Abstract
Background
Sickle haemoglobin (HbS) and haemoglobin C (HbC) are both caused by point mutations in the beta globin gene, and both offer substantial malaria protection. Despite the fact that the blood disorder caused by homozygosity for HbC is much less severe than that caused by homozygosity for HbS (sickle cell anaemia), it is the sickle mutation which has come to dominate many old-world malarious regions, whilst HbC is highly restricted in its geographical distribution. It has been suggested that this discrepancy may be due to sickle cell heterozygotes enjoying a higher level of malaria protection than heterozygotes for HbC. A higher fitness of sickle cell heterozygotes relative to HbC heterozygotes could certainly have allowed the sickle cell allele to spread more rapidly. However, observations that carrying either HbC or HbS enhances an individual’s capacity to transmit malaria parasites to mosquitoes could also shed light on this conundrum.
Methods
A population genetic model was used to investigate the evolutionary consequences of the strength of malaria selection being correlated with either HbS frequency or HbC frequency.
Results
If the selection pressure from malaria is positively correlated with the frequency of either HbS or HbC, it is easier for HbS to succeed in the competitive interaction between the two alleles.
Conclusions
A feedback process whereby the presence of variant haemoglobins increases the level of malaria selection in a population could have contributed to the global success of HbS relative to HbC, despite the former’s higher blood disorder cost.
Electronic supplementary material
The online version of this article (doi:10.1186/s12936-015-1077-5) contains supplementary material, which is available to authorized users.
Keywords: Malaria, Plasmodium falciparum, Sickle cell, Haemoglobin C, Haemoglobinopathies, Human evolution, Gametocytes, Transmission, Sickle haemoglobin
Background
Falciparum malaria has had a profound effect on human evolution, evidenced by the high frequencies of malaria protective mutations observed in populations from historically malarious regions. Many of the protective variants identified thus far affect erythrocytes, where the malaria parasite spends a crucial stage of its life cycle. Several of the best studied of these mutations affect the globin genes encoding haemoglobin [1]. However, the benefits provided by malaria protective haemoglobin mutations are offset by the fact that such mutations can also lead to genetic blood disorders (haemoglobinopathies).
Haemoglobin C (HbC) is caused by a mutation (henceforth ‘βC’) in the 6th position of the amino acid sequence of beta globin, where glutamic acid is substituted by lysine. A recent meta-analysis [2] concluded that homozygotes for βC (genotype CC) were strongly protected against severe malaria, and heterozygotes (genotype AC) were mildly protected. It has also been found that both heterozygotes and homozygotes for βC may be less susceptible to uncomplicated clinical malaria than individuals with the ‘normal’ genotype, AA [3], although a recent cohort study in Mali reports an increase in the incidence of clinical malaria in AC individuals relative to AA [4]. Several mechanisms have been proposed to explain the malaria protection offered by HbC, including: abnormal intraerythrocytic development of the parasite leading to lower Plasmodium falciparum replication rates in subsets of CC erythrocytes [5]; abnormal P. falciparum erythrocyte membrane protein 1 (PfEMP-1) display, leading to reduced cytoadherence and possibly reduced parasite sequestration [6], and accelerated acquisition of immunity against malaria [7].
Sickle haemoglobin (HbS) is likewise caused by a single amino acid substitution at position 6 of beta globin. The sickle cell mutation (henceforth ‘βS’) replaces glutamic acid with valine. Heterozygosity for the sickle mutation (genotype AS) offers considerable protection against all forms of severe malaria, as well as protection against uncomplicated malaria [2] and parasitaemia [8, 9]. The battery of potential protective mechanisms that have been proposed for sickle cell include, like HbC, the abnormal display of PfEMP-1 [10] and the acceleration of acquired immunity [11]. It has also been shown that the growth rate of P. falciparum is retarded in HbS containing erythrocytes under conditions of low oxygen tension in vitro [12]; studies in mice have suggested that the protective effect of HbS is lost upon removal of the spleen [13], and an intriguing recent finding is that miRNAs are translocated from erythrocytes to malaria parasites, and specific miRNAs found more commonly in sickle cell trait cells than in normal cells inhibit parasite growth [14].
