Abstract
Given the well-documented symptom overlap between Autism Spectrum Disorder (ASD) and Attention Deficit/Hyperactivity Disorder (ADHD), careful evaluation of potential differentiation and overlap is critical for accurate diagnostic decisions. Although research has considered the use of symptom checklists and parent/teacher report questionnaires for symptom differentiation, standardized observational methods, typically utilized in the context of ASD evaluation, have received less attention. The present study examined the continuum of communication and social interaction impairment for youth diagnosed with ASD and ADHD, as indexed by the Autism Diagnostic Observation Schedule (ADOS). Participants were 209 youth ages 3 to 18 years with ASD, ADHD, Dual Diagnosis (ASD+ADHD) or No Diagnosis. Differences across diagnostic groups were observed for mean communication and social interaction total scores on the ADOS, with the highest scores (i.e., greater impairment) observed for the ASD group and lowest scores for the ADHD and No Diagnosis groups. Results provide the first evidence for use of the ADOS for distinguishing youth who have ADHD alone versus ASD alone or co-occurring ASD+ADHD. Findings are discussed in light of implications for clinical practice and future research.
Keywords: Autism spectrum disorder, ASD, Attention Deficit/Hyperactivity Disorder, ADHD, Autism Diagnostic Observation Schedule, ADOS, communication and social interaction, differential diagnosis
1. Introduction
At first glance, core symptom profiles of Autism Spectrum Disorder (ASD) and Attention Deficit/Hyperactivity Disorder (ADHD) appear clearly distinctive for diagnostic purposes, but in reality the picture is often more complex. In fact, multiple studies have documented the co-occurrence of ASD and ADHD, as well as overlapping genetic and neurobiological commonalities (for reviews see Matson, Rieske, & Williams, 2013; Reiersen & Todd, 2008). This consensus has resulted in a change of diagnostic convention to allow co-occurring diagnoses of ASD and ADHD in The Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association, 2013). However, diagnostic evaluation of differential and co-occurring conditions still poses a significant challenge for clinicians and researchers. Currently, it is unclear to what extent standardized diagnostic measures can effectively capture differentiation in these symptom profiles in order to facilitate valid clinical diagnoses. The current study examines a primary domain of symptom overlap across ASD and ADHD – communication and social interaction impairment – using a standardized assessment measure, the Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000) as a means of identifying differentiation in diagnostic classification for children with ASD, ADHD or co-occurring ASD+ADHD. Characterizing the continuum of communication/social interaction profiles among individuals with ASD, ADHD and ASD+ADHD is not only relevant from a diagnostic and treatment perspective, but also critical for etiological research. Reliable differences in ADOS symptom profiles associated with ASD, ADHD and ASD+ADHD would offer a valuable means of systematically examining pathways towards ASD and ADHD.
1.1. ASD and ADHD Commonalities
Core characteristics of ASD include impairments in social communication and social interaction and the presence of restricted, repetitive patterns of behavior, interests or activities, while ADHD is characterized by core symptoms of inattention, hyperactivity and impulsivity (APA, 2013). Prevalence rates are estimated at 5% for ADHD and 1% for ASD (APA, 2013). A co-occurring diagnosis is given when core symptoms of one disorder do not adequately account for the clinically significant symptom elevations of the other.
Noteworthy for diagnostic consideration, many children with ASD (22–83% depending on clinical or community samples) present with symptoms of attention deficits and hyperactivity, similar to those observed in children with an ADHD-only diagnosis (Frazier et al., 2001; Gadow, Devincent, Pomeroy, & Azizian, 2005; Goldstein & Schwebach, 2004; Hattori et al., 2006; Lee & Ousley, 2006; Rommelse, Geurts, Franke, Buitelaar, & Hartman, 2011; Sinzig, Walter, & Doepfner, 2009). Likewise, 20–65% of children with ADHD also display symptoms of ASD that are clinically significant, including deficits in social communication, peer relationship difficulties, lack of social and emotional reciprocity, difficulty adapting to change, and restricted and repetitive behavior (Clark, Feehan, Tinline, & Vostanis, 1999; Grzadzinski et al., 2011; Hartley & Sikora, 2009; Hattori et al., 2006; Koyama, Tachimori, Osada, & Kurita, 2006; Santosh & Mijovic, 2004).
In addition to behavioral links, ASD and ADHD are both considered highly heritable and display a moderate degree of shared genetic and familial overlap across the lifespan (for a review see Matson et al., 2013). For example, family and twin research has yielded evidence for shared genetic factors, both among individuals with a diagnosis as well as among individuals within the general population with subclinical features (Lichtenstein, Carlstrom, Rastam, Gillberg, & Anckarsater, 2010). Theoretical perspectives on the phenotypic and neuropsychological overlap between ASD and ADHD highlight the role of executive functioning deficits. It has been suggested that damage or dysfunction to the frontostriatal regions (frontal lobes, basal ganglia and a range of associated neurotransmitters), which are the slowest developing regions within the central nervous system, underlie neurodevelopmental disorders such as ASD and ADHD (Bradshaw, 2001). Overall, research to date indicates that while ASD and ADHD appear distinctive in their “pure” form, the existence of common behavioral, cognitive, and neurobiological features provides important opportunities to examine shared origins. This creates an imperative for measurement studies aimed at identifying reliable tools to aid in diagnosis when presented with a referral for differential or co-occurring diagnosis of ASD and ADHD.
1.2. Diagnostic Considerations
The symptom overlap between ASD and ADHD can present a diagnostic puzzle for clinicians, and oftentimes a diagnosis of ASD may be delayed or initially misdiagnosed as ADHD (Hartley & Sikora, 2009). Furthermore, diagnosis may be even more challenging when ASD and ADHD are co-occurring (Gargaro, Rinehart, Bradshaw, Tonge, & Sheppard, 2011), which is especially concerning given their high rate of co-occurrence, as discussed above.
