Abstract
Rapidly emerging evidence implicates perineuronal nets (PNNs) and extracellular matrix (ECM) molecules that compose or interact with PNNs, in the pathophysiology of several psychiatric disorders. Studies on schizophrenia, autism spectrum disorders, mood disorders, Alzheimer's disease, and epilepsy point to the involvement of ECM molecules such as chondroitin sulfate proteoglycans, Reelin, and matrix metalloproteases, as well as their cell surface receptors. In many of these disorders, PNN abnormalities have also been reported. In the context of the “quadripartite” synapse concept, that is, the functional unit composed of the pre- and postsynaptic terminals, glial processes, and ECM, and of the role that PNNs and ECM molecules play in regulating synaptic functions and plasticity, these findings resonate with one of the most well-replicated aspects of the pathology of psychiatric disorders, that is, synaptic abnormalities. Here we review the evidence for PNN/ECM-related pathology in these disorders, with particular emphasis on schizophrenia, and discuss the hypothesis that such pathology may significantly contribute to synaptic dysfunction.
1. Introduction
The classic view of psychiatric disorders as “neuronal” disorders has been challenged in recent years by rapidly emerging evidence pointing to the involvement of the extracellular matrix (ECM), glial cells, and their interactions [1–8]. This evidence represents a significant departure from mainstream views and is driving the field toward a growing understanding of these elements as closely interacting components of functional units, such as the “tetrapartite synapse.” This latter term, originally proposed by Dityatev et al. [9], aptly describes the functional unit composed of the of pre- and postsynaptic terminals, astroglial processes, and synaptic/perisynaptic ECM complexes [10–14]. Here, we review evidence for the involvement of the ECM in psychiatric disorders and focus on the hypothesis that ECM abnormalities may contribute to a critical pathological component shared by a large subgroup of these disorders, that is, disruption of synaptic functions [15–21]. First, evidence for ECM abnormalities in schizophrenia, the main focus of these authors' studies, is discussed, with particular emphasis on loss of perineuronal nets (PNNs) in several brain regions in this disorder. We then briefly review evidence for a significant involvement of synaptic pathology in this disorder and follow with a discussion on the potential mechanisms linking such pathology to ECM/PNN abnormalities. Finally, evidence for ECM involvement in other psychiatric disorders is reviewed, with reference to molecular families known to play a role in synaptic functions. The specific patterns and causes of ECM abnormalities in each of these disorders are not yet well understood and may be disorder-specific. We postulate that overlapping patterns of ECM/PNN abnormalities may underlie shared synaptic pathology in these disorders.
It should be emphasized here that synaptic regulation is only one of several critical functions performed by the ECM during pre- and postnatal brain development as well as adulthood (for reviews see [22–30]). Thus, in addition to synaptic dysregulation, the consequences of brain ECM abnormalities may be complex and far-reaching, spanning from disruption of axonal guidance, neuronal differentiation, and migration in early brain development to circuit consolidation and closure of critical periods in postnatal development and finally axonal signal conduction and regulation of the blood/brain barrier in the adult brain [1, 2, 31–38].
2. Schizophrenia
2.1. ECM/PNN Abnormalities in Schizophrenia
Schizophrenia is a chronic, severe, and disabling brain disorder characterized by psychotic symptoms and disruptions of normal emotions and behaviors. Growing evidence points to ECM abnormalities as a component of the core pathophysiology of schizophrenia. Converging results from human genetic and postmortem studies show genetic vulnerabilities for genes encoding several key ECM molecules, including chondroitin sulfate proteoglycans (CSPGs), Reelin, semaphorin 3A, integrins, and remodeling enzymes, as well as dysregulated expression of these molecules in glial cells, and disruption of organized ECM structures such as PNNs (see references below). Animal models indicate that these abnormalities may have far-reaching consequences on neural circuits involved in schizophrenia [39–41]. These findings are briefly reviewed below.
2.1.1. CSPGs
In subjects with schizophrenia, we first reported marked decreases of CSPG-labeled PNNs in the amygdala and entorhinal cortex [42], interconnected brain regions involved in emotion-related learning and associative sensory information processing and in the pathophysiology of schizophrenia [43–47]. In this study, PNNs were detected using the lectin wisteria floribunda agglutinin (WFA; Figure 1), which labels PNNs predominantly associated with GABAergic neurons expressing the calcium binding protein parvalbumin (PVB) [48–54]. Consistently, lower numbers of WFA-labeled PNNs were observed in the lateral nucleus of the amygdala and the superficial layers of the entorhinal cortex, where these interneurons are primarily located [42]. A similar distribution pattern of PNN decreases was detected using antibodies against aggrecan, one of the main CSPGs in the brain [55]. In contrast, immunolabeling with antibodies raised against a specific chondroitin sulfate 6 (CS-6; Figure 1) pattern revealed more extensive PNN distribution in the normal human amygdala and decreases in subjects with schizophrenia, including not only the lateral nucleus but also the basal, accessory basal, cortical, and medial amygdala nuclei [55] (Figure 2). PNN reduction in this latter nucleus is of particular interest, as it suggests that GABAergic projection neurons are also affected by PNN abnormalities. Notably, PNN decreases were not accompanied by neuron number reductions [42, 43], pointing to actual loss, or altered neurochemical composition, of PNNs. Lower densities of WFA-labeled PNNs were also detected in layers III and V of the prefrontal cortex of subjects with schizophrenia [56]. Interestingly, the visual cortex did not show similar changes [56], suggesting that while being widespread PNN decreases may spare brain regions that are not heavily involved in the pathology of schizophrenia.
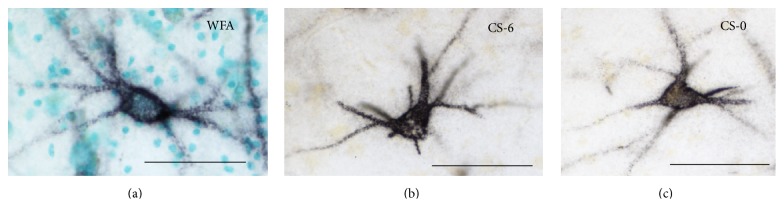
Figure 1.
PNNs in the human amygdala. (a) PNN labeled with wisteria floribunda agglutinin (WFA) lectin, which binds to N-acetyl-galactosamine on the terminal end of chondroitin sulfate chains. (b) PNN immunolabeled using the mAB antibody 3B3 against native chondroitin sulfate motifs specific for chondroitin-6-sulfate (CS-6). 3B3-immunolabeled PNNs are more numerous and show a much broader distribution in the human amygdala with respect to those labeled with WFA. (c) PNN immunolabeled with mAB antibody 1B5, raised against nonsulfated chondroitin sulfate (CS-0) (3B3 and 1B5 are a generous gift from Dr. Bruce Caterson, University of Cardiff, UK). Scale bar = 50 μm.
Figure 2.
Decreased CS-6 in the amygdala of subjects with schizophrenia. In the amygdala of control subjects, CS-6(3B3)-labeled PNNs and glial cell clusters are distributed in the lateral (LN), basal (BN), accessory basal (AB), and corticomedial (CO-Me) nuclei (a, b). In subjects with schizophrenia, marked decreases of PNNs and glia cell clusters immunolabeled for CS-6(3B3) were observed in the amygdala of (c, d) [55]. ECx: entorhinal cortex. HP: hippocampus.
In addition to CSPG-labeled PNN decreases, markedly altered CSPG expression in schizophrenia was also detected in glial cells and “glial clusters” in the amygdala, as well as in olfactory receptor neurons in the olfactory epithelium [42, 55, 57]. In parallel to PNN-related findings, these changes did not appear to depend on altered cell numbers and did not depend on disease-related confounding factors such as exposure to pharmacological treatment, substance abuse, onset and duration of the illness, and so forth, further supporting the idea that altered CSPG expression in schizophrenia may represent a core feature of this disorder [42, 55, 57].
Further support for CSPG involvement in schizophrenia comes from molecular dissection of the neuregulin-ErbB4 pathway, which revealed an association with a genetic polymorphism in PTPRZ1, the gene encoding for receptor phosphotyrosine phosphatase beta/zeta (RPTPbeta) with schizophrenia [58]. RPTPbeta is a transmembrane CSPG shown to play a role in synaptic plasticity and learning [59–63]. Increased mRNA expression of PTPRZ1 has been reported in the amygdala and prefrontal cortex of subjects with schizophrenia [39, 42]. Genetic studies have further identified associations of schizophrenia with the genes encoding for the CSPGs neurocan (NCAN) and neuroglycan-C [64, 65], suggesting that abnormal CSPG expression in schizophrenia may be due, at least in part, to genetic factors.
2.1.2. Reelin
The glycoprotein Reelin is arguably one of the ECM molecules most extensively investigated in schizophrenia and other psychiatric disorders. In subjects with schizophrenia, it has been widely reported to be decreased in a number of cortical areas [66–70]. Several studies have shown that Reelin expression is reduced concurrently with GAD67, one of the main synthetic enzymes for GABA, in cortical GABAergic interneurons, and that these changes may be the consequence of an epigenetic hypermethylation of RELN and GAD67 promoters in these interneurons [70–74]. Notably, Reelin expression was found to be decreased in interstitial white matter neurons, in a study that also confirmed increased density of these neurons in schizophrenia [75, 76]. Together, these studies elegantly link a disruption of Reelin expression in GABAergic neurons to dendritic spine loss and altered neuronal migration in schizophrenia.
2.1.3. Semaphorins
Members of the semaphorin family, and semaphorin 3a in particular, have also been shown to be altered in schizophrenia, potentially in conjunction with Reelin [66, 77]. In particular, increased semaphorin 3A and decreased Reelin expression were detected in the cerebellum of subjects with schizophrenia, while altered expression of multiple members of the semaphorin family was observed in the prefrontal cortex [66]. Genetic polymorphisms of genes encoding for semaphorin 3D and semaphorin receptor plexin A2 have also been associated with schizophrenia ([78, 79], but see also [80]).
2.1.4. Integrins
Integrins, a family of heterodimeric cell adhesion molecules (CAMs) consisting of several different α- and β-subunits, interact with ECM molecules to carry out a multitude of developmental and adult brain functions. Support for the idea that integrins may be implicated in the pathology of schizophrenia comes in part from genetic studies pointing to association of this disorder with a number of integrin gene variants, such as SNPs in the ITGA8 and ITGB3 genes [81, 82]. Additional evidence supporting the involvement of integrins in schizophrenia includes increased expression of integrin α(IIb) and β(IIIa) in first episode subjects with schizophrenia and, notably, abnormal cell adhesion in cultures from olfactory mucosa biopsies from patients with this disorder, which was ameliorated by antibodies blocking integrins [83, 84].
2.1.5. Matrix Metalloproteases
Proteolytic ECM remodeling, shown to play a key role in synaptic plasticity, is mediated by matrix metalloproteases (MMPs), “a disintegrin and metalloproteases” (ADAMs), and “a disintegrin and metalloproteases with a thrombospondin motif” (ADAMTS), through their substrates, such as CAMs, CSPGs, and ECM receptors [85–89]. Several of these enzymes have been implicated in the pathophysiology of schizophrenia. Elevated levels of MMP-9, and “tissue inhibitor of metalloproteinases 1” (TIMP-1) which blocks MMP-9 activity, were reported in blood samples from subjects with this disorder [90, 91]. Increased MMP-9 blood serum levels were also identified in treatment resistant patients [92]. A recent gene expression profiling study of the superior temporal gyrus showed altered mRNA expression of MMPs and ADAMTSs in schizophrenia, including MMP-16 [93]. The possibility that genetic vulnerability may contribute to altered expression of matrix metalloproteases in schizophrenia is supported by converging results from several recent genetic association and genome-wide association studies showing that gene variants encoding for a number of these enzymes, including ADAMTSL3, ADAMTS12, ADAMTS16, ADAM22, and MMP-16, may be associated with this disorder [94–98].
2.1.6. Evidence for ECM Abnormalities from Animal Model Studies
Consistent with human studies, animal models provide evidence that abnormalities affecting the ECM, and CSPGs in particular, may contribute to the pathophysiology of schizophrenia. Transgenic mice overexpressing PTPRZ1 show numerous anatomical and behavioral abnormalities also observed in this disorder, including delayed oligodendrocyte maturation, working memory deficits, and altered glutamatergic, dopaminergic, and GABAergic activity [39]. Experimentally induced enzymatic PNN digestion in the mouse hippocampus mimics several functional abnormalities, including increased activity of dopamine neurons in the ventral tegmental area, which is suspected to occur in schizophrenia [40]. Finally, a rodent model for oxidative stress in schizophrenia showed that PNNs protect neurons expressing PVB from oxidative stress, while at the same time they are vulnerable to it [41]. Thus, loss of PNNs may render these neurons more susceptible to the excitotoxic effects of oxidative stress believed to occur in schizophrenia [99–101].
2.2. Synaptic Pathology in Schizophrenia
Solid and growing evidence shows that disruption of synaptic functions represents a core component of the pathology of schizophrenia. Altered synaptic transmission of key CNS neurotransmitters, including glutamate and GABA, altered expression of synaptic molecules, and loss of dendritic spines have been consistently observed in schizophrenia [16, 102–111]. These interlinked components are briefly reviewed below and placed in the context of ECM/PNN abnormalities.
2.2.1. Glutamatergic Synaptic Signaling and GABAergic Inhibitory Neurons
Several neurotransmitter systems have been implicated in the pathophysiology of schizophrenia. For the purpose of this review, we focus on the involvement of glutamatergic transmission and GABAergic inhibitory neurons in schizophrenia and discuss the potential contribution of ECM/PNN pathology to abnormalities affecting these systems. Importantly, abnormalities affecting these neurotransmitters are closely linked to one another. For instance, GABAergic interneurons powerfully regulate intrinsic information processing and glutamatergic efferents (e.g., [112–115]). Conversely, these interneurons are particularly sensitive to glutamate NMDA receptor hypofunction [116, 117].
Abnormalities affecting the GABAergic system have been consistently reported in several brain regions in schizophrenia [115, 118–129]. These include decreases of inhibitory neurons, loss of GABAergic terminals, and expression of glutamatergic receptors on distinct populations of GABAergic interneurons [115, 130, 131]. The regulation of glutamatergic inputs to these neurons, and PVB-positive neurons in particular, has been a specific focus of attention in schizophrenia, as these inputs play a key role in controlling synchronous oscillations at gamma band frequencies, known to be affected in schizophrenia, and are critical to information processing in cortical circuits involved in this disorder [122, 126, 132, 133].
Altered expression of NMDA and, perhaps to a lesser extent, AMPA receptor proteins has been reported in subjects with schizophrenia, pointing to a disruption of synaptic glutamate signaling networks in this disorder [134–142]. In addition, and perhaps more consistently, the expression of a large number of glutamate receptor accessory proteins, including proteins associated with the postsynaptic density, is altered in several brain regions in people with schizophrenia (for review see [141]). Converging evidence from postmortem, genetic, and animal models also points to abnormal expression of the NMDA receptor coagonists, D-serine and glycine, and the endogenous glycine modulatory site antagonist kynurenic acid [143–150]. This well-replicated finding resonates with intriguing evidence for ECM-mediated modulation of the NMDA receptor glycine site [151].
2.3. Potential Contribution of ECM Abnormalities to Synaptic Glutamatergic Transmission on GABAergic Neurons
PNNs tightly surround synaptic contacts on the somata, dendrites, and proximal axon segment of distinct populations of neurons. These consist of several GABAergic interneuron populations, including, but not limited to, those expressing PVB or somatostatin, and GABAergic projection neurons such as those in the reticular nucleus of the thalamus, the central nucleus of the amygdala, and Purkinje cells in the cerebellum [2, 48, 153–158]. A subset of excitatory corticocortical pyramidal cells and spinal cord motor neurons have also been found to bear PNNs [159]. It is likely that the range of neuronal populations associated with PNNs has not yet been fully accounted for, particularly as the molecular and structural heterogeneity of these ECM structures is still not well understood. For instance, in the human amygdala, a small population of WFA-labeled PNNs ensheathes neurons lacking expression of glutamic acid decarboxylase (GAD) and thus likely represented excitatory neurons (unpublished results; Figure 3). In addition, we recently reported that PNNs labeled with an antibody (3B3) targeting a native chondroitin-6-sulfate motif are far more numerous and widely distributed than those labeled with the lectin wisteria floribunda agglutinin (WFA) and well represented in amygdalar nuclei virtually devoid of PVB-positive neurons [55]. Therefore, abnormalities affecting PNNs may potentially impact a broad variety of inhibitory, as well as excitatory, neuronal populations. Converging evidence suggests that, in schizophrenia, ECM/PNN components known to regulate glutamatergic and GABAergic inputs on GABAergic neurons are abnormal, potentially contributing to intrinsic information processing and activity outflow.
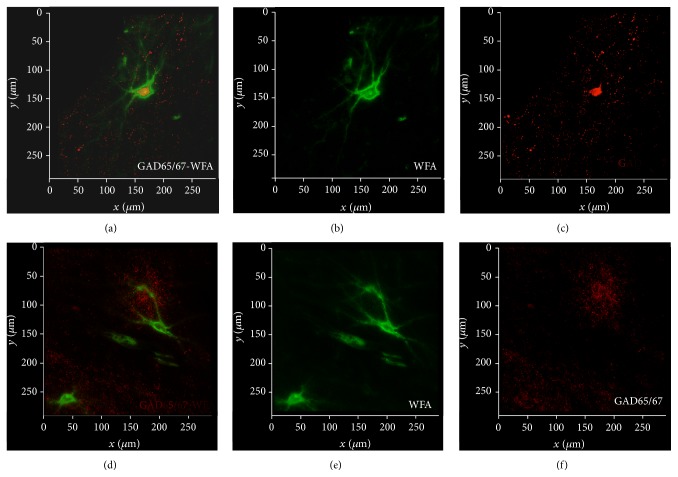
Figure 3.
PNNs are associated with heterogeneous neuronal populations. Confocal micrographs depicting WFA-labeled PNNs surrounding GABAergic neurons expressing GAD65/67 in the healthy human amygdala (a–c). Consistently, WFA-labeled PNNs have been shown to be typically associated with neurons expressing parvalbumin. However, we have previously reported that a small subpopulation of these PNNs ensheathes parvalbumin-negative neurons [152]. Preliminary findings shown in (d)–(f) suggest that these neurons do not express GAD65/67 and may therefore correspond to excitatory neurons.
