Abstract
To evaluate the association between a series of retinal information and cardiovascular disease (CVD) and to evaluate whether this association is independent of traditional CVD risk factors in type 2 diabetes patients, we undertook an age-sex matched case-control study with 79 CVD cases and 150 non-CVD controls. All the participants underwent standardized physical examinations and retinal imaging. Retinal information was extracted from the retinal images using a semi-automatic computer program. Three stepwise logistic regression models were evaluated: model 1 with cardiovascular risk factors only; model 2 with retinal information only and model 3 with both cardiovascular risk factors and retinal information. The areas under the receiver operating characteristic curves (AUCs) were used to compare the performances of different models. Results showed that the AUCs were 0.692 (95%CI: 0.622−0.761) and 0.661 (95%CI: 0.588−0.735) for model 1 and model 2, respectively. In addition, model 3 had an AUC of 0.775 (95%CI: 0.716−0.834). Compared to the previous two models, the AUC of model 3 increased significantly (p < 0.05 in both comparisons). In conclusion, retinal information is independently associated with CVD in type 2 diabetes. Further work is needed to validate the translational value of applying retinal imaging analysis into clinical practice.
Cardiovascular disease (CVD) is a major macrovascular complication in diabetes and the leading cause of mortality worldwide. It causes 17.3 million deaths per year, a number that is expected to project to over 23.6 million by 20301. Traditional risk factors of CVD include hypertension, kidney disease, elevated levels of total cholesterol and blood sugar2,3,4,5. Nevertheless, traditional risk factors are insufficient to identify or predict all the CVD events6, which means that other factors could also explain part of the CVD risk.
Retinal vessels are the only vessels that can be directly seen in the human body and provide rich information, including vascular diameter, attenuation, geometry at the branching and measures reflecting how effectively the vascular network fills the retinal space. Recently, the information obtained from retinal vessels has been linked to CVD7,8,9,10. The Atherosclerosis Risk in Communities (ARIC) Study in the general population showed that narrower retinal arterioles, wider retinal venules and the presence of focal arteriolar narrowing were predictive of lacunar stroke after 11.2 years of follow-up7. The Blue Mountain Eye Study showed that participants with the lowest and highest quartiles of fractal dimension (FD), a dimensionless measure reflecting the complexity and density of the retinal vasculature, had a 50% higher risk of coronary heart disease mortality during 14 years of follow-up than those with optimal FD (middle quartiles)8.
However, inconsistent findings were found between other retinal vascular parameters with CVD. For example, a cross-sectional study showed that both retinal arteriolar and venular tortuosity were positively associated with stroke prevalence10. Yet, no association could be demonstrated in a follow-up study11. Furthermore, most studies investigating the association between retinal vascular parameters and CVD were conducted in the general population7,8,9,10,11, rather than diabetic patients12,13,14,15, a group with higher risk of developing CVD (2−5 times) than the general population due to the clustering of risk factors16. In addition, most studies only looked at a single retinal vascular parameter7,8,9, rather than a combination of various retinal information10,11. Therefore, in this study, we attempt to assess the association between a spectrum of retinal information and CVD among type 2 diabetes patients, and evaluate whether this association is independent of traditional cardiovascular risk factors. Our findings should add fuel to the ongoing research on the association between retinal microvascular characteristics and cardiovascular risk.
Results
Comparison of clinical and retinal characteristics
Among the eligible patients, there were 79 patients with CVD (20 patients only had stroke, 54 patients only had coronary heart disease, and 5 patients had both stroke and coronary heart disease). We further identified 150 age-sex matched controls from the recruited patients. Compared to the controls, CVD patients had longer diabetes duration (median years [inter-quartile range (IQR)]: 8 [4−13] vs. 4 [1−9] years, p < 0.001). They were more likely to have hypertension (92.4% vs. 79.3%, p = 0.011) and increased level of HbA1c (mean [standard deviation (SD)]: 7.3% [1.4] vs. 6.8% [1.4], p = 0.024). Other clinical factors were similar in patients with CVD and those without (Table 1).
Table 1. Comparison of clinical characteristics between CVD and non-CVD participants with type 2 diabetes.
| Parameter | CVD | Non-CVD | p value |
|---|---|---|---|
| Number | 79 | 150 | |
| Age (years) | 62.7 (8.3) | 62.0 (7.9) | 0.480 |
| Female, n (%) | 16 (20.3%) | 31 (20.7%) | 0.983 |
| Diabetes duration (years)a | 8 (4 – 13) | 4 (1 – 9) | < 0.001 |
| HbA1c (%) | 7.3 (1.4) | 6.8 (1.4) | 0.024 |
| Current smoker n (%) | 5 (6.3%) | 19 (12.7%) | 0.315 |
| Hypertension, n (%) | 73 (92.4%) | 119 (79.3%) | 0.011 |
| Systolic BP (mmHg) | 132.6 (17.7) | 133.3 (18.2) | 0.794 |
| Diastolic BP (mmHg) | 75.3 (8.6) | 76.8 (8.3) | 0.213 |
| Spot urine ACR (mg/mmol)a | 1.5 (0.4−10.1) | 1.1 (0.4−3.2) | 0.404 |
| eGFR (ml/min/1.73 m2) | 98.6 (23.3) | 103.1 (22.5) | 0.156 |
| Total cholesterol (mmol/L) | 4.2 (1.0) | 4.4 (0.9) | 0.201 |
| Triglycerides (mmol/L)a | 1.4 (1.0−1.9) | 1.3 (1.0−1.8) | 0.772 |
| HDL-cholesterol (mmol/L) | 1.1 (0.3) | 1.2 (0.3) | 0.048 |
| LDL-cholesterol (mmol/L) | 2.3 (0.9) | 2.4 (0.8) | 0.203 |
All data were expressed as mean ± SD or median (IQR) or number (percentages), as appropriate.
