Abstract
Background
Oxidized regenerated cellulose polymer (ORCP) may be used for reshaping and filling lack of volume in breast-conserving surgery (BCS). The study aimed to observe both the aesthetic and diagnostic outcomes in patients with different age, BMI, breast volume, and breast tissue composition over 36 months after BCS with ORCP.
Patients and methods
18 patients with early breast cancer and with proliferative benign lesions underwent BCS with ORCP that was layered in three-dimensional wafer, and placed into the Chassaignac space between the mammary gland and the fascia of pectoralis major with no fixation. After surgery, patients started a clinical and instrumental 36-month follow-up with mammography, ultrasonography, magnetic resonance imaging (MRI) and cytological examination with fine needle aspiration when seroma occurred.
Results
Below the median age of 66 years old no complications were observed even in case both of overweight, and large breasts with low density. Over the median age seromas occurred with either small or large skin retraction, with the exception of 1 patient having quite dense breasts and low BMI, which had no complications. In elderly patients, 1 case with quite dense breasts and high BMI showed severe seroma and skin retraction, while 1 case with low BMI and less dense breasts highlighted milder complications.
Conclusion
During 36 months after BCS with ORCP, a significant correlation between positive diagnostic and aesthetic outcomes and low age, dense breasts, and low BMI of patient was observed. Despite of the few number of cases, either low BMI, or high breast density improved the aesthetic outcomes and reduced the entity of complications even in the elderly patients.
Keywords: Breast cancer, Breast-conserving surgery, Oncoplastic breast surgery, Oxidized regenerated cellulose polymer
Abbreviations: BCS, breast-conserving surgery; OBS, oncoplastic breast surgery; ORCP, oxidized regenerated cellulose polymer
Highlights
-
•
The oncoplastic breast surgery (OBS) joins tumor excision with reconstruction techniques.
-
•
The oxidized regenerated cellulose polymer is a filler to support volume and shape.
-
•
18 patients with T1-T2 breast cancer and proliferative benign lesion were selected.
-
•
Complications occurred within 36-month after OBS in elderly patients with fatty breasts.
-
•
Aesthetic outcomes improved with lower age, higher dense breasts and lower BMI.
1. Introduction
In the last few years, breast surgeons have learned a new discipline for breast cancer treatment: oncoplastic breast surgery (OBS) [1]. Breast and plastic surgeons often work together to ensure a radical surgery and achieve the best possible cosmetic result, including acceptable breast symmetry [2]. Breast-conserving surgery (BCS) could provide better aesthetic results when compared to mastectomy. It has become the mainstream surgery for early breast cancer [1], [2]. If less than 20% of the breast volume is excised, a level I procedure is adequate and a breast surgeon who lacks specific training in plastic surgery can carry it out; excisions that exceed 20–50% of the breast volume require a level II procedure that is based on mammoplasty techniques and specific training [3]. OBS requires preoperative planning according to the volume of the breast and location of the tumour for proper reduction, displacement, and replacement technique to fill the breast deformation. Breast reshaping absorbs the volume loss and decreases the risk of localized defects, although some zones have a high risk of deformity and cosmetic failure [4]. There is a wide spectrum of reconstructive options, allowing patients and surgeons to choose the best reconstruction technique [5]. Usually, reconstruction after oncological resection can be performed with expanders and implants or autologous grafts (fat or muscle) to correct volume and shape defects [6].
The oxidized regenerated cellulose polymer (ORCP) has been used in recent years to fill resection defects, to adjust the shape, the volume and the symmetry of the breast and to prevent the skin retraction. The ORCP is a haemostatic agent with bactericidal effects against aerobic and anaerobic bacteria due to its acidic pH, and it acts as a scaffold for fibrin deposition, creating a three-dimensional structure as a permanent filler [7]. This haemostatic agent may be peeled off in the desired amount, facilitating placement of the customized pieces under both the gland and skin.
Despite of its role in promoting dermal fibroblast proliferation and cell migration [8], [9], [10], it is not yet established whether the use of ORCP can be extended to all types of breast [11]. To address this gap in knowledge, a 36-month follow-up was set up in order to evaluate which factors related to patients (age, BMI, breast volume and breast density) could either improve or worsen the diagnostic and aesthetic outcomes from the use of the ORCP in BCS.
2. Materials and methods
2.1. Study design and setting
From January 2012 to May 2013, 18 women underwent BCS with ORCP at the Department of General Surgery of the “San Giacomo” Hospital in Novi Ligure (Italy) with hospitalization in day hospital and hospital discharge after 24 h from BCS.
All the 18 patients started a clinical and instrumental 36-month follow-up with mammography, ultrasonography, magnetic resonance imaging (MRI) and cytological examination with fine needle aspiration when seroma occurred. Postoperative adjuvant therapy and follow-up were carried out according to the Breast Cancer Follow-Up and Management Guidelines [12].
2.2. Eligibility criteria of the patients
The social and physical criteria of patient selection were as follows: a) sufficient hygiene and the ability to match pre and postoperative prescriptions; b) possessing a telephone and having the support of a responsible caretaker at home; c) age under 90.
2.3. Exclusion criteria of the patients
The exclusion criteria for patient selection were as follows: a) absence of morbid obesity i.e., BMI >40, or pathologic thinness i.e., BMI <18.7; b) absence of a history of addiction to alcohol, drug or tobacco; c) absence of suffering from skin disease, rheumatic disease or metabolic disease, such as diabetes.
