Abstract
The reservoir of Mycobacterium ulcerans causing Buruli ulcer (BU) remains unknown. Here, sterilized watery soil was mixed with 2 × 106 colony-forming units (CFU)/g of M. ulcerans Agy99 or M. ulcerans ATCC 33728 and incubated in a microaerophilic atmosphere in the presence of negative controls. Both M. ulcerans strains survived in soil for 4 months with a final inoculum of 300–440 CFU/g. Further, three groups of five mice with and without footpad scarification were exposed to control soil or M. ulcerans-inoculated soil. Although no specific clinical and histopathological lesions were observed in control animals, red spots observed on 8/20 scarified feet in 8/10 challenged mice yielded inflammatory infiltrates and positive real-time polymerase chain reaction detection of M. ulcerans DNA in five mice. BU can be acquired as an inoculation infection with watery soil as a transient source of infection. These experimental observations warrant additional field observations.
The source of Mycobacterium ulcerans responsible for Buruli ulcer (BU) remains unknown.1 Epidemiological studies conducted in West Africa traced to stagnant freshwater points.2 Several studies have reported the detection of M. ulcerans DNA in stagnant freshwater3,4 and aquatic environments.5,6 Moreover, the only environmental M. ulcerans isolate was recovered from a water strider in Benin.7 These observations suggest a link between BU and stagnant and slow-flowing aquatic environments in West Africa. However, freshwater itself may not be the ultimate source of M. ulcerans. In particular, fishermen who are presumably in frequent contact with water have a lower prevalence of BU than other groups in endemic regions in Africa.8,9 In addition, the M. ulcerans inoculum has been estimated to be 100–1,000 mycobacteria/mL in water, based on real-time polymerase chain reaction (RT-PCR) targeting IS2404.3 This estimated inoculum level is three to four times lower than the levels reported for major waterborne human pathogens such as Vibrio.10
We have recently shown that Mycobacterium tuberculosis, a Mycobacterium that is phylogenetically closely related to M. ulcerans, retains its infectivity after an extended stay in soil.11 We therefore hypothesized that watery soil could be a source of M. ulcerans.
To test the hypothesis, M. ulcerans ATCC 19423TMT (strain Agy99) and M. ulcerans ATCC 33728 (both obtained from the American Type Culture Collection, Masassas, VA) were cultured in an incubator at 32°C on Middlebrook 7H10 Agar (Becton Dickinson, Le Pont de Claix, France), supplemented with OADC (oleic acid, bovine albumin, dextrose, and catalase) (Becton Dickinson). Natural soil was steam sterilized at 134°C for 15 minutes, and the sterility was then assessed by inoculating 2 g of steam-sterilized soil onto Middlebrook 7H10 Agar incubated at 32°C for 4 weeks. A 20-g sample of sterilized soil was inoculated and mixed with 2 × 106 colony-forming units (CFU)/g of each of the two M. ulcerans isolates, placed into 25-cm2 cell culture flasks (Corning, Corning, NY) and thoroughly mixed. Three flasks were prepared for each M. ulcerans strain. The flasks were placed inside a transparent sterile plastic container where they were exposed to a microaerophilic atmosphere created using a CampyGen atmosphere generation system (Oxoid Ltd., Basingstoke, United Kingdom). Two negative control flasks were used; one containing non-inoculated and sterilized soil and one containing a probe to monitor temperature and humidity. The soil temperature ranged from 18°C to 25°C and its humidity ranged from 47% to 69% during this 4-month