2.4. Regulation of Glutamatergic and GABA Synapses by PNNs and Perisynaptic ECM Condensations
Growing evidence points to a key role played by PNNs in synaptic regulation, particularly of glutamatergic synapses (for extensive reviews see [11, 12, 38, 160, 161]). In particular, ECM/PNNs affect the diffusion of glutamate receptors laterally within the plasma membrane, as well as receptor clustering within the synapse, thus controlling a fundamental mechanism of synaptic regulation and plasticity [162, 163]. It is thought that this key PNN function may be accomplished by a combination of passive and active mechanisms [160, 162]. Although less is currently known with regard to PNN regulation of GABAergic inputs, a recent study reported that PNN enzymatic digestion increases the number of inhibitory synapses on PVB-positive interneurons [164]. We briefly describe below some examples according to their potential relevance to schizophrenia. We suggest that, in schizophrenia, concurrent disruption of CSPG expression and molecular families interacting with PNN components may contribute synergistically to glutamatergic synapse dysregulation on neurons associated with PNNs.
2.4.1. PNNs as a Passive Barrier
Highly viscous CSPGs, and other ECM/PNN components, form an effective passive diffusion barrier, controlling the lateral diffusion exchanges of AMPA receptors between the synaptic and extrasynaptic compartments [162]. By restricting the lateral diffusion of AMPA receptors from the extrasynaptic space to the synapse, PNNs allow synaptic desensitization during high frequency firing [160, 162, 165]. Consistent with this function, PNN enzymatic digestion results in increased excitability of interneurons [166]. In pathological states, such as schizophrenia, PNN disruption may result in unregulated lateral membrane diffusion of AMPA receptors, thus impacting excitatory synaptic activation and resembling a more “juvenile” state of synaptic regulation.
2.4.2. Chondroitin Sulfate Proteoglycans
CSPGs are key contributors to the composition of PNNs [167–169] and are also found in other structures described as perisynaptic coats [154, 170–174]. An increasing number of studies show that these molecules are critically involved in the regulation of synaptic plasticity. For example, electrophysiological recordings from in vitro mouse hippocampal slices treated with chABC to remove CSPGs show a twofold decrease in long term potentiation (LTP) but not in short term plasticity [175]. A similar decrease of LTP was also observed in mice lacking a key PNN component, tenascin-R, suggesting that CSPG regulation of long term synaptic plasticity occurs through modulation of PNN composition [175].
Studies focused on specific CSPG molecules and CS-sulfation reveal a complex role in developmental and adult regulation of synaptic plasticity. For example, overexpression of CS-6 sulfation in mice leads to failure to instate an adult form of restricted plasticity, resulting in abnormally persistent synaptic plasticity and reduced PNN formation [176]. In the cortex and hippocampus, expression of the CSPG PTPRZ1 was found to be associated with synaptic remodeling [59–62]. Knockout of PTPRZ1 in mice results in enhanced LTP and deficits in spatial learning exclusively in adults [63]. In contrast, mice overexpressing PTPRZ1 show hippocampal LTP deficits, as well as a number of molecular, anatomical, and behavioral abnormalities reminiscent of those observed in subjects with schizophrenia [39]. Together with the increased expression of PTPRZ1 in subjects with this disorder [39, 42], these findings are consistent with the possibility that increased PTPRZ1 expression may contribute to deficits in synaptic plasticity in schizophrenia. Other CSPGs have also been shown to regulate plasticity. Adult mice deficient for the CSPG brevican display deficits in hippocampal early stage LTP and decreased PNN formation [177], whereas mice deficient for neurocan display decreased late stage LTP but normal PNN formation [178]. Further evidence comes from studies showing that brevican and versican are increased in the hippocampus of rats during memory retrieval in the Morris water maze spatial memory task [179]. Overall, altered expression of CSPGs and CS-sulfation patterns have the potential to contribute to disregulated synaptic plasticity in psychiatric disorders during developmental stages, particularly during critical periods of plasticity, as well as adult regulation of synaptic plasticity.
2.4.3. Reelin
Perhaps one of the most well-replicated findings in the pathophysiology of schizophrenia and, incidentally, autism is a disruption of Reelin expression [66–74, 76]. In the adult brain, Reelin is secreted in the ECM by subpopulations of GABAergic interneurons and takes part in the composition of at least a subpopulation of PNNs [180–182]. Reelin's effects are mediated through its main lipoprotein receptors, apolipoprotein E receptor 2 (ApoER2) and very-low-density lipoprotein receptor (VLDLR) [183, 184], as well as through the CAMs of the integrin family and the Src family kinases [184–188]. Accumulating evidence shows that secreted Reelin powerfully enhances LTP and glutamatergic synaptic transmission by regulating NMDA and AMPA receptors [187, 188]. For instance, Reelin regulates the composition of NMDA receptors, controlling the predominance and/or phosphorylation of the NR2 NMDA receptor subunits, and enhances AMPA responses by increasing the number of AMPA receptors on the postsynaptic membrane [180, 188].
2.4.4. Integrins
Interactions between integrins and ECM/PNN components, including Reelin, thrombospondins, fibrinogen, and others, have been shown to regulate synaptic glutamatergic transmission [160]. Notably, integrin signaling is bidirectional; that is, it can activate intracellular signaling pathways in response to changes in the extracellular environment and impact on cell adhesion in response to intracellular signaling [189]. This may allow integrins to play complex roles in synaptic plasticity, including carrying out structural and functional changes that accompany LTP [189–191]. Integrin-ECM interactions have been shown to regulate AMPA receptor internalization, surface mobility of NMDA receptor subunits, and synaptic dwell time of glycine receptors and their scaffolding molecule gephyrin [151, 192, 193].
2.4.5. Neuronal Activity-Regulated Pentraxin
An intriguing example of interactions between ECM molecules and factors regulating synaptic plasticity is represented by the “neuronal activity-regulated pentraxin” (NARP). NARP is an immediate early gene in which its protein product is secreted in an activity-dependent manner by excitatory terminals onto GABAergic PVB-positive neurons, where it promotes clustering of AMPA receptor subunits [194, 195]. This mechanism regulates homeostatic scaling of excitatory inputs so that increased network activity strengthens the excitatory inputs on PVB-positive interneurons, in turn powerfully inhibiting excitatory projection neurons [195]. PNNs ensheathing PVB-positive neurons are critical to the maintenance of high levels of NARP at excitatory synapses on these neurons [195]. CSPG enzymatic digestion markedly decreased NARP at excitatory synapses on PVB-positive neurons without decreasing the overall NARP expression [195]. In subjects with schizophrenia, marked Narp mRNA decreases were reported in the prefrontal cortex [196], a brain region where PNN decreases were also detected [56]. Although a causal relationship between these two findings has not been established thus far, it is reasonable to postulate that, in conjunction, NARP and PNN decreases may synergistically impact glutamatergic synapses on PVB-positive neurons in schizophrenia.
2.4.6. Matrix Metalloproteases
Secreted extracellular matrix proteases, such as “tissue plasminogen activator” (tPA) and MMPs, affect excitatory transmission. For instance, tPA has been found to play a role in LTP through several mechanisms, including cleavage of the NR1 subunit of the NMDA receptor, resulting in potentiation of NMDA current, and cleavage of proBDNF resulting in availability of mature BDNF [197–200]. Altered levels of tPA have been reported in subjects with schizophrenia [201–203]. Although it is not currently known whether these abnormalities are linked to comorbidities, such as alcoholism, inflammatory, and autoimmune disorders, or metabolic disorders [201–203], these findings support the intriguing possibility that tPA abnormalities may contribute to a disruption of glutamatergic transmission in schizophrenia. Interestingly, the amygdala, where marked PNN decreases were detected in schizophrenia, is particularly enriched in tPA [42, 55, 204–206]. MMP-9 has also been shown to powerfully regulate synaptic plasticity and LTP in particular, a role mediated by 1-containing integrin receptors [207]. Interestingly, MMP-9 is transiently released in response to enhanced neuronal activity and impacts both synaptic potentiation and dendritic spine enlargement in a dependent manner [207, 208]. As discussed above, the possibility that MMP-9, as well as other MMPs with potentially related functions, may represent genetic vulnerabilities in schizophrenia has been gaining evidence in recent times [98, 208–210].
2.5. Loss of Dendritic Spines in Schizophrenia
Marked reductions of dendritic spines have been consistently reported in schizophrenia, encompassing several cortical areas, including prefrontal and auditory cortical areas and the hippocampus [104, 109–111, 211]. In addition, the expression of postsynaptic density (PSD) proteins, such as PSD95 and Homer-1, and associated glutamate signaling pathway proteins has been shown to be altered in subjects with this disorder, as well as with autism spectrum disorders [107, 108]. In support of the idea that these changes reflect a structural loss of dendritic spines, altered expression of molecules involved in the actin cytoskeleton has been reported in subjects with schizophrenia [102, 103, 105].
2.6. Potential Contribution of ECM Abnormalities to Loss of Dendritic Spines
Dendritic spines contain the membrane-associated postsynaptic density (PSD) and its associated network of neurotransmitter receptors and downstream signaling molecules and are supported by a mesh of filamentous F-actin and scaffolding proteins [212–218]. ECM proteins, their surface receptors, and remodeling ECM enzymes play a critical role in regulating dendritic spine plasticity in adulthood (see review by [197]). CAMs, among which integrins are perhaps the most well studied, link the PSD to the actin cytoskeleton on one side and to the ECM and presynaptic terminal on the other side. Through this arrangement, CAMs mediate ECM and PSD signaling, influencing the dendritic spine actin network and thus the spine shape [219–225]. In turn, the spine size has a direct impact on synaptic strength, as larger spines/PSDs containing more numerous glutamate receptors have stronger effects on neuronal excitation and signal transmission [212, 226–232].
Several ECM molecules found to modulate spine formation, size, and stability through ECM receptors are also implicated in the pathology of schizophrenia (see above). CSPGs have been shown to actively stabilize dendritic spines, while their removal by enzymatic digestion results in increased spine motility [233–236]. Reelin promotes spine remodeling, impacting not only spine size and stability, but also the number of synaptic contacts per spine, effects at least in part mediated by its receptor ApoER2 [237–242]. The potential contribution of decreased Reelin expression to dendritic spine decreases in schizophrenia has long been postulated [243, 244]. Semaphorin 3A, a secreted ECM molecule expressed in PNNs, exerts a powerful effect on synapses, possibly through its plexin and neuropilin receptors [38, 197, 245–248]. Finally, and importantly, ECM proteases including tPA and MMPs have been shown to robustly affect dendritic spine stability [197]. tPA decreases spine stability, and its activation increases spine loss [249, 250]. This effect is particularly interesting as it relates to the impact of chronic stress in the amygdala and hippocampus, where tPA knockout decreases stress-induced spine loss [249, 250]. During development, MMPs play a key role in spine formation and maturation [197, 251, 252]. In mature neurons, MMPs, and their interactions with integrins, are required for spine volume changes induced by LTP and LTD [207, 253].
In summary, ECM molecules and their cell surface receptors mediate a broad range of synaptic regulatory functions impacting glutamatergic and GABAergic synapses, inhibitory neurons, and dendritic spine plasticity on excitatory neurons. The expression of several ECM molecules and their receptors involved in these functions has been shown to be altered in subjects with schizophrenia. Overall, these considerations support the hypothesis that ECM/PNN abnormalities in this disorder may disrupt synaptic functions and plasticity, perhaps leading to a dysregulation of inhibitory circuits and synaptic instability. The impact of these abnormalities is likely to be region specific, given the heterogeneous representation of these molecules in cortical and subcortical regions (e.g., [42, 55, 204–206, 254]).
3. ECM Pathology in Autism Spectrum Disorders
Multiple lines of evidence implicate ECM abnormalities in autism spectrum disorders, a heterogeneous group of neurodevelopmental disorders characterized by persistent deficits in social communication and social interaction and restricted, repetitive patterns of behavior, interests, or activities. Synaptic pathology is a well-established core pathological component of these disorders (e.g., [16]). Genetic studies have identified several ECM and related molecules as potential contributors to the etiology of autism. Analysis of six genome-wide association studies (GWAS) on autism implicates a number of ECM and PNN regulating molecules, including the ECM remodeling enzymes ADAMTS3, ADAMTS5, ADAMTS14, ECM molecules RELN, SEM3A, SEM4D, the hyaluronan surface receptor CD44, and OTX2, a transcription factor involved in PNN formation [255–263].
By far the strongest evidence for ECM involvement in the pathophysiology of autism comes from investigations on Reelin. GWAS, several association studies specifically investigating Reelin involvement in autism, and a meta-analysis report point to Reelin as a vulnerability gene for autism [257, 264–272]. Consistent with these findings, altered expression of Reelin and Reelin signaling pathways has been observed in the frontal, parietal, and cerebellar cortices of subjects with autism [273–275]. Reduced Reelin levels have also been shown in blood samples from subjects with this disorder [273]. Finally, the “reeler” mouse, which carries an autosomal recessive mutation in the Reelin gene, displays neurodevelopmental deficits reminiscent of psychiatric disorders including autism [273].
Emerging evidence suggests a role for heparan sulfate proteoglycans (HSPGs) in the pathophysiology of autism. Decreased HSPG expression was reported in the subventricular zone of subjects with autism [276]. Notably, this decrease was associated with increased neurogenesis in comparison to age-matched controls [276]. These findings are in agreement with an animal model of autism, the BTBR T+tf/J mouse, characterized by abnormal social behavior, communication deficits, and repetitive stereotyped behaviors as well as altered heparan sulfate expression in the subventricular zone, smaller amygdala volume, and other neurodevelopmental deficits reminiscent of those detected in autism [277–280]. Mutant mice lacking heparan sulfate show many features reflective of autism, including impaired social interaction, repetitive behavior, and deficits in ultrasonic vocalization [281]. Taken together, decreased heparan sulfate in autism may contribute to neurodevelopmental abnormalities focused on areas of cell proliferation as well as regions involved in memory and emotional processing.
4. ECM Pathology in Fragile-X Syndrome
Fragile-X is a single gene, inherited intellectual disability with predominant autistic symptoms [282–284]. The role that MMP-9 plays in the pathophysiology of this disorder represents a compelling example of interactions between ECM molecules and synaptic pathology in psychiatric disorders. Fragile-X results from transcriptional silencing of the Fmr1 gene, which encodes for the mRNA binding protein “Fragile-X mental retardation protein” (FMRP) (for review see [285]). FMRP controls, in an activity-dependent manner, mRNAs encoding for pre- and postsynaptic proteins, scaffolding proteins, neurotransmitter receptors, and signaling molecules [286, 287]. Decreased FMRP expression results in elevated protein synthesis at the synapse, with loss of regulation by neuronal activity, increase in neuronal excitability, and immature, abnormal spine morphology [285, 288–293]. Converging evidence indicates that the interactions between FMRP and the matrix metalloproteinase MMP-9, known to play a role in dendritic spine plasticity in an activity-dependent manner [192, 294], may be critical to these synaptic abnormalities. Recent findings show that FMRP regulates the transport and translation of MMP-9 mRNA within the synapse: decreased FMRP results in increased MMP-9 [295]. Consistently, increased levels of MMP-9 have been reported in Fragile-X syndrome subjects while pharmacologically induced MMP-9 decrease leads to some degree of clinical improvement [296]. Elevated levels of MMP-9 were reported in the amnionic fluid of subjects who went on to develop autism later in life, including a subset of individuals without Fragile-X syndrome [297]. In parallel, Fmr1 knockout mice present with delayed dendritic spine maturation, increased MMP-9, and Fragile-X associated behaviors [295, 298, 299]. Genetic or pharmacological disruption of MMP-9 expression in these mice rescues many of these abnormalities, including dendritic spine maturation and behavioral deficits [299, 300].
5. ECM Pathology in Rett Syndrome
Rett syndrome is a neurodevelopmental disorder characterized by stereotypical hand movements, language regression, decreased rate of brain growth, autonomic dysfunction, and seizures [301]. Deficits in dendritic spines and synaptic plasticity have been consistently reported in subjects with Rett syndrome and in animal models of this disorder [302–306]. Rett syndrome is caused by a de novo genetic mutation in the X-linked methyl-CpG-binding protein 2 gene (MeCP2) [301, 307, 308]. Increased mRNA for RELN was reported in MeCP2 mutant mice [309]. Furthermore, increased PNN labeling with WFA was observed in the motor cortex of subjects with Rett syndrome [310]. Notably, these changes are opposite to those observed in autism and schizophrenia, suggesting that different patterns of pathological deviations of ECM composition may result in synaptic abnormalities, such as those detected in these disorders.
6. ECM Pathology in Mood Disorders
Mood disorders are a category of psychiatric disorders characterized by a persistent altered emotional state; they include bipolar disorder and major depression. Involvement of ECM molecules, and presence of synaptic pathology, in these disorders has been extensively documented [15, 55, 67, 311–315]. For instance, decreased Reelin expression has been reported in the prefrontal cortex, hippocampus, and cerebellum, as well as in blood, of subjects with bipolar disorder or major depression [311, 313, 316, 317]. Our postmortem studies in bipolar disorder show marked decreased of CS-6(3B3)-immunolabeled PNNs across several nuclei in the amygdala, while more moderate decreases of aggrecan-immunolabeled PNNs were observed in the accessory basal nucleus of the amygdala [55]. Furthermore, similar to schizophrenia and autism, increased levels of MMP-9 have been reported in blood samples from subjects with major depression and young subjects with bipolar disorder in a depressed state [91, 318, 319]. GWAS in bipolar disorder have identified a genetic variant of NCAN, encoding for the CSPG neurocan, as a risk factor for this disorder [314]. Consistently, NCAN gene variants are associated with manic symptoms in human subjects [320], and NCAN knockout in mice results in manic-like behaviors [320].
Intriguingly, some of the most effective treatments for mood disorders impact ECM molecules and PNN composition. For example, chronic treatment with the selective serotonin reuptake inhibitor fluoxetine, effective in treating depression and anxiety, results in decreased numbers of WFA-labeled PNNs in the hippocampus and medial prefrontal cortex of mice, accompanied by increased immature neuronal markers and dendritic spine density on interneurons [321, 322]. Fluoxetine exposure in utero has also been shown to delay the formation of PNNs during adolescence in the amygdala and hippocampus of mice [323]. Lithium, one of the most effective treatments for bipolar disorder, contributes to CSPG digestion [324, 325]. Consistently, numbers of “glial clusters” labeled with a CS-6 specific antibody (CS56), shown to be decreased in the amygdala of subjects with bipolar disorder, showed a positive correlation with lifetime exposure to lithium, raising the possibility that chronic lithium exposure may exert therapeutic effects on CSPG sulfation patterns in bipolar disorder [55].