2.4. Oncological criteria of the patients
Oncological criteria were evaluated by mammography, ultrasonography, core biopsy, and histological diagnosis and were as follows: proliferative benign breast lesions and T1-T2 breast cancer with low-medium probability of a positive lymph-node.
2.5. Patient characteristics
The 18 patients who met the inclusion criteria were female with age, provenience, BMI, breast volume, and breast tissue composition class according to BiRADS classification [13] as detailed in Table 1. Interquartile range for age corresponded to: minimum value of 33 years old; 1st quartile of 44 years old; median of 66 years old; 3rd quartile of 74.5 years old; maximum value of 88 years old. With regards to breast volume of the patients, classification was done using cup size as follows: >350 cm3 (large breasts); 250–300 cm3 (medium breasts), <250 cm3 (small breasts).
Table 1.
Demographics, BMI, breast volumea, and BiRADS breast tissue composition class [13] for patients who underwent BCS with ORCP.
| Patient | Age | Provenience | BMI | Breast volume (cm3) | BiRADS class |
|---|---|---|---|---|---|
| 1 | 33 | North Italy | 20 | 200 | 4 |
| 2 | 37 | North Italy | 22 | 300 | 3 |
| 3 | 38 | North Italy | 20 | 250 | 3 |
| 4 | 39 | Romania | 21 | 300 | 3 |
| 5 | 44 | North Italy | 20 | 250 | 3 |
| 6 | 44 | China | 19 | 300 | 4 |
| 7 | 45 | North Italy | 22 | 200 | 3 |
| 8 | 60 | North Italy | 29 | 350 | 2 |
| 9 | 63 | North Italy | 29 | 400 | 2 |
| 10 | 69 | North Italy | 25 | 300 | 2 |
| 11 | 70 | North Italy | 29 | 350 | 2 |
| 12 | 71 | North Italy | 32 | 500 | 1 |
| 13 | 73 | North Italy | 33 | 500 | 1 |
| 14 | 75 | North Italy | 31 | 500 | 1 |
| 15 | 76 | South Italy | 21 | 300 | 3 |
| 16 | 76 | South Italy | 30 | 300 | 3 |
| 17 | 87 | North Italy | 20 | 200 | 1 |
| 18 | 88 | North Italy | 26 | 300 | 1 |
Cup size was used for breast volume measurement.
2.6. Patient assessment
A preliminary visit was scheduled, where the surgeon selected the patient for the one-day surgical procedure based on the previously mentioned inclusion criteria. Written informed consent was obtained from the patient for the involvement in this study, for the storage and use of data, and for the publication of this report and any accompanying images. Moreover, a detailed information sheet was then provided, which also included telephone numbers of the ward. Preoperative exams (chest X-ray, electrocardiography, blood sample) were coordinated by nurses and performed in a prepared ambulatory setting.
The day before the surgical intervention the patient was invited to undergo a psychological counselling session to assess her expectations and the impact of her outpatient treatment. The same day the patient was taken to the Department of General Surgery for mapping with ultrasonography the tumour localization.
On the day of the surgery the patient arrived after fasting for at least 6 h. The evening before she was advised to take a bath or shower after accurate self-epilation of the axilla. Postoperative observation was for at least 5 h, after which both the surgeon and the anaesthesiologist evaluated the patient.
The patient was discharged the day after the surgery, and should any complications arise the surgeon then promptly extended the admission of the patient to the hospital. Fifteen days after the surgery, the patient was invited to the Department of General Surgery to change the dressing.
2.7. Breast-conserving surgery (BCS)
Surgical intervention was performed following standard techniques. The negative margins of the excision cavity were confirmed by intraoperative pathological examination.
T1-T2 breast cancer with an average node size of 19 mm (range 8–34 mm) affected 14 patients, while proliferative benign lesions interested 4 patients. The patients with T1-T2 breast cancer underwent an oncological wide excision or quadrantectomy [14] as detailed in Table 2, with sentinel lymph node biopsy and axillary lymph node dissection if positive nodes were confirmed for tumour metastasis. Patients with proliferative benign breast lesions received an adequate volume excision, which is in agreement with the previous histological diagnosis by core biopsy. The average weight of the surgical specimens was 72.6 g (range 32–120 g) for large breasts, 51.2 g (range 25–88 g) for medium breasts, and 30.5 g (range 18–50 g) for small breasts, respectively.
Table 2.
Distribution of breast volume and breast density, histology and location of lesions, and of amount of ORCP among the 18 patients who underwent BCS with ORCP.
| Breast volumea | |
| Small | 27.7% |
| Medium | 38.9% |
| Large | 33.3% |
| Breast density (BiRADS class)[13] | |
| 1 | 27.7% |
| 2 | 22.2% |
| 3 | 38.9% |
| 4 | 11.1% |
| Lesion histology | |
| Benign | 22.2% |
| Malignant | 77.7% |
| Location of lesionsb | |
| Q1 | 44.4% |
| Q1 – Q2 | 22.2% |
| Q2 | 11.1% |
| Q3 | 11.1% |
| Q5 | 5.55% |
| Q3-Q4 | 5.55% |
| ORCP used for BCS | |
| Half of 1 piece | 5.55% |
| Single piece | 83.3% |
| Two pieces | 11.1% |
Breast size classification was done using cup size as follows: large breasts (>350 cm3); medium breasts (250–300 cm3), small breasts (<250 cm3).