The differences between CVD and non-CVD patients were compared with independent two-sample T test for continuous variables and χ2 test for categorical variables, unless otherwise indicated. aComparison was made with Wilcoxon rank-sum test.
Abbreviations: ACR: albumin to creatinine ratio; BP: blood pressure; CVD: cardiovascular disease; eGFR: estimated glomerular filtration rate; HbA1c: glycated haemoglobin; HDL: high-density lipoprotein; LDL: low-density lipoprotein.
In terms of retinal characteristics, CVD patients were more likely to have diabetic retinopathy (DR) (38.0% vs. 25.3%, p = 0.047) and smaller arteriolar-to-venular diameter ratio (AVR) (0.70 [0.04] vs. 0.72 [0.05], p = 0.006) when compared to non-CVD controls (Table 2). CVD patients had less complex retinal arteriolar branching pattern (arteriolar FD: 1.15 [0.05] vs. 1.16 [0.04], p = 0.028). Furthermore, larger arteriolar branching coefficient (BCa) (1.67 [0.23] vs. 1.60 [0.24], p = 0.042) and smaller of arteriolar junctional exponent (JEa) (−0.66 [0.23] vs. −0.54 [0.26], p = 0.001) were observed in CVD patients.
Table 2. Retinal information comparison between CVD and non-CVD patients.
| Parameter | CVD | Non- CVD | p value |
|---|---|---|---|
| Number | 79 | 150 | |
| DR | 30 (38.0%) | 38 (25.3%) | 0.047 |
| CRAE | 138.94 (11.44) | 140.39 (12.86) | 0.401 |
| CRVE | 195.13 (15.98) | 193.14 (14.82) | 0.348 |
| AVR | 0.70 (0.04) | 0.72 (0.05) | 0.006 |
| BSTDa | 10.19 (1.92) | 9.79 (1.78) | 0.117 |
| BSTDv | 9.02 (1.46) | 8.99 (1.71) | 0.902 |
| FDa | 1.15 (0.05) | 1.16 (0.04) | 0.028 |
| FDv | 1.17 (0.04) | 1.17 (0.04) | 0.746 |
| TORTa ( × 105) | 7.26 (1.12) | 7.15 (0.98) | 0.459 |
| TORTv ( × 105) | 8.46 (1.26) | 8.22 (1.04) | 0.120 |
| BAa | 78.64 (10.83) | 79.34 (8.62) | 0.683 |
| BAv | 80.27 (8.46) | 79.52 (7.78) | 0.498 |
| BCa | 1.67 (0.23) | 1.60 (0.24) | 0.042 |
| BCv | 1.44 (0.22) | 1.40 (0.20) | 0.162 |
| AFa | 0.82 (0.05) | 0.82 (0.05) | 0.729 |
| AFv | 0.75 (0.06) | 0.75 (0.07) | 0.997 |
| JEa | −0.66 (0.23) | −0.54 (0.26) | 0.001 |
| JEv | −0.33 (0.30) | −0.28 (0.27) | 0.226 |
| AAa | 32.67 (10.67) | 32.64 (9.81) | 0.996 |
| AAv | 42.10 (9.78) | 40.87 (10.45) | 0.535 |
| LDRa | 9.94 (6.40) | 10.85 (6.89) | 0.387 |
| LDRv | 11.97 (5.69) | 11.21 (5.46) | 0.345 |
All data were expressed as mean ± SD or number (percentages), as appropriate.
The differences between CVD and non-CVD patients were compared with independent two-sample T test for continuous variables and χ2 test for categorical variables.
Abbreviations: AA: angular asymmetry; AF: asymmetry factor; AVR: arteriolar-to-venular diameter ratio; BA: branching angle; BC: branching coefficient; BSTD: standard deviation of the vessel width; CRAE: central retinal arteriolar equivalent; CRVE: central retinal venular equivalent; DR: diabetic retinopathy; FD: fractal dimension; JE: junctional exponent; LDR: length-to-diameter ratio; TORT: curvature tortuosity. A lowercase “a” or “v” at the end of the parameter name indicates arteriolar or venular measurements.
