Abstract
Background
Anterior cervical discectomy and fusion (ACDF) remains the standard of care for patients with cervical radiculopathy who are unresponsive to conservative care. However, the maintenance and restoration of cervical alignment as a predictive factor for outcome has not yet been fully evaluated. The purpose of this study was to evaluate the impact of maintaining or restoring cervical alignment on one and two level ACDF patients’ outcome.
Methods
Data were collected from 104 patients who underwent one and two level ACDF. Cervical alignment was measured preoperatively and at follow-up visits. The patients were classified into three groups based on the postoperative change of their cervical alignment. Neck pain, arm pain, and Neck Disability Index (NDI) scores were obtained preoperatively and at the latest follow-up visit. Incidences of adjacent segment degeneration (ASD) and reoperations because of ASD were recorded.
Results
There were 64 patients in the Maintained group, 17 patients in the Restored group and 23 patients in the Kyphotic group. Pre-operatively, the neck pain scores, arm pain scores and NDI scores were not statistically different among the three groups (p>0.05). On average at 12 months follow-up, the neck pain scores improved by 2.7, 4.2, and 2.7 points respectively in the three groups (p>0.05). The patients’ arm pain scores improved by 2.1, 2.4, and 2.8 points respectively (p>0.05). NDI scores improved by 12, 31 and 13.7 points respectively (p<0.05). The incidences of ASD and reoperations because of ASD were 16%, 12% and 35% respectively (p>0.05).
Conclusions
The patients with restored cervical alignment had significantly greater NDI improvement and relatively better neck pain improvement. There was a trend for patients who had unchanged cervical kyphosis to have a higher incidence of ASD. Our study suggests that restoration of cervical alignment will contribute to improved clinical outcome in the patients who have one and two level ACDF surgeries.
Level of Evidence
This is a level III study.
Keywords: anterior cervical discectomy and fusion, cervical alignment, lordosis, adjacent segment degeneration, clinical outcome
Introduction
Anterior cervical discectomy and fusion (ACDF) is one of the most commonly performed spine surgeries with more than 150,000 procedures performed annually in the United States.1 Many studies have shown that the clinical outcome of ACDF is good or excellent for most patients.2–5 There are still however some patients that have only fair or even poor outcome.6 Early identification and proper management of potentially remediable factors related to a fair or poor outcome will help to ensure a good outcome for even more patients.
Normal cervical lordosis (C2-7) averages approximately 34 degrees.7 The normal sagittal weightbearing axis lies posterior to the radiographic arc of the vertebral bodies from C2-7. Once normal lordosis is reversed, the weight-bearing axis moves anteriorly, which predisposes to further progression of kyphosis and may contribute to accelerated degeneration with the development of radiculopathy, myelopathy and pseudarthrosis.8–10 Some studies have also shown that the loss of normal cervical lordotic alignment can directly alter flexion-extension dynamics and is associated with postoperative axial symptoms and adjacent segment degeneration.11–14 Regardless of the above, the impact of maintaining or restoring cervical alignment on the outcome of patients following ACDF surgery has not been fully evaluated.
The aim of this study was to review a series of patients undergoing one and two level ACDF surgeries to evaluate the impact of maintaining or restoring cervical alignment on the patients’ clinical outcome.
Materials and Methods
Data were retrospectively collected from a series of patients who underwent one and two level ACDF at a single institution between 2011 and 2013. All the surgeries were performed by a team of fellowship trained spine surgeons. Patients who had previous cervical surgeries and those with less than 6 months’ follow up were excluded from the study. Preoperative and the latest postoperative lateral cervical radiographs were measured by an independent researcher to record the global cervical lordosis/kyphosis angles (C2-7). The patients were classified into three groups based on the angle: Maintained group (patients had lordotic or neutral cervical angle preoperatively and the angle was maintained postoperatively); Restored group (patients had cervical kyphosis preoperatively and the angle was restored to lordosis or neutral postoperatively); and Kyphotic group (patients had cervical kyphosis preoperatively and the angle was unchanged postoperatively).
