Abstract
Background
Modular revision femoral components allow the surgeon to make more precise intraoperative adjustments in anteversion and sizing, which may afford lower dislocation rates and improved osseointegration, but may not offer distinct advantages when compared with less expensive monoblock revision stems.
Questions/purposes
We compared modular and monoblock femoral components for revision of Paprosky Type I to IIIA femoral defects to determine (1) survivorship of the stems; and (2) complications denoted as intraoperative fracture, dislocation, or failure of osseointegration.
Methods
Between 2004 and 2010, participating surgeons at three centers revised 416 total hip arthroplasties (THAs) with Paprosky Type I to IIIA femoral defects. Of those with minimum 2-year followup (343 THAs, mean followup 51 ± 13 months), 150 (44%) were treated with modular stems and 193 (56%) were treated with monoblock, cylindrical, fully porous-coated stems. During this time, modular stems were generally chosen when there was remodeling of the proximal femur into retroversion and/or larger canal diameters (usually > 18 mm). A total of 27 patients died (6%) with stems intact before 2 years, 46 THAs (13%) were lost to followup before 2 years for reasons other than death, and there was no differential loss to followup between the study groups. The modular stems included 101 with a cylindrical distal geometry (67%) and 49 with a tapered geometry (33%). Mean age (64 versus 68 years), percentage of women (53% versus 47%), and body mass index (31 versus 30 kg/m2) were not different between the two cohorts, whereas there was trend toward a slightly greater case complexity in the modular group (55% versus 65% Type 3a femoral defects, p = 0.06). Kaplan-Meier survivorship was calculated for the endpoint of aseptic revision. Proportions of complications in each cohort (dislocation, intraoperative fracture, and failure of osseointegration) were compared.
Results
Femoral component rerevision for any reason (including infection) was greater (OR, 2.01; 95% CI, 1.63–2.57; p = 0.03) in the monoblock group (27 of 193 [14%]) compared with the modular cohort (10 of 150 [7%]). Femoral component survival free from aseptic rerevision was greater in the modular group with 91% survival (95% CI, 89%–95%) at 9 years compared with 86% survival (95% CI, 83%–88%) for the monoblock group in the same timeframe. There was no difference in the proportion of mechanically relevant aseptic complications (30 of 193 [16%] in the monoblock group versus 34 of 150 [23%] in the modular group, p = 0.10; OR, 1.47; 95% CI, 0.86–2.53). There were more intraoperative fractures in the modular group (17 of 150 [11%] versus nine of 193 [5%]; OR, 2.2; 95% CI, 1.68–2.73; p = 0.02). There were no differences in the proportions of dislocation (13 of 193 [7%] monoblock versus 14 of 150 [9%] modular; OR, 0.96; 95% CI, 0.67–1.16; p = 0.48) or failure of osseointegration (eight of 193 [4%] monoblock versus three of 150 [2%] modular; OR, 1.92; 95% CI, 0.88–2.84; p = 0.19) between the two groups with the number of hips available for study.
Conclusions
Although rerevisions were less common in patients treated with modular stems, aseptic complications such as intraoperative fractures were more common in that group, and the sample was too small to evaluate corrosion-related or fatigue concerns associated with modularity. We cannot therefore conclude from this that one design is superior to the other. Larger studies and pooled analyses will need to be performed to answer this question, but we believe modularity should be avoided in more straightforward cases if possible.
Level of Evidence
Level III, therapeutic study.
Introduction
It has been estimated that the number of revision THAs performed annually in the United States will reach approximately 100,000 by 2030 [10, 11]. As of 2006, hip and knee arthroplasty accounted for 8.5% of the expenditures for the Center for Medicare & Medicaid Services, double the next largest category (cardiac surgery). Given the current climate for healthcare delivery, providers have a responsibility to define which hip implants carry the most value. Both modular and nonmodular cementless stems that engage the diaphysis are in use for femoral revision, but it is unclear whether modular stems provide any distinct advantage that justifies their cost when used in simpler femoral revisions.
