Abstract
Many of the drugs used for chemotherapy treatments are known to be ototoxic, and can result in permanent hearing threshold shifts. The degree of ototoxic damage can be influenced by many factors including dosage, duration of exposure, genetics, and coadministration with other ototoxic agents. Cisplatin is known for its ototoxic effects on hearing thresholds, particularly in the high frequencies. Recent studies have indicated a synergistic relationship between Cisplatin administration and moderate to high noise level exposure starting between 70–85 dB SPL. This study measured the noise levels in the Portland Veteran’s Affairs Medical Center’s outpatient chemotherapy clinic. Average (LAeq) and peak (LCpeak) noise measures were recorded every minute from 7 am until 6 pm on the two busiest clinic days. Patients, visitors, and staff members filled out anonymous surveys regarding their reactions to noise levels. Cumulative noise levels were not at levels known to interact with Cisplatin for a significant period of time. Noise measurement analysis indicated that levels were at or above 70 dB SPL for less than ten minutes during the 11-hour recording window. The patient and visitor surveys indicated that both groups were unbothered by noise in the clinic. However, most staff members were bothered by or concerned about noise levels, and many felt that it caused stress and difficulty communicating on the phone.
Keywords: Chemotherapy, cisplatin, noise disturbance, noise
Introduction
There are many ototoxic agents in our environment. Solvents,[1] metals (e.g., lead), chemotherapeutic drugs, aminoglycosides, and high levels of noise can all cause hearing loss.[1] Ototoxic agents are responsible for a range of damage within the inner ear affecting both the Organ of Corti and the vestibular system.[2]
Chemotherapeutic agents, particularly Cisplatin, are known to cause permanent damage to the outer and inner hair cells.[3,4] Cisplatin, a heavy-metal antineoplastic agent,[4] is commonly used to treat many cancers including testicular cancer, head and neck cancer, lung cancer,[5] and bladder cancer. [4] The ototoxic effects of Cisplatin are strongly correlated with the dosage[5] and duration of exposure.[3] Other factors that have been shown to influence Cisplatin ototoxicity include the mode of drug administration, the tumor site, age, renal function, genetic predisposition, cumulative dose, and interaction with other ototraumatic agents.[3] The resultant damage to the cochlea leads to a bilateral, usually symmetrical, sensorineural hearing loss which first affects the high frequencies.[4]
Another commonly encountered ototoxic agent is noise. A single short-duration exposure to a very high level of noise or longer-term exposure to lower levels of noise can damage hair cells and structures of the cochlea.[4] When noise damage occurs, it begins at the base of the cochlea and then ascends to the apex, affecting first the outer hair cells.[6] The Occupational Safety and Health Administration (OSHA) has stipulated that all employees must wear hearing protection if they are exposed to an eight-hour time-weighted average of 90 dB SPL or more per workday.[7] A combination of impulse and continuous noise results in more cochlear damage than continuous exposure to noise.[4]
Although self-reported noise annoyance is largely dependent on individual sensitivity,[8] many studies have found relationships between noise exposure and adverse psychological and physiological effects.[9] Some of these effects include difficulty concentrating on work,[10] increased heart rate and blood pressure,[11] fatigue,[12] decreased motivation, elevated epinephrine levels (increasing the risk for heart disease),[13] annoyance,[14] long- and short-term sickness with absence from work,[15] and decreased high-information processing abilities.[13] Moderate-to-high levels of noise have been shown to negatively affect safety in hospitals, and diminish quality of care given to patients by hospital staff.[10] Similarly, Topf and Dillon found that noise-sensitive critical care nurses had a higher burn-out rate than nurses who were not as sensitive to noise.[16] In terms of patients, even moderate noise levels above 50 dB SPL can lengthen the hospital stay and patient healing time.[17]
When two ototoxic agents are combined, a synergistic effect can result, leading to increased damage to the hearing organ. Research in chinchillas has shown that a synergistic relationship between Cisplatin and noise occurs when noise levels reach 70–85 dB SPL. That is, the combination of a standard Cisplatin treatment dose and noise levels between 70 and 85 dB SPL resulted in significantly more hearing and hair cell loss in the high frequencies[3] than the added independent effects. This finding is particularly important because noise is not usually considered to be damaging to the ear until it reaches levels of 85 dB or more. This synergistic effect, however, appeared to be dependent on the order of exposure. Specifically, the increased hair cell damage was observed when noise was present at the time of Cisplatin administration,[3,4] and when noise preceded Cisplatin administration by between 30 minutes and three days, but there was no interaction when noise exposure followed Cisplatin by two or three days.[18]
The data of Gratton et al.[3] suggest that patients undergoing chemotherapy with Cisplatin in a moderately noisy clinic (sustained levels of 70 dB SPL or more) may be at greater risk for damage to their auditory systems than if receiving Cisplatin in a quieter clinic. It may thus be important to monitor and reduce noise levels in moderately noisy chemotherapy clinics.
