Abstract
The development of good quality and affordable ultrasound machines has led to the establishment and implementation of numerous point-of-care ultrasound (POCUS) protocols in various medical disciplines. POCUS for major infectious diseases endemic in tropical regions has received less attention, despite its likely even more pronounced benefit for populations with limited access to imaging infrastructure. Focused assessment with sonography for HIV-associated TB (FASH) and echinococcosis (FASE) are the only two POCUS protocols for tropical infectious diseases, which have been formally investigated and which have been implemented in routine patient care today. This review collates the available evidence for FASH and FASE, and discusses sonographic experiences reported for urinary and intestinal schistosomiasis, lymphatic filariasis, viral hemorrhagic fevers, amebic liver abscess, and visceral leishmaniasis. Potential POCUS protocols are suggested and technical as well as training aspects in the context of resource-limited settings are reviewed. Using the focused approach for tropical infectious diseases will make ultrasound diagnosis available to patients who would otherwise have very limited or no access to medical imaging.
Introduction
Ultrasound (US) has been used to aid diagnosis and to guide therapy in a large number of tropical infectious diseases for a long time.1 During the past two decades, technological advances have improved image quality and significantly reduced the size and price of US equipment. As a result, US has been established as a point-of-care test in clinical decision making and for procedural guidance in various medical specialties.2 Point-of-care ultrasound (POCUS) is one of the few novel diagnostic tools to which the criticism of inflationary use of the term point-of-care does not apply.3 Emergency medicine (EM) physicians have pioneered and greatly advanced the point-of-care application of US. Today, the “focused assessment with sonography for trauma” (FAST) protocol is not only well recognized as a standardized diagnostic test in emergency departments, but also constitutes an integral part of diagnostic algorithms and EM training.4–7 The fundamental difference between POCUS and conventional US examination is that POCUS is performed by the treating physician who aims to answer simple, usually binary questions relevant to immediate patient management (e.g., “Is there a pleural effusion, yes or no?”). POCUS is not a comprehensive US assessment.8 Diagnoses for which POCUS is suitable should fulfill two criteria: 1) diagnosis must be relevant to consecutive treatment decision making and 2) diagnosis must be easily and accurately recognizable by physicians applying US without the necessity for extended US training. Whereas patients' benefit from POCUS in affluent settings is mainly a reduced time to diagnosis and further management, POCUS in resource-constrained settings provides the additional benefit that it is frequently the only diagnostic imaging modality available.9,10
This review first describes the development and application of “focused assessment with sonography for human immunodeficiency virus (HIV)–associated tuberculosis (TB)” (FASH),11–16 which is the most widely studied and implemented application of POCUS in infectious diseases to date. Subsequently, other infectious diseases, endemic in tropical or resource-limited settings and accounting for significant morbidity and mortality in affected populations and for which POCUS has been investigated or for which POCUS may be a potential diagnostic tool, are reviewed and discussed. In view of the required focused approach of POCUS, it is important not only to define diagnostic criteria and test accuracy for each disease, but also to identify the target population in which the diseases of interest are highly prevalent and for whom POCUS will therefore be valid and most beneficial (e.g., HIV/TB coinfection in South Africa, echinococcosis in rural Argentina, or the Kenyan Turkana region). Finally, technical and teaching considerations are discussed.
Focused Assessment with Sonography for HIV/TB
TB is one of the most frequent opportunistic infections in HIV patients living in tropical countries and constitutes an immense problem in sub-Saharan Africa and beyond.17 Extrapulmonary TB (EPTB) is seen more frequently in immunocompromised patients and is more difficult to diagnose than pulmonary TB. Disseminated TB is a major cause of death in patients with HIV.18 Clinical symptoms are fever, weight loss, and night sweats, possibly with cough, shortness of breath, or other focal symptoms; frequently, cardinal signs and symptoms are less clearly evident in HIV coinfected individuals.
The diagnosis of EPTB in HIV-infected patients is challenging but vital to patient management. The majority of EPTB patients in resource-poor settings are diagnosed on the basis of clinical case definitions (e.g., World Health Organization [WHO]19) and only in a minority of cases is microbiological confirmation feasible. The value of US for diagnosing EPTB has long been recognized. The sonographic features suggestive of EPTB, in populations with a high prevalence of HIV/TB coinfection, are as follows:
-
1.
Pleural effusion, particularly when unilateral. In a study from sub-Saharan Africa, unilateral pleural effusion was caused by TB in over 90% of cases and was highly associated with HIV infection.20
-
2.
Pericardial effusion is consistently reported to be due to TB and to be associated with HIV coinfection in the majority of cases in Africa.21 Pericardial fluid can easily be identified by POCUS,22 as well as its hemodynamic significance and potential need for pericardiocentesis.23
-
3.
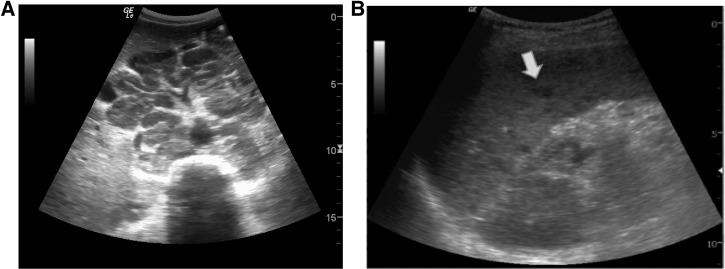
Although not included in current WHO guidelines, enlarged abdominal lymph nodes and splenic microabscesses have been repeatedly reported as characteristic findings of abdominal TB in HIV-infected patients (Figure 1A).24 Lymph nodes affected by TB present as hypoechoic round structures and are considered pathological when larger than 1.5–2 cm. Abdominal tuberculous lymphadenopathy is frequently located in the upper abdomen, for example, in the liver hilum, around the celiac axis and in the para-aortic area. In some cases, lymphadenopathy can also be found in the mesentery of the caecum (especially in cases of cecal involvement of TB) and in the splenic hilum. Splenic microabscesses are visible as multiple hypoechoic lesions between 0.5 and 1 cm, in an often enlarged spleen (Figure 1B). Presence of ascites can also be a sign of peritoneal TB, especially, if further features suggestive of abdominal TB are demonstrated.
Figure 1.
(A) Epigastric transverse view: enlarged round hypoechoic tuberculous lymph nodes behind the liver in the area of the celiac trunk. (B) Left longitudinal flank view: enlarged spleen with small hypoechoic lesions (arrow) due to tuberculous microabscesses.
The feasibility and success of training clinicians to accurately detect abdominal lymphadenopathy and splenic microabscesses through short courses, using a curriculum developed in South Africa, has been demonstrated.25 It has also been documented extensively in EM that pleural,26 pericardial,27 and ascitic4 fluid can be detected by POCUS with high sensitivity and specificity. There is no reason to doubt the similar value of POCUS for the detection of effusions and ascites secondary to infectious diseases. As a logical consequence, a single POCUS protocol for EPTB (FASH) has been compiled using the US views of FAST and US views for detection of abdominal lymphadenopathy and splenic microabscesses11 (Figure 2 ). Because of the high prevalence of HIV/TB coinfection, FASH has become one of the most frequently used POCUS modules in South Africa.15 Further studies showed that in approximately 25% of patients with a FASH examination suggesting EPTB, the patient's chest X-ray was not suggestive of TB, indicating a significant proportion of patients in whom the diagnosis will be missed if only chest X-ray is performed as part of their diagnostic TB work-up.13 The use of FASH in pediatric patients is currently under investigation, but preliminary data indicate that FASH is also applicable in the pediatric population.16 An evaluation of FASH as a tool to monitor response to treatment in HIV-infected patients with EPTB showed that the persistence of positive findings, after a treatment period of 3 months, is an indicator of treatment complications such as mycobacterial resistance, poor compliance, or immune reconstitution inflammatory syndrome.14 It needs to be emphasized that a definitive diagnosis of the etiology underlying FASH findings is not possible by US only; however, in a high-prevalence setting, commencing TB treatment based on clinical and sonographic findings and observing the patient's clinical and sonographic response is justified.28
Figure 2.
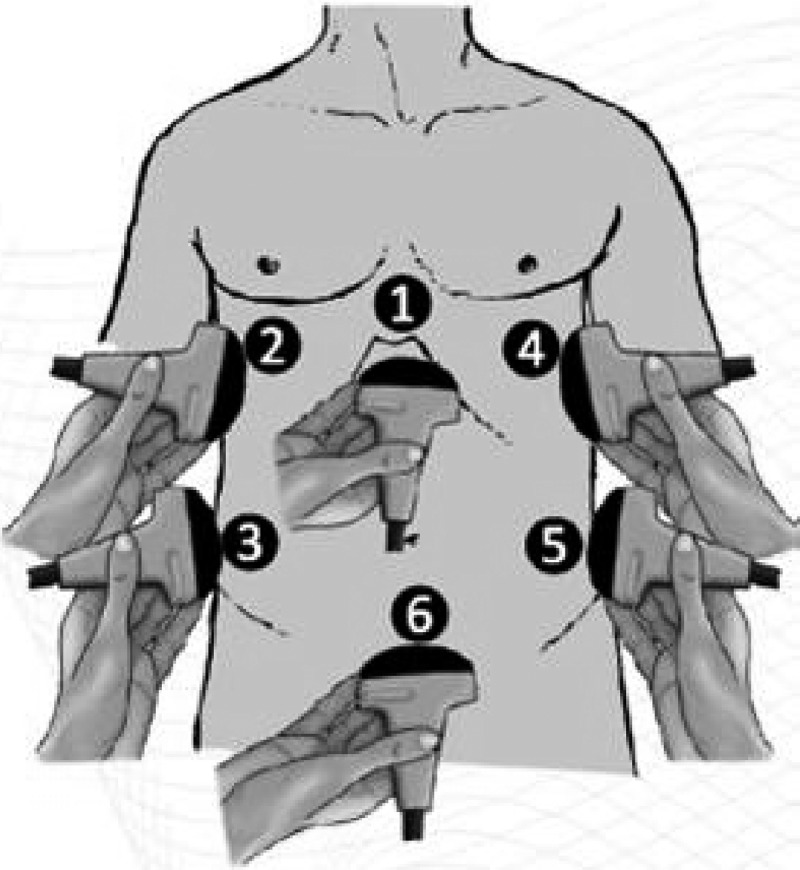
Ultrasound (US) probe positions used in focused assessment with sonography for human immunodeficiency virus–associated tuberculosis (FASH) protocol. (1) Epigastric/subxiphoidal transverse view, (2) longitudinal pleural view right, (3) longitudinal right flank/upper quadrant view, (4) longitudinal pleural view left, (5) longitudinal left flank/upper quadrant view, and (6) transverse pelvic view (adapted from Heller et al. 201211).