βS is associated with a high genetic load due to the low fitness of its homozygotes (genotype SS), who suffer from the severe blood disorder sickle cell anaemia. In contrast, the blood disorder associated with the genotype CC is relatively mild [15]. βC frequencies are low in most malaria endemic regions, with the exception of a few locations in West Africa [16], whilst βS is found at frequencies of up to 18 % across sub-Saharan Africa, the middle East and in scattered populations throughout India [17]. These observations create an apparent paradox: why should a malaria protective allele with such minor costs be so limited in its geographical distribution, whilst an allele associated with a severe blood disorder has come to dominate continents?
Recent epidemiological studies have generated the data necessary to estimate the relative malaria protection offered by AC or AS heterozygosity [3, 18]. AC seems to offer lower protection than AS against life-threatening falciparum disease. Furthermore, the genotype SC has been associated with a clinically significant blood disorder, although this condition is less severe than sickle cell disease [19]. It, therefore, seems reasonable to conclude that the relative fitnesses (w) for the genotypes AS, AC and SC have the following relationship wAS > wAC ≫ wSC. The low fitness of SC individuals leads to competitive exclusion between βS and βC. The fact that AS individuals enjoy more protection against severe malaria than AC individuals [2] means βS will outcompete βC if both are introduced simultaneously in a given population. In a population in Burkina Faso where βS and βC coexist, Modiano et al. [20] showed that βC has been present for approximately four times as long as βS. Only by arriving first has βC managed to maintain a relatively high frequency in Burkina Faso, despite the invasion of βS.
When considering the factors contributing to the limited geographical distribution of βC, Modiano et al. [20] suggest that βC increases in frequency by a predominantly recessive mechanism of selection (since the CC homozygote seems to enjoy more malaria protection than the AC heterozygote), whilst βS spreads much more rapidly through heterozygote advantage. However, there is a further, potentially crucial, feature of the interrelationship between HbS, HbC and P. falciparum yet to be considered. Gametocytes (the sexual stage of malaria parasites) are the only form of the parasite that can successfully infect a mosquito taking a blood meal [21]. Host factors, including immune responses, potentially influence gametocyte density during infection [21, 22]. Mutations affecting beta globin have also been associated with different levels of circulating gametocytes and of human infectivity to mosquitoes [23–25]. Ringelhann et al. [24] studied asymptomatic children under five years of age and showed that AC individuals had higher microscopically-detectable gametocyte prevalence than AA individuals. Robert et al. [25] observed that AS gametocyte carriers could infect twice as many mosquitoes as AA gametocyte carriers. Gouagna et al. [23] demonstrated that individuals carrying βC have a higher potential to transmit P. falciparum to anopheline vectors than individuals with the genotype AA. Taken together, these studies suggest that the diversity and frequency of beta globin variants could impact local malaria transmission intensity.
In 2004, Feng et al. [26] investigated the possible population genetic consequences of enhanced malaria parasite transmission from sickle cell heterozygotes, showing that such an effect could lead to increased selection for βS. In the population genetic model presented here, selection pressure from malaria is linked to either βS or βC frequency, and the consequences of such feedbacks for the competitive relationship between βS and βC are explored.
