Summary
Hypocalcemia is frequent in the setting of endocrine disorders, bone diseases and renal failure. When hypocalcemia is severe it can predispose to life-threatening ventricular arrhythmias; in such cases a rapid admission to hospital and a prompt correction of electrolyte imbalance are needed. We report the case of an old patient suffering from renal failure that was admitted to our cardiac step-down unit because of severe hypocalcemia associated with ventricular arrhythmias. Hypocalcemia was promptly treated and an endocrinologic consult was requested for investigating the causes of this electrolyte imbalance. Our experience suggests the creation of a new synergy between cardiologists and endocrinologists that led us to build a simple and schematic algorithm for the diagnosis and treatment of hypocalcemia.
Keywords: hypocalcemia, ventricular arrhythmias, diagnostic algorhytm
Introduction
Electrolyte disorders can alter cardiac ionic currents kinetics thus promoting pro-arrhythmic effects (1). In particular, calcium plays a pivotal role since it regulates for neural transmission, membrane stability, bone structure, blood coagulation and intracellular signaling. Hypocalcemia is defined as total serum calcium (Ca) concentration < 8.5 mg/dL in the presence of normal plasma protein concentrations or a serum ionized Ca concentration < 4.7 mg/dL (2) and is frequent in the setting of chronic renal dysfunction. Hypocalcemia can result in both ST segment modification and QT interval prolongation and, when severe, can predispose to life-threatening ventricular arrhythmias (3). Acute hypocalcemia can result in severe symptoms that require rapid admission to hospital and prompt correction. In contrast, when hypocalcemia develops slowly, patients can be surprisingly free of symptoms (4).
Case report
An 87-year-old woman was admitted to our cardiac step-down unit because of asthenia, nausea, emesis and oliguria. She had an history of previous myocardial infarction complicated by ischemic stroke.
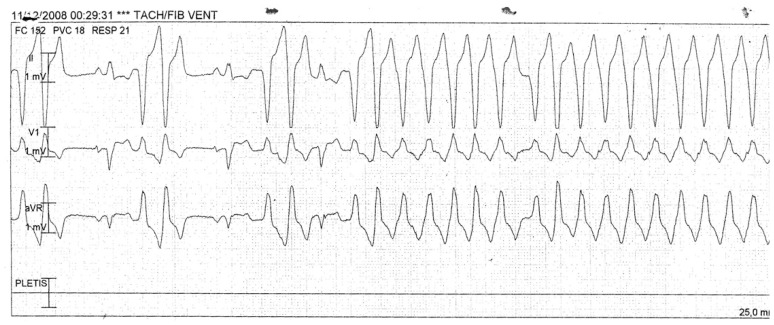
The electrocardiogram (EKG) showed sinus rhythm, pre-existing left bundle branch block (LBBB), and a frequent non-sustained ventricular tachycardia (VT) (Figures 1 and 2).
Figure 1.
EKG at admission.
Figure 2.
Allarm during continuous EKG monitoring.
An echocardiogram showed an a-kinetic posterior wall and a hypokinetic middle-basal lateral wall, with a mild reduction in left ventricular ejection fraction, and a mild mitral regurgitation.
Blood examinations showed severe hypocalcemia (3.5 mg/dL; n.v. 8.2 – 10.7 mg/dL), ionized calcium levels of 2.69 mg/dL (n.v. 4.30 – 5.30 mg/dL), hyperfosforemia (9.0 mg/dL; n.v 2.5 – 5 mg/dL) normal total proteins (6.1 g/dL n.v 6.0 –8.6 g/dL) and serum creatinine values of 2.7 mg/dL.