Modular implants in femoral revision surgery have proven effective through the first decade of in vivo service [2, 5, 7, 8, 15, 16]. These modular implants were popularized on the concept of improved “fit and fill.” It was espoused that modularity would allow matching of both the intraosseous as well as the extraosseous portions of the femoral reconstruction. This is important in the revision setting where remodeling, often into varus and retroversion, creates metaphyseal-diaphyseal mismatches. The expectation was that improved “fit and fill” would allow for a higher likelihood of osseointegration, a lower risk of intraoperative fracture, and fewer dislocations (through optimal sizing, offset, and anteversion) when compared with the previous generation of monoblock revision femoral implants. However, there are disadvantages to modularity including risks of mechanical failure and corrosion [3, 7, 8]. These implants are also generally more expensive than nonmodular components and, perhaps most importantly, may simply not be necessary for more straightforward revisions, which we consider as Paprosky Types I to IIIA femoral defects [19]. We specifically selected these femoral defects because both monoblock and modular stems have been successfully used for these less severe femoral defects, but it is not known whether either possesses distinct advantages. In higher grade femoral defects (3b or 4) when less than 4 cm of isthmus is available for distal fixation, a higher rate of failed osseointegration has been demonstrated with monoblock cylindrical femoral components, and other methods of reconstruction are recommended [18].
We therefore compared modular and monoblock femoral components for revision of Paprosky Types I to IIIA femoral defects to determine (1) survivorship of the stems; and (2) complications denoted as intraoperative fracture, dislocation, or failure of osseointegration.
Patients and Methods
Between 2004 and 2010, participating surgeons at three centers revised 416 THAs with Paprosky Types I to IIIA femoral defects. Of those with minimum 2-year followup (343 THAs, mean followup 51 ± 13 months), 150 (44%) were treated with modular stems and 193 (56%) were treated with monoblock, cylindrical, fully porous-coated stems and compared in this retrospective study. During this time, modular stems were generally chosen when there was remodeling of the proximal femur into retroversion and/or larger canal diameters (usually > 18 mm). However, during this time, there was some selection bias based on surgeon preference, because most of the monoblock stems (192 of 193 [99%]) came from a single institution (Rush). The proportions of modular stems at each site were 70 of 150 (47%) at Massachusetts General Hospital, 38 of 150 (25%) at Rush, and 42 of 150 (28%) at Stanford (p = 0.01). All operations were performed through a posterior approach by three fellowship-trained surgeons from each institution.
In the monoblock cohort, 25 of the 193 hips were lost to followup (13%) and 21 died before 2 years; of those who died, none were known to have been revised before death. In the modular group, 21 of 150 (14%) were lost with less than 2 years of followup, and six others died (likewise, all without revision). The remaining 193 monoblock and 150 modular THAs were analyzed at a minimum of 2 years followup (mean, 51 ± 13 months; range, 2–11.1 years). Mean followup was 47 ± 12 months in the monoblock group and 56 ± 15 months in the modular group (p < 0.001). Each center’s institutional review board approved the study.
Reasons for revision varied (Table 1). One hundred ninety-three patients received femoral components with a monoblock design. One hundred fifty patients received femoral components that were modular, ie, contained separate proximal body and distal stem parts. The distal geometry was cylindrical for all monoblock components. The monoblock cohort included 172 VerSys Beaded Full-coats (Zimmer, Warsaw, IN, USA), 13 Echelons (Smith & Nephew, Memphis TN, USA), three Epoch IIs (Zimmer), two Bantams (DePuy/Johnson and Johnson, Warsaw, IN, USA), and one Solution (DePuy). For the modular components, the distal stem geometries were cylindrical in 67% (101 of 150) and fluted, tapered in 33% (49 of 150) of the cases. The modular cohort included 132 ZMRs (Zimmer), 13 Restorations (Stryker, Mahwah, NJ, USA), and five MDFs (Smith & Nephew). In the monoblock cohort, there were 37 of 193 (19%) hips with a femoral head size of 32 mm or less. In the modular cohort, there were 62 of 150 (41%) with head size 32 mm or less (p = 0.01) (Table 2).
Table 1.
Reasons for revision
| Indication | Monoblock (N = 193) | Modular (N = 150) | p value |
|---|---|---|---|
| Aseptic loosening | 93 (47%) | 75 (50%) | NS |
| Infection | 67 (34%) | 51 (34%) | NS |
| Periprosthetic fracture | 14 (7%) | 15 (10%) | 0.09 |
| Femoral component fracture | 11 (6%) | 4 (3%) | 0.04 |
| Instability | 11 (6%) | 5 (3%) | 0.04 |
NS = nonsignificant.