Methods
The rate of change in the frequency of each genotype was given by the following equation:
| 1 |
where yi is the frequency of genotype i (i = 1–6, where 1 = AA, 2 = AC, 3 = AS, 4 = CC, 5 = SS, 6 = SC); is the birth rate; p is the frequency of βC; q is the frequency of βS, and gi(p, q) is a function of p and q that assigns the proportion of births of each genotype (see Additional file 1 for further details). A non malaria-associated mortality rate (µBi), and a level of susceptibility to death from malaria (ri) were estimated for each genotype based on their known properties (see Additional file 1: Tables S1 and S2). The maximum possible malaria mortality rate was made a function of βC or βS frequencies by fj(p, q). If malaria mortality was positively correlated with allele frequency, function f1 was applied (Eq. 2); if malaria mortality was negatively correlated with the frequency of an allele, function f2 was applied (Eq. 3).
| 2 |
| 3 |
x is the minimum level of malaria related mortality assumed possible; z is the maximum level of malaria related mortality assumed possible, and γ is a coefficient scaling the effect of allele frequency on the level of mortality due to malaria. u may be equal to the frequency of the sickle cell allele (q) or the HbC allele (p).
The population size was set to be constant (limited by an external carrying capacity) by making the birth rate equal to the total death rate (Eq. 4):
| 4 |
Results
A positive correlation between malaria mortality and either βS or βC frequency favours βS at equilibrium
Specific conditions must be met if stable coexistence between three alleles is to be achieved, and, given realistic assumptions about each genotype’s relative susceptibility to severe malaria and blood disorder costs, stable coexistence between βS, βC and βA is not possible [27]. There will always be a “winner” in the competition between βS and βC, and, with the mortality rates used here, if both alleles are seeded in a population at equal frequencies, βS will always eliminate βC.
Figure 1 explores a scenario in which βC is present in a population prior to the arrival of βS, as seems to have occurred in West Africa. If βC is at a threshold frequency before the introduction of βS, βC will be able to prevent βS from successfully invading (Fig. 1a). However, if the cost of malaria increases linearly with the frequency of βC (Fig. 1b), then even with exactly the same starting conditions as in panel a, there will come a point where the strength of malaria selection is such that βS can eliminate βC. If malaria mortality is linked to βS frequency, βS will still replace βC, but it will take longer and the frequency of βS at equilibrium will be higher (Fig. 1c).
Fig. 1.
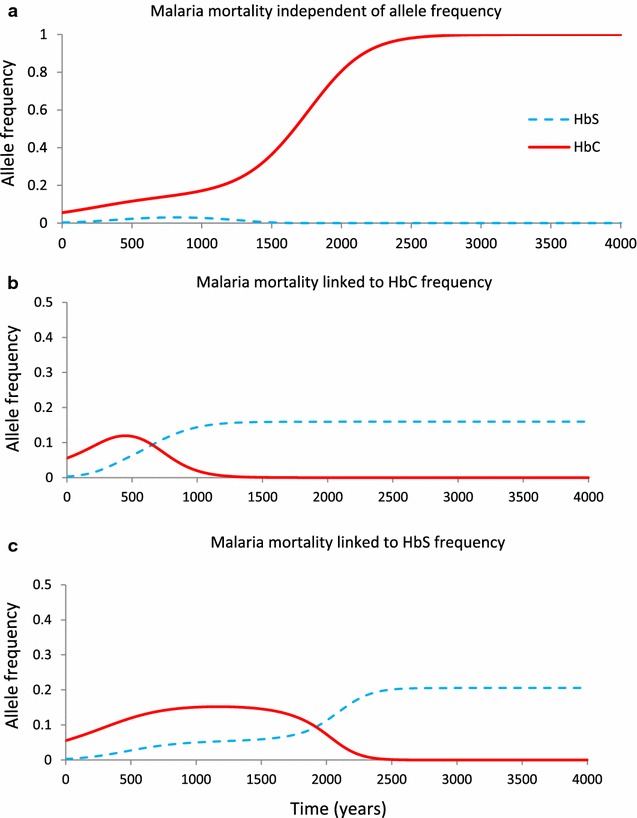
Dynamics of βC and βS frequencies under different malaria mortality functions. In each simulation shown, βC starts at a frequency of 5.6 % and βS starts at a frequency of 0.3 %, equivalent to a single βS heterozygote in a population of 150 individuals (e.g., after a mutation arises de novo or is imported into a small population). The malaria mortality function applied in all panels is f 1, where x = 0.01 and z = 0.015. In a, γ = 0, thus malaria mortality is independent of allele frequency. In b, γ = 10 and malaria mortality increases with βC frequency (u = p); in c, γ = 10 and malaria mortality increases with βS frequency (u = q). Baseline mortality rates and malaria susceptibilities of each genotype are given in tables S1 and S2
Figure 2 illustrates the minimum initial frequency of βC required to prevent its elimination by βS under different conditions. If βC acts to increase malaria mortality in a population, the threshold frequency increases with the intensity of this effect (Fig. 2a, red line). If malaria mortality increases with βS frequency, the threshold initial frequency also increases with the intensity of the effect, but not so steeply (Fig. 2a, blue line).
