Abstract
Background
Multiple clinical trials have shown that arthroscopy for knee osteoarthritis is not efficacious. It is unclear how these studies have affected orthopaedic practice in the USA.
Questions/purposes
We questioned whether, in the Veterans Health Administration system, rates of knee arthroscopy in patients with osteoarthritis have changed after publication of the initial clinical trial by Moseley et al. in 2002, and whether rates of arthroplasty within 2 years of arthroscopy have changed during the same period.
Methods
Patients 50 years and older with knee osteoarthritis who underwent arthroscopy between 1998 and 2010 were retrospectively identified and an annual arthroscopy rate was calculated from 1998 through 2002 and from 2006 through 2010. Patients who underwent knee arthroplasty within 2 years of arthroscopy during each period were identified, and a 2-year conversion to arthroplasty rate was calculated.
Results
Between 1998 and 2002, the annual arthroscopy rate decreased from 4% to 3%. Of these arthroscopies, 4% were converted to arthroplasty within 2 years. Between 2006 and 2010, the annual arthroscopy rate increased from 3% to 4%. Of these arthroscopies, 5% were converted to arthroplasty within 2 years.
Conclusions
Rates of arthroscopy in patients with knee osteoarthritis and conversion to arthroplasty within 2 years have not decreased with time. It may be that evidence alone is not sufficient to alter practice patterns or that arthroscopy rates for arthritis for patients in the Veterans Health Administration system were already so low that the results of the initial clinical trial had no substantial effect.
Level of Evidence
Level III, Retrospective cohort study.
Introduction
Randomized trials have shown that arthroscopic treatment of knee osteoarthritis is not efficacious. A landmark randomized controlled trial was published in the New England Journal of Medicine in 2002, which compared arthroscopic débridement for osteoarthritis with placebo surgery, and it found no difference in outcomes [18]. Subsequent studies have consistently shown the same findings [14, 15].
Despite high-quality evidence against arthroscopic treatment of degenerative knee arthritis, the effect of this evidence on clinical practice is less clear. Studies regarding the use of arthroscopic procedures for knee arthritis are inconsistent—some show decreasing use of arthroscopy with time [10, 12, 19], whereas another does not [1]. Some studies also show high rates of conversion from arthroscopy to arthroplasty within a short time, suggesting that the worst candidates for arthroscopy (ie, those with substantial enough degenerative changes to warrant knee arthroplasty) continue to be selected for the procedure [5, 8, 9, 22, 23]. Such findings raise concerns regarding the translation of evidence from major studies to real clinical practice.
With this study, we sought to determine if, in the Veterans Health Administration (VHA) system, (1) rates of knee arthroscopy in patients with osteoarthritis decreased with time after publication of the trial by Moseley et al. [18] and (2) rates of conversion from arthroscopy to arthroplasty within 2 years have decreased during this same period.
Patients and Methods
With the approval of our institutional review board, 467,977 patients 50 years and older who had a new diagnosis of knee osteoarthritis (based on International Classification of Diseases, 9th Revision [ICD-9] codes 715.16, 715.26, 715.36, 715.86, 715.96) between 1998 and 2010 were retrospectively identified through the VHA National Patient Care Database. The VHA National Patient Care Database includes full diagnostic and procedural data from all inpatient and outpatient encounters at all VHA facilities throughout the country [16]. Patients 50 years and older were selected to focus on those who were most likely to have osteoarthritis. Laterality was not available in this database.
Patients with knee osteoarthritis were divided into two groups: “prestudy”, which was composed of patients who were diagnosed before the study by Moseley et al. [18] (1998–2002) and “poststudy” was composed of patients who were diagnosed after their study was published (2006–2010). A 3-year lag period was intentionally placed between the two periods to allow time for potential adaptations in practice after publication of the study by Moseley et al. During the prestudy period (1998–2002), 190,659 patients with an average age of 67 years had a diagnosis of knee osteoarthritis (Table 1). There were 184,054 men (97%) and 6605 women (3%). During the poststudy period (2006–2010), 277,318 patients with an average age of 67 years had knee osteoarthritis. There were 262,415 men (95%) and 14,903 women (5%).
Table 1.