Table 2.
Head size
| Head size (mm) | Monoblock (N = 193) | Modular (N = 150) | p value |
|---|---|---|---|
| < 36 | 39 (20%) | 76 (50%) | 0.001 |
| ≥ 36 | 154 (80%) | 74 (50%) | 0.004 |
When comparing the two cohorts, the mean age of the patients was 64 ± 5 years in the monoblock group and 68 ± 7 years in the modular group (p = 0.15). There were 91 of 193 (47%) men in the monoblock group and 80 of 150 (53%) men in the modular group (p = 0.26). Mean body mass indices were 31± 6 kg/m2 in the monoblock cohort and 30 ± 5 kg/m2 in the modular cohort (p > 0.05).
Each patient was reviewed for the presence of other aseptic complications, including periprosthetic fracture, dislocation events, and repeat revision surgery. Radiographs to determine both Paprosky defect and femoral component osseointegration [3, 4] were reviewed by two or three reviewers at each site. Discrepancies between reviewers were classified by the majority or the attending surgeon (JIH, SBG, CJDV, HB, or SMS). We did not perform an analysis for intraobserver or interobserver differences. There was a trend toward increasing complexity of the femoral revision (65% versus 55% Type 3a; p = 0.06) in the modular cohort compared with the modular group (Table 3).
Table 3.
Femoral defect classification
| Paprosky type | Monoblock (N = 193) | Modular (N = 150) | p value |
|---|---|---|---|
| I | 2 (1%) | 3 (2%) | |
| II | 84 (44%) | 49 (33%) | 0.02 |
| IIIA | 107 (55%) | 98 (65%) | 0.06 |
Data were compared with the Fisher’s exact test (failures of osseointegration) and Pearson chi-square tests. Kaplan-Meier survivorship analysis was performed. The total number of aseptic complications was compared using logistic regression. Power analysis, assuming an α = 0.05, was based on the aggregate rates of dislocation, failure of osseointegration, and intraoperative fracture and yielded β = 0.86. It was determined that a sample size of 136 cases in each group would be required to detect a clinically significant difference (20% reduction) in the aggregate rate of aseptic complications (intraoperative fracture, dislocation, and failure of osseointegration) between the two groups.
Results
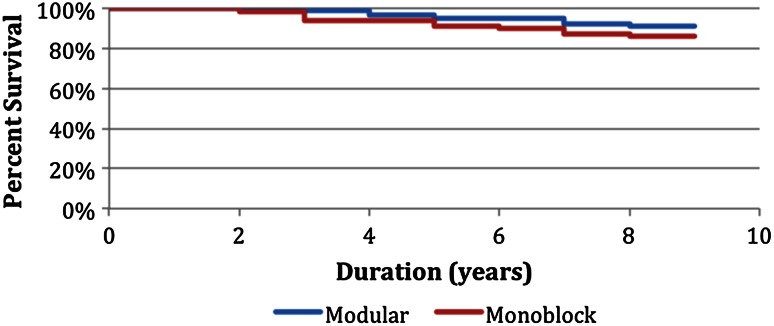
Femoral component survival free from aseptic rerevision was greater in the modular group with 91% survival (95% confidence interval [CI], 89%–95%) at 9 years compared with 86% survival (95% CI, 83%–88%) for the monoblock group in the same timeframe (Fig. 1). There were more repeat aseptic femoral revisions in the monoblock cohort with 9% (17 of 193) versus 5% (eight of 150) (odds ratio [OR], 1.80; 95% CI, 1.39–2.57; p = 0.03; Table 4). There were more total repeat femoral revisions (septic and aseptic) in the monoblock cohort (27 of 193 [14%] versus 10 of 150 [7%]; OR, 2.01; 95% CI, 1.63–2.57; p = 0.03; Table 4). Additional aseptic revisions included two femoral implant fractures in the modular group (at the junction of the stem and body), two monoblock components for periprosthetic fracture (neither femoral implant was loose), one monoblock implant for mechanically assisted crevice corrosion at the trunnion, and one additional monoblock implant to facilitate acetabular exposure at the time of repeat revision.
Fig. 1.
This figure shows the Kaplan-Meier aseptic femoral survivorship estimates.
Table 4.
