Abstract
Background:
One complication of anteroinferior glenohumeral shoulder dislocation is a critical bone defect that requires surgical repair to prevent recurrent instability. However, controversy exists regarding the surgical management because both open and arthroscopic surgeries have respective advantages and disadvantages. Moreover, it is difficult to determine the patient’s preferred treatment, as factors that influence treatment choice include recurrence rates, morbidity of the procedures, and patient preferences.
Hypothesis:
Patients who have a higher probability of recurrent instability after arthroscopic surgery will select open surgery whereas patients with a lower probability of recurrent instability after arthroscopic surgery will favor arthroscopy.
Study Design:
Economic and decision analysis; Level of evidence, 2.
Methods:
A decision tree was constructed to model each hypothetical outcome after open or arthroscopic surgery for glenohumeral instability in patients with bone defects. A literature review was performed to determine the probability of occurrence for each node while utility values for each outcome were obtained via patient-administered surveys given to 50 patients without prior history of shoulder injury or dislocation. Fold-back analysis was then performed to show the optimal treatment strategy. Finally, sensitivity analysis established the thresholds at which open treatment becomes the optimal treatment.
Results:
The ultimate expected value—the objective evaluation of all potential outcomes after choosing either open or arthroscopic surgery—was found to be greater for arthroscopic surgery than for open surgery (87.17 vs 81.64), indicating it to be the preferred treatment. Results of sensitivity analysis indicated that open surgery becomes the preferred treatment when probability of recurrence after arthroscopic treatment is ≥23.8%, although varying the utility, defined as an aggregate patient preference for a particular outcome, has no effect on the model. When the rate of no complication after open surgery is 97.6%, open surgery becomes the patient’s preferred treatment.
Conclusion:
Arthroscopic surgery is an acceptable treatment if recurrent instability occurs consistently at ≤23.8%. This has important implications given the technical difficulty of successfully performing arthroscopic fixation to resolve recurrent anteroinferior glenohumeral dislocations associated with critical osseous defects. However, due to a lack of clinical outcomes studies, more research is needed to better predict the optimal operative treatment.
Keywords: shoulder instability, shoulder dislocation, Latarjet, arthroscopic, decision analysis, glenoid
The proper management of first-time traumatic anterior glenohumeral dislocation is a subject of much debate. Traditional treatment has included nonoperative immobilization of the joint, although studies have shown that there is a high rate of recurrence in these patients, especially in young athletes.23 As a result, both open and arthroscopic surgical techniques that repair the capsule and labrum are commonly used as a primary operative procedure.18
A large volume of previous research has compared the effectiveness of different surgical treatments to repair the labrum, including various open and arthroscopic techniques2,34,36; however, one of the major factors that contributes to the failure of these soft tissue repairs is the presence of bone damage in the glenohumeral joint. Acute fracture of the anteroinferior glenoid can occur, as well as chronic attrition of the anterior glenoid with multiple dislocations. A Hill-Sachs lesion, an impaction of the humeral head where it contacts the glenoid during dislocation, can also occur.17 These bone defects increase in size with recurrent dislocations. Larger bone defects are associated with higher recurrence rates after soft tissue reconstruction,15,25 so some surgeons have recommended surgery to address bone injury at the time of the initial operation.
There is significant controversy regarding this management decision because most clinicians and investigators agree that open procedures to address bone loss have greater morbidity than arthroscopic procedures, but arthroscopic procedures in the presence of bone loss have greater postoperative treatment failures (recurrent instability) than open procedures.3 Even though it is an arthroscopic procedure, remplissage is still aimed at addressing humeral bone loss by suturing the infraspinatus muscle into the Hill-Sachs lesion, and it still may have additional morbidity compared with standard arthroscopic labrum repair. For example, this procedure has been associated with postoperative loss of motion and infraspinatus strength deficits.9 Therefore, making a decision about what type of surgery is best for the patient is difficult.
The application of expected value decision analysis to medical decision making is a borrowed approach from economic analysis that involves the construction and subsequent analysis of a decision tree to guide optimal decision making when faced with uncertainty. In this technique, given outcomes, each with distinct utility values and probabilities of occurrence, are created for a primary situation in which there is uncertainty. Following construction of a model, a technique known as “fold-back analysis” can be performed, which evaluates the model and elucidates the optimal decision. Afterward, sensitivity analysis allows for relative manipulation of both probabilities and utility values in the decision tree, allowing the investigator to highlight the effect of varying probabilities and utilities on optimal decision strategy.
The intent of this study was to use the technique of expected value decision analysis to determine whether arthroscopic or open treatment is the optimal surgical treatment choice for primary anterior glenohumeral shoulder instability with a “critical bone defect.” In addition, a secondary goal was to identify which patient utility values and potential terminal nodes are most influential on optimal decision making. It was hypothesized that patients who preoperatively have a high probability of recurrent instability after arthroscopic surgery would, in fact, be more likely to select open surgery, while patients with a low probability of recurrent instability after arthroscopic surgery would choose arthroscopic treatment.