One critical point for decision making about differential or co-occurring diagnosis is consideration of the degree of social communication and social interaction deficits. While identifying behaviors associated with inattention and hyperactivity/impulsivity or restricted repetitive behaviors are central to diagnostic decision making about ADHD and ASD, these behaviors are often clearly distinguishable via clinical interview, assessment and observation (for a review of neuropsychological testing in ASD, see Corbett, Carmean, & Fein, 2009). While the clinician may be tasked with identifying the degree of severity in each of these domains (i.e., whether symptoms of inattention/hyperactivity clinically impairing; whether restricted/repetitive behaviors are clinically significant), the presence of significant impairment in either category of symptoms points to a clear diagnostic category. Comparatively, social communication and interaction impairments can be more challenging to objectively categorize in the context of an evaluation, as these behaviors can derive from core impairments associated with either ASD or ADHD. Within the DSM-5, the following guidance for differential diagnosis of the social communication and interaction impairment is offered: “the social dysfunction and peer rejection seen in individuals with ADHD must be distinguished from the social disengagement, isolation, and indifference to focal and tonal communication cues seen in individuals with ASD” (APA, 2013 p.64).
In practice, children with ASD and ADHD often both present with difficulties in conversational skills and recognizing social cues, not listening to others, initiating conversations at inappropriate times, interrupting/intruding on others, high rates of off-task behaviors, and disruptive or rule-violating behavior. The challenge then is to identify standardized tools for characterizing social communication and interaction profiles. A variety of screening and parent-report tools are available for this purpose, designed either to capture ASD type social communication and interaction impairments (e.g., Social Communication Questionnaire, Rutter, Bailey & Lord, 2003; Children’s Communication Checklist, Bishop, 2006; Social Responsiveness Scale, Constantino, 2012) or to capture broadband non-specific impairments in social interaction (e.g., Behavior Assessment System for Children, Reynolds & Kamphaus, 2004; Child Behavior Checklist, Achenbach & Ruffle, 2000). Note that a comprehensive review of these measures is beyond the scope of the current paper and available elsewhere (see for example Falkmer, Anderson, Falkmer, & Horlin, 2013; Jones & Lord, 2013). For differential and co-occurring diagnoses, the challenge in all cases is the extent to which the respective measure can effectively differentiate whether an elevation in social communication impairment is the result of ADHD driven and/or ASD driven deficits in social interaction. For example, the SRS and CCC-2 have high sensitivity for ASD, but only moderate specificity in the presence of ADHD (Charman et al., 2007), meaning that elevated social communication impairment can reflect underlying ASD symptoms or non-specific socialization difficulties. Importantly, it is likely that a standardized observational measure such as the ADOS, which is administered by trained clinicians, may have greater utility for this purpose than questionnaire measures vulnerable to rater bias. For example, although parents may endorse high impairment across multiple symptom scales on checklist measures, diagnoses in all elevated symptom domains may not be appropriate; conversely, low symptom ratings by parent/teacher report do not always rule out a diagnosis. As such, it is worth considering whether a standardized observation measure, designed to allow clinicians to conduct a structured, developmentally appropriate evaluation of communication, social interaction and play behaviors, can contribute to this kind of diagnostic decision-making.
1.3. Current Study
The majority of studies that have considered the overlap of ASD and ADHD symptomatology described above have utilized retrospective chart reviews and parent or teacher report measures to identify correspondence using symptom counts and checklists. However, within an evaluation setting, communication and social interaction functioning can be more objectively and appropriately assessed by a clinician with the additional information provided by standardized observational diagnostic measures. Use of a standardized observation procedure is particularly important when a diagnosis of ASD is in question. As such, it is critical to identify measures that can effectively capture and differentiate broadband impairments across diagnostic categories to further support the diagnostic process.
The aim of the present study was to evaluate the extent to which the gold standard diagnostic tool used for the assessment of ASD symptoms, the Autism Diagnostic Observation Schedule (ADOS; Lord et al., 2000), would characterize differences in communication and social interaction as it relates to both ASD and ADHD symptomatology. To do this, we compared ADOS communication and social interaction scores across groups of youth with the following diagnoses: ASD; ADHD; Dual Diagnosis (ASD+ADHD); or No Diagnosis of ASD or ADHD. We predicted that each of the ASD and ADHD diagnosis groups would display deficits in this domain, but that the level of symptom impairment, as measured by ADOS communication/social interaction functioning, within each group would differentiate between diagnostic categories, ranging as follows: No Diagnosis and ADHD with few or some observable impairment in social communication and social interaction, through ASD with clear impairment in social communication and social interaction, to ASD+ADHD dual diagnosis with the highest level of impairment in social communication and social interaction (No Diagnosis < ADHD < ASD < ASD+ADHD Dual Diagnosis).
2. Methods
2.1. Procedure
Data were gathered from a comprehensive research database of electronic medical records at a university-based medical center. Youth were evaluated between July of 2010 and August of 2012 in an interdisciplinary specialty clinic for neurodevelopmental disorders by an experienced diagnostic team, which consisted of at least a clinical psychologist (PhD), and a developmental pediatrician (MD) or nurse, with some clinical teams also including a speech-language pathologist and/or an occupational or physical therapist. Youth were evaluated at the clinic for a variety of referral questions (e.g., developmental disabilities, autism spectrum disorder, language, behavior). The record review was approved by the Human Subjects Committee at the University of Kansas Medical Center.
The diagnostic process included administration of standardized assessment measures, behavioral reports, a clinical diagnostic interview and a review of medical history. A developmental hierarchy of measures (selected based on age and language ability) was used to determine cognitive ability, including the Bayley Scales of Infant and Toddler Development-Third Edition (BSID-III; Bayley, 2005), Kauffman Assessment Battery for Children-Second Edition (KABC-II; Kaufman & Kaufman, 2004a),Wechsler Preschool and Primary Scale of Intelligence – Third Edition (WPPSI-III; Wechsler, 2002), Wechsler Intelligence Scale for Children – Fourth Edition (WISC-IV; Wechsler, 2003), Psychoeducational Profile - Third Edition (PEP-3; Schopler, Lansing, Reichler, & Marcus, 2005), and Kaufman Brief Intelligence Test, Second Edition (KBIT-2; Kaufman & Kaufman, 2004b). Cognitive measures were administered as appropriate for the referral and are available for a subset of the sample included here. Across measures, scores are standardized with a mean of 100 and a standard deviation of 15. Therefore, general cognitive ability across measures was comparable given the similar metric used for each standard score.