Fig. 2.

How the threshold starting frequency of βC required to prevent the invasion of βS varies with different malaria mortality functions. The starting frequency of βS was always 0.3 %. βS was deemed to have failed to successfully invade the population if its frequency (q) was <(1/300) after 15,000 years of evolution. Each panel shows how the minimum starting frequency of βC required to prevent βS invading varies with different values of γ (x axis). In a, function f 1 has been applied; in b, function f 2 is used. In both panels, the red line indicates the case where malaria mortality is linked to βC frequency (u = p) and the blue line indicates the case where malaria mortality is linked to βS frequency (u = q). Baseline mortality rates and malaria susceptibilities of each genotype are given in tables S1 and S2
In Fig. 1 and Fig. 2a, higher frequencies of βS and βC are assumed to be associated with increasing malaria mortality. However, the incidence of severe malaria during childhood may be inversely related to transmission intensity. Snow et al. [28] showed that the risk of severe malaria declines between low-to-moderate and high malaria transmission intensity regions, perhaps because in a highly endemic area, individuals are infected very early in their lives and build up protective immunity whilst shielded by maternal antibodies. It is therefore conceivable that by increasing malaria transmission, higher frequencies of βS or βC could result in lower overall malaria mortality. A positive relationship between beta globin mutation frequencies and malaria mortality benefits the ‘more protective yet costly’ allele (βS). A negative relationship between beta globin mutation frequencies and malaria mortality, benefits the ‘less protective yet mild’ allele (βC), as illustrated in Fig. 2b.
Linking malaria selection pressure to allele frequency dramatically alters the fitness landscape
Figure 3 illustrates the effects of different combinations of βC and βS frequencies on the mean fitness of a population. If the presence of βC amplifies malaria mortality, there is a critical zone where increasing βC frequency, in the presence of a low frequency of βS, decreases the mean fitness of the population. In this zone, βS will clearly be favoured—hence an increased likelihood of βS dominating the population. By contrast, when βC frequency is negatively correlated with malaria mortality, increasing βC frequency in the presence of a low level of βS always increases the mean fitness of the population. In this fitness landscape, it is harder for βS to displace βC.
Fig. 3.
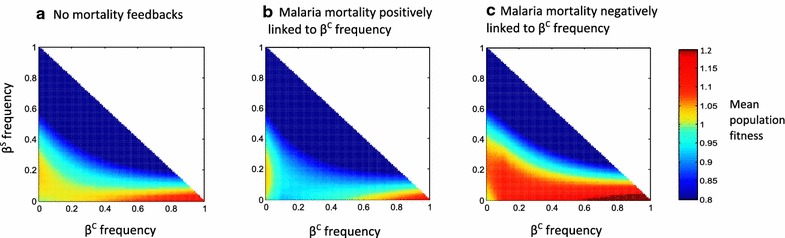
The combined effect of βC and βS frequencies on overall population fitness. The colours in each panel indicate the mean fitness of a population with a specific combination of βC frequency (x-axis) and βS frequency (y-axis), relative to the fitness of an AA individual in a population of only AA individuals. The malaria mortality function applied in a is f 1, where x = 0.01, z = 0.015 and γ = 0; the malaria mortality function applied in b is f 1, where x = 0.01, z = 0.015 and γ = 10, and the malaria mortality function applied in c is f 2, where x = 0.01, z = 0.015 and γ = 10. In all three panels, u = p
Discussion
These results demonstrate that a link between the frequency of βC or βS and the strength of malaria selection can change the outcome of the competitive interaction between these two malaria protective alleles. If there is a positive relationship between βC or βS frequencies and malaria selection, then the allele that offers more protection in the heterozygous state (βS) will be favoured.
