Abstract
Background
As payment models shift toward a focus on value and reimbursement becomes increasingly tied to quality and patient experience, minimizing unexpected acute health needs has become a priority for both policymakers and clinical leaders. Despite recent emphasis on emergency department (ED) visits as a quality measure in surgery, little is known about the role of the ED in the early postoperative period after hand surgery.
Questions/purposes
The purpose of this study was to determine the rates, reasons, and factors associated with ED visits within 30 days of elective outpatient hand surgery.
Methods
Using our institutional database for 2009 through 2013, we assessed ED visit rates for 2332 patients undergoing carpal tunnel or trigger finger release. Medical records were manually reviewed to ascertain the primary reason for the ED visit. Multivariable logistic regression modeling was used to identify factors independently associated with ED use.
Results
A total of 67 patients (3%) experienced at least one ED visit within 30 days of hand surgery (carpal tunnel: 3%; trigger finger: 3%). Most visits (66%) occurred within the first 2 weeks of surgery, and 31% led to hospitalization. The most common reasons for ED visits were pain (18%) and wound issues (16%). Unmarried and medically infirm patients were more likely to visit the ED.
Conclusions
ED visits after hand surgery are common, often related to the procedure, and potentially responsive to quality improvement initiatives. Targeted efforts to educate patients about pain management, wound care, and the expected course of recovery before surgery, together with close postoperative contact (eg, routine phone calls, facsimile correspondence by email, or secure messaging) may limit visits to the ED.
Level of Evidence
Level IV, prognostic study.
Introduction
Emergency department (ED) visits within 30 days of inpatient surgery are common, costly, and may result in readmission [7, 11, 15, 18]. These events often reflect suboptimal postoperative care coordination and perhaps patient anxiety about pain, swelling, or the appearance of the wound in particular [11]. Because the financial risk of uncoordinated care increasingly falls on hospitals and providers, ED visit rates are receiving considerable attention as a quality and cost-containment indicator [2, 7, 11, 15, 18].
Although nearly two-thirds of all surgeries are now outpatient [1, 17], research on postoperative ED use has focused largely on inpatient surgeries [7, 11, 15, 16, 18, 20]. For instance, little is known regarding ED use among patients undergoing common outpatient hand procedures such as carpal tunnel and trigger finger release. An understanding of the reasons, timing, and factors associated with ED visits after hand surgery can inform the development of effective strategies aimed at simultaneously improving quality and reducing costs.
To address this gap in knowledge, we sought to examine ED visit rates within 30 days of hand surgery and to characterize the underlying reasons and predisposing factors for ED use.
Materials and Methods
This retrospective cohort study was conducted at a large urban academic hospital in the United States. After institutional review board approval, we used Current Procedural Terminology (CPT) codes to identify all patients undergoing minor elective hand surgery between January 1, 2009, and December 31, 2013. We considered carpal tunnel release (CPT code 64721) and trigger finger release (CPT code 26055) because they are the two most commonly performed hand surgeries.
To select a homogenous cohort of adult patients at low surgical risk, we excluded patients aged younger than 18 years of age, patients undergoing more than one procedure on the same visit, and those who had been seen in the ED in the 30 days before surgery. The final study cohort consisted of 2332 records with 1507 (65%) carpal tunnel releases and 825 (35%) trigger finger releases.
The primary outcome of interest was an ED visit within 30 days of surgery. Visits to the ED within our system were identified using electronic health and claims data. Medical records of patients with an ED visit were then manually reviewed to ascertain the primary reason for this event. Reasons for the ED visit that were considered to be directly related to the procedure included pain, wound complications (infection, dehiscence), and hematoma. Additionally, our institutional database was queried to collect data on demographic characteristics that might be associated with ED visits after hand surgery. Specifically, we collected data on age, sex, race/ethnicity, primary language, and marital status. Baseline comorbidity status was quantified using the Charlson Comorbidity Index [3, 5, 14].