The ASD diagnostic evaluation included administration of either the Childhood Autism Rating Scale (CARS-2; Schopler, Van Bourgondien, Wellman, & Love, 2010) or the Autism Diagnostic Interview-Revised (ADI-R; Le Couteur, Lord, & Rutter, 2006), unstructured and structured (ADOS) observation. The ADOS and ADI-R administration and scoring were completed by clinically trained teams members; all teams included at least one member with ADOS or ADI-R research training. Symptoms of ADHD were evaluated through clinical interview, observation and the use of parent and teacher rating scales, the Behavioral Assessment Schedule for Children (BASC-2; Reynolds & Kamphaus, 2004), and behavioral observation using DSM-IV-TR criteria for ADHD. It is important to note that although the ADOS was included as part of the diagnostic information, final diagnostic determination was not based solely on ADOS results. Immediately after completion of all testing and observation during assessment visits, the multidisciplinary team members discussed clinical observations, CARS or ADI-R, cognitive testing, behavioral rating scale results and history to determine appropriate diagnoses. Thus, in making the final diagnostic decision, information from a broader range of sources and contexts was utilized – including all standardized measures, behavioral observations, diagnostic interview, and medical interview/case history.
It should be noted that The Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association, 2000) was used for diagnosis of the current sample. Although an ASD diagnosis precluded an ADHD diagnosis in DSM-IV, both diagnoses were given as appropriate due to the presence of symptoms beyond what would be expected given either diagnosis alone, which is in line with current DSM-5 criteria allowing co-occurring diagnosis of ASD+ADHD. However, a systematic review of recent research comparing ASD diagnoses across DSM-IV and DSM-5 criteria indicates that between 50 to 75% of individuals maintain diagnoses, with diagnostic change most often observed among individuals with higher cognitive ability level (IQ >70) or a diagnosis of Pervasive Developmental Disorder – Not Otherwise Specified or Asperger’s disorder (Smith, Reichow, & Volkmar, 2015). As such, the current sample can be considered to effectively reflect DSM-5 criteria in terms of co-occurring diagnoses, but should be considered more cautiously as a reflection of DSM-5 ASD diagnosis.
2.2. Participants
Participants were 209 youth ages 3 to 18 years, with a mean age of 7.39 years (SD = 3.84 years). Youth were primarily White (65%), followed by Biracial (9%), Black or African American (8%), Hispanic (8%) and Other (10%). Inclusion criteria were that youth received a diagnosis of ASD and/or ADHD and had been administered the Autism Diagnostic Observation Schedule - Revised (ADOS; Lord et al., 2000). A comparison group consisted of youth who received no ASD or ADHD diagnoses but were individuals who were similarly referred to the clinic for an evaluation of possible ASD. This comparison group may have received no diagnosis or some other diagnosis such as Disruptive Behavior Disorder, Global Developmental Delay, or Speech/Language Disorder. Diagnoses were obtained from clinical assessment records and were collapsed across ASD (Autism, Asperger’s Syndrome, Pervasive Developmental Disorder NOS) and ADHD (Combined, Predominantly Hyperactive-Impulsive, Predominantly Inattentive) groups. Cognitive scores were available for only a subset of the current sample, given the nature of the referral question and the availability of previous evaluation records. On measures of IQ, data provided by 76 participants showed a mean IQ score of 93 (SD = 18.86).
2.3. Measures
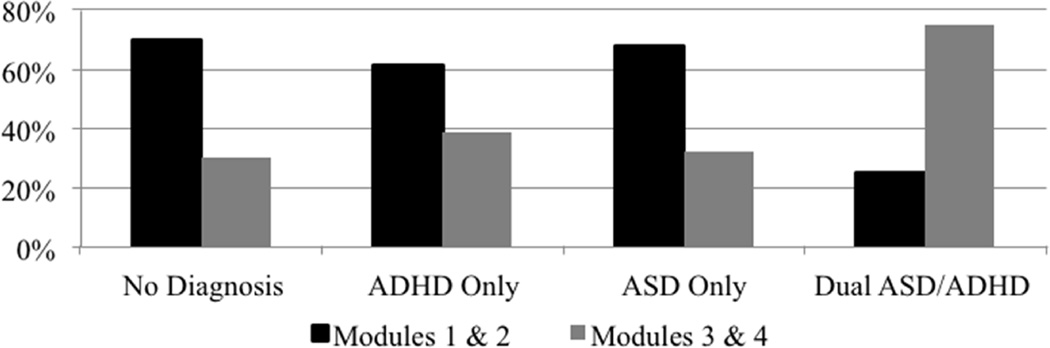
Demographic information was provided by parents via an online data system prior to the assessment. Outcome assessment of observed communication and social interaction deficits was provided through algorithm scores obtained on the Autism Diagnostic Observation Schedule – Revised (ADOS; Lord et al., 2000). The ADOS is a semi-structured, standardized assessment of communication, social interaction and play behaviors for individuals suspected of having autism spectrum disorder, ranging in age from toddlers to adults. The ADOS consists of four separate but overlapping modules, with selection based on age and expressive language level (pre-verbal, phrase speech or fluent speech), and yields algorithm-based scores for the domains of communication, social interaction, play and restricted/repetitive behaviors. The current sample includes participants who were administered Modules 1, 2, 3, or 4. The distribution of Modules across diagnostic groups was assessed and revealed similar distributions across all groups with the exception of the dual ASD/ADHD diagnosis group; there was an overrepresentation of Modules 3 and 4 in the dual ASD/ADHD diagnostic group as compared to the other groups (see Figure 1).
