This study analyzed palliative/supportive care use in a single cancer center over 8 years. Billing data showed the inpatient consultations as a percentage of hospital admissions and the ratio of inpatient consultations to hospital beds almost doubled. In the outpatient setting, data revealed earlier access to outpatient referrals to palliative care service (from 4.8 months to 7.9 months; p = .001) during the study period.
Keywords: Palliative care, Supportive Care, Cancer, End-of-life care
Abstract
Background.
Despite increasing prevalence of palliative care (PC) services in cancer centers, most referrals to the service occur exceedingly late in the illness trajectory. Over the years, we have made several attempts to promote earlier patient access to our PC program, such as changing the name of our service from PC to supportive care (SC). This study was conducted to determine the use of PC/SC service over the past 8 years.
Methods.
We reviewed billing data for all PC/SC encounters. We examined five metrics for use: inpatient consultations as a percentage of hospital admissions, ratio of inpatient consultations to average number of operational beds, time from hospital registration to outpatient consultation, time from advanced cancer diagnosis to consultation, and time from first outpatient consultation to death/last follow-up.
Results.
Over the years, we found a consistent increase in patient referrals to the PC/SC program. In the inpatient setting, we found approximate doubling of the inpatient consultations as a percentage of hospital admissions and the ratio of inpatient consultations to hospital beds (from 10% to 19% and from 2.4 to 4.9, respectively; p < .001). In the outpatient setting, we observed variations in referral pattern between oncology services, but, overall, the time from consultation to death/last follow-up increased from 4.8 months to 7.9 months (p = .001), which was accompanied by a significant decrease in the interval to consultation from hospital registration and advanced cancer diagnosis (p < .001).
Conclusion.
We have observed a consistent annual increase in new patient referrals as well as earlier access for outpatient referrals to our SC service, supporting increased use of palliative care at our cancer center.
Implications for Practice:
In response to accumulating evidence on the benefits of palliative care (PC) referral to oncology patients, efforts are being made to increase PC use. This study, conducted at MD Anderson Cancer Center, demonstrates consistent annual growth in PC referrals, which was accompanied by a significant increase in the outpatient referral of patients with nonadvanced cancer and earlier referral of those with advanced cancer. However, significant variations in the referral patterns between oncology services were observed. These results have implications for other cancer centers looking to enhance use of PC services by having a business model that allows for appropriate space and staff expansion.
Introduction
Patients with advanced cancer experience a number of physical and psychosocial symptoms that adversely impact quality of life [1–4]. Early referral of these patients to specialized palliative care (PC) programs contributes to timely symptom management, and is supported by randomized clinical trials [5–7]. In the U.S., the Institute of Medicine and leading oncology organizations such as the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network advocate for early access to PC services wherein oncological and PC services are offered concurrently [8–11]. In response, there has been a progressive increase in the establishment of nonhospice PC programs in cancer centers and general hospitals all around the U.S. [12, 13]. The prevalence of PC services in hospitals with 50 or more beds has dramatically increased in the past 12 years, with more than two-thirds reporting the presence of a PC program in 2012, as compared with less than one-quarter in 2000 [13]. However, in the overwhelming majority of situations, these referrals either do not occur or, when they do, are exceedingly late in the illness trajectory [12, 14–19].
Although a number of barriers to early PC referrals have been recognized [20], the name palliative care was found to be a deterrent by our group [21] and by others [22, 23]. To promote earlier patient access to our PC program, we changed the name of our inpatient consultation team and outpatient center from PC to supportive care (SC) in November 2007. As previously reported [24], immediately following the service name change, we observed a significant increase in the number of new patient referrals in the inpatient setting, and a significant increase in the number of patients in earlier stages of illness in the outpatient center. These findings supported our hypothesis that the term supportive care is more conducive to referral and would facilitate integration between oncology and PC teams. We conducted this study to determine the changes in the pattern of PC/SC referral over time, and to examine the use of PC/SC services at our comprehensive cancer center for the past 8 years.
Patients and Methods
The institutional review board at The University of Texas MD Anderson Cancer Center (UTMDACC) reviewed and approved this retrospective study and waived the requirement of informed consent.
We obtained financial data corresponding to the institution’s fiscal year (FY) from FY 2007 through 2014 to record all billed PC/SC patient encounters. These included consultation and follow-up visits for the inpatient and outpatient settings. We excluded visits by the psychologist, for the purpose of this study, to adhere to a maximum of one billing by the service for each patient per day. Each FY starts on September 1 of the preceding year and ends with August 31 of that FY. As an example, FY 2007 started on September 1, 2006, and concluded August 31, 2007. Because the service name change from PC to SC occurred in November 2007 (FY 2008), we defined FY 2007 as the period prename change, FY 2009 as the period immediately following name change, and FY 2013 as the period 5 years following the name change.
In this study, we report data on the absolute number of patient encounters for the inpatient and outpatient settings, and the relative (%) growth from one FY as compared with the prior FY. We also compared the annual growth rate for the PC/SC program with the growth rate of the Division of Cancer Medicine (DoCM) and the whole institution (UTMDACC) for the past 5 years.
In the inpatient setting, we examined two metrics for use. First, we looked at the Center to Advance Palliative Care (CAPC) recommended PC consultation service metrics of the number of PC consultations per 100 admissions [25], as a measure of PC integration at our cancer center. This PC consultation rate (%) for each FY was calculated as the number of inpatient PC consultations divided by the total number of admissions for the DoCM and Internal Medicine service. Second, we also used our previously reported metric of the ratio of inpatient consultations to the average number of inpatient operational beds per FY [26].
In the outpatient setting, we examined the timing of access for new patient consultations by examining the following time intervals: (a) the interval between date of first visit to the cancer center (date of hospital registration) to first PC/SC consultation, (b) the interval between date of advanced cancer diagnosis to first PC/SC consultation, and (c) the interval between date of first PC/SC consultation and date of death or last follow-up.