Both βS and βC are point mutations. However, βS is caused by a A→T mutation (a transversion from a purine to a pyrimidine), whilst βC is caused by a G→A mutation (a transition between purines). Transitions occur at a higher rate than transversions [29]: the βC substitution should, therefore, arise spontaneously at a higher rate than the βS substitution. Given this discrepancy, the relative absence of βC in malarious regions is all the more surprising. Even if, as Modiano et al. pointed out [20], βC needs a longer time to establish itself, should it not have had more opportunities to do so? An increase in malaria-related selection pressure with increasing βC or βS frequencies could be precisely the mechanism required to account for the preponderance of βS. Furthermore, the behaviour exhibited by the population genetic framework presented here includes the elimination of βC even after it reaches a relatively high frequency. It is possible, therefore, that βC dominated a much larger area of West Africa historically before βS arrived.
Gametocytogenesis in P. falciparum is still poorly understood [30], so the processes underlying increased gametocyte prevalence in the presence of βC [24] and βS [31] are unknown. It is possible that the presence of haemoglobin S or HbC is associated with a harsh environment for parasite development, and that this stimulates P. falciparum to commit to the sexual stage. Previous studies have suggested that rodent and avian malaria parasites’ transmission-related phenotypes (conversion rate and sex ratio) change in response to a deterioration of the blood environment [32–34]. Trager et al. [35] have shown that P.falciparum parasites formed up to seven times more gametocytes in reticulocyte-rich blood from individuals with sickle cell anaemia compared to control blood. Understanding this phenotypic plasticity is a central part of understanding the transmission biology of malaria parasites.
The relationship between clinical severity and transmission potential during malaria infections is far from clear, and the model presented here was not intended to explore this question. Hypothetically, however, if (i) severe disease is caused by a subset of particularly virulent parasite strains, e.g., strains with cytoadherence properties that favour sequestration in vital organs, and (ii) virulence is associated with increased transmission, as has been demonstrated for rodent malarias [36], it is conceivable that the very presence of HbS and HbC in a population could encourage the circulation of more virulent and transmissible parasites. Gupta & Hill have shown that the presence of a host allele that confers resistance to death from infection can increase the likelihood of a virulent (and more transmissible) pathogen strain persisting, despite competition from less virulent strains [37]. The presence of inherently more virulent and transmissible parasites in populations containing either HbS or HbC could be a further factor increasing malaria selection wherever HbS or HbC are spreading. As shown by the results presented here, any increase in malaria selection under such circumstances favours the ultimate success of HbS over HbC.
The framework presented here demonstrates a point of principle. There are two obvious ways in which this work can be extended: (i) the incorporation of parasite strains that differ in their virulence and transmissibility, enabling the consequences of feedbacks between βC, βS, virulence and transmissibility to be explored; (ii) the extension of this model into a metapopulation framework, which would allow the inclusion of spatial heterogeneities in malaria selection pressure. Further studies are also needed to place the observed effects of haemoglobin variants on malaria transmissibility [23] into their full epidemiological context. Studies controlling for factors influencing transmission intensity (e.g., the spatial and temporal distribution of anopheline mosquitoes) and comparing malaria infection rates, malaria mortality rates and βC and βS frequencies in different communities will help to establish the strength and direction of the effects of βC and βS on malaria dynamics in different transmission environments.