Focused Assessment with Sonography for Echinococcosis
Cystic echinococcosis (CE) is highly prevalent in sheep farming areas, especially in central Asia, China, South America, the Mediterranean, eastern Europe, and considerable parts of Africa.29,30 In humans, CE cysts develop predominantly in the liver (60–70%) and lungs (20–30%). On average, 60–75% of infected patients with hepatic CE are asymptomatic.31 When present, symptoms may be local (most commonly right upper quadrant pain) or systemic (fever, jaundice, or allergic manifestations), due to mass effect, communication with hollow structures, superinfection, or loss of integrity of the cyst's wall. Based on individual case reports, it has been hypothesized that HIV may affect the course of CE and lead to unusual and potentially more severe clinical disease.32
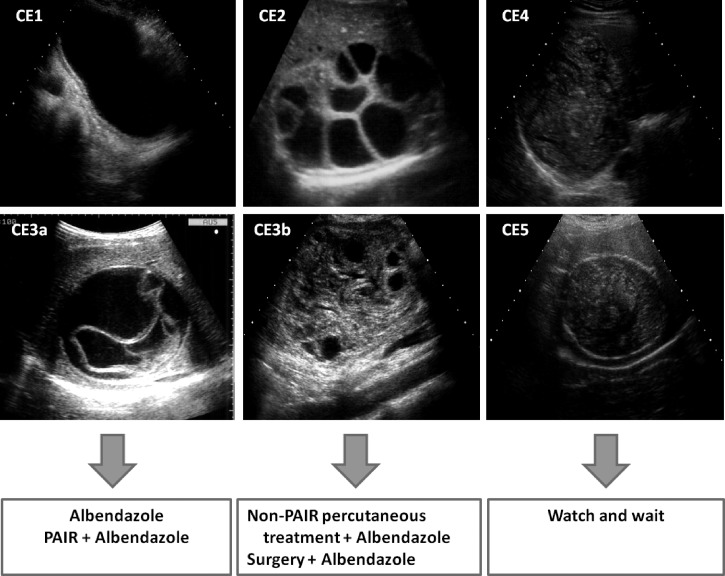
US is the technique of choice for abdominal CE diagnosis, staging, and follow-up33 and enables US-assisted percutaneous therapeutic procedures. The different types of cysts can be grouped according to the WHO-IWGE (Informal Working Group on Echinococcosis) classification, which is also the basis of the stage-specific approach to the clinical management of CE (Figure 3 ).34,35
Figure 3.
Suggested cystic echinococcosis (CE) stage-specific clinical management options according to World Health Organization Informal Working Group on Echinococcosis (WHO-IWGE) Expert consensus.34 PAIR = puncture, aspiration, injection of a scolicidal agent, and re-aspiration. Non-PAIR percutaneous treatments include several percutaneous techniques using cutting instruments and large bore catheters to evacuate the entire cyst content.
Sonographic features of CE cysts are as follows35:
-
1.
Double wall of the cyst, especially evident in fluid-filled CE1 cysts.
-
2.
“Water lily sign” of CE3a cysts, which reflects the detached endocyst fluctuating in the cyst fluid content.
-
3.
“Honeycomb appearance” of multivesiculated cysts (CE2 and CE3b), in which the impression of “septa” is formed by the adjacent walls of daughter vesicles (CE2) or in which daughter vesicles have formed in pseudo-solid, hyperechoic, and nonhomogeneous cyst content (CE3b).
-
4.
The “ball-of-wool” sign of CE4 cysts, characterized by the appearance of hypoechoic, degenerating cyst membranes folded inside pseudo-solid cyst content.
-
5.
The wall calcification of cysts with pseudo-solid content (CE5).
Key in the differentiation between CE1 and simple cysts is the visualization of the double wall, which is absent in nonparasitic cysts. Serology and, if necessary, US-guided aspiration and microscopic analysis of the cyst content will further aid the diagnosis.
US screening for hepatic CE has been conducted in many endemic countries for years.36–40 For example, in Argentina, a yearly 2-day “focused assessment with sonography for echinococcosis” (FASE) training course has been implemented since 2000, where general practitioners working in rural endemic areas with no previous experience with US are trained in FASE. Four standard images are acquired, and according to results of scans and consultations with experts, patients are offered stage-specific clinical management.36 Annual screening of large populations and regular long-term follow-up of diagnosed cases without costly travel by the patients to tertiary care facilities, as well as reduction in loss to follow-up, were achieved. The repeated annual training ensures sustainability, by compensating for the high turnover of general practitioners in rural areas.
In other endemic settings, the implementation of short protocols allowing the diagnosis and classification of CE cysts according to the WHO-IWGE criteria could provide the basis for early detection and clinical management of the infection. As cysts of different stages show very different responses to various management options,41–44 staging supported through remote advice by experts in treatment centers could be helpful.
Other Infectious Diseases with Potential for Pocus Application
Amebic liver abscess.
Amebiasis is one of the most common parasitic diseases worldwide and is prevalent in all tropical countries.45 Amebic liver abscess is more common in adults than in children and more common in men than in women. Patients usually present with fever, possibly right upper quadrant pain and jaundice. The condition is well suited for a POCUS approach.46
Sonographically, amebic liver abscess presents as a focal hepatic lesion, which is single in 60% of cases and is most commonly located in the posterior part of the right lobe (Figure 4A ). The amebic abscess is usually hypoechoic compared with normal liver tissue, without an appreciable rim or capsule. In the center or at the periphery of the amebic abscess, hyperechoic areas may be seen. After anti-amebic treatment,47 the lesion tends to become more hypoechoic and the margins become better defined.48,49 Serology can support the diagnosis when available; US-guided aspiration shows material of necrotic hepatocytes (“anchovy sauce”) typical in amebic abscesses. Diagnosis does usually not require aspiration. The clinical and sonographic picture, in conjunction with a history of possible exposure, is sufficient to start metronidazole treatment. Today, the indication for aspiration as diagnostic or therapeutic intervention is mainly limited to cases with an acute risk of rupture.50
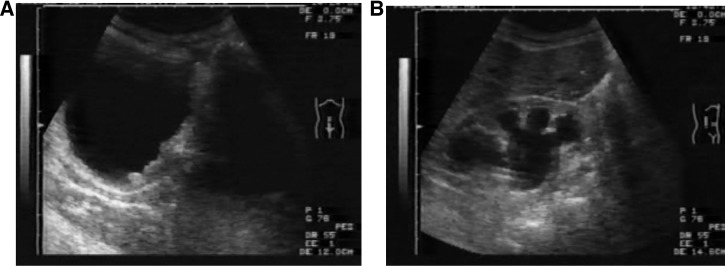
Figure 4.
(A) Right longitudinal upper quadrant view: amebic liver abscess posteriorly in the right lobe of the liver, presenting as a round hypoechoic lesion with hyperechoic debris and without a clearly discernable wall. (B) Right longitudinal upper quadrant view: pyogenic liver abscess presenting as an irregularly shaped, hypo- to anechoic lesion, containing hyperechoic gas bubbles with posterior acoustic shadowing.
The main clinical and sonographic differential diagnosis of amebic liver abscess is pyogenic liver abscess (Figure 4B). These are more commonly reported outside the tropics, often in patients with risk factors, such as biliary tree infections, diverticulitis, and a history of abdominal intervention. Although occasionally difficult to identify in the early stages, because of similar echogenicity of the surrounding liver tissue, pyogenic lesions eventually become hypoechoic compared with liver and can be more variable in shape and often have irregular walls. Pyogenic liver abscesses are also more often multiple, involving both lobes of the liver, and some show areas of marked echogenicity due to gas bubbles, which are not a feature of amebic abscesses unless superinfected. Treatment can be attempted with broad-spectrum antibiotics covering gram-negative and anaerobic bacteria.
A few further etiologic infectious differentials of abscess-like liver lesions need to be mentioned. If a central calcification is visible within the abscess, Brucella infection should be considered.51 Fasciola infection may present with hypoechoic lesions, especially subcapsular, and forming linear “tracks” through the liver.52 As with hepatic CE, other differential diagnoses of focal liver lesions, infectious and noninfectious, need to be considered.
Apart from individual case descriptions,46 no published data on the use of POCUS to diagnose amebic and other liver abscesses is available. POCUS protocols to screen the liver using 3–4 scan positions, including an intercostal and epigastric approach appear feasible, but will need validation in further studies. Upon finding a characteristic lesion, antibiotic treatment may be started. However, if a liver lesion does not show the typical, characteristic appearances of an abscess or CE cyst for example, and the binary approach of POCUS cannot be applied, the findings should be viewed with caution and treatment decision should be guided by clinical assessment. Referral for a formal US assessment or other imaging, where available, should also be considered.
Schistosomiasis.
Schistosomiasis is a waterborne helminthic infection mainly affecting either the urogenital tract (Schistosoma haematobium) or the gastrointestinal tract (Schistosoma mansoni, Schistosoma japonicum). To a lesser extent, all can affect the lung causing pulmonary hypertension.53 More than 250 million people are affected worldwide and there are more than 200,000 deaths per year attributable to schistosomiasis in sub-Saharan Africa.54
Schistosomiasis-associated morbidity is due to inflammation and consecutive fibrosis around entrapped eggs in the tissues. This leads to progressive organ damage and failure.53 It is important to note that morbidity persists even after eggs are no longer detectable in stool or urine. This highlights the importance of early antihelminthic therapy to prevent and reverse early fibrosis.55
Urogenital schistosomiasis.
Urogenital infection is seen mainly in sub-Saharan Africa, Egypt, and on the Arabian Peninsula. Schistosoma haematobium adult worms mature in the vesical plexus. The hallmark symptoms of urogenital schistosomiasis are dysuria and hematuria; earlier symptoms, particularly in children, include fatigue and anemia.56 The peak of morbidity is observed in children aged 7–14 years; however, infection occurs as early as infancy in endemic areas.57 In longstanding infections, symptoms of urinary tract obstruction and kidney failure are seen, secondary to fibrosis of bladder and ureter. Squamous cell carcinoma of the bladder is a possible late complication.
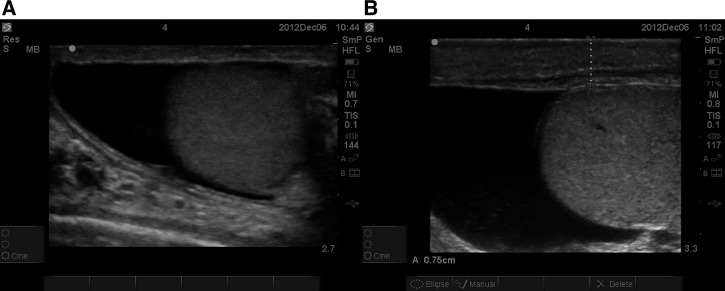
Fibrotic changes of the urinary tract because of schistosomiasis can easily be identified by US,58 and findings are described in WHO guidelines for identification and reporting of schistosomiasis.59 Bladder wall thickening and intravesical masses are common observations; in advanced disease, upper urinary tract obstruction is characterized by dilatation of the renal pelvis (Figure 5 ).