An infusion with calcium gluconate (2 g in 250 mL saline solution at a rate of 10 ml/h) was immediately started and after 12 hours the serum calcium concentration was 5.8 mg/dL (n.v. 8.2 – 10.7 mg/dL). An oral administration of 3 g per day of calcium carbonate was then added and after other 24 hours calcium serum concentration resulted 6.8 mg/dL. An EKG at 24 hours from the admission showed sinus rhythm, pre-existing LBBB, some ectopic ventricular beats that gradually became less frequent as calcium concentration raised above 6 mg/dL. An endocrinologic consult was acquired after which the dosage of parathormone (PTH) and vitamin D3 were requested. The following exams showed mild increase in serum PTH (8.4 pmol/L; n.v. 1.3 – 7.6 pmol/L), normal magnesium concentration, 25-0H vitamin D deficiency (7.5 ng/mL; n.v. >20 ng/mL), phosphate was 9.4 mg/dL (n.v. 2.5 – 5 mg/dL). Thyroid function indices were normal. The endocrinologic diagnosis was “hypocalcemic crisis in a patient with chronic kidney disease and severe vitamin D deficiency”. The patient fully recovered and was dismissed in a medical ward after few days; her EKG once the calcium levels were partially corrected is reported in Figure 3.
Figure 3.
EKG once the calcium level was partially corrected.
Protocol
This experience led us to draft a protocol regarding the optimal diagnostic and therapeutic strategy in patients presenting with severe hypocalcemia in a cardiology unit. This protocol was designed together with our colleagues of the Endocrinology Department and is composed of the following steps (Figure 4), in agreement with data reported in literature (4, 5).
Figure 4.
Protocol for patients presenting with severe hypocalcemia in cardiology unit (7, 8).
Conclusion
Severe electrolytes imbalances can trigger life-threatening arrhythmias and patients admitted to hospital with these alterations are frequently monitored in Cardiac Care Units.
In particular, patients with coronary artery disease and previous myocardial infarction are more prone to develop ventricular arrhythmias, so that a close monitoring is crucial in the first hours of electrolytes deficits correction.
However, whereas magnesium and potassium depletion can be easily managed and seldom require an endocrinologic consult, hypocalcemia requires a particular attention and a different approach given the complex physiological mechanisms that regulates calcium metabolism. Altered vitamin D metabolism, phosphate retention and skeletal resistance to the actions of PTH represent the main causes of hypocalcemia in patients with renal failure like the one we described in our report.
Moreover, in old patients like the one here reported, physical examination can be challenging and some of the typical signs of hypocalcemia (i.e. Trousseau’s sign, Chvostek’s sign) (4, 6) could be misinterpreted or difficult to assess.
Severe hypocalcemia is not very common in clinical practice and finding the real cause can be troublesome. In patients experiencing such severe electrolyte disorder a special attention must be paid to home medications possibly leading to this condition. In the case of our patient suffering from hypocalcemia, none of the drugs she was taking at home was found to be correlated with such dramatic low levels of calcium.
The aim of this report was to provide a tool for cardiologists and internists approaching to patients with severe hypocalcemia and severe life threatening arrhytmias. In particular, we tried to furnish an initial algorithm to distinguish between mild and severe disorders and investigate the possible etiology of this condition which is of primary importance also for early treatment. First line exams can be initially requested by cardiologists and internists; an endocrinologic consult represents the following step to investigate more deeply the causes of such a life-threatening electrolyte imbalance and outline the proper diagnostic and therapeutic approach. Our experience suggests the creation of a new synergy between cardiologists and endocrinologists.
References
- 1.El-Sherif N, Turitto G. Electrolyte disorders and arrhythmogenesis. Cardiol J. 2011;18(3):233–45. [PubMed] [Google Scholar]
- 2.Liamis G, Milionis HJ, Elisaf M. A review of drug-induced hypocalcemia. J Bone Miner Metab. 2009;27(6):635–42. doi: 10.1007/s00774-009-0119-x. [DOI] [PubMed] [Google Scholar]
- 3.Nijjer S, Ghosh AK, Dubrey SW. Hypocalcaemia, long QT interval and atrial arrhythmias. BMJ Case Reports. 2010 doi: 10.1136/bcr.08.2009.2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper MS, Gittoes NJ. Diagnosis and management of hypocalcaemia. BMJ. 2008;336(7656):1298–302. doi: 10.1136/bmj.39582.589433.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fong J, Khan A. Hypocalcemia, updates in diagnosis and management for primary care. Can Fam Physician. 2012;58(2):158–62. [PMC free article] [PubMed] [Google Scholar]
- 6.Urbano FL. Signs of hypocalcemia: Chvostek’s and Trousseau’s. Hosp Physician. 2000;36:43–5. [Google Scholar]