In the outpatient chemotherapy clinic of the Portland Veterans Affairs Medical Center, many of the staff members have reported that the clinic is very noisy, particularly on the busier days of the week on which the majority of outpatient appointments are scheduled. These reports, in combination with the data of Gratton et al.,[3] led to the present study in which the primary purpose was to determine if noise levels in the Portland VA Medical Center outpatient chemotherapy clinic were high enough to increase the patients’ risks of hearing impairment due to the synergistic interaction of Cisplatin and noise. The study’s secondary purpose was to determine if noise levels were disturbing to patients, visitors, and staff. To achieve these goals, sound levels and sources of noise were measured during clinic hours and questionnaires were administered to assess subjective responses of patients, visitors, and staff members to clinic noise.
Methods
This study was approved by the Portland Veterans’ Affairs Research and Development Department and was given exemption by the Institutional Review Board.
Chemotherapy outpatient unit
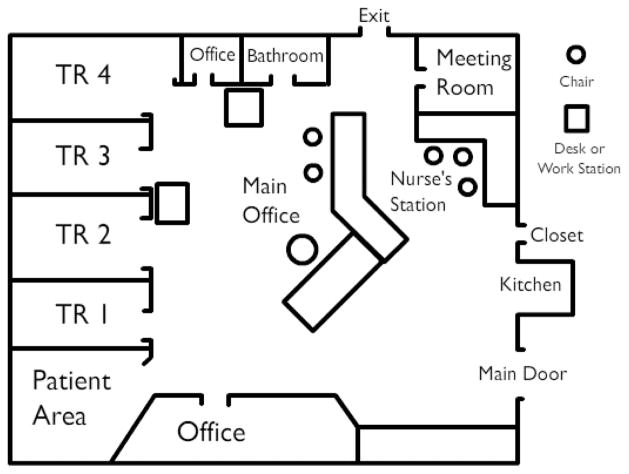
The outpatient chemotherapy unit consists of four treatment rooms and an outpatient area. Within each treatment room, there are four reclining chairs for patients, additional chairs for visitors, monitors, and equipment for chemotherapy administration. One of the four walls is primarily made up of a window to the outside, while another is a sliding glass door that leads to the main office. Between two and four patients are treated in each room at one time. Patients are often accompanied by a visitor for part or all, of their treatment visit. The doors to each treatment room remain open all day long, and rooms are located within a couple of feet from the main office area. Figure 1 shows a diagram of the unit.
Figure 1.
Diagram of the outpatient chemotherapy clinic
Materials
Noise measurement
Noise levels were recorded with a sound level meter (SLM; Bruel and Kjaer 2250). The sound level meter was calibrated daily using an acoustic sound calibrator (Bruel and Kjaer 4231). The microphone was a pre-polarized Free-field ½ inch 4189. The microphone was covered with a windscreen during all measurements. Using a microphone extension cable, the microphone was hung approximately one foot from the ceiling in the middle of each recording room. The microphone was centered in the room at an equal distance from all of the patients.
Survey
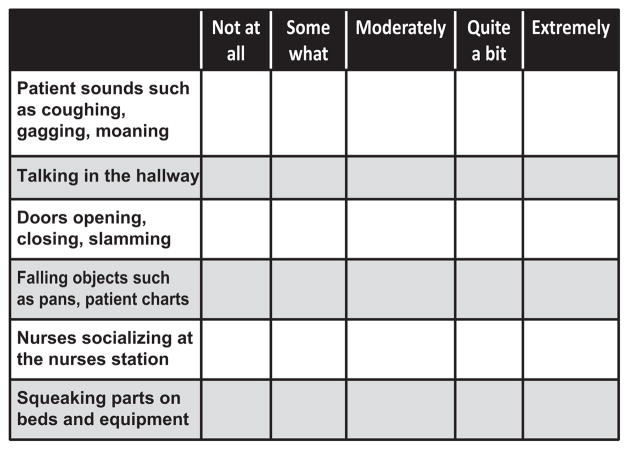
The Adapted Topf Sound Disturbance Survey[8] was used to assess how much the noise in the unit disturbed patients, visitors, and staff members [Appendix A]. The survey consists of 20 items. Each question has patients rate their level of disturbance from specified common hospital noises as “not at all,” “somewhat,” “moderately,” “quite a bit,” or “extremely disturbed.” Staff members were asked additional questions to determine when they felt the clinic was noisiest, how they thought the noise levels affected their job performance, and what they had done to reduce noise levels. Figure 2 shows some example questions as they appear on the Topf Sound Disturbance Survey.
