Abstract
Background
Patients with failed distal femoral megaprostheses often have bone loss that limits reconstructive options and contributes to the high failure rate of revision surgery. The Compress® Compliant Pre-stress (CPS) implant can reconstruct the femur even when there is little remaining bone. It differs from traditional stemmed prostheses because it requires only 4 to 8 cm of residual bone for fixation. Given the poor long-term results of stemmed revision constructs, we sought to determine the failure rate and functional outcomes of the CPS implant in revision surgery.
Questions/purposes
(1) What is the cumulative incidence of mechanical and other types of implant failure when used to revise failed distal femoral arthroplasties placed after oncologic resection? (2) What complications are characteristic of this prosthesis? (3) What function do patients achieve after receiving this prosthesis?
Methods
We retrospectively reviewed 27 patients who experienced failure of a distal femoral prosthesis and were revised to a CPS implant from April 2000 to February 2013. Indications for use included a minimum 2.5 mm cortical thickness of the remaining proximal femur, no prior radiation, life expectancy > 10 years, and compliance with protected weightbearing for 3 months. The cumulative incidence of failure was calculated for both mechanical (loss of compression between the implant anchor plug and spindle) and other failure modes using a competing risk analysis. Failure was defined as removal of the CPS implant. Followup was a minimum of 2 years or until implant removal. Median followup for patients with successful revision arthroplasty was 90 months (range, 24–181 months). Functional outcomes were measured with the Musculoskeletal Tumor Society (MSTS) functional assessment score.
Results
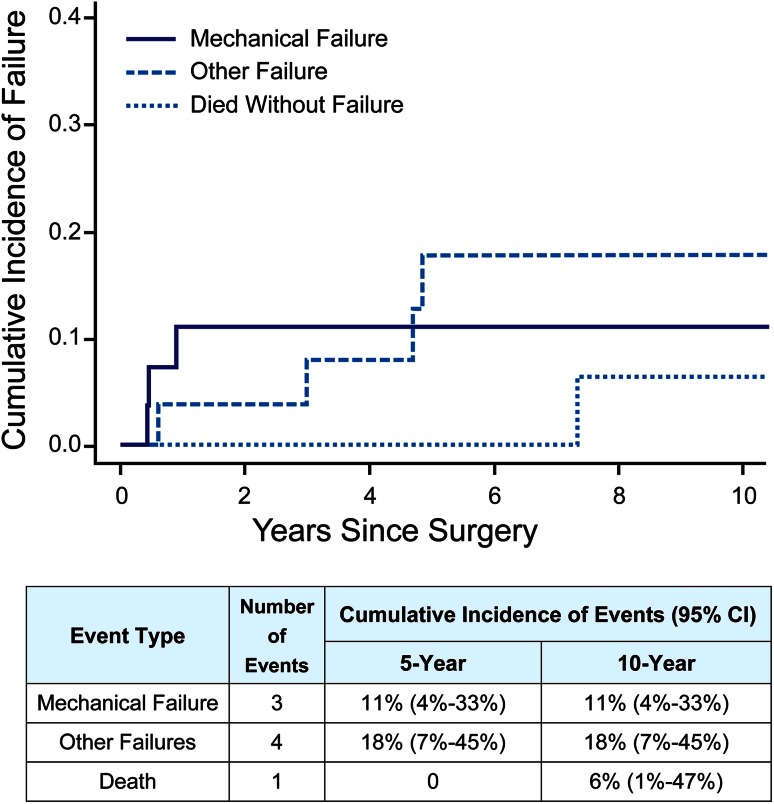
The cumulative incidence of mechanical failure was 11% (95% confidence interval [CI], 4%–33%) at both 5 and 10 years. These failures occurred early at a median of 5 months. The cumulative incidence of other failures was 18% (95% CI, 7%–45%) at 5 and 10 years, all of which were deep infection. Three patients required secondary operations for cortical insufficiency proximal to the anchor plug in bone not spanned by the CPS implant and unrelated to the prosthesis. Median MSTS score was 27 (range, 24–30).
Conclusions
Revision distal femoral replacement arthroplasty after a failed megaprosthesis is often difficult as a result of a lack of adequate bone. Reconstruction with the CPS implant has an 11% failure rate at 10 years. Our results are promising and demonstrate the durable fixation provided by the CPS implant. Further studies to compare the CPS prosthesis and other reconstruction options with respect to survival and functional outcomes are warranted.
Level of Evidence
Level IV, therapeutic study.
Introduction
After oncologic resection of the distal femur, primary reconstruction with a stemmed distal femoral megaprosthesis has become the most widely used reconstruction strategy. However, with the growing population of young, active cancer survivors, long-term reconstructive failure awaits most of these patients. The most common reasons for failure include femoral stem loosening and infection with hardware failure and local recurrence accounting for a small percentage [1, 4, 6, 11, 14–16, 18, 20, 21, 23, 26, 29–31, 33, 34]. Failures of stemmed megaprostheses leave surgeons with few reconstructive solutions and present a challenging surgical problem. Severe femoral bone deficiency after fracture or loosening of a prior stem traditionally results in revision to a cemented or large-diameter press-fit stemmed implant, an allograft-prosthetic composite (APC) reconstruction, or a total femur replacement [7, 23, 26, 33]. Unfortunately, short residual proximal femur segments cannot be addressed by these options and these constructs have high failure rates, often exceeding 30% at 5 years [20, 22, 23, 26, 29, 33]. We need to improve our current strategies to preserve or reconstitute the remaining femoral bone stock while creating a more durable revision construct.