Figure 5.
(A) Longitudinal pelvic view: thickened and irregular wall of the urinary bladder secondary to Schistosoma haematobium infection. (B) Right longitudinal flank view: dilatation of the renal collecting system, secondary to fibrosis and obstruction in S. haematobium infection.
US in urinary schistosomiasis has been reported to be an “simple-to-learn” examination.60 In support of this assertion, the detection of urinary tract dilatation (e.g., as a consequence of urolithiasis) is commonly taught in POCUS courses in EM for the evaluation of flank pain. A POCUS protocol for urinary schistosomiasis using the lateral abdominal scans to visualize the kidneys, and a pelvic scan for the bladder could be developed and studied for clinical feasibility and value. As schistosomiasis has a highly focal geographical distribution, it is important to identify endemic areas and patient groups at risk. In former hyperendemic regions, where control programs have reduced the prevalence of infection, patients with low-intensity infection and sequelae may still be found. Diagnosis may be missed if it is only based on the detection of eggs in urine, as the egg excretion does not necessarily correlate with egg entrapment. Patients with urogenital schistosomiasis could therefore be identified by suggestive POCUS and then treated with praziquantel. Most bladder pathology regresses after treatment and can be monitored by US. Urinary tract dilatation frequently persists even in successfully treated patients.61 Non-resolving masses, especially in adult patients, should be investigated further by cystoscopy in view of the risk of bladder cancer.
Intestinal schistosomiasis.
Although the highest prevalence of S. mansoni infection leading to intestinal and hepatosplenic disease is found in sub-Saharan Africa, cases are also encountered in the Caribbean and South America, mostly Brazil. Schistosoma japonicum, affecting similar organs, remains endemic in limited areas of China, the Philippines, and parts of Indonesia.62 As S. mansoni adult worms mature in the portal vein, schistosomiasis-associated morbidity develops as eggs become entrapped in the tissues (bowel wall and periportal area) causing initial inflammation and subsequent fibrosis. Liver changes evolve from mild to severe periportal fibrotic changes with preservation of parenchyma until the final stages. Reactive splenic hyperplasia and portal hypertension ensue and dire downstream consequences include death from bleeding of esophageal varices.63
The diagnostic sonographic liver features, such as echogenic rings or streaks around the portal venous branches and echogenic bands extending from the main portal vein to the liver surface, are well described; various fibrosis patterns are summarized in a WHO report (Figure 6 ).59 In S. japonicum infections, the additional finding of a network of fibrosis may be seen, resulting in a so-called “tortoise back” appearance.59 The WHO patterns are well established and widely used.64
Figure 6.

Epigastric transverse view: liver with bright hyperechoic fibrosis surrounding the intrahepatic portal vessels, due to Schistosoma mansoni.
Focused US in intestinal schistosomiasis could be used for different purposes depending on the stage of the disease: 1) identifying early, potentially reversible fibrotic changes (WHO patterns B–D) in patients (mostly children) from endemic areas, who would benefit from medical treatment with antiparasitic drugs (praziquantel) and 2) identifying affected patients at imminent risk of bleeding (WHO patterns E and F), who might benefit from endoscopy.
WHO patterns B–D, representing patients with mild liver fibrosis, are not pathognomonic and can be difficult to differentiate from normal liver or other disease etiologies.65 The interobserver agreement has been found to be low, especially for mild cases.66 Without the US imaging experience needed to subcategorize these patients accurately, misdiagnosis of milder cases of intestinal schistosomiasis can easily occur. Patients with image pattern B and C rarely need endoscopy as their risk of bleeding is low. However, in endemic areas, those patients could benefit from early treatment that potentially slows down the development of ongoing disease, and reverses early fibrosis.
US can reliably visualize significant hepatic fibrosis (WHO patterns E and F), which is helpful in identifying patients with clinically advanced disease. These patients are at higher risk of variceal bleeding67 and should undergo endoscopy if possible. The patient's risk for variceal bleeding increases when portal hypertension is present. Sonographic changes suggestive of portal hypertension are an increased diameter of the portal vein (normally < 12 mm in adults) or splenic vein (normally < 9 mm),68 the presence of ascites, and the development of portosystemic collateral vessels.59 The most commonly described collateral veins are the perigastric, the paraumbilical, and the splenorenal veins. Detection is increased by color Doppler, which also allows detection of hepatofugal circulation.68 Enlargement of the caudate lobe compared with the right lobe is another finding, which is relatively easy to visualize by US, and reflects changes in portal blood supply in the cirrhotic liver. Caudate lobe enlargement has been described in patients with schistosomiasis.69 Splenomegaly can also be a sign of portal hypertension, and in schistosomiasis, the spleen may show multiple nonspecific tiny echogenic foci (Gamna–Gandy bodies).70 The size of the spleen is easy to assess; however, possible alternative diagnoses such as chronic splenomegaly in areas hyperendemic for malaria, visceral leishmaniasis (VL), or chronic HIV infection reduce its entity-specific diagnostic value in the absence of collaterals. When signs of portal hypertension are present, patients should undergo endoscopy whenever possible even if they only show milder forms of periportal fibrosis (pattern D).
For busy clinicians, the entire WHO protocol, including multiple measurements, might be too complicated and time consuming. A simplified POCUS protocol applying a few standardized liver views could be devised to identify patients with hepatosplenic involvement in intestinal schistosomiasis and to identify in particular those patients at risk of variceal bleeding. The results would guide management decisions: antihelminthic treatment47 and sonographic follow-up for mild cases and antihelminthic treatment and referral to a tertiary center with capacity to perform endoscopic sclerotherapy for severe cases.
Lymphatic filariasis.
Lymphatic filariasis, predominantly caused by Wuchereria bancrofti, is a disfiguring and disabling disease affecting an estimated 120 million people throughout the tropics. The highest burden of pathology is born by infected men showing hydrocele; another sign is lower limb lymphedema.
US has proven particularly useful in detecting pathology in male patients. So far, it has mainly been used to detect moving worms in supratesticular lymphatic vessels of infected men participating in clinical trials (the so-called “filarial dance sign”). Worm nest finding in women may also be possible, although less frequently documented.71 Large volume hydrocele in males, hyperechoic appearance of scrotal fluid, and presence of lymph scrotum (thickened scrotal skin > 0.45 cm, porous and wart like skin appearance, pain attacks, and leakage of lymph fluid) are associated with increased risk of testicular inflammation and necrosis (Figure 7 ).72 Recently, it has been reported that 56% of examined males in an endemic area in Ghana presented with hydroceles of variable degree and 9% showed echodense fluid,73 suggesting a considerable proportion of patients to be at risk of testicular inflammation and necrosis; the relative frequency of different “filaricele” conditions is, however, unknown.
Figure 7.
(A) Longitudinal scan of hemiscrotum showing anechoic fluid hydrocele. (B) Longitudinal scan of hemiscrotum showing low-intensity echoes in hydrocele fluid and thickened scrotal skin.
The use of POCUS approach beyond clinical trials for management of individual patients has received much less attention. Brief US protocols scanning the scrotum for abovementioned signs could be useful in allocating patients with hydrocele to high- or low-risk groups and to adapt the therapeutic approach. Medical treatment with doxycycline ameliorates lymphedema and hydrocele in infected patients (i.e., with detectable filarial circulating antigens).74,75 Interestingly, doxycycline treatment has also been found to ameliorate mild to moderate lymphedema in patients without active infection (i.e., filarial antigen negative),76 but so far it is unknown if this treatment is also effective in early stages of hydrocele in patients without active infection. Surgical programs for hydrocele due to lymphatic filariasis have been launched,77 and it is crucial to identify patients at high risk of scrotal complications for referral to surgery. POCUS could play a decisive role in this identification.
Visceral Leishmaniasis.
Each year, an estimated 500,000 new patients suffer from VL caused by many different species of Leishmania; the disease burden is particularly high on the Indian subcontinent and in east Africa.78 Patients present with fever, cough, abdominal pain, diarrhea, wasting, and pancytopenia. US consistently reveals hepatosplenomegaly, and, in a large proportion of cases, abdominal lymphadenopathy.79,80 In recent reports, nodular changes in the spleen have been reported, particularly in children81 but also in adults.82
Whether these US findings, which could be incorporated into a POCUS protocol, could help with the diagnosis or follow-up of VL and/or with the differential diagnosis between TB and VL in coendemic areas, remains to be studied. The hardest-hit regions (southern Sudan; Bihar State, India) would be locations where such POCUS protocols could be of value and where studies of the validity of such POCUS protocols could be conducted.
Viral hemorrhagic fever.
Viral hemorrhagic fevers (VHFs) are caused by a variety of viruses (Arenaviridae, Filoviridae, Bunyaviridae, Flaviviridae, and Rhabdoviridae). Worldwide, dengue virus is the most common VHF, but in specific geographic areas other viruses such as Crimean–Congo hemorrhagic fever (CCHF) virus may be also prevalent. Because of the large-scale outbreak in west Africa in 2014 and its high mortality rate,83 the Ebola virus has recently gained much importance. Clinically, VHF infections present with fever, headache and muscle pain, rashes, and abdominal symptoms. On progression, hemorrhagic phenomena such as thrombocytopenia, bruises, and internal bleeding occur, which may be followed by shock and death.
Effusions detected by US (pleural, pericardial, and ascitic) have been described as signs of plasma leakage in children84 and adults85 with dengue infection. The presence of effusions correlated with progression to more severe forms of the disease (dengue hemorrhagic fever (DHF), dengue shock syndrome), and its negative predictive value was found to be very high.85 Gallbladder wall thickening85,86 and subcapsular splenic and hepatic fluid collections87 have also been reported as signs of plasma leakage. It has been suggested that during a dengue epidemic, the diagnosis of DHF should be considered when US demonstrates gallbladder wall thickening, ascites, splenomegaly, and pleural effusion in a febrile patient with thrombocytopenia.88
Similarly, in a multivariate analysis in CCHF, gallbladder wall thickening, and intra-abdominal fluid collections were found to be significantly associated with disease severity.89,90 Validation of a standardized POCUS protocol to diagnose and predict severity of VHF in epidemic situations and to adapt monitoring and supportive treatment accordingly appears worthwhile.
