Summary
Osteoarthritis is one of the most common joint disorder. For treatment of hip symptomatic osteoarthritis, when conservative medical therapy has failed, total hip arthroplasty (THA) is a successful orthopaedic procedures that reduces pain and improves function and quality of life.
Incidence of osteoarthritis is constantly increasing with raising life expectancy. This aging process also has led to an increasing number of patients with osteoporosis who need hip replacement for osteoarthritis.
Osteoporosis have 3 major potential complications in total hip arthroplasty: perioperative fracture, an increased risk of periprosthetic fracture, and late aseptic loosening.
The purpose of the present study was to examine the effects of osteoporosis on total hip replacement procedure outcome and highlight the importance of adequate study of calcium-phosphorus metabolism in patient candidate for hip surgery, and the need to start a suitable therapy to recover the bone mass before surgery. Bone quality of the hip joint has become an important risk factor limiting the durability of THA.
Keywords: total hip replacement, bone metabolism, perioperative and periprosthetic fracture
Introduction
Against a general assumption, osteoarthritis (OA) does not seem to protect from generalized primary osteoporosis. The majority (74%) of the female hip OA patients were osteopenic or osteoporotic with signs of increased bone turnover. The observed prevalence of reduced BMD corresponds with the published data of age-matched population (1). Osteoporosis and osteoarthritis are not mutually exclusive conditions, and many patients undergoing hip replacement also have unrecognized osteoporosis or deficiency of vitamin D (2).
Osteoporosis have 3 major potential complications in total hip arthroplasty (THA): perioperative fracture, an increased risk of periprosthetic fracture (Figure 1), and a risk of late aseptic loosening (Figure 2) due to mechanical failure of ingrown trabecular bone (3, 4).
Figure 1.
Periprosthetic fracture in primary osteoporosis.
Figure 2.
Aseptic loosening in patient with hyperparathyroidism.
Osteoarthritis is one of the most common joint disorder. The number of people affected with symptomatic OA is likely to increase due primarily to the aging of the population. OA has a multi-factorial etiology and it’s due to local and systemic factors. THA is a successful orthopaedic procedure for treatment of hip symptomatic OA when conservative medical therapy has failed that reduces pain and improves function and quality of life.
With increasing life expectancy the prevalence of osteoarthritis is substantially rising and hand in hand is also increasing patients that undergo surgical hip replacement (5).
The total number of THAs per year increased by 73% overall, by 123% for those 45–64 and by 54% for those 65–84 from 2000 to 2009. The rate of THA per 100K U.S. population per year increased by 59% overall, by 73% for those 45–64 and by 36% for those 65–84 (6). This aging process has led to an increasing number of patients with osteoporosis who need hip replacement for osteoarthritis.
Osteoporosis is characterized by reduced bone mass and disruption of normal bone architecture, resulting in increased risk of fragility fractures which represent the worst clinical consequence of this pathology. In 2010, 22 million women and 5.5 million men were estimated to have osteoporosis in the EU (7). Incidences of osteoporosis and fragility fractures are constantly increasing with consequent increased morbidity and mortality.
Osteoporosis can affect people of every age, mostly in adults and old people. It can be divided in primary and secondary, that depending to many cases, iatrogenic too. The primitive osteoporosis is divided in 2 types: type 1 is postmenopausal, while type 2 is senile osteoporosis. The secondary osteoporosis is a consequence of other pathological conditions, as for example: hypogonadism and other endocrine or metabolic disorders (Cushing’s syndrome, hyperparathyroidism, thyrotoxicosis, diabetes, …), neoplastic diseases and connected therapies, connective tissue diseases (rheumatoid arthritis, ankylosing spondylitis), chronic diseases (chronic obstructive pulmonary disease, congestive heart failure, chronic kidney disease), gastroenteric diseases (Crohn’s disease, celiac disease,…), nutritional problems, alcoholism, prolonged inactivity and chronic use of medicines (glucocorticoids, thyroid hormones, immunosuppressant, anticonvulsant) (8, 9).
Elderly patients have often many comorbidities and multiple general and local problems could influence the outcome of prosthetic surgery procedures. Changes in osteoporotic bone tissue lead to increased fragility and ensuing insufficient primary stability. This bone fragility implies a greater risk of iatrogenic intraoperative fractures. The long-term success of a prosthetic surgery is also the result of delicate interactions between bone and prosthesis material. Osteoporosis and abnormal bone metabolism can predispose to complications as aseptic loosening (3, 10).