7. ECM Pathology in Alzheimer's Disease
Alzheimer's disease, an irreversible late life brain disorder that progressively disrupts memory and independent living skills, is associated with dendritic spine loss [326–328]. A key neuropathological feature in Alzheimer's disease is the formation of β-amyloid plaques associated with mutations in the presenilin-1 and presenilin-2 genes [329, 330]. These plaques are generated by cleavage of the amyloid precursor protein (APP) by β-site APP cleaving enzyme-1 (BACE1) [331]. Converging evidence points to a role for HSPGs and CSPGs in the formation of amyloid plaques. Heparan sulfates regulate cleavage of APP by BACE1, and several HSPGs, including syndecan, glypican, and agrin, can be detected within amyloid plaques [332–340]. Notably, syndecan is involved in the formation of dendritic spines [341–344]. Finally, increased expression of HSPGs has been reported in postmortem brain samples from subjects with AD [335–338, 345, 346]. CSPGs, specifically CS-4, CS-6, and nonsulfated CS, have also been reported in β-amyloid plaques [347]. Intriguingly, a splice variant of APP corresponds to the CSPG appican, expressed primarily by astrocytes in the brain [5, 348]. Interestingly, APP cleavage by ADAM10 results in a beneficial form, amyloid-α, and in turn suppresses amyloid-β [349]. Physiologically, ADAM10 and APP are highly concentrated at the PSD site and are involved in the regulation of synaptic plasticity [350], suggesting that disrupted levels of amyloid-α and amyloid-β in Alzheimer's disease may contribute to synaptic deficits. Similarly, MMP-9 has been reported to cleave APP through α-secretase activity, thus promoting the nonamyloidogenic form and functioning as a protective factor from amyloid-β accumulation and subsequent cognitive deficits, accompanied by increased levels of presynaptic proteins [351, 352]. Furthermore, MMP-9 has been shown to degrade extracellular amyloid-β in amyloid plaques, providing further protection against AD pathology [353, 354].
Of relevance to this review, decreased densities of PNNs have been reported in Alzheimer's disease [355]. In particular, decreased WFA-labeled PNNs were observed in the frontal cortex of subjects with Alzheimer's disease, while densities of neurons expressing PVB were not altered [355]. These findings are in agreement with data from our group, showing dramatic decreased numbers and degraded morphology of WFA-labeled PNNs in the entorhinal cortex of Alzheimer's disease patients (Figure 4, unpublished results). Other authors have suggested that aggrecan-containing PNNs may play a protective role against tau pathology in Alzheimer's disease [356].
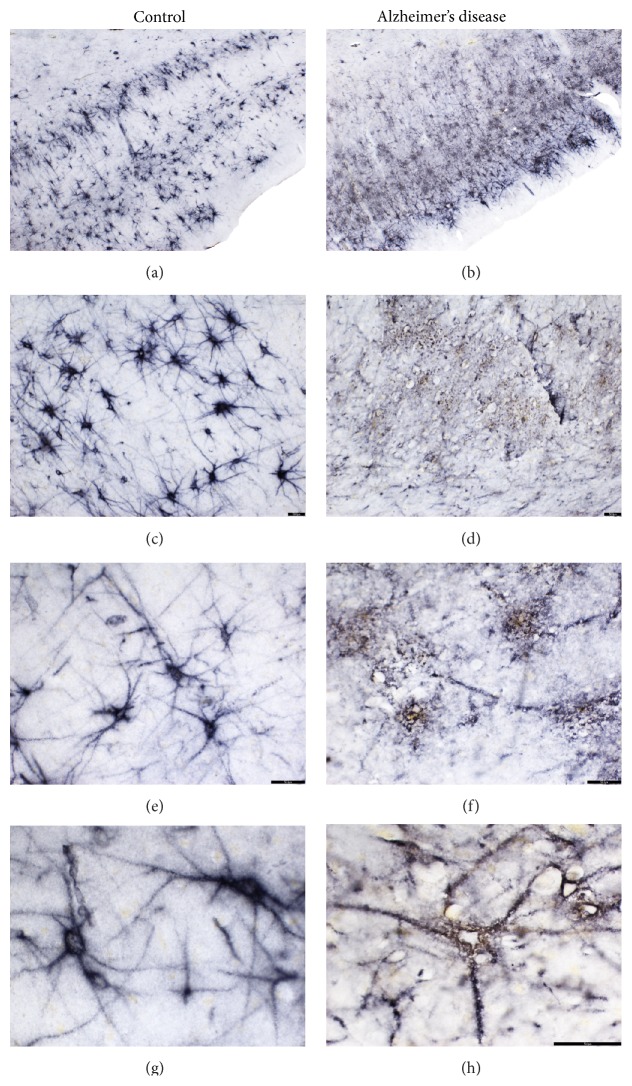
Figure 4.
PNN structure is altered in Alzheimer's disease. Examples of WFA-labeled PNNs in the entorhinal cortex of healthy subjects (a, c, e, g) and subjects with Alzheimer's disorder (b, d, f, h). In healthy subjects, WFA-labeled PNNs are distributed across all layers of the ECx, with preferential concentration in layers II-III and layers V-VI (a). In subjects with Alzheimer's disease, WFA labeling appears to be more loosely distributed, in aggregates throughout the ECx, often suggestive of degraded PNNs (b, d, f, h).
8. ECM Pathology in Epilepsy
Epilepsy encompasses a spectrum of severe to benign brain disorders characterized by disturbances of the normal pattern of neuronal activity, causing unusual emotions, behaviors, sensations, or sometimes loss of consciousness, convulsions, and muscle spasms. Compelling evidence from animal models supports the involvement of the ECM in seizure disorders. The ECM undergoes extensive remodeling in response to seizures, including increased production of CSPGs by glial cells, and cleavage of CSPGs by MMPs [357–362]. As part of such ECM remodeling, PNNs are decreased, at least in part as a consequence to aggrecan cleavage by MMPs [357, 358]. It has been proposed that ECM remodeling may allow for synaptic reorganization, such as it occurs following seizures [36, 363]. Conversely, intriguing evidence suggests that ECM abnormalities may contribute to susceptibility to seizures. For example, enzymatic PNN digestion lowers the threshold for seizure induction [358]. Similarly, inhibition of MMP activity prevents seizure induction and PNN breakdown in an amygdala kindled seizure model [363]. Kainic acid-induced seizures trigger short term CSPG changes followed by more prolonged ones, resulting in altered neurocan and phosphacan levels in limbic brain regions; this latter phase coincides with increases of spontaneous recurrent seizures [357]. In addition, mice lacking the hyaluronan synthesizing enzyme Has3 present with reduced extracellular space and display increased epileptic activity [364]. Further evidence that ECM abnormalities contribute to seizure susceptibility comes from studies on MMP-9. Levels of MMP-9 are increased in blood samples from subjects with epilepsy [365–367]. Mice lacking MMP-9 are less susceptible to induction of seizures, whereas rats overexpressing MMP-9 are more susceptible [368]. MMP-9 has been proposed as a potential therapeutic target for this disorder [365].
It is interesting to note that seizures are often comorbid with several of the disorders discussed above, including autism, schizophrenia, Fragile-X, and Rett syndrome, each presenting with ECM abnormalities. Particularly frequent in these disorders are altered levels of MMP-9 and PNN numbers [369–378]. Given the compelling relationship between ECM molecules and seizures, such comorbidity may not be surprising and, on a speculative level, may point to partially shared mechanisms.
9. Conclusions
The role of PNNs, and more in general ECM, represents an emerging field in the pathophysiology of psychiatric disorders. Evolving in parallel with a growing understanding of the role of the ECM in the regulation of synaptic plasticity, this field is beginning to integrate the concept of the quadripartite synapse in hypotheses on the pathophysiology of synaptic dysregulation in these disorders. Overlapping patterns of ECM abnormalities, in disorders that also share clinical features and synaptic deficits, may underlie common “end-point” mechanisms; that is, anomalies affecting one or more elements of functionally similar molecular families in each of these disorders may lead to convergent effects on synaptic functions and, potentially, clinical domains. Cell and regional specificity may be determined by nonoverlapping pathological aspects in each disorder, as well as by neurodevelopmental determinants specifying the age range at which these anomalies become pathologically relevant.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Berretta S. Extracellular matrix abnormalities in schizophrenia. Neuropharmacology. 2012;62(3):1584–1597. doi: 10.1016/j.neuropharm.2011.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berretta S., Pantazopoulos H., Markota M., Brown C., Batzianouli E. T. Losing the sugar coating: potential impact of perineuronal net abnormalities on interneurons in schizophrenia. Schizophrenia Research. 2015;16(1–3):18–27. doi: 10.1016/j.schres.2014.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bitanihirwe B. K. Y., Woo T.-U. W. Perineuronal nets and schizophrenia: the importance of neuronal coatings. Neuroscience & Biobehavioral Reviews. 2014;45:85–99. doi: 10.1016/j.neubiorev.2014.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Folsom T. D., Fatemi S. H. The involvement of Reelin in neurodevelopmental disorders. Neuropharmacology. 2013;68:122–135. doi: 10.1016/j.neuropharm.2012.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pangalos M. N., Shioi J., Efthimiopoulos S., Wu A., Robakis N. K. Characterization of appican, the chondroitin sulfate proteoglycan form of the Alzheimer amyloid precursor protein. Neurodegeneration. 1996;5(4):445–451. doi: 10.1006/neur.1996.0061. [DOI] [PubMed] [Google Scholar]
- 6.Kato T. A., Watabe M., Kanba S. Neuron-glia interaction as a possible glue to translate the mind-brain gap: a novel multi-dimensional approach toward psychology and psychiatry. Frontiers in Psychiatry. 2013;4, article 139 doi: 10.3389/fpsyt.2013.00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prinz M., Priller J. Microglia and brain macrophages in the molecular age: from origin to neuropsychiatric disease. Nature Reviews Neuroscience. 2014;15(5):300–312. doi: 10.1038/nrn3722. [DOI] [PubMed] [Google Scholar]
- 8.Yamamuro K., Kimoto S., Rosen K. M., Kishimoto T., Makinodan M. Potential primary roles of glial cells in the mechanisms of psychiatric disorders. Frontiers in Cellular Neuroscience. 2015;9, article 154 doi: 10.3389/fncel.2015.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dityatev A., Seidenbecher C. I., Schachner M. Compartmentalization from the outside: the extracellular matrix and functional microdomains in the brain. Trends in Neurosciences. 2010;33(11):503–512. doi: 10.1016/j.tins.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 10.John N., Krügel H., Frischknecht R., et al. Brevican-containing perineuronal nets of extracellular matrix in dissociated hippocampal primary cultures. Molecular and Cellular Neuroscience. 2006;31(4):774–784. doi: 10.1016/j.mcn.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 11.Faissner A., Pyka M., Geissler M., et al. Contributions of astrocytes to synapse formation and maturation—potential functions of the perisynaptic extracellular matrix. Brain Research Reviews. 2010;63(1-2):26–38. doi: 10.1016/j.brainresrev.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Dityatev A., Rusakov D. A. Molecular signals of plasticity at the tetrapartite synapse. Current Opinion in Neurobiology. 2011;21(2):353–359. doi: 10.1016/j.conb.2010.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heikkinen A., Pihlajaniemi T., Faissner A., Yuzaki M. Neural ECM and synaptogenesis. Progress in Brain Research. 2014;214:29–51. doi: 10.1016/B978-0-444-63486-3.00002-5. [DOI] [PubMed] [Google Scholar]
- 14.Smith A. C., Scofield M. D., Kalivas P. W. The tetrapartite synapse: extracellular matrix remodeling contributes to corticoaccumbens plasticity underlying drug addiction. Brain Research. 2015 doi: 10.1016/j.brainres.2015.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams A. J., Umemori H. The best-laid plans go oft awry: synaptogenic growth factor signaling in neuropsychiatric disease. Frontiers in Synaptic Neuroscience. 2014;6, article 4 doi: 10.3389/fnsyn.2014.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Penzes P., Buonanno A., Passafaro M., Sala C., Sweet R. A. Developmental vulnerability of synapses and circuits associated with neuropsychiatric disorders. Journal of Neurochemistry. 2013;126(2):165–182. doi: 10.1111/jnc.12261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernardinelli Y., Nikonenko I., Muller D. Structural plasticity: mechanisms and contribution to developmental psychiatric disorders. Frontiers in Neuroanatomy. 2014;8, article 123 doi: 10.3389/fnana.2014.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rotaru D. C., Lewis D. A., Gonzalez-Burgos G. The role of glutamatergic inputs onto parvalbumin-positive interneurons: relevance for schizophrenia. Reviews in the Neurosciences. 2012;23(1):97–109. doi: 10.1515/revneuro-2011-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duman R. S. Pathophysiology of depression and innovative treatments: remodeling glutamatergic synaptic connections. Dialogues in Clinical Neuroscience. 2014;16(1):11–27. doi: 10.31887/DCNS.2014.16.1/rduman. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu X., Miller E. C., Pozzo-Miller L. Dendritic spine dysgenesis in Rett syndrome. Frontiers in Neuroanatomy. 2014;8, article 97 doi: 10.3389/fnana.2014.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scheff S. W., Neltner J. H., Nelson P. T. Is synaptic loss a unique hallmark of Alzheimer's disease? Biochemical Pharmacology. 2014;88(4):517–528. doi: 10.1016/j.bcp.2013.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tissir F., Goffinet A. M. Reelin and brain development. Nature Reviews Neuroscience. 2003;4(6):496–505. doi: 10.1038/nrn1113. [DOI] [PubMed] [Google Scholar]
- 23.Zimmermann D. R., Dours-Zimmermann M. T. Extracellular matrix of the central nervous system: from neglect to challenge. Histochemistry and Cell Biology. 2008;130(4):635–653. doi: 10.1007/s00418-008-0485-9. [DOI] [PubMed] [Google Scholar]
- 24.Giger R. J., Hollis E. R., II, Tuszynski M. H. Guidance molecules in axon regeneration. Cold Spring Harbor Perspectives in Biology. 2010;2(7) doi: 10.1101/cshperspect.a001867.a001867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maeda N., Fukazawa N., Ishii M. Chondroitin sulfate proteoglycans in neural development and plasticity. Frontiers in Bioscience. 2010;15:626–644. doi: 10.2741/3637. [DOI] [PubMed] [Google Scholar]
- 26.Barros C. S., Franco S. J., Müller U. Extracellular matrix: functions in the nervous system. Cold Spring Harbor perspectives in biology. 2011;3(1) doi: 10.1101/cshperspect.a005108.a005108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Franco S. J., Müller U. Extracellular matrix functions during neuronal migration and lamination in the mammalian central nervous system. Developmental Neurobiology. 2011;71(11):889–900. doi: 10.1002/dneu.20946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kwok J. C. F., Dick G., Wang D., Fawcett J. W. Extracellular matrix and perineuronal nets in CNS repair. Developmental Neurobiology. 2011;71(11):1073–1089. doi: 10.1002/dneu.20974. [DOI] [PubMed] [Google Scholar]
- 29.Sirko S., von Holst A., Wizenmann A., Götz M., Faissner A. Chondroitin sulfate glycosaminoglycans control proliferation, radial glia cell differentiation and neurogenesis in neural stem/progenitor cells. Development. 2007;134(15):2727–2738. doi: 10.1242/dev.02871. [DOI] [PubMed] [Google Scholar]
- 30.Bandtlow C. E., Zimmermann D. R. Proteoglycans in the developing brain: new conceptual insights for old proteins. Physiological Reviews. 2000;80(4):1267–1290. doi: 10.1152/physrev.2000.80.4.1267. [DOI] [PubMed] [Google Scholar]
- 31.Berretta S. Astrocytes in the pathophysiology of schizophrenia: abnormal expression of extracellular matrix molecules. Schizophrenia Research. 2008;102(1–3) supplement 2:p. 11. doi: 10.1016/s0920-9964(08)70038-0. [DOI] [Google Scholar]
- 32.Rhodes K. E., Fawcett J. W. Chondroitin sulphate proteoglycans: preventing plasticity or protecting the CNS? Journal of Anatomy. 2004;204(1):33–48. doi: 10.1111/j.1469-7580.2004.00261.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Syková E. Diffusion properties of the brain in health and disease. Neurochemistry International. 2004;45(4):453–466. doi: 10.1016/j.neuint.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 34.Viapiano M. S., Matthews R. T. From barriers to bridges: chondroitin sulfate proteoglycans in neuropathology. Trends in Molecular Medicine. 2006;12(10):488–496. doi: 10.1016/j.molmed.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 35.Fatemi S. H. Co-occurrence of neurodevelopmental genes in etiopathogenesis of autism and schizophrenia. Schizophrenia Research. 2010;118(1–3):303–304. doi: 10.1016/j.schres.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McRae P. A., Porter B. E. The perineuronal net component of the extracellular matrix in plasticity and epilepsy. Neurochemistry International. 2012;61(7):963–972. doi: 10.1016/j.neuint.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lubbers B. R., Smit A. B., Spijker S., van den Oever M. C. Neural ECM in addiction, schizophrenia, and mood disorder. Progress in Brain Research. 2014;214:263–284. doi: 10.1016/B978-0-444-63486-3.00012-8. [DOI] [PubMed] [Google Scholar]
- 38.Fawcett J. W. Progress in Brain Research. chapter 10. Vol. 218. Elsevier; 2015. The extracellular matrix in plasticity and regeneration after CNS injury and neurodegenerative disease; pp. 213–226. [DOI] [PubMed] [Google Scholar]
- 39.Takahashi N., Sakurai T., Bozdagi-Gunal O., et al. Increased expression of receptor phosphotyrosine phosphatase-β/ζ is associated with molecular, cellular, behavioral and cognitive schizophrenia phenotypes. Translational Psychiatry. 2011;1, article e8 doi: 10.1038/tp.2011.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shah A., Lodge D. J. A loss of hippocampal perineuronal nets produces deficits in dopamine system function: relevance to the positive symptoms of schizophrenia. Translational Psychiatry. 2013;3, article e215 doi: 10.1038/tp.2012.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cabungcal J.-H., Steullet P., Morishita H., et al. Perineuronal nets protect fast-spiking interneurons against oxidative stress. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(22):9130–9135. doi: 10.1073/pnas.1300454110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pantazopoulos H., Woo T.-U. W., Lim M. P., Lange N., Berretta S. Extracellular matrix-glial abnormalities in the amygdala and entorhinal cortex of subjects diagnosed with schizophrenia. Archives of General Psychiatry. 2010;67(2):155–166. doi: 10.1001/archgenpsychiatry.2009.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Berretta S., Pantazopoulos H., Lange N. Neuron numbers and volume of the amygdala in subjects diagnosed with bipolar disorder or schizophrenia. Biological Psychiatry. 2007;62(8):884–893. doi: 10.1016/j.biopsych.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 44.Lavenex P., Amaral D. G. Hippocampal-neocortical interaction: a hierarchy of associativity. Hippocampus. 2000;10(4):420–430. doi: 10.1002/1098-1063(2000)10:460;420::aid-hipo862;3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 45.de Curtis M., Paré D. The rhinal cortices: a wall of inhibition between the neocortex and the hippocampus. Progress in Neurobiology. 2004;74(2):101–110. doi: 10.1016/j.pneurobio.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 46.Prasad K. M. R., Patel A. R., Muddasani S., Sweeney J., Keshavan M. S. The entorhinal cortex in first-episode psychotic disorders: a structural magnetic resonance imaging study. The American Journal of Psychiatry. 2004;161(9):1612–1619. doi: 10.1176/appi.ajp.161.9.1612. [DOI] [PubMed] [Google Scholar]