The Compress® Compliant Pre-Stress (CPS) implant (Biomet, Warsaw, IN, USA) provides compliant self-adjusting compression through a short (4 cm or 8 cm) intramedullary traction bow that generates compressive forces that promote biologic fixation using the principle of Wolff’s law [2, 8]. In retrieval studies, this FDA-approved device has been shown to induce bone hypertrophy at the distal bone–prosthetic junction in stably fixed implants [5, 17]. These features make this implant an attractive option when a short distal femoral segment remains and revision surgery is needed. The CPS implant has a published survival rate of as high as 89% at 5 years [19] and 80% at 10 years [13] when used for primary oncologic reconstruction [24]. In short-term comparison studies, it was shown to have equivalent or higher survival than cemented [3, 24] and press-fit [10] stemmed implants for primary oncologic reconstruction [3, 24]. Given the versatility of the CPS implant, we began using it for revision of failed distal femoral prostheses, particularly when the residual femoral bone segment was very short, precluding use of a stemmed implant. The performance of this implant in the setting of revision arthroplasty has not been evaluated.
We therefore asked: (1) What is the cumulative incidence of mechanical and other types of implant failure when used to revise failed distal femoral arthroplasties placed after oncologic resection? (2) What complications are characteristic of this prosthesis? (3) What function do patients achieve after receiving this prosthesis?
Patients and Methods
An institutional review board-approved retrospective review of our surgical database identified all patients with a distal femoral Compress® placed for revision of a failed distal femoral oncologic megaprosthesis. All operations were performed at a single tertiary cancer center by three orthopaedic oncologists (JHH, CDM, PJB) between April 2000 and February 2013.
During this study period, a total of 71 patients required revision surgery for a failed distal femoral megaprosthesis. Indications for revision to a CPS implant included a minimum 2.5-mm cortical thickness of remaining proximal femur without significant areas of attenuation, cortical defect, or osteolysis. Intraoperative physical measurement confirmed our preoperative radiographic assessment. Additional indications included a minimum 4 cm of residual subtrochanteric femur to accommodate the anchor plug, no history of previous femoral radiation therapy, life expectancy greater than 10 years, the ability to comply with protected weightbearing for 3 months, and having had a previous minimum distal femoral resection of 14 cm required for the implant diaphyseal components. Forty-four patients did not meet these indications and were therefore revised using a cemented stem, custom large-diameter press-fit stem with interlocking screws for proximal fixation, or APCs; severely attenuated bone was the most common contraindication to a CPS implant.
The remaining 27 patients underwent 30 procedures in which a failed distal femoral prosthesis was revised to a CPS implant. Minimum followup for inclusion was 24 months or until implant removal. Our final study group had 13 females and 14 males with a mean age of 30 years (range, 13–62 years) at the time of surgery. The most common diagnosis necessitating primary oncologic resection and reconstruction was osteogenic sarcoma (Table 1). All patients undergoing revision had completed adjuvant oncologic treatment before the time of their revision surgery. Twenty-four of the 27 patients undergoing revision had their primary resection and reconstruction performed at our institution. The remaining three were externally referred. The median time from the primary procedure to revision was 57 months (range, 6–167 months). Surgical indications for revision included aseptic loosening, infection, mechanical failure, and others (Table 1).
Table 1.
Patient demographics and clinical characteristics
| Demographics and characteristics | Revision CPS implant patients |
|---|---|
| Number of patients | 27 |
| Age (years; range) | 30 (13–62) |
| Sex | |
| Male | 14 |
| Female | 13 |
| Tumor diagnosis | |
| High-grade osteogenic sarcoma | 20 |
| Parosteal osteogenic sarcoma | 2 |
| Chondrosarcoma | 1 |
| Malignant fibrous histiocytoma of bone | 1 |
| Other tumor (pigmented villonodular synovitis, hemangiomatosis, synovial chondromatosis) | 2 |
| No tumor (infected periprosthetic fracture) | 1 |
| Indication for revision | |
| Aseptic loosening press-fit femoral stem | 11 |
| Aseptic loosening cemented femoral stem | 5 |
| Infection of primary prosthesis | 6 |
| Mechanical failure of primary Compress® | 2 |
| Periprosthetic fracture | 1 |
| Failed osteoarticular allograft | 1 |
| Failed Guepar prosthesis | 1 |
CPS = Compress® Compliant Pre-stress.