The major complication in placing the femoral stem into osteoporotic bone is the periprosthetic fracture, that is associated with a high rate of postoperative complications and often a poor clinical result. The intraoperative fracture rate is approximately 4% after hip replacement (11). Variability in the reported prevalence between 0.3% and 7.8% may reflect differences in sample size or use of different femoral stems and insertion techniques (12). Risk factors for fracture have been well categorized and include: age, female sex, uncemented implants, revision surgery, and other conditions with weakens bone such as rheumatoid arthritis, Paget’s disease, and polyneuropathies (12, 13). Insertion fractures most commonly occur in the calcar region of the hip. Osteoporotic bones are very breakable and much more susceptible to intraoperative fracture than normal bone. If the bone fragility isn’t recognized at the time of stem placement, it can cause propagation of the fracture, with sharp cut fracture or stem loosening. When a periprosthesic fracture is recognize during surgery, the stem should be removed and cables should be placed around the femur shaft. Meanwhile, if the fracture propagates, plate fixation may be necessary, with a revision implant to give adequate stability. Intraoperative radiographs should be performed to ensure that the stem appears stable and that the synthesis is reliable. Prevention of these fractures is the best target, and a careful preoperative patient assessment must be performed (14).
There are no absolute age limit or weight restriction for total hip replacement. Recommendations for surgery are based on a patient’s disability and pain, not only age. Total hip replacements have been performed successfully at all ages, from the young teenager with juvenile arthritis to the elderly patient with degenerative arthritis. But higher age implies a worse functional outcome, major technical difficulties and higher operative risks. Before surgery, several factors should be evaluated: symptoms, comorbidities, physical examination, X-rays.
Discussion
Therefore, for a good success of the prosthesis, it’s essential, in addition to a good pre-surgery planning, the choice of the implant and its right surgical technique. Investigations into risk factors influencing success of total hip arthroplasty have focused primarily on the type of prosthesis and surgical technique (15). It’s also important proper focus on the patient, trying to delete all that elements that can bad influence the correct integration between bone and prosthesis, first of all the low quality of the bone (16).
Normally, during the preparation phase of hip prosthetic surgery, the patient has to undergo blood tests (complete blood count, liver and kidney function, electrolytes, coagulation profile), ECG, chest X-ray, anesthesiologist visit and additional controls about the underlying disorders. Generally, it’s not necessary to study the calcium and phosphorus metabolism. But for the importance of bone quality in implant survival, this study should be done to all women aged more 65 candidate to a prosthesis procedure, and people less than 65 but with risk factors of bone fragility. These factors are represented by: female gender, chronic drug use (e.g. glucocorticoids), previous fragility fractures, prolonged bed rest, primary and secondary amenorrhea, hypogonadism, alcohol abuse, low calcium intake, familiarity, low BMI (17).
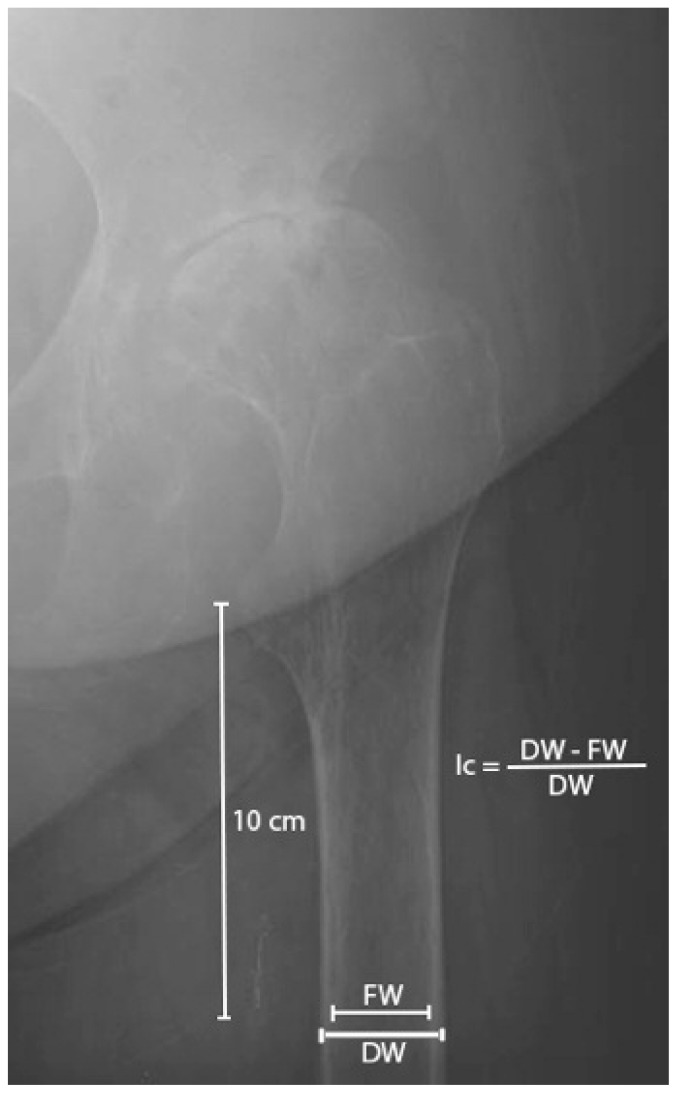