Beside the potential predictive value for severity assessment in VHF, US can be used to determine hemodynamic parameters in patients with VHF. POCUS is well established in the care of critically ill patients for the assessment of the filling status of the inferior vena cava and the left ventricle.91 Intercostal scanning of the lung can show suggestive signs of interstitial pulmonary edema, and thus guide fluid administration.92 This is particularly helpful in patients with highly contagious VHF as other forms of physical examination such as auscultation may be hindered by isolation measures and protective equipment. A preliminary report on the use of US in patients infected with Ebola virus supports these indications and suggests the use of focused POCUS done by infectious disease clinicians trained in isolation measures and in relevant POCUS protocols.93 Small mobile US equipment should remain in the isolation unit to prevent spread of the infection.
Miscellane Infectious Diseases
The potential value of US in supporting diagnosis and management of a range of other infectious diseases in tropical areas and beyond appears huge and increasing. Varying experience with US for assessment of infectious diseases has been reported and some are mentioned in brief below. The suitability and value of POCUS protocols in these diseases remains to be studied. Diagnostic usefulness of US in infections caused by flukes other than Schistosoma spp. has been reported for fascioliasis-related hepatic and biliary disease,52,94,95 pulmonary and abdominal paragonimiasis,96 and clonorchiasis.97 Other helminthic infections for which US has been used include onchocerciasis,98–100 abdominal and ocular toxocariasis,101,102 and ascariasis and its complications such as bile duct invasion.103–105 Further parasitic diseases for which experimental US experience is available include Chagas disease,106 myiasis,106,107 and even malaria.108 The usefulness of POCUS in bacterial infectious diseases has recently been reviewed, describing differentiation between cellulitis and abscesses, diagnosis of septic arthritis, identifying underlying causes of sepsis, and pneumonia.109 Further US applications have been reported for leprosy,110,111 rheumatic heart disease as sequelae of Streptococcus pyogenes infection,112 mycetoma,105 and opportunistic infections in patients living with HIV.113,114 With US getting closer to the point of care and into the hands of treating physicians, its use in infectious diseases may increase, and further POCUS indications may become established.
Technical and Training Requirements
Technical.
Technical requirements for POCUS equipment are relatively basic. Most commercially available machines can be used.
The size of the device plays an important role when mobile scanning is intended.
The availability of electricity and US gel needs to be considered in remote settings, and a voltage stabilizer may be required in a situation where voltage peaks put the machine at risk of damage.
In many places, only gray-scale (“black and white”) scanners will be available, which can perfectly serve the purpose. The additional availability of color Doppler on the scanner is helpful to identify blood flow. It will, for example, be helpful to find collaterals in abdominal schistosomiasis, but also be of value in identifying vessels in other anatomical regions. It does, however, significantly increase the cost of the equipment.
To facilitate web-based, remote review and support, an option to extract digital images and video clips onto an external storage device is highly desirable.
The final choice of equipment will mainly depend on local availability and maintenance provision. Obviously, the available budget plays a substantial role, but cost of equipment has come down significantly in recent years, improving affordability.
Training.
US is a highly operator-dependent tool, which can easily lead to misdiagnosis if implemented inappropriately and without adequate training. The WHO scientific Group on Clinical Diagnostic Imaging concluded that “… more important than the equipment is the availability of skills….”115 For comprehensive US use, the WHO recommends that physicians should undergo training over 3–6 months, including 300–500 examinations. However, these formal training programs, while ideal, are often too time consuming to achieve meaningful coverage in resource-limited settings. In the absence of formally trained sonographers or radiologists, US training should be aimed at health-care professionals, especially those working on the front line. In particular, this means general physicians and clinical officers in district hospitals and clinics who have little or no experience with imaging technology and who cannot afford to be away from their clinical duties for a long training course. Focused POCUS applications do not require as much training, and thus allow a degree of flexibility. If physicians could be trained in short courses, which will reduce their absence from clinical duties, while providing them with the most relevant US skills,10 this would widen access to this very useful diagnostic modality.
Short courses have been reported to be sufficient to teach POCUS modules.116 Regular, short US courses with a focus on infectious diseases are held in Pavia, Italy,117 in Lima, Peru,118 and previously in Liverpool, United Kingdom.119
However, the great advantage of courses held directly in low-resource settings is that they will allow local physicians to participate without excessive travel expenses or lengthy leave of absence. In addition, this allows for more rapid and relevant learning, as infection-specific pathologic findings are more prevalent in endemic areas. Short training courses have been reported from various sites in resource-limited settings.9,120–122 However, there has been neither widespread dissemination nor standardization of these training initiatives nor robust validation, particularly in terms of the operator's maintenance of adequate technical ability in the long term.
In addition, there is no literature available on how many exams are needed to achieve competency in US skills for clinicians in developing countries. However, in industrialized countries, figures of approximately 30–40 supervised examinations are consistently reported in the literature to master one particular POCUS protocol. For example, 40 exams are reportedly necessary to accurately detect intrauterine first trimester pregnancy and complications,123 while only 30 may be needed to learn how to detect hydronephrosis.124 As it has become apparent that some operators acquire skills more rapidly than others, there is an increasing move toward uniform, cross-specialty competency-based assessment, which may be of benefit when designing future courses.125
As external trainers are often only available for short periods, other methods to ensure continuous support and quality assurance need to be considered. With increasing availability of internet access and faster connections in geographically remote settings, the application of telemedicine solutions could be expanded to support practitioners in areas where direct supervision is scarce or absent. Recently, the feasibility of a tele-US system using Skype™ (Luxembourg, Luxembourg) and cheap, widely available, consumer electronics equipment, was successfully piloted for remote supervision of FASH exams in Lambaréné, Gabon.12 Another, even easier, option is the extraction of digital images and video clips that can then be sent via secure telemedicine servers for review and second opinion.
A number of introductory texts covering the use of US in infectious diseases exist.126–128 All are specifically aimed at physicians with limited imaging experience working in resource-limited settings and are available free or at low cost.
Several associations such as the American College of Emergency Physicians129 endorse the approach of focused US exams. A section of the International Federation for Emergency Medicine has recently developed a consensus document drawing on regional and national guideline standards and training requirements to summarize recommendations for an appropriate level of training that will allow for the provision of a safe and effective US service.130 Analogous to these recommendations, the development of standardized training and practice guidelines for POCUS courses in the field of infectious diseases, based on previous experience and available training material, is a key priority in the field. Recommendations and standards, building on those existing for EM US, should be created. In our opinion, a modular approach consisting of theoretical and practical sessions would be feasible. Initially, protocols and questions, which are easier to master, such as FASH or the detection of urinary tract changes in schistosomiasis can be taught. Once the trainee gains experience in the technology of US, technically more demanding topics such as liver POCUS, echinococcal cyst morphology, and even the assessment of collateral vessels may be taught in further modules. A rigorous evaluation of these training methods is highly desired, but unfortunately not yet available. Modular training could facilitate the availability and accelerate the spread of POCUS.
Conclusions
US is a powerful diagnostic tool, which has become increasingly available and affordable. From the aforementioned considerations and our own clinical experience, we are of the opinion that POCUS is ideally suited to the diagnosis of several infectious conditions in resource-limited settings (Table 1). We believe that focused, high-quality training will be the key to the successful expansion of US applications. To facilitate this, standardized protocols and training curricula that enable health-care workers to answer dedicated, “focused” questions need to be developed and validated in the field. Using the focused approach will make US diagnosis available to patients who would otherwise have very limited or no access to medical imaging.
Table 1.
Summary of reported experiences of POCUS assessment of tropical infectious diseases
| Disease (protocol) | Population | Clinical symptoms | US findings | Suggested action | Evidence | Reference |
|---|---|---|---|---|---|---|
| TB (FASH) | Africa (particularly southern Africa), Asia, and South America with high HIV/TB coinfection prevalence | Fever | Enlarged hypoechoic lymph nodes | Do sputum smear exam | Well described and widely used in South Africa | 11–15,127 |
| Weight loss | Micro-abscesses in spleen and/or liver | Start empirical TB treatment | ||||
| Cough | Pleural effusion | Test for HIV if not done previously and treat accordingly | ||||
| Abdominal symptoms (diarrhea, pain, and abdominal distension), shortness of breath | Pericardial effusion | |||||
| Hypotension | Ascites | |||||
| Echinococcosis (FASE) | Sheep farming populations, South America, Middle East, eastern Europe, The Mediterranean, Central Asia, China, east Africa | Symptoms depend on cyst's size, number, and organ affected | Appearance depends on cyst stage (WHO-IWGE) | Stage-specific treatment of liver CE (WHO-IWGE) | FASE implemented in Argentina | 33–36,40,43 |
| Jaundice | CE1: anechoic with double wall | |||||
| Right upper quadrant pain | CE2: honeycomb appearance, adjacent anechoic daughter vesicles contained in the “mother” cyst's wall | |||||
| Most cases have few or no symptoms | CE3a: anechoic with “lily sign” (detached endocyst) | |||||
| CE3b: daughter vesicles within a solid matrix of the “mother” cyst | ||||||
| CE4: inhomogeneous content with visible hypoechoic folded endocyst (“ball of wool” sign) | ||||||
| CE5: same as CE4 with calcified wall | ||||||
| Amebic liver abscess | Worldwide in tropical countries | Fever | Hypoechoic, but not anechoic, round homogenous liver lesion: possible amebic abscess | Start antibiotic e.g., metronidazole treatment | Individual descriptive studies only | 46,48,49 |
| Right upper quadrant abdominal pain | Differentials: | Amebic serology | ||||
| a) Lesion containing gas, irregular shape: possible pyogenic abscess | In imminent rupture, US-guided aspiration | |||||
| b) Central calcification: possible Brucella abscess | Brucella serology | |||||
| c) Noninfectious lesion, e.g., necrotic tumor | ||||||
| Intestinal schistosomiasis | People in contact with fresh water in Africa, southeast Asia, and Brazil | Abdominal pain | Increasingly wide echogenic fibrosis around portal tracts (pattern D–F) | Refer for endoscopy for patterns E + F | WHO guidelines available for population screening | 59,64–70 |
| Intestinal bleeding | “Tortoise back” pattern in Asia | Refer also if pattern D and signs of portal hypertension | ||||
| Malabsorption | Dilated portal and splenic vein and collateral vessels | Treat medically and advise against exposure for other cases | ||||
| Hepatosplenomegaly | Enlarged caudate lobe | |||||
| Fever | Splenomegaly | |||||
| Eosinophilia | Ascites | |||||
| Malnutrition, anemia | ||||||
| Urogenital schistosomiasis | People in contact with fresh water in Egypt and sub-Saharan Africa | Hematuria | Irregular, thickened bladder wall (in fully distended bladder) | Medical treatment | WHO guidelines available for population screening | 58–60 |
| Urinary tract symptoms | Upper urinary tract dilation | Possibly referral for cystoscopy in case of persistence | ||||
| Fever | Bladder polyps and masses | |||||
| Eosinophilia | ||||||
| Malnutrition, anemia | ||||||
| Dyspareunia | ||||||
| Infertility | ||||||
| VHFs (e.g., Dengue, CCHF, Ebola) | Widely prevalent throughout the tropics | Fever | Effusions (pericardial, pleural) and ascites as signs of plasma leakage | Intensified surveillance for patients with negative prognostic signs | Individual descriptive studies only | 84–87,89,90,93 |
| Muscle pain | Gall bladder wall thickening | Changes in fluid replacement therapy in shock | ||||
| Headache | Subcapsular hepatic fluid | Consider vast differential diagnoses | ||||
| Rash | Volume status assessment (IVC, left ventricle, and pulmonary edema) | |||||
| Petechia | ||||||
| Lymphatic filariasis | Sub-Saharan Africa, southeast Asia, and endemic areas of Central and South America | Hydrocele | Dilation of inguinal lymphatic vessels | Scrotal surgery for hyperechoic, complex hydrocele | Individual descriptive studies only | 71,73 |
| Lower limb lymphedema | Filarial dance sign | Conservative treatment with doxycycline and deferred surgery for echo-free hydrocele | ||||
| Echo-free or hyperechoic hydrocele | ||||||
| Thickened scrotal skin | ||||||
| Visceral leishmaniasis | Indian subcontinent, Sudan | Fever | Hepatosplenomegaly | Unclear | Individual descriptive studies only | 79,80 |
| Abdominal pain | Lymph node enlargement | |||||
| Pancytopenia | Nodular splenic lesions (diagnostic accuracy of these findings is currently unclear for diagnosis of visceral leishmaniasis) |
CCHF = Crimean–Congo hemorrhagic fever; CE = cystic echinococcosis; FASE = focused assessment with sonography for echinococcosis; FASH = focused assessment with sonography for HIV-associated TB; HIV = human immunodeficiency virus; IVC = inferior vena cava; POCUS = point-of-care ultrasound; TB = tuberculosis; US = ultrasound; VHFs = viral hemorrhagic fever; VL = visceral leishmaniasis; WHO-IWGE = World Health Organization Informal Working Group on Echinococcosis.