Quadrant per quadrant Atlas (orientation for left breast) has been intended as follows [14]: Q1 = upper outer quadrant 1–2 o'clock; Q2 = upper inner quadrant 9–11 o'clock; Q3 = lower outer quadrant 4–5 o'clock; Q4 = lower inner quadrant 7–8 o'clock; Q5 = central subareolar with NAC resection; Q1–Q2 = upper pole 12 o'clock; Q3–Q4 = lower pole 5–7 o'clock.
The patients underwent BCS involving correction of the shape and volume replacement by an ORCP (Tabotamp fibrillar®, Johnson & Johnson; Ethicon, New Brunswick, NJ, USA). The ORCP was layered in three-dimensional wafer, and placed into the Chassaignac space between the mammary gland and the fascia of pectoralis major with no fixation. This hemostatic agent may be peeled off in standard piece size (5 × 7.5 cm). It was placed as follows: 2 pieces in patient n.15 and n.16; half of 1 piece for a central quadrantectomy in subareolar space for the patient n.6; 1 piece for the remaining 15 patients who underwent standard quadrantectomy.
All cases with breast cancer underwent radiation therapy for the whole breast starting from 1 month after BCS, 3 patients (n.4, n.10, and n.15) were submitted to chemotherapy. No neo-adjuvant treatment has been provided to the patients.
All the 18 patients started a clinical and instrumental 36-month follow-up mainly addressed to evaluate the aesthetic outcome of the surgery, the type, frequency, and magnitude of complications. The timing of follow up was focused on the absorption of oxidized regenerated cellulose and on its possible interference with radiological studies. It was monthly for the first 6 months, then 6 monthly for 2 years, and then one more annual follow-up.
2.8. Statistical analysis
The data from patients (age, BMI, breast volume and breast density), considered as numerical variables, and the data from complication and aesthetic outcomes, considered as ranked variables, were processed by a two-tailed bivariate correlation Pearson's test. The statistics were performed in software SPSS Statistics 21 (IBM Corp., Armonk, NY).
3. Results
The complications that could be observed in either large and fatty or small and glandular breasts after the implantation of an ORCP were evaluated by mammography, ultrasonography, and magnetic resonance imaging (MRI). The occurrence of seroma was clinically detected and then confirmed by ultrasonography; moreover, cytological examination with fine needle aspiration was performed.
Surgeon and patient considered as positive the following aesthetic outcomes: recovery of symmetry, volume replacement, no skin retraction, and no NAC dislocation which showed, as expected, significant correlations among themselves (Table 4).
Table 4.
Pearson's correlation coefficients for age, BMI, breast volume, breast density, seroma occurrence, skin retraction, recovery of symmetry, and NAC dislocation observed in the 18 patients within 36 months after BCS with ORCP.
| BMI | Breast volume | Breast density | Seroma | Skin retraction | Recovery of symmetry | NAC dislocation | |
|---|---|---|---|---|---|---|---|
| Age | 0.56* | n.s. | −0.78** | 0.79** | 0.68** | n.s. | n.s. |
| BMI | 0.84** | −0.67** | 0.62** | 0.67** | −0.54* | 0.54* | |
| Breast volume | −0.61** | n.s. | n.s. | n.s. | n.s. | ||
| Breast density | −0.75** | −0.56* | n.s. | n.s. | |||
| Seroma | 0.90** | −0.50* | 0.50* | ||||
| Skin retraction | −0.82** | 0.82** | |||||
| Recovery of symmetry | 0.99** |
n.s. = Not significant correlation.
* = Significant correlation at p ≤ 0.05.
** = Significant correlation at p ≤ 0.01.
3.1. Complications observed within 36 months from BCS with ORCP
Seroma complication and skin retraction correlated with older age, higher BMI, and lower density breasts; lost of symmetry and NAC dislocation were significantly related to higher BMI values (Table 4).
With the exception of the case n.15 (Table 3), the seroma appeared in all the older patients with low-density breast in the first 3 months after surgery (Fig. 1 A and B). At this moment, MRI showed in 1 patient thickening of the dermis and hypodermis, lymphatic duct dilatation, and fluid collection (Fig. 1C). After 6 months, ultrasonography highlighted an anechoic fluid collection due to the presence of fibrillary material (Fig. 2A). Fine needle aspiration showed whitish fluid and small pieces (Fig. 2B), which were negative at microbiological study (Fig. 2C). After 8 months, scar retraction after episode of mastitis with seroma appeared in 2 patients (Fig. 3A). In such patients, the recurrent mastitis was characterized at 1 year from BCS by erythematous and oedematous aspect of the whole breast with “orange peel” skin without changes in the temperature (Fig. 3B). Finally, at 36 months from BCS, fluid collection with typical hyperechoic and lobular masses inside without any vascular signals were detected (Fig. 4). The patients with complications gradually improved with the use of 40 mg of oral bromelain twice a day for 7 days, and with repeated aspirations of the collected fluids.
Table 3.
