Abstract
Aseptic necrosis of the femoral head is a disease whose etiology is not completely elucidated and generally affects young adults aged between 30 and 50 years. In a significant number of patients bilateral disease occurs, which makes detection in its early stages constitute an important objective. We present the case of a male patient, aged 23 years, with the following risk factors: smoking and chronic alcohol consumption, who is diagnosed with aseptic necrosis of the left femoral head, ARCO stage IV, and in just six months after the diagnosis and hip arthroplasty, he suffers an injury which leads to the same diagnosis in the contralateral hip. We want to emphasize that for all patients with a high index of suspicion there should be an MRI examination, because the plane radiographs or CT are most often not relevant in detecting early signs of this condition. Diagnosis of aseptic necrosis of the femoral head in the early stages is a necessity in order to obtain an optimal result of conservative treatment.
Keywords: aseptic necrosis, femoral head, MRI
Introduction
Aseptic necrosis of the femoral head is a disease whose etiology is not completely elucidated, the triggering event being the suppression of blood supply to the femoral head. [1-6].
The disease is common especially among the younger population, patients usually being between the 3rd and 5th decade of life, particularly affecting men [7, 8]. For the early diagnosis of aseptic necrosis of the femoral head the physician should have a high index of suspicion, especially in patients with risk factors.
The main risk factors of the disease are represented by trauma, chronic alcohol consumption, smoking, corticosteroid treatment [1, 7]. This is particularly important in patients where the disease is already present in one femoral joint as aseptic necrosis often occurs bilaterally [1, 3].
Case Presentation
Patient MI, aged 23, from an urban environment, construction worker, smoker (40 cigarettes per day from age 11), chronic alcohol consumption (beer, wine / daily), without significant pathological personal history, presented in June 2014 in the Medical Rehabilitation Clinic accusing pain in the left hip irradiated in the knee with functional impotence of the left lower limb with onset of about 3 months.
Physical examination of the patient revealed the following aspects- normal weight, discrete erythrose of the cheekbone, BP = 130/70 mmHg, AV = 72 bpm, scoliotic attitude, paravertebral muscle stiffness in the lumbar spine, pain when mobilizing the coxo-femoral joint, limitation of flexion, abduction and rotation in the left hip joint, positive left Faber test, positive left Patrick maneuver, intensely painful Trandelenburg positive sign on the left.
The results of laboratory tests were normal, except ESR = 24mm / 1 hour 46 mm / 2h, Fibrinogen = 423 mg / 100ml, alkaline phosphatase = 138 IU / l, Gamma glutamyltransferase = 79 U / l, GOT (glutamic oxaloacetate transferase) = 57 U / L, GPT (glutamic pyruvate transaminase) = 62 U / l total cholesterol = 231 mg / dl.
The pelvic radiography (Fig.1) noted loss of sphericity and collapse of the left femoral head, left joint space narrowing and acetabular changes. No changes were found in the right femoral head. Imaging investigations continued with a CT scan, which surprised the following aspects: sclerosis, the presence of cysts, microfracture and changes of the trabecular bone, highlighting the femoral head collapse and degeneration of the left coxo femoral joint.
Fig.1.

Coxal X-ray. It can be seen marked narrowing of the left coxal-femoral joint space, left femoral head deformation, circumscribed areas at the femoral neck, anterior-superior region and subchondral bone attachment aspect.
With imaging investigations (Fig.2) the patient was diagnosed with aseptic necrosis of the left femoral head stage IV (ARCO classification) and obtained transfer to the Orthopaedics-Traumatology Clinic in order to undergo surgery. The patient underwent surgery for hip arthroplasty with implantation of a left prosthetic bipolar partial hip. Upon discharge the following the recommendations were made: physical therapy to recover walking and change of lifestyle: quit smoking and severely limit alcohol consumption.
Fig.2.
Coxal CT - left coxo-femoral articular effusion with edema and bone sclerosis aspect, the presence of cysts, microfractures in the left femoral head. The collapse of the femoral head and joint degeneration in the left coxo-femoral joint.