Electronic medical records were reviewed to obtain information pertinent to patient demographics (age at first consultation, sex, and ethnicity), date of birth, cancer type and stage, date of first known advanced cancer status at UTMDACC, and the date of hospital registration. Advanced cancer was defined as the presence of locally recurrent or metastatic disease for solid tumors, and relapsed or refractory disease status for hematologic malignancies; data on patients with advanced cancer were extracted for years 2007, 2009, 2012, and 2013. Patients who were unable or unwilling to receive curative- intent therapies for any reason, or were referred for phase I treatment, were considered to have advanced cancer. The date of advanced cancer status was the first date when the patient was identified as having advanced disease status by the oncologist. In cases of patients with multiple malignancies, data were collected for the cancer most likely responsible for the patient’s death. The date of death was obtained from a Social Security Death Index interactive search and hospital administrative records.
Statistical Analysis
Descriptive statistics were used to summarize outpatient demographics, including medians, 95% confidence intervals (CIs), ranges, frequencies, and percentages. Comparison between time periods was conducted using the Kruskal-Wallis test for continuous variables and the chi-square test for categorical variables. The timing of outpatient PC/SC was examined with survival curves, using the Kaplan-Meier method and compared among years using the log-rank test of equality over strata and using the Cox proportional hazards regression model. Significance levels less then 0.05 were considered statistically significant. The Statistical Package for the Social Sciences version 19.0 (IBM Corp., Chicago, IL, http://www-01.ibm.com) software was used for statistical analysis.
Results
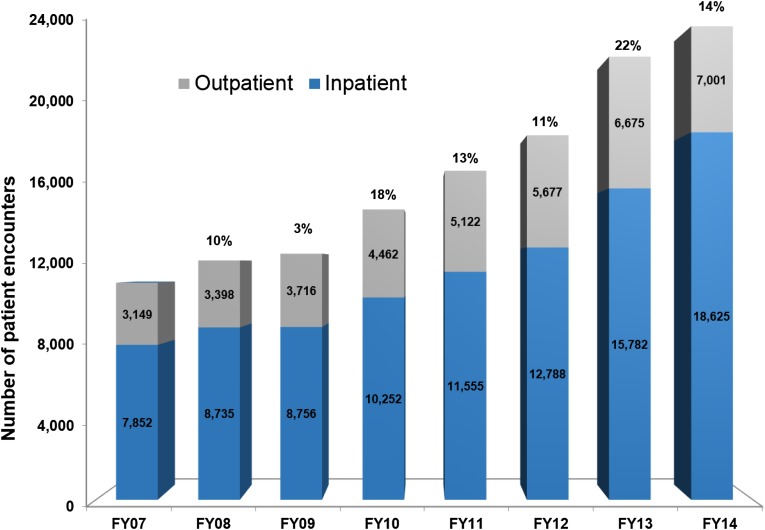
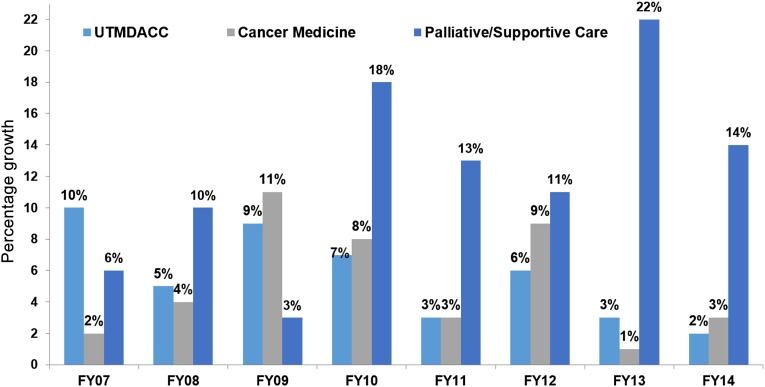
Figure 1 shows the total number of patient encounters seen by the PC/SC service during FYs 2007–2014, as well as the percentage growth for each FY as compared with the prior year. As shown, a majority of patient activity and growth occurred in the inpatient setting. Figure 2 demonstrates that the rate of growth in patient activity for the PC/SC service was higher relative to the Division of Cancer Medicine and the whole institution for the past 5 years.
Figure 1.
Increase in total patient activity for both inpatient and outpatient palliative/supportive care services (FYs 2007–2014).
Abbreviation: FY, fiscal year.
Figure 2.
Comparison of the percentage growth in total patient activity among the palliative/supportive care service, Division of Cancer Medicine, and the UTMDACC (FYs 2007–2014).
Abbreviations: FY, fiscal year; UTMDACC, University of Texas MD Anderson Cancer Center.
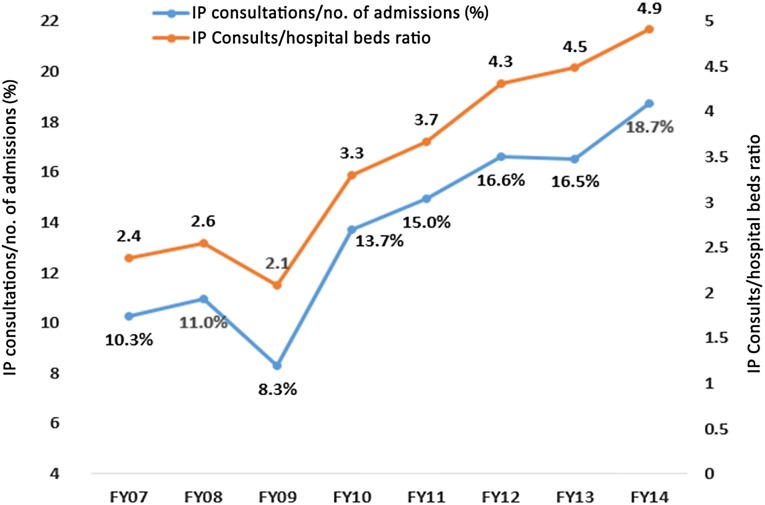
Figure 3 illustrates the dramatic growth in the use of PC/SC services in the inpatient setting for the past 8 years, as assessed by the percentage of PC/SC consultations to hospital admissions, a measure proposed by CAPC, as well as the ratio of inpatient consultation to the average number of operational beds [26]. As shown in Figure 3, the inpatient consultations as a percentage of hospital admissions increased from 10% in FY 2007 to 19% in FY 2014 (p < .001), and the ratio of the number of inpatient consultations to average hospital beds also increased (2.4 to 4.9; p < .001) during this time.