Complications and aesthetic outcomes observed in patients within the 36 months from BCS with ORCP.
| Patient | Seroma | Skin retraction | Volume replacement | Symmetry | NAC dislocation |
|---|---|---|---|---|---|
| 1 | No | No | Yes | Yes | No |
| 2 | No | No | Yes | Yes | No |
| 3 | No | No | Yes | Yes | No |
| 4 | No | No | Yes | Yes | No |
| 5 | No | No | Yes | Yes | No |
| 6 | No | No | Yes | Yes | No |
| 7 | No | No | Yes | Yes | No |
| 8 | No | No | Yes | Yes | No |
| 9 | No | No | Yes | Yes | No |
| 10 | Yes | Small | Yes | Yes | No |
| 11 | Yes | Large | Yes | No | Yes |
| 12 | Yes | Small | Yes | Yes | No |
| 13 | Yes | Large | Yes | No | Yes |
| 14 | Yes | Small | Yes | Yes | No |
| 15 | No | No | Yes | Yes | No |
| 16 | Yes | Large | Yes | No | Yes |
| 17 | Yes | Small | Yes | Yes | No |
| 18 | Yes | Small | Yes | Yes | No |
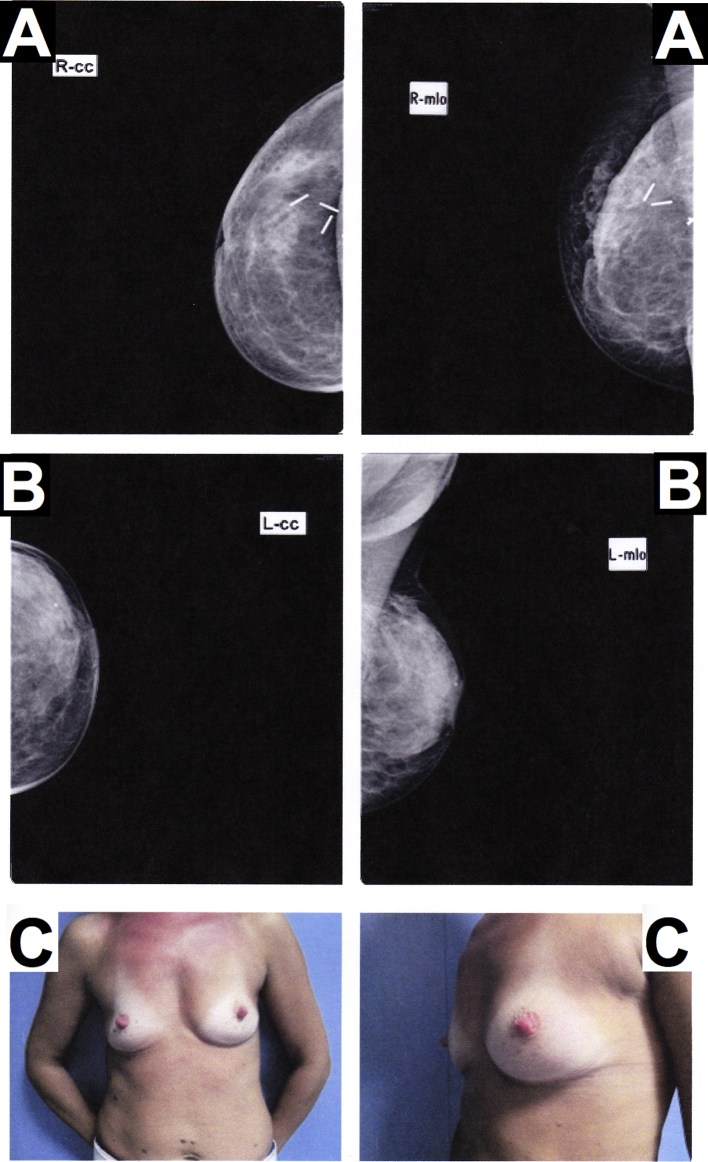
Fig. 1.
Complications observed in patients over the median age (66 years old) with low-dense breasts within the first 3 months from BCS with ORCP. (A) Breast seroma at 1 month. (B) Breast seroma at 3 months. (C) Scarring and thickening of the dermis and hypodermis as result of a postoperative seroma detected with MRI at 3 months.