- 47.Aleman A., Kahn R. S. Strange feelings: do amygdala abnormalities dysregulate the emotional brain in schizophrenia? Progress in Neurobiology. 2005;77(5):283–298. doi: 10.1016/j.pneurobio.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 48.Pantazopoulos H., Lange N., Hassinger L., Berretta S. Subpopulations of neurons expressing parvalbumin in the human amygdala. Journal of Comparative Neurology. 2006;496(5):706–722. doi: 10.1002/cne.20961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hartig W., Brauer K., Bruckner G. Wisteria floribunda agglutinin-labelled nets surround parvalbumin-containing neurons. NeuroReport. 1992;3(10):869–872. doi: 10.1097/00001756-199210000-00012. [DOI] [PubMed] [Google Scholar]
- 50.Celio M. R. Perineuronal nets of extracellular matrix around parvalbumin-containing neurons of the hippocampus. Hippocampus. 1993;3:55–60. [PubMed] [Google Scholar]
- 51.Bruckner G., Seeger G., Brauer K., Hartig W., Kacza J., Bigl V. Cortical areas are revealed by distribution patterns of proteoglycan components and parvalbumin in the Mongolian gerbil and rat. Brain Research. 1994;658(1-2):67–86. doi: 10.1016/s0006-8993(09)90012-9. [DOI] [PubMed] [Google Scholar]
- 52.Härtig W., Brauer K., Bigl V., Brückner G. Chondroitin sulfate proteoglycan-immunoreactivity of lectin-labeled perineuronal nets around parvalbumin-containing neurons. Brain Research. 1994;635(1-2):307–311. doi: 10.1016/0006-8993(94)91452-4. [DOI] [PubMed] [Google Scholar]
- 53.Morris N. P., Henderson Z. Perineuronal nets ensheath fast spiking, parvalbumin-immunoreactive neurons in the medial septum/diagonal band complex. European Journal of Neuroscience. 2000;12(3):828–838. doi: 10.1046/j.1460-9568.2000.00970.x. [DOI] [PubMed] [Google Scholar]
- 54.Vitellaro-Zuccarello L., Meroni A., Amadeo A., De Biasi S. Chondroitin sulfate proteoglycans in the rat thalamus: expression during postnatal development and correlation with calcium-binding proteins in adults. Cell and Tissue Research. 2001;306(1):15–26. doi: 10.1007/s004410100425. [DOI] [PubMed] [Google Scholar]
- 55.Pantazopoulos H., Markota M., Jaquet F., et al. Aggrecan and chondroitin-6-sulfate abnormalities in schizophrenia and bipolar disorder: a postmortem study on the amygdala. Translational Psychiatry. 2015;5(1, article e496) doi: 10.1038/tp.2014.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mauney S. A., Athanas K. M., Pantazopoulos H., et al. Developmental pattern of perineuronal nets in the human prefrontal cortex and their deficit in schizophrenia. Biological Psychiatry. 2013;74(6):427–435. doi: 10.1016/j.biopsych.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pantazopoulos H., Boyer-Boiteau A., Holbrook E. H., et al. Proteoglycan abnormalities in olfactory epithelium tissue from subjects diagnosed with schizophrenia. Schizophrenia Research. 2013;150(2-3):366–372. doi: 10.1016/j.schres.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Buxbaum J. D., Georgieva L., Young J. J., et al. Molecular dissection of NRG1-ERBB4 signaling implicates PTPRZ1 as a potential schizophrenia susceptibility gene. Molecular Psychiatry. 2008;13(2):162–172. doi: 10.1038/sj.mp.4001991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kawachi H., Tamura H., Watakabe I., Shintani T., Maeda N., Noda M. Protein tyrosine phosphatase zeta/RPTPbeta interacts with PSD-95/SAP90 family. Brain Research. Molecular Brain Research. 1999;72(1):47–54. doi: 10.1016/s0169-328x(99)00204-1. [DOI] [PubMed] [Google Scholar]
- 60.Snyder S. E., Li J., Schauwecker P. E., McNeill T. H., Salton S. R. J. Comparison of RPTPζ/β, phosphacan, and trkB mRNA expression in the developing and adult rat nervous system and induction of RPTPζ/β and phosphacan mRNA following brain injury. Molecular Brain Research. 1996;40(1):79–96. doi: 10.1016/0169-328x(96)00039-3. [DOI] [PubMed] [Google Scholar]
- 61.Nishiwaki T., Maeda N., Noda M. Characterization and developmental regulation of proteoglycan-type protein tyrosine phosphatase zeta/RPTPbeta isoforms. Journal of Biochemistry. 1998;123(3):458–467. doi: 10.1093/oxfordjournals.jbchem.a021959. [DOI] [PubMed] [Google Scholar]
- 62.Shintani T., Watanabe E., Maeda N., Noda M. Neurons as well as astrocytes express proteoglycan-type protein tyrosine phosphatase ζ/RPTPβ: analysis of mice in which the PTPζ/RPTPβ gene was replaced with the LacZ gene. Neuroscience Letters. 1998;247(2-3):135–138. doi: 10.1016/s0304-3940(98)00295-x. [DOI] [PubMed] [Google Scholar]
- 63.Niisato K., Fujikawa A., Komai S., et al. Age-dependent enhancement of hippocampal long-term potentiation and impairment of spatial learning through the Rho-associated kinase pathway in protein tyrosine phosphatase receptor type Z-deficient mice. The Journal of Neuroscience. 2005;25(5):1081–1088. doi: 10.1523/jneurosci.2565.04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mühleisen T. W., Mattheisen M., Strohmaier J., et al. Association between schizophrenia and common variation in neurocan (NCAN), a genetic risk factor for bipolar disorder. Schizophrenia Research. 2012;138(1):69–73. doi: 10.1016/j.schres.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 65.Schizophrenia Working Group of the Psychiatric Genomics Consortium. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511(7510):421–427. doi: 10.1038/nature13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eastwood S. L., Law A. J., Everall I. P., Harrison P. J. The axonal chemorepellant semaphorin 3A is increased in the cerebellum in schizophrenia and may contribute to its synaptic pathology. Molecular Psychiatry. 2003;8(2):148–155. doi: 10.1038/sj.mp.4001233. [DOI] [PubMed] [Google Scholar]
- 67.Guidotti A., Auta J., Davis J. M., et al. Decrease in reelin and glutamic acid decarboxylase67 (GAD67) expression in schizophrenia and bipolar disorder: a postmortem brain study. Archives of General Psychiatry. 2000;57(11):1061–1069. doi: 10.1001/archpsyc.57.11.1061. [DOI] [PubMed] [Google Scholar]
- 68.Habl G., Schmitt A., Zink M., et al. Decreased reelin expression in the left prefrontal cortex (BA9) in chronic schizophrenia patients. Neuropsychobiology. 2012;66(1):57–62. doi: 10.1159/000337129. [DOI] [PubMed] [Google Scholar]
- 69.Harvey L., Boksa P. A stereological comparison of GAD67 and reelin expression in the hippocampal stratum oriens of offspring from two mouse models of maternal inflammation during pregnancy. Neuropharmacology. 2012;62(4):1767–1776. doi: 10.1016/j.neuropharm.2011.11.022. [DOI] [PubMed] [Google Scholar]
- 70.Impagnatiello F., Guidotti A. R., Pesold C., et al. A decrease of reelin expression as a putative vulnerability factor in schizophrenia. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(26):15718–15723. doi: 10.1073/pnas.95.26.15718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dong E., Agis-Balboa R. C., Simonini M. V., Grayson D. R., Costa E., Guidotti A. Reelin and glutamic acid decarboxylase67 promoter remodeling in an epigenetic methionine-induced mouse model of schizophrenia. Proceedings of the National Academy of Sciences of the United States of America. 2005;102(35):12578–12583. doi: 10.1073/pnas.0505394102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Abdolmaleky H. M., Cheng K.-H., Russo A., et al. Hypermethylation of the reelin (RELN) promoter in the brain of schizophrenic patients: a preliminary report. American Journal of Medical Genetics B: Neuropsychiatric Genetics. 2005;134(1):60–66. doi: 10.1002/ajmg.b.30140. [DOI] [PubMed] [Google Scholar]
- 73.Guidotti A., Auta J., Chen Y., et al. Epigenetic GABAergic targets in schizophrenia and bipolar disorder. Neuropharmacology. 2011;60(7-8):1007–1016. doi: 10.1016/j.neuropharm.2010.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Guidotti A., Ruzicka W., Grayson D. R., et al. S-adenosyl methionine and DNA methyltransferase-1 mRNA overexpression in psychosis. Neuroreport. 2007;18(1):57–60. doi: 10.1097/wnr.0b013e32800fefd7. [DOI] [PubMed] [Google Scholar]
- 75.Eastwood S. L., Harrison P. J. Interstitial white matter neurons express less reelin and are abnormally distributed in schizophrenia: towards an integration of molecular and morphologic aspects of the neurodevelopmental hypothesis. Molecular Psychiatry. 2003;8(9):821–831. doi: 10.1038/sj.mp.4001371. [DOI] [PubMed] [Google Scholar]
- 76.Akbarian S., Bunney W. E., Jr., Potkin S. G., et al. Altered distribution of nicotinamide-adenine dinucleotide phosphate-diaphorase cells in frontal lobe of schizophrenics implies disturbances of cortical development. Archives of General Psychiatry. 1993;50(3):169–177. doi: 10.1001/archpsyc.1993.01820150007001. [DOI] [PubMed] [Google Scholar]
- 77.Arion D., Horváth S., Lewis D. A., Mirnics K. Infragranular gene expression disturbances in the prefrontal cortex in schizophrenia: signature of altered neural development? Neurobiology of Disease. 2010;37(3):738–746. doi: 10.1016/j.nbd.2009.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fujii T., Uchiyama H., Yamamoto N., et al. Possible association of the semaphorin 3D gene (SEMA3D) with schizophrenia. Journal of Psychiatric Research. 2011;45(1):47–53. doi: 10.1016/j.jpsychires.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 79.Mah S., Nelson M. R., DeLisi L. E., et al. Identification of the semaphorin receptor PLXNA2 as a candidate for susceptibility to schizophrenia. Molecular Psychiatry. 2006;11(5):471–478. doi: 10.1038/sj.mp.4001785. [DOI] [PubMed] [Google Scholar]
- 80.Fujii T., Iijima Y., Kondo H., et al. Failure to confirm an association between the PLXNA2 gene and schizophrenia in a Japanese population. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2007;31(4):873–877. doi: 10.1016/j.pnpbp.2007.01.027. [DOI] [PubMed] [Google Scholar]
- 81.Supriyanto I., Watanabe Y., Mouri K., et al. A missense mutation in the ITGA8 gene, a cell adhesion molecule gene, is associated with schizophrenia in Japanese female patients. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2013;40(1):347–352. doi: 10.1016/j.pnpbp.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 82.Wang K.-S., Liu X., Arana T. B., et al. Genetic association analysis of ITGB3 polymorphisms with age at onset of schizophrenia. Journal of Molecular Neuroscience. 2013;51(2):446–453. doi: 10.1007/s12031-013-0059-8. [DOI] [PubMed] [Google Scholar]
- 83.Fan Y., Abrahamsen G., Mills R., et al. Focal adhesion dynamics are altered in schizophrenia. Biological Psychiatry. 2013;74(6):418–426. doi: 10.1016/j.biopsych.2013.01.020. [DOI] [PubMed] [Google Scholar]
- 84.Walsh M.-T. H., Ryan M., Hillmann A., et al. Elevated expression of integrin alpha(IIb) beta(IIIa) in drug-naive, first-episode schizophrenic patients. Biological Psychiatry. 2002;52(9):874–879. doi: 10.1016/s0006-3223(02)01400-2. [DOI] [PubMed] [Google Scholar]
- 85.Muir E. M., Adcock K. H., Morgenstern D. A., et al. Matrix metalloproteases and their inhibitors are produced by overlapping populations of activated astrocytes. Molecular Brain Research. 2002;100(1-2):103–117. doi: 10.1016/s0169-328x(02)00132-8. [DOI] [PubMed] [Google Scholar]
- 86.Porter S., Clark I. M., Kevorkian L., Edwards D. R. The ADAMTS metalloproteinases. Biochemical Journal. 2005;386(1):15–27. doi: 10.1042/bj20040424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Medina-Flores R., Wang G., Bissel S. J., Murphey-Corb M., Wiley C. A. Destruction of extracellular matrix proteoglycans is pervasive in simian retroviral neuroinfection. Neurobiology of Disease. 2004;16(3):604–616. doi: 10.1016/j.nbd.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 88.Hobohm C., Günther A., Grosche J., Roßner S., Schneider D., Brückner G. Decomposition and long-lasting downregulation of extracellular matrix in perineuronal nets induced by focal cerebral ischemia in rats. Journal of Neuroscience Research. 2005;80(4):539–548. doi: 10.1002/jnr.20459. [DOI] [PubMed] [Google Scholar]
- 89.Bajor M., Kaczmarek L. Proteolytic remodeling of the synaptic cell adhesion molecules (CAMs) by metzincins in synaptic plasticity. Neurochemical Research. 2013;38(6):1113–1121. doi: 10.1007/s11064-012-0919-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Okulski P., Jay T. M., Jaworski J., et al. TIMP-1 abolishes MMP-9-dependent long-lasting long-term potentiation in the prefrontal cortex. Biological Psychiatry. 2007;62(4):359–362. doi: 10.1016/j.biopsych.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 91.Domenici E., Willé D. R., Tozzi F., et al. Plasma protein biomarkers for depression and schizophrenia by multi analyte profiling of case-control collections. PLoS ONE. 2010;5(2) doi: 10.1371/journal.pone.0009166.e9166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yamamori H., Hashimoto R., Ishima T., et al. Plasma levels of mature brain-derived neurotrophic factor (BDNF) and matrix metalloproteinase-9 (MMP-9) in treatment-resistant schizophrenia treated with clozapine. Neuroscience Letters. 2013;556:37–41. doi: 10.1016/j.neulet.2013.09.059. [DOI] [PubMed] [Google Scholar]
- 93.Pietersen C. Y., Mauney S. A., Kim S. S., et al. Molecular profiles of pyramidal neurons in the superior temporal cortex in schizophrenia. Journal of Neurogenetics. 2014;28(1-2):53–69. doi: 10.3109/01677063.2014.882918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dow D. J., Huxley-Jones J., Hall J. M., et al ADAMTSL3 as a candidate gene for schizophrenia: gene sequencing and ultra-high density association analysis by imputation. Schizophrenia Research. 2011;127(1–3):28–34. doi: 10.1016/j.schres.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 95.Bespalova I. N., Angelo G. W., Ritter B. P., et al. Genetic variations in the ADAMTS12 gene are associated with schizophrenia in Puerto Rican patients of Spanish descent. NeuroMolecular Medicine. 2012;14(1):53–64. doi: 10.1007/s12017-012-8169-y. [DOI] [PubMed] [Google Scholar]
- 96.McGrath L. M., Cornelis M. C., Lee P. H., et al. Genetic predictors of risk and resilience in psychiatric disorders: a cross-disorder genome-wide association study of functional impairment in major depressive disorder, bipolar disorder, and schizophrenia. American Journal of Medical Genetics, Part B: Neuropsychiatric Genetics. 2013;162(8):779–788. doi: 10.1002/ajmg.b.32190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ripke S., Sanders A. R., Kendler K. S., et al. Genome-wide association study identifies five new schizophrenia loci. Nature Genetics. 2011;43(10):969–976. doi: 10.1038/ng.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ripke S., Neale B. M., Corvin A., et al. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511(7510):421–427. doi: 10.1038/nature13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Do K. Q., Trabesinger A. H., Kirsten-Krüger M., et al. Schizophrenia: glutathione deficit in cerebrospinal fluid and prefrontal cortex in vivo. European Journal of Neuroscience. 2000;12(10):3721–3728. doi: 10.1046/j.1460-9568.2000.00229.x. [DOI] [PubMed] [Google Scholar]
- 100.Do K. Q., Cuenod M., Hensch T. K. Targeting oxidative stress and aberrant critical period plasticity in the developmental trajectory to schizophrenia. Schizophrenia Bulletin. 2015;41(4):835–846. doi: 10.1093/schbul/sbv065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Steullet P., Cabungcal J., Monin A., et al. Redox dysregulation, neuroinflammation, and NMDA receptor hypofunction: a ‘central hub’ in schizophrenia pathophysiology? Schizophrenia Research. 2014 doi: 10.1016/j.schres.2014.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Datta D., Arion D., Corradi J. P., Lewis D. A. Altered expression of CDC42 signaling pathway components in cortical layer 3 pyramidal cells in schizophrenia. Biological Psychiatry. 2015 doi: 10.1016/j.biopsych.2015.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shelton M. A., Newman J. T., Gu H., et al. Loss of microtubule-associated protein 2 immunoreactivity linked to dendritic spine loss in Schizophrenia. Biological Psychiatry. 2015;78(6):374–385. doi: 10.1016/j.biopsych.2014.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Konopaske G. T., Lange N., Coyle J. T., Benes F. M. Prefrontal cortical dendritic spine pathology in schizophrenia and bipolar disorder. JAMA Psychiatry. 2014;71(12):1323–1331. doi: 10.1001/jamapsychiatry.2014.1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Konopaske G. T., Subburaju S., Coyle J. T., Benes F. M. Altered prefrontal cortical MARCKS and PPP1R9A mRNA expression in schizophrenia and bipolar disorder. Schizophrenia Research. 2015;164(1–3):100–108. doi: 10.1016/j.schres.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Moyer C. E., Shelton M. A., Sweet R. A. Dendritic spine alterations in schizophrenia. Neuroscience Letters. 2015;601:46–53. doi: 10.1016/j.neulet.2014.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.MacDonald M. L., Ding Y., Newman J., et al. Altered glutamate protein co-expression network topology linked to spine loss in the auditory cortex of schizophrenia. Biological Psychiatry. 2015;77(11):959–968. doi: 10.1016/j.biopsych.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.De Bartolomeis A., Latte G., Tomasetti C., Iasevoli F. Glutamatergic postsynaptic density protein dysfunctions in synaptic plasticity and dendritic spines morphology: relevance to schizophrenia and other behavioral disorders pathophysiology, and implications for novel therapeutic approaches. Molecular Neurobiology. 2014;49(1):484–511. doi: 10.1007/s12035-013-8534-3. [DOI] [PubMed] [Google Scholar]