Methods
Outcome Probabilities
A critical component to modeling any decision tree with the technique of decision analysis requires one to determine the occurrence probabilities for each terminal node in the decision tree. For our project, to determine these probabilities, a literature review for recurrent anterior glenohumeral dislocation with “critical bone defects” was performed using the PubMed database from 1970 to January 2014. The search criterion used variations of recurrent shoulder dislocation, critical bone defect, glenohumeral instability, Bristow-Latarjet, bony Bankart, arthroscopic Bankart repair, glenoid, and surgery. Critical bone defects were loosely defined as a bony Bankart lesion comprising at least 25% of the glenoid rim, although 2 articles that were included in the review were less clear as to the definition of critical bone defect.27,40 Numerous articles were discarded due to bone defect cohorts with less than 25% glenoid deficiency.§ Additional articles looking at both arthroscopic and open surgery were not included in the final literature review data as these articles did not independently report the final postoperative outcomes of the critical bone defect cohort subset.5 Articles were discarded if they described a novel surgical approach to the glenoid, such as the 2B3 approach described by Boileau et al,8 but were included if they described a novel bone graft technique (eg, iliac crest craft).46 Most open and arthroscopic techniques described were variations of the coracoid transfer initially described independently by Bristow22 and Latarjet.30 Mean follow-up varied between studies, but was at minimum 5 months24 with an overall mean follow-up among all 14 articles of 42.23 months.||
To calculate the probabilities of occurrence for each terminal node in the decision tree, each study was reviewed for outcome data after either arthroscopic or open repair for critical osseous deficits with anterior glenohumeral instability. Probabilities for both open and arthroscopic repair were calculated independently by dividing the aggregate sum of occurrences for a given outcome by the total number of shoulders for the given operative course such that the sum of probabilities for all terminal nodes for both open and arthroscopic surgery equaled 1. For both arthroscopic and open repair, “no complications” was defined as no further episodes of subluxation or recurrent dislocation following surgical repair, while “recurrence” was defined as 1 or more episodes of subluxation or dislocation following surgery. “Infection” was noted per each individual study, and “stiffness” was broadly defined as any decrease in the range of motion postoperatively. For open repair, a fifth outcome—nerve damage—was added because of the inherent increased risk for damage to the musculocutaneous nerve during an open bone grafting procedure. Per the model, any given shoulder could only have 1 independent outcome (ie, infection could not also be recurrent instability).
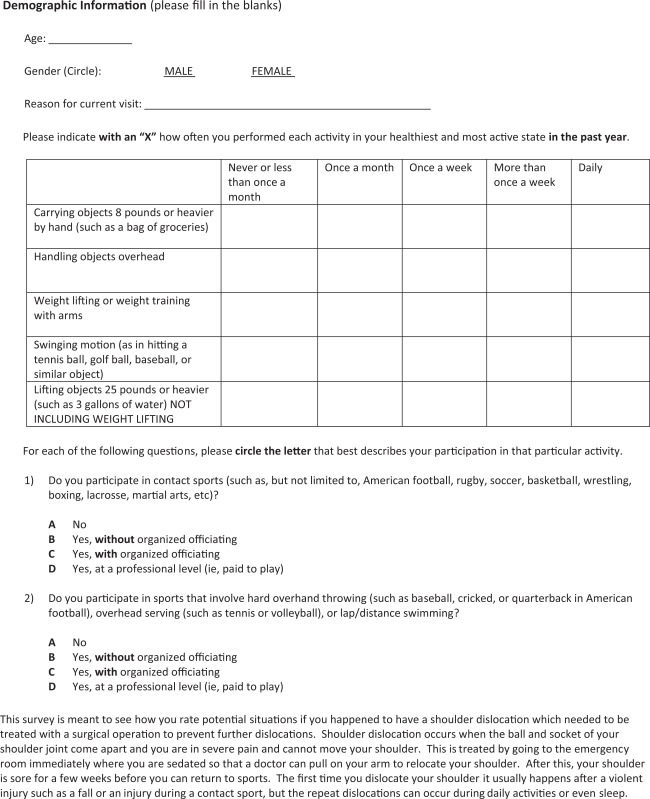
Utilities
Utility refers to a value assigned to patient preferences given a specific outcome. In this study, following expedited institutional review board approval, utility values were obtained via direct survey of 50 ambulatory orthopaedic patients at a tertiary care orthopaedic sports clinic. Patients were aged 18 to 35 years so as to most closely represent the age groups with the highest prevalence of recurrent instability after arthroscopic surgery.28,32 The survey was designed with a visual number line utility score, as that has been shown to be most effective as per Parkin and Devlin39 (see the Appendix). Subjects who had a prior history of dislocation, subluxation, shoulder surgery, or other shoulder injury were excluded from participation to limit positive or negative bias in the subject’s ability to assign utility values. In addition, the survey included the shoulder activity scale described by Brophy et al14 to correlate utility values, with individual activity levels ranging from a minimum score of 5 to maximum of 20. The survey presented hypothetical scenarios after recurrent anterior glenohumeral instability that represented terminal end points in the decision tree. Participants were asked to identify their utility preferences by both vertical line and associated number. The scale was prefaced by a predetermined best outcome (arthroscopic surgery followed by no recurrent instability) and worst outcome (open surgery followed by recurrent instability) at 100 and 0, respectively. The parameter for best outcome was chosen because it combined the optimal surgical outcome (resolution of instability with no postoperative complications or recurrence) with the least morbid intervention technique (arthroscopy). This similar methodology was applied in selecting the worst possible outcome, as this option combined recurrent postoperative instability with the most morbid operative technique (open surgery). For survey responses that did not include a value associated with the number line, the primary reviewer assessed the utility value and then a second reviewer independently assessed the same survey. Discrepant measures were averaged if found. After data collection, the average response for each utility outcome was calculated and applied to the initial decision tree construction and subsequent fold-back analysis.