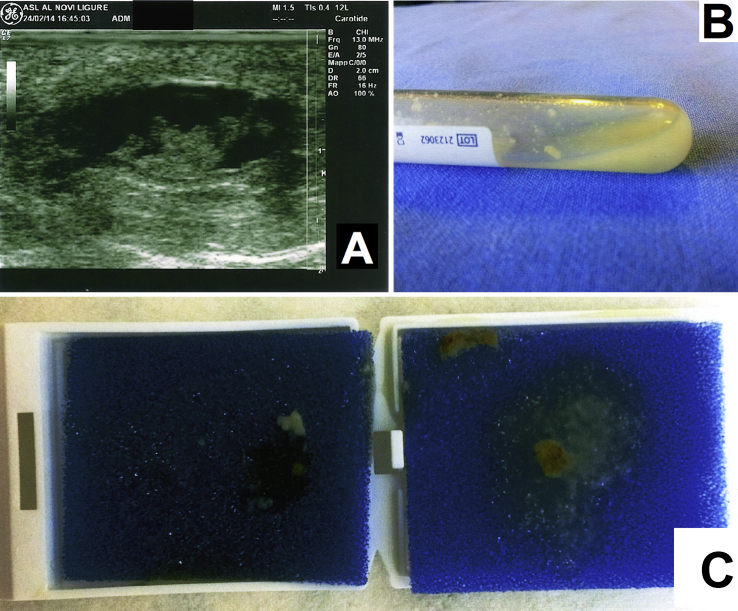
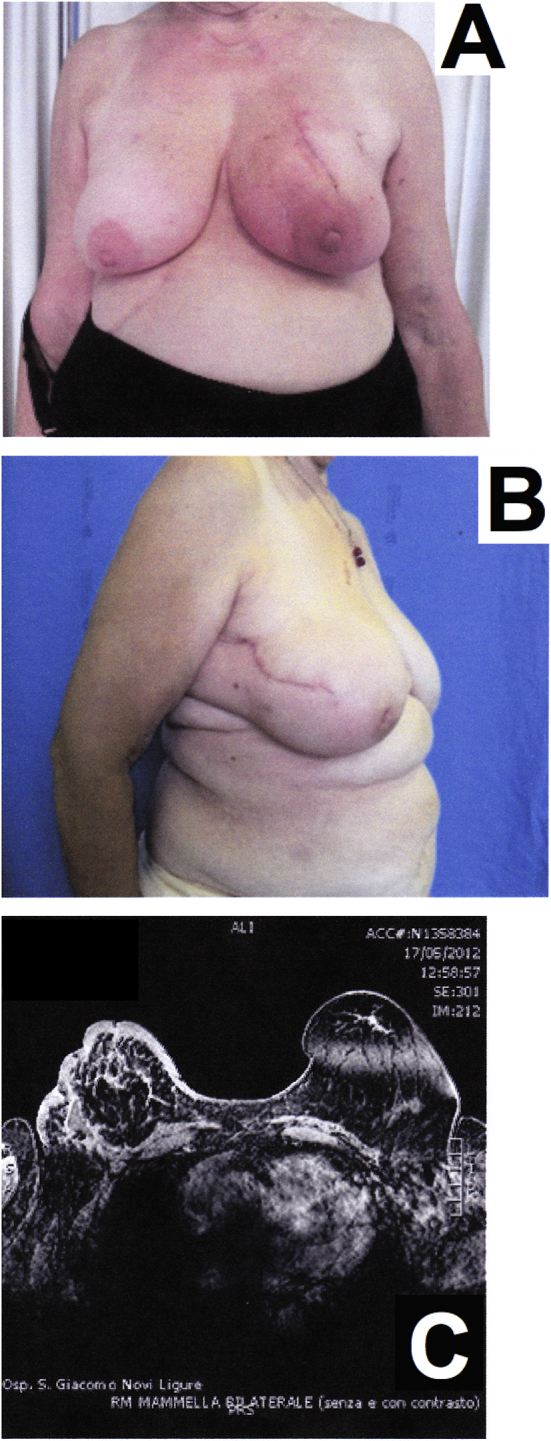
Fig. 2.
Complications observed in patients over the median age (66 years old) with low-dense breasts at 6 months from BCS with ORCP. (A) Anaechoic fluid collection with the presence of a small hyperechoic lobular mass detected with ultrasonography. (B) Fine needle aspiration of the fluid collection. (C) Microbiological test carried out on small pieces of fibrillary biomaterial detected in the fluid collection.
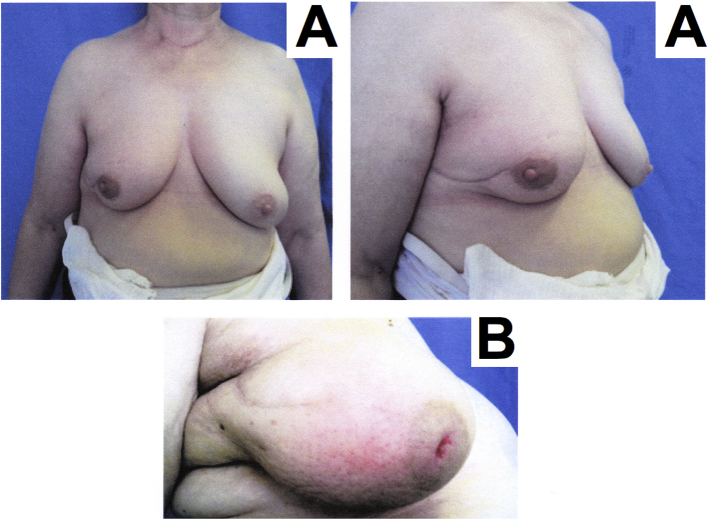
Fig. 3.
Complications observed in patients over the median age (66 years old) with low-dense breasts from 8 months to 1 year after BCS with ORCP. (A) Scar retraction as a result of a postoperative seroma at 8 months. (B) Breast pain in the absence of fever observed 1 year after BCS.
Fig. 4.
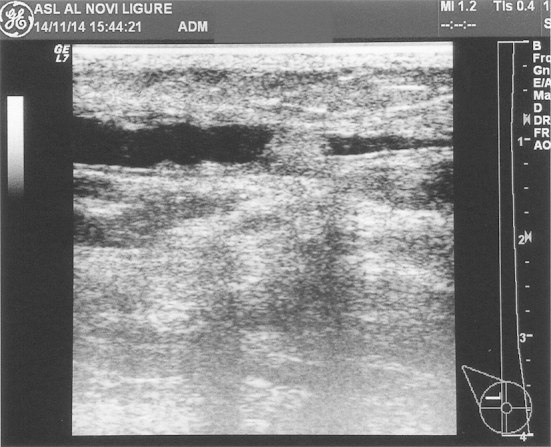
Fluid collection with typical hyperechoic and round lobular mass without any vascular signals observed in low-dense breasts in patients over the median age (66 years old) with ultrasonography at 36 months from BCS with ORCP.