Figure 3.
Palliative/supportive care (PC/SC) service use among hospital admissions as assessed by percentage of PC/SC consultations divided by number of hospital admissions for oncology and internal medicine service (blue) and the ratio of the number of consultations to the average number of nonsurgical hospital beds (orange) (FYs 2007–2014).
Abbreviations: FY, fiscal year; IP, inpatient.
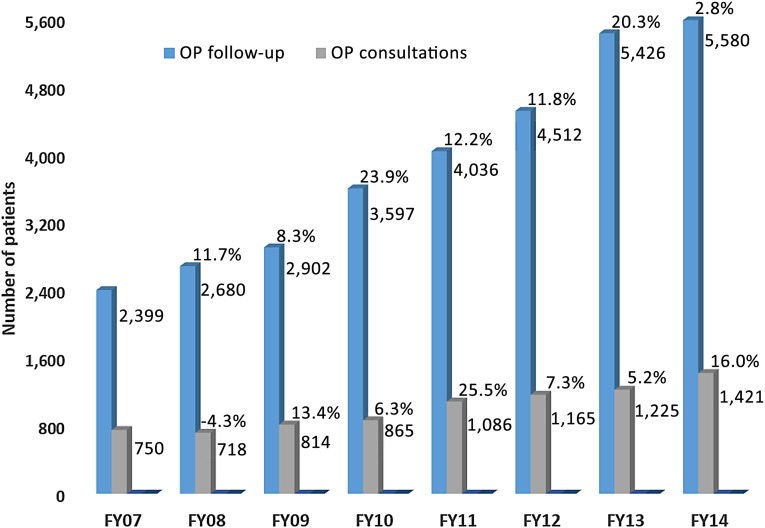
Outpatient Clinical Activity: Follow-Up and New Consultation Visits
Figure 4 demonstrates total outpatient activity (consultation and follow-up visits) and the percentage growth in activity each FY as compared with the prior year. We observed an increased growth in new consultations in the period immediately following the name change (FY 2009; 13%), which was followed by an increased growth in follow-up visits (24%) in following year (FY 2010; 24%). In FY 2011, we observed the highest percentage growth in new consultations (26%), which was followed by a higher growth in follow-up activity as compared with new consultations in FYs 2012 (12%) and 2013 (20%).
Figure 4.
Growth of OP consultations and follow-up visits (FYs 2007–2014).
Abbreviations: FY, fiscal year; OP, outpatient.
Timing of Referral to the Outpatient Palliative/Supportive Care Service
Timing of patient access to the SC/PC service was evaluated by examining when the patient was referred with respect to hospital registration, first known date of advanced cancer status, and the time interval from consultation to death/or last follow-up. Advanced cancer status and the date of hospital registration was available for FYs 2007, 2009, 2012, and 2013.
Referral of Patients With Advanced Versus Those With Nonadvanced Cancer
In FY 2007, approximately 12% of new patient consultations (n = 92) were with patients who had a nonadvanced cancer diagnosis; this increased significantly to 19% (n = 155; p < .001) in FY 2009. In FYs 2012 and 2013, respectively 19% (n = 221) and 21% (n = 257) of patients seen for new consultations had a nonadvanced cancer diagnosis, which was not significantly different from FY 2009 (p = .39).
Time Interval From Advanced Cancer Diagnosis to Consultation
Among patients with advanced cancer, the median interval from date of advanced cancer status to PC/SC consultation was 5.5 months in FY 2013, which was significantly shorter than in FY 2007 (7.9 months; hazard ratio [HR]: 0.8; 95% CI: 0.7–0.9) but not in FY 2009 (4.7 months; HR: 1.0; 95% CI: 0.9–1.1) (Table 1).
Table 1.
Time interval to outpatient PC/SC consultation from date of registration and dates of advanced cancer diagnosis and hospital registration for FYs 2007, 2009, and 2012 compared with FY 2013
Time Interval From Hospital Registration to First PC/SC Consultation
The median interval from date of hospital registration to PC/SC consultation was significantly shorter in FY 2013 (6.7 months) as compared with FY 2007 (14.8 months; HR: 0.8; 95% CI: 0.7–0.8) and 2009 (9.4 months; HR: 0.8; 95% CI: 0.8–1.0) (Table 1).