Footnotes
Authors' addresses: Sabine Bélard, Department of Pediatric Pneumology and Immunology, Charité Universitätsmedizin Berlin, Berlin, Germany, E-mail: sabine.belard@charite.de. Francesca Tamarozzi, Department of Clinical, Surgical, Diagnostic and Pediatric Sciences, University of Pavia, Pavia, Italy, E-mail: f_tamarozzi@yahoo.com. Amaya L. Bustinduy, Paediatric Infectious Diseases Research Group, Institute of Infection and Immunity, St. George's University of London, United Kingdom, E-mail: bustinji06@gmail.com. Claudia Wallrauch, Department of Medicine, Klinikum Muenchen-Perlach, Munich, Germany, E-mail: claudiawallrauch@web.de. Martin P. Grobusch and Tom Heller, Center of Tropical Medicine and Travel Medicine, Department of Infectious Diseases, Division of Internal Medicine, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands, E-mails: m.p.grobusch@amc.uva.nl and echnatom@web.de. Walter Kuhn, Emergency Medicine, Medical College of Georgia, Georgia Regents University, Augusta, GA, E-mail: tkuhn@gru.edu. Enrico Brunetti, Division of Infectious and Tropical Diseases, University of Pavia/IRCCS San Matteo Hospital Foundation, Pavia, Italy, E-mail: enrico.brunetti@unipv.it. Elizabeth Joekes, Department of Radiology, Liverpool School of Tropical Medicine, Liverpool, United Kingdom, E-mail: e.joekes@liverpool.ac.uk.
References
- 1.Richter J, Hatz C, Haussinger D. Ultrasound in tropical and parasitic diseases. Lancet. 2003;362:900–902. doi: 10.1016/S0140-6736(03)14334-6. [DOI] [PubMed] [Google Scholar]
- 2.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364:749–757. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 3.Hanscheid T, Rebelo M, Grobusch MP. Point-of-care tests: where is the point? Lancet. 2014;14:922. doi: 10.1016/S1473-3099(14)70914-4. [DOI] [PubMed] [Google Scholar]
- 4.Ma OJ, Mateer JR, Ogata M, Kefer MP, Wittmann D, Aprahamian C. Prospective analysis of a rapid trauma ultrasound examination performed by emergency physicians. J Trauma. 1995;38:879–885. doi: 10.1097/00005373-199506000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Mateer J, Plummer D, Heller M, Olson D, Jehle D, Overton D, Gussow L. Model curriculum for physician training in emergency ultrasonography. Ann Emerg Med. 1994;23:95–102. doi: 10.1016/s0196-0644(94)70014-1. [DOI] [PubMed] [Google Scholar]
- 6.American Institute of Ultrasound in Medicine AIUM practice guideline for the performance of the focused assessment with sonography for trauma (FAST) examination. J Ultrasound Med. 2014;33:2047–2056. doi: 10.7863/ultra.33.11.2047. [DOI] [PubMed] [Google Scholar]
- 7.Mohammad A, Hefny AF, Abu-Zidan FM. Focused Assessment Sonography for Trauma (FAST) training: a systematic review. World J Surg. 2014;38:1009–1018. doi: 10.1007/s00268-013-2408-8. [DOI] [PubMed] [Google Scholar]
- 8.Brunetti E. Ultrasound in tropical medicine. In: Farrar J, Junghanss T, Kang G, Lalloo D, White NJ, editors. Manson's Tropical Diseases. 23rd edition. Endinburgh, United Kingdom: Elsevier; 2013. pp. 60–67. [Google Scholar]
- 9.Shah S, Noble VE, Umulisa I, Dushimiyimana JM, Bukhman G, Mukherjee J, Rich M, Epino H. Development of an ultrasound training curriculum in a limited resource international setting: successes and challenges of ultrasound training in rural Rwanda. Int J Emerg Med. 2008;1:193–196. doi: 10.1007/s12245-008-0053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maru DS, Schwarz R, Jason A, Basu S, Sharma A, Moore C. Turning a blind eye: the mobilization of radiology services in resource-poor regions. Global Health. 2010;6:18. doi: 10.1186/1744-8603-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heller T, Wallrauch C, Goblirsch S, Brunetti E. Focused assessment with sonography for HIV-associated tuberculosis (FASH): a short protocol and a pictorial review. Crit Ultrasound J. 2012;4:21. doi: 10.1186/2036-7902-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Janssen S, Grobusch MP, Heller T. ‘Remote FASH’ tele-sonography—a novel tool to assist diagnosing HIV-associated extrapulmonary tuberculosis in remote areas. Acta Trop. 2013;127:53–55. doi: 10.1016/j.actatropica.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 13.Heller T, Goblirsch S, Bahlas S, Ahmed M, Giordani MT, Wallrauch C, Brunetti E. Diagnostic value of FASH ultrasound and chest X-ray in HIV-co-infected patients with abdominal tuberculosis. Int J Tuberc Lung Dis. 2013;17:342–344. doi: 10.5588/ijtld.12.0679. [DOI] [PubMed] [Google Scholar]
- 14.Heller T, Wallrauch C, Brunetti E, Giordani MT. Changes of FASH ultrasound findings in TB-HIV patients during anti-tuberculosis treatment. Int J Tuberc Lung Dis. 2014;18:837–839. doi: 10.5588/ijtld.13.0029. [DOI] [PubMed] [Google Scholar]
- 15.van Hoving DJ, Lamprecht HH, Stander M, Vallabh K, Fredericks D, Louw P, Muller M, Malan JJ. Adequacy of the emergency point-of-care ultrasound core curriculum for the local burden of disease in South Africa. Emerg Med J. 2013;30:312–315. doi: 10.1136/emermed-2012-201358. [DOI] [PubMed] [Google Scholar]
- 16.Belard S, Heller T, Grobusch MP, Zar HJ. Point-of-care ultrasound: a simple protocol to improve diagnosis of childhood tuberculosis. Pediatr Radiol. 2014;44:679–680. doi: 10.1007/s00247-014-2971-7. [DOI] [PubMed] [Google Scholar]
- 17.WHO Global Tuberculosis Report 2014. 2014. http://apps.who.int/iris/bitstream/10665/137094/1/9789241564809_eng.pdf?ua=1 Available at. Accessed May 29, 2015.
- 18.von Reyn CF, Kimambo S, Mtei L, Arbeit RD, Maro I, Bakari M, Matee M, Lahey T, Adams LV, Black W, Mackenzie T, Lyimo J, Tvaroha S, Waddell R, Kreiswirth B, Horsburgh CR, Pallangyo K. Disseminated tuberculosis in human immunodeficiency virus infection: ineffective immunity, polyclonal disease and high mortality. Int J Tuberc Lung Dis. 2011;15:1087–1092. doi: 10.5588/ijtld.10.0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.WHO Improving the Diagnosis and Treatment of Smear-Negative Pulmonary and Extrapulmonary Tuberculosis among Adults and Adolescents: Recommendations for HIV-Prevalent and Resource-Constrained Settings. 2006. http://www.who.int/tb/publications/2006/tbhiv_recommendations.pdf Available at. Accessed May 17, 2015.
