Abstract
In the first three decades of life, more individuals in the USA die from injuries and violence than from any other cause. Millions more people survive and are left with physical, emotional, and financial problems. Injuries and violence are not accidents; they are preventable. Prevention has a strong scientific foundation, yet efforts are not fully implemented or integrated into clinical and community settings. In this Series paper, we review the burden of injuries and violence in the USA, note effective interventions, and discuss methods to bring interventions into practice. Alliances between the public health community and medical care organisations, health-care providers, states, and communities can reduce injuries and violence. We encourage partnerships between medical and public health communities to consistently frame injuries and violence as preventable, identify evidence-based interventions, provide scientific information to decision makers, and strengthen the capacity of an integrated health system to prevent injuries and violence.
Introduction
Nearly 180 000 people in the USA die every year from injuries and violence related to preventable events such as car crashes, drug overdoses, falls, assaults, drowning, and self-harm, according to numbers from the US Centers for Disease Control and Prevention (CDC).1 This number is equivalent to one injury death every 3 mins. Millions more people survive these events every year and are left with substantial physical, emotional, and financial problems as a result of acts of violence or unintentional injury. No individual is immune from these tragedies— people of all ages, races, and levels of education and income are affected. Injuries and violence are not accidents and are not inevitable. They can be prevented. Yet, although figures in public health maintain a common understanding for the definition, causes, and solutions to injuries and violence, this recognition might not be widely accepted by other audiences, including policy makers, clinical health professionals, and the public. Injuries and violence can be seen as inevitable and unpredictable.2,3 Representatives in public health have struggled to change this perception in some key stakeholders such as policy makers and even health professionals. When the need for injury prevention is recognised by individuals in health systems, training, time, and skill are often insufficient to enable a suitable response.
In clinical settings, injury prevention is not integrated fully in practice and patients are not as familiar with ways to prevent injuries as they are with those for other major killers such as heart disease, stroke, and cancer.4 Physicians and other health-care workers have not yet included screening for injury risk into routine standards of care. National estimates are that one in five adults visiting health-care providers receive counselling about injury prevention.5 This absence might be partly due to the increase in demands on practitioners—if primary care physicians were to satisfy fully the clinical recommendations of the US Preventive Services Task Force, then they would need to devote longer than 7 h per day to preventive services alone.6 Managed-care organisations and other health-care institutions have not fully codified injury prevention counselling into clinical workflow and electronic medical records to improve the delivery of injury prevention services.7
Although the USA has achieved some important milestones in injury and violence prevention in the past century, greater improvements are attainable.8 Even in individuals who have awareness of the preventability of injuries and violence, perception of risk is incongruent with actual risk.9 The tendency for optimistic bias, an attitude of self-exception, or an inaccurate perception of the consequences of actions can all disrupt prevention efforts. And similar to other major public health challenges (especially those attached to broad public policy solutions), tension exists between the protections of personal freedom and the sought after benefits for public health. Stated simply, how does the USA achieve the greatest good for the greatest number of people, while also respecting civil liberties? In a Comment in a 2012 issue of The Lancet, Shakur and colleagues10 stated that “…to reduce the human and economic effect of injury, we need better prevention, effective and affordable treatments, and the tenacity to ensure their universal access”. The viability of attention to public health issues is linked to features of the problem, the way in which stakeholders portray the issue, the policy environment, and the strength of organisations concerned with the issue.11 Using these perspectives, we posit that to advance injury and violence prevention, the communication frame should be enhanced (so that messages increase awareness and change perceptions), success stories be shared, science be translated, data be provided to decision makers, effective interventions be disseminated, and public health be integrated with clinical medicine.