Repeat femoral revision
| Reason for rerevision | Monoblock (N = 193) | Modular (N = 150) | p value |
|---|---|---|---|
| Failure of osseointegration | 8 (4%) | 3 (2%) | 0.19 |
| Recurrent instability | 5 (3%) | 3 (2%) | NS |
| Stem fracture | 0 | 2 (2%) | NS |
| Periprosthetic fracture | 2 (1%) | 0 | NS |
| Corrosion | 1 (1%) | 0 | NS |
| Facilitate socket exposure | 1 (1%) | 0 | NS |
| Any aseptic failure mode | 17 (9%) | 8 (5%) | 0.03 |
| Septic failure mode | 10 (5%) | 2 (2%) | 0.047 |
| Any reason | 27 (14%) | 10 (7%) | 0.03 |
NS = nonsignificant.
There was not a difference in the proportion of aseptic complications in the monoblock group (30 of 193 [16%]) compared with the modular group (34 of 150 [23%]; OR, 1.47; 95% CI, 0.86–2.53; p = 0.10; Table 5). This included more intraoperative fractures in the modular cohort (17 of 150 [11%] versus nine of 193 [5%]; OR, 2.2; 95% CI, 1.68–2.73; p = 0.02). A single trochanteric fracture occurred in the monoblock group and five trochanteric fractures occurred in the modular group. Femoral shaft fractures occurred in eight of the monoblock patients and 12 of the modular patients (p = 0.13). Of the 12 intraoperative shaft fractures in the modular cohort, there was not a difference in the proportion of fractures seen in tapered compared with cylindrical distal geometries (seven versus five, p = 0.21). There were nine postoperative periprosthetic fractures in the monoblock group (5%, six Paprosky IIIA and two Paprosky II) compared with seven in the modular group (5%, five Paprosky IIIA and two Paprosky II), resulting in revision of two of the monoblock femoral components. Neither one of these femoral implants was loose. There was not a difference in the proportion of patients that sustained a dislocation (13 of 193 [7%] in the monoblock cohort versus 14 of 150 [9%]) in the modular cohort (OR, 0.96; 95% CI, 0.67–1.16; p = 0.48). Five patients in the monoblock cohort underwent rerevision for recurrent instability. Three patients in the modular cohort were rerevised for recurrent instability. All revisions for instability entailed combinations of modular head exchange, modular liner exchange, and/or entire socket exchange. There was not a difference in the proportion of stems that osseointegrated (eight of 193 [4%] monoblock stems versus three of 150 [2%] modular stems; OR, 1.92; 95% CI, 0.88–2.84; p = 0.19).
Table 5.
Aseptic complications
| Complication | Monoblock (N = 193) | Modular (N = 150) | p value | Odds ratio (95% CI) |
|---|---|---|---|---|
| Intraoperative fracture | 9 (5%) | 17 (11%) | 0.02 | 2.2 (1.68–2.73) |
| Dislocation | 13 (7%) | 14 (9%) | NS | 0.96 (0.67–1.16) |
| Failure of osseointegration | 8 (4%) | 3 (2%) | NS | 1.92 (0.88–2.84) |
| Total | 30 (16%) | 34 (23%) | NS | 1.47 (0.86–2.53) |
CI = confidence interval; NS = nonsignificant.
Discussion
Modular femoral components offer many potential theoretical advantages over monoblock components in femoral revision surgery. It is plausible that the opportunity to independently optimize hoop stresses proximally and distally with modular components would yield fewer intraoperative fractures and higher rates of osseointegration compared with monoblock components. One might also expect that a surgeon’s ability to better adjust femoral component anteversion in modular components would yield lower dislocation rates compared with monoblock components. We sought to determine whether there were differences in survivorship or common mechanically relevant complications between modular and nonmodular femoral components when used for Paprosky Type I to IIIA femoral revisions.