The patients’ age, gender, body mass index (BMI), level(s) operated and the follow-up intervals were recorded. Visual analog scale (VAS) scores for neck pain, arm pain, and the Neck Disability Index (NDI) were obtained from each patient preoperatively and at the latest follow-up visit. Pain intensity for arm pain and neck pain were measured separately using scales ranging from 0 (no pain) to 10 (worst possible pain). Incidences of adjacent segment degeneration and reoperations because of adjacent segment degeneration were determined and collected from radiographs and medical records. The relationship between maintaining or restoring cervical alignment and the patients’ clinical outcome was analyzed.
Data Analysis
The mean demographic and outcome scores were compared among the three group using ANOVA analyses and the differences between two groups were compared using t test. Categorical data were compared using Chi-square analyses.
Results
One hundred four patients who underwent one and two level ACDF were included in this study. There were 64 patients in the Maintained group, 17 patients in the Restored group and 23 patients in the Kyphotic group. The most common primary diagnoses were disc herniation and stenosis (Table 1). The patients’ gender, BMI, number of levels operated and follow-up interval were not significantly different among the groups (p>0.05; Table 2). The patients were younger in the Kyphotic group (48 years old) comparing with the Maintained group (54 years old) and the Restored group (55 years old) (p<0.05, Table 2).
Table 1.
Primary diagnosis of the patients.
| Primary diagnosis | Maintained Group, n (%) | Restored Group, n (%) | Kyphotic Group, n (%) |
|---|---|---|---|
| Disc herniation | 24 (38%) | 6 (35%) | 14 (61%) |
| Stenosis | 23 (36%) | 8 (47%) | 6 (26%) |
| Spondylosis/Spondylolisthesis | 11 (17%) | 2 (12%) | 2 (9%) |
| Degenerative disc disease | 6 (9%) | 1 (6%) | |
| Kyphosis | 1 (4%) |
Table 2.
Overview of patients in the three groups.
| Maintained Group | Restored Group | Kyphotic Group | p value | |
|---|---|---|---|---|
| Gender (female, male) | 33, 31 | 7, 10 | 12, 11 | >0.05 |
| Mean age (years) | 54 | 55 | 48 | <0.05 |
| Mean BMI (kg/cm2) | 29 | 28 | 29 | >0.05 |
| One level surgery, n (%) | 29 (45%) | 8 (47%) | 9 (39%) | >0.05 |
| Two levels surgery, n (%) | 35 (55%) | 9 (53%) | 14 (61%) | >0.05 |
| Mean follow up time (months) | 12 | 12 | 12 | >0.05 |
Preoperatively, there were no significant differences in the mean neck pain VAS, arm pain VAS, and NDI scores when comparing the three groups (all p>0.05; ANOVA; Table 3, Table 4, Table 5). At mean 12 months’ (range 6 to 33 months) follow-up, all three groups had improved neck pain (Table 3), arm pain (Table 4) and NDI (Table 5) scores from preoperative values, although the arm pain score improvement in the Restored group and the NDI score improvement in the Kyphotic group were not statistically significant (Table 4, Table 5).
Table 3.
Preoperative and postoperative neck pain VAS scores and the net change in these three groups.
| Neck pain VAS scores | Preop | Postop | Change | p value |
|---|---|---|---|---|
| Maintained Group | 6.5 | 3.8 | 2.7 | <0.001 |
| Restored Group | 6.7 | 2.5 | 4.2 | <0.001 |
| Kyphotic Group | 6.3 | 3.6 | 2.7 | 0.015 |
Table 4.
Preoperative and postoperative arm pain VAS scores and the net change in these three groups.
| Arm pain VAS scores | Preop | Postop | Change | p value |
|---|---|---|---|---|
| Maintained Group | 4.3 | 2.2 | 2.1 | 0.001 |
| Restored Group | 4.7 | 2.3 | 2.4 | 0.067 |
| Kyphotic Group | 5.7 | 2.9 | 2.8 | 0.011 |
Table 5.