Morbidity, mortality, and the effect of injuries and violence
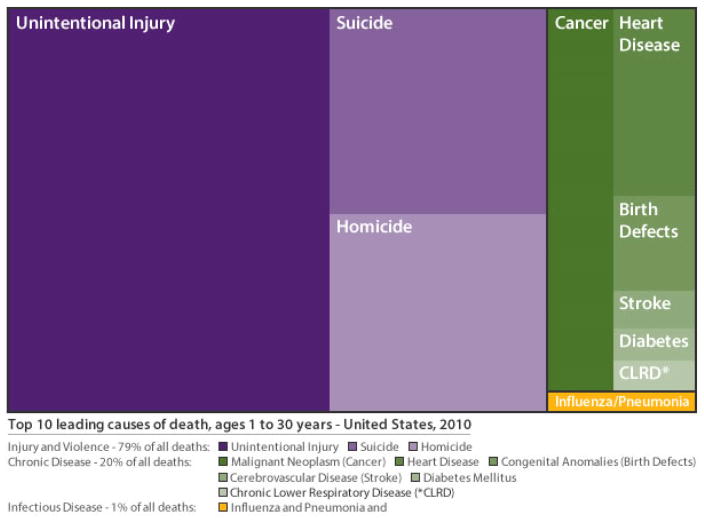
From age 1 year to age 30 years, more individuals in the USA die from injuries and violence than from any other cause (figure 1).1 In 2010, the ten leading causes of death in this age group were, in order, unintentional injury, suicide, homicide, cancer, heart disease, congenital anomalies, cerebrovascular disease, influenza and pneumonia, diabetes, and chronic low respiratory disease. An alarming 79% (n=41 121) of deaths were due to injuries, whereas 20% were due to chronic diseases and 1% were due to infectious diseases including influenza and pneumonia. Of injury deaths, 59·6% were caused by unintentional injuries, 20·5% by suicide, and 19·9% by homicide.1 In 2010, almost 121 000 people of all ages died from unintentional injuries in the USA (age-adjusted rate of 37·9 deaths per 100 000). The most frequent causes were motor-vehicle crashes (33 687), poisoning (33 041), falls (26 009), suffocation (6165), drowning (3782), and fires (2845). In that same year, more than 55 000 violence-related deaths occurred in the USA (17·5 per 100 000). The number of deaths tells only part of the story. In 2011, about 2·3 million people were treated in US emergency departments for an assault or act of self-harm, and about one in ten people had a nonfatal unintentional injury that was serious enough for them to need to visit an emergency department. Beyond these injuries, millions of Americans every year are victims of intimate partner violence, sexual violence, and child maltreatment (panel 1).12,16 The results extend beyond injury affliction. Injuries and violence can have other physical, mental, sexual, and reproductive health consequences that can become chronic and result in substantial health burden and costs.21,22 More than 31·2 million unintentional and violence-related injuries occurred in 2010, resulting in an estimated annual cost (indexed to 2010 prices) of more than US$513 billion in medical care and lost productivity across the lifespan of victims.1 This figure does not include the costs associated with non-medically treated injuries, legal costs, or indirect costs from other health problems associated with or exacerbated by violence and injuries.
Figure 1. Top 10 leading causes of death for ages 1 to 30 years – United States, 2010.
CDC. Web-based Injury Statistics Query and Reporting System (WISQARS). 2013 February 19, 2013; Available from: http://www.cdc.gov/ncipc/wisqars.
Pressing challenges
Choice of focus
Some types of injury, such as homicide, suicide, prescription drug overdose, falls in older adults, traumatic brain injury, and child injury, have received increased recognition because of changing trends, striking disparities, and rising public concern. These topics underscore new pressing demands in the USA and offer compelling reasons to respond swiftly. Other types that we have not expanded on in this article, such as road traffic injuries, have reduced substantially and are considered winnable battles after many public health achievements, partly due to effective policies and strategies identified through research (panel 1).