Decision Tree and Fold-Back Analysis
The decision tree was constructed with 1 decision node, 2 chance nodes, and 9 outcome nodes. Per convention, time was not modeled because the events are discrete and the decision occurs over an acute period. The standard way to display a decision tree involves the corresponding utility value to be placed to the right of its outcome node while the probability of that outcome be placed underneath the node.
Fold-back analysis was performed by multiplying the utility value for the given outcome by its probability of occurrence. This provided the “expected value” for the terminal node. To determine the optimal decision course, the expected values for each independent outcome node of both chance nodes (open vs arthroscopic surgery) were summated to create an “ultimate expected value.” This value allowed for comparison of both potential choices, as the highest ultimate expected value is the optimal decision choice.
Sensitivity Analysis
One-way sensitivity analysis was performed to determine the importance of each variable to the decision tree model and also to determine the effect of changing probability values on the optimal treatment outcome. Manipulating the probability of occurrence for arthroscopic surgery followed by recurrent dislocation was the primary focus during analysis to identify the precise probability of recurrent instability after arthroscopic surgery at which the optimal treatment outcome changes (“threshold value”). Furthermore, 1-way sensitivity analysis was performed on open surgery with no recurrence, open surgery with nerve damage, and arthroscopic surgery with no recurrence.
Two-way sensitivity analysis is a similar technique that is used to evaluate the effect of simultaneously changing 2 discrete variables on the overall outcome of the model. This analysis technique was employed primarily to determine the preferential treatment outcome while varying the probabilities of open surgery and no complication with arthroscopic surgery and recurrent instability. Throughout this analysis, utility values were largely held constant and not evaluated with 1-way and 2-way sensitivity analysis with the exception for the node defined as arthroscopic surgery followed by recurrent instability. This utility value was analyzed since the primary focus of the sensitivity analysis was to determine the threshold value between arthroscopic surgery with recurrence and open surgery without recurrence.
Results
Probabilities
Following the search strategy outlined in the methods, 9 articles were found that pertained to open surgical treatment for glenoid osseous critical bone defects, while 5 articles were found that pertained to arthroscopic surgical treatment (Tables 1 and 2). In total, there were 240 shoulders that underwent open treatment, of which 91.3% had no recurrence or complication, 5.8% had recurrent instability, 0.8% had infection, 2.1% had stiffness, and 0% had nerve damage. In contrast, there were 186 shoulders that underwent arthroscopic treatment, of which 81.7% had no recurrence or complication, 16.1% had recurrent instability, 0% had infection, and 2.2% had stiffness.
TABLE 1.
Probability Values for Arthroscopic Surgery and Associated Outcomes
TABLE 2.
Probability Values for Open Surgery and Associated Outcomes
| Outcome | Auffarth et al4 | Burkhart et al16 | Warner et al46 | Weng et al47 | Khazzam et al26 | Scheibel et al42 | Pagnani37 | Hovelius et al24 | DiPaola et al19 | Total Shoulders | Probabilities |
|---|---|---|---|---|---|---|---|---|---|---|---|
| No complications | 42 | 97 | 9 | 7 | 10 | 10 | 4 | 36 | 4 | 219 | .913 |
| Recurrent instability | 0 | 5 | 0 | 2 | 0 | 0 | 0 | 7 | 0 | 14 | .058 |
| Infection | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | .008 |
| Stiffness | 3 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | .021 |
| Nerve damage | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | .000 |
| Total | 47 | 102 | 11 | 9 | 10 | 10 | 4 | 43 | 4 | 240 | 1.000 |
Utilities
The mean age for the survey respondents was 25.38 years; 18 respondents were women while the remaining 32 were men. Mean Brophy shoulder activity score was 12.94. A complete listing of utility values including predetermined best and worst outcomes (arthroscopic surgery with no complication and open surgery with recurrent instability) with associated SDs can be found in Table 3. The population surveyed was similar in age and activity to populations previously analyzed for recurrent instability,6 although there was a lower male:female ratio (16:9) than previously described. Many of the utilities obtained through the patient survey were found to have large SDs (Table 3). This was not considered to be a major concern for fold-back analysis given the relatively low probabilities of occurrence for these nodes, and thus, their relative lack of contribution to the ultimate expected value of the model.
TABLE 3.
Utility Values From Survey Responses
| Utility | Response, mean ± SD |
| Arthroscopic + no complicationa | 100 ± 0 |
| Open + recurrent instabilityb | 0 ± 0 |
| Arthroscopic + recurrent instability | 28.08 ± 24.85 |
| Arthroscopic + infection | 52.9 ± 30.26 |
| Arthroscopic + stiffness | 43.02 ± 24.54 |
| Open + no complication | 88.34 ± 18.04 |
| Open + nerve damage | 18.26 ± 21.71 |
| Open + infection | 37.36 ± 30.71 |
| Open + stiffness | 32.72 ± 22.76 |
aPredetermined scenario with given maximum utility value (100).
bPredetermined scenario with given minimum utility value (0).