Statistical Analysis
Descriptive statistics were used to report the rates and reasons for ED visits after surgery. We calculated overall and procedure-specific observed rates of ED visits at 14 and 30 days as well as the timing of visits and the proportion of visits that resulted in hospital admission (Table 1). The reasons for ED visits were assessed to determine if they were directly related to the procedure. In addition, we classified ED visits into categories on the basis of the primary reason for the visit and reported the five most common causes of ED visits (Table 2).
Table 1.
Rates of 30-day emergency department visits after hand surgery
| ED visit | Procedure | ||
|---|---|---|---|
| Overall | Carpal tunnel release | Trigger finger release | |
| (n = 2332) | (n = 1507) | (n = 825) | |
| Within 14 days, number (%) | 44 (2) | 26 (2) | 18 (2) |
| Within 30 days, number (%) | 67 (3) | 42 (3) | 25 (3) |
| Days to ED visit, mean ± SD | 13 ± 8 | 14 ± 8 | 12 ± 9 |
| Resulting in hospital admission, number (%) | 21 (1) | 13 (1) | 8 (1) |
ED = emergency department.
Table 2.
Reasons for 30-day emergency department visits after hand surgery
| Reason for ED visit | Procedure | ||
|---|---|---|---|
| Overall | Carpal tunnel release | Trigger finger release | |
| (n = 67) | (n = 42) | (n = 25) | |
| Directly related to the procedure, number (%) | 24 (36) | 15 (36) | 9 (36) |
| Five most common reasons related to all ED visits, number (%) | |||
| Pain | 12 (18) | 9 (21) | 3 (12) |
| Wound complication* | 11 (16) | 5 (12) | 6 (25) |
| Gastrointestinal | 8 (12) | 6 (14) | 2 (8) |
| Musculoskeletal injury/fall | 8 (12) | 4 (9.5) | 4 (16) |
| Opioid-related | 5 (7) | 3 (7) | 2 (8) |
* Includes surgical site infection and wound dehiscence; ED = emergency department.
Multivariable logistic regression modeling was performed to identify which patient characteristics were independently associated with at least one ED visit within 30 days of surgery (Table 3). The model included age (as a continuous variable), sex, race/ethnicity (white, nonwhite, unknown), primary language (English, non-English), marital status (single, married, separated/divorced, widowed), the Charlson Comorbidity Index (as a continuous variable), and procedure type (carpal tunnel, trigger finger). All covariates were entered into the model simultaneously without further selection. Results were reported as odds ratios (ORs) with 95% confidence intervals (CIs). Statistical significance was set at p value < 0.05.
Table 3.
Factors associated with 30-day emergency department visits after hand surgery
| Parameter | 30-day ED visit | ED visit rate | Adjusted OR (95% CI)* | p value | |
|---|---|---|---|---|---|
| No | Yes | per 100 | |||
| Age (years), mean ± SD | 61 ± 14 | 61 ± 19 | – | 0.92 (0.74–1.1), per 10-year increase | 0.42 |
| Sex (%) | |||||
| Female | 58 | 54 | 2.7 | Reference | |
| Male | 42 | 46 | 3 | 1.2 (0.71–2.1) | 0.48 |
| Race/ethnicity (%) | |||||
| White | 84 | 88 | 3.0 | Reference | |
| Nonwhite | 13 | 12 | 2.7 | 0.85 (0.35–2.1) | 0.73 |
| Unknown | 3.5 | 0 | – | – | – |
| Primary language (%) | |||||
| English | 91 | 96 | 3.0 | Reference | |
| Non-English | 9.3 | 4.5 | 1.4 | 1.6 (0.47–5.8) | 0.44 |
| Marital status (%) | |||||
| Single | 20 | 30 | 4.2 | 2.0 (1.1–3.8) | 0.036 |
| Married | 62 | 43 | 2.0 | Reference | |
| Separated or divorced | 9.5 | 13 | 4.0 | 1.7 (0.72–4.0) | 0.23 |
| Widowed | 8.6 | 13 | 4.4 | 2.8 (1.2–6.4) | 0.016 |
| Charlson Comorbidity Index, mean ± SD | 1.6 ± 1.9 | 2.2 ± 2.0 | – | 1.1 (1.01–1.3), per 1-unit increase | 0.043 |
| Procedure (%) | |||||
| Carpal tunnel release | 65 | 63 | 2.8 | Reference | |
| Trigger finger release | 35 | 37 | 3.0 | 1.1 (0.64–1.9) | 0.73 |
* Area under the receiver operating characteristic curve = 0.74 (95% CI, 0.73–0.75); Nagelkerke R2 = 0.074; p value for Hosmer and Lemeshow test = < 0.001; ED = emergency department; OR = odds ratio; CI = confidence interval.