Homicide and suicide
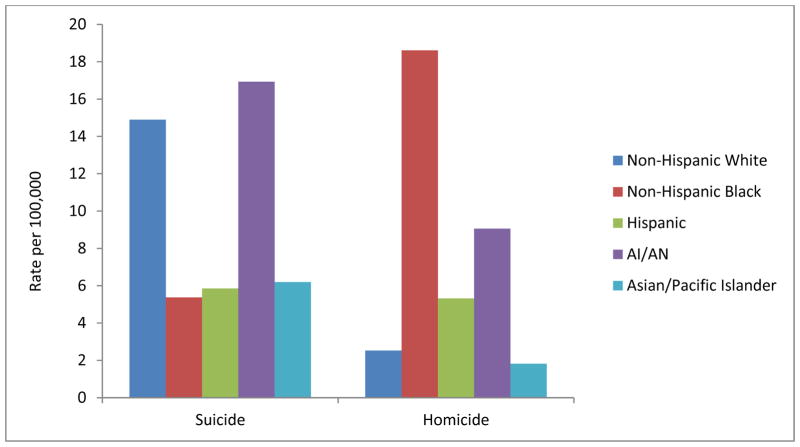
In 2010, the number of people who died by suicide (38 364 deaths; 12·0 per 100 000) was more than double the number of individuals who died by homicide (16 259; 5·29).1 The highest rate of violent deaths occurred in men and ethnic minorities. Rates of homicide were nearly four times higher for men than for women (8·3 deaths per 100 000 men vs 2·2 per 100 000 women). This sex difference was also present for individuals who died by suicide (19·8 vs 5·0). Although rates of suicide were highest in American Indian and Alaskan Natives (16·9) and non-Hispanic whites (14·9), rates of homicide in African Americans were double those for American Indian or Alaskan Natives (18·6 vs 9·1) and exceeded those of men of other races or ethnic background by several times (figure 2). One in every two suicides and about 68% of all homicides in the USA are carried out with a firearm. In 2010, an average of 83 people died each day as a result of firearm-related homicide or suicide.
Figure 2. Age-adjusted suicide and homicide rates by race/ethnicity – United States, 2010.
CDC. Web-based Injury Statistics Query and Reporting System (WISQARS). 2013 February 19, 2013; Available from: http://www.cdc.gov/ncipc/wisqars.
Prescription drug overdose
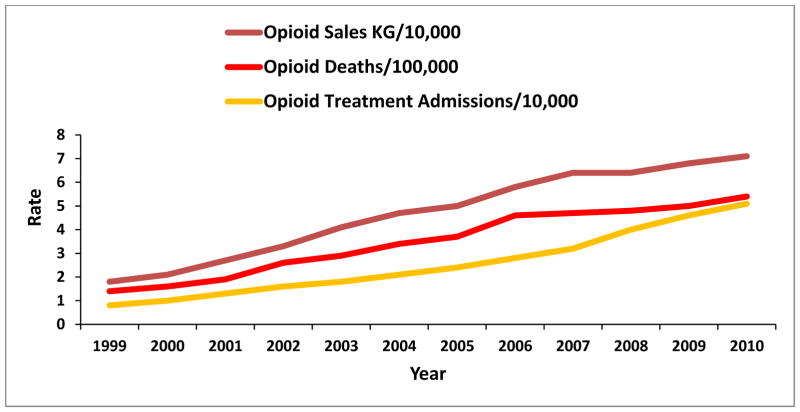
Overdose can occur through intentional or unintentional means, although most deaths from overdose are unintentional.1 In 2010, 38 329 people in the USA died from a drug overdose. Prescription drugs were involved in most of these deaths (22 134 deaths; nearly 60%). 75% of prescription drug deaths were from overdose of opioid analgesics such as oxycodone, hydrocodone, and methadone; deaths from opioid analgesics have nearly quadrupled since 1990 (figure 3).23,24 Drug overdose is commonly viewed as an issue of substance misuse, mental health, or law enforcement rather than an injury and public health concern; however, this rise in overdose deaths coincides with an increase in the supply of prescription painkillers, indicating a need for intervention from health professionals. Four times more prescription painkillers were sold to pharmacies, hospitals, and doctors’ offices in 2010 than in 1999.24
Figure 3. Rates of opioid overdose deaths, sales and treatment admissions – United States, 1999–2010.
Adapted from Centers for Disease Control and Prevention, Vital Signs: Overdoses of prescription opioid pain relievers -- United States, 1999–2008. Morbidity and Mortality Weekly Report, 2011. 60: p. 1487–1492. Updated with 2009 mortality and 2010 treatment admission data.
Falls in older adults
Falls are the largest cause of injury deaths for older adults in the USA. About a third of adults aged 65 years and older have a fall every year and those who fall are two to three times more likely to fall again within 1 year.25,26 More than 21 000 people aged 65 years and older died from an unintentional fall in 2010. Equally troubling are the more than 2·4 million injuries from non-fatal, unintentional falls that occurred in 2011.1 After adjustment for inflation, the direct medical costs of falls in 2010 was $30 billion.27 About 20% of falls in older adults cause serious injuries such as fractures and head injuries—injuries that can restrict mobility, decrease quality of life, and increase the risk of premature death.28 Given the ageing of the US population, the effect of falls on health-care systems is likely to grow.