Figure 2.
Example questions as they appear on the Topf sound disturbance survey
Procedures
Noise measurements
Sound levels were recorded in all four treatment rooms and in the main office of the outpatient chemotherapy unit, once on a Monday and once on a Thursday (i.e., a total of ten sets of recordings). LAeq and LCpeak measurements were automatically recorded by the SLM every minute during clinic hours (7 am to 6 pm) using B and K software. Mondays and Thursdays were chosen because according to Clinic Staff, these were the busiest days in the clinic and we wanted to take measurements on the days on which sound levels were likely to be highest.
Sources of noise
Observations of noise sources in the clinic were made to determine which common activities contributed to the overall noise levels in the clinic and the levels of those activities. To this end, the researcher first observed the clinic to determine the most commonly occurring noise sources (e.g., the main door to clinic opening and closing, phones ringing). She then returned to record the frequency of occurrence of each source over a period of four hours on a Monday and four hours on a Thursday. The sound levels of each source were then measured individually after patient treatment had ended for the day using the sound level meter. Measurements were made from within the main office area and from each of the four treatment rooms. The sound levels for each noise source were recorded twice and then averaged.
Survey
Staff members handed out surveys to each patient and visitor toward the end of the patient’s appointment. No personal health information was collected. Individuals were told the purpose of the study and that their participation was voluntary. If a patient or visitor agreed to complete the survey, a staff member would note the time the patient arrived at the clinic and the time they handed back the survey. Individuals filled out the surveys on their own, and then returned them back to the staff member. Staff surveys were completed by each staff member at the end of the experimental period. The experimenter distributed the surveys to the office assistant who then handed them to all clinic staff. The surveys were anonymous, and were filled out on the staff members’ individual time. The office assistant collected staff surveys in a manila envelope.
Results
Statistical Package for the Social Sciences (SPSS) v17.0 was used to conduct all analyses. Analyses of variance were used to compare sound levels across the treatment rooms and on different days, and descriptive analyses were used to determine the mean and mode of LAeq and LCpeak occurrences. ANOVAs were also used to compare responses of patients, visitors, and staff members to the Sound Disturbance Survey, and to determine whether there was an interaction between reported disturbance and duration of time spent in the clinic. A P value <0.05 was considered statistically significant.
Noise measurements
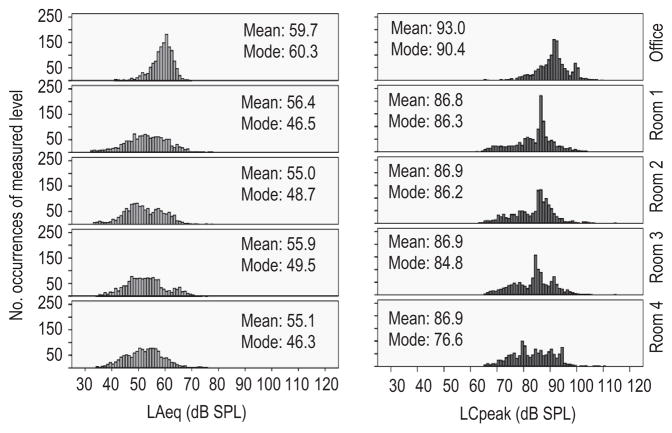
LAeq and LCpeak levels were measured on Mondays and Thursdays in the main office and in all four treatment rooms. We see no need to examine the data from each day separately; therefore, data from the two days were combined for all analyses. Figure 3 displays histograms of LAeq values (left hand side) and LCpeak values (right hand side) for the office area and each Treatment Room separately. Univariate analyses of variance (ANOVAs) were used to compare LAeq and LCpeak levels in each location. For the LAeq, analyses showed a significant main effect of measurement location (F(4,6605) = 238.6, P<0.001). Tukey HSD post hoc testing showed that levels in the Office area were significantly higher than in all other locations, and that levels in Treatment room 1 were significantly higher than in Rooms two and four. Sounds levels in Treatment Rooms two, three, and four did not differ significantly from each other. Analyses of LCpeak levels showed almost the same, with the exception that levels in treatment room one did not differ from those in Rooms two and four (Main effect of measurement location: F(4,6605) = 272.1, P<0.001).
Figure 3.