During the revision procedure, after removal of the primary femoral prosthesis or antibiotic spacer, the remaining distal femoral bone stock was assessed. If the bone appeared attenuated or atrophic, a fresh cut was made until bleeding, viable bone was observed. Based on a retrieval study finding osteonecrotic bone adjacent to failed CPS implants [13], we excised dysvascular or necrotic bone to improve the potential for bone hypertrophy and implant osteointegration. Aided by fluoroscopy, residual cement from the previous surgery was removed with standard cement removal instruments (eg, a high-speed burr or ultrasonic cement removal tool). Small areas of well-integrated cement that did not span the entire compression distance were retained to prevent jeopardizing the host bone as long as there was sufficient space to insert an anchor plug in the medullary canal. The implant was then placed in accordance with the manufacturer’s recommended technique and attached to an Orthopaedic Salvage System rotating hinged platform (Biomet, Warsaw, IN, USA) in most patients. Derotational pins were not placed in any patient. Two patients had a Biomet custom extensible diaphyseal component and one patient had a custom adapter made to connect the CPS implant with a Global Modular Replacement System (Stryker, Kalamazoo, MI, USA). If well aligned and fixed, the original tibial component was left in place. Before closure, autogenous bone graft from the resected distal femoral bone stock was placed adjacent to the bone-spindle interface and held in place with Vicryl® (Ethicon, Somerville, NJ, USA) mesh.
The CPS implant requires a minimum femoral cortical thickness of ≥ 2.5 mm to support the minimum 400 pounds of compression between the spindle and anchor plug. Per the manufacturer’s recommendation, the magnitude of compression is selected after measuring the thinnest cortical width on the cut surface of the distal femur (2.5–3.9 mm: 400 lbs; 4–5.4 mm: 600 lbs; ≥ 5.5 mm: 800 lbs). In our patient series, the magnitude of compression used was 400 lbs (n = 4), 600 lbs (n = 15), and 800 lbs (n = 8). Any cortical defect between the spindle and anchor plug increases the risk of periprosthetic fracture and is therefore a relative contraindication to using the CPS implant for primary or revision surgery. Evaluation of femoral cortical thickness in revision patients was performed with preoperative radiographs, intraoperative examination, and, more recently, with a preoperative CT scan. In one patient with prior mechanical failure of a CPS implant, the holes from the prior anchor plug pins were located between the spindle and new anchor plug when the revision implant was placed. Rather than resect an additional 8 cm of bone, these five small bicortical holes were bone-grafted at the time of revision surgery without further event.
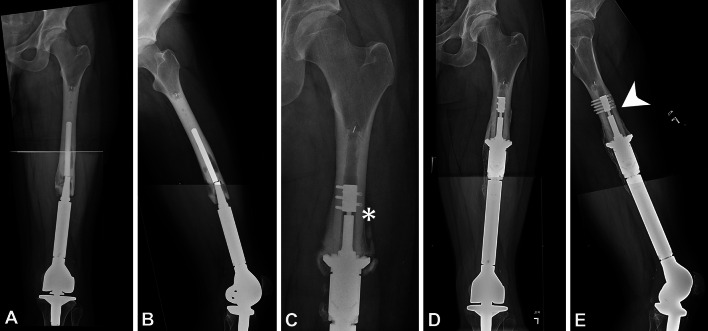
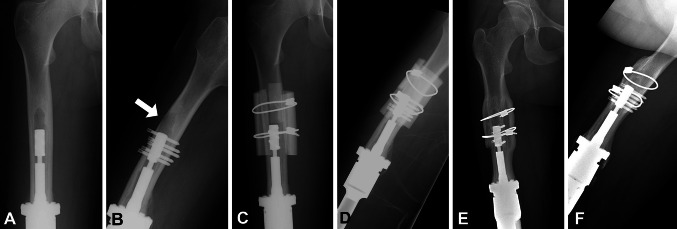
Postoperatively, patients were allowed toe-touch weightbearing for the first 6 weeks, 50% weightbearing for the subsequent 6 weeks, and then allowed to progress to full weightbearing as tolerated if clinically and radiographically stable. Clinical stability was confirmed if, on physical examination, there was no pain with internal and external hip rotation with the knee fixed at 90° of flexion. Radiographic stability was confirmed by maintenance of compression distance of the traction bar between the anchor plug and spindle (Fig. 1) and by evidence of bone hypertrophy proximal to the spindle.
Fig. 1A–E.
Preoperative (A) AP and (B) lateral radiographs of a 22-year-old man show a fractured cemented femoral stem 4 years after resection of a distal femoral osteogenic sarcoma. (C) An AP radiograph reveals mechanical failure, defined as a loss of compression between the anchor plug and spindle (asterisk), 5 months after placement of a revision CPS implant. (D) AP and (E) lateral radiographs taken 5 years after his second revision CPS implant show radiographic evidence of bone hypertrophy proximal to the spindle that is seen when there is osteointegration and an appropriately maintained traction distance (arrowhead).
At each followup visit, patients were assessed for mobility, knee ROM, and pain by their primary surgeon. Radiographs were closely reviewed to assess implant integrity and to monitor for evidence of recurrent disease. A functional evaluation was performed using the revised 30-point functional classification system established by the Musculoskeletal Tumor Society (MSTS) [9].