Decision Analysis
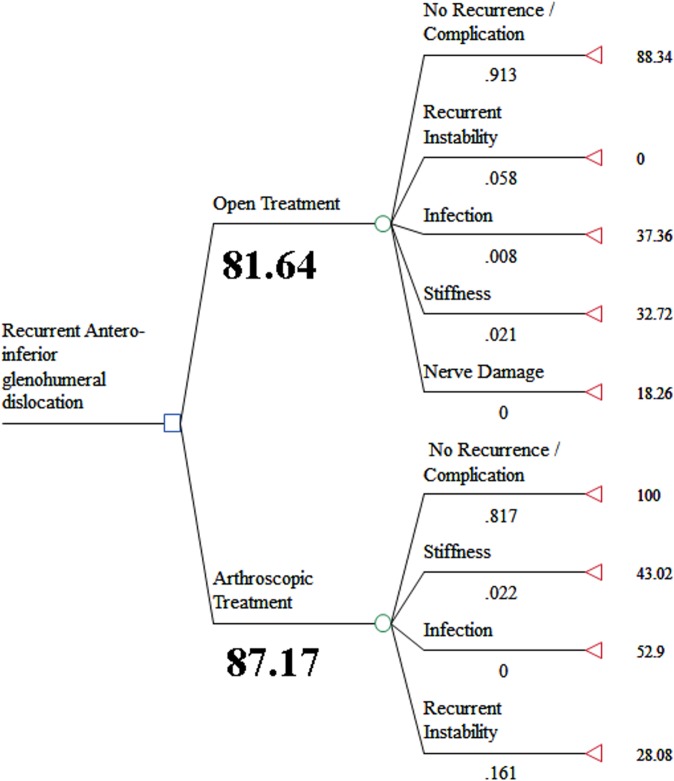
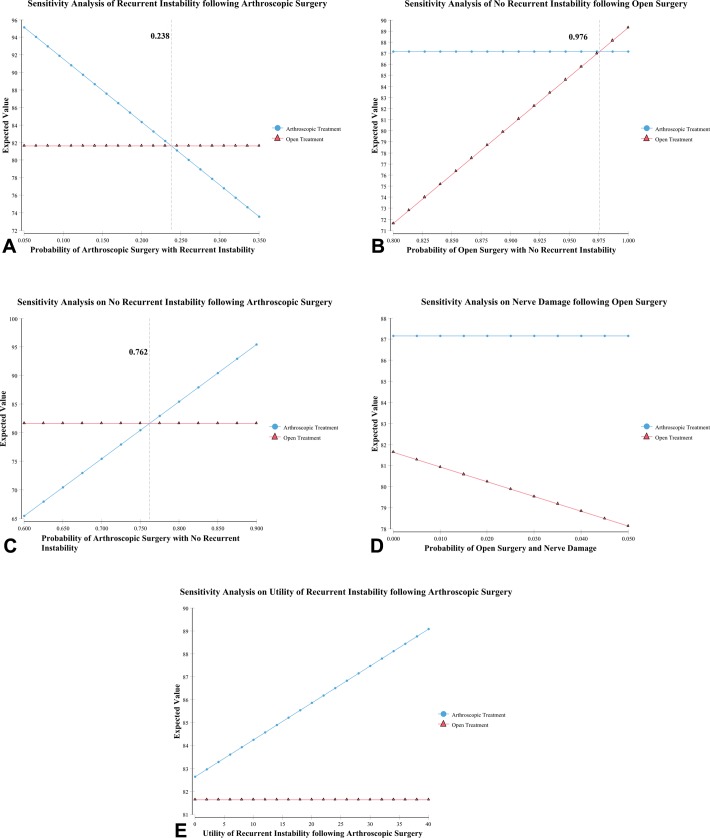
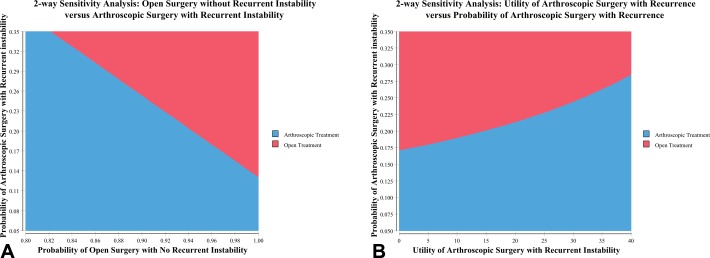
Fold-back analysis on the initial decision tree revealed the ultimate expected value for arthroscopic surgery to be 87.17 and the ultimate expected value for open surgery to be 81.64 (Figure 1), indicating arthroscopic treatment to be preferred. One-way sensitivity analysis of arthroscopic surgery followed by recurrent instability indicated a probability threshold value of 0.238 (Figure 2A), demonstrating that when the probability of recurrent instability following arthroscopic surgery eclipses 23.8%, the desired course is no longer arthroscopic fixation but rather open treatment. Probability threshold values for open surgery without recurrence and arthroscopic surgery without recurrence were 0.976 (Figure 2B) and 0.762 (Figure 2C), respectively. These values indicate that when either the probability of open surgery without complication is 97.6% or the probability of arthroscopic surgery without complication is only 76.2%, the desired treatment choice changes from arthroscopic to open surgery. No probability threshold value for open surgery followed by nerve damage was obtained, indicating that arthroscopic stabilization is the patient’s preferred treatment irrespective of the probability of occurrence of nerve damage after open stabilization. This lack of threshold value was primarily due to the low utility value (18.26) that patients assigned to this scenario; given an understanding of expected value decision analysis, it becomes clear that a low utility value for a terminal node combined with a low probability of occurrence for that same node will have little, if any, effect on the overall model. One-way sensitivity analysis was also performed on the utility value for arthroscopic surgery with recurrent instability, but yielded no threshold value (Figure 2D). Two-way sensitivity analysis was performed to determine the effect on the model of changing 2 variables simultaneously. The probability values for open surgery without recurrence and arthroscopic surgery with recurrence were varied in accordance with 2-way sensitivity analysis (Figure 3A), while both the probability of arthroscopic surgery with recurrent instability and the utility value for that event were also analyzed (Figure 3B). By comparing probability values for open surgery without recurrence to arthroscopic surgery with recurrence, there appears a general inverse relationship indicating that as open fixation becomes more successful (ie, less recurrence), the probability of arthroscopic surgery with recurrence must similarly decrease to remain the preferred surgical method. Likewise, there was a general positive correlation when comparing the probability of arthroscopic surgery with recurrent instability with the utility of arthroscopic surgery with recurrent instability, implying that as the recurrence after arthroscopic surgery increases, so too must the patient utility for that event if arthroscopic surgery is to remain the patient’s preferred treatment.