Histogram display of LAeq values (left hand side) and LCpeak values (right hand side) for the office area and each treatment room separately
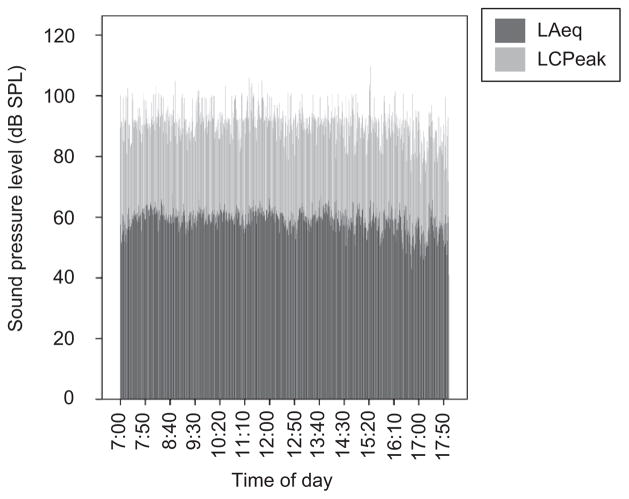
Figure 4 shows the LAeq and LCpeak noise levels in the main office over the duration of a “typical” day in the outpatient chemotherapy unit. The time of day is on the x-axis, and the sound pressure level is on the y-axis. The LAeq at each moment of time is shown in dark grey, while the LCPeak is shown in light grey. Note that over most the day, levels were fairly steady but that after about 16.10 (4.10 pm), when patient load decreased, the levels decreased also. Noise levels peaked above 90 dB SPL every minute and, although LAeq levels were only around average conversational speech levels throughout the day (55–60 dBSPL), unlike conversational speech, the noise levels remained constant throughout the day, without breaks.
Figure 4.
LAeq and LCpeak noise levels in the main office over the duration of a “typical” day in the outpatient chemotherapy unit. The time of day is on the x-axis, and the sound pressure level is on the y-axis. The LAeq at each moment of time is shown in dark grey, while the LCPeak is shown in light grey
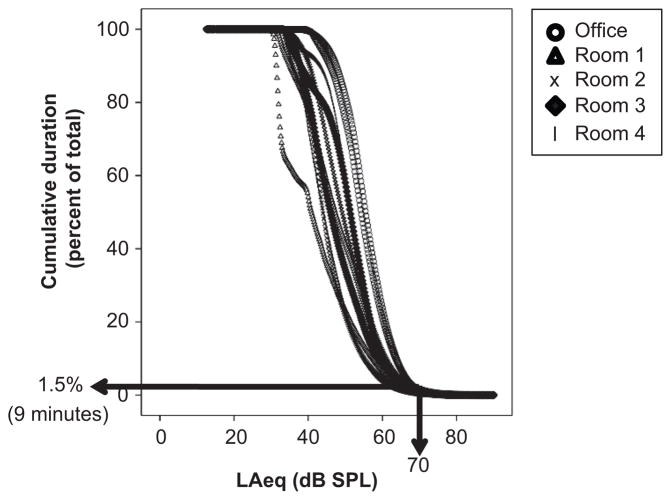
So, are these levels dangerously loud? That is, were sound levels 70 dB SPL and above for long durations during the day? To examine this, the sound pressure level (LAeq) vs cummulative percent of time at that level was plotted for each day and location separately [Figure 5]. Although it is difficult to distinguish between the data for each location, it is clear that the two sets of readings from the office area (open circle) had the highest levels over time, while the level in treatment room one was lowest (open triangles). Most importantly, looking just at levels in the office area, the figure shows that sound levels were at 70 dB SPL and above for just a short time each day. Analyses show this to be 1.5% of the time, which is equivalent to about nine minutes of the 11-hour recording time.
Figure 5.
The sound pressure level (LAeq) vs cummulative percent of time at that level plotted for each day and location separately
Sources of noise
Clinic observation lead the researcher to determine that there were seven main sources of noise in the outpatient chemotherapy unit. These are shown in Table 1, along with the number of times each hour they occurred and their peak sound pressure levels, measured in each location. During some recordings (such as the main phone ringing measured in the treatment rooms), the levels of the noise sources were below that of the ambient noise and thus could not be recorded. These data are shown in the table by an “X.” As is seen, the sound pressure level of the main door opening and closing is extremely high when measured from the office area (90 dB SPL). It was opened and closed frequently throughout the day and not surprisingly, the measured level decreased as the distance between the door and the measurement location increased [Table 1].
Table 1.