This study has several limitations. First, the lack of randomization introduces potential selection bias. Almost all the monoblock stems were placed by two surgeons at one of the institutions. Although all surgeons who participated in this study are skilled using both monoblock and modular implants, it is possible that surgeon experience could have affected our results in either direction. A randomized controlled trial would have been better to compare these two types of revision femoral components. However, randomized trials involving large numbers of patients requiring revision surgery are complex and costly undertakings. Second, a total of 19% of patients were lost to followup (6% died and 13% lost). It is unclear how this influenced our results, but the percentage of patients lost in each group was similar. Third, because this was a multicenter study, certain important variables such as femoral head size and grade of femoral defect were different among the groups and this may have affected some of our measured outcomes. Multiple surgeons performed the procedures with varying levels of experience, although all were experienced fellowship-trained arthroplasty surgeons. Although general demographics were similar, we did not account for comorbidities, and infection rates may also vary between institutions, which could influence the frequency of septic revisions. Fourth, although our sample size was large compared with many of the series reported in the literature of revision femoral components, we still may have been underpowered to detect smaller differences in some of the outcomes reported such as the rate of dislocation or complications associated with modularity (eg, stem breakage and adverse local tissue reaction). However, the study was powered appropriately for the primary outcome, the overall rate of mechanically relevant complications (intraoperative fracture, dislocation, and failure of osseointegration). Fifth, numerous variables were not considered that may have influenced our results. These include acetabular component positioning (dislocation), bone quality (fracture), and various patient factors that increase the risk, complexity, or time spent in the procedure. However, it is difficult to control or account for every variable in revision surgery and our intent was to compare these stem designs for survivorship and certain common complications. Lastly, nearly all the implants used in this study were made by a single manufacturer. It is unclear if the outcomes would be different if stems from a different manufacturer were compared [6].
The data yielded higher rates of reoperation in the monoblock cohort for all reasons as well as for aseptic causes alone. This is clinically important given the cost and morbidity associated with reoperation, especially in the revision hip patient population. This was predominantly driven by the higher rate of both failed osseointegration as well as a higher rate of infection in the monoblock group, the reasons for which are unclear. The survivorship rates in this study are comparable to early and midterm rates ranging from 86% to 99% reported previously for modular and nonmodular stems [1, 9, 12–14, 17, 20]. Concerns regarding the use of modular femoral components include mechanically assisted crevice corrosion at the taper junction of the proximal body and distal stem as well as implant fracture at this same junction [17]. Two patients in the modular cohort sustained femoral implant fracture in the setting of compromised proximal bone stock. Concerns regarding mechanically assisted crevice corrosion have not been evident clinically at the current duration of followup in this cohort. Interestingly, one patient in the monoblock cohort required rerevision for mechanically assisted crevice corrosion at the head-neck junction [3].
Given the opportunity to match metaphyseal and diaphyseal sizing with modular prostheses, we anticipated a lower rate of intraoperative fracture in this cohort. The higher rate of fractures seen in the modular cohort could be explained by differences in surgical technique (amount of underreaming, in vivo assembly of the modular femoral prosthesis versus assembly “on the back table,” etc). Specifically, if distal and proximal sizing are optimized with the trial, it may be that the inevitable failure of the real prosthesis to sit in exactly the same orientation as the trial results in hoop stresses above the threshold for fracture. The proximal and distal “fit and fill” with a monoblock prosthesis may be less optimal than with a modular construct, and the difference in the final position of the real implant compared with the trial may be better tolerated with a monoblock implant. The rates of intraoperative fractures seen in the current study are comparable to previous reports ranging from 2% to 30% for both monoblock as well as modular cylindrical and tapered designs [1, 9, 12–14, 17, 20]. The distal geometry of the stem (cylindrical versus tapered) and the variability in the complexity of the defects may have also influenced fracture rates as well. Based on the current literature, the type of distal stem design (cylindrical versus tapered) does not appear to have a significant influence of the rate of intraoperative femur fracture [1, 9, 12–14, 17].
In conclusion, although rerevisions were less common in patients treated with modular stems, aseptic complications such as intraoperative fractures were more common in that group, and the sample was too small to evaluate corrosion-related or fatigue concerns associated with modularity, so we cannot conclude from this that one approach is superior to the other. Larger studies and pooled analyses will need to be performed to answer this question, but we believe in general that modular prostheses should be avoided in femoral revisions of this type if possible.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Stanford University Medical School, Stanford, CA, USA.