Patient demographics
| Demographics | Prestudy period (1998–2002) | Poststudy period (2006–2010) | ||||
|---|---|---|---|---|---|---|
| Patients with osteoarthritis | Patients with osteoarthritis treated with arthroscopy | Patients with osteoarthritis treated with arthroscopy followed by arthroplasty | Patients with osteoarthritis | Patients with osteoarthritis treated with arthroscopy | Patients with osteoarthritis treated with arthroscopy followed by arthroplasty | |
| Total number of patients | 190,659 | 6972 | 266 | 277,318 | 10,645 | 496 |
| Gender | ||||||
| Male (%) | 184,054 (97%) |
6645 (95%) |
255 (96%) |
262,415 (95%) |
9924 (93%) |
466 (94%) |
| Female (%) | 6605 (3%) |
327 (5%) |
11 (4%) |
14,903 (5%) |
721 (7%) |
30 (6%) |
| Age | ||||||
| Average age (years) | 67.1 | 59.3 | 62.0 | 67.0 | 59.3 | 60.3 |
| Patients 50–55 years (%) | 35,850 (19%) |
3036 (44%) |
75 (28%) |
38,054 (14%) |
3218 (30%) |
118 (24%) |
| Patients 55–65 years (%) | 44,355 (23%) |
2429 (35%) |
100 (38%) |
109,103 (39%) |
5963 (56%) |
294 (59%) |
| Patients 65 years and older (%) | 110,454 (58%) |
1507 (21%) |
91 (34%) |
130,161 (47%) |
1464 (14%) |
84 (117%) |
Of these patients, those who underwent knee arthroscopy were identified using Current Procedural Terminology (CPT) codes 29877 (chondroplasty), 29880 (medial AND lateral meniscectomy), or 29881 (medial OR lateral meniscectomy). CPT code 29877 was selected because arthroscopic débridement was the main procedure evaluated by Moseley et al. [18]. Although studies evaluating meniscectomy in osteoarthritis were published more recently, we elected to include meniscectomy codes in the current study to concurrently evaluate the use of this procedure, which is commonly used in osteoarthritis and may be coded in lieu of a débridement code [12, 21].
The arthroscopy rate was defined as the number of patients with the diagnosis of knee osteoarthritis within a given year who underwent arthroscopy within 1 year of the diagnosis divided by the total number of patients with the diagnosis of knee osteoarthritis within that given year. The arthroscopy rate was calculated for each of the 5 years from 1998 through 2002 (prestudy period) and from 2006 through 2010 (poststudy period).
Patients with the diagnosis of knee osteoarthritis who underwent knee arthroscopy during either of the two study periods were further reviewed. Those who underwent unicompartmental or TKA within 2 years of knee arthroscopy in each period were identified by ICD-9 code 81.54. The 2-year conversion to arthroplasty rate was defined as the number of patients in a given year with the diagnosis of knee osteoarthritis who underwent arthroscopy and subsequently underwent a knee arthroplasty within 2 years of arthroscopy divided by the total number of patients with the diagnosis of knee osteoarthritis who underwent arthroscopy within that given year. The 2-year conversion to arthroplasty rate was calculated for each of the 5 years from 1998 through 2002 and from 2006 through 2010 with the same interposing 3-year lag period as described previously.
Statistical Analysis
An interrupted time-series analysis was performed to assess changes in use of knee arthroscopy and 2-year conversion to arthroplasty between the start and end of each period and between the two periods of study. The statistical significance of the change in each of these annual rates in the prestudy period, between the pre- and poststudy periods, and in the poststudy period was determined. SAS® software (SAS® Inc, Cary, NC, USA) was used to perform all analyses.