- 20.Luzze H, Elliott AM, Joloba ML, Odida M, Oweka-Onyee J, Nakiyingi J, Quigley M, Hirsch C, Mugerwa RD, Okwera A, Johnson JL. Evaluation of suspected tuberculous pleurisy: clinical and diagnostic findings in HIV-1-positive and HIV-negative adults in Uganda. Int J Tuberc Lung Dis. 2001;5:746–753. [PubMed] [Google Scholar]
- 21.Reuter H, Burgess LJ, Doubell AF. Epidemiology of pericardial effusions at a large academic hospital in South Africa. Epidemiol Infect. 2005;133:393–399. doi: 10.1017/s0950268804003577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brindle HE, Allain TJ, Kampondeni S, Kayange N, Faragher B, Bates I, Joekes E. Utilization of ultrasound in medical inpatients in Malawi. Trans R Soc Trop Med Hyg. 2013;107:405–410. doi: 10.1093/trstmh/trt034. [DOI] [PubMed] [Google Scholar]
- 23.Heller T, Lessells RJ, Wallrauch C, Brunetti E. Tuberculosis pericarditis with cardiac tamponade: management in the resource-limited setting. Am J Trop Med Hyg. 2010;83:1311–1314. doi: 10.4269/ajtmh.2010.10-0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giordani MT, Brunetti E, Binazzi R, Benedetti P, Stecca C, Goblirsch S, Heller T. Extrapulmonary mycobacterial infections in a cohort of HIV-positive patients: ultrasound experience from Vicenza, Italy. Infection. 2012;41:409–414. doi: 10.1007/s15010-012-0336-4. [DOI] [PubMed] [Google Scholar]
- 25.Heller T, Wallrauch C, Lessells RJ, Goblirsch S, Brunetti E. Short course for focused assessment with sonography for human immunodeficiency virus/tuberculosis: preliminary results in a rural setting in South Africa with high prevalence of human immunodeficiency virus and tuberculosis. Am J Trop Med Hyg. 2010;82:512–515. doi: 10.4269/ajtmh.2010.09-0561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma OJ, Mateer JR. Trauma ultrasound examination versus chest radiography in the detection of hemothorax. Ann Emerg Med. 1997;29:312–315. doi: 10.1016/s0196-0644(97)70341-x. discussion 315–316. [DOI] [PubMed] [Google Scholar]
- 27.Rozycki GS, Feliciano DV, Ochsner MG, Knudson MM, Hoyt DB, Davis F, Hammerman D, Figueredo V, Harviel JD, Han DC, Schmidt JA. The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. J Trauma. 1999;46:543–551. doi: 10.1097/00005373-199904000-00002. discussion 551–552. [DOI] [PubMed] [Google Scholar]
- 28.Heller T, Goblirsch S, Wallrauch C, Lessells R, Brunetti E. Abdominal tuberculosis: sonographic diagnosis and treatment response in HIV-positive adults in rural South Africa. Int J Infect Dis. 2010;14((Suppl 3)):e108–e112. doi: 10.1016/j.ijid.2009.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev. 2004;17:107–135. doi: 10.1128/CMR.17.1.107-135.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wahlers K, Menezes CN, Wong ML, Zeyhle E, Ahmed ME, Ocaido M, Stijnis C, Romig T, Kern P, Grobusch MP. Cystic echinococcosis in sub-Saharan Africa. Lancet. 2012;12:871–880. doi: 10.1016/S1473-3099(12)70155-X. [DOI] [PubMed] [Google Scholar]
- 31.Eckert J, Gemmell M, Meslin F-X, Pawlowski Z. WHO/OIE Manual on Echinococcosis in Humans and Animals: A Public Health Problem of Global Concern. Geneva, Switzerland: World Organisation for Animal Health (Office International des Epizooties) and World Health Organization; 2001. http://whqlibdoc.who.int/publications/2001/929044522X.pdf Available at. Accessed May 17, 2015. [Google Scholar]
- 32.Wahlers K, Menezes CN, Romig T, Kern P, Grobusch MP. Cystic echinococcosis in South Africa: the worst yet to come? Acta Trop. 2013;128:1–6. doi: 10.1016/j.actatropica.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 33.Stojkovic M, Rosenberger K, Kauczor HU, Junghanss T, Hosch W. Diagnosing and staging of cystic echinococcosis: how do CT and MRI perform in comparison to ultrasound? PLoS Negl Trop Dis. 2012;6:e1880. doi: 10.1371/journal.pntd.0001880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brunetti E, Kern P, Vuitton DA. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114:1–16. doi: 10.1016/j.actatropica.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 35.WHO-IWGE International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop. 2003;85:253–261. doi: 10.1016/s0001-706x(02)00223-1. [DOI] [PubMed] [Google Scholar]
- 36.Del Carpio M, Mercapide CH, Salvitti JC, Uchiumi L, Sustercic J, Panomarenko H, Moguilensky J, Herrero E, Talmon G, Volpe M, Araya D, Mujica G, Calabro A, Mancini S, Chiosso C, Labanchi JL, Saad R, Goblirsch S, Brunetti E, Larrieu E. Early diagnosis, treatment and follow-up of cystic echinococcosis in remote rural areas in Patagonia: impact of ultrasound training of non-specialists. PLoS Negl Trop Dis. 2012;6:e1444. doi: 10.1371/journal.pntd.0001444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li T, Ito A, Pengcuo R, Sako Y, Chen X, Qiu D, Xiao N, Craig PS. Post-treatment follow-up study of abdominal cystic echinococcosis in Tibetan communities of northwest Sichuan Province, China. PLoS Negl Trop Dis. 2011;5:e1364. doi: 10.1371/journal.pntd.0001364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elmahdi IE, Ali QM, Magzoub MM, Ibrahim AM, Saad MB, Romig T. Cystic echinococcosis of livestock and humans in central Sudan. Ann Trop Med Parasitol. 2004;98:473–479. doi: 10.1179/000349804225003578. [DOI] [PubMed] [Google Scholar]
- 39.Macpherson CN, Kachani M, Lyagoubi M, Berrada M, Shepherd M, Fields PF, El Hasnaoui M. Cystic echinococcosis in the Berber of the Mid Atlas mountains, Morocco: new insights into the natural history of the disease in humans. Ann Trop Med Parasitol. 2004;98:481–490. doi: 10.1179/000349804225021343. [DOI] [PubMed] [Google Scholar]
- 40.Muhtarov M. First portable ultrasound based screening study in Bulgaria on the prevalence of cystic echinococcosis in Kardzhali district. Trakia J Sci. 2014;12((Suppl 1)):170–174. [Google Scholar]
- 41.Stojkovic M, Zwahlen M, Teggi A, Vutova K, Cretu CM, Virdone R, Nicolaidou P, Cobanoglu N, Junghanss T. Treatment response of cystic echinococcosis to benzimidazoles: a systematic review. PLoS Negl Trop Dis. 2009;3:e524. doi: 10.1371/journal.pntd.0000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rinaldi F, De Silvestri A, Tamarozzi F, Cattaneo F, Lissandrin R, Brunetti E. Medical treatment versus “Watch and Wait” in the clinical management of CE3b echinococcal cysts of the liver. BMC Infect Dis. 2014;14:492. doi: 10.1186/1471-2334-14-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Piccoli L, Tamarozzi F, Cattaneo F, Mariconti M, Filice C, Bruno A, Brunetti E. Long-term sonographic and serological follow-up of inactive echinococcal cysts of the liver: hints for a “watch-and-wait” approach. PLoS Negl Trop Dis. 2014;8:e3057. doi: 10.1371/journal.pntd.0003057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Golemanov B, Grigorov N, Mitova R, Genov J, Vuchev D, Tamarozzi F, Brunetti E. Efficacy and safety of PAIR for cystic echinococcosis: experience on a large series of patients from Bulgaria. Am J Trop Med Hyg. 2011;84:48–51. doi: 10.4269/ajtmh.2011.10-0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stanley SL., Jr Amoebiasis. Lancet. 2003;361:1025–1034. doi: 10.1016/S0140-6736(03)12830-9. [DOI] [PubMed] [Google Scholar]
- 46.Elia F, Campagnaro T, Salacone P, Casalis S. Goal-directed ultrasound in a limited resource healthcare setting and developing country. Crit Ultrasound J. 2011;3:51–53. [Google Scholar]
- 47.The Medical Letter Drugs for parasitic infections. Treat Guidel Med Lett. 2013;11((Suppl)):e1–e31. [Google Scholar]
- 48.Stoopen M, Kimura K. Amebiasis. The technology of the 80's. I. Ultrasound, computerized tomography and magnetic resonance: have they helped improve the diagnosis of hepatic abscess? Rev Gastroenterol Mex. 1989;54:167–175. [PubMed] [Google Scholar]
- 49.Mortele KJ, Segatto E, Ros PR. The infected liver: radiologic-pathologic correlation. Radiographics. 2004;24:937–955. doi: 10.1148/rg.244035719. [DOI] [PubMed] [Google Scholar]
- 50.Weinke T, Grobusch MP, Guthoff W. Amebic liver abscess—rare need for percutaneous treatment modalities. Eur J Med Res. 2002;7:25–29. [PubMed] [Google Scholar]
- 51.Heller T, Bélard S, Wallrauch C, Carretto E, Lissandrin R, Filice C, Brunetti E. Patterns of hepatosplenic Brucella abscesses on cross-sectional imaging. Am J Trop Med Hyg. 2015;93:761–766. doi: 10.4269/ajtmh.15-0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kabaalioglu A, Ceken K, Alimoglu E, Saba R, Cubuk M, Arslan G, Apaydin A. Hepatobiliary fascioliasis: sonographic and CT findings in 87 patients during the initial phase and long-term follow-up. Am J Roentgenol. 2007;189:824–828. doi: 10.2214/AJR.07.2127. [DOI] [PubMed] [Google Scholar]
- 53.Colley DG, Bustinduy AL, Secor WE, King CH. Human schistosomiasis. Lancet. 2014;383:2253–2264. doi: 10.1016/S0140-6736(13)61949-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.WHO Schistosomiasis. 2015. http://www.who.int/schistosomiasis/epidemiology/en/ Available at. Accessed May 29 2015.
- 55.King CH. Long-term outcomes of school-based treatment for control of urinary schistosomiasis: a review of experience in Coast Province, Kenya. Mem Inst Oswaldo Cruz. 2006;101((Suppl 1)):299–306. doi: 10.1590/s0074-02762006000900047. [DOI] [PubMed] [Google Scholar]
- 56.Bustinduy AL, Parraga IM, Thomas CL, Mungai PL, Mutuku F, Muchiri EM, Kitron U, King CH. Impact of polyparasitic infections on anemia and undernutrition among Kenyan children living in a Schistosoma haematobium-endemic area. Am J Trop Med Hyg. 2013;88:433–440. doi: 10.4269/ajtmh.12-0552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stothard JR, Sousa-Figueiredo JC, Betson M, Bustinduy A, Reinhard-Rupp J. Schistosomiasis in African infants and preschool children: let them now be treated! Trends Parasitol. 2013;29:197–205. doi: 10.1016/j.pt.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.King CH. Ultrasound monitoring of structural urinary tract disease in Schistosoma haematobium infection. Mem Inst Oswaldo Cruz. 2002;97((Suppl 1)):149–152. doi: 10.1590/s0074-02762002000900028. [DOI] [PubMed] [Google Scholar]
- 59.Richter J, Hatz C, Campagne G, Bergquist N, Jenkins J. Ultrasound in Schistosomiasis—A Practical Guide to the Standardized Use of Ultrasonography for the Assessment of Schistosomiasis-Related Morbidity. 2000. http://www.who.int/tdr/publications/documents/ultrasound-schistosomiasis.pdf Available at. Accessed May 17, 2015.
- 60.Bonnard P, Boutouaba S, Diakhate I, Seck M, Dompnier JP, Riveau G. Learning curve of vesico-urinary ultrasonography in Schistosoma haematobium infection with WHO practical guide: a “simple to learn” examination. Am J Trop Med Hyg. 2011;85:1071–1074. doi: 10.4269/ajtmh.2011.11-0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wagatsuma Y, Aryeetey ME, Sack DA, Morrow RH, Hatz C, Kojima S. Resolution and resurgence of Schistosoma haematobium-induced pathology after community-based chemotherapy in Ghana, as detected by ultrasound. J Infect Dis. 1999;179:1515–1522. doi: 10.1086/314786. [DOI] [PubMed] [Google Scholar]
- 62.WHO Health Topics: Schistosomiasis. 2015. http://www.who.int/topics/schistosomiasis/en/ Available at. Accessed May 27, 2015.