Results
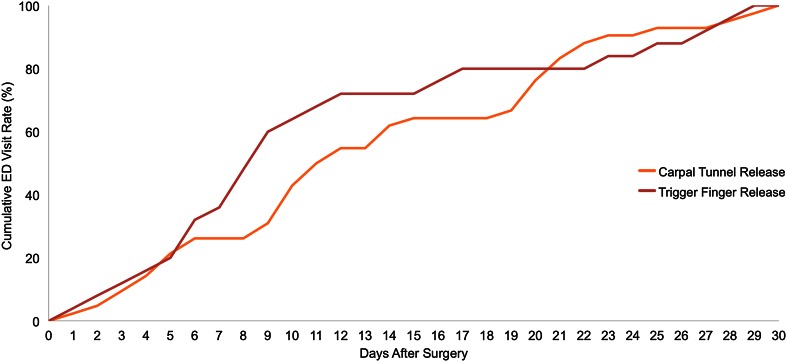
The overall rate of postoperative ED visits was 1.9% at 14 days (carpal tunnel: 1.7%; trigger finger: 2%) and 3% at 30 days (carpal tunnel: 2.8%; trigger finger: 3.0%). Most ED visits after both trigger finger (72%) and carpal tunnel (62%) surgery occurred within the first 14 days (Fig. 1). Nearly one-third (31%) of all ED visits resulted in hospital admission (Table 1) with wound complications being the most common reason for hospitalization.
Fig. 1.
Figure showing cumulative ED visit rates after carpal tunnel and trigger finger release.
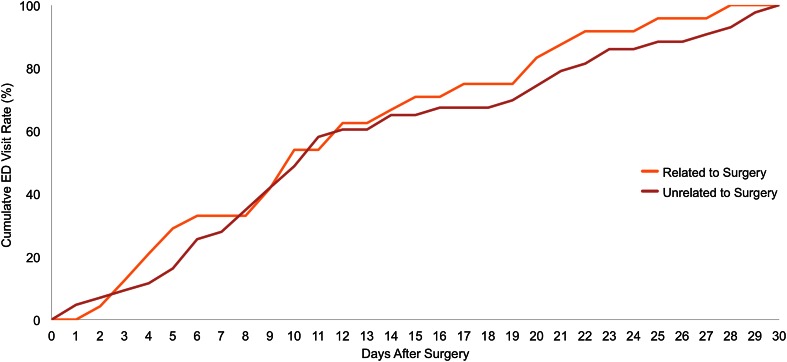
The most common overall reason for ED visits within 30 days was pain (18%) followed by wound issues (16%), gastrointestinal problems (12%), musculoskeletal injury/fall (12%), and opioid-related adverse events (7%). Over one-third (36%) of all ED visits were directly related to the surgical procedure (Table 2). Thirty-three percent of the ED visits related to the procedure occurred within the first week compared with 28% of the ED visits unrelated to the procedure (Fig. 2).
Fig. 2.
Figure showing cumulative ED visit rates for reasons related and unrelated to surgery.
After controlling for potential confounding effects in multivariable modeling (Table 3), factors independently associated with 30-day ED visits included greater comorbidity burden (OR, 1.1 per one-unit increase in the Charlson index; 95% CI, 1.01–1.3; p = 0.043) and being single (OR, 2.0; 95% CI, 1.1–3.8; p = 0.036) or widowed (OR, 2.8; 95% CI, 1.2–6.4; p = 0.016 versus married).