- 109.Glantz L. A., Lewis D. A. Decreased dendritic spine density on prefrontal cortical pyramidal neurons in schizophrenia. Archives of General Psychiatry. 2000;57(1):65–73. doi: 10.1001/archpsyc.57.1.65. [DOI] [PubMed] [Google Scholar]
- 110.Law A. J., Weickert C. S., Hyde T. M., Kleinman J. E., Harrison P. J. Reduced spinophilin but not microtubule-associated protein 2 expression in the hippocampal formation in schizophrenia and mood disorders: molecular evidence for a pathology of dendritic spines. The American Journal of Psychiatry. 2004;161(10):1848–1855. doi: 10.1176/appi.ajp.161.10.1848. [DOI] [PubMed] [Google Scholar]
- 111.Kolomeets N. S., Orlovskaya D. D., Rachmanova V. I., Uranova N. A. Ultrastructural alterations in hippocampal mossy fiber synapses in schizophrenia: a postmortem morphometric study. Synapse. 2005;57(1):47–55. doi: 10.1002/syn.20153. [DOI] [PubMed] [Google Scholar]
- 112.Le Magueresse C., Monyer H. GABAergic interneurons shape the functional maturation of the cortex. Neuron. 2013;77(3):388–405. doi: 10.1016/j.neuron.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 113.Hu H., Gan J., Jonas P. Fast-spiking, parvalbumin+ GABAergic interneurons: from cellular design to microcircuit function. Science. 2014;345(6196) doi: 10.1126/science.1255263.1255263 [DOI] [PubMed] [Google Scholar]
- 114.Kullmann D. M., Moreau A. W., Bakiri Y., Nicholson E. Plasticity of inhibition. Neuron. 2012;75(6):951–962. doi: 10.1016/j.neuron.2012.07.030. [DOI] [PubMed] [Google Scholar]
- 115.Benes F. M., Berretta S. GABAergic interneurons: implications for understanding schizophrenia and bipolar disorder. Neuropsychopharmacology. 2001;25(1):1–27. doi: 10.1016/s0893-133x(01)00225-1. [DOI] [PubMed] [Google Scholar]
- 116.Gonzalez-Burgos G., Lewis D. A. NMDA receptor hypofunction, parvalbumin-positive neurons, and cortical gamma oscillations in schizophrenia. Schizophrenia Bulletin. 2012;38(5):950–957. doi: 10.1093/schbul/sbs010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Coyle J. T., Basu A., Benneyworth M., Balu D., Konopaske G. Handbook of Experimental Pharmacology. Springer; 2012. Glutamatergic synaptic dysregulation in schizophrenia: therapeutic implications; pp. 267–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Akbarian S., Huang H.-S. Molecular and cellular mechanisms of altered GAD1/GAD67 expression in schizophrenia and related disorders. Brain Research Reviews. 2006;52(2):293–304. doi: 10.1016/j.brainresrev.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 119.Akbarian S., Huntsman M. M., Kim J. J., et al. GABAA receptor subunit gene expression in human prefrontal cortex: comparison of schizophrenics and controls. Cerebral Cortex. 1995;5(6):550–560. doi: 10.1093/cercor/5.6.550. [DOI] [PubMed] [Google Scholar]
- 120.Benes F. M. Altered glutamatergic and GABAergic mechanisms in the cingulate cortex of the schizophrenic brain. Archives of General Psychiatry. 1995;52(12):1015–1024. doi: 10.1001/archpsyc.1995.03950240033007. [DOI] [PubMed] [Google Scholar]
- 121.Costa E., Davis J. M., Dong E., et al. A GABAergic cortical deficit dominates schizophrenia pathophysiology. Critical Reviews in Neurobiology. 2004;16(1-2):1–23. doi: 10.1615/critrevneurobiol.v16.i12.10. [DOI] [PubMed] [Google Scholar]
- 122.Glausier J. R., Lewis D. A. Selective pyramidal cell reduction of GABAA receptor α1 subunit messenger RNA expression in schizophrenia. Neuropsychopharmacology. 2011;36(10):2103–2110. doi: 10.1038/npp.2011.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Guidotti A., Auta J., Davis J. M., et al. GABAergic dysfunction in schizophrenia: new treatment strategies on the horizon. Psychopharmacology. 2005;180(2):191–205. doi: 10.1007/s00213-005-2212-8. [DOI] [PubMed] [Google Scholar]
- 124.Hashimoto T., Arion D., Unger T., et al. Alterations in GABA-related transcriptome in the dorsolateral prefrontal cortex of subjects with schizophrenia. Molecular Psychiatry. 2008;13(2):147–161. doi: 10.1038/sj.mp.4002011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kimoto S., Bazmi H. H., Lewis D. A. Lower expression of glutamic acid decarboxylase 67 in the prefrontal cortex in schizophrenia: contribution of altered regulation by Zif268. The American Journal of Psychiatry. 2014;171(9):969–978. doi: 10.1176/appi.ajp.2014.14010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lewis D. A., Hashimoto T., Volk D. W. Cortical inhibitory neurons and schizophrenia. Nature Reviews Neuroscience. 2005;6(4):312–324. doi: 10.1038/nrn1648. [DOI] [PubMed] [Google Scholar]
- 127.Reynolds G. P., Beasley C. L. GABAergic neuronal subtypes in the human frontal cortex—development and deficits in schizophrenia. Journal of Chemical Neuroanatomy. 2001;22(1-2):95–100. doi: 10.1016/s0891-0618(01)00113-2. [DOI] [PubMed] [Google Scholar]
- 128.Simpson M. D. C., Slater P., Deakin J. F. W., Royston M. C., Skan W. J. Reduced GABA uptake sites in the temporal lobe in schizophrenia. Neuroscience Letters. 1989;107(1–3):211–215. doi: 10.1016/0304-3940(89)90819-7. [DOI] [PubMed] [Google Scholar]
- 129.Volk D. W., Austin M. C., Pierri J. N., Sampson A. R., Lewis D. A. GABA transporter-1 mRNA in the prefrontal cortex in schizophrenia: decreased expression in a subset of neurons. American Journal of Psychiatry. 2001;158(2):256–265. doi: 10.1176/appi.ajp.158.2.256. [DOI] [PubMed] [Google Scholar]
- 130.Woo T.-U. W., Shrestha K., Amstrong C., Minns M. M., Walsh J. P., Benes F. M. Differential alterations of kainate receptor subunits in inhibitory interneurons in the anterior cingulate cortex in schizophrenia and bipolar disorder. Schizophrenia Research. 2007;96(1–3):46–61. doi: 10.1016/j.schres.2007.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Woo T.-U. W., Shrestha K., Lamb D., Minns M. M., Benes F. M. N-methyl-D-aspartate receptor and calbindin-containing neurons in the anterior cingulate cortex in schizophrenia and bipolar disorder. Biological Psychiatry. 2008;64(9):803–809. doi: 10.1016/j.biopsych.2008.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gonzalez-Burgos G., Cho R. Y., Lewis D. A. Alterations in cortical network oscillations and parvalbumin neurons in schizophrenia. Biological Psychiatry. 2015;77(12):1031–1040. doi: 10.1016/j.biopsych.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Glausier J. R., Fish K. N., Lewis D. A. Altered parvalbumin basket cell inputs in the dorsolateral prefrontal cortex of schizophrenia subjects. Molecular Psychiatry. 2014;19(1):30–36. doi: 10.1038/mp.2013.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Laruelle M. Schizophrenia: from dopaminergic to glutamatergic interventions. Current Opinion in Pharmacology. 2014;14(1):97–102. doi: 10.1016/j.coph.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 135.Olney J. W., Farber N. B. Glutamate receptor dysfunction and schizophrenia. Archives of General Psychiatry. 1995;52(12):998–1007. doi: 10.1001/archpsyc.1995.03950240016004. [DOI] [PubMed] [Google Scholar]
- 136.Tamminga C. A. Schizophrenia and glutamatergic transmission. Critical Reviews in Neurobiology. 1998;12(1-2):21–36. doi: 10.1615/critrevneurobiol.v12.i1-2.20. [DOI] [PubMed] [Google Scholar]
- 137.Goff D. C., Coyle J. T. The emerging role of glutamate in the pathophysiology and treatment of schizophrenia. The American Journal of Psychiatry. 2001;158(9):1367–1377. doi: 10.1176/appi.ajp.158.9.1367. [DOI] [PubMed] [Google Scholar]
- 138.Coyle J. T. The glutamatergic dysfunction hypothesis for schizophrenia. Harvard Review of Psychiatry. 1996;3(5):241–253. doi: 10.3109/10673229609017192. [DOI] [PubMed] [Google Scholar]
- 139.Coyle J. T. NMDA receptor and schizophrenia: a brief history. Schizophrenia Bulletin. 2012;38(5):920–926. doi: 10.1093/schbul/sbs076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Beneyto M., Kristiansen L. V., Oni-Orisan A., McCullumsmith R. E., Meador-Woodruff J. H. Abnormal glutamate receptor expression in the medial temporal lobe in schizophrenia and mood disorders. Neuropsychopharmacology. 2007;32(9):1888–1902. doi: 10.1038/sj.npp.1301312. [DOI] [PubMed] [Google Scholar]
- 141.Rubio M. D., Drummond J. B., Meador-Woodruff J. H. Glutamate receptor abnormalities in schizophrenia: implications for innovative treatments. Biomolecules & Therapeutics. 2012;20(1):1–18. doi: 10.4062/biomolther.2012.20.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Weickert C. S., Fung S. J., Catts V. S., et al. Molecular evidence of N-methyl-D-aspartate receptor hypofunction in schizophrenia. Molecular Psychiatry. 2013;18(11):1185–1192. doi: 10.1038/mp.2012.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Schwarcz R., Rassoulpour A., Wu H.-Q., Medoff D., Tamminga C. A., Roberts R. C. Increased cortical kynurenate content in schizophrenia. Biological Psychiatry. 2001;50(7):521–530. doi: 10.1016/s0006-3223(01)01078-2. [DOI] [PubMed] [Google Scholar]
- 144.Bendikov I., Nadri C., Amar S., et al. A CSF and postmortem brain study of d-serine metabolic parameters in schizophrenia. Schizophrenia Research. 2007;90(1–3):41–51. doi: 10.1016/j.schres.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 145.Erhardt S., Blennow K., Nordin C., Skogh E., Lindstrom L. H., Engberg G. Kynurenic acid levels are elevated in the cerebrospinal fluid of patients with schizophrenia. Neuroscience Letters. 2001;313:96–98. doi: 10.1016/s0304-3940(01)02242-x. [DOI] [PubMed] [Google Scholar]
- 146.Goltsov A. Y., Loseva J. G., Andreeva T. V., et al. Polymorphism in the 5′-promoter region of serine racemase gene in schizophrenia. Molecular Psychiatry. 2006;11(4):325–326. doi: 10.1038/sj.mp.4001801. [DOI] [PubMed] [Google Scholar]
- 147.Hashimoto K., Engberg G., Shimizu E., Nordin C., Lindström L. H., Iyo M. Reduced D-serine to total serine ratio in the cerebrospinal fluid of drug naive schizophrenic patients. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2005;29(5):767–769. doi: 10.1016/j.pnpbp.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 148.Labrie V., Wang W., Barger S. W., Baker G. B., Roder J. C. Genetic loss of D-amino acid oxidase activity reverses schizophrenia-like phenotypes in mice. Genes, Brain and Behavior. 2010;9(1):11–25. doi: 10.1111/j.1601-183x.2009.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Morita Y., Ujike H., Tanaka Y., et al. A genetic variant of the serine racemase gene is associated with schizophrenia. Biological Psychiatry. 2007;61(10):1200–1203. doi: 10.1016/j.biopsych.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 150.Balu D. T., Coyle J. T. The NMDA receptor ‘glycine modulatory site’ in schizophrenia: D-serine, glycine, and beyond. Current Opinion in Pharmacology. 2015;20:109–115. doi: 10.1016/j.coph.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Charrier C., MacHado P., Tweedie-Cullen R. Y., Rutishauser D., Mansuy I. M., Triller A. A crosstalk between β1 and β3 integrins controls glycine receptor and gephyrin trafficking at synapses. Nature Neuroscience. 2010;13(11):1388–1395. doi: 10.1038/nn.2645. [DOI] [PubMed] [Google Scholar]
- 152.Pantazopoulos H., Lange N., Hassinger L., Berretta S. Subpopulations of neurons expressing parvalbumin in the human amygdala. The Journal of Comparative Neurology. 2006;496(5):706–722. doi: 10.1002/cne.20961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ajmo J. M., Eakin A. K., Hamel M. G., Gottschall P. E. Discordant localization of WFA reactivity and brevican/ADAMTS-derived fragment in rodent brain. BMC Neuroscience. 2008;9, article 14 doi: 10.1186/1471-2202-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Gati G., Lendvai D. The ‘dress’ makes the neuron—different forms of the extracellular matrix in the central nervous system of vertebrates. Orvosi Hetilap. 2013;154(27):1067–1073, 1078–1079. doi: 10.1556/OH.2013.29646. [DOI] [PubMed] [Google Scholar]
- 155.Brückner G., Brauer K., Härtig W., et al. Perineuronal nets provide a polyanionic, glia-associated form of microenvironment around certain neurons in many parts of the rat brain. Glia. 1993;8(3):183–200. doi: 10.1002/glia.440080306. [DOI] [PubMed] [Google Scholar]
- 156.Brauer K., Hartig W., Fritschy J.-M., Bruckner G., Bigl V. Co-occurrence of perineuronal nets with GABA(A) receptor alpha1 subunit-immunoreactive neurones in the rat septal region. NeuroReport. 1995;6(5):733–736. doi: 10.1097/00001756-199503270-00007. [DOI] [PubMed] [Google Scholar]
- 157.Härtig W., Brückner G., Brauer K., Schmidt C., Bigl V. Allocation of perineuronal nets and parvalbumin-, calbindin-D28k- and glutamic acid decarboxylase-immunoreactivity in the amygdala of the rhesus monkey. Brain Research. 1995;698(1-2):265–269. doi: 10.1016/0006-8993(95)01016-O. [DOI] [PubMed] [Google Scholar]
- 158.Seeger G., Brauer K., Härtig W., Brückner G. Mapping of perineuronal nets in the rat brain stained by colloidal iron hydroxide histochemistry and lectin cytochemistry. Neuroscience. 1994;58(2):371–388. doi: 10.1016/0306-4522(94)90044-2. [DOI] [PubMed] [Google Scholar]
- 159.Wegner F., Härtig W., Bringmann A., et al. Diffuse perineuronal nets and modified pyramidal cells immunoreactive for glutamate and the GABA(A) receptor alpha1 subunit form a unique entity in rat cerebral cortex. Experimental Neurology. 2003;184(2):705–714. doi: 10.1016/s0014-4886(03)00313-3. [DOI] [PubMed] [Google Scholar]
- 160.Frischknecht R., Gundelfinger E. D. Synaptic Plasticity. Vol. 970. Berlin, Germany: Springer; 2012. The brain's extracellular matrix and its role in synaptic plasticity; pp. 153–171. (Advances in Experimental Medicine and Biology). [DOI] [PubMed] [Google Scholar]
- 161.Gundelfinger E. D., Frischknecht R., Choquet D., Heine M. Converting juvenile into adult plasticity: a role for the brain's extracellular matrix. European Journal of Neuroscience. 2010;31(12):2156–2165. doi: 10.1111/j.1460-9568.2010.07253.x. [DOI] [PubMed] [Google Scholar]
- 162.Frischknecht R., Heine M., Perrais D., Seidenbecher C. I., Choquet D., Gundelfinger E. D. Brain extracellular matrix affects AMPA receptor lateral mobility and short-term synaptic plasticity. Nature Neuroscience. 2009;12(7):897–904. doi: 10.1038/nn.2338. [DOI] [PubMed] [Google Scholar]
- 163.Fawcett J. Molecular control of brain plasticity and repair. Progress in Brain Research. 2009;175:501–509. doi: 10.1016/s0079-6123(09)17534-9. [DOI] [PubMed] [Google Scholar]
- 164.Donato F., Rompani S. B., Caroni P. Parvalbumin-expressing basket-cell network plasticity induced by experience regulates adult learning. Nature. 2013;504(7479):272–276. doi: 10.1038/nature12866. [DOI] [PubMed] [Google Scholar]
- 165.Heine M., Groc L., Frischknecht R., et al. Surface mobility of postsynaptic AMPARs tunes synaptic transmission. Science. 2008;320(5873):201–205. doi: 10.1126/science.1152089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Dityatev A., Brückner G., Dityateva G., Grosche J., Kleene R., Schachner M. Activity-dependent formation and functions of chondroitin sulfate-rich extracellular matrix of perineuronal nets. Developmental Neurobiology. 2007;67(5):570–588. doi: 10.1002/dneu.20361. [DOI] [PubMed] [Google Scholar]
- 167.Giamanco K. A., Matthews R. T. Deconstructing the perineuronal net: cellular contributions and molecular composition of the neuronal extracellular matrix. Neuroscience. 2012;218:367–384. doi: 10.1016/j.neuroscience.2012.05.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Giamanco K. A., Morawski M., Matthews R. T. Perineuronal net formation and structure in aggrecan knockout mice. Neuroscience. 2010;170(4):1314–1327. doi: 10.1016/j.neuroscience.2010.08.032. [DOI] [PubMed] [Google Scholar]
- 169.Deepa S. S., Carulli D., Galtrey C., et al. Composition of perineuronal net extracellular matrix in rat brain: a different disaccharide composition for the net-associated proteoglycans. The Journal of Biological Chemistry. 2006;281(26):17789–17800. doi: 10.1074/jbc.m600544200. [DOI] [PubMed] [Google Scholar]
- 170.Gaál B., Kecskes S., Matesz C., Birinyi A., Hunyadi A., Rácz É. Molecular composition and expression pattern of the extracellular matrix in a mossy fiber-generating precerebellar nucleus of rat, the prepositus hypoglossi. Neuroscience Letters. 2015;594:122–126. doi: 10.1016/j.neulet.2015.03.056. [DOI] [PubMed] [Google Scholar]
- 171.Jäger C., Lendvai D., Seeger G., et al. Perineuronal and perisynaptic extracellular matrix in the human spinal cord. Neuroscience. 2013;238:168–184. doi: 10.1016/j.neuroscience.2013.02.014. [DOI] [PubMed] [Google Scholar]
- 172.Lendvai D., Morawski M., Négyessy L., et al. Neurochemical mapping of the human hippocampus reveals perisynaptic matrix around functional synapses in Alzheimer's disease. Acta Neuropathologica. 2013;125(2):215–229. doi: 10.1007/s00401-012-1042-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Lendvai D., Morawski M., Brückner G., et al. Perisynaptic aggrecan-based extracellular matrix coats in the human lateral geniculate body devoid of perineuronal nets. Journal of Neuroscience Research. 2012;90(2):376–387. doi: 10.1002/jnr.22761. [DOI] [PubMed] [Google Scholar]
- 174.Gáti G., Morawski M., Lendvai D., et al. Chondroitin sulphate proteoglycan-based perineuronal net establishment is largely activity-independent in chick visual system. Journal of Chemical Neuroanatomy. 2010;40(3):243–247. doi: 10.1016/j.jchemneu.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 175.Bukalo O., Schachner M., Dityatev A. Modification of extracellular matrix by enzymatic removal of chondroitin sulfate and by lack of tenascin-R differentially affects several forms of synaptic plasticity in the hippocampus. Neuroscience. 2001;104(2):359–369. doi: 10.1016/S0306-4522(01)00082-3. [DOI] [PubMed] [Google Scholar]