Preoperative and postoperative NDI scores and the net change in these three groups.
| NDI scores | Preop | Postop | Change | p value |
|---|---|---|---|---|
| Maintained Group | 42.8 | 30.8 | 12 | 0.004 |
| Restored Group | 50.4 | 19.4 | 31 | 0.007 |
| Kyphotic Group | 46.3 | 32.6 | 13.7 | 0.114 |
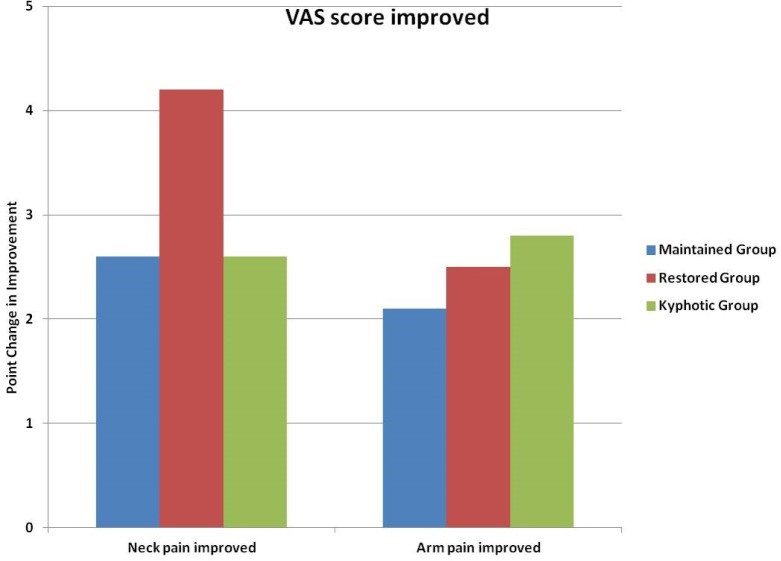
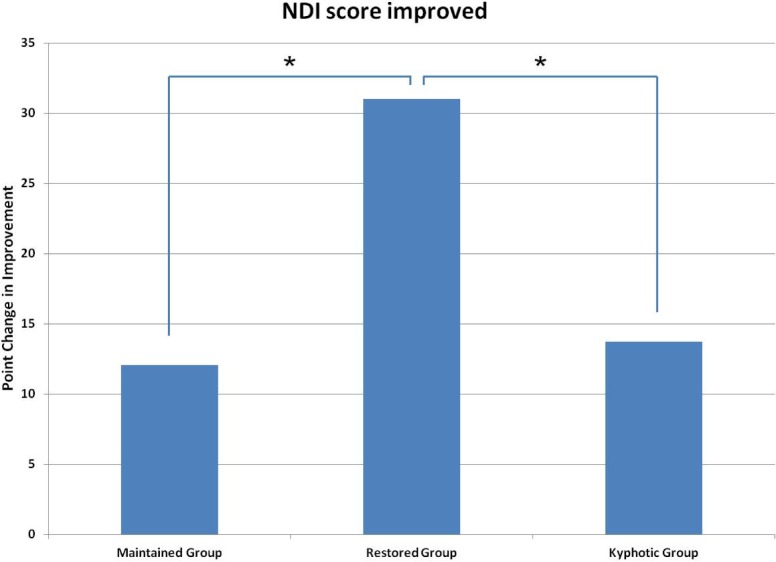
There were no statistically significant differences in the degree of improvement in neck pain or arm pain VAS scores when comparing the three groups (p>0.05; Figure 1). The mean NDI score improvement was statistically significantly greater in the Restored group compared with the other groups (p=0.02 between the Maintained group and the Restored group, p=0.03 between group the Restored group and the Kyphotic group) (Figure 2).
Fig. 1.