Also the radiographic patterns may help to identify patients with low bone quality. Standard radiographs are not a test for osteoporosis and have been considered less helpful in the assessment of bone mineral density because only at least a loss of 30–50% of bone mass can be detected on plain film. Cortical Thickness Index is the ratio between the endosteal and outer diameters of the proximal femur at 10 cm below the lesser trochanter (Figure 3). It showed a strong correlation with the T score (r = −0.71, P<0.001) and the best overall performance in diagnosing osteoporosis (18). Finding a hip radiography with Cortical Thickness Index value ≤ 0.40 should be a caution to recommend referral for osteoporosis evaluation and bone mineral density testing (19, 20).
Figure 3.
Femoral thickness cortical index, measured at 10 cm below the lesser trochanter. Ic: cortical index. DW: femoral diaphysis width. FW: femoral canal width.
In case of the secondary osteoporosis suspect, it’s essential to make specific exams to do a diagnosis, like: bone densitometry DXA and specific blood sample evaluation. With Ca-P metabolism we can do a differential diagnosis with other diseases that can create a clinic or densitometric profile similar to osteoporosis.
In patients that surely have severe osteoporosis, it’s essential to postpone the surgery up to the recovery of the bone mass. Anyway, it’s necessary to start a suitable integrative therapy and keep attention during the surgery (intraoperative maneuver, cemented implants). It’s strictly important to distinguish patients with secondary ostheoporosis in which the therapy of the primary cause lead to a great improvement of the osteoporosis state.
Bisphosphonates (BF) are the principal pharmaceutical agents for managing osteoporosis by the inhibition of osteoclasts resorption (21). Studies show that, in osteoporotic condition, bisphosphonates can enhance periprosthesis bone mass and the effects on osseointegration between host bone and prosthesis (22). Moreover, some studies have suggested that bisphosphonates may prevent or may be used to treat aseptic loosening (23), or to prevent the decrease in proximal femoral BMD usually seen after hip replacement (24, 25). Patients with THA and risk factors for loosening should be screened for osteoporosis and have regular radiological surveillance (3), especially if treated with BF for monitoring of any atypical periprosthesis fractures, in particular in areas neighboring the end of the prosthesis stem (26, 27).
Bone quality of the hip joint has become an important risk factor limiting the durability of THA (28).
Conclusion
In patients with an increased suspect (e.g. low femoral cortical index, previous fragility fractures, decreased T-score, …) it’s essential, as well as an evaluation of the osteoarthritic conditions, a correct study of calcium-phosphorus metabolism, to understand if we’re facing a type 1 or 2 osteoporosis, if it’s needed a therapy to increase the integration of the bone or, in case of secondary osteoporosis, if it’s necessary to treat the primary cause of the increasing bone resorption before going on with the surgery (29). It’s very important to recognize the presence of osteoporosis as it’s crucial for the final result. Our suggestion is to always do a densitometric scanning and an hematochemical evaluation for osteoporosis for all the patients who are candidate to prosthesis surgery aged more than 65 or people who have risk factors for bone fragility. The use of bisphosphonates has been effective to reduce periprosthetic bone loss and to improve implant osseointegration, but to guarantee the efficacy of this therapy it’s essential to always exclude secondary causes of osteoporosis. It’s also necessary to monitor the patient, both clinically and radiographically and with blood tests, especially in cases of BF therapies lasted for long periods.
Footnotes
Disclosure
No benefits or funds were received in support of this study. None of the Authors has any conflict of interests to disclose.