Median followup for patients without implant failure was 90 months (range, 24–181 months). No patients were lost to followup. After close followup at our institution for at least 2 years after their surgery, three patients have been followed at outside institutions and have remained in contact with updated notes and radiographs. One patient died from a secondary malignancy 7 years after revision surgery. Thus, the cumulative incidence of death was 6% (95% confidence interval [CI], 1%–47%) at 10 years.
Statistical Analysis
Given the risk of death from oncologic or associated causes in our patient population, a competing risk analysis was performed [25]. The cumulative incidence of all CPS implant failures was first calculated with death as a competing event, and failure was defined as removal of the spindle and anchor plug for any reason. We then calculated the cumulative incidence of mechanical failure alone, defined as loss of compression between the anchor plug and spindle, and compared this with all other modes of failure necessitating implant removal such as infection, periprosthetic fracture, or amputation. Repeat procedures for polyethylene or bushing wear, arthrofibrosis, limb lengthening, or fracture elsewhere in the extremity were not included in the analysis.
Results
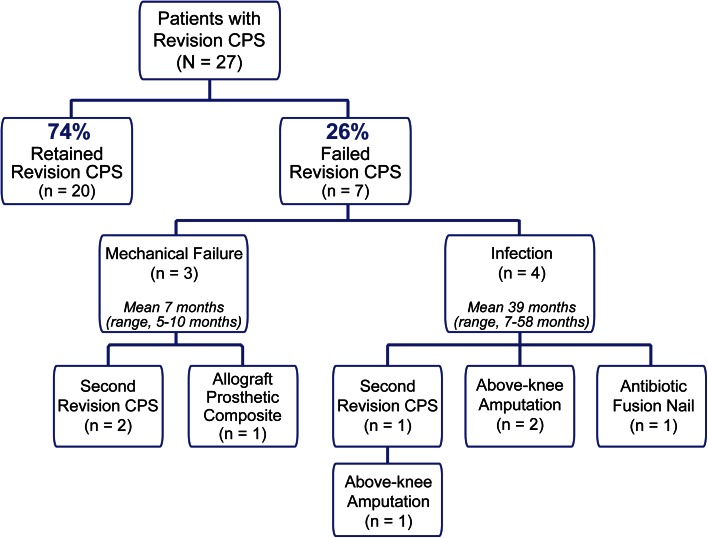
The cumulative incidence of mechanical failure was 11% (95% CI, 4%–33%) at both 5 and 10 years (Fig. 2). These failures occurred early at a median of 5 months (range, 5–10 months). The cumulative incidence of other failures was 18% (95% CI, 7%–45%) at 5 and 10 years; all of these failures were the result of infection (Fig. 2). Thus, the cumulative incidence of all failures was 29% (95% CI, 15%–56%) at 5 and 10 years. The entire implant, including the anchor plug and spindle, was removed from seven patients (26%) at a median of 10 months (range, 5–58 months) (Fig. 3). Mechanical failure, with radiographic evidence of loss of compression accompanied by a lack of bone hypertrophy, occurred in three patients who presented with pain and rotational instability. The remaining four patients (15%) developed infections, necessitating the removal of an osteointegrated CPS implant at a mean of 39 months (range, 7–58 months); half of these patients had an infected prosthesis and antibiotic spacer before placement of the revision CPS implant. Two of the four patients with infection were treated with an above-knee amputation. One patient was treated with an antibiotic cement fusion nail and suppressive antibiotics and has been well for 3.5 years. The fourth patient underwent a two-stage operation with placement of a second CPS implant. However, 6 years later, the patient presented with a deep infection and underwent a high above-knee amputation.
Fig. 2.
The cumulative incidence of mechanical failures and other failures of revision CPS reconstruction was calculated with death as a competing event.
Fig. 3.
The clinical course of all revision CPS patients is summarized in the flow diagram, with mean time to failure listed for both mechanical failure and other failures.
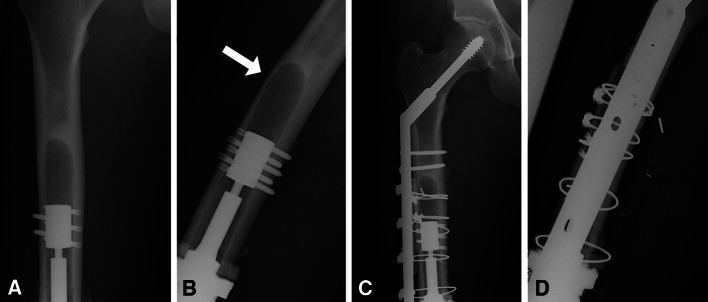
Three patients with revision implants developed unique complications related to cortical insufficiency and required reoperation. All underwent a secondary operation within 4 months of the revision surgery to address a femoral cortical bone deficiency proximal to and not involving the anchor plug; these deficiencies were located at the proximal aspect of the previously loose stemmed implant. None of these patients had a preoperative CT scan and these defects were not appreciated on preoperative radiographs. Two patients fractured through these cortical defects (Fig. 4) without disrupting the anchor plug transfixion pins. These fractures were treated with a plate and strut allograft. One patient’s fracture healed and he has had excellent function for 10 years, but the other patient developed an infected nonunion and underwent an amputation. The third patient was successfully treated for an impending fracture with an onlay strut allograft that healed uneventfully and has maintained excellent function (Fig. 5). In each case, CPS fixation and compression were maintained after the trauma of fracture or secondary procedure.