Conclusions
The population genetic model presented here demonstrates that a positive relationship between the frequency of either βC or βS and malaria selection intensity favours the predominance of βS. Recent observations that both of these mutations are associated with increased malaria transmission potential [23–25, 31] may, therefore, help to account for the fact that βS attains high frequencies throughout sub Saharan Africa, whilst high frequencies of βC are limited to parts of West Africa.
In the long term, understanding the mechanisms underlying the influence of βC and βS on gametocyte levels and infectivity will provide important insights not only for understanding the evolutionary genetics of malaria but also for public health. If higher frequencies of βC and βS enhance transmission, targeted transmission blocking strategies in populations prone to infect more mosquitoes could be part of malaria intervention programmes.
Authors’ contributions
BPG, SG and BSP conceived the study. BPG, SG and BSP designed the analysis. BPG and BSP performed the analysis and wrote the manuscript. All authors read and approved the final manuscript.
Acknowledgements
B.S.P. was supported by a Sir Henry Wellcome Postdoctoral Fellowship (Grant 096063/Z/11/Z) and a Junior Research Fellowship at Merton College. S.G. is a Royal Society Wolfson Research Fellow and an ERC advanced investigator (DIVERSITY).
Competing interests
The authors declare that they have no competing interests.
Additional file
10.1186/s12936-015-1077-5 Supplementary Methods and Supplementary Tables.
Contributor Information
Bronner P. Gonçalves, Email: bronner.goncalves@lshtm.ac.uk
Sunetra Gupta, Email: sunetra.gupta@zoo.ox.ac.uk.
Bridget S. Penman, Phone: +44(0)1865 271132, Email: bridget.penman@zoo.ox.ac.uk
References
- 1.Williams TN. Human red blood cell polymorphisms and malaria. Curr Opin Microbiol. 2006;9:388–394. doi: 10.1016/j.mib.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 2.Taylor SM, Parobek CM, Fairhurst RM. Haemoglobinopathies and the clinical epidemiology of malaria: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:457–468. doi: 10.1016/S1473-3099(12)70055-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Modiano D, Luoni G, Sirima BS, Simpore J, Verra F, Konate A, et al. Haemoglobin C protects against clinical Plasmodium falciparum malaria. Nature. 2001;414(6861):305–308. doi: 10.1038/35104556. [DOI] [PubMed] [Google Scholar]
- 4.Lopera-Mesa TM, Doumbia S, Konate D, Anderson JM, Doumbouya M, Keita AS, et al. Impact of red blood cell variants on childhood malaria in Mali: a prospective cohort study. Lancet Haematol. 2015;2:e140–e149. doi: 10.1016/S2352-3026(15)00043-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fairhurst RM, Fujioka H, Hayton K, Collins KF, Wellems TE. Aberrant development of Plasmodium falciparum in hemoglobin CC red cells: implications for the malaria protective effect of the homozygous state. Blood. 2003;101:3309–3315. doi: 10.1182/blood-2002-10-3105. [DOI] [PubMed] [Google Scholar]
- 6.Fairhurst RM, Baruch DI, Brittain NJ, Ostera GR, Wallach JS, Hoang HL, et al. Abnormal display of PfEMP-1 on erythrocytes carrying haemoglobin C may protect against malaria. Nature. 2005;435:1117–1121. doi: 10.1038/nature03631. [DOI] [PubMed] [Google Scholar]