- 176.Miyata S., Komatsu Y., Yoshimura Y., Taya C., Kitagawa H. Persistent cortical plasticity by upregulation of chondroitin 6-sulfation. Nature Neuroscience. 2012;15(3):414–422. doi: 10.1038/nn.3023. [DOI] [PubMed] [Google Scholar]
- 177.Brakebusch C., Seidenbecher C. I., Asztely F., et al. Brevican-deficient mice display impaired hippocampal CA1 long-term potentiation but show no obvious deficits in learning and memory. Molecular and Cellular Biology. 2002;22(21):7417–7427. doi: 10.1128/mcb.22.21.7417-7427.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Zhou X.-H., Brakebusch C., Matthies H., et al. Neurocan is dispensable for brain development. Molecular and Cellular Biology. 2001;21(17):5970–5978. doi: 10.1128/MCB.21.17.5970-5978.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Saroja S. R., Sase A., Kircher S. G., et al. Hippocampal proteoglycans brevican and versican are linked to spatial memory of Sprague-Dawley rats in the morris water maze. Journal of Neurochemistry. 2014;130(6):797–804. doi: 10.1111/jnc.12783. [DOI] [PubMed] [Google Scholar]
- 180.Campo G. C., Sinagra M., Verrier D., Manzoni O. J., Chavis P. Reelin secreted by GABAergic neurons regulates glutamate receptor homeostasis. PLoS ONE. 2009;4(5) doi: 10.1371/journal.pone.0005505.e5505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Lacor P. N., Grayson D. R., Auta J., Sugaya I., Costa E., Guidotti A. Reelin secretion from glutamatergic neurons in culture is independent from neurotransmitter regulation. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(7):3556–3561. doi: 10.1073/pnas.050589597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Pesold C., Impagnatiello F., Pisu M. O., et al. Reelin is preferentially expressed in neurons synthesizing γ-aminobutyric acid in cortex and hippocampus of adult rats. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(6):3221–3226. doi: 10.1073/pnas.95.6.3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.D'Arcangelo G., Homayouni R., Keshvara L., Rice D. S., Sheldon M., Curran T. Reelin is a ligand for lipoprotein receptors. Neuron. 1999;24(2):471–479. doi: 10.1016/s0896-6273(00)80860-0. [DOI] [PubMed] [Google Scholar]
- 184.Herz J., Chen Y. Reelin, lipoprotein receptors and synaptic plasticity. Nature Reviews Neuroscience. 2006;7(11):850–859. doi: 10.1038/nrn2009. [DOI] [PubMed] [Google Scholar]
- 185.Dulabon L., Olson E. C., Taglienti M. G., et al. Reelin binds α3β1 integrin and inhibits neuronal migration. Neuron. 2000;27(1):33–44. doi: 10.1016/s0896-6273(00)00007-6. [DOI] [PubMed] [Google Scholar]
- 186.Chen Y., Beffert U., Ertunc M., et al. Reelin modulates NMDA receptor activity in cortical neurons. Journal of Neuroscience. 2005;25(36):8209–8216. doi: 10.1523/jneurosci.1951-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Förster E., Bock H. H., Herz J., Chai X., Frotscher M., Zhao S. Emerging topics in Reelin function. European Journal of Neuroscience. 2010;31(9):1511–1518. doi: 10.1111/j.1460-9568.2010.07222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Qiu S., Zhao L. F., Korwek K. M., Weeber E. J. Differential reelin-induced enhancement of NMDA and AMPA receptor activity in the adult hippocampus. Journal of Neuroscience. 2006;26(50):12943–12955. doi: 10.1523/jneurosci.2561-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.McGeachie A. B., Cingolani L. A., Goda Y. A stabilising influence: integrins in regulation of synaptic plasticity. Neuroscience Research. 2011;70(1):24–29. doi: 10.1016/j.neures.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Babayan A. H., Kramár E. A., Barrett R. M., et al. Integrin dynamics produce a delayed stage of long-term potentiation and memory consolidation. The Journal of Neuroscience. 2012;32(37):12854–12861. doi: 10.1523/jneurosci.2024-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Chan C.-S., Chen H., Bradley A., Dragatsis I., Rosenmund C., Davis R. L. α8-integrins are required for hippocampal long-term potentiation but not for hippocampal-dependent learning. Genes, Brain and Behavior. 2010;9(4):402–410. doi: 10.1111/j.1601-183x.2010.00569.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Dityatev A., Schachner M., Sonderegger P. The dual role of the extracellular matrix in synaptic plasticity and homeostasis. Nature Reviews Neuroscience. 2010;11(11):735–746. doi: 10.1038/nrn2898. [DOI] [PubMed] [Google Scholar]
- 193.Pozo K., Goda Y. Unraveling mechanisms of homeostatic synaptic plasticity. Neuron. 2010;66(3):337–351. doi: 10.1016/j.neuron.2010.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Sia G.-M., Béïque J.-C., Rumbaugh G., Cho R., Worley P. F., Huganir R. L. Interaction of the N-terminal domain of the AMPA receptor GluR4 subunit with the neuronal pentraxin NP1 mediates GluR4 synaptic recruitment. Neuron. 2007;55(1):87–102. doi: 10.1016/j.neuron.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 195.Chang M. C., Park J. M., Pelkey K. A., et al. Narp regulates homeostatic scaling of excitatory synapses on parvalbumin-expressing interneurons. Nature Neuroscience. 2010;13(9):1090–1097. doi: 10.1038/nn.2621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Kimoto S., Zaki M. M., Bazmi H. H., Lewis D. A. Altered markers of cortical γ-aminobutyric acid neuronal activity in schizophrenia: role of the NARP gene. JAMA Psychiatry. 2015;72(8):747–756. doi: 10.1001/jamapsychiatry.2015.0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Levy A. D., Omar M. H., Koleske A. J. Extracellular matrix control of dendritic spine and synapse structure and plasticity in adulthood. Frontiers in Neuroanatomy. 2014;8, article 116 doi: 10.3389/fnana.2014.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Madani R., Hulo S., Toni N., et al. Enhanced hippocampal long-term potentiation and learning by increased neuronal expression of tissue-type plasminogen activator in transgenic mice. The EMBO Journal. 1999;18(11):3007–3012. doi: 10.1093/emboj/18.11.3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Nicole O., Docagne F., Ali C., et al. The proteolytic activity of tissue-plasminogen activator enhances NMDA receptor-mediated signaling. Nature Medicine. 2001;7(1):59–64. doi: 10.1038/83358. [DOI] [PubMed] [Google Scholar]
- 200.Pang P. T., Teng H. K., Zaitsev E., et al. Cleavage of proBDNF by tPA/plasmin is essential for long-term hippocampal plasticity. Science. 2004;306(5695):487–491. doi: 10.1126/science.1100135. [DOI] [PubMed] [Google Scholar]
- 201.Hoirisch-Clapauch S., Nardi A. Multiple roles of tissue plasminogen activator in schizophrenia pathophysiology. Seminars in Thrombosis and Hemostasis. 2013;39(8):950–954. doi: 10.1055/s-0033-1357505. [DOI] [PubMed] [Google Scholar]
- 202.Hoirisch-Clapauch S., Nardi A. E. Markers of low activity of tissue plasminogen activator/plasmin are prevalent in schizophrenia patients. Schizophrenia Research. 2014;159(1):118–123. doi: 10.1016/j.schres.2014.08.011. [DOI] [PubMed] [Google Scholar]
- 203.Hoirisch-Clapauch S., Nardi A. E. Low activity of plasminogen activator: a common feature of non-iatrogenic comorbidities of schizophrenia. CNS & Neurological Disorders—Drug Targets. 2015;14(3):325–330. doi: 10.2174/1871527314666150225142705. [DOI] [PubMed] [Google Scholar]
- 204.Sappino A.-P., Madani R., Huarte J., et al. Extracellular proteolysis in the adult murine brain. The Journal of Clinical Investigation. 1993;92(2):679–685. doi: 10.1172/jci116637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Lochner J. E., Honigman L. S., Grant W. F., et al. Activity-dependent release of tissue plasminogen activator from the dendritic spines of hippocampal neurons revealed by live-cell imaging. Journal of Neurobiology. 2006;66(6):564–577. doi: 10.1002/neu.20250. [DOI] [PubMed] [Google Scholar]
- 206.Baranes D., Lederfein D., Huang Y.-Y., Chen M., Bailey C. H., Kandel E. R. Tissue plasminogen activator contributes to the late phase of LTP and to synaptic growth in the hippocampal mossy fiber pathway. Neuron. 1998;21(4):813–825. doi: 10.1016/s0896-6273(00)80597-8. [DOI] [PubMed] [Google Scholar]
- 207.Wang X.-B., Bozdagi O., Nikitczuk J. S., Zu W. Z., Zhou Q., Huntley G. W. Extracellular proteolysis by matrix metalloproteinase-9 drives dendritic spine enlargement and long-term potentiation coordinately. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(49):19520–19525. doi: 10.1073/pnas.0807248105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Lepeta K., Kaczmarek L. Matrix metalloproteinase-9 as a novel player in synaptic plasticity and schizophrenia. Schizophrenia Bulletin. 2015;41(5):1003–1009. doi: 10.1093/schbul/sbv036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Ripke S., O'Dushlaine C., Chambert K., et al. Genome-wide association analysis identifies 13 new risk loci for schizophrenia. Nature Genetics. 2013;45(10):1150–1159. doi: 10.1038/ng.2742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Chopra K., Baveja A., Kuhad A. MMPs: a novel drug target for schizophrenia. Expert Opinion on Therapeutic Targets. 2015;19(1):77–85. doi: 10.1517/14728222.2014.957672. [DOI] [PubMed] [Google Scholar]
- 211.Sweet R. A., Henteleff R. A., Zhang W., Sampson A. R., Lewis D. A. Reduced dendritic spine density in auditory cortex of subjects with schizophrenia. Neuropsychopharmacology. 2009;34(2):374–389. doi: 10.1038/npp.2008.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Harris K. M., Stevens J. K. Dendritic spines of CA1 pyramidal cells in the rat hippocampus: serial electron microscopy with reference to their biophysical characteristics. Journal of Neuroscience. 1989;9(8):2982–2997. doi: 10.1523/JNEUROSCI.09-08-02982.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Kennedy M. B. The biochemistry of synaptic regulation in the central nervous system. Annual Review of Biochemistry. 1994;63:571–600. doi: 10.1146/annurev.bi.63.070194.003035. [DOI] [PubMed] [Google Scholar]
- 214.Kennedy M. B. The postsynaptic density at glutamatergic synapses. Trends in Neurosciences. 1997;20(6):264–268. doi: 10.1016/s0166-2236(96)01033-8. [DOI] [PubMed] [Google Scholar]
- 215.Hunt C. A., Schenker L. J., Kennedy M. B. PSD-95 is associated with the postsynaptic density and not with the presynaptic membrane at forebrain synapses. The Journal of Neuroscience. 1996;16(4):1380–1388. doi: 10.1523/JNEUROSCI.16-04-01380.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Walikonis R. S., Jensen O. N., Mann M., Provance D. W., Jr., Mercer J. A., Kennedy M. B. Identification of proteins in the postsynaptic density fraction by mass spectrometry. The Journal of Neuroscience. 2000;20(11):4069–4080. doi: 10.1523/JNEUROSCI.20-11-04069.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Sheng M., Kim E. The postsynaptic organization of synapses. Cold Spring Harbor Perspectives in Biology. 2011;3(12) doi: 10.1101/cshperspect.a005678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Harris K. M., Weinberg R. J. Ultrastructure of synapses in the mammalian brain. Cold Spring Harbor Perspectives in Biology. 2012;4(5) doi: 10.1101/cshperspect.a005587.a005587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Benson D. L., Huntley G. W. Synapse adhesion: a dynamic equilibrium conferring stability and flexibility. Current Opinion in Neurobiology. 2012;22(3):397–404. doi: 10.1016/j.conb.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Huntley G. W., Gil O., Bozdagi O. The Cadherin family of cell adhesion molecules: multiple roles in synaptic plasticity. Neuroscientist. 2002;8(3):221–233. doi: 10.1177/1073858402008003008. [DOI] [PubMed] [Google Scholar]
- 221.Washbourne P., Dityatev A., Scheiffele P., et al. Cell adhesion molecules in synapse formation. The Journal of Neuroscience. 2004;24(42):9244–9249. doi: 10.1523/jneurosci.3339-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Lin Y. C., Koleske A. J. Mechanisms of synapse and dendrite maintenance and their disruption in psychiatric and neurodegenerative disorders. Annual Review of Neuroscience. 2010;33(1):349–378. doi: 10.1146/annurev-neuro-060909-153204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Cheadle L., Biederer T. The novel synaptogenic protein farp1 links postsynaptic cytoskeletal dynamics and transsynaptic organization. Journal of Cell Biology. 2012;199(6):985–1001. doi: 10.1083/jcb.201205041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Sloniowski S., Ethell I. M. Looking forward to EphB signaling in synapses. Seminars in Cell and Developmental Biology. 2012;23(1):75–82. doi: 10.1016/j.semcdb.2011.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Koleske A. J. Molecular mechanisms of dendrite stability. Nature Reviews Neuroscience. 2013;14(8):536–550. doi: 10.1038/nrn3486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Harris K. M., Stevens J. K. Dendritic spines of rat cerebellar Purkinje cells: serial electron microscopy with reference to their biophysical characteristics. The Journal of Neuroscience. 1988;8(12):4455–4469. doi: 10.1523/JNEUROSCI.08-12-04455.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Matsuzaki M., Ellis-Davies G. C. R., Nemoto T., Miyashita Y., Iino M., Kasai H. Dendritic spine geometry is critical for AMPA receptor expression in hippocampal CA1 pyramidal neurons. Nature Neuroscience. 2001;4(11):1086–1092. doi: 10.1038/nn736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Matsuzaki M., Honkura N., Ellis-Davies G. C. R., Kasai H. Structural basis of long-term potentiation in single dendritic spines. Nature. 2004;429(6993):761–766. doi: 10.1038/nature02617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Nägerl U. V., Eberhorn N., Cambridge S. B., Bonhoeffer T. Bidirectional activity-dependent morphological plasticity in hippocampal neurons. Neuron. 2004;44(5):759–767. doi: 10.1016/j.neuron.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 230.Zhou Q., Homma K. J., Poo M.-M. Shrinkage of dendritic spines associated with long-term depression of hippocampal synapses. Neuron. 2004;44(5):749–757. doi: 10.1016/j.neuron.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 231.Oh W. C., Hill T. C., Zito K. Synapse-specific and size-dependent mechanisms of spine structural plasticity accompanying synaptic weakening. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(4):E305–E312. doi: 10.1073/pnas.1214705110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Bastrikova N., Gardner G. A., Reece J. M., Jeromin A., Dudek S. M. Synapse elimination accompanies functional plasticity in hippocampal neurons. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(8):3123–3127. doi: 10.1073/pnas.0800027105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Pizzorusso T., Medini P., Landi S., Baldini S., Berardi N., Maffei L. Structural and functional recovery from early monocular deprivation in adult rats. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(22):8517–8522. doi: 10.1073/pnas.0602657103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Majewska A., Sur M. Motility of dendritic spines in visual cortex in vivo: changes during the critical period and effects of visual deprivation. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(26):16024–16029. doi: 10.1073/pnas.2636949100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.de Vivo L., Landi S., Panniello M., et al. Extracellular matrix inhibits structural and functional plasticity of dendritic spines in the adult visual cortex. Nature Communications. 2013;4, article 1484 doi: 10.1038/ncomms2491. [DOI] [PubMed] [Google Scholar]
- 236.Orlando C., Ster J., Gerber U., Fawcett J. W., Raineteau O. Perisynaptic chondroitin sulfate proteoglycans restrict structural plasticity in an integrin-dependent manner. The Journal of Neuroscience. 2012;32(50):18009–18017. doi: 10.1523/jneurosci.2406-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Pujadas L., Gruart A., Bosch C., et al. Reelin regulates postnatal neurogenesis and enhances spine hypertrophy and long-term potentiation. Journal of Neuroscience. 2010;30(13):4636–4649. doi: 10.1523/JNEUROSCI.5284-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Beffert U., Weeber E. J., Durudas A., et al. Modulation of synaptic plasticity and memory by Reelin involves differential splicing of the lipoprotein receptor Apoer2. Neuron. 2005;47(4):567–579. doi: 10.1016/j.neuron.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 239.Pribiag H., Peng H., Shah W. A., Stellwagen D., Carbonetto S. Dystroglycan mediates homeostatic synaptic plasticity at GABAergic synapses. Proceedings of the National Academy of Sciences of the United States of America. 2014;111(18):6810–6815. doi: 10.1073/pnas.1321774111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Satz J. S., Ostendorf A. P., Hou S., et al. Distinct functions of glial and neuronal dystroglycan in the developing and adult mouse brain. The Journal of Neuroscience. 2010;30(43):14560–14572. doi: 10.1523/jneurosci.3247-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Beffert U., Durudas A., Weeber E. J., et al. Functional dissection of Reelin signaling by site-directed disruption of disabled-1 adaptor binding to apolipoprotein E receptor 2: distinct roles in development and synaptic plasticity. Journal of Neuroscience. 2006;26(7):2041–2052. doi: 10.1523/jneurosci.4566-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Trotter J. H., Klein M., Jinwal U. K., et al. ApoER2 function in the establishment and maintenance of retinal synaptic connectivity. The Journal of Neuroscience. 2011;31(40):14413–14423. doi: 10.1523/jneurosci.3135-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Costa E., Davis J., Grayson D. R., Guidotti A., Pappas G. D., Pesold C. Dendritic spine hypoplasticity and downregulation of reelin and GABAergic tone in schizophrenia vulnerability. Neurobiology of Disease. 2001;8(5):723–742. doi: 10.1006/nbdi.2001.0436. [DOI] [PubMed] [Google Scholar]