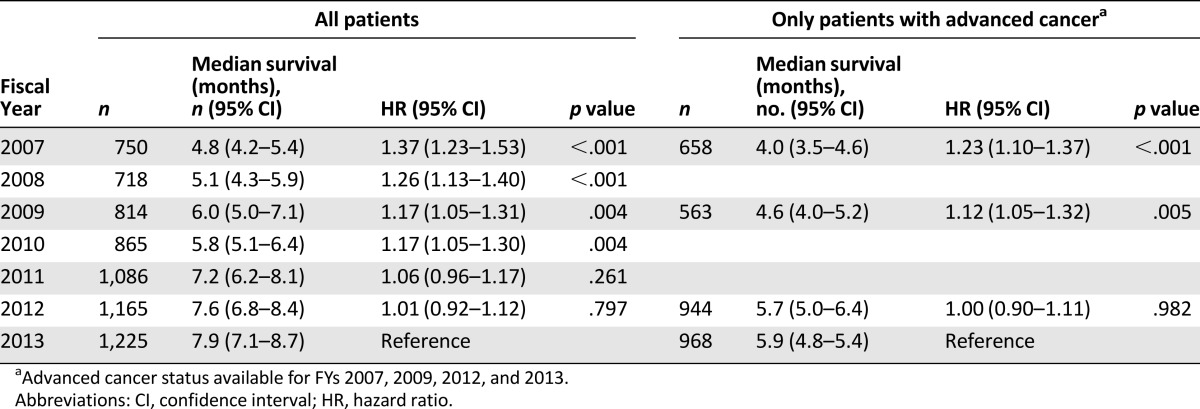
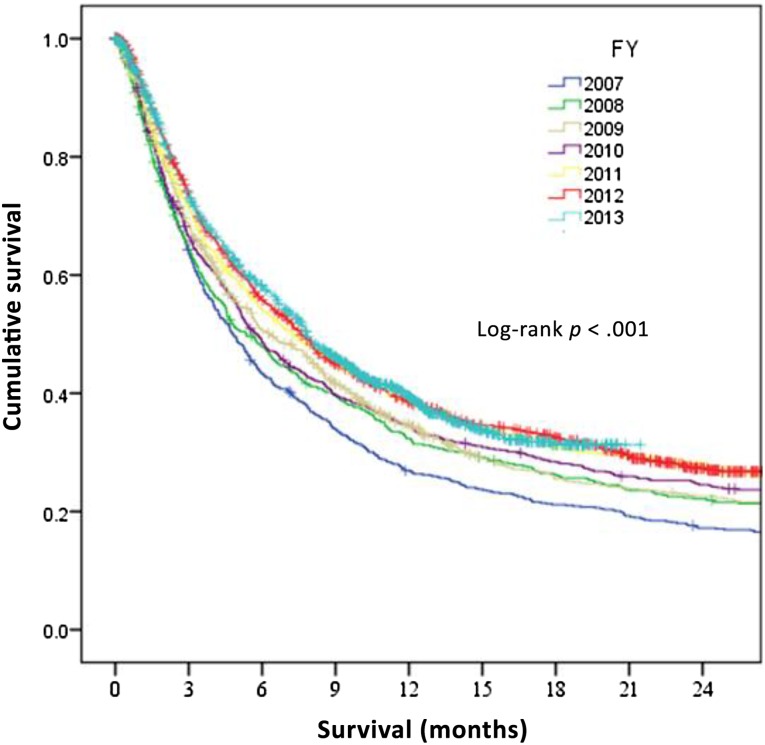
Time Interval First PC/SC Consultation to Death or Last Follow-Up
The median interval between PC/SC and death consistently increased between FY 2007 and FY 2013, from 4.8 months to 7.9 months (Table 2; Fig. 5). When only patients with advanced cancer were included, the median interval between PC/SC and death in FY 2013 remained significantly higher than in FYs 2007 and 2009, and was similar to FY 2012 (Table 2).
Table 2.
Median survival estimates from date of outpatient consultation for FYs 2007–2012 as compared with FY 2013
Figure 5.
Kaplan-Meier estimates for overall survival from first outpatient palliative/supportive care consultation for FYs 2007–2013.
Abbreviation: FY, fiscal year.
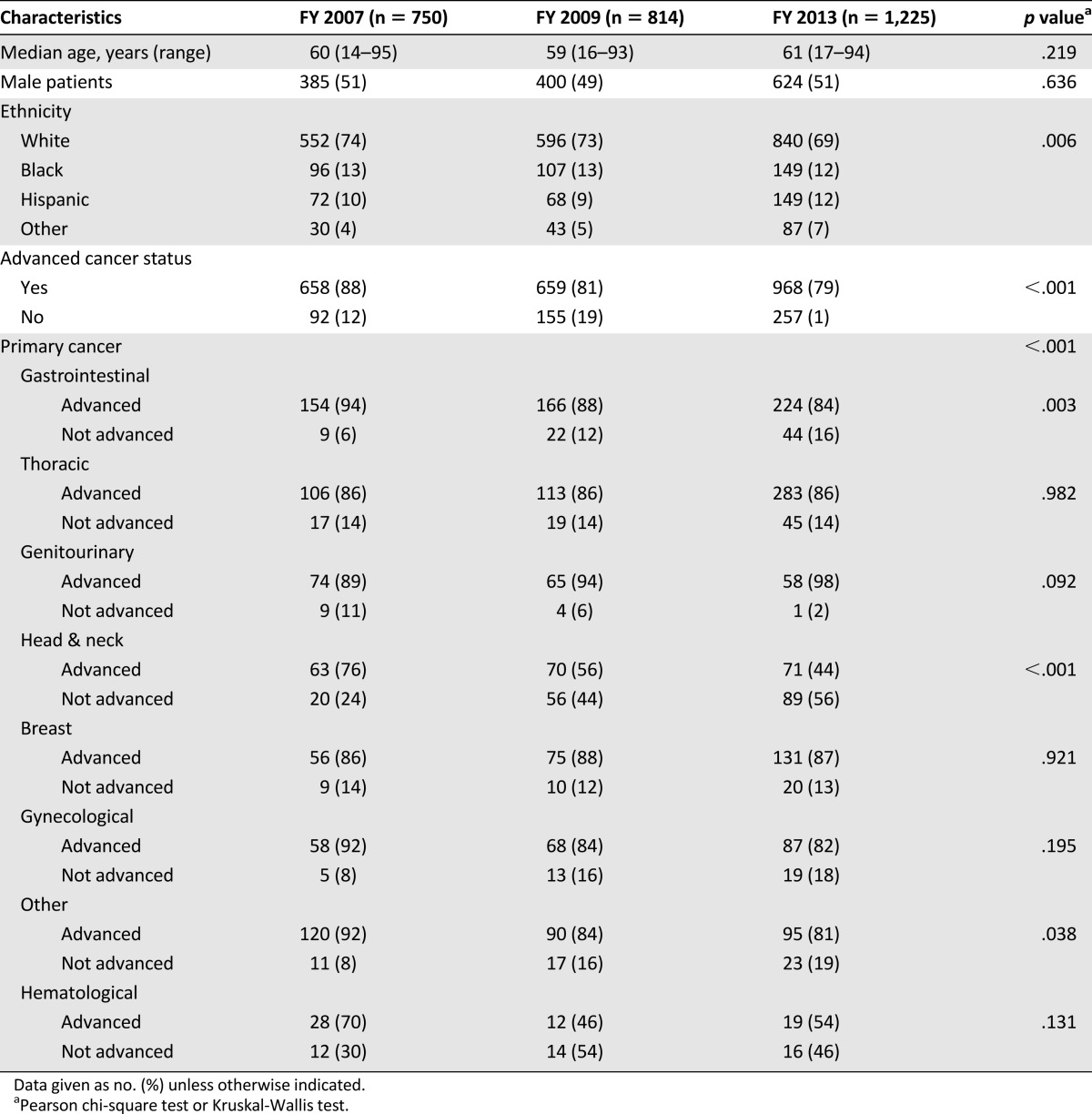
Characteristics of New Patient Referrals in the Outpatient Center
Table 3 compares patient demographics and referring oncology services for FYs 2007, 2009, and 2013. The table further characterizes patients based on whether they had advanced or nonadvanced cancer status.