experiment. One hour, 1 week, 2 weeks, and every month after the soil infections, a 250-mg aliquot of soil was sampled using a sterile loop and mixed in an Eppendorf tube with 500 μL of sterile phosphate-buffered saline. A 10-fold serial dilution was performed from 100 to 105, and 100 μL of each dilution was inoculated onto Middlebrook 7H10 medium and incubated at 32°C. The colonies were observed via autofluorescence,12 and autofluorescent colonies were counted, 10 days after inoculation onto Middlebrook plates, using the Leica Application Suite Software (Leica, Nanterre, France). The colonies were identified as M. ulcerans after Ziehl–Neelsen staining and RT-PCR targeting of the IS2404 and IS260613 insertion sequences and a sequence encoding the ketoreductase B domain,14 as previously reported.15
A previously reported M. ulcerans mouse model was used with modifications.16 The animal model protocol no. 02552.02 was reviewed and approved by the “Comité d*Ethique de Marseille C2EA-14” and “Comité National de Reflexion éthique sur l*expérimentation animale” on November 17, 2014. Fifteen 3-month-old BALB/c female mice, weighing 17–20 g (Charles River, L*Arbresle, France) were housed and acclimated in our laboratory animal facility for a week before exposure to contaminated soil. Each mouse was anesthetized for 1 hour by intraperitoneal injection of ketamine (120 mg/kg) and xylazine (8 mg/kg). The left foreleg and the right hind footpads were scarified with a sterile razor. The mice were randomly allocated to one of three groups. The challenge group A mice (N = 5) were placed in a box containing M. ulcerans Agy99-contaminated soil, the challenge group B mice (N = 5) were placed in a box containing M. ulcerans strain ATCC 33728-contaminated soil, and the control group mice (group C, N = 5) were placed in a box containing non-inoculated soil. The boxes were placed in a ventilated cabinet, and the mice were fed and observed daily. The mice were observed for the appearance of peeling, whole body redness, footpad alterations, displacement, and feeding. The mice from each group were euthanized 30 days after challenge and biopsies were taken of the scarified and inoculated footpads. Each footpad was processed individually. Total DNA was extracted from biopsies using a tissue DNA Extraction Kit (Macherey-Nagel, Düren, Germany) according to the manufacturer and was incorporated in M. ulcerans RT-PCRs as described above. The biopsies were cultured on Middlebrook 7H10 Agar as described above. Histological testing was performed on biopsies fixed with 4% buffered formalin and embedded in paraffin. Serial sections (3 μm) of these specimens were obtained for routine hematoxylin–eosin–saffron and special stains, including Giemsa, periodic acid Schiff, Grocott–Gomori methenamine silver, and Ziehl–Neelsen stains.
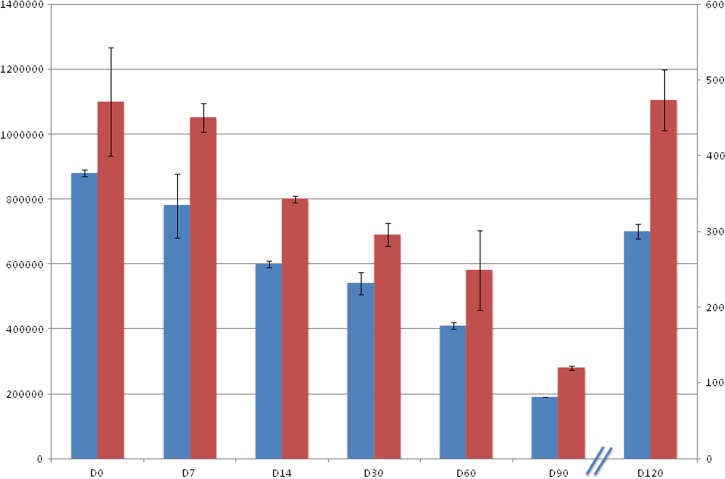
Whereas the negative controls remained sterile, the soil seeded with M. ulcerans reproducibly grew M. ulcerans at every checkpoint for each of the two tested M. ulcerans strains. Concerning the M. ulcerans Agy99 strain, the inoculum decreased from 8.8 × 105 CFU/g at day 0 to 300 CFU/g at month 4 (Figure 1 ). As for the M. ulcerans ATCC 33728 strain, the inoculum decreased from 11 × 105 CFU/g at day 0 to 450 CFU/g at month 4 (Figure 1).
Figure 1.
Histogram of changes in Mycobacterium ulcerans inoculum in soil. Blue boxes, M. ulcerans Agy99; red boxes, M. ulcerans ATCC 33728; x axis, time (days), note that x axis was broken after D90 to change the y axis scale; left-hand y axis and right-hand y axis, M. ulcerans inoculum (colony-forming units).