Models using different strategies
In the model only using traditional cardiovascular risk factors (model 1), hypertension, longer diabetes duration and decreased high-density lipoprotein (HDL)-cholesterol were associated with CVD (Table 3). The area under the receiver-operating characteristic curve (AUC) was 0.692 (95%CI: 0.622−0.761) (Table 3, Fig. 1). In the model using retinal information alone (model 2), patients with DR, smaller AVR and arteriolar JE were more likely to have CVD, and the model had an AUC of 0.661 (95%CI: 0.588−0.735). Furthermore, in the comprehensive model using both traditional cardiovascular risk factors and retinal characteristics (model 3), hypertension, longer diabetes duration, higher HbA1c level, smaller AVR, arteriolar BC and JE, as well as larger venular length-to-diameter ratio (LDR) were associated with CVD. The AUC for the comprehensive model was 0.775 (95%CI: 0.716−0.834). Compared to the previous two models, the AUC of model 3 increased significantly (model 3 vs. model 1, p = 0.010; model 3 vs. model 2, p = 0.002) (Table 4). No significant difference was found between model 1 and model 2 (p = 0.544).
Table 3. Stepwise logistic regression analysis showing factors associated with CVD in different models.
| Included parameter | Odds ratio | 95%CI | p value |
|---|---|---|---|
| Model 1: Inclusion of traditional cardiovascular risk factors only | |||
| Diabetes duration | 1.09 | 1.04–1.14 | < 0.001 |
| Hypertension | 2.63 | 1.02–6.78 | 0.46 |
| HDL-cholesterol | 0.39 | 0.14–1.09 | 0.72 |
| Hosmer- Lemeshow p-value: 0.490; AUC: 0.692 (95%CI: 0.622–0.761) | |||
| Model 2: Inclusion of retinal characteristics only | |||
| DR | 1.79 | 0.92–3.11 | 0.091 |
| AVR | 0.002 | 0.00–1.40 | 0.063 |
| JEa | 0.19 | 0.06–0.62 | 0.006 |
| Hosmer- Lemeshow p-value: 0.672; AUC: 0.661 (95%CI: 0.588–0.735) | |||
| Model 3: Inclusion of traditional cardiovascular risk factors and retinal characteristics | |||
| Diabetes duration | 1.08 | 1.03–1.14 | 0.001 |
| Hypertension | 2.47 | 0.90–6.75 | 0.077 |
| HbA1c | 1.29 | 1.02–1.61 | 0.031 |
| AVR | 0.002 | 0.00–1.94 | 0.080 |
| BCa | 0.10 | 0.01–1.06 | 0.056 |
| JEa | 0.03 | 0.003–0.33 | 0.004 |
| LDRv | 1.06 | 1.00–1.12 | 0.057 |
| Hosmer- Lemeshow p-value: 0.267; AUC: 0.775 (95%CI: 0.716–0.834) | |||
Abbreviations: AVR: arteriolar-to-venular diameter ratio; AUC: area under receiver operating characteristic curves; BC: branching coefficient; DR: diabetic retinopathy; HbA1c: glycated haemoglobin; HDL: high density lipoprotein; JE: junctional exponent; LDR: length-to-diameter ratio. A lowercase “a” or “v” at the end of the parameter name indicates arteriolar or venular measurements.
Figure 1. AUC comparison between different models.
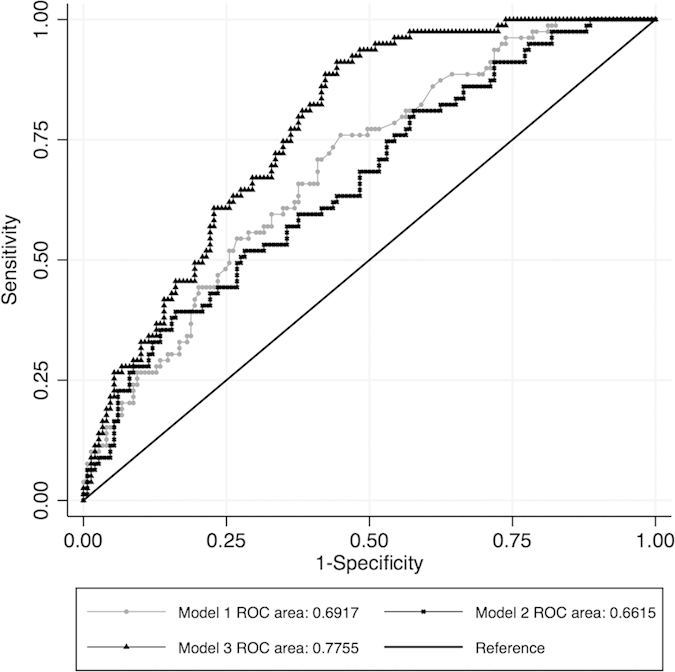
(Model 1: Inclusion of traditional cardiovascular risk factors only; Model 2: Inclusion of retinal information only; Model 3: Inclusion of traditional cardiovascular risk factors + retinal information).
Table 4. Comparison of area under receiver operating characteristic curves (AUC) between different models using DeLong method.
| Model comparison | p value |
|---|---|
| Model 1 vs Model 2 | 0.544 |
| Model 1 vs Model 3 | 0.010 |
| Model 2 vs Model 3 | 0.002 |
Model 1: Inclusion of traditional cardiovascular risk factors only.
Model 2: Inclusion of retinal information only.
Model 3: Inclusion of traditional cardiovascular risk factors + retinal information.