Results
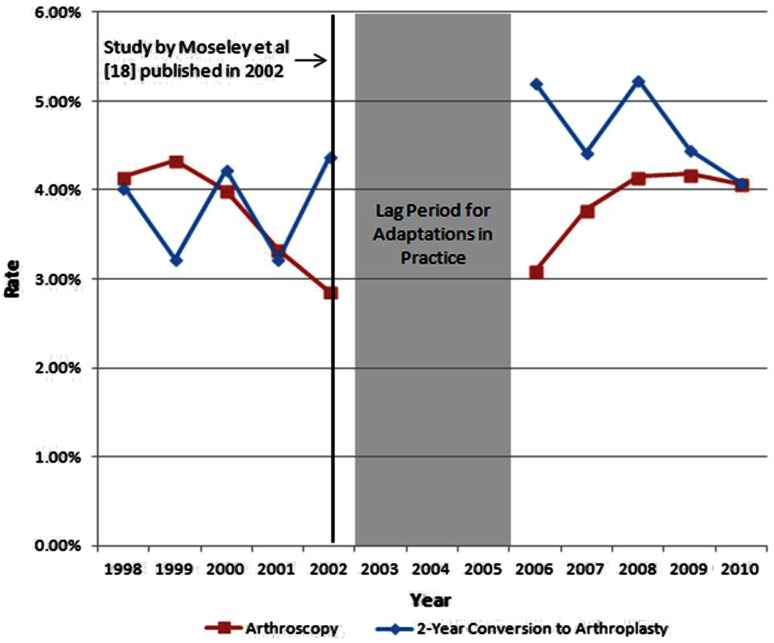
There was no change in rates of knee arthroscopy with time, even after publication of the article by Moseley et al. [18]. During the prestudy period, 6972 patients (4%) underwent knee arthroscopy within 1 year of diagnosis. The mean age of these patients was 59 years (SD, 7.8 years) (Table 1). There were 6645 men (95%) and 327 women (5%). During this time, the annual rate of knee arthroscopy for patients with osteoarthritis decreased from 4% in 1998 to 3% in 2002 (p = 0.001) (Fig. 1). During the poststudy period, 10,645 patients (4%) underwent arthroscopy within 1 year of diagnosis. The mean age of patients undergoing arthroscopy was 59 years (SD, 6.5 years) (Table 1). There were 9924 men (93%) and 721 women (7%). The arthroscopy rate at the beginning of the second period (3.09% in 2006) was higher than the rate at the end of the first period (2.86% in 2002; p = 0.013). In addition, the yearly arthroscopy rate increased during the second period, from 3.09% in 2006 to 4.07% in 2010 (p < 0.001) (Fig. 1).
Fig. 1.
This graph shows the trend in the use of arthroscopy for knee osteoarthritis and 2-year conversion rate to arthroplasty in the Veterans Administration hospital system from 1998 to 2010.
There was no change in the conversion rates between the pre- and poststudy periods (p = 0.15). The 2-year conversion to arthroplasty rate during the prestudy period was 4% (266 patients). The mean age of these patients was 62 years (SD, 8.5 years) (Table 1). Two hundred fifty-five (96%) were men and 11 (4%) were women. This rate was stable during this period, varying between 3% and 4% each year (p = 0.98) (Fig. 1). The 2-year conversion rate from arthroscopy to arthroplasty in the poststudy period was 5% (496 patients). The mean age of these patients was 60 years (SD, 6.7 years) (Table 1). There were 466 men (94%) and 30 women (6%). The annual conversion rate was between 4% and 5%, which was stable (p = 0.19) (Fig. 1).
Discussion
There is Level I evidence against arthroscopy in the setting of knee osteoarthritis [14, 15, 18], yet the effect of this evidence on clinical practice has been unclear. It is important to evaluate the effect of high-quality studies in orthopaedics, to confirm the wide adoption of evidence-based practices, and to justify the commitment of the resources necessary to conduct such studies. Our study shows that the rates of arthroscopy for knee osteoarthritis have not decreased with time in the VHA population after the initial study by Moseley et al. [18]. Additionally, the 2-year conversion to arthroplasty rate did not change significantly throughout the period of study.
This study has limitations, which should be noted. First, we used an administrative database that relies on coding data, which may be inconsistent with physician records [11, 17]. It does not provide laterality of the diagnosis or surgical procedures, so it is possible that the procedures were performed on the knee contralateral to the arthritic one. However, even if that is true, our reported arthroscopy rates would include procedures on nonarthritic knees and these rates therefore would be over- rather than underestimated. Thus, it is unlikely to change our conclusions. This administrative database also does not provide any clinical context for the procedures in question. Although there is sufficient evidence against arthroscopic débridement for osteoarthritis [15, 18], indications such as a loose body or a bucket handle meniscal tear blocking full ROM may still be considered appropriate [13, 24]. Presumably, by restricting arthroscopy codes, we have eliminated many of those cases. However, because clinical details were not available, it is possible that some cases in this study were performed for such reasons. Another limitation of this database is that it does not indicate the severity of arthritis. It is possible that many patients had only mild degenerative changes. This could explain the continued use of arthroscopy and the overall low conversion rate to arthroplasty. Finally, we have no information regarding outcomes in this patient population, and it is possible that patients benefited from these surgeries.