Neck pain and arm pain VAS score improvement in the three groups.
Fig. 2.
NDI score improvement in the three groups (*: p<0.05).
There was a trend toward a greater incidence of adjacent segment degeneration in the Kyphotic group compared with the other two groups (p=0.15 between the Restored group and the Kyphotic group, p=0.08 between the Maintained group and the Kyphotic group, Chi-square analyses) (Table 6). Reoperation due to adjacent segment degeneration was required in only one patient (4%), who was in the Kyphotic group (Table 6).
Table 6.
Incidences of adjacent segment degeneration and reoperations due to adjacent segment degeneration in the three groups.
| Maintained Group | Restored Group | Kyphotic Group | |
|---|---|---|---|
| Adjacent segment degeneration, n (%) | 10 (16%) | 2 (12%) | 7 (30%) |
| Reoperation due to adjacent segment degeneration, n (%) | 0 | 0 | 1 (4%) |
Discussion
The normal cervical spine has a gentle lordotic curve and its stability is provided by bone morphology and ligamentous structures. The normal sagittal weight bearing axis lies posterior to the cervical vertebral bodies. This helps to maintain the normal sagittal balance and minimize the demands on the posterior cervical musculature.15 Loss of cervical lordosis or straightening of the cervical spine can be caused by degenerative, inflammatory, traumatic or iatrogenic damage. The sagittal weight bearing axis shifts anteriorly with the loss of the normal cervical lordosis to kyphosis. This predisposes to further progression of kyphosis and may contribute to accelerated degeneration and the development of radiculopathy, myelopathy and pseudarthrosis.8–10 Some studies have also shown that the loss of normal cervical lordotic alignment can directly alter flexion-extension dynamics and is associated with postoperative axial symptoms and adjacent segment degeneration.11–14
ACDF is a well established and commonly performed procedure for the treatment of cervical disc disease. It was first described and popularized by Robinson and Smith and also Cloward in the 1950s.16, 17 Most studies have shown that the clinical outcome after ACDF is good or excellent.2–5 Some studies suggest that cervical lordosis is important in order to achieve a good outcome for the surgical treatment of patients with neurological deficits. Katsuura et al. examined 42 patients who underwent ACDF for cervical spondylosis and disc herniation. At an average of 9.8 years’ follow-up, they found that 43% of the 21 patients who showed adjacent segment degeneration had malalignment of the cervical spine, such as kyphosis or sigmoid curvature.11 Jenkins et al. studied the patients’ radiographic and clinical outcomes after cervical spine fusion for trauma and found that the patients who had 20 or more degrees of kyphosis had a significant increase in complaints of cervical pain.18 Kawakami et al. studied the relationship between axial symptoms and cervical alignment after cervical anterior spinal fusion for patients with cervical myelopathy, and they found that the loss of cervical lordosis was associated with axial symptoms such as neck pain, stiff neck, shoulder pain, neck dullness, or shoulder dullness.12
In contrast, there are also some studies showing that the cervical alignment does not correlate with the clinical outcome of cervical surgeries. Kaptain et al. reported that kyphosis may develop in up to 21% of patients who have undergone laminectomy for cervical spondylotic myelopathy, but clinical outcome did not correlate with either pre- or postoperative sagittal alignment.19 Rajshekhar et al. found that after oneor two-level uninstrumented central corpectomy, cervical spine curvature tended to undergo a kyphotic change but this kyphotic change did not affect the neurological outcome.20
In this study, we analyzed whether alterations in the cervical alignment after one and two level ACDF have an impact on clinical outcome. We divided the patients into three groups based on changes in their pre- to postoperative cervical alignment. Our results showed that the patients in all three groups had improved neck pain, arm pain and NDI scores from the preoperative baseline, which suggests that ACDF is an effective surgery regardless of the alternation in cervical alignment. This improvement may mainly come from the decompression and the restoration of disc height even if the global cervical alignment remained in kyphosis. This is consistent with the existing published data regarding outcome after ACDF. As an extension to the existing literature, we found that the patients whose cervical alignment was restored from preoperative kyphosis to postoperative lordosis or neutral alignment had a significantly higher degree of improvement in NDI scores compared to patients whose cervical alignment was unchanged. These patients also seemed to have higher degree of improvement in neck pain although the difference was not statistically significant. These results suggest that the restoration of cervical alignment from kyphosis to lordosis or neutral does contribute to the patients’ clinical outcome in addition to the benefits of decompression and disc height restoration. It is still not clear exactly how the restoration of cervical alignment contributes to the patients’ outcome, but it may be attributed to the complex posture-related muscle and ligament interactions.21 It will be interesting to see if the differences we noted among these three groups will be maintained at a longer follow up time. A further important finding that we observed was that the incidence of adjacent segment degeneration was lower in the patients who had restored cervical alignment. This result is consistent with some previous reports22, 23 which further highlights the importance of restoring cervical alignment even in one and two level ACDF surgeries. Longer follow-up will also allow us to see if this translates into a higher reoperation rate for adjacent level degenerative disc disease.