- 244.Eastwood S. L., Harrison P. J. Cellular basis of reduced cortical reelin expression in schizophrenia. The American Journal of Psychiatry. 2006;163(3):540–542. doi: 10.1176/appi.ajp.163.3.540. [DOI] [PubMed] [Google Scholar]
- 245.Uesaka N., Uchigashima M., Mikuni T., et al. Retrograde semaphorin signaling regulates synapse elimination in the developing mouse brain. Science. 2014;344(6187):1020–1023. doi: 10.1126/science.1252514. [DOI] [PubMed] [Google Scholar]
- 246.Carulli D., Foscarin S., Faralli A., Pajaj E., Rossi F. Modulation of semaphorin3A in perineuronal nets during structural plasticity in the adult cerebellum. Molecular and Cellular Neuroscience. 2013;57:10–22. doi: 10.1016/j.mcn.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 247.Dick G., Tan C. L., Alves J. N., et al. Semaphorin 3A binds to the perineuronal nets via chondroitin sulfate type E motifs in rodent brains. The Journal of Biological Chemistry. 2013;288(38):27384–27395. doi: 10.1074/jbc.m111.310029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Vo T., Carulli D., Ehlert E. M. E., et al. The chemorepulsive axon guidance protein semaphorin3A is a constituent of perineuronal nets in the adult rodent brain. Molecular and Cellular Neuroscience. 2013;56:186–200. doi: 10.1016/j.mcn.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 249.Pawlak R., Rao B. S. S., Melchor J. P., Chattarji S., McEwen B., Strickland S. Tissue plasminogen activator and plasminogen mediate stress-induced decline of neuronal and cognitive functions in the mouse hippocampus. Proceedings of the National Academy of Sciences of the United States of America. 2005;102(50):18201–18206. doi: 10.1073/pnas.0509232102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Bennur S., Shankaranarayana Rao B. S., Pawlak R., Strickland S., McEwen B. S., Chattarji S. Stress-induced spine loss in the medial amygdala is mediated by tissue-plasminogen activator. Neuroscience. 2007;144(1):8–16. doi: 10.1016/j.neuroscience.2006.08.075. [DOI] [PubMed] [Google Scholar]
- 251.Michaluk P., Wawrzyniak M., Alot P., et al. Influence of matrix metalloproteinase MMP-9 on dendritic spine morphology. Journal of Cell Science. 2011;124(19):3369–3380. doi: 10.1242/jcs.090852. [DOI] [PubMed] [Google Scholar]
- 252.Bilousova T. V., Rusakov D. A., Ethell D. W., Ethell I. M. Matrix metalloproteinase-7 disrupts dendritic spines in hippocampal neurons through NMDA receptor activation. Journal of Neurochemistry. 2006;97(1):44–56. doi: 10.1111/j.1471-4159.2006.03701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Nagy V., Bozdagi O., Matynia A., et al. Matrix metalloproteinase-9 is required for hippocampal late-phase long-term potentiation and memory. The Journal of Neuroscience. 2006;26(7):1923–1934. doi: 10.1523/jneurosci.4359-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Tsamis K., Mytilinaios D., Psaroulis D., Njau S. N., Costa V., Baloyannis S. J. Reelin immunoreactivity and morphological analysis of the human visual cortex. International Journal of Neuroscience. 2007;117(1):25–46. doi: 10.1080/00207450500535974. [DOI] [PubMed] [Google Scholar]
- 255.Spatazza J., Lee H. H. C., DiNardo A. A., et al. Choroid-plexus-derived otx2 homeoprotein constrains adult cortical plasticity. Cell Reports. 2013;3(6):1815–1823. doi: 10.1016/j.celrep.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Beurdeley M., Spatazza J., Lee H. H. C., et al. Otx2 binding to perineuronal nets persistently regulates plasticity in the mature visual cortex. Journal of Neuroscience. 2012;32(27):9429–9437. doi: 10.1523/jneurosci.0394-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Poelmans G., Franke B., Pauls D. L., Glennon J. C., Buitelaar J. K. AKAPs integrate genetic findings for autism spectrum disorders. Translational Psychiatry. 2013;3, article e270 doi: 10.1038/tp.2013.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Ma D., Salyakina D., Jaworski J. M., et al. A genome-wide association study of autism reveals a common novel risk locus at 5p14.1. Annals of Human Genetics. 2009;73(3):263–273. doi: 10.1111/j.1469-1809.2009.00523.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Wang K., Zhang H., Ma D., et al. Common genetic variants on 5p14.1 associate with autism spectrum disorders. Nature. 2009;459(7246):528–533. doi: 10.1038/nature07999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Weiss L. A., Arking D. E., Daly M. J., Chakravarti A. A genome-wide linkage and association scan reveals novel loci for autism. Nature. 2009;461(7265):802–808. doi: 10.1038/nature08490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Salyakina D., Ma D. Q., Jaworski J. M., et al. Variants in several genomic regions associated with asperger disorder. Autism Research. 2010;3(6):303–310. doi: 10.1002/aur.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Hussman J. P., Chung R.-H., Griswold A. J., et al. A noise-reduction GWAS analysis implicates altered regulation of neurite outgrowth and guidance in Autism. Molecular Autism. 2011;2, article 1 doi: 10.1186/2040-2392-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Anney R., Klei L., Pinto D., et al. A genome-wide scan for common alleles affecting risk for autism. Human Molecular Genetics. 2010;19(20):4072–1082. doi: 10.1093/hmg/ddq307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Persico A. M., D'agruma L., Maiorano N., et al. Reelin gene alleles and haplotypes as a factor predisposing to autistic disorder. Molecular Psychiatry. 2001;6(2):150–159. doi: 10.1038/sj.mp.4000850. [DOI] [PubMed] [Google Scholar]
- 265.Fatemi S. H. The role of Reelin in pathology of autism. Molecular Psychiatry. 2002;7(9):919–920. doi: 10.1038/sj.mp.4001248. [DOI] [PubMed] [Google Scholar]
- 266.Zhang H., Liu X., Zhang C., et al. Reelin gene alleles and susceptibility to autism spectrum disorders. Molecular Psychiatry. 2002;7(9):1012–1017. doi: 10.1038/sj.mp.4001124. [DOI] [PubMed] [Google Scholar]
- 267.Bartlett C. W., Gharani N., Millonig J. H., Brzustowicz L. M. Three autism candidate genes: a synthesis of human genetic analysis with other disciplines. International Journal of Developmental Neuroscience. 2005;23(2-3):221–234. doi: 10.1016/j.ijdevneu.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 268.Skaar D. A., Shao Y., Haines J. L., et al. Analysis of the RELN gene as a genetic risk factor for autism. Molecular Psychiatry. 2005;10(6):563–571. doi: 10.1038/sj.mp.4001614. [DOI] [PubMed] [Google Scholar]
- 269.Serajee F. J., Zhong H., Mahbubul Huq A. H. M. Association of Reelin gene polymorphisms with autism. Genomics. 2006;87(1):75–83. doi: 10.1016/j.ygeno.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 270.Li H., Li Y., Shao J., et al. The association analysis of RELN and GRM8 genes with autistic spectrum disorder in Chinese Han population. American Journal of Medical Genetics, Part B: Neuropsychiatric Genetics. 2008;147(2):194–200. doi: 10.1002/ajmg.b.30584. [DOI] [PubMed] [Google Scholar]
- 271.Li X., Zou H., Brown W. T. Genes associated with autism spectrum disorder. Brain Research Bulletin. 2012;88(6):543–552. doi: 10.1016/j.brainresbull.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 272.Wang Z., Hong Y., Zou L., et al. Reelin gene variants and risk of autism spectrum disorders: an integrated meta-analysis. American Journal of Medical Genetics, Part B: Neuropsychiatric Genetics. 2014;165(2):192–200. doi: 10.1002/ajmg.b.32222. [DOI] [PubMed] [Google Scholar]
- 273.Fatemi S. H., Stary J. M., Halt A. R., Realmuto G. R. Dysregulation of Reelin and Bcl-2 proteins in autistic cerebellum. Journal of Autism and Developmental Disorders. 2001;31(6):529–535. doi: 10.1023/a:1013234708757. [DOI] [PubMed] [Google Scholar]
- 274.Fatemi S. H., Snow A. V., Stary J. M., et al. Reelin signaling is impaired in autism. Biological Psychiatry. 2005;57(7):777–787. doi: 10.1016/j.biopsych.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 275.Fatemi S. H. Reelin glycoprotein in autism and schizophrenia. International Review of Neurobiology. 2005;71:179–187. doi: 10.1016/s0074-7742(05)71008-4. [DOI] [PubMed] [Google Scholar]
- 276.Pearson B. L., Corley M. J., Vasconcellos A., Blanchard D. C., Blanchard R. J. Heparan sulfate deficiency in autistic postmortem brain tissue from the subventricular zone of the lateral ventricles. Behavioural Brain Research. 2013;243(1):138–145. doi: 10.1016/j.bbr.2012.12.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Meyza K. Z., Blanchard D. C., Pearson B. L., Pobbe R. L. H., Blanchard R. J. Fractone-associated N-sulfated heparan sulfate shows reduced quantity in BTBR T+tf/J mice: a strong model of autism. Behavioural Brain Research. 2012;228(2):247–253. doi: 10.1016/j.bbr.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Mercier F., Kwon Y. C., Douet V. Hippocampus/amygdala alterations, loss of heparan sulfates, fractones and ventricle wall reduction in adult BTBR T+ tf/J mice, animal model for autism. Neuroscience Letters. 2012;506(2):208–213. doi: 10.1016/j.neulet.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 279.Schumann C. M., Amaral D. G. Stereological analysis of amygdala neuron number in autism. Journal of Neuroscience. 2006;26(29):7674–7679. doi: 10.1523/jneurosci.1285-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Bauman M., Kemper T. L. Histoanatomic observations of the brain in early infantile autism. Neurology. 1985;35(6):866–874. doi: 10.1212/wnl.35.6.866. [DOI] [PubMed] [Google Scholar]
- 281.Irie F., Badie-Mahdavi H., Yamaguchi Y. Autism-like socio-communicative deficits and stereotypies in mice lacking heparan sulfate. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(13):5052–5056. doi: 10.1073/pnas.1117881109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Gillberg C., Billstedt E. Autism and Asperger syndrome: coexistence with other clinical disorders. Acta Psychiatrica Scandinavica. 2000;102(5):321–330. doi: 10.1034/j.1600-0447.2000.102005321.x. [DOI] [PubMed] [Google Scholar]
- 283.Wahlstrom J., Gillberg C., Gustavson K.-H., Holmgren G. Infantile autism and the fragile X. A Swedish multicenter study. American Journal of Medical Genetics. 1986;23(1-2):403–408. doi: 10.1002/ajmg.1320230132. [DOI] [PubMed] [Google Scholar]
- 284.Gillberg C. Identical triplets with infantile autism and the fragile-X syndrome. British Journal of Psychiatry. 1983;143(3):256–260. doi: 10.1192/bjp.143.3.256. [DOI] [PubMed] [Google Scholar]
- 285.O'Donnell W. T., Warren S. T. A decade of molecular studies of fragile X syndrome. Annual Review of Neuroscience. 2002;25:315–338. doi: 10.1146/annurev.neuro.25.112701.142909. [DOI] [PubMed] [Google Scholar]
- 286.Antar L. N., Afroz R., Dictenberg J. B., Carroll R. C., Bassell G. J. Metabotropic glutamate receptor activation regulates fragile x mental retardation protein and FMR1 mRNA localization differentially in dendrites and at synapses. The Journal of Neuroscience. 2004;24(11):2648–2655. doi: 10.1523/jneurosci.0099-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Darnell J. C., Van Driesche S. J., Zhang C., et al. FMRP stalls ribosomal translocation on mRNAs linked to synaptic function and autism. Cell. 2011;146(2):247–261. doi: 10.1016/j.cell.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Irwin S. A., Galvez R., Greenough W. T. Dendritic spine structural anomalies in fragile-X mental retardation syndrome. Cerebral Cortex. 2000;10(10):1038–1044. doi: 10.1093/cercor/10.10.1038. [DOI] [PubMed] [Google Scholar]
- 289.Irwin S. A., Patel B., Idupulapati M., et al. Abnormal dendritic spine characteristics in the temporal and visual cortices of patients with fragile-X syndrome: a quantitative examination. American Journal of Medical Genetics. 2001;98(2):161–167. doi: 10.1002/1096-8628(20010115)98:238;lt;161::aid-ajmg1025x0003e;3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 290.Lu R., Wang H., Liang Z., et al. The fragile X protein controls microtubule-associated protein 1B translation and microtubule stability in brain neuron development. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(42):15201–15206. doi: 10.1073/pnas.0404995101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Muddashetty R. S., Kelić S., Gross C., Xu M., Bassell G. J. Dysregulated metabotropic glutamate receptor-dependent translation of AMPA receptor and postsynaptic density-95 mRNAs at synapses in a mouse model of fragile X syndrome. The Journal of Neuroscience. 2007;27(20):5338–5348. doi: 10.1523/jneurosci.0937-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Zalfa F., Giorgi M., Primerano B., et al. The Fragile X syndrome protein FMRP associates with BC1 RNA and regulates the translation of specific mRNAs at synapses. Cell. 2003;112(3):317–327. doi: 10.1016/S0092-8674(03)00079-5. [DOI] [PubMed] [Google Scholar]
- 293.Rudelli R. D., Brown W. T., Wisniewski K., Jenkins E. C., Laure-Kamionowska M., Connell F. Adult fragile X syndrome. Clinico-neuropathologic findings. Acta Neuropathologica. 1985;67(3-4):289–295. doi: 10.1007/bf00687814. [DOI] [PubMed] [Google Scholar]
- 294.Michaluk P., Kolodziej L., Mioduszewska B., et al. Beta-dystroglycan as a target for MMP-9, in response to enhanced neuronal activity. The Journal of Biological Chemistry. 2007;282(22):16036–16041. doi: 10.1074/jbc.m700641200. [DOI] [PubMed] [Google Scholar]
- 295.Janusz A., Miłek J., Perycz M., et al. The Fragile X mental retardation protein regulates matrix metalloproteinase 9 mRNA at synapses. Journal of Neuroscience. 2013;33(46):18234–18241. doi: 10.1523/JNEUROSCI.2207-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Dziembowska M., Pretto D. I., Janusz A., et al. High MMP-9 activity levels in fragile X syndrome are lowered by minocycline. American Journal of Medical Genetics Part A. 2013;161(8):1897–1903. doi: 10.1002/ajmg.a.36023. [DOI] [PubMed] [Google Scholar]
- 297.Abdallah M. W., Pearce B. D., Larsen N., et al. Amniotic fluid MMP-9 and neurotrophins in autism spectrum disorders: an exploratory study. Autism Research. 2012;5(6):428–433. doi: 10.1002/aur.1254. [DOI] [PubMed] [Google Scholar]
- 298.Nimchinsky E. A., Oberlander A. M., Svoboda K. Abnormal development of dendritic spines in FMR1 knock-out mice. The Journal of Neuroscience. 2001;21(14):5139–5146. doi: 10.1523/JNEUROSCI.21-14-05139.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Bilousova T. V., Dansie L., Ngo M., et al. Minocycline promotes dendritic spine maturation and improves behavioural performance in the fragile X mouse model. Journal of Medical Genetics. 2009;46(2):94–102. doi: 10.1136/jmg.2008.061796. [DOI] [PubMed] [Google Scholar]
- 300.Sidhu H., Dansie L. E., Hickmott P. W., Ethell D. W., Ethell I. M. Genetic removal of matrix metalloproteinase 9 rescues the symptoms of fragile X syndrome in a mouse model. The Journal of Neuroscience. 2014;34(30):9867–9879. doi: 10.1523/jneurosci.1162-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Chahrour M., Zoghbi H. Y. The story of Rett syndrome: from clinic to neurobiology. Neuron. 2007;56(3):422–437. doi: 10.1016/j.neuron.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 302.Moretti P., Levenson J. M., Battaglia F., et al. Learning and memory and synaptic plasticity are impaired in a mouse model of Rett syndrome. Journal of Neuroscience. 2006;26(1):319–327. doi: 10.1523/JNEUROSCI.2623-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Chapleau C. A., Calfa G. D., Lane M. C., et al. Dendritic spine pathologies in hippocampal pyramidal neurons from Rett syndrome brain and after expression of Rett-associated MECP2 mutations. Neurobiology of Disease. 2009;35(2):219–233. doi: 10.1016/j.nbd.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Weng S.-M., Bailey M. E. S., Cobb S. R. Rett syndrome: from bed to bench. Pediatrics and Neonatology. 2011;52(6):309–316. doi: 10.1016/j.pedneo.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 305.Nguyen M. V. C., Du F., Felice C. A., et al. MeCP2 is critical for maintaining mature neuronal networks and global brain anatomy during late stages of postnatal brain development and in the mature adult brain. The Journal of Neuroscience. 2012;32(29):10021–10034. doi: 10.1523/jneurosci.1316-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Della Sala G., Pizzorusso T. Synaptic plasticity and signaling in Rett syndrome. Developmental Neurobiology. 2014;74(2):178–196. doi: 10.1002/dneu.22114. [DOI] [PubMed] [Google Scholar]
- 307.Amir R. E., Van Den Veyver I. B., Wan M., Tran C. Q., Francke U., Zoghbi H. Y. Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2. Nature Genetics. 1999;23(2):185–188. doi: 10.1038/13810. [DOI] [PubMed] [Google Scholar]
- 308.Colvin L., Leonard H., de Klerk N., et al. Refining the phenotype of common mutations in Rett syndrome. Journal of Medical Genetics. 2004;41(1):25–30. doi: 10.1136/jmg.2003.011130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Jordan C. R., Li H. H., Kwan H. C., Francke U. Cerebellar gene expression profiles of mouse models for Rett syndrome reveal novel MeCP2 targets. BMC Medical Genetics. 2007;8, article 36 doi: 10.1186/1471-2350-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Belichenko P. V., Hagberg B., Dahlström A. Morphological study of neocortical areas in Rett syndrome. Acta Neuropathologica. 1997;93(1):50–61. doi: 10.1007/s004010050582. [DOI] [PubMed] [Google Scholar]
- 311.Fatemi S. H., Earle J. A., McMenomy T. Reduction in Reelin immunoreactivity in hippocampus of subjects with schizophrenia, bipolar disorder and major depression. Molecular Psychiatry. 2000;5(6):654–663. doi: 10.1038/sj.mp.4000783. [DOI] [PubMed] [Google Scholar]