Discussion:
Using an age-sex matched case-control model, our study first shows that a series of vascular information, such as vascular diameter and bifurcation-related parameters, is associated with CVD in type 2 diabetes patients. The association was independent of traditional cardiovascular risk factors. These results implied that in type 2 diabetes, assessment of retinal vasculature may have the potential to provide more information in risk estimation of CVD. However, longitudinal studies are needed to further confirm the findings in our study.
In diabetes patients, presence of DR is a marker of increased CVD risk in type 2 diabetes; this has been demonstrated in several studies17,18,19,20. In ARIC among type 2 diabetes patients, DR was an independent risk factor for incident stroke (relative risk [RR]: 2.34, 95%CI: 1.13−4.86), heart failure (RR: 2.71, 95%CI: 1.46–5.05) and coronary heart disease (RR: 2.07, 95%CI: 1.38−3.11) after multivariate adjustment of cardiovascular risk factors17,18,19. The severity of DR was also positively associated with the incidence of cardiovascular events20. Our findings suggest a positive association between DR and CVD as well.
In terms of the association between retinal vascular parameters and CVD, the Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) in type 2 diabetes patients did show that smaller retinal arteriolar caliber or larger retinal venular caliber were more likely to be associated with increased stroke mortality after 22-years of follow-up12. No significant association was found between retinal vascular diameter and mortality of ischemic heart disease in the same study12. Another WESDR study conducted in type 1 diabetes patients showed that smaller AVR was associated with increased risk of myocardial infarction, but not angina or stroke13. The Pittsburgh Epidemiology of Diabetes Complications study revealed a positive association between smaller CRAE and incidence of coronary heart disease among female type 1 diabetes patients14. Similar findings were also demonstrated in an African American population with type 1 diabetes, where smaller CRAE was associated with increased 6-year incidence of CVD15. We also found that retinal diameter-related parameters were associated with CVD. We further demonstrated that retinal bifurcation related parameters were associated with CVD in type 2 diabetes patients. However, all the studies in the same area were conducted in the general population8,10,11 and no comparable study focused on diabetes population. It might be because the accurate and reliable detection of complex retinal vascular parameters, such as vascular tortuosity, FD or bifurcation-related parameters, was only available recent years with the advancement of digital retinal imaging technology and computer program21.
Our findings, reported in this study, are not fully consistent with previously published studies8,9,11, which showed that retinal vascular fractal dimension, but not tortuosity or bifurcation angle, was related to CVD in the general population. Our study, however, shows that bifurcation-related parameters are significantly associated with CVD in type 2 diabetes. One possible explanation might be that different statistical methods were used in analyzing retinal vascular characteristics. Most of the previous studies assessed the association based on per quartile or per SD change of these continuous retinal vascular characteristics7,8,9,10,12,22. A second possible reason might be that different study populations were not comparable, with most studies conducted in the general population7,8,9,10,11,22 and only a few studies focused on diabetes patients12. Third, we included a wide spectrum of retinal vascular characteristics and investigated the overall association with CVD, while most previous studies only focused on one particular characteristic7,8,9,10,12,22. Last, our study randomly selected one eye to extract the vascular information, while some other studies measured all retinal vascular parameters exclusively from right eyes8 or left eyes9, or used the mean value from both eyes12,13,15. Although the left and the right eyes were substantially correlated23,24,25, there were still some differences caused by the different intrinsic ocular factors and non-simultaneous retinal image taking time, which may lead to the differences observed between eyes25,26. Our results add further knowledge to the ongoing debate of the association between retinal information and CVD.
The association between retinal information and CVD has several possible underlying biological mechanisms. First, there is a close connection of retinal and cerebral microvasculature during the embryonic development and they share similar vascular regulatory processes, which imply that retinal vessels may alter with changes of the cerebral vasculature27,28,29,30. Second, according to the Murray principle of minimum work, the human circulatory systems are optimized to achieve the fastest transportation rates with the minimal energy costs across any vascular network31,32,33. Under disease conditions, both retinal and cerebral microcirculations are affected at the same time. The vascular topography has to change in both systems in order to meet the new physiological condition. Thus, changes of retinal vessels may parallel the vascular changes in the cerebral circulation.
To our knowledge, this is the first study that considers the association between a combination of various retinal information and CVD. We found one study using retinal imaging analysis that looked at a series of retinal vascular parameters and Alzheimer’s disease34, and demonstrated the clinical usefulness of various retinal information. We discussed the possible underlying biological and physiological mechanisms, and the findings in our study clearly indicated an independent association of retinal information and CVD, despite the current absence of a comparable study. We are aware of the necessity of more investigations before we can promote the comprehensive retinal imaging analysis with retinal vascular measures into clinical practice. First of all, the additional significant value of various retinal parameters for CVD prediction must be demonstrated versus relying solely on the traditional cardiovascular risk factors. A study in 9,155 non-diabetic participants showed that retinal vascular diameter provides only slightly superior prediction value to coronary heart disease incidence when compared to the Framingham risk model (AUC increased from 0.695 to 0.706)22. Thus, whether adding more retinal information into the risk evaluation model improves the model performance still requires further investigations. Second, automatic vessel tracking technique is needed to reduce the observer input and increase efficiency. Numerous studies are now focusing on isolating the information from retinal images by automatic computer programs35,36,37. Retinal imaging analysis with various retinal vascular measures may soon be clinically available and provide real-time information of an individual’s potential, future CVD risk38. But large population studies are urgently needed to understand the normal ranges of the retinal vascular parameters.