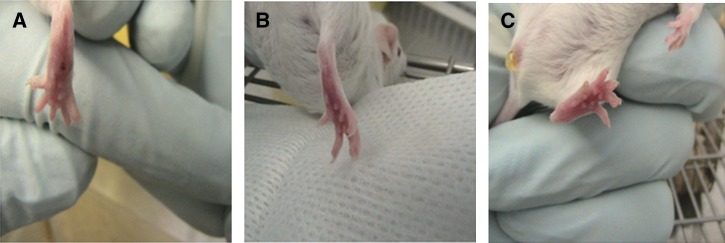
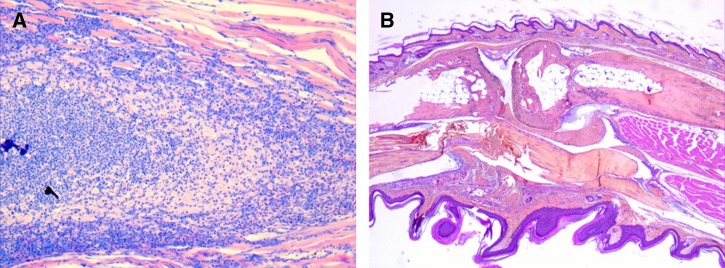
The animal study yielded no deaths in any of the three mouse groups, and all animals ate regularly and exhibited normal behavior. As for macroscopic examinations, all of the animals had normal coats and no injuries were observed on the non-scarified legs in either group (Table 1). In the M. ulcerans Agy99 strain–inoculated group, red spots were observed on 5/10 scarified feet in 5/5 mice. In the M. ulcerans ATCC 33728 strain–inoculated group, we observed red spots on 3/10 scarified feet in 3/5 mice; one foot exhibited an increased size and was edematous. In both groups, the lesions were observed on the hind scarified feet only. In the control group (group C), we did not observe any specific lesions on the scarified feet (lesion 0/10 legs; 0/5 mice) (Figure 2 ). RT-PCRs were positive in two M. ulcerans Agy99–inoculated and one M. ulcerans ATCC 33728–inoculated mice whereas negative controls remained negative. Cultures from skin lesion biopsies, however, remained negative. A blind histopathology examination found no specific lesions in the 10 hind feet collected in group C mice (control group), whereas inflammatory infiltrates, composed mainly of neutrophils and foamy macrophages, were observed in the footpads in 5/5 observed hind feet of group A mice (M. ulcerans Agy99) and in 3/5 group B mice (M. ulcerans ATCC 33728) (Figure 3 ). No granulomas were observed and no microorganisms were detected when using the special stains.
Table 1.
Summary of experimental procedures and final results
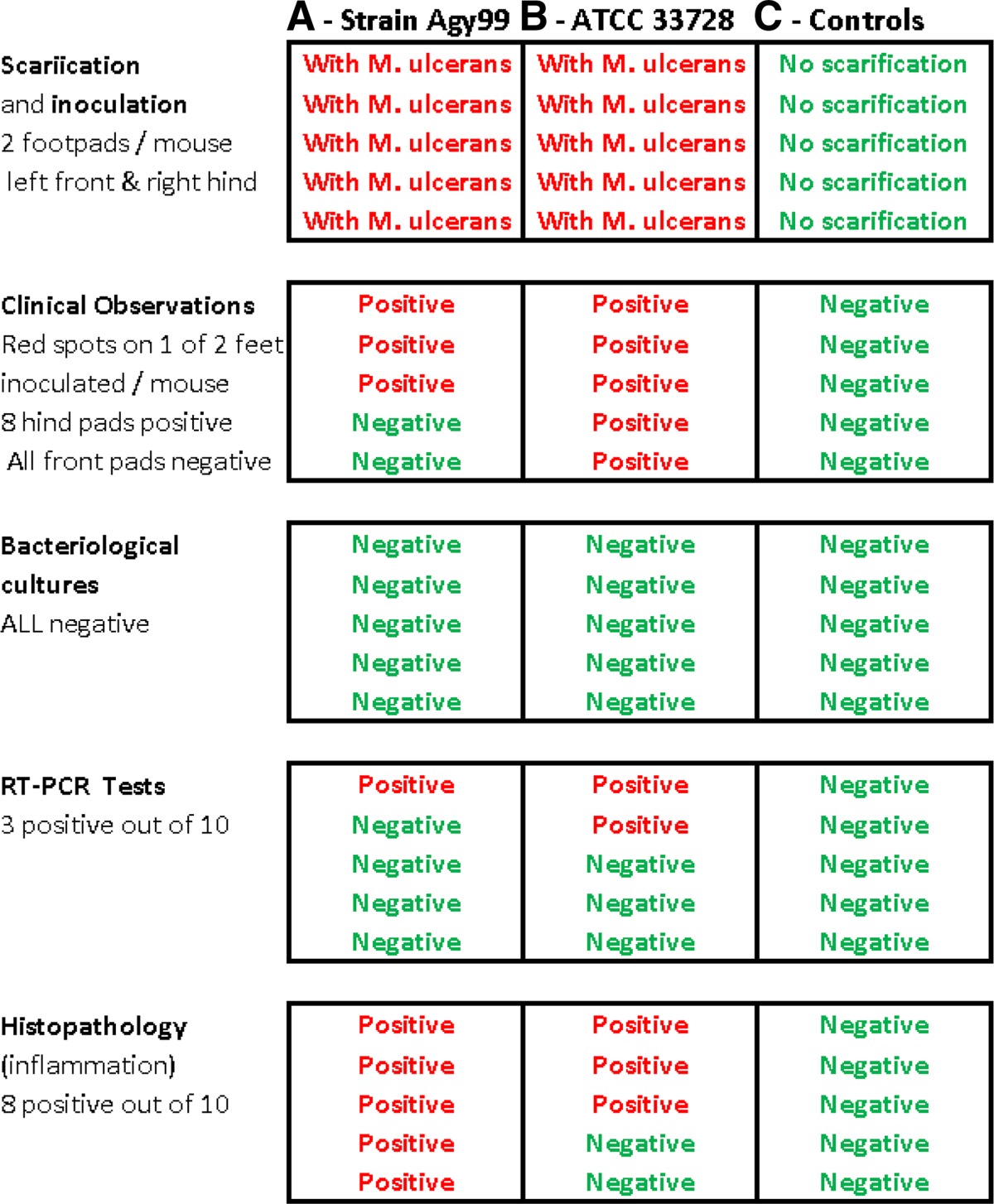
RT-PCR = real-time polymerase chain reaction.
Figure 2.