Fig. 1.
Distribution of Categorized ADOS Modules across Diagnostic Groups.gr1
A total algorithm score has an identified cutoff for broad autism spectrum diagnosis. Algorithm items for the communication domain (e.g., social overtures, stereotyped language, pointing and gestures, and intonation) and the reciprocal social interaction domain (e.g., eye contact, directed facial expressions, shared enjoyment in interactions, showing, initiation of joint attention, quality of social overtures and response) are summed to yield the communication + social interaction total score (with higher scores indicating a higher number of symptoms), which is consistent with DSM-5 conceptualization of this core deficit area. The communication + social interaction total score was used to quantify the continuum of communication and social interaction deficits observed across diagnostic groups. Given that Modules 3 and 4 have one less item on the communication domain, results should interpreted with consideration of the higher representation of these modules in the dual ASD/ADHD group. The ADOS demonstrates excellent interrater reliability, internal consistency and test–retest reliability on the item and domain levels for ASD and non-spectrum disorders (Lord et al., 2000).
2.4. Analytic Plan
All data were cleaned and examined for outliers and distributional assumptions using SPSS Statistics Software, Version 22. Correlations and group mean comparisons were conducted to address the inclusion of relevant covariates. Analysis of covariance (ANCOVA) was employed to determine the presence of mean differences across diagnostic groups on a combined score of communication + social interaction from the ADOS while accounting for the influence of age. Post-hoc comparisons were employed to identify significant differences across specific groups with Sidak correction to account for multiple comparisons. Given the sample size and power estimates, a criterion value of p < .01 was employed for these analyses and provided greater than .80 power.
3. Results
Examination of the percentage of youth who met the autism spectrum cut-off criterion on the communication + social interaction score on the ADOS revealed that 29% of the no diagnosis group, 40% of the ADHD only group, 98% of the ASD only group, and 94% of the ASD/ADHD group met the criterion. Results revealed a significant association between child age and communication/social interaction ADOS score (Pearson’s r = −0.144; p = 0.039). For the 76 youth with available data on cognitive ability, no statistically significant relation was present in the correlations between cognitive ability and age (Pearson’s r = .013; p = .913) or ADOS score (Pearson’s r = −.058; p = .618). Further, an ANOVA test evaluating the relation between cognitive ability and diagnostic categories revealed no significant differences across diagnostic groups in overall mean cognitive ability scores, F(3, 75) = 1.82; p = .151. Please refer to Table 1 for more information on descriptives across diagnostic category.
Table 1.
Study Descriptives across Diagnostic Category.
| Autism Diagnostic Observation Schedule (ADOS) Scores | |||||||
|---|---|---|---|---|---|---|---|
| N | Mean (Sd) Age |
Mean (Sd) IQ* |
Mean (Sd) Social Interaction |
Mean (Sd) Creativity/ Play |
Mean (Sd) Stereotyped Behavior |
Mean (Sd) Communication |
|
| No Diagnosis | 51 | 6.66 (3.56) |
89.63 (21.79) |
3.38 (2.96) | .47 (.79) | .48 (1.09) | 1.70 (2.25) |
| ADHD Only | 31 | 7.56 (3.48) |
97.18 (20.71) |
3.90 (2.07) | .48 (.51) | .11 (.32) | 1.71 (1.04) |
| ADHD/ASD Combined |
36 | 9.18 (3.68) |
101.13 (15.61) |
7.03 (1.83) | .64 (.11) | .81 (.90) | 3.22 (1.42) |
| ASD Only | 91 | 7.03 (4.01) |
89.27 (16.93) |
8.31 (2.97) | 1.33 (1.24) | 2.10 (2.06) | 4.69 (2.25) |
| Total Sample | 209 | 7.39 (3.84) |
93.00 (18.86) |
6.20 (3.44) | .89 (1.04) | 1.20 (1.73) | 3.25 (2.31) |
Note. Not all participants had IQ scores. Approximately 36% of participants had IQ data and these participants were evenly distributed across diagnostic group categories.
To identify differences across diagnostic groups on ADOS communication/social interaction scores above and beyond the contributions of score differences based on age, an ANCOVA model was evaluated. Age was included in the model as a covariate under the assumption that it would not be correlated to the grouping factor of diagnostic category (the independent variable), but may be related to the outcome factor of communication/social interaction ADOS score. This assumption was evaluated through an ANOVA test revealing that age was not associated with diagnostic category based on our criterion of p < .01 (F(3, 205) = 3.62; p = .014). To test the assumption of homogeneity of regression slopes, the age by diagnostic category interaction term was added to the model and was not statistically significant at the criterion value set, F(3, 207) = 2.50, p = .060 (Table 2).
Table 2.
Final ANCOVA Model of ADOS Communication/Social Interaction Total Scores.