References
- 1.Amanatullah DF, Howard JL, Siman H, Trousdale RT, Mabry TM, Berry DJ. Revision total hip arthroplasty in patients with extensive proximal femoral bone loss using a fluted, tapered, modular femoral component. Bone Joint J. 2015;97:312–317. doi: 10.1302/0301-620X.97B3.34684. [DOI] [PubMed] [Google Scholar]
- 2.Cameron HU. The long-term success of modular proximal fixation stems in revision total hip arthroplasty. J Arthroplasty. 2002;17:138–141. doi: 10.1054/arth.2002.32462. [DOI] [PubMed] [Google Scholar]
- 3.Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655–1661. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 5.Garbuz DS, Masri BA, Duncan CP, Greidanus NV, Bohm ER, Petrak MJ, DellaValle CJ, Gross AE. The Frank Stinchfield Award: Dislocation in revision THA: do large heads (36 and 40 mm) result in reduced dislocation rates in a randomized clinical trial? Clin Orthop Relat Res. 2012;470:351–356. doi: 10.1007/s11999-011-2146-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jasty M, Bragdon CR, Haire T, Mulroy RD, Jr, Harris WH. Comparison of bone ingrowth into cobalt chrome sphere and titanium fiber mesh porous coated cementless canine acetabular components. J Biomed Mater Res. 1993;27:639–644. doi: 10.1002/jbm.820270511. [DOI] [PubMed] [Google Scholar]
- 7.Jibodh SR, Schwarzkopf R, Anthony SG, Malchau H, Dempsey KE, Estok DM. Revision hip arthroplasty with a modular cementless stem: mid-term follow up. J Arthroplasty. 2013;28:1167–1172. doi: 10.1016/j.arth.2012.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Kang MN, Huddleston JI, Hwang K, Imrie S, Goodman SB. Early outcome of a modular femoral component in revision total hip arthroplasty. J Arthroplasty. 2008;23:220–225. doi: 10.1016/j.arth.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Konan S, Garbuz DS, Masri BA, Duncan CP. Non-modular tapered fluted titanium stems in hip revision surgery. Bone Joint J. 2014;96:56–59. doi: 10.1302/0301-620X.96B11.34302. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz SM, Ong KL, Schmier J, Mowat F, Saleh K, Dybvik E, Kärrholm J, Garellick G, Havelin LI, Furnes O, Malchau H, Lau E. Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am. 2007;89(Suppl 3):144–151. doi: 10.2106/JBJS.G.00587. [DOI] [PubMed] [Google Scholar]
- 12.Lachiewicz PF, Soileau ES. What is the survivorship of fully-coated femoral components in revision hip arthroplasty. Clin Orthop Relat Res. 2015;473:549–554. doi: 10.1007/s11999-014-3689-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lakstein D, Backstein D, Safir O, Kosashvili Y, Gross AE. Revision total hip arthroplasty with a porous-coated modular stem. Clin Orthop Relat Res. 2010;468:1310–1315. doi: 10.1007/s11999-009-0937-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meek RMD, Garbuz DS, Masri BA, Greidanus NV, Duncan CP. Intraoperative fracture of the femur in revision total hip arthroplasty with a diaphyseal fitting stem. J Bone Joint Surg Am. 2004;86:480–485. doi: 10.2106/00004623-200403000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Moreland JR, Moreno MA. Cementless femoral revision arthroplasty of the hip: minimum 5 years followup. Clin Orthop Relat Res. 2001;393:194–201. doi: 10.1097/00003086-200112000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–242. doi: 10.1097/00003086-199912000-00024. [DOI] [PubMed] [Google Scholar]
- 17.Richards CJ, Duncan CP, Masri BA, Garbuz DS. Femoral revision hip arthroplasty: a comparison of two stem designs. Clin Orthop Relat Res. 2010;468:491–496. doi: 10.1007/s11999-009-1145-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tetreault MW, Shukla SK, Yi PH, Sporer SM, Della Valle CJ. Are short fully coated stems adequate for ‘simple’ femoral revisions? Clin Orthop Relat Res. 2014;472:577–583. doi: 10.1007/s11999-013-3167-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Valle CJD, Paprosky WG. Classification and an algorithmic approach to the reconstruction of femoral deficiency in revision total hip arthroplasty. J Bone Joint Surg Am. 2003;85(Suppl 4):1–6. doi: 10.2106/00004623-200300004-00001. [DOI] [PubMed] [Google Scholar]
- 20.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17:134–137. doi: 10.1054/arth.2002.32461. [DOI] [PubMed] [Google Scholar]