The strengths of our study include using a reliable program to measure a wide spectrum of retinal vascular parameters21. We also separate retinal arterioles and venules in the analysis, as they may have different optimal microcirculation characteristics, due to the differences of physiological function between arterioles and venules39. Another strength is that we used the same questionnaires, with standardized protocol of clinical characteristics measurements, and the same laboratory tests. Furthermore, two trained endocrinologists graded each retinal image separately and DR was confirmed only if they agreed with each other on these results; this guaranteed the reliability of the DR grading in this study. The following limitations should also be addressed: first, this is an age-sex matched case-control study with a small sample size. The study settings precluded us from exploring the casual relationship between retinal vascular parameters and CVD. A prospective cohort study with larger sample size is needed to confirm the findings in our study and further evaluate the value of using retinal imaging as a tool to predict CVD. Second, we failed to consider the confounding effect of other cardiovascular risk factors on changes of retinal vessel parameters due to the stepwise logistic regression analysis. Last, we only considered Chinese type 2 diabetes patients. The results may not be applicable to other ethnic populations40.
In conclusion, we observed that retinal characteristics were associated with CVD by conducting a case-control study in type 2 diabetes patients. Our results implied that comprehensive retinal imaging analysis with retinal vascular measures may provide additional information to identify CVD. However, one still needs to define “the norm” values of these retinal parameters in the general population in order to aid the understanding in clinical settings. Also, further studies are needed to validate the translational value of retinal imaging analysis in clinical practice.
Methods:
Patient enrollment and study design
The study, together with all experimental protocols, was approved by the Joint Chinese University of Hong Kong – New Territories East Cluster Clinical Research Ethics Committee (CREC) and was endorsed by the Jockey Club School of Public Health and Primary Care of the Chinese University of Hong Kong. The study was performed in accordance with the approved guidelines of CREC and informed consent form was obtained from all participants. We consecutively recruited type 2 diabetes patients from January 2008 to May 2010 at Ma On Shan Family Medicine Center. Eligible participants were those aged over 18 years with diagnosed type 2 diabetes. Female patients who were pregnant or lactating, or patients with type 1 diabetes defined as presentation with diabetic ketoacidosis, unprovoked ketosis, or requirement of insulin within 12 months of diagnosis were excluded. A total of 644 Chinese type 2 diabetes patients were recruited. Every patient underwent comprehensive assessments, including questionnaires of demographic information and medical history, blood and urine tests, as well as retinal images.
Patients with CVD (1. stroke or transient ischemic attack; 2. coronary heart disease) were defined as cases, and patients without CVD were defined as controls. Medical history of CVD was first self-reported through questionnaires by the patients. Then, the CVD history of every patient was cross-checked with records from the electronic Clinical Management System (CMS) in Hong Kong or from the referring physician41. The CMS captures admission information of all public hospitals and it is the sole portal for information used in all public clinical settings41. Age and sex matched controls without medical history of CVD were selected at a ratio of around 1:2.
Traditional risk factors measurements
Demographic information was collected using questionnaires. Smoking habits were recorded and encoded as current or non-current smokers. Blood pressure (BP) was measured from both arms after at least 5 minutes of resting and the average value was used in the analysis. Hypertension was defined as known hypertension, and/or systolic BP/diastolic BP ≥ 130/80 mmHg with/without anti-hypertension treatment.
Blood and urine samples were collected after overnight fasting to assess the level of blood glucose, glycated haemoglobin (HbA1c), lipid profile (total cholesterol, triglycerides, HDL-cholesterol and calculated low density lipoprotein [LDL]-cholesterol) and renal functions. Estimated glomerular filtration rate (eGFR) was calculated based on age, gender and serum creatinine level42. A spot urine sample was used to estimate urine albumin to creatinine ratio (ACR). One patient without complete clinical information was excluded from the analysis.
Retinal information assessment
Digital fundus photographs were acquired by a trained technician using a Topcon non-mydriatic retinal camera of both eyes respectively (TRC-NW6S, Tokyo Optical Co, Tokyo). The spatial resolution of each image was 2896 by 1944 pixels and the images were stored without compression before analysis. DR was graded by two trained endocrinologists according to the International Diabetic Retinopathy Disease Severity Scale43. The participant was defined as having DR if either eye had hemorrhage, hard exudates, cotton wool spots or any other signs of DR43.