Fig. 4A–D.
(A) AP and (B) lateral radiographs of a 28-year-old man show an anterior cortical defect proximal to the anchor plug (arrow) at the previous location of a loose stem. Postoperative (C) AP and (D) lateral radiographs show placement of a side plate and strut allograft for treatment of a nondisplaced fracture that occurred at the prior cortical defect.
Fig. 5A–F.
(A) AP and (B) lateral radiographs of a 15-year-old girl show an anterior cortical defect (arrow) proximal to the anchor plug at the previous location of a loose stem. Postoperative (C) AP and (D) lateral radiographs show strut allografts and cables placed to prevent fracture. Five-year followup (E) AP and (F) lateral radiographs show complete bony incorporation of the allograft.
At a median of 90 months (range, 24–181 months), the median MSTS score of the 21 patients who retained their implant was 27 (range, 24–30). An active 90° arc of motion of the affected knee was maintained in 17 (81%) patients. Four (19%) patients had an extensor lag greater than 10° (range, 20°–40°).
Discussion
The best approach to the revision of failed distal femoral megaprostheses has not been defined. This problem is especially important in young patients who are surgically cured of a primary bone malignancy. Existing options include press-fit and cemented stemmed prostheses and APCs. Although they provide the mainstay of available primary and revision constructs, long-term implant survival is often poor at or beyond 5 years [12, 20, 23, 26, 28, 29, 32, 33]. Other reconstructive options are also limited due to the severe bone loss that is commonly associated with the prosthetic failure. The minimal residual femoral bone needed to accommodate the CPS implant makes it a useful option in these difficult situations. We reviewed our experience with the CPS implant to determine the failure rate and functional outcome when used in patients with failed distal femoral megaprostheses with severe bone loss but with sufficient remaining bone to accommodate the implant. We found an 11% cumulative incidence of mechanical failure and 18% cumulative incidence of all other types of failure at 5 and 10 years, even in patients with prior megaprosthesis infection. There were few surgical complications. Three patients required early reoperation to address adjacent regional cortical defects proximal to the anchor plug and unrelated to the CPS implant. Patients had very good functional results. The median MSTS score of the 21 patients who retained their revision CPS implant was 27. Thus, there was good function in these durable reconstructions.
Our study has several limitations. This is a retrospective analysis of patients who had revision of failed prior oncologic megaprostheses. Our series of 27 patients is small but homogeneous with respect to anatomic location and prosthetic device used, unlike other studies in which revision patients with different prostheses and anatomic sites were analyzed as a single heterogeneous group [20, 23, 26, 28, 29, 33] (Table 2). A major limitation is that we lack a comparison group of revision patients reconstructed by other methods such as a cemented stem, a press-fit stem, or an APC and are thus limited to comparison with only a handful of published studies. Lastly, we are using a modern prosthesis with only 10 years of published survival data for primary oncologic reconstruction. Although our incidence of failure is low in this revision study, we cannot predict the long-term performance of this implant.
Table 2.
Summary of studies reporting revision megaprosthesis survivorship
| Study | Year | Number of Patients | Site | Prosthesis | Kaplan-Meier survival (%) | Years of Kaplan-Meier survival (years) |
|---|---|---|---|---|---|---|
| Unwin et al. [28] | 1991 | 47 | Distal femur | Stanmore custom (Elstree, UK) | 18.8 | 5 |
| Unwin et al. [29] | 1995 | 83 | Mixed | Stanmore custom | 45 | 5 |
| Wirganowicz et al. [33] | 1999 | 48 | Mixed | Kinematic® (Howmedica now Stryker, Kalamazoo, MI, USA), Noiles® (Techmedica, Inc, Camarillo, CA, USA), Lacey® (Dow-Corning/Wright Medical, Memphis, TN, USA) | 34 (± 9) (failure rate) | 7 |
| Shin et al. [26] | 1999 | 35 | Distal femur and proximal tibia | Custom | 65 | 10 |
| Morgan et al. [20] | 2006 | 32 | Distal femur and proximal tibia | HMRS (Stryker, Kalamazoo, MI, USA) | 44 | 10 |
| Pala et al. [23] | 2015 | 72 | Distal femur and proximal tibia | GMRS (Stryker, Kalamazoo, MI, USA) | 72 | 8 |
GMRS = Global Modular Replacement System; HMRS = Howmedica Modular Replacement System.