Table 3.
Characteristics of outpatient referrals for FYs 2007, 2009, and 2013
Overall, a majority of the patients referred in all 3 years were from the gastrointestinal (GI) and thoracic service. In FY 2013, there was a significant increase (p < .001) in referrals from the thoracic service (n = 328) as compared with FYs 2007 and 2009 (123 and 132 patients, respectively), from the breast service as compared with FY 2007 (151 vs. 65 patients) and a significant decline (p < .001) in referral from the genitourinary (GU) service (as compared with both prior years) and hematological services as compared with FY 2007. For head and neck cancers, there was a significant increase in referrals in FY 2009 as compared with FY 2007, and with no further significant increase in FY 2013. For other oncology services, such as GI and gynecological (GYN), although there was an increase in the number of patients in FY 2013 as compared with prior years, this did not achieve statistical significance.
For patients with head and neck cancers, we observed a significant increase in referral of patients with nonadvanced cancer in 2009 (44% vs. 24% in FY 2007; p < .001) that was not associated with further significant increase in FY 2013 (56%). We also observed an increase in referral of patients with nonadvanced cancer in FY 2013 as compared with FY 2007 for GI (16% vs. 6%; p = 0.003) and other cancers (19% vs. 8%; p = 0.04). Table 3 also demonstrates that for breast and thoracic cancers that were associated with increases in referral in FY 2013, there was no corresponding change in percentage of patients with nonadvanced cancer status.
We found no differences in the median age and sex between these time periods. There were significantly more Hispanic patients referred in FY 2013, however, as compared with FY 2009 and other ethnicities as compared with FY 2007.
Discussion
In this study, we have observed consistent growth in the number of new patient referrals to a SC/PC program for both the inpatient and outpatient settings, and that this number exceeded the growth in new patient referrals of both the medical oncology and the overall cancer center. In addition, in the outpatient center, we observed earlier referral to the service in the patient’s cancer trajectory, as evidenced by an increase in the number of referrals of patients with nonadvanced cancer status, a longer median time interval from initial consultation date to death, and shorter time intervals from dates of advanced cancer diagnosis and hospital registration to consultation.
In response to the accumulating evidence demonstrating improved clinical outcomes for patients with advanced cancer [5–7], leading national and international oncology organizations advocate for early access to PC services where oncological and PC services are offered concurrently [8–11, 27]. Over the years, our team has made several efforts to increase referral to our service from various oncology services, such as providing grand-round presentations and discussing perceived challenges to such referral by oncologists [28]. In response to a survey of oncology clinicians conducted at our cancer center [21], we changed the name of our consultation service from PC to supportive care, and, as previously reported, found a significant increase in the number of referrals overall, although earlier referral to the service was only demonstrated for the outpatient center [24]. The results of our current study, conducted 5 years after the name change, is highly encouraging, as it demonstrates continued growth in use of PC/SC services, as shown in Figures 1–4. In the outpatient center, we also observed an increase in the referral of patients with nonadvanced cancer in FY 2009, with 19% of referrals having a nonadvanced cancer status as compared with 12% in FY 2007, although this increase appeared to have plateaued in subsequent years (19% and 21% for FYs 2012 and 2013, respectively). The increased growth in PC/SC services use overall and at earlier times in the illness trajectory at UTMDACC is highly encouraging; however, this represents only one measure of such integration. Integration is a complex and heterogeneous concept [29]. Findings from a recent Delphi Survey conducted by our team resulted in the proposal of 13 major and 30 minor indicators of integration among clinical structures, processes and outcomes, education, and research [30]. Although presence of both inpatient and outpatient PC services is a major indicator of integration, a majority of PC services offered across U.S. cancer centers and hospitals are inpatient consultation services, and these lack outpatient clinics [12, 13]. These inpatient programs are much easier to set up than outpatient clinics, and although they provide much-needed symptomatic relief to hospitalized ill patients [31], referral to these inpatient programs has consistently occurred exceedingly late in the illness trajectory [12, 14–19]. This is not surprising, as admissions to acute care facilities are mainly due to complications of disease or its treatment, such as infections, thrombosis, and/or uncontrolled symptoms that are more common in advanced stages of illness. In the inpatient setting, we found an approximate doubling of the percentage (from 10% to 19%) of inpatient PC/SC consultations to number of hospital oncology service admissions as well as in the ratio (from 2.4 to 4.9) of the number of inpatient consultations to number of oncology service hospital beds.