Figure 1.
Initial decision tree surrounding optimal treatment following primary anteroinferior glenohumeral dislocation revealing 1 decision node (blue square), 2 chance nodes (green circles), and 9 terminal nodes (red triangles). The numbers listed to the right of the terminal nodes are the utility values for the corresponding terminal node, while the probability of occurrence for that node is located below the line segment. The numbers listed below the chance nodes indicate the ultimate expected value for the decision path, clearly indicating arthroscopic treatment as the optimal treatment.
Figure 2.
One-way sensitivity analysis showing threshold values for instability after (A) arthroscopic surgery and (B) open surgery without complication or instability. One-way sensitivity analysis showing threshold values for (C) arthroscopic surgery without instability or complication and (D) open surgery with nerve damage. (E) One-way sensitivity analysis showing no threshold value for the utility of recurrent instability after arthroscopic surgery.
Figure 3.
Two-way sensitivity analysis for (A) the probability of recurrent instability after arthroscopic surgery and open surgery without recurrent instability and (B) utility of recurrent instability after arthroscopic surgery and probabilities of recurrent instability after arthroscopic surgery.
Discussion
The optimal management for anterior glenohumeral instability with a critical osseous defect remains controversial. While arthroscopic labrum repair allows for treatment with less morbidity, there is a considerably higher probability for recurrent instability. In contrast, open treatment has less risk of recurrent instability while having increased morbidity. Our study utilized decision analysis techniques to assess patient preferences for various treatment outcomes and to develop a decision tree model, and we concluded that arthroscopic treatment is preferred for the treatment of patients with critical bone defects as long as the risk of recurrent instability is less than 23.8%. Patients seem to be willing to accept the risk of recurrent surgery or failure if the success rate is approximately 75% or greater. This value is consistent with recent studies that have highlighted the need for open surgery as a primary treatment option with glenoid osseous defects due to the correlation with recurrent instability.42,47 The problem is determining what a critical osseous defect is and how an isolated glenoid or humeral defect or a combination of the 2 affects the failure rate of surgery. Therefore, it is important to better define the relationship between bone defects and recurrent instability in future research so that patients can be better selected for either arthroscopic or open treatment and they can therefore make better informed decisions about their surgery.
We found that when the combined complication rates (including recurrence) after open surgery are less than 2.4% (corresponding to a probability threshold value of 0.976), then open surgery is preferable to arthroscopic surgery. While this represents a low complication and recurrence rate, this value is still feasible, as large cohorts have been previously described with similar success rates without complication.13,15 This is a critical conclusion that similarly warrants continued research to create open fixation techniques that have both successful and reproducible outcomes.
While varying probability threshold values were important, so too was modeling threshold utility values because it seems plausible that some individuals may prefer open surgery to arthroscopic surgery, largely because of the lower chance of recurrent instability. However, modeling this scenario demonstrated no threshold utility value where the expected value for open surgery was greater than that for arthroscopic surgery (see Figure 2E). This surprising result is explained by the low rate of recurrent instability after arthroscopic surgery, as significant alterations to the model did not occur while utility values were manipulated because the low probability rate of this terminal node prevents it from having significant contributions to the overall model. Because of this result, 2-way sensitivity analysis was then performed in an attempt to model the relationship between the utility value and probability value for recurrent instability after arthroscopic surgery as both variables were simultaneously manipulated. This analysis yielded distinct combinations of both utilities and probabilities for which open surgery would be optimal (see Figure 3B), suggesting that higher values of instability after arthroscopic fixation are associated with lower utility values and, thus, allow for situations in which open treatment is the patient’s preferred surgical procedure.
Musculocutaneous nerve damage has traditionally been a concern for surgeons and a well-documented adverse effect of open shoulder surgery.12 It is interesting to note the terminal node defined as open surgery followed by nerve damage contributed little to the overall decision analysis because of the low utility value and probability of occurrence. While the probability of occurrence for this node obtained through the literature review of papers employing Latarjet specifically for shoulders with critical bone defects was 0, this value is likely underrepresentative of the actual patient population following open surgical fixation. However, even with sensitivity analysis, it was clear that no feasible probability value would enable this node to influence optimal decision of technique; it had no bearing on final outcome. Thus, one can conclude that while nerve damage is a feared outcome of open surgical fixation, it should not prevent surgeons from choosing this treatment option when it is the optimal treatment.