Our cohort of 27 patients with revision CPS implants had an 11% incidence of mechanical failure at 10 years, which is lower than that of other revision studies and comparable to the results observed when this implant is used in the primary reconstruction setting [13]. We believe these data support the potential long-term durability of an osteointegrated CPS implant. Aseptic mechanical failures occurred early, within 1 year of revision surgery, a finding comparable to other primary CPS implant studies [10, 13, 19, 24]. Few publications have described the outcomes of revision distal femoral prostheses (Table 2). In 1991, Unwin et al. [28] reported a dismal 19% 5-year survival of revision distal femoral prostheses. His followup study in 1995 found a 45% 5-year survival in 83 patients with prostheses of various anatomic locations [29]. Wirganowicz et al. [33] described a 34% failure rate at 5 years among 48 patients requiring prosthetic revision of any anatomic location. Among the 32 revision knee prosthesis patients described by Morgan et al. [20], 56% failed at 10 years. In a review of modern knee prostheses, Pala et al. [23] calculated a 19% rate of failure among 72 revision patients with a mean followup of less than 4 years. These high failure rates not only reflect the difficulty in achieving long-term survival of a revised distal femoral endoprosthesis, but offer a notable contrast to the lower failure rate we observed in our patients who received the CPS implant. Further studies with more patients and direct comparison are necessary to confirm this impression.
The three patients who sustained early mechanical failure of their revision CPS implants were carefully scrutinized to identify any contributing factors in otherwise healthy patients. We found that all three patients were young and engaging in strenuous activity or not strictly complying with weightbearing restrictions, which may have contributed to the loss of compression before the implant was stable and osteointegrated. Patients are allowed to progress to full weight bearing 3 months postoperatively even though it is too soon to see bone hypertrophy as an indicator of implant stability. Because not all patients who are active sustain mechanical failure of the CPS implant, a definitive causal relationship cannot be established, but we advise caution with all patient activity until hypertrophic bone is observed around the implant spindle. The cumulative incidence of all types of implant failure in our revision patients was 29% at 10 years, representative of the addition of infection as a problem plaguing patients who require multiple operations and revisions. However, this overall rate, encompassing all reasons for performing a revision, is still equal or better than previously published revision studies [20, 23, 26, 28, 29, 33].
A unique complication we encountered when using the CPS implant as a revision construct occurred in our three patients who sustained impending or complete femoral fractures proximal to the anchor plug. Tyler et al. [27] described periprosthetic fractures around six of 154 distal femoral CPS implants. Five of those fractures were in a similar location, proximal to the anchor plug, and were treated with strut grafting and internal fixation. In managing our revision patients, we naively assumed that it was acceptable to use a CPS implant when there was adequate cortical bone at the cut interface. This was necessary but not sufficient. Experience showed that it was essential to have ample cortical bone proximal to the anchor plug intrinsically or by augmenting the femur with bone grafts. Shortly after this complication was observed, we began routinely ordering preoperative CT scans for patients requiring revision to identify cortical bone at risk for fracture and plan for intraoperative bone grafting. We have not placed any cortical strut grafts since then nor have we observed any postoperative fractures in any of our revision patients, so we cannot yet comment on the influence of a preoperative CT in preventing this complication. In our series, strut allografts for the impending fracture and strut allografts with osteosynthesis plates for completed fractures (Figs. 4, 5) treated the problem without sacrificing the prosthesis but required a second operation. Careful scrutiny of the entire host bone for possible sites of weakness could have prevented secondary surgery in this series. An alternative strategy would have been to resect the attenuated bone proximal to the prior prosthetic stem tip. However, this would have required loss of an additional 10 to 15 cm of femoral shaft and would have left insufficient bone for reconstruction in two of our three fracture cases; thus, we believed this to be excessive.
Functional results in this series of revision patients were similar to those reported after primary distal femur prosthetic reconstructions [4, 14–16, 18, 21, 22] and better than those reported in the limited number of revision megaprosthesis studies published to date. Pala et al. [23] reported a mean MSTS score of 24 in all revision patients, but this included all anatomic locations so a direct comparison is not possible. Eighty-one percent of our revision patients had a 90° arc of motion, but ROM is frequently unreported in studies of primary or revision CPS implants, so a comparison is not possible. No statistically significant correlation could be made between ROM and MSTS score in our patient group. Admittedly, the MSTS score has limitations in that it is a subjective assessment in which five of six parameters are evaluated by the healthcare provider rather than the patient.
This study indicates that using CPS implant technology is a reasonable option to consider when revising failed endoprostheses used for tumor reconstruction of the distal femur. However, we did not examine whether the survival and functional outcomes of the CPS prosthesis are superior to other means of reconstruction reported in the literature. A larger study with a direct comparison group is needed to answer that question definitively. For patients in whom the remaining femur is too short to accept a conventional stem (120–150 mm), the Compress® may be considered as an alternative to an APC or total femur replacement, and future studies comparing those therapeutic alternatives will be beneficial. We learned that meticulous attention to the quality of the bone proximal to the anchor plug is imperative before, during, and after revision surgery to avoid unnecessary complications.