References
- 1.Mäkinen TJ, Alm JJ, Laine H, Svedström E, Aro HT. The incidence of osteopenia and osteoporosis in women with hip osteoarthritis scheduled for cementless total joint replacement. Bone. 2007 Apr;40(4):1041–7. doi: 10.1016/j.bone.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 2.Glowacki J, Hurwitz S, Thornhill TS, Kelly M, LeBoff MS. Osteoporosis and vitamin-D deficiency among postmenopausal women with osteoarthritis undergoing total hip arthroplasty. J Bone Joint Surg [Am] 2003;85-A:2371–7. doi: 10.2106/00004623-200312000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Nixon M, Taylor G, Sheldon P, Iqbal SJ, Harper W. Does bone quality predict loosening of cemented total hip replacements? J Bone Joint Surg Br. 2007 Oct;89(10):1303–8. doi: 10.1302/0301-620X.89B10.19038. [DOI] [PubMed] [Google Scholar]
- 4.Franklin J, Malchau H. Risk factors for periprosthetic femoral fracture. Injury. 2007 Jun;38(6):655–60. doi: 10.1016/j.injury.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 5.Giannotti S, Bottai V, Dell’Osso G, De Paola G, Bugelli G, Guido G. The hip prosthesis in lateral femur fracture: current concepts and surgical technique. Clin Cases Miner Bone Metab. 2014 Sep;11(3):196–200. [PMC free article] [PubMed] [Google Scholar]
- 6.Jacob MD, Jeffrey KL, Virginia B, Patricia F, David CA. Trends in Total Hip Arthroplasty in the United States: The Shift to a Younger Demographic. [Accessed 26 August 2015]. http://www.abstractsonline.com/Plan/ViewAbstract.aspx?mID=3358&sKey=d07c3db3-cf5f-4768-8384-2da45a32be4a&cKey=c1b27dc5-0efd-49a8-ad3c-19d6e9b6dd6f&mKey=4393d428-d755-4a34-8a63-26b1b7a349a1.
- 7.Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA) Arch Osteoporos. 2013;8:136. doi: 10.1007/s11657-013-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamaguchi T, Sugimoto T. Secondary osteoporosis UPDATE. The etiology, prevalence, and characteristics of secondary osteoporosis. Clin Calcium. 2010 May;20(5):637–44. [PubMed] [Google Scholar]
- 9.Fitzpatrick LA. Secondary causes of osteoporosis. Mayo Clin Proc. 2002 May;77(5):453–68. doi: 10.4065/77.5.453. [DOI] [PubMed] [Google Scholar]
- 10.James SJ, Mirza SB, Culliford DJ, Taylor PA, Carr AJ, Arden NK. Baseline bone mineral density and bone turnover in pre-operative hip and knee arthroplasty patients. Bone Joint Res. 2014 Jan 17;3(1):14–9. doi: 10.1302/2046-3758.31.2000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999 Apr;30(2):183–90. doi: 10.1016/s0030-5898(05)70073-0. [DOI] [PubMed] [Google Scholar]
- 12.Davidson D, Pike J, Garbuz D, Duncan CP, Masri BA. Intraoperative periprosthetic fractures during total hip arthroplasty. Evaluation and management. J Bone Joint Surg Am. 2008 Sep;90(9):2000–12. doi: 10.2106/JBJS.H.00331. [DOI] [PubMed] [Google Scholar]
- 13.Schwarzkopf R, Oni JK, Marwin SE. Total hip arthroplasty periprosthetic femoral fractures: a review of classification and current treatment. Bull Hosp Jt Dis. 2013;71(1):68–78. [PubMed] [Google Scholar]
- 14.Chana R, Mansouri R, Jack C, et al. The suitability of an uncemented hydroxyapatite coated (HAC) hip hemiarthroplasty stem for intracapsular femoral neck fractures in osteoporotic elderly patients: the Metaphyseal-Diaphyseal Index, a solution to preventing intra-operative periprosthetic fracture. J Orthop Surg Res. 2011;6:59. doi: 10.1186/1749-799X-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Broos P, Fourneau I. Host factors that affect outcome of total hip arthroplasty. Lancet. 2000 Apr 29;355(9214):1479–80. doi: 10.1016/S0140-6736(00)02159-0. [DOI] [PubMed] [Google Scholar]