Clinical appearance of hind footpads in (A) scarified group A mice exposed to Mycobacterium ulcerans Agy99 illustrating skin lesions, (B) scarified group B mice exposed to M. ulcerans ATCC 33728, and (C) non-scarified control group C with no lesions.
Figure 3.
Histological observation of mouse footpads from (A) group A (exposed to Mycobacterium ulcerans Agy99-inoculated soil) mice and (B) group C mice (negative control). In the group A mice, but not in the group C mice, we observed an abundance of inflammatory infiltrate composed of neutrophils and foamy macrophages (Giemsa stain, original magnification ×100).
The proximity of BU patients to wetlands is an acknowledged risk factor for BU.17 Here, we showed that M. ulcerans can survive in watery soil for at least 4 months. Because the experimental conditions reported here clearly did not take into account the soil complexity in natural settings, the choice of humidity, temperature, and the use of a natural soil aimed to mimic natural conditions in Africa. Indeed, the inoculum we used is in the range of what has been reported in the field.3 Later, field investigation in Benin detected M. ulcerans DNA in 12/46 (26.1%) soil samples at higher inoculum levels than those measured in the water in the same area.3 Furthermore, M. ulcerans DNA has been detected in groundwater sources.3 Under these conditions, we observed a rapid drop in inoculum, indicating that the soil itself is most likely not a reservoir for M. ulcerans. However, these data suggest that watery soil could be a transient infection source.
We tested this hypothesis in an animal model.16 Mycobacterium ulcerans was not cultured from the lesions but its DNA was reliably detected in three of 10 inoculated footpads by RT-PCR.
