. Thorax. 1977 Oct;32(5):525–533. doi: 10.1136/thx.32.5.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguilar M. J., Gerbode F., Hill J. D. Neuropathologic complications of cardiac surgery. J Thorac Cardiovasc Surg. 1971 May;61(5):676–685. [PubMed] [Google Scholar]
- Branthwaite M. A. Prevention of neurological damage during open-heart surgery. Thorax. 1975 Jun;30(3):258–261. doi: 10.1136/thx.30.3.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan R. W., Patterson R. H., Jr, Kessler J. Cerebral blood flow and metabolism during cardiopulmonary bypass: evidence of microembolic encephalopathy. Neurology. 1971 Jul;21(7):665–672. doi: 10.1212/wnl.21.7.665. [DOI] [PubMed] [Google Scholar]
- Gallagher E. G., Pearson D. T. Ultrasonic identification of sources of gaseous microemboli during open heart surgery. Thorax. 1973 May;28(3):295–305. doi: 10.1136/thx.28.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill J. D., Osborn J. J., Swank R. L., Aguilar M. J., Gerbode F., de Lanerolle P. Experience using a new dacron wool filter during extracorporeal circulation. Arch Surg. 1970 Dec;101(6):649–652. doi: 10.1001/archsurg.1970.01340300005002. [DOI] [PubMed] [Google Scholar]
- Karlson K. E., Murphy W. R., Kakvan M., Anthony P., Cooper G. N., Jr, Richardson P. D., Galletti P. M. Total cardiopulmonary bypass with a new microporous Teflon membrane oxygenator. Surgery. 1974 Dec;76(6):935–945. [PubMed] [Google Scholar]
- Loop F. D., Szabo J., Rowlinson R. D., Urbanek K. Events related to microembolism during extracorporeal perfusion in man: effectiveness of in-line filtration recorded by ultrasound. Ann Thorac Surg. 1976 May;21(5):412–420. doi: 10.1016/s0003-4975(10)63890-8. [DOI] [PubMed] [Google Scholar]
- Patterson R. H., Jr, Kessler J. Microemboli during cardiopulmonary bypass detected by ultrasound. Surg Gynecol Obstet. 1969 Sep;129(3):505–510. [PubMed] [Google Scholar]
- Siderys H., Herod G. T., Halbrook H., Pittman J. N., Rubush J. L., Kasebaker V., Berry G. R., Jr A comparison of membrane and bubble oxygenation as used in cardiopulmonary bypass in patients. The importance of pericardial blood as a source of hemolysis. J Thorac Cardiovasc Surg. 1975 May;69(5):708–712. [PubMed] [Google Scholar]
- Solis R. T., Noon G. P., Beall A. C., Jr, DeBakey M. E. Particulate microembolism during cardiac operation. Ann Thorac Surg. 1974 Apr;17(4):332–344. doi: 10.1016/s0003-4975(10)65661-5. [DOI] [PubMed] [Google Scholar]
- Tufo H. M., Ostfeld A. M., Shekelle R. Central nervous system dysfunction following open-heart surgery. JAMA. 1970 May 25;212(8):1333–1340. [PubMed] [Google Scholar]
- Wright G., Sanderson J. M. Brain damage and mortality in dogs following pulsatile and non-pulsatile blood flows in extracorporeal circulation. Thorax. 1972 Nov;27(6):738–747. doi: 10.1136/thx.27.6.738. [DOI] [PMC free article] [PubMed] [Google Scholar]