- 16.Fini M, Giavaresi G, Torricelli P, Krajewski A, Ravaglioli A, Belmonte MM, Biagini G, Giardino R. Biocompatibility and osseointegration in osteoporotic bone. J Bone Joint Surg Br. 2001 Jan;83(1):139–43. doi: 10.1302/0301-620x.83b1.10162. [DOI] [PubMed] [Google Scholar]
- 17.Malabanan AO, Rosen HN, Vokes TJ, Deal CL, Alele JD, Olenginski TP, Schousboe JT. Indications of DXA in women younger than 65 yr and men younger than 70 yr: the 2013 Official Positions. J Clin Densitom. 2013 Oct-Dec;16(4):467–71. doi: 10.1016/j.jocd.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Yeung Y, Chiu KY, Yau WP, Tang WM, Cheung WY, Ng TP. Assessment of the proximal femoral morphology using plain radiograph-can it predict the bone quality? J Arthroplasty. 2006 Jun;21(4):508–13. doi: 10.1016/j.arth.2005.04.037. [DOI] [PubMed] [Google Scholar]
- 19.Sah AP, Thornhill TS, LeBoff MS, Glowacki Correlation of plain radiographic indices of the hip with quantitative bone mineral density. Osteoporos Int. 2007 Aug;18(8):1119–26. doi: 10.1007/s00198-007-0348-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Giannotti S, Bottai V, Dell’Osso G, Donati D, Bugelli G, De Paola G, Guido G. Indices of risk assessment of fracture of the proximal humerus. Clin Cases Miner Bone Metab. 2012 Jan;9(1):37–9. [PMC free article] [PubMed] [Google Scholar]
- 21.Stepan JJ, Alenfeld F, Boivin G, Feyen JH, Lakatos P. Mechanisms of action of antiresorptive therapies of postmenopausal osteoporosis. Endocr Regul. 2003;37:225–38. [PubMed] [Google Scholar]
- 22.Chen BL, Xie DH, Zheng ZM, Lu W, Ning CY, Li YQ, Li FB, Liao WM. Comparison of the effects of alendronate sodium and calcitonin on bone-prosthesis osseointegration in osteoporotic rats. Osteoporos Int. 2011 Jan;22(1):265–70. doi: 10.1007/s00198-010-1186-5. [DOI] [PubMed] [Google Scholar]
- 23.O’Hara LJ, Nivbrant B, Röhrl S. Cross-linked polyethylene and bisphosphonate therapy for osteolysis in total hip arthroplasty: a case report. J Orthop Surg (Hong Kong) 2004 Jun;12(1):114–21. doi: 10.1177/230949900401200121. [DOI] [PubMed] [Google Scholar]
- 24.Cavalli L, Brandi ML. Periprosthetic bone loss: diagnostic and therapeutic approaches. F1000Res. 2014 Jun 17;2:266. doi: 10.12688/f1000research.2-266.v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhandari M, Bajammal S, Guyatt GH, et al. Effect of bisphosphonates on periprosthetic bone mineral density after total joint arthroplasty: a meta-analysis. J Bone Joint Surg [Am] 2005;87-A:293–301. doi: 10.2106/JBJS.D.01772. [DOI] [PubMed] [Google Scholar]
- 26.Foster C, Robert L, Ajay L, Sun JK, David MH, Evan MS. Atypical Vancouver Type-C Periprosthetic Fracture Complicated by Nonunion A Case Report. JBJS Case Connect. 2015 May 27; doi: 10.2106/JBJS.CC.N.00180. [DOI] [PubMed] [Google Scholar]
- 27.Bottai V, Giannotti S, Dell’Osso G, De Paola G, Menconi A, Falossi F, Raffaetà G, Guido G. Atypical femoral fractures: retrospective radiological study of 319 femoral fractures and presentation of clinical cases. Osteoporos Int. 2014 Mar;25(3):993–7. doi: 10.1007/s00198-013-2546-8. [DOI] [PubMed] [Google Scholar]
- 28.Kobayashi S. Whether bone quality matters or not in durability of total hip arthroplasty? Bone quality matters in durability of total hip arthroplasty. Clin Calcium. 2011 May;21(5):746–50. [PubMed] [Google Scholar]
- 29.Giannotti S, Bottai V, Pini E, Dell’Osso G, De Paola G, Guido G. Clinical and surgical approach of severe bone fragility fracture: clinical case of 4 fragility fracture in patient with heavy osteoporosis. Clinical cases in mineral and bone metabolism. 2013;10(1):52. doi: 10.11138/ccmbm/2013.10.1.052. [DOI] [PMC free article] [PubMed] [Google Scholar]