| Sum of Squares | df | Mean Square | F | p-value | Partial η2 | |
|---|---|---|---|---|---|---|
| Corrected Model | 2754.722 | 4 | 688.680 | 41.897 | .000 | .453 |
| Intercept | 18463.889 | 1 | 18463.889 | 1123.274 | .000 | .848 |
| Age | 125.426 | 1 | 125.426 | 7.630 | .006 | .036 |
| Diagnosis | 2629.296 | 3 | 876.432 | 53.319 | .000 | .442 |
| Error | 3320.389 | 202 | 16.438 | |||
| Total | 24539.000 | 207 | ||||
| Corrected Total | 6075.111 | 206 |
R2 = .453 (Adjusted R2 = .443)
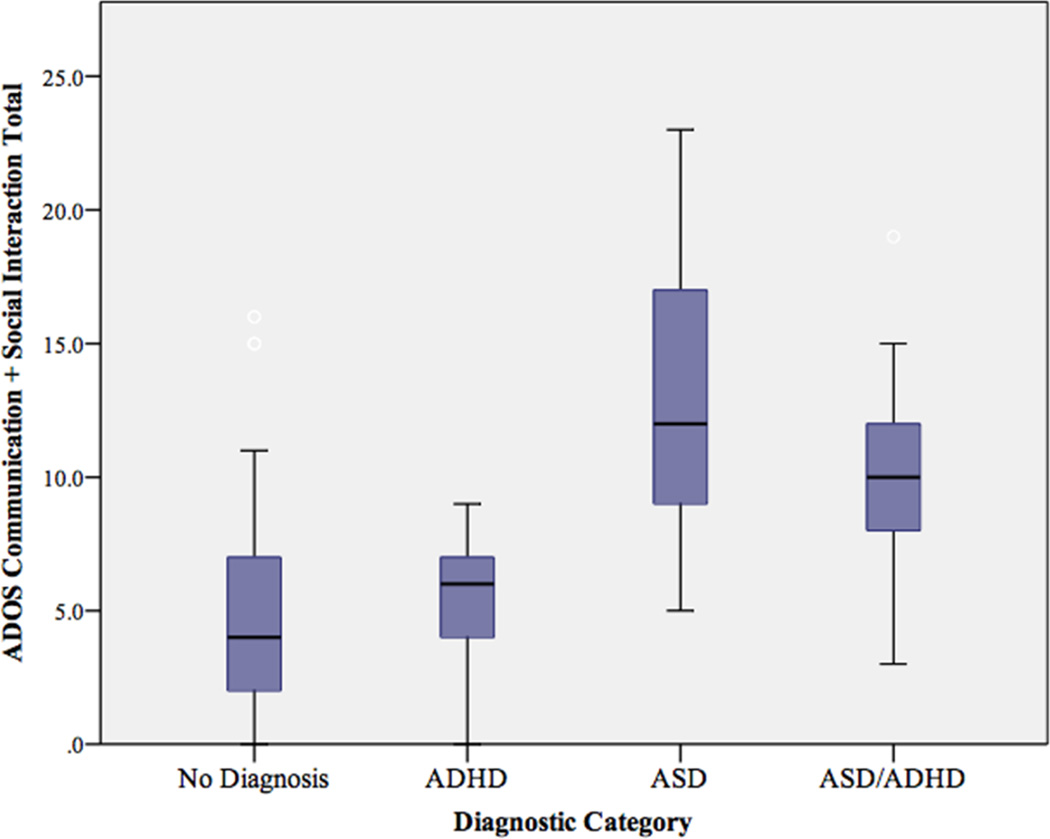
The hypothesized direction of mean levels of social impairment was generally supported with the No Diagnosis group mean of 5.08, ADHD group mean score of 5.40, the Dual Diagnosis group mean score of 10.25, and the ASD group mean score of 12.94 on the communication/social interaction ADOS scale (see Figure 2 for graphical representation of mean differences and distribution of scores across groups). Further, above the effects of age, F(1, 207) = 7.63; p = 0.006; Partial η2= .036, diagnostic category was a significant contributor to the ANCOVA model, F(3, 207) = 53.32; p < 0.001; Partial η2 = .442. More specifically, those youth receiving no diagnosis had the lowest ADOS mean score, followed by those with an ADHD only diagnosis, next those with dual ADHD/ASD diagnosis, and finally those with an ASD only diagnosis (see Table 3 for estimated marginal mean ADOS scores). To evaluate the impact of age as a covariate on the overall variance explained adjusted R2 values were compared between the ANCOVA model (R2 = .453) and the ANOVA model without age included (R2 = .426).
Fig. 2.
Mean ADOS Communication + Social Interaction Total Score Differences Across Diagnostic Groups.gr2
Table 3.
Mean ADOS Communication/Social Interaction Total Scores by Diagnostic Category
| Diagnostic Category | Mean | SE | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| No Diagnosis | 4.902 | .570 | 3.777 | 6.027 |
| ADHD | 5.452 | .740 | 3.992 | 6.912 |
| ASD+ADHD | 10.674 | .689 | 9.316 | 12.032 |
| ASD | 12.858 | .428 | 12.013 | 13.702 |
Covariates appearing in the model are evaluated at the following values: Age (yrs) = 7.40.
Post-hoc follow up tests to identify differences between the diagnostic groups revealed scores reflective of a bimodal distribution with significant differences between ASD-diagnosed youth as compared to youth without ASD diagnosis. Using group mean comparisons with age adjustment, the ASD and ADHD/ASD combined diagnosis group did significantly differ in mean scores (mean difference = 2.69), but the no diagnosis group and ADHD only group did not significantly differ in mean scores (mean difference = .32). Please note, however, that with the Sidak correction the mean difference between ASD and combined diagnosis groups was not significant (See Table 4). The ASD group had significantly higher scores than the no diagnosis group (mean difference = 7.87) and the ADHD only group (mean difference = 7.54). Further, the ASD+ADHD combined group also had significantly higher scores than the no diagnosis group (mean difference = 5.17) and the ADHD only group (mean difference = 4.85). To see values for pairwise comparison adjusted for marginal means using the Sidak correction for multiple comparisons, please see Table 4.
Table 4.
Pairwise Comparison of Mean ADOS Communication/Social Interaction Total Score Differences Across Diagnostic Groups.
| Reference Diagnostic Category |
Comparative Diagnostic Category |
Mean Difference |
SE | p | 95% Confidence Intervalb |
|
|---|---|---|---|---|---|---|
| Lower Bound |
Upper Bound |
|||||
| ASD | No Diagnosis | 7.956* | .711 | .000 | 6.066 | 9.845 |
| ADHD | 7.406* | .856 | .000 | 5.132 | 9.680 | |
| ADHD | No Diagnosis | .550 | .936 | .992 | −1.936 | 3.036 |
| ASD+ADHD | −5.222* | 1.009 | .000 | −7.903 | −2.541 | |
| ASD+ADHD | No Diagnosis | 5.772* | .903 | .000 | 3.373 | 8.170 |
| ASD | −2.184 | .816 | .047 | −4.351 | −.017 | |
Based on estimated marginal means of age = 7.40 yrs; Adjustment for multiple comparisons: Sidak.