- 7.Verra F, Simpore J, Warimwe GM, Tetteh KK, Howard T, Osier FH, et al. Haemoglobin C and S role in acquired immunity against Plasmodium falciparum malaria. PLoS One. 2007;2:e978. doi: 10.1371/journal.pone.0000978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mangano VD, Kabore Y, Bougouma EC, Verra F, Sepulveda N, Bisseye C, et al. Novel insights into the protective role of Hemoglobin S and C against Plasmodium falciparum parasitemia. J Infect Dis. 2015;212:626–634. doi: 10.1093/infdis/jiv098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Billo MA, Johnson ES, Doumbia SO, Poudiougou B, Sagara I, Diawara SI, et al. Sickle cell trait protects against Plasmodium falciparum infection. Am J Epidemiol. 2012;176:S175–S185. doi: 10.1093/aje/kws323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cholera R, Brittain NJ, Gillrie MR, Lopera-Mesa TM, Diakite SA, Arie T, et al. Impaired cytoadherence of Plasmodium falciparum-infected erythrocytes containing sickle hemoglobin. Proc Natl Acad Sci USA. 2008;105:991–996. doi: 10.1073/pnas.0711401105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams TN, Mwangi TW, Roberts DJ, Alexander ND, Weatherall DJ, Wambua S, et al. An immune basis for malaria protection by the sickle cell trait. PLoS Med. 2005;2:e128. doi: 10.1371/journal.pmed.0020128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pasvol G, Weatherall DJ, Wilson RJ. Cellular mechanism for the protective effect of haemoglobin S against P. falciparum malaria. Nature. 1978;274:701–703. doi: 10.1038/274701a0. [DOI] [PubMed] [Google Scholar]
- 13.Shear HL, Roth EF, Jr, Fabry ME, Costantini FD, Pachnis A, Hood A, et al. Transgenic mice expressing human sickle hemoglobin are partially resistant to rodent malaria. Blood. 1993;81:222–226. [PubMed] [Google Scholar]
- 14.LaMonte G, Philip N, Reardon J, Lacsina JR, Majoros W, Chapman L, et al. Translocation of sickle cell erythrocyte microRNAs into Plasmodium falciparum inhibits parasite translation and contributes to malaria resistance. Cell Host Microbe. 2012;12:187–199. doi: 10.1016/j.chom.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duflo B, Maiga I, Pichard E, Diallo D, Diallo AN, Coulibaly T, et al. [Hemoglobin C in a hospital milieu in Bamako (Mali)](in French) Bull Soc Pathol Exot. 1985;78:393–400. [PubMed] [Google Scholar]
- 16.Piel FB, Howes RE, Patil AP, Nyangiri OA, Gething PW, Bhatt S, et al. The distribution of haemoglobin C and its prevalence in newborns in Africa. Sci Rep. 2013;3:1671. doi: 10.1038/srep01671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piel FB, Patil AP, Howes RE, Nyangiri OA, Gething PW, Williams TN, et al. Global distribution of the sickle cell gene and geographical confirmation of the malaria hypothesis. Nat Commun. 2010;1:104. doi: 10.1038/ncomms1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.May J, Evans JA, Timmann C, Ehmen C, Busch W, Thye T, et al. Hemoglobin variants and disease manifestations in severe falciparum malaria. JAMA. 2007;297:2220–2226. doi: 10.1001/jama.297.20.2220. [DOI] [PubMed] [Google Scholar]
- 19.Nagel RL, Fabry ME, Steinberg MH. The paradox of hemoglobin SC disease. Blood Rev. 2003;17:167–178. doi: 10.1016/S0268-960X(03)00003-1. [DOI] [PubMed] [Google Scholar]
- 20.Modiano D, Bancone G, Ciminelli BM, Pompei F, Blot I, Simpore J, et al. Haemoglobin S and haemoglobin C: ‘quick but costly’ versus ‘slow but gratis’ genetic adaptations to Plasmodium falciparum malaria. Hum Mol Genet. 2008;17:789–799. doi: 10.1093/hmg/ddm350. [DOI] [PubMed] [Google Scholar]