As retinal image with blurred optic disc edge or small retinal vessels may not be reliably and accurately measured, we excluded patients without acceptable quality of retinal images (n = 78) from the analysis. Then, a total of 21 retinal vascular characteristics were extracted from a randomly selected eye with a commercially available semi-automatic computer program - Singapore I Vessel Assessment program21. The detailed information on retinal vessel measurements was published earlier21. In general, retinal arterioles and venules were separated in the analysis with a lowercase ‘a’ or ‘v’ at the end of the parameter name, indicating arteriolar or venular measurements. Retinal diameter was presented as central retinal arteriolar equivalent (CRAE) and central retinal venular equivalent (CRVE) using the Knudtson-Parr-Hubbard formula from the largest six arterioles and venules, respectively44. The AVR was defined as the ratio of CRAE to CRVE. Standard deviation of the vessel width (BSTD) was used to indicate the difference of the diameters of the included vessels. The length-to-diameter ratio (LDR) was calculated as the ratio of vessel length from the midpoint of one vascular bifurcation to the midpoint of the next bifurcation, to the diameter of the parent vessel at the first bifurcation45. It reflects the diameter change independent of refractive magnification power of the eye. The complexity of the retinal vascular network was assessed using fractal dimension (FD)46. Vessel curvature tortuosity (TORT) was defined as the ratio of the integral of the total squared curvature of the vessel segment to the length of the vessel arc47. A series of bifurcation-related parameters were also extracted from retinal images. Branching angle (BA) was denoted as the angle between two daughter vessels48. Branching coefficient (BC) was defined as (d1 + d2)2/d02, where d0 was the width of the trunk vessel and d1 and d2 were the two branching vessels48,49. Asymmetry factor (AF) was calculated as d12/d22, where d1 is greater than or equal to d2. Angular asymmetry (AA) was defined as the difference between two daughter angles of a bifurcation. Junctional exponent (JE) was defined as JE = (d03 − d13 − d23)1/3/d0. These parameters describe the deviation from optimality at a bifurcation.
Statistical analysis
The differences of clinical and retinal characteristics between CVD and non-CVD patients were compared using independent two-sample T test or Wilcoxon rank-sum test for continuous data and χ2 test for categorical variables. All data were expressed as mean ± SD or median (IQR) or percentages, as appropriate.
To evaluate the association between retinal information and CVD in type 2 diabetes patients and to assess whether the association is independent of the traditional risk factors of CVD, three stepwise logistic regression analyses were applied: Model 1: using traditional cardiovascular risk factors only50,51,52, namely HbA1c, diabetes duration, current smoking status, BP, total cholesterol, HDL-cholesterol, urine ACR and eGFR; Model 2: using retinal information only, including DR and 21 retinal vessel-related parameters mentioned above; Model 3: using both traditional cardiovascular risk factors and retinal information. All the covariates with a p value less than 0.1 were kept in the final model. To compare the performances of different models, the AUCs were compared using Delong method53.
All the statistical procedures were analyzed using Stata/SE (StataCorp LP, Release 12.1, College Station, TX, USA).
Additional Information
How to cite this article: Guo, V.Y. et al. Retinal Information is Independently Associated with Cardiovascular Disease in Patients with Type 2 diabetes. Sci. Rep. 6, 19053; doi: 10.1038/srep19053 (2016).
Acknowledgments
This study was partially supported by the Chinese University of Hong Kong Technology and Business Development Fund (TBF) No.TBF12MED012. We thank Professor Georges M Halpern from The City University of Hong Kong for his help on the English editing and scientific comments.
Footnotes
Author Contributions V.Y.G. and B.C.Z. initially conceived the concept of this study; V.Y.G. performed the statistical analysis and wrote the manuscript; B.C.Z. provided supervision on the rationale, methodology and interpretation of the study; J.C.C. provided supervision and mentorship on the data; J.C.C. and H.C. provided the data and ensure data quality; J.L. provided input in statistical analysis; R.O., W.S., A.L.U.K. and A.L.A.M. were involved in data collection. All the authors made substantial contribution to the study and have reviewed the manuscript.
References
- Mendis S., Puska P. & Norrving B. Global Atlas on Cardiovascular Disease Prevention and Control, by the World Health Organization (Shanthi Mendis) in collaboration with the World Heart Federation (Pekka Puska) and the World Stroke Organization (Bo Norrving), Geneva 2011. Available at: http://www.world-heart-federation.org/fileadmin/user_upload/images/CVD_Health/Global_CVD_Atlas.pdf. (Accessed: 10 April. 2015).