Main sources of noise in the outpatient chemotherapy unit along with the number of times each hour they occurred and their peak sound pressure levels, measured in each location
| Noise source | Location
|
|||||
|---|---|---|---|---|---|---|
| Office area | Room 1 | Room 2 | Room 3 | Room 4 | Frequency of occurrence (times/hour) | |
| Main door opening | 89.9 | 80.1 | 79.2 | 79.3 | 75.4 | 20–30 |
| Main door closing | 91.7 | 86.2 | 86.3 | 85.6 | 78.8 | |
| Ice machine in use | 84.4 | 69.8 | 71.6 | 69.8 | 69.6 | 1–3 |
| Main phone ringing | 79.9 | X | X | X | X | 2–18 |
| Nurses’ phone ringing | 70.7 | X | X | X | X | |
| Squeaky nurses’ chair | 83.7 | X | X | X | X | 20 |
| Nurses’ door opening | 95.2 | 85.7 | 86.0 | 86.0 | 83.3 | 6–10 |
X = level below that of ambient noise
Survey
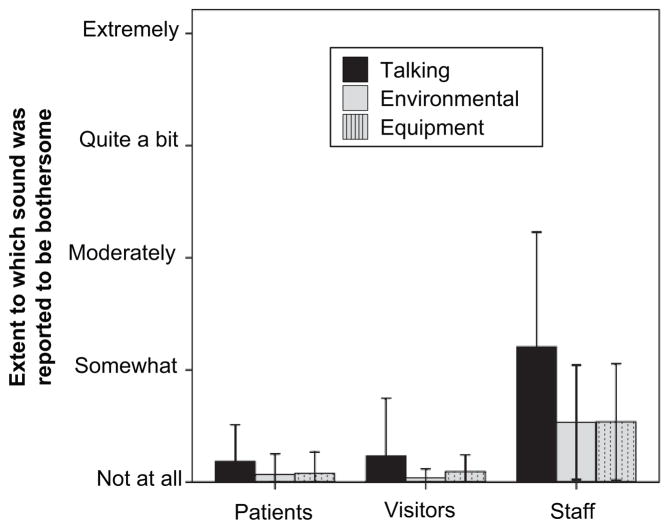
Survey data were collected from 30 patients, 16 visitors and nine staff members. There were 20 questions in the Adapted Topf Sound Disturbance Survey. Of these, seven items referred to sounds associated with talking (e.g., loud conversations between hospital personnel, conversations between patients, televisions/radios, intercoms/paging systems); five were associated with environmental sounds in the hospital (e.g., doors opening and closing, footsteps, falling objects such as pans and patient charts); and six were associated with equipment (e.g., cleaning equipment, alarms from hospital equipment, air conditioning/heating systems, cleaning equipment). The ratings given for items in each of these categories were averaged. The results are shown in the bar graph in Figure 6 for patients, visitors, and staff separately, along with error bars showing one standard deviation. It is seen that neither patients nor visitors found noise levels in the outpatient chemotherapy clinic to be bothersome. Staff responses however show that the staffs were considerably more bothered by different noises in the clinic. It is interesting to note that among all three groups, noises associated with talking were the most bothersome. The total score on the Topf sound survey was computed by adding up all responses. An ANOVA to compare the three participant groups (Visitors, Staff, and Patients) showed a significant main effect of group (F(2,52) = 15.7, P <0.001), with staff having significantly higher scores than patients or visitors. When responses to individual questions were examined, it is seen that all three groups found “Talking in the hallway,” “Nurses socializing at the nurses’ station,” “Loud conversations between hospital personnel,” “Telephones and phone conversations,” and “Conversations between other patients” to be among their top five sources of disturbing sound. Alarms from hospital equipment were also reported by Staff and visitors to be among their top five disturbing sounds.
Figure 6.
Results for the Adapted Topf Sound Disturbance Survey are shown in the bar graph for patients, visitors, and staff separately, along with error bars showing one standard deviation
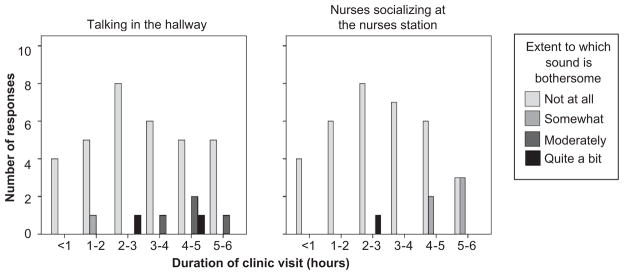
One explanation for why staff might report noise in the clinic to be more disturbing than do patients or visitors is the duration of time they spend there. To further examine this, the duration of each patient and visitor visit to the outpatient chemotherapy unit was examined in relation to their responses on the survey to the noises that patients, visitors, and staff all found to be most bothersome (“Talking in the hallway” and “nurses socializing at the nurses’ station”). Figure 7 shows bar charts of the duration of clinic visit categorized as < one hour, one to two hour, two to three hour, etc. by the number of individuals who reported each degree of disturbance (not at all, somewhat, etc.). There is an indication that the longer a patient/visitor spent in the clinic, the more they tended to be disturbed by the noise.