As reported in the current study and in our prior study [24], the outpatient clinic allows for earlier access to the PC service, which has been described as one of the major indicators for integration [30]. While not assessed in the current study, our group has previously observed that earlier and outpatient referrals are much more likely to be associated with favorable end-of-life care quality indicators such as chemotherapy in the last 14 days of life, emergency room visits, and hospital and intensive care unit admissions in the last 30 days of life, defined by the ASCO Quality Oncology Practice Initiative [32] and the National Quality Forum [33], as compared with late and inpatient referrals [34]. In addition, among the three randomized controlled trials (RCTs) that demonstrated improved cancer patient-related outcomes of PC [5–7], two were conducted in the outpatient setting and at earlier times in the illness [5, 7]. Collectively, these data suggest that the outpatient PC programs are crucial in achieving the objectives of providing earlier access to PC services and improving relevant clinical outcomes for these patients.
Our present study demonstrates that the adoption of PC by different oncology services was not uniform, as there were significant variations in referral patterns between services (Table 3). A majority of the significant growth in referrals observed in FY 2013 occurred because of increased referrals from the thoracic and breast oncology services, whereas some services such as GU, hematological, and other cancer types had significant declines in referral. Although there was an increase in the number of patient referred from GI and GYN services in FY 2013 as compared with prior years, this did not achieve significance.
Furthermore, the increased referral of patients with nonadvanced cancer observed in FY 2009 and that persisted in FY 2013 was mainly due to the significant increase in patients with head and neck cancer. In FY 2013, 35% of all patients with nonadvanced cancer were from the head and neck oncology service, followed by GI and thoracic services (17% each). Among patients referred from head and neck oncology services, those with nonadvanced cancer accounted for 44% of referrals, which was significantly higher than 24% in FY 2007; in FY 2013, a majority (56%) of referrals had a nonadvanced cancer diagnosis. The increased referral of patients with nonadvanced cancer initially observed in 2009 may partly be explained by the change in the service name that occurred in FY 2008. It is well recognized that patients with head and neck cancer in early stages of illness have several sources of physical and emotional distress secondary to pain, limitations in basic functions, need for nutritional support, and visible deformities. Furthermore, treatments such as radiation therapy that are standard of care in many early stages of illness cause transient, expected side effects of painful mucositis in these patients, who can benefit from the PC/SC team. In contrast to head and neck cancers, the increase in referral of outpatients with thoracic and breast cancers seen in FYs 2009 or 2013 was not associated with a corresponding increase in the percentage of patients with nonadvanced cancer.
Overall, the time interval from first outpatient consultation to death/last follow-up increased over time, from a median of approximately 5 months in 2007 to 6 months in 2009 and to 8 months in 2013. Our data also confirm that it was not just the inclusion of patients with nonadvanced cancer that influenced the survival interval from PC/SC consultation, because when we only included patients with advanced cancer in the analysis, significant improvements persisted in FY 2013 as compared with FYs 2007 and 2009 (Table 2), suggesting that patients with advanced cancer were being referred at an earlier time in their illness. However, our data also reveal that the timing of access to the service was reaching a plateau, as evident by no further increases in the percentage of referrals of patients with nonadvanced cancer since FY 2009 and the time interval from consultation to death for 2013, as compared with 2011 and 2012 (Table 2). Despite this, these data are highly encouraging, as they are an indication of dramatically earlier access as compared with our prior survey of national cancer centers [12], which found that the survival from PC referral ranged from 41 to 90 days, and as compared with hospice programs in which the median survival from hospice enrollment to death was less than 3 weeks [35].
Our data have implications for other cancer centers looking to enhance the PC services use. One challenging aspect of seeing increased numbers of patients and at earlier times in the illness trajectory are the limitations in space and resources. Particularly in the outpatient center, increased growth will have an impact on existing clinic resources such as space, staffing, and clinic templates. Increased numbers of new patient referrals would impact the ability to accommodate adequate follow-up visits for previously established patients. Findings from our group suggest that patients who are seen as outpatient consultations require early follow-up visits because multiple symptoms remain uncontrolled after the first SC/PC encounter [36, 37]. Thus, a business model that allows for space and staff expansion will be necessary to accommodate the increase in patient referrals without compromising patient care and adequate number of follow-up visits for previously established patients. We have previously shown that to keep up with increased growth in referral and workload, there needs to be appropriate and timely recruitment of PC clinicians [26]. In FY 2012, we added a second outpatient clinic and increased outpatient palliative clinic physicians from 2 to 3, and again, based on the continued growth, expanded the clinic to 3 locations within the cancer center and increased clinic physicians to 4 per day in FY 2014. Recent data highlight a high burnout rate among PC clinicians (62%) when the workload is high [38]. Our data are useful in characterizing the potential time of referral within the patients’ cancer trajectory. Cancer centers may need to make decisions regarding thresholds of patient referral depending on available resources.
The current study has several limitations. First, data collection was done retrospectively. An alternative design of a prospective trial was not feasible logistically or financially. Second, our results are based on patients seen at our tertiary care cancer center who may differ from a community practice setting in regard to receiving more cancer treatments or in their participation in clinical trials for advanced disease, thereby limiting the generalizability of our findings. Third, while the name change of service may have contributed to increasing referrals, especially of patients with head and neck cancer in earlier changes of illness, it is not possible for us to definitely establish a causal relationship. Other potential confounders, such as familiarity with our program and changing attitudes and beliefs of referring oncology professionals, likely contributed. Fourth, while we demonstrated earlier referral of patients with cancer in their illness trajectory to the outpatient center, the clinical significance of such earlier referral is not known. The ASCO provisional clinical opinion recommends early PC referral for patient with metastatic cancers and/or high symptom burden [8]; however, there is no consensus on the optimal timing of PC initiation. In the Temel et al. study of patients with metastatic lung cancer [5], PC referral within 8 weeks of diagnosis improved patient outcomes, whereas in the recently published ENABLE III (Early vs. Later Palliative Cancer Care: Clinical and Biobehavioral Outcomes) RCT [39], no difference in patient-reported outcomes was found when patients were referred early (within 2 months of advanced cancer diagnosis) or late (more than 3 months after diagnosis). Findings from our team have shown that outpatients who are referred to PC teams and who fail to show for their follow-up visits are more likely to have a lower symptom burden at baseline than those patients who return for their scheduled follow-up visit [36]. These findings suggest that some patients in earlier stages of illness with low burden of symptoms may find outpatient palliative care to be less useful. More research on the optimal timing of referral of cancer patients is needed.