- 63.Bustinduy A, King CH. Schistosomiasis. In: Farrar J, Hotez PJ, Junghanss T, Kang G, Lalloo D, White NJ, editors. Manson's Tropical Diseases. 23rd edition. Edinburgh, United Kingdom: Elsevier; 2013. [Google Scholar]
- 64.el Scheich T, Holtfreter MC, Ekamp H, Singh DD, Mota R, Hatz C, Richter J. The WHO ultrasonography protocol for assessing hepatic morbidity due to Schistosoma mansoni. Acceptance and evolution over 12 years. Parasitol Res. 2014;113:3915–3925. doi: 10.1007/s00436-014-4117-0. [DOI] [PubMed] [Google Scholar]
- 65.Ruiz-Guevara R, de Noya BA, Valero SK, Lecuna P, Garassini M, Noya O. Clinical and ultrasound findings before and after praziquantel treatment among Venezuelan schistosomiasis patients. Rev Soc Bras Med Trop. 2007;40:505–511. doi: 10.1590/s0037-86822007000500003. [DOI] [PubMed] [Google Scholar]
- 66.King CH, Magak P, Salam EA, Ouma JH, Kariuki HC, Blanton RE. Measuring morbidity in schistosomiasis mansoni: relationship between image pattern, portal vein diameter and portal branch thickness in large-scale surveys using new WHO coding guidelines for ultrasound in schistosomiasis. Trop Med Int Health. 2003;8:109–117. doi: 10.1046/j.1365-3156.2003.00994.x. [DOI] [PubMed] [Google Scholar]
- 67.Richter J, Correia Dacal AR, Vergetti Siqueira JG, Poggensee G, Mannsmann U, Deelder A, Feldmeier H. Sonographic prediction of variceal bleeding in patients with liver fibrosis due to Schistosoma mansoni. Trop Med Int Health. 1998;3:728–735. doi: 10.1046/j.1365-3156.1998.00285.x. [DOI] [PubMed] [Google Scholar]
- 68.Pinto-Silva RA, Queiroz LC, Azeredo LM, Silva LC, Lambertucci JR. Ultrasound in schistosomiasis mansoni. Mem Inst Oswaldo Cruz. 2010;105:479–484. doi: 10.1590/s0074-02762010000400021. [DOI] [PubMed] [Google Scholar]
- 69.Abdalla Balla E, Abdalla Abdo M, Ayad C. Evaluation of caudate and right hepatic lobes ratio in patients with Schistosoma mansoni using ultrasound in Al-Fao area. Indian J Soc Res. 2013;4:11. [Google Scholar]
- 70.Gonzalez TD, Santos JEM, Sales DM, Takemoto K, Capobianco J, Brant PE, Colleoni R, Ahmed M, D'Ippolito G. Ultrasonographic assessment of splenic siderotic nodules in schistosomal patients with portal hypertension. Radiol Bras. 2008;41:69–73. [Google Scholar]
- 71.Mand S, Debrah A, Batsa L, Adjei O, Hoerauf A. Reliable and frequent detection of adult Wuchereria bancrofti in Ghanaian women by ultrasonography. Trop Med Int Health. 2004;9:1111–1114. doi: 10.1111/j.1365-3156.2004.01304.x. [DOI] [PubMed] [Google Scholar]
- 72.DeVries CR. The role of the urologist in the treatment and elimination of lymphatic filariasis worldwide. BJU Int. 2002;89((Suppl 1)):37–43. doi: 10.1046/j.1465-5101.2001.vries.137.x. [DOI] [PubMed] [Google Scholar]
- 73.Mand S, Debrah AY, Klarmann U, Mante S, Kwarteng A, Batsa L, Marfo-Debrekyei Y, Adjei O, Hoerauf A. The role of ultrasonography in the differentiation of the various types of filaricele due to bancroftian filariasis. Acta Trop. 2011;120((Suppl 1)):S23–S32. doi: 10.1016/j.actatropica.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 74.Debrah AY, Mand S, Specht S, Marfo-Debrekyei Y, Batsa L, Pfarr K, Larbi J, Lawson B, Taylor M, Adjei O, Hoerauf A. Doxycycline reduces plasma VEGF-C/sVEGFR-3 and improves pathology in lymphatic filariasis. PLoS Pathog. 2006;2:e92. doi: 10.1371/journal.ppat.0020092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Debrah AY, Mand S, Marfo-Debrekyei Y, Batsa L, Pfarr K, Lawson B, Taylor M, Adjei O, Hoerauf A. Reduction in levels of plasma vascular endothelial growth factor-A and improvement in hydrocele patients by targeting endosymbiotic Wolbachia sp. in Wuchereria bancrofti with doxycycline. Am J Trop Med Hyg. 2009;80:956–963. [PubMed] [Google Scholar]
- 76.Mand S, Debrah AY, Klarmann U, Batsa L, Marfo-Debrekyei Y, Kwarteng A, Specht S, Belda-Domene A, Fimmers R, Taylor M, Adjei O, Hoerauf A. Doxycycline improves filarial lymphedema independent of active filarial infection: a randomized controlled trial. Clin Infect Dis. 2012;55:621–630. doi: 10.1093/cid/cis486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.WHO Surgical Approaches to the Urogenital Manifestations of Lymphatic Filariasis. 2002. http://whqlibdoc.who.int/hq/2002/WHO_CDS_CPE_CEE_2002.33.pdf?ua=1 Available at. Accessed May 17, 2015.
- 78.Guerin PJ, Olliaro P, Sundar S, Boelaert M, Croft SL, Desjeux P, Wasunna MK, Bryceson AD. Visceral leishmaniasis: current status of control, diagnosis, and treatment, and a proposed research and development agenda. Lancet. 2002;2:494–501. doi: 10.1016/s1473-3099(02)00347-x. [DOI] [PubMed] [Google Scholar]
- 79.Mahmoud M. Assessment of visceral leishmaniasis consequences using ultrasound. Open J Radiol. 2014;4:201–206. [Google Scholar]
- 80.Abdalla E, Ayad C, Fadl A, ElGaddal A, Saeed A. Ultrasound findings in patients with visceral leishmaniasis. Int J Med Imaging. 2014;2:5–9. [Google Scholar]
- 81.Melchionda F, Varani S, Carfagnini F, Belotti T, Di Muccio T, Tigani R, Bergamaschi R, Pession A. Spleen nodules: a potential hallmark of visceral leishmaniasis in young children. BMC Infect Dis. 2014;14:620. doi: 10.1186/s12879-014-0620-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bukte Y, Nazaroglu H, Mete A, Yilmaz F. Visceral leishmaniasis with multiple nodular lesions of the liver and spleen: CT and sonographic findings. Abdom Imaging. 2004;29:82–84. doi: 10.1007/s00261-003-0076-0. [DOI] [PubMed] [Google Scholar]
- 83.Grobusch MP, Visser BJ, Boersma J, Huson M, Janssen S, Greve P, Browne JL, Ende-Bouwman J, Ende J, Zwinkels N, Huizenga E, Bree GJ, Stijnis C, Vugt M, Goorhuis A. Ebola virus disease: basics the medical specialist should know. Netherlands J Crit Care. 2015;22:6–14. [Google Scholar]
- 84.Balasubramanian S, Janakiraman L, Kumar SS, Muralinath S, Shivbalan S. A reappraisal of the criteria to diagnose plasma leakage in dengue hemorrhagic fever. Indian Pediatr. 2006;43:334–339. [PubMed] [Google Scholar]
- 85.Michels M, Sumardi U, de Mast Q, Jusuf H, Puspita M, Dewi IM, Sinarta S, Alisjahbana B, van der Ven AJ. The predictive diagnostic value of serial daily bedside ultrasonography for severe dengue in Indonesian adults. PLoS Negl Trop Dis. 2013;7:e2277. doi: 10.1371/journal.pntd.0002277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Srikiatkhachorn A, Krautrachue A, Ratanaprakarn W, Wongtapradit L, Nithipanya N, Kalayanarooj S, Nisalak A, Thomas SJ, Gibbons RV, Mammen MP, Jr, Libraty DH, Ennis FA, Rothman AL, Green S. Natural history of plasma leakage in dengue hemorrhagic fever: a serial ultrasonographic study. Pediatr Infect Dis J. 2007;26:283–290. doi: 10.1097/01.inf.0000258612.26743.10. discussion 291–292. [DOI] [PubMed] [Google Scholar]
- 87.Bharath Kumar Reddy KR, Laksmana RR, Veerappa BG, Shivananda Ultrasonography as a tool in predicting the severity of dengue fever in children–a useful aid in a developing country. Pediatr Radiol. 2013;43:971–977. doi: 10.1007/s00247-013-2642-0. [DOI] [PubMed] [Google Scholar]
- 88.Oliveira R, Rios L, Branco M, Braga Junior L, Nascimento J, Silva G, Bandeira K. Usefulness of ultrasonography in children with suspected dengue hemorrhagic fever: a literature review. Radiol Bras. 2010;43:401–407. [Google Scholar]
- 89.Tufan ZK, Yigit H, Kacar M, Bulut C, Canpolat G, Hatipoglu CA, Kinikli S, Kosar P, Demiroz AP. Sonographic findings in patients with Crimean-Congo hemorrhagic fever. J Ultrasound Med. 2014;33:1999–2003. doi: 10.7863/ultra.33.11.1999. [DOI] [PubMed] [Google Scholar]
- 90.Ziraman I, Celikbas A, Ergonul O, Degirmenci T, Uyanik SA, Koparal S, Dokuzoguz B. Crimean-Congo hemorrhagic fever: aid of abdominal ultrasonography in prediction of severity. Vector Borne Zoonotic Dis. 2014;14:817–820. doi: 10.1089/vbz.2014.1662. [DOI] [PubMed] [Google Scholar]
- 91.Carr BG, Dean AJ, Everett WW, Ku BS, Mark DG, Okusanya O, Horan AD, Gracias VH. Intensivist bedside ultrasound (INBU) for volume assessment in the intensive care unit: a pilot study. J Trauma. 2007;63:495–500. doi: 10.1097/TA.0b013e31812e51e5. discussion 500–502. [DOI] [PubMed] [Google Scholar]
- 92.Lichtenstein D. FALLS-protocol: lung ultrasound in hemodynamic assessment of shock. Heart Lung Vessel. 2013;5:142–147. [PMC free article] [PubMed] [Google Scholar]
- 93.Moreno CC, Kraft CS, Vanairsdale S, Kandiah P, Klopman MA, Ribner BS, Tridandapani S. Performance of bedside diagnostic ultrasound in an Ebola isolation unit: the Emory University Hospital experience. Am J Roentgenol. 2015;204:1157–1159. doi: 10.2214/AJR.15.14344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mekky MA, Tolba M, Abdel-Malek MO, Abbas WA, Zidan M. Human fascioliasis: a re-emerging disease in upper Egypt. Am J Trop Med Hyg. 2015;93:76–79. doi: 10.4269/ajtmh.15-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Teichmann D, Grobusch MP, Gobels K, Muller HP, Koehler W, Suttorp N. Acute fascioliasis with multiple liver abscesses. Scand J Infect Dis. 2000;32:558–560. doi: 10.1080/003655400458884. [DOI] [PubMed] [Google Scholar]