The results from the initial fold-back analysis indicated that arthroscopic surgery was the patient’s preferred management option for a patient with recurrent anteroinferior glenohumeral instability with a critical osseous defect. The data supporting this conclusion were obtained via the literature review and the patient-administered survey. This finding is surprising given the increasing number of research studies that advocate for open treatment for critical osseous deficits,10,15,24,31 although concrete treatment protocols are lacking due to individualized patient preferences,6 novel surgical techniques,1,4,46 and improved understanding of glenoid reconstruction.1,31 However, it is important to note that age and activity level were not directly modeled in this study. Age was indirectly involved in the utility scores by controlling the population to which the survey was administered and was also represented in the probability values through the studies used in the literature review. Similarly, activity level was presumably an indirect component in the utility values, as more active individuals expressed less utility for recurrence. Most important, however, was the inability to determine the direct effect of changes to the size of the critical bone defect to the model, as there is currently no research that allows for accurate prediction of recurrent instability associated with glenoid defects though correlation has been strongly suggested.1,15,31 It is important to remember, however, that patient preferences outside of those assessed in this study exist in the community, and it is important for the surgeon to elicit these from the patient prior to deciding on a particular operative intervention.
Anterior shoulder instability has previously been analyzed through the use of a similar decision analysis technique. A prior study published by Bishop et al6 focused on operative versus nonoperative care as the 2 initial decision nodes in the decision tree analysis. The authors concluded that the patient’s preferred treatment for primary anterior glenohumeral dislocation was arthroscopy, but they did not evaluate the differences in recurrence related to critical osseous defects, nor did they evaluate open versus arthroscopic surgery. It is important to note that osseous defects are quite common with anterior shoulder dislocation, and a relationship between defect and recurrent instability has been demonstrated previously.31
There are published studies that have reviewed open versus arthroscopic treatment for anterior glenohumeral instability in the setting of critical bone defect while also providing guidelines for management.1,11 Anakwenze et al1 discussed the effectiveness of open surgical fixation for glenoid repair and arthroscopic treatment for moderately sized humeral head defects. Bollier and Arciero11 advocated for open surgical fixation when glenoid loss eclipsed 20%, an engaging Hill-Sachs lesion was present, and the instability severity index score was greater than 6, and further advised either arthroscopic remplissage or open bone grafting for a Hill-Sachs lesion greater than 30%. These studies support our conclusion of open surgery as the patient’s preferred treatment for glenohumeral surgical repair given a high arthroscopic surgical failure rate; at the core of both studies was the effect of the critical bone defect on the treatment choice, indicating that arthroscopic surgery under these conditions produced a high recurrence rate. While both of these studies acknowledge the need for further research into the area of surgical fixation of critical bone defects, they do not address patient preferences or utility for a given treatment modality—something that has been considered in our analysis.
There were a few limitations that were encountered in this study. While the probability data were acquired through an exhaustive literature search, there were relatively few studies that discussed critical bone defects in the setting of anterior glenohumeral instability, and this paucity of literature has a potentially negative effect on both treatment modalities. Although studies have begun to address critical bone defects and even categorize glenoid osseous defects,5 there is still a lack of consensus regarding what constitutes a “critical bone defect.” Bigliani et al5 proposed a 25% osseous glenoid deficiency to be the defect necessary to characterize a critical bone defect, but even more important, there has yet to be an established relationship between the size of defect and recurrence after arthroscopic surgery. This is an extremely important undefined variable given the effect of this relationship to our model. As such, further research is warranted to not only universally define a critical bone defect, but also to better establish its effect on recurrent instability. Last, it is important to note that the advent of arthroscopic surgery to address critical glenoid bony defects is a technically demanding procedure, and the outcomes used in this study came from experienced shoulder surgeons, many of whom are pioneers with these techniques. As a result, these procedures may not necessarily be reproduced with similar success rates by other surgeons in the community.
The data from this study may help us to better understand the optimal surgical treatment for recurrent glenohumeral instability in the setting of a critical osseous defect. To determine optimal treatment, both the probability of a certain outcome happening and the individual’s utility for that outcome must be considered. Large defects have been associated with a higher probability of recurrent instability, and we conclude that the optimal treatment should be open surgery to address bone loss when the rate of arthroscopic recurrent instability eclipses 23.8%. Furthermore, it is important to have better outcome studies to predict the rate of recurrence with arthroscopic treatment based on patient osseous defects, as this would allow for accurate predictive modeling in the clinical setting. However, a strong patient-doctor relationship that emphasizes trust and collaboration will be crucial to achieving any successful outcome, as obtaining patient preferences can help elucidate the optimal surgical treatment.
Appendix. Critical Bone Defect Patient Utility Survey
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: R.J.M. received the Crile Fellowship, a competitive unrestricted stipend to support summer research between the first and second years of medical school at Case Western Reserve University, during which he worked on this project.