Conclusion
Our findings indicate that the growth of a supportive/palliative care program at the UTMDACC has been larger than the growth of the medical oncology program and the institution as a whole. Our findings also suggest that earlier access has accompanied increased access, as demonstrated by the increasing time from supportive and palliative care referrals to death and the increasing percentage of patients with early cancer seen in the outpatient setting.
Acknowledgments
David Hui is supported in part by a National Institutes of Health grant (R21CA186000-01A1) and an American Cancer Society Mentored Research Scholar Grant in Applied and Clinical Research (MRSG-14-1418-01-CCE). Eduardo Bruera is supported in part by National Institutes of Health Grants R01NR010162-01A1, R01CA122292-01, and R01CA124481-01.
This study was reported in part as a poster presentation at the 2014 Annual Meeting of the American Society of Clinical Oncology.
Footnotes
For Further Reading: David Hui, Minjeong Park, Diane Liu et al. Attitudes and Beliefs Toward Supportive and Palliative Care Referral Among Hematologic and Solid Tumor Oncology Specialists. The Oncologist 2015;20:1326–1332.
Implications for Practice: The present survey of oncology specialists found that hematologic specialists were less likely than solid tumor specialists to report that they would refer symptomatic patients with newly diagnosed cancer to palliative care. However, both groups were significantly more willing to refer patients early in the disease trajectory if the service name “supportive care” were used instead of “palliative care.” These findings suggest that rebranding might help to overcome the stigma associated with palliative care and improve patient access to palliative care services.
Author Contributions
Conception/Design: Shalini Dalal, Sebastian Bruera, David Hui, Sriram Yennu, Rony Dev, Janet Williams, Eduardo Bruera
Provision of study material or patients: Shalini Dalal, Janet Williams, Emmanuel Obasi, Eduardo Bruera
Collection and/or assembly of data: Shalini Dalal, Sebastian Bruera, Janet Williams, Charles Masoni, Ijeoma Ihenacho, Emmanuel Obasi
Data analysis and interpretation: Shalini Dalal, David Hui, Eduardo Bruera
Manuscript writing: Shalini Dalal, Sebastian Bruera, David Hui, Sriram Yennu, Rony Dev, Eduardo Bruera
Final approval of manuscript: Shalini Dalal, David Hui, Sriram Yennu, Rony Dev, Eduardo Bruera
Disclosures
The authors indicated no financial relationships.
References
- 1.Cheung WY, Le LW, Zimmermann C. Symptom clusters in patients with advanced cancers. Support Care Cancer. 2009;17:1223–1230. doi: 10.1007/s00520-009-0577-7. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 3.Walsh D, Donnelly S, Rybicki L. The symptoms of advanced cancer: Relationship to age, gender, and performance status in 1,000 patients. Support Care Cancer. 2000;8:175–179. doi: 10.1007/s005200050281. [DOI] [PubMed] [Google Scholar]
- 4.McMillan SC, Small BJ. Symptom distress and quality of life in patients with cancer newly admitted to hospice home care. Oncol Nurs Forum. 2002;29:1421–1428. doi: 10.1188/02.ONF.1421-1428. [DOI] [PubMed] [Google Scholar]
- 5.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 6.Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The Project ENABLE II randomized controlled trial. JAMA. 2009;302:741–749. doi: 10.1001/jama.2009.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: A cluster-randomised controlled trial. Lancet. 2014;383:1721–1730. doi: 10.1016/S0140-6736(13)62416-2. [DOI] [PubMed] [Google Scholar]
- 8.Smith TJ, Temin S, Alesi ER, et al. American Society of Clinical Oncology provisional clinical opinion: The integration of palliative care into standard oncology care. J Clin Oncol. 2012;30:880–887. doi: 10.1200/JCO.2011.38.5161. [DOI] [PubMed] [Google Scholar]
- 9.Levy MH, Adolph MD, Back A, et al. Palliative care. J Natl Compr Canc Netw. 2012;10:1284–1309. doi: 10.6004/jnccn.2012.0132. [DOI] [PubMed] [Google Scholar]
- 10.Levit L, Balogh E, Nass S, et al. Washington, DC: National Academies Press; 2013. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. [PubMed] [Google Scholar]
- 11.Foley KM, Gelband H, editors. Washington, DC: National Academies Press; 2001. Improving Palliative Care for Cancer: Summary and Recommendations. National Cancer Policy Board; Institute of Medicine; National Research Council. [PubMed] [Google Scholar]
- 12.Hui D, Elsayem A, De la Cruz M, et al. Availability and integration of palliative care at US cancer centers. JAMA. 2010;303:1054–1061. doi: 10.1001/jama.2010.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Center to Advance Palliative Care. Growth of palliative care in U.S. hospitals: 2014 snapshot. Available at https://media.capc.org/filer_public/6d/db/6ddbbaa1-0c03-4e34-9186-696bbc158950/capc_growth_snapshot_2014.pdf. Accessed November 10, 2015.