Despite the limitations of using an administrative database, it allows an opportunity to evaluate the use of arthroscopy in patients with osteoarthritis on a wide scale. Our results differ from those in previously published studies on the US population [10, 12, 19]; however, each of the studies has its own limitations, making comparisons difficult. Potts et al. [19] reported a 40% decline in cases of knee arthroscopy for osteoarthritis among orthopaedic surgeons in their American Board of Orthopaedic Surgery examination case-collection period between 2003 and 2009. However, their data are based on the practices of new surgeons at a time when their cases are subject to substantial scrutiny; therefore, it behooves these surgeons to follow evidence-based practices during this time. It is possible that outside the board collection period, their practices would be different. Another study reviewed the Florida State Ambulatory Surgery Database—which includes all outpatient surgeries covered by any payer in Florida—for trends in arthroscopic débridement and lavage and found a 47% decrease between 2001 and 2010 [12]. Howard et al. [12] noted significant decreases in this procedure after publication of the studies by Moseley et al. [18] and Kirkley et al. [15], but they also noted significant decreases after the Centers for Medicare & Medicaid Services discontinued coverage for this procedure in 2003 [3]. However, the study by Howard et al. [12] is limited by its exclusion of meniscectomy procedure codes from the analysis, which they acknowledge could be used to bill for débridement of osteoarthritis. Another study using the same database included all arthroscopic knee procedures for the primary diagnosis of osteoarthritis and noted a 49% decrease between 2000 and 2008; however, only cases from one state were evaluated [10]. It is difficult to distinguish the effect of clinical evidence from the effect of other outside forces such as board certification examinations, changes in insurance coverage, and geographic practice variability, from these studies. We attempted to mitigate these potential confounders by using data from a single national healthcare system that is shielded from the influence of outside payers and financial incentives to perform more surgeries, as VHA surgeons are salaried employees; however, other differences in methodology further preclude reasonable comparisons between our study and the published studies. We evaluated trends in the number of arthroscopies in patients with knee osteoarthritis relative to the number of patients with the diagnosis. Other studies use different denominators, including total adult population (which includes patients without knee osteoarthritis) [10, 12] and a finite number of surgical cases (which includes nonarthroscopic and nonknee cases) [19]. Although these other representations allow for historical comparisons in the same study, our methodology most directly answers the question of how many patients with knee osteoarthritis are being treated arthroscopically. Nevertheless, the arthroscopy rates in our study were relatively low—approximately 3% to 4% of patients with a diagnosis of knee osteoarthritis underwent knee arthroscopy in our study, before and after the study by Moseley et al. [18]. It is possible that this rate is already sufficiently low, leaving minimal room for further reduction.
Another important finding in our study is the relatively low conversion rate of knee arthroscopy to arthroplasty within 2 years. Our overall 2-year conversion to arthroplasty rate of less than 4% was much less than rates reported in other studies. Harris et al. [8] reported a 2-year conversion rate greater than 20% in patients 65 years and older in Australia; however, the minimum age of patients in their study was older than that in our study and advanced age has been shown to be a risk factor for early conversion to arthroplasty [9, 25]. Another study of patients in Ontario, Canada, showed a 1-year conversion rate of 9% and 3-year conversion rate of 18% among patients 50 and older [25]. Multiple factors could contribute to the differences between our study and these previously published reports, including geographic variability in practices, differences in patient population, and variability in the reporting of conversion rates, ranging between 1 and 3 years after arthroscopy. It also is possible that, relative to other studies, a preponderance of the patients in our cohort had mild degenerative disease such that they were not candidates for arthroplasty. Another possibility is that patients in our cohort with failed arthroscopies did not or were unable to undergo arthroplasty within 2 years owing to patient preference and/or systemic constraints in the VHA system. Finally, similar to our low arthroscopy rate, our 2-year conversion rate might be so low that there no room for additional improvement.