References
- 1. Anakwenze OA, Hsu JE, Abboud JA, Levine WN, Huffman GR. Recurrent anterior shoulder instability associated with bony defects. Orthopedics. 2011;34:538–544. [DOI] [PubMed] [Google Scholar]
- 2. Anakwenze OA, Huffman GR. Evaluation and treatment of shoulder instability. Phys Sportsmed. 2011;39:149–157. [DOI] [PubMed] [Google Scholar]
- 3. Ando A, Sugaya H, Takahashi N, Kawai N, Hagiwara Y, Itoi E. Arthroscopic management of selective loss of external rotation after surgical stabilization of traumatic anterior glenohumeral instability: arthroscopic restoration of anterior transverse sliding procedure. Arthroscopy. 2012;28:749–753. [DOI] [PubMed] [Google Scholar]
- 4. Auffarth A, Kralinger F, Resch H. Anatomical glenoid reconstruction via a J-bone graft for recurrent posttraumatic anterior shoulder dislocation. Oper Orthop Traumatol. 2011;23:453–461. [DOI] [PubMed] [Google Scholar]
- 5. Bigliani LU, Newton PM, Steinmann SP, Connor PM, Mcllveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med. 1998;26:41–45. [DOI] [PubMed] [Google Scholar]
- 6. Bishop JS, Crall TS, Kocher MS. Operative versus nonoperative treatment after primary traumatic anterior glenohumeral dislocation. J Shoulder Elbow Surg. 2012;21:e17–e18. [DOI] [PubMed] [Google Scholar]
- 7. Boileau P, Bicknell RT, El Fegoun AB, Chuinard C. Arthroscopic Bristow procedure for anterior instability in shoulders with a stretched or deficient capsule: the “belt-and-suspenders” operative technique and preliminary results. Arthroscopy. 2007;23:593–601. [DOI] [PubMed] [Google Scholar]
- 8. Boileau P, Mercier N, Old J. Arthroscopic Bankart-Bristow-Latarjet (2B3) procedure: how to do it and tricks to make it easier and safe. Orthop Clin North Am. 2010;41:381–392. [DOI] [PubMed] [Google Scholar]
- 9. Boileau P, O’Shea K, Vargas P, Pinedo M, Old J, Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am. 2012;94:618–626. [DOI] [PubMed] [Google Scholar]
- 10. Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755–1763. [DOI] [PubMed] [Google Scholar]
- 11. Bollier MJ, Arciero R. Management of glenoid and humeral bone loss. Sports Med Arthrosc. 2010;18:140–148. [DOI] [PubMed] [Google Scholar]
- 12. Bono CM, Grossman MG, Hochwald N, Tornetta P., III Radial and axillary nerves. Anatomic considerations for humeral fixation. Clin Orthop Relat Res. 2000;373:259–264. [PubMed] [Google Scholar]
- 13. Brilakis E, Mataragas E, Deligeorgis A, Maniatis V, Antonogiannakis E. Midterm outcomes of arthroscopic remplissage for the management of recurrent anterior shoulder instability [published online February 1, 2014]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-2848-1 [DOI] [PubMed] [Google Scholar]
- 14. Brophy RH, Beauvais RL, Jones EC, Cordasco FA, Marx RG. Measurement of shoulder activity level. Clin Orthop Relat Res. 2005;439:101–108. [DOI] [PubMed] [Google Scholar]
- 15. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic bankart repairs. Arthroscopy. 2000;16:677–694. [DOI] [PubMed] [Google Scholar]
- 16. Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23:1033–1041. [DOI] [PubMed] [Google Scholar]
- 17. Calandra JJ, Baker CL, Uribe J. The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations. J Arthrosc Relat Surg. 1989;5:254–257. [DOI] [PubMed] [Google Scholar]
- 18. DeLee JC, Drez D, Miller MD. Delee & Drez’s Orthopaedic Sports Medicine. 3rd ed Philadelphia, PA: Saunders; 2010. [Google Scholar]
- 19. DiPaola MJ, Jazrawi LM, Rokito AS, et al. Management of humeral and glenoid bone loss associated with glenohumeral instability. Bull NYU Hosp Jt Dis. 2010;68:245–250. [PubMed] [Google Scholar]
- 20. Franceschi F, Papalia R, Rizzello G, et al. Remplissage repair—new frontiers in the prevention of recurrent shoulder instability: a 2-year follow-up comparative study. Am J Sports Med. 2012;40:2462–2469. [DOI] [PubMed] [Google Scholar]
- 21. Haviv B, Mayo L, Biggs D. Outcomes of arthroscopic “remplissage”: capsulotenodesis of the engaging large Hill-Sachs lesion. J Orthop Surg Res. 2011;6:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Helfet AJ. Coracoid transplantation for recurring dislocation of the shoulder. J Bone Joint Surg Br. 1958;40-B:198–202. [DOI] [PubMed] [Google Scholar]
- 23. Hovelius L, Saeboe M. Neer Award 2008: arthropathy after primary anterior shoulder dislocation-- 223 shoulders prospectively followed up for twenty-five years. J Shoulder Elbow Surg. 2009;18:339–347. [DOI] [PubMed] [Google Scholar]
- 24. Hovelius L, Sandstrom B, Olofsson A, Svensson O, Rahme H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): long-term follow-up in 319 shoulders. J Shoulder Elbow Surg. 2012;21:647–660. [DOI] [PubMed] [Google Scholar]
- 25. Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82:35–46. [DOI] [PubMed] [Google Scholar]