- 96.Shim SS, Kim Y, Lee JK, Lee JH, Song DE. Pleuropulmonary and abdominal paragonimiasis: CT and ultrasound findings. Br J Radiol. 2012;85:403–410. doi: 10.1259/bjr/30366021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Jeon HK, Lee D, Park H, Min DY, Rim HJ, Zhang H, Yang Y, Li X, Eom KS. Human infections with liver and minute intestinal flukes in Guangxi, China: analysis by DNA sequencing, ultrasonography, and immunoaffinity chromatography. Korean J Parasitol. 2012;50:391–394. doi: 10.3347/kjp.2012.50.4.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mand S, Marfo-Debrekyei Y, Debrah A, Buettner M, Batsa L, Pfarr K, Adjei O, Hoerauf A. Frequent detection of worm movements in onchocercal nodules by ultrasonography. Filaria J. 2005;4:1. doi: 10.1186/1475-2883-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Darge K, Troeger J, Engelke C, Leichsenring M, Nelle M, Awadzi K, Buettner DW. Evaluation of ultrasonography for the detection of drug-induced changes in onchocercal nodules. Am J Trop Med Hyg. 1994;51:800–808. doi: 10.4269/ajtmh.1994.51.800. [DOI] [PubMed] [Google Scholar]
- 100.Poltera AA, Reyna O, Zea-Flores G, Beltranena F, Nowell de Arevalo A, Zak F. Use of an ophthalmologic ultrasoundscanner in human onchocercal skin nodules for non-invasive sequential assessment during a macrofilaricidal trial with amocarzine in Guatemala. The first experiences. Trop Med Parasitol. 1991;42:303–307. [PubMed] [Google Scholar]
- 101.Mazur-Melewska K, Jonczyk K, Modlinska-Cwalinska A, Figlerowicz M, Sluzewski W. Visceral larva migrans syndrome: analysis of serum cytokine levels in children with hepatic lesions confirmed in radiological findings. Parasite Immunol. 2014;36:668–673. doi: 10.1111/pim.12143. [DOI] [PubMed] [Google Scholar]
- 102.Brennan RC, Wilson MW, Kaste S, Helton KJ, McCarville MB. US and MRI of pediatric ocular masses with histopathological correlation. Pediatr Radiol. 2012;42:738–749. doi: 10.1007/s00247-012-2374-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Umetsu S, Sogo T, Iwasawa K, Kondo T, Tsunoda T, Oikawa-Kawamoto M, Komatsu H, Inui A, Fujisawa T. Intestinal ascariasis at pediatric emergency room in a developed country. World J Gastroenterol. 2012;20:14058–14062. doi: 10.3748/wjg.v20.i38.14058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Majid Z, Masood I, Pirzada MT. Ascaris lumbricoides and its invasion of the accessory cystic duct: an unusual presentation. Trop Doct. 2015;45:129–131. doi: 10.1177/0049475514556571. [DOI] [PubMed] [Google Scholar]
- 105.Wu S. Sonographic findings of Ascaris lumbricoides in the gastrointestinal and biliary tracts. Ultrasound Q. 2009;25:207–209. doi: 10.1097/RUQ.0b013e3181c47a2d. [DOI] [PubMed] [Google Scholar]
- 106.Pereira Junior Cde B, Markman Filho B. Clinical and echocardiographic predictors of mortality in chagasic cardiomyopathy—systematic review. Arq Bras Cardiol. 2014;102:602–610. doi: 10.5935/abc.20140068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Quintanilla-Cedillo MR, Leon-Urena H, Contreras-Ruiz J, Arenas R. The value of Doppler ultrasound in diagnosis in 25 cases of furunculoid myiasis. Int J Dermatol. 2005;44:34–37. doi: 10.1111/j.1365-4632.2004.02471.x. [DOI] [PubMed] [Google Scholar]
- 108.Zha Y, Zhou M, Hari A, Jacobsen B, Mitragotri N, Rivas B, Ventura OG, Boughton J, Fox JC. Ultrasound diagnosis of malaria: examination of the spleen, liver, and optic nerve sheath diameter. World J Emerg Med. 2015;6:10–15. doi: 10.5847/wjem.j.1920-8642.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Henriquez-Camacho C, Garcia-Casasola G, Guillen-Astete C, Losa J. Ultrasound for the diagnosis of infectious diseases: approach to the patient at point of care and at secondary level. J Infect. 2015;71:1–8. doi: 10.1016/j.jinf.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 110.Polat Ekinci A, Karabacak E, Tekin L, Ozarmagan G, Ozcakar L. Ultrasound imaging for the follow-up of patients with leprosy: a pictorial essay. Br J Dermatol. 2015;172:265–267. doi: 10.1111/bjd.13421. [DOI] [PubMed] [Google Scholar]
- 111.Frade MA, Nogueira-Barbosa MH, Lugao HB, Furini RB, Marques Junior W, Foss NT. New sonographic measures of peripheral nerves: a tool for the diagnosis of peripheral nerve involvement in leprosy. Mem Inst Oswaldo Cruz. 2013;108 doi: 10.1590/S0074-02762013000300001. pii: S0074-02762013000300257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mirabel M, Bacquelin R, Tafflet M, Robillard C, Huon B, Corsenac P, de Fremicourt I, Narayanan K, Meunier JM, Noel B, Hagege AA, Rouchon B, Jouven X, Marijon E. Screening for rheumatic heart disease: evaluation of a focused cardiac ultrasound approach. Circulation. 2015;8 doi: 10.1161/CIRCIMAGING.114.002324. pii: e002324. [DOI] [PubMed] [Google Scholar]
- 113.Heuvelings CC, Belard S, Janssen S, Wallrauch C, Grobusch MP, Brunetti E, Giordani MT, Heller T. Chest ultrasonography in patients with HIV: a case series and review of the literature. Infection. 2015 doi: 10.1007/s15010-015-0780-z. doi:10.1007/s15010-015-0780-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nabeta HW, Bahr NC, Rhein J, Fossland N, Kiragga AN, Meya DB, Dunlop SJ, Boulware DR. Accuracy of noninvasive intraocular pressure or optic nerve sheath diameter measurements for predicting elevated intracranial pressure in cryptococcal meningitis. Open Forum Infect Dis. 2014;1:ofu093. doi: 10.1093/ofid/ofu093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.WHO Training in diagnostic ultrasound: essentials, principles and standards. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1998;875:i–46. back cover. [PubMed] [Google Scholar]
- 116.Torres-Macho J, Anton-Santos JM, Garcia-Gutierrez I, de Castro-Garcia M, Gamez-Diez S, de la Torre PG, Latorre-Barcenilla G, Majo-Carbajo Y, Reparaz-Gonzalez JC, de Casasola GG. Initial accuracy of bedside ultrasound performed by emergency physicians for multiple indications after a short training period. Am J Emerg Med. 2012;30:1943–1949. doi: 10.1016/j.ajem.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 117.Short Course on Ultrasound in Infectious Diseases and Tropical Medicine. www.tropicalultrasound.org Available at. Accessed May 17, 2015.
- 118.Clinical Ultrasound in Tropical Infectious Diseases. http://www.tropicalultrasound.org/docs/Lima_Ultrasound_2015_Registration.pdf Available at. Accessed May 17, 2015.
- 119.New Course: Introduction to Ultrasound in Low Resource Settings. http://www.lstmliverpool.ac.uk/about-lstm/news-and-media/latest-news/2013/jan-june/new-course-cl03/ Available at. Accessed May 15, 2015.
- 120.Adler D, Mgalula K, Price D, Taylor O. Introduction of a portable ultrasound unit into the health services of the Lugufu refugee camp, Kigoma District, Tanzania. Int J Emerg Med. 2008;1:261–266. doi: 10.1007/s12245-008-0074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Beira in Mozambique Emergency Care Teaching Visit November 2012. http://www.emergencyultrasound.org.uk/20.html Available at. Accessed May 2, 2015.
- 122.FASH Ultrasound Course. Krole Bu Teaching Hospital; Accra, Ghana: 2012. http://www.tropicalultrasound.org/FASH/FASH_report.pdf 24 May. Available at. [Google Scholar]
- 123.Jang TB, Ruggeri W, Dyne P, Kaji AH. Learning curve of emergency physicians using emergency bedside sonography for symptomatic first-trimester pregnancy. J Ultrasound Med. 2010;29:1423–1428. doi: 10.7863/jum.2010.29.10.1423. [DOI] [PubMed] [Google Scholar]
- 124.Jang TB, Casey RJ, Dyne P, Kaji A. The learning curve of resident physicians using emergency ultrasonography for obstructive uropathy. Acad Emerg Med. 2010;17:1024–1027. doi: 10.1111/j.1553-2712.2010.00850.x. [DOI] [PubMed] [Google Scholar]
- 125.Tolsgaard MG, Todsen T, Sorensen JL, Ringsted C, Lorentzen T, Ottesen B, Tabor A. International multispecialty consensus on how to evaluate ultrasound competence: a Delphi consensus survey. PLoS One. 2013;8:e57687. doi: 10.1371/journal.pone.0057687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.WHO WHO Manual of Diagnostic Ultrasound. 2011. http://whqlibdoc.who.int/publications/2011/9789241547451_eng.pdf Available at. Accessed May 15, 2015.
- 127.Heller T. Focus Assessment with Sonography for HIV/TB: A Practical Manual. 2013. http://www.talcuk.org/books/focused-assessment-with-sonography-for-hivtb.htm Available at. Accessed May 15, 2015. [Google Scholar]
- 128.Partners in Health Manual of Ultrasound for Resource-Limited Settings. 2011. http://www.pih.org/library/manual-of-ultrasound-for-resource-limited-settings Available at. Accessed May 15, 2015.
- 129.American College of Emergency Physicians Emergency Ultrasound Guidelines. 2008. http://www.acep.org/workarea/DownloadAsset.aspx?id=32878 Available at. Accessed May 15, 2015.
- 130.International Federation for Emergency Medicine Point-of-Care Ultrasound Curriculum Guidelines. 2014. http://www.ifem.cc/site/DefaultSite/filesystem/documents/Policies%20and%20Guidelines/IFEM%20Point-of-Care%20Ultrasound%20Curriculum%20Guidelines%202014.pdf Available at. Accessed May 15, 2015. [DOI] [PubMed]