- 14.Hui D, Kim SH, Kwon JH, et al. Access to palliative care among patients treated at a comprehensive cancer center. The Oncologist. 2012;17:1574–1580. doi: 10.1634/theoncologist.2012-0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng WW, Willey J, Palmer JL, et al. Interval between palliative care referral and death among patients treated at a comprehensive cancer center. J Palliat Med. 2005;8:1025–1032. doi: 10.1089/jpm.2005.8.1025. [DOI] [PubMed] [Google Scholar]
- 16.Osta BE, Palmer JL, Paraskevopoulos T, et al. Interval between first palliative care consult and death in patients diagnosed with advanced cancer at a comprehensive cancer center. J Palliat Med. 2008;11:51–57. doi: 10.1089/jpm.2007.0103. [DOI] [PubMed] [Google Scholar]
- 17.Good PD, Cavenagh J, Ravenscroft PJ. Survival after enrollment in an Australian palliative care program. J Pain Symptom Manage. 2004;27:310–315. doi: 10.1016/j.jpainsymman.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 18.Morita T, Akechi T, Ikenaga M, et al. Late referrals to specialized palliative care service in Japan. J Clin Oncol. 2005;23:2637–2644. doi: 10.1200/JCO.2005.12.107. [DOI] [PubMed] [Google Scholar]
- 19.Reville B, Miller MN, Toner RW, et al. End-of-life care for hospitalized patients with lung cancer: Utilization of a palliative care service. J Palliat Med. 2010;13:1261–1266. doi: 10.1089/jpm.2010.0057. [DOI] [PubMed] [Google Scholar]
- 20.Von Roenn JH, Voltz R, Serrie A. Barriers and approaches to the successful integration of palliative care and oncology practice. J Natl Compr Canc Netw. 2013;11(suppl 1):S11–S16. doi: 10.6004/jnccn.2013.0209. [DOI] [PubMed] [Google Scholar]
- 21.Fadul N, Elsayem A, Palmer JL, et al. Supportive versus palliative care: What’s in a name?: A survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer. 2009;115:2013–2021. doi: 10.1002/cncr.24206. [DOI] [PubMed] [Google Scholar]
- 22.Miyashita M, Hirai K, Morita T, et al. Barriers to referral to inpatient palliative care units in Japan: A qualitative survey with content analysis. Support Care Cancer. 2008;16:217–222. doi: 10.1007/s00520-007-0215-1. [DOI] [PubMed] [Google Scholar]
- 23.Morstad Boldt A, Yusuf F, Himelstein BP. Perceptions of the term palliative care. J Palliat Med. 2006;9:1128–1136. doi: 10.1089/jpm.2006.9.1128. [DOI] [PubMed] [Google Scholar]
- 24.Dalal S, Palla S, Hui D, et al. Association between a name change from palliative to supportive care and the timing of patient referrals at a comprehensive cancer center. The Oncologist. 2011;16:105–111. doi: 10.1634/theoncologist.2010-0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weissman DE, Meier DE, Spragens LH. Center to Advance Palliative Care palliative care consultation service metrics: Consensus recommendations. J Palliat Med. 2008;11:1294–1298. doi: 10.1089/jpm.2008.0178. [DOI] [PubMed] [Google Scholar]
- 26.Dev R, Del Fabbro E, Miles M, et al. Growth of an academic palliative medicine program: patient encounters and clinical burden. J Pain Symptom Manage. 2013;45:261–271. doi: 10.1016/j.jpainsymman.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cherny N, Catane R, Schrijvers D, et al. European Society for Medical Oncology (ESMO) Program for the integration of oncology and Palliative Care: A 5-year review of the Designated Centers’ incentive program. Ann Oncol. 2010;21:362–369. doi: 10.1093/annonc/mdp318. [DOI] [PubMed] [Google Scholar]
- 28.Rhondali W, Burt S, Wittenberg-Lyles E, et al. Medical oncologists’ perception of palliative care programs and the impact of name change to supportive care on communication with patients during the referral process. A qualitative study. Palliat Support Care. 2013;11:397–404. doi: 10.1017/S1478951512000685. [DOI] [PubMed] [Google Scholar]
- 29.Hui D, Kim YJ, Park JC, et al. Integration of oncology and palliative care: A systematic review. The Oncologist. 2015;20:77–83. doi: 10.1634/theoncologist.2014-0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hui D, Bansal S, Strasser F, et al. Indicators of integration of oncology and palliative care programs: An international consensus. Ann Oncol. 2015;26:1953–1959. doi: 10.1093/annonc/mdv269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith TJ, Coyne PJ, Cassel JB. Practical guidelines for developing new palliative care services: Resource management. Ann Oncol. 2012;23(Suppl 3):70–75. doi: 10.1093/annonc/mds092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McNiff KK, Neuss MN, Jacobson JO, et al. Measuring supportive care in medical oncology practice: Lessons learned from the quality oncology practice initiative. J Clin Oncol. 2008;26:3832–3837. doi: 10.1200/JCO.2008.16.8674. [DOI] [PubMed] [Google Scholar]
- 33.National Consensus Project for Quality Palliative Care Clinical Practice Guidelines for Quality Palliative Care. 2nd ed. Pittsburgh, PA: National Consensus Project for Quality Palliative Care, 2009. [Google Scholar]
- 34.Hui D, Kim SH, Roquemore J, et al. Impact of timing and setting of palliative care referral on quality of end-of-life care in cancer patients. Cancer. 2014;120:1743–1749. doi: 10.1002/cncr.28628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Hospice and Palliative Care Organization. NHPCO’s Facts and Figures: Hospice Care in America. Alexandria, VA: National Hospice and Palliative Care Organization; 2013.
- 36.Yennurajalingam S, Urbauer DL, Casper KL, et al. Impact of a palliative care consultation team on cancer-related symptoms in advanced cancer patients referred to an outpatient supportive care clinic. J Pain Symptom Manage. 2011;41:49–56. doi: 10.1016/j.jpainsymman.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 37.Kang JH, Kwon JH, Hui D, et al. Changes in symptom intensity among cancer patients receiving outpatient palliative care. J Pain Symptom Manage. 2013;46:652–660. doi: 10.1016/j.jpainsymman.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 38.Kamal A, Bull J, Wolf S, et al. Burnout among palliative care clinicians in the United States: Results of a national survey. J Clin Oncol. 2014;32(suppl):e20530. [Google Scholar]
- 39.Bakitas MA, Tosteson TD, Li Z, et al. Early versus delayed initiation of concurrent palliative oncology care: Patient outcomes in the ENABLE III randomized controlled trial. J Clin Oncol. 2015;33:1438–1445. doi: 10.1200/JCO.2014.58.6362. [DOI] [PMC free article] [PubMed] [Google Scholar]