- 26. Khazzam M, Kane SM, Smith MJ. Open shoulder stabilization procedure using bone block technique for treatment of chronic glenohumeral instability associated with bony glenoid deficiency. Am J Orthop (Belle Mead NJ). 2009;38:329–335. [PubMed] [Google Scholar]
- 27. Lafosse L, Boyle S. Arthroscopic Latarjet procedure. J Shoulder Elbow Surg. 2010;19(suppl):2–12. [DOI] [PubMed] [Google Scholar]
- 28. Larrain MV, Botto GJ, Montenegro HJ, Mauas DM. Arthroscopic repair of acute traumatic anterior shoulder dislocation in young athletes. Arthroscopy. 2001;17:373–377. [DOI] [PubMed] [Google Scholar]
- 29. Larrain MV, Montenegro HJ, Mauas DM, Collazo CC, Pavon F. Arthroscopic management of traumatic anterior shoulder instability in collision athletes: analysis of 204 cases with a 4- to 9-year follow-up and results with the suture anchor technique. Arthroscopy. 2006;22:1283–1289. [DOI] [PubMed] [Google Scholar]
- 30. Latarjet M. Treatment of recurrent dislocation of the shoulder [in French]. Lyon Chir. 1954;49:994–997. [PubMed] [Google Scholar]
- 31. Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy. 2004;20:169–174. [DOI] [PubMed] [Google Scholar]
- 32. McLaughlin HL, MacLellan DI. Recurrent anterior dislocation of the shoulder. J Trauma. 1967;7:191–201. [DOI] [PubMed] [Google Scholar]
- 33. Mologne TS, Provencher MT, Menzel KA, Vachon TA, Dewing CB. Arthroscopic stabilization in patients with an inverted pear glenoid: results in patients with bone loss of the anterior glenoid. Am J Sports Med. 2007;35:1276–1283. [DOI] [PubMed] [Google Scholar]
- 34. Nho SJ, Provencher MT, Seroyer ST, Romeo AA. Bioabsorbable anchors in glenohumeral shoulder surgery. Arthroscopy. 2009;25:788–793. [DOI] [PubMed] [Google Scholar]
- 35. Nourissat G, Kilinc AS, Werther JR, Doursounian L. A prospective, comparative, radiological, and clinical study of the influence of the “remplissage” procedure on shoulder range of motion after stabilization by arthroscopic Bankart repair. Am J Sports Med. 2011;39:2147–2152. [DOI] [PubMed] [Google Scholar]
- 36. O’Brien SJ, Allen AA, Coleman SH, Drakos MC. The trans-rotator cuff approach to SLAP lesions: technical aspects for repair and a clinical follow-up of 31 patients at a minimum of 2 years. Arthroscopy. 2002;18:372–377. [DOI] [PubMed] [Google Scholar]
- 37. Pagnani MJ. Open capsular repair without bone block for recurrent anterior shoulder instability in patients with and without bony defects of the glenoid and/or humeral head. Am J Sports Med. 2008;36:1805–1812. [DOI] [PubMed] [Google Scholar]
- 38. Park MJ, Tjoumakaris FP, Garcia G, Patel A, Kelly JD., 4th Arthroscopic remplissage with Bankart repair for the treatment of glenohumeral instability with Hill-Sachs defects. Arthroscopy. 2011;27:1187–1194. [DOI] [PubMed] [Google Scholar]
- 39. Parkin D, Devlin N. Is there a case for using visual analogue scale valuations in cost-utility analysis? Health Econ. 2006;15:653–664. [DOI] [PubMed] [Google Scholar]
- 40. Porcellini G, Paladini P, Campi F, Paganelli M. Long-term outcome of acute versus chronic bony Bankart lesions managed arthroscopically. Am J Sports Med. 2007;35:2067–2072. [DOI] [PubMed] [Google Scholar]
- 41. Provencher MT, Frank RM, Leclere LE, et al. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg. 2012;20:242–252. [DOI] [PubMed] [Google Scholar]
- 42. Scheibel M, Magosch P, Lichtenberg S, Habermeyer P. Open reconstruction of anterior glenoid rim fractures. Knee Surg Sports Traumatol Arthrosc. 2004;12:568–573. [DOI] [PubMed] [Google Scholar]
- 43. Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JJ. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am. 2012;94:495–501. [DOI] [PubMed] [Google Scholar]
- 44. Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A. Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Joint Surg Am. 2005;87:1752–1760. [DOI] [PubMed] [Google Scholar]
- 45. van der Linde JA, van Kampen DA, Terwee CB, Dijksman LM, Kleinjan G, Willems WJ. Long-term results after arthroscopic shoulder stabilization using suture anchors: an 8- to 10-year follow-up. Am J Sports Med. 2011;39:2396–2403. [DOI] [PubMed] [Google Scholar]
- 46. Warner JJ, Gill TJ, O’hollerhan JD, Pathare N, Millett PJ. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med. 2006;34:205–212. [DOI] [PubMed] [Google Scholar]
- 47. Weng PW, Shen HC, Lee HH, Wu SS, Lee CH. Open reconstruction of large bony glenoid erosion with allogeneic bone graft for recurrent anterior shoulder dislocation. Am J Sports Med. 2009;37:1792–1797. [DOI] [PubMed] [Google Scholar]
- 48. Zhu YM, Lu Y, Zhang J, Shen JW, Jiang CY. Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year follow-up. Am J Sports Med. 2011;39:1640–1647. [DOI] [PubMed] [Google Scholar]