Figure 7.
Bar charts of the duration of clinic visit by the number of individuals who reported each degree of disturbance
The nine staff members answered questions additional to those on the Topf survey regarding the extent to which noise bothered them. Specifically, they were asked to identify how noisy they thought it was in the chemotherapy unit, how concerned they were about the noise levels, how the noise affected their ability to concentrate, to hear patients, coworkers, and alarms, whether they thought the noise would damage their own hearing or the hearing of patients, whether the noise gave them difficulty hearing on the phone, and whether the noise made they feel stressed. They were also asked whether they had taken action to address the noise levels and whether they thought the noise bothered patients. All eight of the nine staff considered the noise levels to be “loud” or “very loud,” only one considered the level to be “OK.” Six members of staff were “quite” or “moderately” concerned about the levels, but only two had taken any action to address the noise. The actions taken included closing doors, asking other members of staff not to shout across a room, and asking them to speak in softer voices. Five staff members thought patients were “somewhat” bothered by the noise levels on the unit, two thought patients were “quite” bothered, and one thought patients were “extremely” bothered by the noise levels. Of the specific difficulties most commonly reported, “difficulty hearing on the telephone” was reported by six of the nine staff members, “the noise makes me feel stressed” was reported by five of the staff members, and “difficulty concentrating on work” was reported by four of the staff members.
Discussion
In summary, average (LAeq) and peak (LCpeak) noise measures were recorded every minute from 7 am until 6 pm on a Monday and a Thursday—the two days of the week, the staff reported the clinic to be busiest. Average LAeq levels ranged between 52 and 60 dB SPL, and average LCpeak levels ranged between 85 and 93 dB SPL; however, cumulative noise levels were not above 70 dB SPL for more than a few minutes each day. 70 dB SPL is the lower level at which noise is thought to synergistically interact with Cisplatin to increase ototoxic damage to the cochlear. Patient and visitor surveys indicated that neither group was bothered by noise in the clinic. However, most staff members were bothered by, or concerned about, noise levels, and many felt that it caused stress and difficulty performing certain tasks.
LAeq and LCpeak levels were measured to determine if noise levels in the chemotherapy clinic were high enough to increase the patients’ risks of hearing impairment. Depending on the room, average LAeq levels ranged from 52 to 60 dB SPL, and LCpeak levels typically peaked above 90 dB SPL every minute. However, even on the reportedly busiest day and in the loudest room, cumulative noise levels were above 70 dB SPL for less than ten minutes over the 11-hour recording period. According to Gratton et al.,[3] there is a synergistic interaction between noise and Cisplatin for levels of noise between 70 and 85 dB SPL. It is therefore unlikely that the noise levels in the outpatient chemotherapy unit are increasing ototoxic damage. It should be noted, however, that staff members were aware of when the recordings took place, and thus might have adjusted their behaviors to decrease noise during measurement periods. Indeed, informal observations and comments received by the researcher indicated that many staff members were concerned about being too noisy during the recording periods, and made attempts to be quieter. Thus, the noise levels measured here might be an underestimation of the true sound levels.
Although the ongoing noise levels were not high enough to likely increase ototoxic damage, they are of concern because staff reported that the noise was highly disturbing. The patients and visitors surveyed here, however, indicated that noise levels did not bother them. This is consistent with previous studies that have surveyed patients and staff. [8] However, the data here indicated a positive relationship between the extent to which patients and visitors found the noise to be disturbing and the time they spent in the chemotherapy unit. This might also explain why staff, who spends a full eight to ten hour shift in the unit, found the noise levels to be so disturbing. Explanations for why patients and visitors were not bothered by the noise could include the fact that many were older veterans who might therefore have had pre-existing hearing loss and thus did not hear much of the clinic noise, or that they were grateful for the level of care being provided, overshadowing any potential for noise disturbance.