- 312.Fatemi S. H., Stary J. M., Earle J. A., Araghi-Niknam M., Eagan E. GABAergic dysfunction in schizophrenia and mood disorders as reflected by decreased levels of glutamic acid decarboxylase 65 and 67 kDa and Reelin proteins in cerebellum. Schizophrenia Research. 2005;72(2-3):109–122. doi: 10.1016/j.schres.2004.02.017. [DOI] [PubMed] [Google Scholar]
- 313.Fatemi S. H., Kroll J. L., Stary J. M. Altered levels of Reelin and its isoforms in schizophrenia and mood disorders. Neuroreport. 2001;12(15):3209–3215. doi: 10.1097/00001756-200110290-00014. [DOI] [PubMed] [Google Scholar]
- 314.Cichon S., Muhleisen T. W., Degenhardt F. A., et al. Genome-wide association study identifies genetic variation in neurocan as a susceptibility factor for bipolar disorder. The American Journal of Human Genetics. 2011;88(3):372–381. doi: 10.1016/j.ajhg.2011.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Licznerski P., Duman R. S. Remodeling of axo-spinous synapses in the pathophysiology and treatment of depression. Neuroscience. 2013;251:33–50. doi: 10.1016/j.neuroscience.2012.09.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Guidotti A., Pesold C., Costa E. New neurochemical markers for psychosis: a working hypothesis of their operation. Neurochemical Research. 2000;25(9):1207–1218. doi: 10.1023/A:1007635927069. [DOI] [PubMed] [Google Scholar]
- 317.Fatemi S. H. Reelin glycoprotein: structure, biology and roles in health and disease. Molecular Psychiatry. 2005;10(3):251–257. doi: 10.1038/sj.mp.4001613. [DOI] [PubMed] [Google Scholar]
- 318.Rybakowski J. K., Remlinger-Molenda A., Czech-Kucharska A., Wojcicka M., Michalak M., Losy J. Increased serum matrix metalloproteinase-9 (MMP-9) levels in young patients during bipolar depression. Journal of Affective Disorders. 2013;146(2):286–289. doi: 10.1016/j.jad.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 319.Yoshida T., Ishikawa M., Niitsu T., et al. Decreased serum levels of mature brain-derived neurotrophic factor (BDNF), but not its precursor proBDNF, in patients with major depressive disorder. PLoS ONE. 2012;7(8) doi: 10.1371/journal.pone.0042676.e42676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Miró X., Meier S., Dreisow M. L., et al. Studies in humans and mice implicate neurocan in the etiology of mania. The American Journal of Psychiatry. 2012;169(9):982–990. doi: 10.1176/appi.ajp.2012.11101585. [DOI] [PubMed] [Google Scholar]
- 321.Guirado R., Perez-Rando M., Sanchez-Matarredona D., Castrén E., Nacher J. Chronic fluoxetine treatment alters the structure, connectivity and plasticity of cortical interneurons. International Journal of Neuropsychopharmacology. 2014;17:1635–1646. doi: 10.1017/s1461145714000406. [DOI] [PubMed] [Google Scholar]
- 322.Ohira K., Takeuchi R., Iwanaga T., Miyakawa T. Chronic fluoxetine treatment reduces parvalbumin expression and perineuronal nets in gamma-aminobutyric acidergic interneurons of the frontal cortex in adult mice. Molecular Brain. 2013;6(1, article 43) doi: 10.1186/1756-6606-6-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Umemori J., Winkel F., Castrén E., Karpova N. N. Distinct effects of perinatal exposure to fluoxetine or methylmercury on parvalbumin and perineuronal nets, the markers of critical periods in brain development. International Journal of Developmental Neuroscience. 2015;44:55–64. doi: 10.1016/j.ijdevneu.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 324.Yick L.-W., So K.-F., Cheung P.-T., Wu W.-T. Lithium chloride reinforces the regeneration-promoting effect of chondroitinase ABC on rubrospinal neurons after spinal cord injury. Journal of Neurotrauma. 2004;21(7):932–943. doi: 10.1089/0897715041526221. [DOI] [PubMed] [Google Scholar]
- 325.Frederick J. P., Tafari A. T., Wu S.-M., et al. A role for a lithium-inhibited Golgi nucleotidase in skeletal development and sulfation. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(33):11605–11612. doi: 10.1073/pnas.0801182105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Knobloch M., Mansuy I. M. Dendritic spine loss and synaptic alterations in Alzheimer's disease. Molecular Neurobiology. 2008;37(1):73–82. doi: 10.1007/s12035-008-8018-z. [DOI] [PubMed] [Google Scholar]
- 327.Gonatas N. K. Neocortical synapses in a presenile dementia. Journal of Neuropathology and Experimental Neurology. 1967;26(1):150–151. [PubMed] [Google Scholar]
- 328.Terry R. D., Masliah E., Salmon D. P., et al. Physical basis of cognitive alterations in Alzheimer's disease: synapse loss is the major correlate of cognitive impairment. Annals of Neurology. 1991;30(4):572–580. doi: 10.1002/ana.410300410. [DOI] [PubMed] [Google Scholar]
- 329.Scheuner D., Eckman C., Jensen M., et al. Secreted amyloid β-protein similar to that in the senile plaques of Alzheimer's disease is increased in vivo by the presenilin 1 and 2 and APP mutations linked to familial Alzheimer's disease. Nature Medicine. 1996;2(8):864–870. doi: 10.1038/nm0896-864. [DOI] [PubMed] [Google Scholar]
- 330.Hardy J., Selkoe D. J. The amyloid hypothesis of Alzheimer's disease: progress and problems on the road to therapeutics. Science. 2002;297(5580):353–356. doi: 10.1126/science.1072994. [DOI] [PubMed] [Google Scholar]
- 331.Vassar R., Bennett B. D., Babu-Khan S., et al. β-secretase cleavage of Alzheimer's amyloid precursor protein by the transmembrane aspartic protease BACE. Science. 1999;286(5440):735–741. doi: 10.1126/science.286.5440.735. [DOI] [PubMed] [Google Scholar]
- 332.Schwörer R., Zubkova O. V., Turnbull J. E., Tyler P. C. Synthesis of a targeted library of heparan sulfate hexa- to dodecasaccharides as inhibitors of beta-secretase: potential therapeutics for Alzheimer's disease. Chemistry—A European Journal. 2013;19(21):6817–6823. doi: 10.1002/chem.201204519. [DOI] [PubMed] [Google Scholar]
- 333.Patey S. J., Edwards E. A., Yates E. A., Turnbull J. E. Engineered heparins: novel β-secretase inhibitors as potential Alzheimer's disease therapeutics. Neurodegenerative Diseases. 2008;5(3-4):197–199. doi: 10.1159/000113701. [DOI] [PubMed] [Google Scholar]
- 334.Scholefield Z., Yates E. A., Wayne G., Amour A., McDowell W., Turnbull J. E. Heparan sulfate regulates amyloid precursor protein processing by BACE1, the Alzheimer's β-secretase. The Journal of Cell Biology. 2003;163(1):97–107. doi: 10.1083/jcb.200303059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Su J. H., Cummings B. J., Cotman C. W. Localization of heparan sulfate glycosaminoglycan and proteoglycan core protein in aged brain and Alzheimer's disease. Neuroscience. 1992;51(4):801–813. doi: 10.1016/0306-4522(92)90521-3. [DOI] [PubMed] [Google Scholar]
- 336.Snow A. D., Sekiguchi R. T., Nochlin D., Kalaria R. N., Kimata K. Heparan sulfate proteoglycan in diffuse plaques of hippocampus but not of cerebellum in Alzheimer's disease brain. The American Journal of Pathology. 1994;144(2):337–347. [PMC free article] [PubMed] [Google Scholar]
- 337.Watanabe N., Araki W., Chui D.-H., Makifuchi T., Ihara Y., Tabira T. Glypican-1 as an Aβ binding HSPG in the human brain: Its localization in DIG domains and possible roles in the pathogenesis of Alzheimer's disease. The FASEB Journal. 2004;18(9):1013–1015. doi: 10.1096/fj.03-1040fje. [DOI] [PubMed] [Google Scholar]
- 338.Bruinsma I. B., te Riet L., Gevers T., et al. Sulfation of heparan sulfate associated with amyloid-β plaques in patients with Alzheimer's disease. Acta Neuropathologica. 2010;119(2):211–220. doi: 10.1007/s00401-009-0577-1. [DOI] [PubMed] [Google Scholar]
- 339.Leonova E. I., Galzitskaya O. V. Role of syndecan-2 in amyloid plaque formation. Molecular Biology. 2015;49(1):89–98. doi: 10.1134/s0026893315010082. [DOI] [PubMed] [Google Scholar]
- 340.Snow A. D., Mar H., Nochlin D., et al. The presence of heparan sulfate proteoglycans in the neuritic plaques and congophilic angiopathy in Alzheimer's disease. The American Journal of Pathology. 1988;133(3):456–463. [PMC free article] [PubMed] [Google Scholar]
- 341.Lin Y.-L., Lei Y.-T., Hong C.-J., Hsueh Y.-P. Syndecan-2 induces filopodia and dendritic spine formation via the neurofibromin-PKA-Ena/VASP pathway. The Journal of Cell Biology. 2007;177(5):829–841. doi: 10.1083/jcb.200608121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Ethell I. M., Irie F., Kalo M. S., Couchman J. R., Pasquale E. B., Yamaguchi Y. EphB/syndecan-2 signaling in dendritic spine morphogenesis. Neuron. 2001;31(6):1001–1013. doi: 10.1016/S0896-6273(01)00440-8. [DOI] [PubMed] [Google Scholar]
- 343.Ethell I. M., Hagihara K., Miura Y., Irie F., Yamaguchi Y. Synbindin, a novel syndecan-2-binding protein in neuronal dendritic spines. Journal of Cell Biology. 2000;151(1):53–67. doi: 10.1083/jcb.151.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Ethell I. M., Yamaguchi Y. Cell surface heparan sulfate proteoglycan syndecan-2 induces the maturation of dendritic spines in rat hippocampal neurons. Journal of Cell Biology. 1999;144(3):575–586. doi: 10.1083/jcb.144.3.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Verbeek M. M., Otte-Höller I., van den Born J., et al. Agrin is a major heparan sulfate proteoglycan accumulating in Alzheimer's disease brain. The American Journal of Pathology. 1999;155(6):2115–2125. doi: 10.1016/s0002-9440(10)65529-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Lindahl B., Eriksson L., Lindahl U. Structure of heparan sulphate from human brain, with special regard to Alzheimer's disease. Biochemical Journal. 1995;306(part 1):177–184. doi: 10.1042/bj3060177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.DeWitt D. A., Silver J., Canning D. R., Perry G. Chondroitin sulfate proteoglycans are associated with the lesions of Alzheimer's disease. Experimental Neurology. 1993;121(2):149–152. doi: 10.1006/exnr.1993.1081. [DOI] [PubMed] [Google Scholar]
- 348.Pangalos M. N., Shioi J., Robakis N. K. Expression of the chondroitin sulfate proteoglycans of amyloid precursor (appican) and amyloid precursor-like protein 2. Journal of Neurochemistry. 1995;65(2):762–769. doi: 10.1046/j.1471-4159.1995.65020762.x. [DOI] [PubMed] [Google Scholar]
- 349.Marcello E., Saraceno C., Musardo S., et al. Endocytosis of synaptic ADAM10 in neuronal plasticity and Alzheimer's disease. Journal of Clinical Investigation. 2013;123(6):2523–2538. doi: 10.1172/jci65401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Hoe H.-S., Fu Z., Makarova A., et al. The effects of amyloid precursor protein on postsynaptic composition and activity. The Journal of Biological Chemistry. 2009;284(13):8495–8506. doi: 10.1074/jbc.m900141200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Fragkouli A., Tsilibary E. C., Tzinia A. K. Neuroprotective role of MMP-9 overexpression in the brain of Alzheimer's 5xFAD mice. Neurobiology of Disease. 2014;70:179–189. doi: 10.1016/j.nbd.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 352.Fragkouli A., Tzinia A. K., Charalampopoulos I., Gravanis A., Tsilibary E. C. Matrix metalloproteinase-9 participates in NGF-induced α-secretase cleavage of amyloid-β protein precursor in PC12 cells. Journal of Alzheimer's Disease. 2011;24(4):705–719. doi: 10.3233/jad-2011-101893. [DOI] [PubMed] [Google Scholar]
- 353.Backstrom J. R., Lim G. P., Cullen M. J., Tökés Z. A. Matrix metalloproteinase-9 (MMP-9) is synthesized in neurons of the human hippocampus and is capable of degrading the amyloid-beta peptide (1–40) The Journal of Neuroscience. 1996;16(24):7910–7919. doi: 10.1523/JNEUROSCI.16-24-07910.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Yin K.-J., Cirrito J. R., Yan P., et al. Matrix metalloproteinases expressed by astrocytes mediate extracellular amyloid-β peptide catabolism. Journal of Neuroscience. 2006;26(43):10939–10948. doi: 10.1523/jneurosci.2085-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Baig S., Wilcock G. K., Love S. Loss of perineuronal net N-acetylgalactosamine in Alzheimer's disease. Acta Neuropathologica. 2005;110(4):393–401. doi: 10.1007/s00401-005-1060-2. [DOI] [PubMed] [Google Scholar]
- 356.Morawski M., Brückner G., Jäger C., Seeger G., Arendt T. Neurons associated with aggrecan-based perineuronal nets are protected against tau pathology in subcortical regions in Alzheimer's disease. Neuroscience. 2010;169(3):1347–1363. doi: 10.1016/j.neuroscience.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 357.Okamoto M., Sakiyama J., Mori S., et al. Kainic acid-induced convulsions cause prolonged changes in the chondroitin sulfate proteoglycans neurocan and phosphacan in the limbic structures. Experimental Neurology. 2003;184(1):179–195. doi: 10.1016/S0014-4886(03)00251-6. [DOI] [PubMed] [Google Scholar]
- 358.Rankin-Gee E. K., McRae P. A., Baranov E., Rogers S., Wandrey L., Porter B. E. Perineuronal net degradation in epilepsy. Epilepsia. 2015;56(7):1124–1133. doi: 10.1111/epi.13026. [DOI] [PubMed] [Google Scholar]
- 359.Wennström M., Hellsten J., Tingström A. Electroconvulsive seizures induce proliferation of NG2-expressing glial cells in adult rat amygdala. Biological Psychiatry. 2004;55(5):464–471. doi: 10.1016/j.biopsych.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 360.Wennström M., Hellsten J., Ekdahl C. T., Tingström A. Electroconvulsive seizures induce proliferation of NG2-expressing glial cells in adult rat hippocampus. Biological Psychiatry. 2003;54(10):1015–1024. doi: 10.1016/s0006-3223(03)00693-0. [DOI] [PubMed] [Google Scholar]
- 361.Matsui F., Kawashima S., Shuo T., et al. Transient expression of juvenile-type neurocan by reactive astrocytes in adult rat brains injured by kainate-induced seizures as well as surgical incision. Neuroscience. 2002;112(4):773–781. doi: 10.1016/S0306-4522(02)00136-7. [DOI] [PubMed] [Google Scholar]
- 362.Naffah-Mazzacoratti M. G., Porcionatto G. A. A., Scorza F. A., et al. Selective alterations of glycosaminoglycans synthesis and proteoglycan expression in rat cortex and hippocampus in pilocarpine-induced epilepsy. Brain Research Bulletin. 1999;50(4):229–239. doi: 10.1016/S0361-9230(99)00195-1. [DOI] [PubMed] [Google Scholar]
- 363.Pollock E., Everest M., Brown A., Poulter M. O. Metalloproteinase inhibition prevents inhibitory synapse reorganization and seizure genesis. Neurobiology of Disease. 2014;70:21–31. doi: 10.1016/j.nbd.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 364.Arranz A. M., Perkins K. L., Irie F., et al. Hyaluronan deficiency due to Has3 knock-out causes altered neuronal activity and seizures via reduction in brain extracellular space. The Journal of Neuroscience. 2014;34(18):6164–6176. doi: 10.1523/jneurosci.3458-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Yin P., Yang L., Zhou H. Y., Sun R. P. Matrix metalloproteinase-9 may be a potential therapeutic target in epilepsy. Medical Hypotheses. 2011;76(2):184–186. doi: 10.1016/j.mehy.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 366.Konopacki F. A., Rylski M., Wilczek E., et al. Synaptic localization of seizure-induced matrix metalloproteinase-9 mRNA. Neuroscience. 2007;150(1):31–39. doi: 10.1016/j.neuroscience.2007.08.026. [DOI] [PubMed] [Google Scholar]
- 367.Suenaga N., Ichiyama T., Kubota M., Isumi H., Tohyama J., Furukawa S. Roles of matrix metalloproteinase-9 and tissue inhibitors of metalloproteinases 1 in acute encephalopathy following prolonged febrile seizures. Journal of the Neurological Sciences. 2008;266(1-2):126–130. doi: 10.1016/j.jns.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 368.Wilczynski G. M., Konopacki F. A., Wilczek E., et al. Important role of matrix metalloproteinase 9 in epileptogenesis. Journal of Cell Biology. 2008;180(5):1021–1035. doi: 10.1083/jcb.200708213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Cascella N. G., Schretlen D. J., Sawa A. Schizophrenia and epilepsy: is there a shared susceptibility? Neuroscience Research. 2009;63(4):227–235. doi: 10.1016/j.neures.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Gelisse P., Samuelian J.-C., Genton P. Is schizophrenia a risk factor for epilepsy or acute symptomatic seizures? Epilepsia. 1999;40(11):1566–1571. doi: 10.1111/j.1528-1157.1999.tb02041.x. [DOI] [PubMed] [Google Scholar]
- 371.Mendez M. F., Grau R., Doss R. C., Taylor J. L. Schizophrenia in epilepsy: seizure and psychosis variables. Neurology. 1993;43(6):1073–1077. doi: 10.1212/wnl.43.6.1073. [DOI] [PubMed] [Google Scholar]
- 372.Lamprecht F. Epilepsy and schizophrenia: a neurochemical bridge. Journal of Neural Transmission. 1977;40(2):159–170. doi: 10.1007/bf01250566. [DOI] [PubMed] [Google Scholar]
- 373.Brooks-Kayal A. Epilepsy and autism spectrum disorders: are there common developmental mechanisms? Brain and Development. 2010;32(9):731–738. doi: 10.1016/j.braindev.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 374.Tuchman R., Rapin I. Epilepsy in autism. Lancet Neurology. 2002;1(6):352–358. doi: 10.1016/s1474-4422(02)00160-6. [DOI] [PubMed] [Google Scholar]
- 375.Wong V. Epilepsy in children with autistic spectrum disorder. Journal of Child Neurology. 1993;8(4):316–322. doi: 10.1177/088307389300800405. [DOI] [PubMed] [Google Scholar]
- 376.Tuchman R. F., Rapin I., Shinnar S. Autistic and dysphasic children. II: epilepsy. Pediatrics. 1991;88(6):1219–1225. [PubMed] [Google Scholar]
- 377.Jellinger K., Armstrong D., Zoghbi H. Y., Percy A. K. Neuropathology of Rett syndrome. Acta Neuropathologica. 1988;76(2):142–158. doi: 10.1007/BF00688098. [DOI] [PubMed] [Google Scholar]
- 378.Deykin E. Y., MacMahon B. The incidence of seizures among children with autistic symptoms. American Journal of Psychiatry. 1979;136(10):1310–1312. doi: 10.1176/ajp.136.10.1310. [DOI] [PubMed] [Google Scholar]