We acknowledge that there are limitations to this study. First, we focused on the clinical effect of global cervical sagittal alignment and we did not assess the effect of segmental sagittal alignment on patients’ outcome. In a multicenter, randomized controlled study, the authors found that the loss of segmental lordosis does not correlate with the patients’ outcome at two years’ follow up.23 It is also found that only 25% of the variance in global cervical sagittal alignment can be attributed to the change in segmental alignment.21We thus believe that assessing the relationship between global cervical sagittal alignment and the patients’ clinical outcome as performed in our study has more clinical significance. Second, the patients’ number differs among these three groups and there are more patients in the Maintained group (patients had lordotic or neutral cervical angle preoperatively and the angle was maintained postoperatively). This is a reflection of the patient population treated in our study. A prospective matched controlled outcomes study would be best to address this limitation. Thirdly, the minimum follow up is relatively short in this series. Lastly, we did not address fusion rates or neurologic improvement, which may affect VAS and NDI scores.
In summary, our study suggests that restoration of cervical alignment from kyphosis to lordosis or neutral will contribute to greater improvement in NDI scores in patients who have one and two level ACDF. These patients also seem to have lower incidence of adjacent segment degeneration. Maintenance or restoration of global cervical sagittal alignment is an important factor in the operative intervention of patients scheduled for one and two level ACDF to optimize their clinical outcome.
Disclosures
The authors declare that there is no direct conflict of interest associated with this manuscript. No funds were received in support of this work.
References
- 1.Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating: a 5- to 11-year radiologic and clinical follow-up study. Spine. 2005;30:2138–44. doi: 10.1097/01.brs.0000180479.63092.17. [DOI] [PubMed] [Google Scholar]
- 2.Papadopoulos EC, Huang RC, Girardi FP, et al. Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine. 2006;31:897–902. doi: 10.1097/01.brs.0000209348.17377.be. [DOI] [PubMed] [Google Scholar]
- 3.Samartzis D, Shen FH, Lyon C, et al. Does rigid instrumentation increase the fusion rate in one-level anterior cervical discectomy and fusion? Spine J. 2004;4:636–43. doi: 10.1016/j.spinee.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 4.Lied B, Roenning PA, Sundseth J, et al. Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage) BMC surgery. 2010;10:10. doi: 10.1186/1471-2482-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine. 2007;32:2310–7. doi: 10.1097/BRS.0b013e318154c57e. [DOI] [PubMed] [Google Scholar]
- 6.Harrison DD, Janik TJ, Troyanovich SJ, et al. Comparisons of lordotic cervical spine curvatures to a theoretical ideal model of the static sagittal cervical spine. Spine. 1996;21:667–75. doi: 10.1097/00007632-199603150-00002. [DOI] [PubMed] [Google Scholar]