The mean difference is significant at the .01 level.
4. Discussion
The aim of the current study was to examine the communication and social interaction impairment in youth diagnosed with ASD and/or ADHD, as indexed by a semi-structured, standardized assessment of communication and social interaction impairment. To our knowledge, this is the first study to examine the use of ADOS defined communication/social interaction deficits to inform diagnostic evaluation of youth suspected of having ADHD and/or ASD.
4.1. ADOS Profiles of Communication and Social Interaction for ASD and ADHD
Our findings are in line with the well-documented overlap in ASD and ADHD symptoms (e.g., Matson et al., 2013; Reiersen & Todd, 2008) and offer promise that the ADOS may be used to inform clinical decision-making about ADHD and ASD as differential and co-occurring diagnoses. Notably, while all youth in this sample demonstrated some degree of impairment in communication and social interaction (as would be expected given that youth were referred to a university-based medical center clinic for neurodevelopmental disabilities), results suggest that diagnostic category (ASD, ADHD, or ASD+ADHD) is related to impairment in socialization and communication at a level that is statistically significant. More precisely, youth diagnosed with ASD demonstrated the highest communication + social interaction deficits, those with a dual diagnosis of ASD+ADHD had the next highest deficit levels; comparatively, youth who received a diagnosis of ADHD or No Diagnosis (of ADHD or ASD) had lower levels of identified communication/social interaction deficits. This pattern of results was significant even when considering developmental status; age emerged as an important covariate in the model, suggesting that older youth presenting for diagnostic evaluation may demonstrate lower levels of impairment in these domains (which is reasonable, given that older youth may not have experienced a high enough level of impairment when they were younger to trigger evaluation referral).
It was somewhat unexpected that the group with the highest level of impairment in socialization and communication was the ASD group and not the dually diagnosed ASD+ADHD group, although this finding should be interpreted in light of the unbalanced distribution of ADOS Modules across the dual diagnosis group. This distribution of Modules may have suppressed overall scores for the dual diagnosis group. While the mean difference across the ASD only group and the dual diagnosis group was no longer significant after correcting for multiple comparisons, we suspect that this may also be in part due to the nature of both the broader referral group and the ASD diagnosed groups. The overall sample consisted of clinically referred youth suspected of neurodevelopmental disabilities, and as a result, the ASD diagnosed groups were likely to present with higher levels of ASD related symptoms. An alternative possibility for the lack of statistically significant mean difference in ADOS scores is that youth with ASD and those with ASD+ADHD may have comparable symptom presentation in terms of communication/social interaction deficits. If this finding is supported by future studies examining ADOS results, it would suggest that the communication/social interaction domain will be less informative for this particular differential.
Perhaps most useful from a clinical viewpoint is the evidence for differential diagnosis of ADHD versus ASD and ASD+ADHD based on level of deficits in communication/social interaction. For those youth with a diagnosis of ADHD, communication/social interaction deficits were present at approximately half the mean level of the ASD and Dual Diagnosis groups, but indistinguishable from the No Diagnosis group (which likely presented with elevated deficits due to the clinical nature of the sample). The current results suggest that for youth suspected of having ASD and/or ADHD, a clear diagnostic differentiation of symptoms may be obtained for communication/social interaction deficits in the context of a standardized, developmentally appropriate interaction paradigm such as the ADOS.
From an evaluation standpoint, the identification of communication and social interaction functioning and level of impairment associated with these specific diagnostic categories has the potential to improve clinical decision making accuracy. Though administration of the ADOS is admittedly more time consuming than checklist measures, clinicians evaluating symptoms of ASD with this gold-standard assessment measure would have this information as part of a routine evaluation process. In such cases, use of a structured observational tool such as the ADOS offers a standardized platform for indexing communication and social interaction behaviors. From a broader perspective, this particular diagnostic differential is critical for treatment planning and associated outcome. Children with a dual diagnosis of ASD+ADHD may respond poorly to standard ADHD treatment, have increased medication side effects and may be at increased risk for persistent ADHD symptoms (Reiersen & Todd, 2008; St. Pourcain et al., 2011). Our findings here are a first step in more detailed analysis of item-level ADOS data, with the goal of articulating specific types of impairment across diagnostic groups to aid in improved diagnostic differentiation of ADHD and ASD.
4.2. Limitations and Future Directions
Some limitations of the current study should be considered. First, the sample included here is a clinically referred group, which contained a high proportion of individuals suspected of having neurodevelopmental disorders, including some level of suspicion about autism spectrum disorder (by parents, teachers/interventionists, clinicians). As such, there was no non-clinically referred control group and results cannot be generalized to a non-clinical population. This may have contributed to a higher level of ASD symptomatology in the sample regardless of final diagnosis, and may have contributed to the lack of significant difference on ADOS social communication and interaction scores between the ADHD and No Diagnosis groups. Moreover, this precluded our ability to methodologically promote an equivalent distribution of the ADOS modules across diagnostic groups, resulting in a higher representation of Modules 3 and 4 in the dual diagnosis group.
Also, because the ADOS was administered in the course of standardized diagnostic procedures and contributed to the final diagnosis, this may have resulted in a clearer difference in ADOS scores between groups with and without an ASD diagnosis than would be present if the ADOS had not been used for clinical diagnosis. However, it should be emphasized that the ADOS was one component of diagnostic decision-making (along with clinical interview, other standardized assessment measures, observation, and parent/teacher report measures) utilized by an experienced multidisciplinary team. The variability in ADOS socialization/communication scores within the ASD diagnosed groups (ASD+ADHD, ASD) is evidence of the wide range of levels of symptom impairment regardless of final ASD diagnosis. In addition, we have considered here ADOS communication + social interaction scores as a means of characterizing the continuum of communication and social interaction across diagnostic groups; however, we were unable to calculate ADOS-2 equivalent algorithm scores (e.g., Gotham, Risi, Pickles, & Lord, 2007) because item scores were not available for our analyses. Results should be interpreted in light of this limitation for making direct comparisons across modules and generalization to DSM-5 criteria. In addition, data in the current study were obtained from standard clinical evaluation procedures and do not include the opportunity for assessment of inter-rater agreement or consensus scoring.