Footnotes
The Department of Epidemiology and Biostatistics at Memorial Sloan Kettering Cancer Center is partially supported by a Cancer Center Support Grant from the National Institutes of Health/National Cancer Institute (# P30 CA008748) (ERR). The Major Family Philanthropic Fund provided financial support of the Orthopaedic Fellowship Program at Memorial Sloan Kettering Cancer Center (MNZ).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Memorial Sloan Kettering Cancer Center, New York, NY, USA.
References
- 1.Ahlmann ER, Menendez LR, Kermani C, Gotha H. Survivorship and clinical outcome of modular endoprosthetic reconstruction for neoplastic disease of the lower limb. J Bone Joint Surg Br. 2006;88:790–795. doi: 10.1302/0301-620X.88B6.17519. [DOI] [PubMed] [Google Scholar]
- 2.Avedian RS, Goldsby RE, Kramer MJ, O’Donnell RJ. Effect of chemotherapy on initial compressive osseointegration of tumor endoprostheses. Clin Orthop Relat Res. 2007;459:48–53. doi: 10.1097/BLO.0b013e3180514c66. [DOI] [PubMed] [Google Scholar]
- 3.Bhangu AA, Kramer MJ, Grimer RJ, O’Donnell RJ. Early distal femoral endoprosthetic survival: cemented stems versus the compress implant. Int Orthop. 2006;30:465–472. doi: 10.1007/s00264-006-0186-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biau D, Faure F, Katsahian S, Jeanrot C, Tomeno B, Anract P. Survival of total knee replacement with a megaprosthesis after bone tumor resection. J Bone Joint Surg Am. 2006;88:1285–1293. doi: 10.2106/JBJS.E.00553. [DOI] [PubMed] [Google Scholar]
- 5.Bini SA, Johnston JO, Martin DL. Compliant prestress fixation in tumor prostheses: interface retrieval data. Orthopedics. 2000;23:707–712. doi: 10.3928/0147-7447-20000701-18. [DOI] [PubMed] [Google Scholar]
- 6.Cipriano CA, Gruzinova IS, Frank RM, Gitelis S, Virkus WW. Frequent complications and severe bone loss associated with the repiphysis expandable distal femoral prosthesis. Clin Orthop Relat Res. 2015;473:831–838. doi: 10.1007/s11999-014-3564-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clarke HD, Berry DJ, Sim FH. Salvage of failed femoral megaprostheses with allograft prosthesis composites. Clin Orthop Relat Res. 1998;356:222–229. doi: 10.1097/00003086-199811000-00030. [DOI] [PubMed] [Google Scholar]
- 8.Cristofolini L, Bini S, Toni A. In vitro testing of a novel limb salvage prosthesis for the distal femur. Clin Biomech. 1998;13:608–615. doi: 10.1016/S0268-0033(98)00024-2. [DOI] [PubMed] [Google Scholar]
- 9.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246. [PubMed] [Google Scholar]
- 10.Farfalli GL, Boland PJ, Morris CD, Athanasian EA, Healey JH. Early equivalence of uncemented press-fit and compress femoral fixation. Clin Orthop Relat Res. 2009;467:2792–2799. doi: 10.1007/s11999-009-0912-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Griffin AM, Parsons JA, Davis AM, Bell RS, Wunder JS. Uncemented tumor endoprostheses at the knee: root causes of failure. Clin Orthop Relat Res. 2005;438:71–79. doi: 10.1097/01.blo.0000180050.27961.8a. [DOI] [PubMed] [Google Scholar]
- 12.Healey JH, Abdeen A, Morris CD, Athanasian EA, Boland PJ. Telescope allograft method to reconstitute the diaphysis in limb salvage surgery. Clin Orthop Relat Res. 2009;467:1813–1819. doi: 10.1007/s11999-008-0548-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Healey JH, Morris CD, Athanasian EA, Boland PJ. Compress knee arthroplasty has 80% 10-year survivorship and novel forms of bone failure. Clin Orthop Relat Res. 2013;471:774–783. doi: 10.1007/s11999-012-2635-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horowitz SM, Glasser DB, Lane JM, Healey JH. Prosthetic and extremity survivorship after limb salvage for sarcoma. How long do the reconstructions last? Clin Orthop Relat Res. 1993;293:280–286. [PubMed] [Google Scholar]
- 15.Kawai A, Muschler GF, Lane JM, Otis JC, Healey JH. Prosthetic knee replacement after resection of a malignant tumor of the distal part of the femur. Medium to long-term results. J Bone Joint Surg Am. 1998;80:636–647. doi: 10.1302/0301-620X.80B4.8216. [DOI] [PubMed] [Google Scholar]
- 16.Kinkel S, Lehner B, Kleinhans JA, Jakubowitz E, Ewerbeck V, Heisel C. Medium to long-term results after reconstruction of bone defects at the knee with tumor endoprostheses. J Surg Oncol. 2010;101:166–169. doi: 10.1002/jso.21441. [DOI] [PubMed] [Google Scholar]