The histopathology, marked by macrophagic inflammation, was similar to that described in BU patients. These data indicate that indeed animals acquired experimental BU after scarification and contacts with M. ulcerans-contaminated soil.
Mycobacterium ulcerans is an actinomycete organism, and numerous other actinomycetes, such as Nocardia spp.,18 are known to be responsible for inoculation infection from a soil source; however, even the closely related M. tuberculosis is seldom responsible for tuberculosis inoculations in feet.19
In conclusion, our observations, combined with previous reports,16 suggest that soil contaminated with M. ulcerans could serve as a transient infectious source for BU. The observations reported here might prompt field observers to assess whether the soil in regions affected by BU is naturally contaminated.
Footnotes
Authors* addresses: Roger D. B. Tian, Hubert Lepidi, Claude Nappez, and Michel Drancourt, Unité de Recherche sur les Maladies Infectieuses et Tropicales Émergentes (UMR/CNRS 7278/IRD 198/INSERM 1095), Faculté de Médecine, Méditerrannée Infection, Marseille, France, E-mails: tianroger@yahoo.fr, hubert.lepidi@univ-amu.fr, claude.nappez@univ-amu.fr, and michel.drancourt@univ-amu.fr.
References
- 1.WHO . Global Buruli Ulcer Initiative. Geneva, Switzerland: World Health Organization; 2000. Buruli Ulcer: Mycobacterium ulcerans Infection; p. 118. [Google Scholar]
- 2.Garchitorena A, Roche B, Kamgang R, Ossomba J, Babonneau J, Landier J, Fontanet A, Eyangoh S, Guéguan JF, Marsollier L. Mycobacterium ulcerans ecological dynamics and its association with freshwater ecosystems and aquatic communities: results from a 12-month environmental survey in Cameroon. PLoS Negl Trop Dis. 2014;8:e2879. doi: 10.1371/journal.pntd.0002879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williamson HR, Benbow ME, Campell LP, Johnson CR, Sopoh G, Baroqui Y, Merrit RW, Small PL. Detection of Mycobacterium ulcerans in the environment predicts prevalence of Buruli ulcer in Benin. PLoS Negl Trop Dis. 2012;6:e1506. doi: 10.1371/journal.pntd.0001506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson HR, Benbow ME, Nguyen KD, Beachboard DC, Kimbirauskas RK, McIntosh MD, Quaye C, Ampadu EO, Boakye D, Merritt RW, Small PL. Distribution of Mycobacterium ulcerans in Buruli ulcer in endemic and non-endemic aquatic sites in Ghana. PLoS Negl Trop Dis. 2008;2:e205. doi: 10.1371/journal.pntd.0000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marion E, Eyangoh S, Yeramian E, Doannio J, Landier J, Aubry J, Fontanet A, Rogier C, Cassia V, Cottin J, Marot A, Eveillard M, Kamdem Y, Legras P, Deshayes C, Saint Andre JP, Marsollier L. Seasonal and regional dynamics of M. ulcerans transmission in environmental context: deciphering the role of water bugs as hosts and vectors. PLoS Negl Trop Dis. 2010;4:e731. doi: 10.1371/journal.pntd.0000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marsollier L, Severin T, Aubry J, Merrit RW, Saint Andre JP, Legras P, Manceau AL, Chauty A, Carbonnelle B. Aquatic snails, passive hosts of Mycobacterium ulcerans. Appl Environ Microbiol. 2004;70:6296–6298. doi: 10.1128/AEM.70.10.6296-6298.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Portaels F, Meyers WM, Ablordey A, Castro AG, Chemlal K, de Rijk P, Elsen P, Fissette K, Fraga AG, Lee R, Mahrous E, Small PL, Stragier P, Torrado E, Van Aerde A, Silva MT, Pedrosa J. First cultivation and characterization of Mycobacterium ulcerans from the environment. PLoS Negl Trop Dis. 2008;2:e178. doi: 10.1371/journal.pntd.0000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raghunathan PL, Whitney EA, Asamoa K, Stienstra Y, Taylor TH, Jr, Amofah GK, Ofori-Adjei D, Dobos K, Guarner J, Martin S, Pathak S, Klutse E, Etuaful S, van der Graaf WT, van der Werf TS, King CH, Tappero JW, Ashford DA. Risk factors for Buruli ulcer disease (Mycobacterium ulcerans infection): results from a case-control study in Ghana. Clin Infect Dis. 2005;40:1445–1453. doi: 10.1086/429623. [DOI] [PubMed] [Google Scholar]