Finally, while mean age differences across groups were not found to be statistically significant, the mean age of the ASD+ADHD was greater than all other groups, which may have resulted in a suppression of ADOS scores for this dual diagnosis group. Despite the approximate two-year mean age difference, it is likely that overarching findings would remain the same were groups age-matched, as significant differences between the ASD+ADHD, no diagnosis, and ADHD only groups would only increase had the ASD+ADHD group ADOS scores been higher.
The current study represents an opportunity to evaluate the ADOS as a measurement tool for the broad range of communication and social interaction impairment evident in both ADHD and ASD. These results represent an important first step in the consideration of the utility of the ADOS as a tool for evaluating reliable diagnostic differences in communication and social interaction among youth with ADHD and/or ASD. The ADOS is widely used and well established as part of a standardized evaluation of ASD symptoms and we provide here evidence to support it’s utility for identification of differential and co-occurring diagnoses of ASD and ADHD. It will be critical for future studies to explore in finer detail profiles of communication and social interaction among youth diagnosed with ADHD and/or ASD by using the ADOS. An important next step will be examination of item-level differences in ADOS scores to consider whether it is possible to identify consistent ADHD-only related socialization and communication elevations, versus ASD or ASD+ADHD related profiles. Future work should also consider incorporating additional objective and clinical measures (e.g., parent/teacher/self report questionnaires, standardized measures of social communication/pragmatic language, etc.) to further characterize the nature of communication and social interaction deficits in these populations. Understanding how ADOS scores translate into diagnostic decision-making about ASD and/or ADHD has important implications for clinicians and researchers.
Highlights.
We examine ADOS communication/social interaction scores in youth with ASD and/or ADHD.
Differences in ADOS scores differentiate diagnostic groups (ASD, ADHD, ASD+ADHD).
Results provide support for utility of ADOS differential and co-occurring diagnosis.
Acknowledgements
Preparation of this manuscript was supported by the Kansas Intellectual and Developmental Disabilities Research Center HD 002528; manuscript preparation was also supported grant HD 075886 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) to Brenda Salley. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NICHD or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatrics in review / American Academy of Pediatrics. 2000;21(8):265–271. doi: 10.1542/pir.21-8-265. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th, text rev. ed. Washington, DC: Author; 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington: Author; 2013. [Google Scholar]
- Bayley N. Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III) San Antonio, TX: Pearson; 2005. [Google Scholar]
- Bishop D. Children’s Communication Checklist - 2 (U.S. ed) San Antonio, TX: Harcourt Assessment; 2006. [Google Scholar]
- Bradshaw JL. Developmental disorders of the frontostriatal system: Neuropsychological, neuropsychiatric and evolutionary perspectives. East Susex: Psychology Press; 2001. [Google Scholar]
- Charman T, Baird G, Simonoff E, Loucas T, Chandler S, Meldrum D, Pickles A. Efficacy of three screening instruments in the identification of autistic-spectrum disorders. The British journal of psychiatry : the journal of mental science. 2007;191:554–559. doi: 10.1192/bjp.bp.107.040196. [DOI] [PubMed] [Google Scholar]
- Clark T, Feehan C, Tinline C, Vostanis P. Autistic symptoms in children with attention deficit-hyperactivity disorder. European Child and Adolescent Psychiatry. 1999;8:50–55. doi: 10.1007/s007870050083. [DOI] [PubMed] [Google Scholar]
- Corbett BA, Carmean V, Fein D. Assessment of neuropsychological functioning in autism spectrum disorders. In: Goldstein S, Naglieri JA, Ozonoff S, editors. Assessment of autism spectrum disorders. New York, NY: Guilford Press; 2009. pp. 253–289. [Google Scholar]
- Falkmer T, Anderson K, Falkmer M, Horlin C. Diagnostic procedures in autism spectrum disorders: a systematic literature review. Eur Child Adolesc Psychiatry. 2013;22(6):329–340. doi: 10.1007/s00787-013-0375-0. [DOI] [PubMed] [Google Scholar]
- Frazier JA, Biederman J, Bellordre CA, Garfield SB, Geller DA, Coffey BJ, Faraone SV. Should the diagnosis of Attention-Deficit/ Hyperactivity disorder be considered in children with Pervasive Developmental Disorder? Journal of Attention Disorders. 2001;4(4):203–211. [Google Scholar]
- Gadow KD, Devincent CJ, Pomeroy J, Azizian A. Comparison of DSM-IV symptoms in elementary school-age children with PDD versus clinic and community samples. Autism. 2005;9(4):392–415. doi: 10.1177/1362361305056079. [DOI] [PubMed] [Google Scholar]
- Gargaro BA, Rinehart NJ, Bradshaw JL, Tonge BJ, Sheppard DM. Autism and ADHD: how far have we come in the comorbidity debate? Neurosci Biobehav Rev. 2011;35(5):1081–1088. doi: 10.1016/j.neubiorev.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Goldstein S, Schwebach AJ. The comorbidity of pervasive developmental disorder and attention deficit hyperactivity disorder: Results of a retrospective chart review. Journal of Autism and Developmental Disorders. 2004;34(3):329–339. doi: 10.1023/b:jadd.0000029554.46570.68. [DOI] [PubMed] [Google Scholar]