After obtaining the agreement of the patient, the left femoral head taken during hip arthroplasty (Fig.3) was fixed in 10% formalin, decalcified and sectioned in order to obtain some histological slices for inclusion in a larger study which followed the morphological changes that occur in patients diagnosed with aseptic necrosis of the femoral head. Macroscopic and microscopic images thus obtained confirmed the diagnosis and extension of the area of necrosis to the adjacent cartilage (Fig.4,5).
Fig.3.
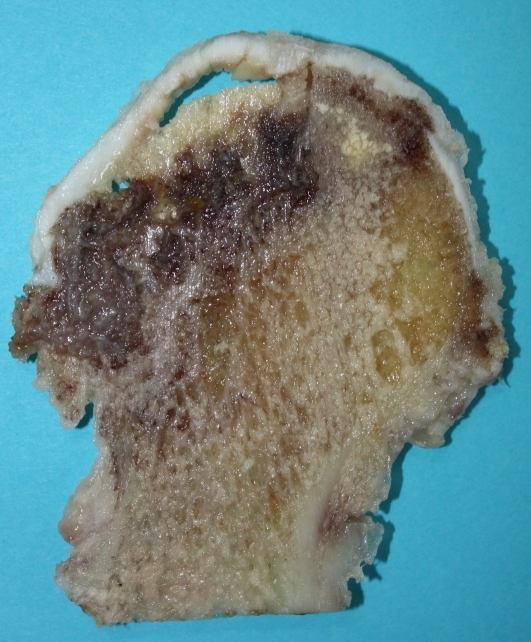
Coxal CT - left coxo-femoral articular effusion with edema and bone sclerosis aspect, the presence of cysts, microfractures in the left femoral head. The collapse of the femoral head and joint degeneration in the left coxo-femoral joint.
Fig.4.
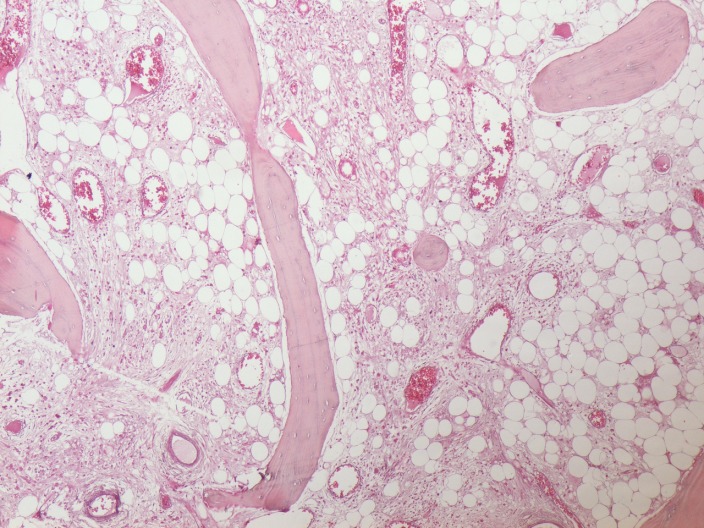
Coxal CT - left coxo-femoral articular effusion with edema and bone sclerosis aspect, the presence of cysts, microfractures in the left femoral head. The collapse of the femoral head and joint degeneration in the left coxo-femoral joint.
Fig.5.
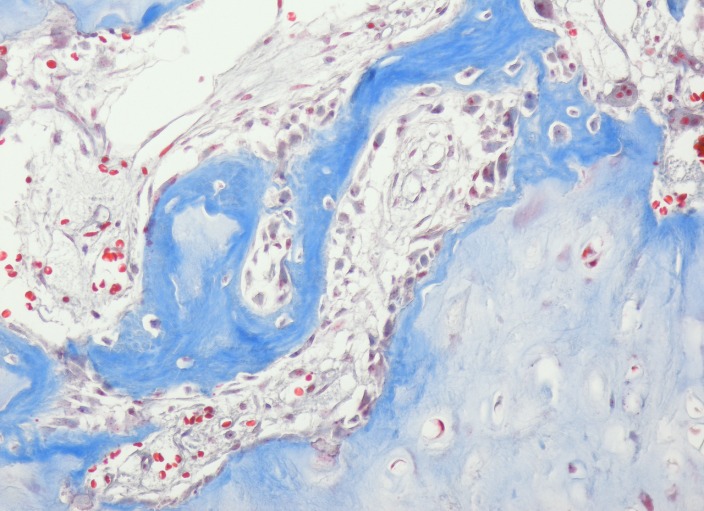
Coxal CT - left coxo-femoral articular effusion with edema and bone sclerosis aspect, the presence of cysts, microfractures in the left femoral head. The collapse of the femoral head and joint degeneration in the left coxo-femoral joint.