We initially expected the rates of arthroscopy and 2-year conversion to arthroplasty to decrease with time. However, physician behavior has been shown to be difficult to change, even with high-quality evidence [4, 7]. For instance, beta blockade has been shown to decrease mortality after acute myocardial infarction, yet the adoption of this practice has been slow [2, 6, 26]. Active interventions, such as educational outreach visits and reminders, rather than passive methods like publications, typically are required to foster evidence-based changes in practice [7]. Clinical practice guidelines, such as the American Academy of Orthopaedic Surgeons guideline entitled “Treatment of Osteoarthritis of the Knee (Non-Arthroplasty),” which incorporated findings from the study by Moseley et al., may help to facilitate changes in practice as well [20]. However, even with such interventions, targets for behavioral change are unclear. Should scientific evidence—even high-quality evidence—be expected to be applied universally to clinical practice, or are there exceptions to every rule? Despite that the rates did not decrease, they were very low to start with, even before the study by Moseley et al. Expectations that the rates would approach 0% are likely unrealistic. Most states of disease, including osteoarthritis, are a spectrum; yet the adoption of evidence-based recommendations typically is viewed from a black-and-white perspective. It is beyond the scope of this study to set standards for rates of arthroscopy in patients with osteoarthritis. Perhaps future studies can help to define appropriate goals for the adoption of evidence-based practices, including the use of arthroscopy in patients with knee osteoarthritis.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at VA Palo Health Care System, Palo Alto, CA, USA.
References
- 1.Bohensky MA, Sundararajan V, Andrianopoulos N, de Steiger RN, Bucknill A, Kondogiannis CM, McColl G, Brand CA. Trends in elective knee arthroscopies in a population-based cohort, 2000–2009. Med J Aust. 2012;197:399–403. doi: 10.5694/mja11.11645. [DOI] [PubMed] [Google Scholar]
- 2.Brand DA, Newcomer LN, Freiburger A, Tian H. Cardiologists’ practices compared with practice guidelines: use of beta-blockade after acute myocardial infarction. J Am Coll Cardiol. 1995;26:1432–1436. doi: 10.1016/0735-1097(95)00362-2. [DOI] [PubMed] [Google Scholar]
- 3.CMS.gov. Centers for Medicare & Medicaid Services. Decision Memo for Arthroscopy for the Osteoarthritic Knee. Available at: http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=7&NcaName=Arthroscopy+for+the+Osteoarthritic+Knee&NCDId=285&ncdver=1&IsPopup=y&bc=AAAAAAAACAAAAA%3D%3D&. Accessed April 13, 2014.
- 4.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–705. doi: 10.1001/jama.1995.03530090032018. [DOI] [PubMed] [Google Scholar]
- 5.Dhawan A, Mather RC, 3rd, Karas V, Ellman MB, Young BB, Bach BR, Jr, Cole BJ. An epidemiologic analysis of clinical practice guidelines for non-arthroplasty treatment of osteoarthritis of the knee. Arthroscopy. 2014;30:65–71. doi: 10.1016/j.arthro.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Everly MJ, Heaton PC, Cluxton RJ., Jr Beta-blocker underuse in secondary prevention of myocardial infarction. Ann Pharmacother. 2004;38:286–293. doi: 10.1345/aph.1C472. [DOI] [PubMed] [Google Scholar]
- 7.Grimshaw JM, Shirran L, Thomas R, Mowatt G, Fraser C, Bero L, Grilli R, Harvey E, Oxman A, O’Brien MA. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39(8 suppl 2):112–145. [PubMed] [Google Scholar]
- 8.Harris IA, Madan NS, Naylor JM, Chong S, Mittal R, Jalaludin BB. Trends in knee arthroscopy and subsequent arthroplasty in an Australian population: a retrospective cohort study. BMC Musculoskelet Disord. 2013;14:143. doi: 10.1186/1471-2474-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hawker G, Guan J, Judge A, Dieppe P. Knee arthroscopy in England and Ontario: patterns of use, changes over time, and relationship to total knee replacement. J Bone Joint Surg Am. 2008;90:2337–2345. doi: 10.2106/JBJS.G.01671. [DOI] [PubMed] [Google Scholar]