3.2. Aesthetic outcomes observed within 36 months from BCS with ORCP
As detailed in Table 3, the filling of the volume lost by surgical resection was fully recovered with the use of an ORCP in each of the patient here considered i.e., irrespective of age, BMI, and breast density. Recovery of symmetry and NAC dislocation were significantly correlated to patient BMI (Table 4).
In detail, no complication was observed in 9 patients aged below the median (66 years old) with either small or medium breast volume. In these cases, breast symmetry was recovered; both no skin retraction and NAC dislocation were observed (Table 3). Even in the elderly patients (>66 years old), 1 case presenting low BMI and quite dense breast did not showed any complication and gained good aesthetic outcomes (Fig. 5).
Fig. 5.

Outcomes of the BCS with ORCP in patient n.15 at 36-month follow-up.
Although the correlations showed that complication diminished, and aesthetic outcomes improved when BMI lowered and breast density increased (Table 4), 2 young patients with high BMI and a low-density breast tissue showed no complications with good recovery of the symmetry, no skin retraction and no NAC dislocation. Thus confirmed the age as a significant factor in determining positive outcomes from the use of ORCP.
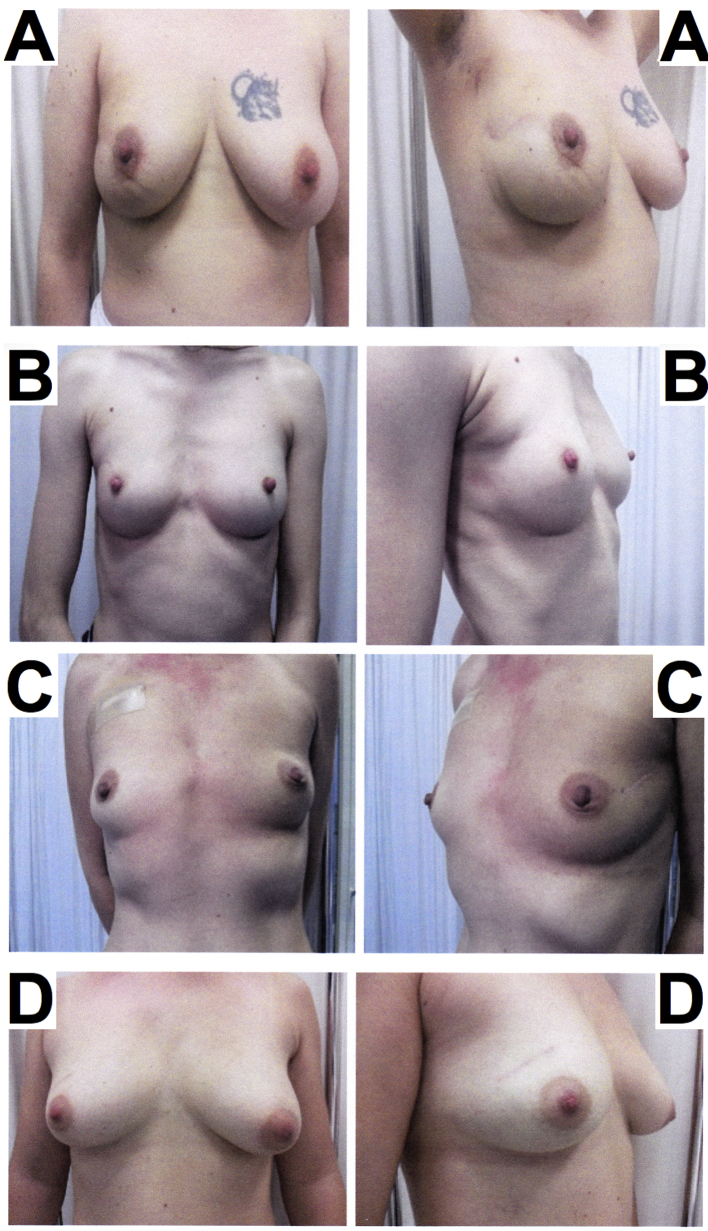
Diagnostic results outlined after 1 month from surgery, the complete absorption of ORCP in breasts (Fig. 6A): the ORCP mass was enclosed in a fibroblastic wall and completely absorbed after 45 days (Fig. 6B). After 6-month from BCS, both patients with breast cancer who underwent radiation therapy and patients with proliferative benign breast lesions showed a good breast reshaping by means of the ORCP with filling of the resection defects, recovery of the breast symmetry and no skin retraction (Fig. 7). Stable diagnostic and cosmetic outcomes were detected -both after 1 year (Fig. 8A) and after 36 months from BCS (Fig. 8 B and C).
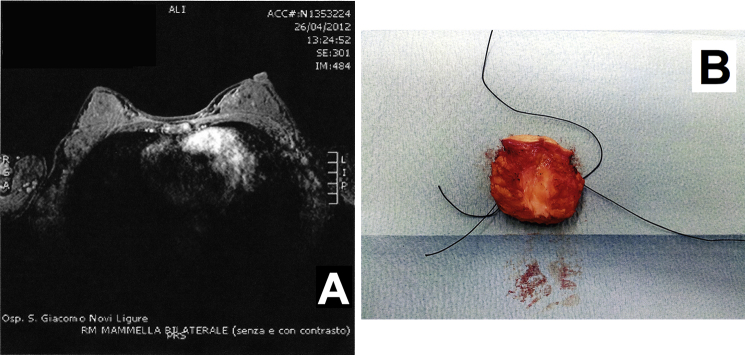
Fig. 6.