Discussion
The peculiarity of the case is the appearance of the disease at a very young age, the patient being only 23 years old and diagnosed in stage IV in the left hip and stage I in the right hip and already undergone arthroplasty of the hip.
Aseptic necrosis of femoral head mainly affects young adults, who are between the 3rd and 5th decade of life [1, 3, 8-11]. It is considered that the average age that patients are diagnosed with aseptic necrosis of the femoral head and the timing of the first hip replacement is 38 years old [4, 8].
Risk factors are represented by chronic alcohol consumption (beer, wine / daily smoking (40 cigarettes per day from age 11) trauma and is more frequent in men.
It is believed that aseptic necrosis of femoral head affects men 4 times more than women [3, 9-11]. Some authors recorded a male to female sex ratio of 8: 1, except that the condition occurs in the context of systemic lupus erythematosus [1].
We cannot predict with certainty whether aseptic necrosis of the femoral head to the right is due to suffered trauma in our patient or that the damage occurred at this level as a consequence of long alcohol consumption and smoking.
It seems appropriate to conduct an MRI exam in detriment of CT in patients with risk factors for aseptic necrosis of the femoral head, even if there are no signs on plain radiography showing the existence of the disease.
Changes in the early stages of aseptic necrosis of the femoral head are hard to detect on plane X-ray. A normal image obtained by X-ray does not necessarily translate into the absence of the disease [1, 3, 9, 12]. Between the occurrence of hip injury and detection on X-ray suggestive images a 5 year interval usually passes [9, 10, 12]. The sensitivity of the method in the diagnosis of early stages is only 41% [13].
In the early stages, the sensitivity of CT is quite low, being only 55% [10, 12], but can be detect certain alterations in bone density when X-ray images are normal [14, 15]. CT is useful in assessing the later stages for lesion extension, such as sclerosis and other events occurring in the state of repair.
MRI is a non-invasive imaging technique with the highest degree of specificity and sensitivity used in the diagnosis of aseptic necrosis of the femoral head [3, 9, 10, 12, 16]. In the early stages is more effective than simple computerized tomography (CT) or the single-photon emission (SPECT), with a degree of increased specificity in the detection of the condition of up to 90% [12, 14].
The young age of the patient makes it very likely that they will need additional hip surgery. It is unlikely that the prosthesis used during hip arthroplasty to retain functionality for 40-45 years, as is the life expectancy of the patient. Long-term results on the use of full or partial dentures (cemented or uncemented) in the treatment of this condition is generally unsatisfactory [17-19].
Conclusions
Knowing the risk factors involved in aseptic necrosis of the femoral head it is essential for early disease detection, because in the early stages the poor or absent symptoms and laboratory imaging investigations detect no changes. A thorough investigation is particularly important for patients whose disease is already present at one of coxo-femoral joint as in 50- 60% of cases bilateral aseptic necrosis occurs.
Patients at high suspicion should undergo an MRI examination, even if the plane X-ray or CT have not detected significant changes, because the diagnosis of aseptic necrosis of the femoral head in the early stages is a necessity in order to obtain an optimal result when performing conservative treatment.