Discussion
As payment models shift toward a focus on value and reimbursement becomes increasingly tied to quality and patient experience, minimizing unexpected acute health needs has become a priority for both policymakers and clinical leaders. Despite recent emphasis on ED visit as a quality measure in surgery, little is known about the role of the ED in the early postoperative period after hand surgery. We therefore sought to determine the rates, causes, and predictors of ED visits after hand surgery.
Our analysis should be interpreted cautiously in light of its shortcomings. This study was performed at a single large academic center in the United States, which may limit generalizability to other settings and populations. Moreover, given that we were unable to capture return to care provided in an ED outside of our system, the incidence of ED visits reported here may be an underestimate. Finally, we were unable to assess health literacy—an increasingly recognized issue that has been associated with healthcare resource use [13].
Given the limited data available on this topic, our work provides important baseline information regarding ED use after hand surgery. We found that 3% of patients experienced at least one ED visit within 30 days of minor elective hand surgery. A recent study by Fox and colleagues [8] in 3,821,670 patients undergoing outpatient surgery at 1295 centers in California, Florida, and Nebraska showed that the rate of ED visits within the first week of surgery was 2%. Another population-based analysis in patients undergoing outpatient colonoscopy yielded a similar rate of acute care visits [6]. The timing of these events is relevant when focusing on how to reduce unnecessary visits to the ED. Our finding that most visits occurred within the first 2 weeks of surgery suggests that interventions such as calling patients after surgery, facilitating contact with the surgeon and his or her team using email and secure messaging, and methods for transforming ED visits to office followups might help. The observation that nearly one-third of all ED visits led to hospitalization underscores the economic repercussions associated with these events and serves to better understand the intense national focus on reducing postoperative acute care visits.
We found that nearly one in five ED visits after elective outpatient hand surgery was related to pain. In line with our finding, Curtin and Hernandez-Boussard [2] showed that pain-related issues constitute the most common reason for ED visits after treatment of a distal radius fracture. Pain is also the most common cause of ED visits after tonsillectomy [4]. It is our opinion that efforts to reduce pain-related ED visits after hand surgery should start the first moment surgery is considered through education about pain management and setting realistic expectations. Another common reason for ED visits was wound complications (eg, infection, dehiscence). Many of these are minor problems such as suture abscesses, unraveling of one suture, or simply concern about how the wound looks. These are problems that can be managed with telephone calls, emails with image exchange, and arrangement for office rather than ED evaluation. Interventions aimed at ensuring that discharge instructions are clear and tailored to all levels of health literacy may also help limit ED visits for discomfort and wound issues.
We observed that higher comorbidity burden—assessed with the Charlson Index— was linked to greater likelihood of ED visits, which is consistent with previous research suggesting that the Charlson Index is useful in predicting readmission after inpatient orthopaedic surgery [9, 12, 19]. Unmarried patients were more likely to visit the ED after hand surgery, possibly because they had less social support than married patients. The latter finding underscores the importance of adjusting for sociodemographic characteristics when linking financial penalties to ED visits or readmissions [10]. Without appropriate risk adjustment, quality incentives might have the unintended consequence of making hand surgeons reluctant to operate on patients with less support at home.