- 10.Holmes R, Moschetti W, Martin B, Tomek I, Finlayson S. Effect of evidence and changes in reimbursement on the rate of arthroscopy for osteoarthritis. Am J Sports Med. 2013;41:1039–1043. doi: 10.1177/0363546513479771. [DOI] [PubMed] [Google Scholar]
- 11.Holt G, Feurer ID, Schwartz HS. An analysis of concordance among hospital databases and physician records. Ann Surg Oncol. 1998;5:553–556. doi: 10.1007/BF02303650. [DOI] [PubMed] [Google Scholar]
- 12.Howard D, Brophy R, Howell S. Evidence of no benefit from knee surgery for osteoarthritis led to coverage changes and is linked to decline in procedures. Health Aff (Millwood). 2012;31:2242–2249. doi: 10.1377/hlthaff.2012.0644. [DOI] [PubMed] [Google Scholar]
- 13.Howell SM. The role of arthroscopy in treating osteoarthritis of the knee in the older patient. Orthopedics. 2010;33:652. doi: 10.3928/01477447-20100722-34. [DOI] [PubMed] [Google Scholar]
- 14.Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL, Donnell-Fink LA, Guermazi A, Haas AK, Jones MH, Levy BA, Mandl LA, Martin SD, Marx RG, Miniaci A, Matava MJ, Palmisano J, Reinke EK, Richardson BE, Rome BN, Safran-Norton CE, Skoniecki DJ, Solomon DH, Smith MV, Spindler KP, Stuart MJ, Wright J, Wright RW, Losina E. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368:1675–1684. doi: 10.1056/NEJMoa1301408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, Feagan BG, Donner A, Griffin SH, D’Ascanio LM, Pope JE, Fowler PJ. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097–1107. doi: 10.1056/NEJMoa0708333. [DOI] [PubMed] [Google Scholar]
- 16.Maynard C, Chapko MK. Data resources in the Department of Veteran Affairs. Diabetes Care. 2004;27(suppl 2):B22–B26. doi: 10.2337/diacare.27.suppl_2.B22. [DOI] [PubMed] [Google Scholar]
- 17.Mont MA, Mears SC, Jones LC, Rajadhyaksha AD, Krackow AM, Bawa M, Hungerford DS. Is coding of diagnoses, comorbidities, and complications in total knee arthroplasty accurate? J Arthroplasty. 2002;17:767–772. doi: 10.1054/arth.2002.33549. [DOI] [PubMed] [Google Scholar]
- 18.Moseley JB, O’Malley K, Petersen NJ, Menke TJ, Brody BA, Kuykendall DH, Hollingsworth JC, Ashton CM, Wray NP. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81–88. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 19.Potts A, Harrast JJ, Harner CD, Miniaci A, Jones MH. Practice patterns for arthroscopy of osteoarthritis of the knee in the United States. Am J Sports Med. 2012;40:1247–1251. doi: 10.1177/0363546512443946. [DOI] [PubMed] [Google Scholar]
- 20.Richmond J, Hunter D, Irrgang J, Jones MH, Levy B, Snyder-Mackler L, Watters WC, 3rd, Haralson RH, 3rd, Turkelson CM, Wies JL, Boyer KM, Anderson S, St Andre J, Sluka P, McGowan R, American Academy of Orthopaedic Surgeons Treatment of osteoarthritis of the knee (nonarthroplasty) J Am Acad Orthop Surg. 2009;17:591–600. doi: 10.5435/00124635-200909000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siparsky P, Ryzewicz M, Peterson B, Bartz R. Arthroscopic treatment of osteoarthritis of the knee: are there any evidence-based indications? Clin Orthop Relat Res. 2007;455:107–112. doi: 10.1097/BLO.0b013e31802fc18c. [DOI] [PubMed] [Google Scholar]
- 22.Skedros JG, Knight AN, Thomas SC, Paluso AM, Bertin KC. Dilemma of high rate of conversion from knee arthroscopy to total knee arthroplasty. Am J Orthop (Belle Mead NJ). 2014;43:E153–E158. [PubMed] [Google Scholar]
- 23.Steadman JR, Briggs KK, Matheny LM, Ellis HB. Ten-year survivorship after knee arthroscopy in patients with Kellgren-Lawrence grade 3 and 4 osteoarthritis of the knee. Arthroscopy. 2013;29:220–225. doi: 10.1016/j.arthro.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 24.Stuart MJ, Lubowitz JH. What, if any, are the indications for arthroscopic débridement of the osteoarthritic knee? Arthroscopy. 2006;22:238–239. doi: 10.1016/j.arthro.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 25.Wai EK, Kreder HJ, Williams JI. Arthroscopic débridement of the knee for osteoarthritis in patients fifty years of age or older: utilization and outcomes in the Province of Ontario. J Bone Joint Surg Am. 2002;84:17–22. doi: 10.2106/00004623-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Weichel AS. Why aren’t we using beta blockers after acute MI? Am Fam Physician. 2000;62:1771–1772. [PubMed] [Google Scholar]