Outcomes of the BCS with ORCP in patients below the median age (66 years old) with dense glandular breasts. Complete adsorption of ORCP: (A) at 1 month in left breast observed with MRI and (B) after 45 day from the site of the implant.
Fig. 7.
Outcomes of the BCS with ORCP in patients below the median age (66 years old) with dense glandular breasts at 6 months after surgery with (A, B, C) and without (D) radiation.
Fig. 8.
Mammographic imaging (A, B) and outcomes (C) of the BCS with ORCP in patients below the median age (66 years old) with dense glandular breasts after (A) 1 year and (B, C) 36-month follow-up.
4. Discussion
Recently, breast surgeons have tried to address the lack of volume after surgical resection through the use of an ORCP having a recognized role in promoting dermal fibroblast proliferation and cell migration [8], [9], [10]. ORCP is an haemostatic agent [15], [16] that is commonly applied in many surgical fields, but it was not yet proven whether it can be used for all types of breast [11] as a filler for BCS.
The observed outcomes from this 36-month follow-up on the use of ORCP in BCS stated the efficacy of this biomaterial as filler for breast volume replacement irrespective of the age, the BMI, and the density of the breast tissue (Table 3). Complications were mainly related to the implantation of an ORCP in older patients with high BMI and low-density breasts (Table 3, Fig. 1, Fig. 2, Fig. 3, Fig. 4). In contrast, younger patients with dense glandular breasts and concurrent low BMI, the ORCP was completely absorbed from the site of the implant (Fig. 6), ensuring the shape, the volume and the symmetry of the breast and reducing the skin retraction (Table 3, Fig. 7, Fig. 8).
The breast inflammatory complications reported for large and fatty breasts and associated with the persistence of biomaterial inside fluid collections (Fig. 2, Fig. 4) were already observed in previous studies [8], [9]. These complications allow at excluding diagnostic mistakes due to oxidized cellulose as it was described in instrumental studies with images very similar to a post-surgical abscess, granuloma or local tumour recurrence [17], [18], [19].
The recurrent mastitis that was continuously observed in elderly patients, with either less dense breast or high BMI (Fig. 1, Fig. 3), which can be traced back to chronic inflammation rather than to an allergic reaction, did not find an explanation in the literature. Franceschini only reported a significant rate of seroma in 45% of patients and 10% of inflammatory reactions that were successfully managed with steroids and antihistamine medications [19].
The ORCP forms a gelatinous clot that acts as a scaffold for fibrin deposition and platelet aggregation, aiding surgical haemostasis and creating a three-dimensional structure as a permanent filler [9]. Nevertheless, the exact absorption mechanism of this biomaterial is not yet well understood: macrophagic processing could play a role, together with others factors, including the amount of gauze used, degree of blood saturation and tissue bed [10].
Results from this follow-up study reinforced the assumption that low tissue density, as fat is, limits the surgeon's ability to perform both extensive and effective breast reshaping because of the high risk of fat necrosis [8]. Moreover, this study led to hypothesize that the fat mass, its volume and composition could play a role in the process of absorption of the ORCP. This is corroborated by the results observed in patients, mostly younger and in 1 case older (Fig. 5), having higher glandular density where a complete absorption of ORCP (Fig. 6) and positive aesthetic outcomes occurred (Table 3). Both the patients with breast cancer and with proliferative benign breast lesions obtained satisfactory diagnostic and cosmetic results stable within months (Fig. 7, Fig. 8).
Taking account of the limited number of patients involved in the study, and the evaluation of aesthetic outcomes by the surgeon who further considered the patient satisfaction, a personal proposal for a possible cut-off mark for the successful use of the ORCP in OBS could be the concurrent occurrence or the combination among two of the following factors: young age, breast tissue within the 3rd or 4th BiRADS class, and low BMI.
5. Conclusion
After mammary resection due to both malignant and benign lesions, the results of this follow-up performed within 36 months from the use of ORCP in BCS demonstrated the efficacy of this biomaterial as filler for breast volume replacement irrespective of the age, the BMI, and the density of the breast tissue of the 18 patients under study. The improvement in the breast projection with a satisfactory recovery of symmetry, no skin retraction, and no NAC dislocation, was demonstrated especially for dense breasts in younger patients, while seroma and skin retraction occurred particularly in case of fatty breasts in elderly patients.
Despite of the few number of patients, these results reinforced the previously published literature [8], [9], [19] and pushed toward the choice of another reconstruction technique in BCS in case of patients with fatty breasts. As a correlated factor with age and breast density, a low BMI demonstrated to enhance the aesthetic outcome and to lessen the extent of complication even in the presence of older patients and fatty breasts.
Ethical approval
None approval form Ethical committee.
Written informed consent for this study was obtained from the patients for their involvement in this study, for the storage and use of their data, and for the publication of this report and any accompanying images.
Funding
None.
Author contribution
The corresponding author provided to perform and to write the study in full.
Conflict of interest
None declared.
Guarantor
The corresponding author acts as Guarantor.