In conclusion, we demonstrated that ED visits after hand surgery are common, often related to the procedure, and potentially responsive to quality improvement initiatives. Targeted efforts to educate patients about pain management, wound care, and the expected course of recovery before surgery, together with close postoperative contact (eg, routine phone calls, facsimile correspondence by email, or secure messaging) may limit visits to the ED. Our data suggest that the ED visit might be a useful indicator to drive quality improvement in hand surgery.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States. Natl Health Stat Report. 2006;2009:1–25. [PubMed] [Google Scholar]
- 2.Curtin CM, Hernandez-Boussard T. Readmissions after treatment of distal radius fractures. J Hand Surg Am. 2014;39:1926–1932. doi: 10.1016/j.jhsa.2014.07.041. [DOI] [PubMed] [Google Scholar]
- 3.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 4.Edmonson MB, Eickhoff JC, Zhang C. A population-based study of acute care revisits following tonsillectomy. J Pediatr. 2015;166(607–612):e605. doi: 10.1016/j.jpeds.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 5.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Fox JP, Burkardt DD, Ranasinghe I, Gross CP. Hospital-based acute care after outpatient colonoscopy: implications for quality measurement in the ambulatory setting. Med Care. 2014;52:801–808. doi: 10.1097/MLR.0000000000000176. [DOI] [PubMed] [Google Scholar]
- 7.Fox JP, Suter LG, Wang K, Wang Y, Krumholz HM, Ross JS. Hospital-based, acute care use among patients within 30 days of discharge after coronary artery bypass surgery. Ann Thorac Surg. 2013;96:96–104. doi: 10.1016/j.athoracsur.2013.03.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fox JP, Vashi AA, Ross JS, Gross CP. Hospital-based, acute care after ambulatory surgery center discharge. Surgery. 2014;155:743–753. doi: 10.1016/j.surg.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hageman MG, Bossen JK, Smith RM, Ring D. Predictors of readmission in orthopaedic trauma surgery. J Orthop Trauma. 2014;28:e247–249. doi: 10.1097/BOT.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 10.Jha AK, Zaslavsky AM. Quality reporting that addresses disparities in health care. JAMA. 2014;312:225–226. doi: 10.1001/jama.2014.7204. [DOI] [PubMed] [Google Scholar]
- 11.Kocher KE, Nallamothu BK, Birkmeyer JD, Dimick JB. Emergency department visits after surgery are common for Medicare patients, suggesting opportunities to improve care. Health Aff (Millwood). 2013;32:1600–1607. doi: 10.1377/hlthaff.2013.0067. [DOI] [PubMed] [Google Scholar]
- 12.Menendez ME, Neuhaus V, van Dijk CN, Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014;472:2878–2886. doi: 10.1007/s11999-014-3686-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mitchell SE, Sadikova E, Jack BW, Paasche-Orlow MK. Health literacy and 30-day postdischarge hospital utilization. J Health Commun. 2012;17(Suppl 3):325–338. doi: 10.1080/10810730.2012.715233. [DOI] [PubMed] [Google Scholar]
- 14.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 15.Rising KL, White LF, Fernandez WG, Boutwell AE. Emergency department visits after hospital discharge: a missing part of the equation. Ann Emerg Med. 2013;62:145–150. doi: 10.1016/j.annemergmed.2013.01.024. [DOI] [PubMed] [Google Scholar]
- 16.Saab S, Noureddine S, Dumit NY. Readmission rates and emergency department visits after coronary artery bypass graft surgery and related factors. J Med Liban. 2013;61:155–160. doi: 10.12816/0001444. [DOI] [PubMed] [Google Scholar]
- 17.Schaefer MK, Jhung M, Dahl M, Schillie S, Simpson C, Llata E, Link-Gelles R, Sinkowitz-Cochran R, Patel P, Bolyard E, Sehulster L, Srinivasan A, Perz JF. Infection control assessment of ambulatory surgical centers. JAMA. 2010;303:2273–2279. doi: 10.1001/jama.2010.744. [DOI] [PubMed] [Google Scholar]
- 18.Vashi AA, Fox JP, Carr BG, D’Onofrio G, Pines JM, Ross JS, Gross CP. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309:364–371. doi: 10.1001/jama.2012.216219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Voskuijl T, Hageman M, Ring D. Higher Charlson Comorbidity Index Scores are associated with readmission after orthopaedic surgery. Clin Orthop Relat Res. 2014;472:1638–1644. doi: 10.1007/s11999-013-3394-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Young WG, Succar E, Hsu L, Talpos G, Ghanem TA. Causes of emergency department visits following thyroid and parathyroid surgery. JAMA Otolaryngol Head Neck Surg. 2013;139:1175–1180. doi: 10.1001/jamaoto.2013.4505. [DOI] [PubMed] [Google Scholar]