- Stokes J. 3rd, Kannel W. B., Wolf P. A., D’Agostino R. B. & Cupples L. A. Blood pressure as a risk factor for cardiovascular disease. The Framingham Study–30 years of follow-up. Hypertension 13, I13–18 (1989). [DOI] [PubMed] [Google Scholar]
- Stratton I. M. et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. Bmj 321, 405–412 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarnak M. J. et al. Kidney disease as a risk factor for development of cardiovascular disease - A statement from the American Heart Association councils on kidney in cardiovascular disease, high blood pressure research, clinical cardiology, and epidemiology and prevention. Circulation 108, 2154–2169 (2003). [DOI] [PubMed] [Google Scholar]
- Neaton J. D. et al. Serum cholesterol level and mortality findings for men screened in the Multiple Risk Factor Intervention Trial. Multiple Risk Factor Intervention Trial Research Group. Archives of internal medicine 152, 1490–1500 (1992). [PubMed] [Google Scholar]
- Chamnan P., Simmons R. K., Sharp S. J., Griffin S. J. & Wareham N. J. Cardiovascular risk assessment scores for people with diabetes: a systematic review. Diabetologia 52, 2001–2014 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatsuya H. et al. Retinal microvascular abnormalities and risk of lacunar stroke: Atherosclerosis Risk in Communities Study. Stroke; a journal of cerebral circulation 41, 1349–1355 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liew G. et al. Fractal analysis of retinal microvasculature and coronary heart disease mortality. Eur Heart J 32, 422–429 (2011). [DOI] [PubMed] [Google Scholar]
- Kawasaki R. et al. Fractal dimension of the retinal vasculature and risk of stroke: a nested case-control study. Neurology 76, 1766–1767 (2011). [DOI] [PubMed] [Google Scholar]
- Ong Y. T. et al. Microvascular structure and network in the retina of patients with ischemic stroke. Stroke 44, 2121–2127 (2013). [DOI] [PubMed] [Google Scholar]
- Cheung C. Y. et al. Retinal microvascular changes and risk of stroke: the Singapore Malay Eye Study. Stroke 44, 2402–2408 (2013). [DOI] [PubMed] [Google Scholar]
- Klein R., Klein B. E., Moss S. E. & Wong T. Y. Retinal vessel caliber and microvascular and macrovascular disease in type 2 diabetes: XXI: the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Ophthalmology 114, 1884–1892 (2007). [DOI] [PubMed] [Google Scholar]
- Klein B. E. et al. Cardiovascular disease, mortality, and retinal microvascular characteristics in type 1 diabetes: Wisconsin epidemiologic study of diabetic retinopathy. Archives of internal medicine 164, 1917–1924 (2004). [DOI] [PubMed] [Google Scholar]
- Miller R. G., Prince C. T., Klein R. & Orchard T. J. Retinal vessel diameter and the incidence of coronary artery disease in type 1 diabetes. Am J Ophthalmol 147, 653–660 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy M. S., Klein R. & Janal M. N. Relationship of retinal vessel caliber to cardiovascular disease and mortality in African Americans with type 1 diabetes mellitus. Arch Ophthalmol 130, 561–567 (2012). [DOI] [PubMed] [Google Scholar]
- Almdal T., Scharling H., Jensen J. S. & Vestergaard H. The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death-A population-based study of 13000 men and women with 20 years of follow-up. Archives of internal medicine 164, 1422–1426 (2004). [DOI] [PubMed] [Google Scholar]
- Cheung N. et al. Diabetic retinopathy and risk of heart failure. Journal of the American College of Cardiology 51, 1573–1578 (2008). [DOI] [PubMed] [Google Scholar]
- Cheung N., Rogers S., Couper D. J., Klein R., Sharrett A. R. & Wong T. Y. Is diabetic retinopathy an independent risk factor for ischemic stroke ? Stroke; a journal of cerebral circulation 38, 398–401 (2007). [DOI] [PubMed] [Google Scholar]
- Cheung N., Wang J. J., Klein R., Couper D. J., Sharrett A. R. & Wong T. Y. Diabetic retinopathy and the risk of coronary heart disease: the Atherosclerosis Risk in Communities Study. Diabetes care 30, 1742–1746 (2007). [DOI] [PubMed] [Google Scholar]
- Gerstein H. C. et al. Diabetic retinopathy, its progression, and incident cardiovascular events in the ACCORD trial. Diabetes care 36, 1266–1271 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung C. Y. et al. Quantitative and qualitative retinal microvascular characteristics and blood pressure. J Hypertens 29, 1380–1391 (2011). [DOI] [PubMed] [Google Scholar]
- McGeechan K. et al. Risk prediction of coronary heart disease based on retinal vascular caliber (from the Atherosclerosis Risk In Communities [ARIC] Study). Am J Cardiol 102, 58–63 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couper D. J. et al. Reliability of retinal photography in the assessment of retinal microvascular characteristics: the Atherosclerosis Risk in Communities Study. Am J Ophthalmol 133, 78–88 (2002). [DOI] [PubMed] [Google Scholar]
- Leung H. et al. Computer-assisted retinal vessel measurement in an older population: correlation between right and left eyes. Clin Experiment Ophthalmol 31, 326–330 (2003). [DOI] [PubMed] [Google Scholar]
- Wong T. Y., Knudtson M. D., Klein R., Klein B. E., Meuer S. M. & Hubbard L. D. Computer-assisted measurement of retinal vessel diameters in the Beaver Dam Eye Study: methodology, correlation between eyes, and effect of refractive errors. Ophthalmology 111, 1183–1190 (2004). [DOI] [PubMed] [Google Scholar]
- Lanigan L. P., Clark C. V. & Hill D. W. Retinal circulation responses to systemic autonomic nerve stimulation. Eye (Lond) 2 (Pt 4), 412–417 (1988). [DOI] [PubMed] [Google Scholar]