Acknowledgments
This paper is supported by the Sectorial Operational Programme Human Resources Development (SOP HRD), financed from the European Social Fund and by the Romanian Government under the contract number POSDRU/159/1.5/S/132395”
References
- 1.Tofferi JK, Gilliland W. Avascular necrosis. Medscape. available at http://emedicine.medscape.com/article/333364 . updated: Jun, 2014. [Google Scholar]
- 2.Davis CM, Parrish WM. Avascular necrosis. University of Pennsylvania Orthopaedic Journal. 2000;13:22–28. [Google Scholar]
- 3.Levine M, Rajadhyaksha A. Hip osteonecrosis. Medscape. available at http://emedicine.medscape.com/article/1247804 . updated: May 1, 2012. [Google Scholar]
- 4.Kelly JD, Sherwin SW. Femoral head avascular necrosis. Medscape. available at http://emedicine.medscape.com/article/86568 . updated: Feb 28, 2010. [Google Scholar]
- 5.Schoenstadt A. Avascular necrosis. eMedTV. available at http://bones.emedtv.com/avscular necrosis/avascular-necrosis.html . last updated: Nov 5, 2008. [Google Scholar]
- 6.Kaushik AP, Das A, Cui Q. Osteonecrosis of the femoral head: an update in year 2012. World J Orthop. 2012;3(5):49–57. doi: 10.5312/wjo.v3.i5.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD, Urbaniak JR. Osteonecrosis of the hip in the 21st century. Instr Course Lect. 2003;52:337–355. [PubMed] [Google Scholar]
- 8.Mont M, Hungerford DS. Non-traumatic avascular necrosis of the femoral head- current concepts review. The Journal of Bone and Joint Surgery. 1995;77-A(3):459–474. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Aiello MR, Chew FS. Imaging in avascular necrosis of the femoral head. Medscape. available at http://emedicine.medscape.com/article/386808 . updated: May 25, 2011. [Google Scholar]
- 10.Orban HB, Cristescu V, Dragușanu M. Avascular necrosis of the femoral head. Maedica- a Journal of Clinical Medicine. 2009;4(1):26–34. [Google Scholar]
- 11.Parvazi J. High yield orthopaedics. Philadelphia: Elsevier Saunders; 2010. pp. 45–46. [Google Scholar]
- 12.Zoia S, Dumitrescu D, Popescu M, Gheonea I, Gabor M, Bogdan N. Imaging of avascular necrosis of the femoral head: familiar methods and newer trends. Current Health Sciences Journal. 2009;35(1):23–28. [PMC free article] [PubMed] [Google Scholar]
- 13.Resnick D, Niwayama G. Osteonecrosis: diagnostic techniques, special situations and complications. In: Resnick D, editor. Diagnosis of Bone and Joint Disorders. Philadelphia: WB Saunders Co,; 1995. pp. 34–95. [Google Scholar]
- 14.Mitchell MD, Kundel HL, Steinberg ME, Kressel HY, Alavi A, Axel L. Avascular necrosis of the hip: comparison of MR, CT and scintigraphy. AJR. 1986;147:67–71. doi: 10.2214/ajr.147.1.67. [DOI] [PubMed] [Google Scholar]
- 15.May DA, Disler DG. Screening for avascular necrosis of the hip with rapid MRI, preliminary experience. J Comput Assis Tomogr. 2000;24(2):284–287. doi: 10.1097/00004728-200003000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Malizos KN, Karantanas AH, Varitimidis SE, Dailiana ZH, Bargiotas K, Maris T. Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol. 2007;63:16–28. doi: 10.1016/j.ejrad.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 17.Brinker MR, Rosenberg AG, Kull L, Galante JO. Primary total hip arthroplasty using noncemented porous- coated femoral componentsin patiens with osteonecrosis of the femoral head. J Arthroplasty. 1998;9:457–468. doi: 10.1016/0883-5403(94)90091-4. [DOI] [PubMed] [Google Scholar]
- 18.Cabanele ME. Bipolar versus total hip arthroplasty for avascular necrosis of the femoral head, a comparison. Clin Orthop. 1990;261:59–62. [PubMed] [Google Scholar]
- 19.Cornell CN, Salveti EA, Pellicci PM. Long-term follow up of total hip replacement in patiens with osteonecrosis. Orthop Clin North America. 1995;16:757–769. [PubMed] [Google Scholar]