- 7.Wang M, Gourab K, McGrady LM, et al. Alteration of load sharing of anterior cervical implants with change in cervical sagittal alignment. Medical engineering & physics. 2008;30:768–73. doi: 10.1016/j.medengphy.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Uchida K, Nakajima H, Sato R, et al. Cervical spondylotic myelopathy associated with kyphosis or sagittal sigmoid alignment: outcome after anterior or posterior decompression. Journal of neurosurgery. 2009;11:521–8. doi: 10.3171/2009.2.SPINE08385. [DOI] [PubMed] [Google Scholar]
- 9.Spivak JM, Giordano CP. Cervical Kyphosis. In: Birdwell KH, DeWald RL, editors. The Textbook of Spine Surgery. 2nd ed. Philadelphia: Lippincott-Raven; 1997. pp. 1027–38. [Google Scholar]
- 10.Katsuura A, Hukuda S, Saruhashi Y, et al. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10:320–4. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawakami M, Tamaki T, Yoshida M, et al. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. Journal of spinal disorders. 1999;12:50–6. [PubMed] [Google Scholar]
- 12.Nagasawa A, Sakakibara T, Takahashi A. Roentgenographic findings of the cervical spine in tension-type headache. Headache. 1993;33:90–5. doi: 10.1111/j.1526-4610.1993.hed3302090.x. [DOI] [PubMed] [Google Scholar]
- 13.Takeshima T, Omokawa S, Takaoka T, et al. Sagittal alignment of cervical flexion and extension: lateral radiographic analysis. Spine. 2002;27:E348–55. doi: 10.1097/00007632-200208010-00014. [DOI] [PubMed] [Google Scholar]
- 14.Panjabi MM, White AA, Johnson R. Cervical spine biomechanics as a function of transection of components. J Biomech. 1975;8:327–36. doi: 10.1016/0021-9290(75)90085-8. [DOI] [PubMed] [Google Scholar]
- 15.Robinson RA, Smith GW. Anterolateral Cervical Disc Removal and Interbody Fusion for Cervical Disc Syndrome. Bulletin of the Johns Hopkins Hospital. 1955;95:223–4. [Google Scholar]
- 16.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–17. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 17.Jenkins LA, Capen DA, Zigler JE, et al. Cervical spine fusions for trauma. A long-term radiographic and clinical evaluation. Orthopaedic review. 1994;(Suppl):13–9. [PubMed] [Google Scholar]
- 18.Kaptain GJ, Simmons NE, Replogle RE, et al. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg. 2000;93:199–204. doi: 10.3171/spi.2000.93.2.0199. [DOI] [PubMed] [Google Scholar]
- 19.Rajshekhar V, Arunkumar MJ, Kumar SS. Changes in cervical spine curvature after uninstrumented one- and two-level corpectomy in patients with spondylotic myelopathy. Neurosurgery. 2003;52:799–804. doi: 10.1227/01.neu.0000054218.50113.40. discussion -5. [DOI] [PubMed] [Google Scholar]
- 20.Villavicencio AT, Babuska JM, Ashton A, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery. 2011;68:1309–16. doi: 10.1227/NEU.0b013e31820b51f3. discussion 16. [DOI] [PubMed] [Google Scholar]
- 21.Lee YS, Kim YB, Park SW. Risk factors for postoperative subsidence of single-level anterior cervical discectomy and fusion: the significance of the preoperative cervical alignment. Spine (Phila Pa 1976) 2014;39:1280–7. doi: 10.1097/BRS.0000000000000400. [DOI] [PubMed] [Google Scholar]
- 22.Park MS, Kelly MP, Lee DH, et al. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J. 2014;14:1228–34. doi: 10.1016/j.spinee.2013.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pitzen T. Loss of lordosis and loss of segmental height do not affect clinical results following ACDF: secondary endpoint results from a multicentric, randomised, controlled study. Spine J. 2010;10:s33. [Google Scholar]