- Risau W. Mechanisms of angiogenesis. Nature 386, 671–674 (1997). [DOI] [PubMed] [Google Scholar]
- Hughes S., Yang H. & Chan-Ling T. Vascularization of the human fetal retina: roles of vasculogenesis and angiogenesis. Investigative ophthalmology & visual science 41, 1217–1228 (2000). [PubMed] [Google Scholar]
- Hardy P., Varma D. R. & Chemtob S. Control of cerebral and ocular blood flow autoregulation in neonates. Pediatr Clin North Am 44, 137–152 (1997). [DOI] [PubMed] [Google Scholar]
- Delaey C. & Van De Voorde J. Regulatory mechanisms in the retinal and choroidal circulation. Ophthalmic Res 32, 249–256 (2000). [DOI] [PubMed] [Google Scholar]
- Zamir M. Cost analysis of arterial branching in the cardiovascular systems of man and animals. Journal of theoretical biology 120, 111–123 (1986). [DOI] [PubMed] [Google Scholar]
- Murray C. D. The Physiological Principle of Minimum Work Applied to the Angle of Branching of Arteries. The Journal of general physiology 9, 835–841 (1926). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossitti S. & Lofgren J. Optimality principles and flow orderliness at the branching points of cerebral arteries. Stroke; a journal of cerebral circulation 24, 1029–1032 (1993). [DOI] [PubMed] [Google Scholar]
- Frost S. et al. Retinal vascular biomarkers for early detection and monitoring of Alzheimer’s disease. Transl Psychiatry 3, e233 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Zee B. C. & Li Q. Detection of neovascularization based on fractal and texture analysis with interaction effects in diabetic retinopathy. Plos One 8, e75699 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben Abdallah M. et al. Automatic extraction of blood vessels in the retinal vascular tree using multiscale medialness. Int J Biomed Imaging 2015, 519024 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez L., Barreira N., Penedo M. G. & Coll De Tuero G. Computer aided diagnosis system for retinal analysis: automatic assessment of the vascular tortuosity. Stud Health Technol Inform 207, 55–64 (2014). [PubMed] [Google Scholar]
- Patton N., Aslam T., MacGillivray T., Pattie A., Deary I. J. & Dhillon B. Retinal vascular image analysis as a potential screening tool for cerebrovascular disease: a rationale based on homology between cerebral and retinal microvasculatures. J Anat 206, 319–348 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton N., Aslam T., Macgillivray T., Dhillon B. & Constable I. Asymmetry of retinal arteriolar branch widths at junctions affects ability of formulae to predict trunk arteriolar widths. Invest Ophthalmol Vis Sci 47, 1329–1333 (2006). [DOI] [PubMed] [Google Scholar]
- Li X. et al. Racial differences in retinal vessel geometric characteristics: a multiethnic study in healthy Asians. Investigative Ophthalmology & Visual Science 54, 3650–3656 (2013). [DOI] [PubMed] [Google Scholar]
- Wong M. C., Jiang J. Y., Tang J. L., Lam A., Fung H. & Mercer S. W. Health services research in the public healthcare system in Hong Kong: an analysis of over 1 million antihypertensive prescriptions between 2004–2007 as an example of the potential and pitfalls of using routinely collected electronic patient data. BMC health services research 8, 138 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y. C. et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol 17, 2937–2944 (2006). [DOI] [PubMed] [Google Scholar]
- Wilkinson C. P. et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 110, 1677–1682 (2003). [DOI] [PubMed] [Google Scholar]
- Knudtson M. D., Lee K. E., Hubbard L. D., Wong T. Y., Klein R. & Klein B. E. Revised formulas for summarizing retinal vessel diameters. Curr Eye Res 27, 143–149 (2003). [DOI] [PubMed] [Google Scholar]
- King L. A., Stanton A. V., Sever P. S., Thom S. A. & Hughes A. D. Arteriolar length-diameter (L:D) ratio: a geometric parameter of the retinal vasculature diagnostic of hypertension. Journal of human hypertension 10, 417–418 (1996). [PubMed] [Google Scholar]
- Mainster M. A. The fractal properties of retinal vessels: embryological and clinical implications. Eye (Lond) 4 (Pt 1), 235–241 (1990). [DOI] [PubMed] [Google Scholar]
- Hart W. E., Goldbaum M., Cote B., Kube P. & Nelson M. R. Measurement and classification of retinal vascular tortuosity. Int J Med Inform 53, 239–252 (1999). [DOI] [PubMed] [Google Scholar]
- Zamir M., Medeiros J. A. & Cunningham T. K. Arterial bifurcations in the human retina. J Gen Physiol 74, 537–548 (1979). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamir M. Nonsymmetrical bifurcations in arterial branching. J Gen Physiol 72, 837–845 (1978). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X. et al. Development and validation of stroke risk equation for Hong Kong Chinese patients with type 2 diabetes: the Hong Kong Diabetes Registry. Diabetes care 30, 65–70 (2007). [DOI] [PubMed] [Google Scholar]
- Yang X. et al. Development and validation of a total coronary heart disease risk score in type 2 diabetes mellitus. The American journal of cardiology 101, 596–601 (2008). [DOI] [PubMed] [Google Scholar]
- Kothari V. et al. UKPDS 60: risk of stroke in type 2 diabetes estimated by the UK Prospective Diabetes Study risk engine. Stroke; a journal of cerebral circulation 33, 1776–1781 (2002). [DOI] [PubMed] [Google Scholar]
- DeLong E. R., DeLong D. M. & Clarke-Pearson D. L. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44, 837–845 (1988). [PubMed] [Google Scholar]