- Gotham K, Risi S, Pickles A, Lord C. The Autism Diagnostic Observation Schedule: revised algorithms for improved diagnostic validity. Journal of autism and developmental disorders. 2007;37(4):613–627. doi: 10.1007/s10803-006-0280-1. [DOI] [PubMed] [Google Scholar]
- Grzadzinski R, Di Martino A, Brady E, Mairena MA, O’Neale M, Petkova E, Lord C, Castellanos FX. Examining autistic traits in children with ADHD: Does the autism spectrum extend to ADHD? Journal of Autism and Developmental Disorders. 2011;41(9):1178–1191. doi: 10.1007/s10803-010-1135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley SL, Sikora DM. Which DSM-IV-TR criteria best differentiate high-functioning autism spectrum disorder from ADHD and anxiety disorders in older children? Autism. 2009;13(5):485–509. doi: 10.1177/1362361309335717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hattori J, Ogino T, Abiru K, Nakano K, Oka M, Ohtsuka Y. Are pervasive developmental disorders and attention-deficit/hyperactivity disorder distinct disorders? Brain and Development. 2006;28(6):371–374. doi: 10.1016/j.braindev.2005.11.009. [DOI] [PubMed] [Google Scholar]
- Jones RM, Lord C. Diagnosing autism in neurobiological research studies. Behav Brain Res. 2013;251:113–124. doi: 10.1016/j.bbr.2012.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. The Kaufman Assessment Battery for Children Second Edition. Circle Pines, MN: American Guidance Service; 2004a. [Google Scholar]
- Kaufman AS, Kaufman NL. The Kaufman Brief Intelligence Test. Second Edition. Bloomington, MN: Pearson, Inc; 2004b. [Google Scholar]
- Koyama T, Tachimori H, Osada H, Kurita H. Cognitive and symptom profiles in high-functioning pervasive developmental disorder not otherwise specified and attention-deficit/hyperactivity disorder. Journal of Autism and Developmental Disorders. 2006;36(3):373–380. doi: 10.1007/s10803-006-0075-4. [DOI] [PubMed] [Google Scholar]
- Le Couteur A, Lord C, Rutter M. The Autism Diagnostic Interview -Revised. Los Angeles, CA: Western Psychological Services; 2006. [Google Scholar]
- Lee DO, Ousley OY. Attention-deficit hyperactivity disorder symptoms in a clinic sample of children and adolescents with pervasive developmental disorders. Journal of Child and Adolescent Pscyhopharmacology. 2006;16(6):737–746. doi: 10.1089/cap.2006.16.737. [DOI] [PubMed] [Google Scholar]
- Lichtenstein P, Carlstrom E, Rastam M, Gillberg C, Anckarsater H. The genetics of autism spectrum disorders and related neuropsychaitric disorders in childhood. American Journal of Psychiatry. 2010;167(11):1357–1363. doi: 10.1176/appi.ajp.2010.10020223. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EHJ, Leventhal BL, DiLavore PC, Pickles A, Rutter M. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30(3):205–223. [PubMed] [Google Scholar]
- Matson JL, Rieske RD, Williams LW. The relationship between autism spectrum disorders and attention-deficit/hyperactivity disorder: an overview. Research in Developmental Disabilities. 2013;34(9):2475–2484. doi: 10.1016/j.ridd.2013.05.021. [DOI] [PubMed] [Google Scholar]
- Reiersen AM, Todd RD. Co-occurrence of ADHD and autism spectrum disorders: Phenomenology and treatment. Expert Review of Neurotherapeutics. 2008;8(4):657–659. doi: 10.1586/14737175.8.4.657. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW. Behavioral Assessment System for Children. 2nd ed. Circle Pines, MN: American Guidance Service; 2004. [Google Scholar]
- Rommelse NN, Geurts HM, Franke B, Buitelaar JK, Hartman CA. A review on cognitive and brain endophenotypes that may be common in autism spectrum disorder and attention-deficit/hyperactivity disorder and facilitate the search for pleiotropic genes. Neuroscience and Biobehavioral Reviews. 2011;35(6):1363–1396. doi: 10.1016/j.neubiorev.2011.02.015. [DOI] [PubMed] [Google Scholar]
- Rutter M, Bailey A, Lord C. Social Communication Questionnaire (SCQ) Los Angeles: Western Psychological Corporation; 2003. [Google Scholar]
- Santosh PJ, Mijovic A. Social impairment in Hyperkinetic Disorder -relationship to psychopathology and environmental stressors. European Child and Adolescent Psychiatry. 2004;13(3):141–150. doi: 10.1007/s00787-004-0372-4. [DOI] [PubMed] [Google Scholar]
- Schopler E, Lansing MD, Reichler RJ, Marcus LM. Psychoeducational Profile. Third Edition. USA: Pro-Ed; 2005. [Google Scholar]
- Schopler E, Van Bourgondien ME, Wellman GJ, Love SR. The Childhood Autism Rating Scale. Second Edition. Los Angeles, CA: Western Psychological Services; 2010. [Google Scholar]
- Sinzig J, Walter D, Doepfner M. Attention deficit/hyperactivity disorder in children and adolescents with autism spectrum disorder: symptom or syndrome? Journal of Attention Disorders. 2009;13(2):117–126. doi: 10.1177/1087054708326261. [DOI] [PubMed] [Google Scholar]
- Smith IC, Reichow B, Volkmar FR. The Effects of DSM-5 Criteria on Number of Individuals Diagnosed with Autism Spectrum Disorder: A Systematic Review. J Autism Dev Disord. 2015;45(8):2541–2552. doi: 10.1007/s10803-015-2423-8. [DOI] [PubMed] [Google Scholar]
- St. Pourcain B, Mandy WP, Heron J, Golding J, Smith GD, Skuse DH. Links Between Co-occurring Social-Communication and Hyperactive-Inattentive Trait Trajectories. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50(9):892e–902e. doi: 10.1016/j.jaac.2011.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. The Wechsler Preschool and Primary Scale of Intelligence. Third Edition. San Antonio, TX: The Psychological Corporation; 2002. [Google Scholar]
- Wechsler D. The Wechsler Intelligence Scale for Children. Fourth Edition. San Antonio, TX: The Psychological Corporation; 2003. [Google Scholar]