Staff reported significantly more noise disturbance than patients. As discussed above, this difference may be because staff spends longer in the clinic than the patients and visitors. It might also be that staff spends more time in the noisier busier office area than the patients, or because their role of healthcare provider requires concentration and communication different to that required from the patients and visitors. The overall noise levels and peaks in the clinic are at levels that can contribute to adverse psychological and physiological effects, which some of the staff members may be experiencing. Consistent exposure to moderate levels of noise can result in increased long-and short-term sickness absence,[15] fatigue,[11] stress, frustration,[14] decreased motivation, and increased risk for heart disease.[13] It is, however, important to note that the surveys did not assess job-related stress independently of noise levels, which could have also contributed to increased disturbance from noise.
In terms of the noise sources, there are at least two points of interest. First, that the modal LCpeak in each measurement location is almost identical to the level of the main door closing in that location [Figure 3 and Table 1] and second that almost all of the major sources of noise can be reduced relatively easily through behavioral or environmental modifications. Because staff reported considerable disturbance from the noise, and because the effects of moderate noise levels are known to be adverse, attempts should be made to do this. Environmental modifications to address the specific sources of noise elucidated in the chemotherapy unit could include moving the ice machine to a location behind a closed door, lubricating squeaky equipment, reducing ringer volume of the phones, providing in-the-ear telephone pieces for staff members to hear better, and possibly replacing the especially noisy door which opened and closed using an air-pressure system. Many other environmental and behavioral modifications could also contribute to decreased noise levels in the clinic such as providing “TV ears” or allowing the use of personal music devices for patients, moving vibrating equipment away from the wall, rearranging furniture to help contain conversational areas, moving noisy equipment away from open areas, and carpeting areas that currently have tile. Behavioral modifications could include having staff members communicate at closer distances to limit shouting across rooms, closing doors more quietly, and being more careful when opening cabinets or using equipment.
To address behavioral modifications, a video has been developed that educates staff members about the effects of moderate noise, and about simple but effective ways to reduce noise levels in the clinic. The effectiveness of this video will be evaluated in several VA clinics by measuring noise levels before and after the video is shown.
Conclusion
Although overall noises were not at levels known to react synergistically with Cisplatin, these levels likely contribute to increased fatigue, stress, frustration, decreased motivation, and increased risk for heart disease among staff, patients, and visitors. Surveys indicated that most staff members were bothered by noise levels in the clinic and felt that the noise contributed to workplace stress and decreased job performance. Because of these effects, precautions must be taken to reduce overall noise levels in the chemotherapy unit. This could be accomplished with inexpensive equipment modifications, behavioral modifications (i.e., staff members talking in closer range when communicating), and through education by hospital audiologists.
Acknowledgments
Support for this work was provided by NIH Predoctoral Training Grant T35 DC008764 and VA RR and D Grant # C4844C. We thank Patricia Pulliam, A.N.P., and other staff and patients of the Portland VA Medical Center Chemotherapy outpatient clinic for their participation, Roger Ellingson for his assistance with the equipment and Sarah Weidman for her assistance with data collection.
Appendix A: Copy of the Noise Disturbance Survey
| Please put a check in the box that best describes how much each of the sounds listed below bothered you today during your chemotherapy treatment
| |||||
|---|---|---|---|---|---|
| Not at all | Somewhat | Moderately | Quite a bit | Extremely | |
| Patient sounds such as coughing, gagging, moaning | □ | □ | □ | □ | □ |
| Talking in the hallway | □ | □ | □ | □ | □ |
| Doors opening, closing, slamming | □ | □ | □ | □ | □ |
| Falling objects such as pans, patient charts | □ | □ | □ | □ | □ |
| Nurses socializing at the nurses station | □ | □ | □ | □ | □ |