- 17.Kramer MJ, Tanner BJ, Horvai AE, O’Donnell RJ. Compressive osseointegration promotes viable bone at the endoprosthetic interface: retrieval study of compress implants. Int Orthop. 2008;32:567–571. doi: 10.1007/s00264-007-0392-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mittermayer F, Krepler P, Dominkus M, Schwameis E, Sluga M, Heinzl H, Kotz R. Long-term followup of uncemented tumor endoprostheses for the lower extremity. Clin Orthop Relat Res. 2001;388:167–177. doi: 10.1097/00003086-200107000-00024. [DOI] [PubMed] [Google Scholar]
- 19.Monument MJ, Bernthal NM, Bowles AJ, Jones KB, Randall RL. What are the 5-year survivorship outcomes of compressive endoprosthetic osseointegration fixation of the femur? Clin Orthop Relat Res. 2015;473:883–890. doi: 10.1007/s11999-014-3724-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morgan HD, Cizik AM, Leopold SS, Hawkins DS, Conrad EU., 3rd Survival of tumor megaprostheses replacements about the knee. Clin Orthop Relat Res. 2006;450:39–45. doi: 10.1097/01.blo.0000229330.14029.0d. [DOI] [PubMed] [Google Scholar]
- 21.Myers GJ, Abudu AT, Carter SR, Tillman RM, Grimer RJ. Endoprosthetic replacement of the distal femur for bone tumours: long-term results. J Bone Joint Surg Br. 2007;89:521–526. doi: 10.1302/0301-620X.89B4.18631. [DOI] [PubMed] [Google Scholar]
- 22.Pala E, Henderson ER, Calabro T, Angelini A, Abati CN, Trovarelli G, Ruggieri P. Survival of current production tumor endoprostheses: complications, functional results, and a comparative statistical analysis. J Surg Oncol. 2013;108:403–408. doi: 10.1002/jso.23414. [DOI] [PubMed] [Google Scholar]
- 23.Pala E, Trovarelli G, Calabro T, Angelini A, Abati CN, Ruggieri P. Survival of modern knee tumor megaprostheses: failures, functional results, and a comparative statistical analysis. Clin Orthop Relat Res. 2015;473:891–899. doi: 10.1007/s11999-014-3699-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pedtke AC, Wustrack RL, Fang AS, Grimer RJ, O’Donnell RJ. Aseptic failure: how does the Compress® implant compare to cemented stems? Clin Orthop Relat Res. 2012;470:735–742. doi: 10.1007/s11999-011-2159-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schuh R, Kaider A, Windhager R, Funovics PT. Does competing risk analysis give useful information about endoprosthetic survival in extremity osteosarcoma? Clin Orthop Relat Res. 2015;473:900–906. doi: 10.1007/s11999-014-3703-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shin DS, Weber KL, Chao EY, An KN, Sim FH. Reoperation for failed prosthetic replacement used for limb salvage. Clin Orthop Relat Res. 1999;358:53–63. [PubMed] [Google Scholar]
- 27.Tyler WK, Healey JH, Morris CD, Boland PJ, O’Donnell RJ. Compress periprosthetic fractures: interface stability and ease of revision. Clin Orthop Relat Res. 2009;467:2800–2806. doi: 10.1007/s11999-009-0946-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Unwin PS, Blunn G, Cobb JP, Walker PS. How successful are revisions of massive prostheses? In: Brown KLB, ed. Complications of Limb Salvage: Prevention, Management and Outcome. Sixth International Symposium. Montreal, Canada: ISOLS; 1991:183–187.
- 29.Unwin PS, Blunn G, Walker PS. Lower limb revision of failed bone tumor endoprosthesis: a survivorship study. J Bone Joint Surg Br. 1995;77(Suppl I):87. [Google Scholar]
- 30.Unwin PS, Cannon SR, Grimer RJ, Kemp HB, Sneath RS, Walker PS. Aseptic loosening in cemented custom-made prosthetic replacements for bone tumours of the lower limb. J Bone Joint Surg Br. 1996;78:5–13. [PubMed] [Google Scholar]
- 31.Unwin PS, Cobb JP, Walker PS. Distal femoral arthroplasty using custom-made prostheses. The first 218 cases. J Arthroplasty. 1993;8:259–268. doi: 10.1016/S0883-5403(06)80087-2. [DOI] [PubMed] [Google Scholar]
- 32.Wilkins RM, Kelly CM. Revision of the failed distal femoral replacement to allograft prosthetic composite. Clin Orthop Relat Res. 2002;397:114–118. doi: 10.1097/00003086-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 33.Wirganowicz PZ, Eckardt JJ, Dorey FJ, Eilber FR, Kabo JM. Etiology and results of tumor endoprosthesis revision surgery in 64 patients. Clin Orthop Relat Res. 1999;358:64–74. [PubMed] [Google Scholar]
- 34.Zimel MN, Cizik AM, Rapp TB, Weisstein JS, Conrad EU., 3rd Megaprosthesis versus condyle-sparing intercalary allograft: distal femoral sarcoma. Clin Orthop Relat Res. 2009;467:2813–2824. doi: 10.1007/s11999-009-1024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]