- 21.Drakeley C, Sutherland C, Bousema JT, Sauerwein RW, Targett GA. The epidemiology of Plasmodium falciparum gametocytes: weapons of mass dispersion. Trends Parasitol. 2006;22:424–430. doi: 10.1016/j.pt.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 22.Talman AM, Domarle O, McKenzie FE, Ariey F, Robert V. Gametocytogenesis: the puberty of Plasmodium falciparum. Malar J. 2004;3:24. doi: 10.1186/1475-2875-3-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gouagna LC, Bancone G, Yao F, Yameogo B, Dabire KR, Costantini C, et al. Genetic variation in human HBB is associated with Plasmodium falciparum transmission. Nat Genet. 2010;42:328–331. doi: 10.1038/ng.554. [DOI] [PubMed] [Google Scholar]
- 24.Ringelhann B, Hathorn MK, Jilly P, Grant F, Parniczky G. A new look at the protection of hemoglobin AS and AC genotypes against Plasmodium falciparum infection: a census tract approach. Am J Hum Genet. 1976;28:270–279. [PMC free article] [PubMed] [Google Scholar]
- 25.Robert V, Tchuinkam T, Mulder B, Bodo JM, Verhave JP, Carnevale P, et al. Effect of the sickle cell trait status of gametocyte carriers of Plasmodium falciparum on infectivity to anophelines. Am J Trop Med Hyg. 1996;54:111–113. doi: 10.4269/ajtmh.1996.54.111. [DOI] [PubMed] [Google Scholar]
- 26.Feng Z, Smith DL, McKenzie FE, Levin SA. Coupling ecology and evolution: malaria and the S-gene across time scales. Math Biosci. 2004;189:1–19. doi: 10.1016/j.mbs.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 27.Cavalli-Sforza LL, Bodmer WF. The genetics of human populations. San Francisco: WH Freeman; 1971. [Google Scholar]
- 28.Snow RW, Omumbo JA, Lowe B, Molyneux CS, Obiero JO, Palmer A, et al. Relation between severe malaria morbidity in children and level of Plasmodium falciparum transmission in Africa. Lancet. 1997;349:1650–1654. doi: 10.1016/S0140-6736(97)02038-2. [DOI] [PubMed] [Google Scholar]
- 29.Nachman MW, Crowell SL. Estimate of the mutation rate per nucleotide in humans. Genetics. 2000;156:297–304. doi: 10.1093/genetics/156.1.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker DA. Malaria gametocytogenesis. Mol Biochem Parasitol. 2010;172:57–65. doi: 10.1016/j.molbiopara.2010.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lawaly YR, Sakuntabhai A, Marrama L, Konate L, Phimpraphi W, Sokhna C, et al. Heritability of the human infectious reservoir of malaria parasites. PLoS One. 2010;5:e11358. doi: 10.1371/journal.pone.0011358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paul RE, Brey PT. Malaria parasites and red blood cells: from anaemia to transmission. Mol Cells. 2003;15:139–149. [PubMed] [Google Scholar]
- 33.Reece SE, Duncan AB, West SA, Read AF. Host cell preference and variable transmission strategies in malaria parasites. Proc Biol Sci. 2005;272:511–517. doi: 10.1098/rspb.2004.2972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reece SE, Ramiro RS, Nussey DH. Plastic parasites: sophisticated strategies for survival and reproduction? Evol Appl. 2009;2:11–23. doi: 10.1111/j.1752-4571.2008.00060.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trager W, Gill GS, Lawrence C, Nagel RL. Plasmodium falciparum: enhanced gametocyte formation in vitro in reticulocyte-rich blood. Exp Parasitol. 1999;91:115–118. doi: 10.1006/expr.1998.4347. [DOI] [PubMed] [Google Scholar]
- 36.Mackinnon MJ, Read AF. Genetic relationships between parasite virulence and transmission in the rodent malaria Plasmodium chabaudi. Evolution. 1999;53:689–703. doi: 10.2307/2640710. [DOI] [PubMed] [Google Scholar]
- 37.Gupta S, Hill AV. Dynamic interactions in malaria: host heterogeneity meets parasite polymorphism. Proc Biol Sci. 1995;261:271–277. doi: 10.1098/rspb.1995.0147. [DOI] [PubMed] [Google Scholar]