References
- 1.Piper M., Peled A.W., Sbitany H. Oncoplastic breast surgery: current strategies. Gland. Surg. 2015;4(2):154–163. doi: 10.3978/j.issn.2227-684X.2015.03.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baildam A., Bishop H., Boland G., Dalglish M., Davies L., Fatah F., Gooch H., Harcourt D., Martin L., Rainsbury D., Rayter Z., Sheppard C., Smith J., Weiler-Mithoff E., Winstanley J., Church J. Association of breast surgery at BASO; association of breast surgery at BAPRAS. Training interface group in breast surgery, oncoplastic breast surgery – a guide to good practice. Eur. J. Surg. Oncol. 2007;33:S1–S23. doi: 10.1016/j.ejso.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Clough K.B., Kaufman G.J., Nos C., Buccimazza I., Sarfati I.M. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann. Surg. Oncol. 2010;17:1375–1391. doi: 10.1245/s10434-009-0792-y. [DOI] [PubMed] [Google Scholar]
- 4.Asgeirsson K.S., Rasheed T., McCulley S.J., Macmillan R.D. Oncological and cosmetic outcomes of oncoplastic breast conserving surgery. EJSO. 2005;31:817–823. doi: 10.1016/j.ejso.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Etienne C.A., Forcellini D., Sagona A., Caviggioli F., Barbieri E., Cornegliani G., Giannasi S., Tinterri C. Breast reconstruction: a quality measure for breast cancer care? Breast. 2012;21(1):105–106. doi: 10.1016/j.breast.2011.08.133. [DOI] [PubMed] [Google Scholar]
- 6.Agha Riaz, Fowler Alexander, Herlin Christian, Goodacre Tim, Orgill Dennis. Use of autologous fat grafting for reconstruction post-mastectomy and breast conserving surgery: a systematic review and meta-analysis. Int. J. Surg. 2014;12:S16. [Google Scholar]
- 7.Spangler D., Rothenburger S., Nguyen K., Jampani H., Weiss S., Bhende S. In vitro antimicrobial activity of oxidized regenerated cellulose against antibiotic-resistant microorganisms. Surg. Infect. 2003;4:255–262. doi: 10.1089/109629603322419599. [DOI] [PubMed] [Google Scholar]
- 8.Franceschini G., Visconti G., Terribile D., Fabbri C., Magno S., Di Leone A., Salgarello M., Masetti R. The role of oxidized regenerate cellulose to prevent cosmetic defects in oncoplastic breast surgery. Eur. Rev. Med. Pharmacol. Sci. 2012;16(7):966–971. [PubMed] [Google Scholar]
- 9.Tanaka S., Sato N., Fujioka H., Takahashi Y., Kimura K., Iwamoto M., Uchiyama K. Breast conserving surgery using volume replacement with oxidized regenerated cellulose: a cosmetic outcome analysis. Breast J. 2014;20(2):154–158. doi: 10.1111/tbj.12229. [DOI] [PubMed] [Google Scholar]
- 10.Rassu P.C., Serventi A., Giaminardi E., Ferrero I., Tava P. Use of oxidized and regenerated cellulose polymer in oncoplastic breast surgery. Ann. Ital. Chir. 2013;84(1):1–5. [PubMed] [Google Scholar]
- 11.Franceschini G., Visconti G., Masetti R. Oncoplastic breast surgery with oxidized regenerated cellulose: appraisals based on five-year experience. Breast J. 2014;20(4):447–448. doi: 10.1111/tbj.12297. [DOI] [PubMed] [Google Scholar]
- 12.Khatcheressian J.L., Wolff A.C., Smith T.J., Grunfeld E., Muss H.B., Vogel V.G., Halberg F., Somerfield M.R., Davidson N.E. American society of clinical oncology 2006. Update of the breast cancer follow-up and management guidelines in the adjuvant setting. J. Clin. Oncol. 2006;24(31) doi: 10.1200/JCO.2006.08.8575. http://www.jco.org/cgi/doi/10.1200/JCO.2006.08.8575 Available at: [DOI] [PubMed] [Google Scholar]
- 13.Percha B., Nassif H., Lipson J., Burnside E., Rubin D. Automatic classification of mammography reports by BI-RADS breast tissue composition class. J. Am. Med. Inf. Assoc. 2012 doi: 10.1136/amiajnl-2011-000607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clough K.B., Kaufman G.J., Nos C., Buccimazza I., Sarfati I.M. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann. Surg. Oncol. 2010 doi: 10.1245/s10434-009-0792-y. [DOI] [PubMed] [Google Scholar]
- 15.Sundaram C.P., Keenan A.C. Evolution of haemostatic agents in surgical practice. Indian J. Urol. 2010;26:374–378. doi: 10.4103/0970-1591.70574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rastogi V., Dy V. Control of port-site bleeding from smaller incisions after laparoscopic cholecystectomy surgery: a new, innovative, and easier technique. Surg. Laparosc. Endosc. Percutan Tech. 2002;12:224–226. doi: 10.1097/00129689-200208000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Young S.T., Paulson E.K., McCann R.L., Baker M.E. Appearance of oxidized cellulose (Surgicel) on postoperative CT scans: similarity to postoperative abscess. AJR Am. J. Roentgenol. 1993;160:275–277. doi: 10.2214/ajr.160.2.8424333. [DOI] [PubMed] [Google Scholar]
- 18.Tam T., Harkins G., Dykes T., Gockley A., Davies M. Oxidized regenerated cellulose resembling vaginal cuff abscess. JSLS. 2014;18(2):353–356. doi: 10.4293/108680813X13693422518597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franceschini G., Visconti G., Masetti R. The use of oxidized regenerated cellulose in oncoplastic breast surgery: “warning” for postoperative follow-up! Ann. Ital. Chir. 2013;84(4):483–484. [PubMed] [Google Scholar]