- 9.Pouillot R, Matias G, Wondje CM, Portaels F, Valin N, Ngos F, Njikap A, Marsollier L, Fontanet A, Eyangoh S. Risk factors for Buruli ulcer: a case control study in Cameroon. PLoS Negl Trop Dis. 2007;1:e101. doi: 10.1371/journal.pntd.0000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asplund ME, Rehnstam-Holm AS, Atnur V, Raghunath P, Saravanan V, Härnström K, Collin B, Karunasagar I, Godhe A. Water column dynamics of Vibrio in relation to phytoplankton community composition and environmental conditions in a tropical costal area. Environ Microbiol. 2011;13:2738–2751. doi: 10.1111/j.1462-2920.2011.02545.x. [DOI] [PubMed] [Google Scholar]
- 11.Ghodbane R, Mba Medie F, Lepidi H, Nappez C, Drancourt M. Long-term survival tuberculosis complex mycobacteria in soil. Microbiology. 2014;160:496–501. doi: 10.1099/mic.0.073379-0. [DOI] [PubMed] [Google Scholar]
- 12.Mougin B, Tian RBD, Drancourt M. Tropical plant extracts modulating the growth of Mycobacterium ulcerans. PLoS One. 2015;10:e0124626. doi: 10.1371/journal.pone.0124626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stinear T, Davies JK, Jenkin GA, Hayman JA, Oppedisamo F, Johnson PD. Identification of Mycobacterium ulcerans in the environment from regions in the southeast Australia in which it is endemic with sequence capture-PCR. Appl Environ Microbiol. 2000;66:3206–3213. doi: 10.1128/aem.66.8.3206-3213.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stinear TP, Mve-Obiang A, Small PL, Frigui W, Pryor MJ, Brosch R, Jenkin GA, Johnson PD, Davies JK, Lee RE, Adusumilli S, Garnier T, Haydock SF, Leadlay PF, Cole ST. Giant plasmid-encoded polyketide synthases produce the macrolide toxin of Mycobacterium ulcerans. Proc Natl Acad Sci USA. 2004;101:1345–1349. doi: 10.1073/pnas.0305877101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fyfe JAM, Lavender CJ, Johnson PDR, Globan M, Sievers A, Azuolas J, Stinear TP. Development and application of two multiplex real-time PCR assays for the detection of Mycobacterium ulcerans in clinical and environmental samples. Appl Environ Microbiol. 2007;73:4733–4740. doi: 10.1128/AEM.02971-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dega H, Bentoucha A, Robert J, Jarlier V, Grosset J. Bactericidal activity of rifampin-amikacin against Mycobacterium ulcerans in mice. Antimicrob Agents Chemother. 2002;46:3193–3196. doi: 10.1128/AAC.46.10.3193-3196.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fyfe JAM, Lavender CJ, Handasyde KA, Legione AR, O*Brien CR, Stinear TP, Pidot SJ, Seemann T, Benbow ME, Wallace JR, McCowan C, Johnson PD. A major role for mammals in the ecology of Mycobacterium ulcerans. PLoS Negl Trop Dis. 2010;4:e791. doi: 10.1371/journal.pntd.0000791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown Elliott BA, Brown JM, Conville PS, Wallace RJ., Jr Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006;19:259–282. doi: 10.1128/CMR.19.2.259-282.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hakimi M, Hashemi F, Mirzaie AZ, Pour AH, Kosari H. Tuberculous osteomyelitis of the long bones and joints. Indian J Pediatr. 2008;75:505–508. doi: 10.1007/s12098-008-0078-6. [DOI] [PubMed] [Google Scholar]