| Squeaking parts on beds and equipment | □ | □ | □ | □ | □ |
| Loud conversations between hospital personnel | □ | □ | □ | □ | □ |
| Air conditioning, heating, or ventilation systems | □ | □ | □ | □ | □ |
| Telephones and phone conversations | □ | □ | □ | □ | □ |
| Cleaning equipment such as vacuum cleaners | □ | □ | □ | □ | □ |
| Intercoms, paging system | □ | □ | □ | □ | □ |
| Conversations between other patients | □ | □ | □ | □ | □ |
| Radios and televisions | □ | □ | □ | □ | □ |
| Hospital equipment such as suction and breathing machines | □ | □ | □ | □ | □ |
| Food trays and eating utensils | □ | □ | □ | □ | □ |
| Medicine and linen carts | □ | □ | □ | □ | □ |
| Alarms from hospital equipment | □ | □ | □ | □ | □ |
| Footsteps | □ | □ | □ | □ | □ |
| Sounds from the kitchen area | □ | □ | □ | □ | □ |
| Other (please specify) | □ | □ | □ | □ | □ |
References
- 1.Cary R, Clarke S, Delic J. Effects of combined exposure to noise and toxic substances--critical review of the literature. Ann Occup Hyg. 1997;41:455–65. doi: 10.1016/S0003-4878(97)00006-9. [DOI] [PubMed] [Google Scholar]
- 2.Kovacic P, Somanathan R. Ototoxicity and noise trauma: Electron transfer, reactive oxygen species, cell signaling, electrical effects, and protection by antioxidants: Practical medical aspects. Med Hypotheses. 2008;70:914–23. doi: 10.1016/j.mehy.2007.06.045. [DOI] [PubMed] [Google Scholar]
- 3.Gratton MA, Salvi RJ, Kamen BA, Saunders SS. Interaction of cisplatin and noise on the peripheral auditory system. Hear Res. 1990;50:211–23. doi: 10.1016/0378-5955(90)90046-r. [DOI] [PubMed] [Google Scholar]
- 4.Boettcher FA, Henderson D, Gratton MA, Danielson RW, Byrne CD. Synergistic interactions of noise and other ototraumatic agents. Ear Hear. 1987;8:192–212. doi: 10.1097/00003446-198708000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Rademaker-Lakhai JM, Crul M, Zuur L, Baas P, Beijnen JH, Simis YJ, et al. Relationship between cisplatin administration and the development of ototoxicity. J Clin Oncol. 2006;24:918–24. doi: 10.1200/JCO.2006.10.077. [DOI] [PubMed] [Google Scholar]
- 6.Guthrie OW. Aminoglycoside induced ototoxicity. Toxicology. 2008;249:91–6. doi: 10.1016/j.tox.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Suter AH. Hearing Conservation Manual. 4. Milwaukee, WI: Council for Accreditation in Occupational Hearing Conservation; 2007. [Google Scholar]
- 8.Topf M. Personal and environmental predictors of patient disturbance due to hospital noise. J Appl Psychol. 1985;70:22–8. [PubMed] [Google Scholar]
- 9.Dratva J, Zemp E, Felber Dietrich D, Bridevaux PO, Rochat T, Schindler C, et al. Impact of road traffic noise annoyance on health related quality of life: Results from a population-based study. Qual Life Res. 2010;19:37–46. doi: 10.1007/s11136-009-9571-2. [DOI] [PubMed] [Google Scholar]
- 10.Simmons D, Graves K, Flynn EA. Threading Needles in the Dark- The Effect of the Physical Work Environment on Nursing Practice. Crit Care Nurs Q. 2009;32:71–4. doi: 10.1097/CNQ.0b013e3181a27d99. quiz 75–6. [DOI] [PubMed] [Google Scholar]
- 11.Tompkins OS. Secondhand noise and stress. AAOHN J. 2009;57:436. doi: 10.3928/08910162-20090928-03. [DOI] [PubMed] [Google Scholar]
- 12.Witterseh T, Wyon DP, Clausen G. The effects of moderate heat stress and open-plan office noise distraction on SBS symptoms and on the performance of office work. Indoor Air. 2004;14:30–40. doi: 10.1111/j.1600-0668.2004.00305.x. [DOI] [PubMed] [Google Scholar]
- 13.Evans GW, Johnson D. Stress and open-office noise. J Appl Psychol. 2000;85:779–83. doi: 10.1037/0021-9010.85.5.779. [DOI] [PubMed] [Google Scholar]
- 14.Morrison WE, Haas EC, Shaffner DH, Garrett ES, Fackler JC. Noise, stress, and annoyance in a pediatric intensive care unit. Crit Care Med. 2003;31:113–9. doi: 10.1097/00003246-200301000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Clausen T, Christensen KB, Lund T, Kristiansen J. Self-reported noise exposure as a risk factor for long-term sickness absence. Noise Health. 2009;11:93–7. doi: 10.4103/1463-1741.50693. [DOI] [PubMed] [Google Scholar]
- 16.Topf M, Dillon E. Noise-induced stress as a predictor of burnout in critical care nurses. Heart Lung. 1988;17:567–74. [PubMed] [Google Scholar]
- 17.Boehm H, Morast S. Quiet time: A daily period without distractions benefits both patients and nurses. Am J Nurs. 2009;109(11 Suppl):29–32. doi: 10.1097/01.NAJ.0000362015.55128.54. [DOI] [PubMed] [Google Scholar]
- 18.Laurell GF. Combined effects of noise and cisplatin: Short- and long-term follow-up. Ann Otol Rhinol Laryngol. 1992;101:969–76. doi: 10.1177/000348949210101202. [DOI] [PubMed] [Google Scholar]