Traumatic brain injury
The Demographics and Clinical Assessment Working Group of the International and Interagency Initiative Toward Common Data Elements for Research on Traumatic Brain Injury and Psychosocial Health Injuries defines traumatic brain injury as a “blunt or penetrating trauma to the head that results in an alteration in brain function, or other evidence of brain pathology, caused by an external force”.29 The main causes of fatal and non-fatal traumatic brain injury combined are falls (35·2%), motor-vehicle crashes (17·3%), blunt impact (16·5%), and assault (10%).30 In 2009, about 2·4 million emergency department visits, hospital admissions, and deaths included a diagnosis of traumatic brain injury.31 From 2007 to 2009, an average of almost 1·2 million visits to outpatient clinics or physician offices each year included a diagnosis of traumatic brain injury. These numbers do not include people who are injured or die while serving in the military. Severity can range from a minor concussion with no loss of consciousness to prolonged coma and death. Observations of progressive neurodegenerative disorders among former athletes who had participated in contact sports (eg, American football and hockey) and veterans and military personnel have led to an understanding that multiple concussions in some people can result in progressive neurodegeneration, termed chronic traumatic encephalopathy.32 Symptoms of chronic traumatic encephalopathy initially include difficulties with attention, concentration, and memory, but the disorder continues to progress and, at its most severe stage, can include dementia and parkinsonian symptoms.32
Child and adolescent injury
Injuries and violence disproportionately affect children and young people. Suffocation is the most common cause of injury deaths in infants (aged younger than 1 year), drowning is the most common cause in children aged 1–4 years, and motor-vehicle crashes are the most common cause in young people aged 5–24 years.1 From 2000 to 2009, the rate of unintentional injury death in children 19 years and younger decreased by 29%; however although the rate for deaths related to motor vehicle traffic fell by 41%, deaths from poisoning in teenagers aged 15–19 years nearly doubled.33 Homicide is the second leading cause of death in young people aged 15–24 years, and suicide is the third largest. More than 40% of women who have been raped in the USA were raped before age 18 years (29·9% aged 11–17 years, 12·3% before age 10 years).12 More than a quarter (27·8%) of men who have been raped were raped when they were aged 10 years or younger.12 Children who have been victims of violence are substantially more likely to engage in health-risking behaviours in adolescence and adulthood, heightening their risk for disease, disability, and early death. A growing amount of evidence links major adult forms of illness and disease (including ischaemic heart disease, cancer, chronic lung diseases, and diabetes) to violence and other adverse exposures in childhood.34–37
Social determinants
Many social and economic factors contribute to disparities in injury risk and outcomes in the USA, including income, education, employment, and community environment. For example, men who are unmarried, have a low-income, are unemployed, or are poorly educated are at increased risk for death by motor-vehicle injury.38 Young people growing up in communities with concentrated disadvantage are more likely to witness violence, attend underperforming schools, and have poor employment opportunities; they are also more likely to be exposed to drug-distribution networks and can access firearms more readily than can young people not growing up in such communities.39 These social and environmental factors can greatly increase an individual’s risk of perpetrating violence and being a victim of violence. Thus, the link between socioeconomic status and injury is mediated by many conditions at home, at work, in communities, and within families and groups, with variations in effects noted across different types of injury.40 Social and economic factors fuel stress; challenge adaptation and coping mechanisms; contribute to social exclusion and isolation, residential instability, workplace pressures, and low community participation; and affect access to safe environments, safety equipment, and services.41 These factors can accumulate and interact to substantially affect experiences and risks. It is crucial that surveillance data and epidemiological research are used to improve understanding for the most vulnerable subgroups and to monitor progress in the reduction of disparities over time. In addition to increases in the availability of health services and prevention programmes to address disparities, strategies to improve access to employment, safe housing, and high-quality education, and to reduce bias and discrimination, are needed to address underlying contributing factors.
Prevention of injuries and violence
Where to aim prevention strategies
Effective interventions
The scientific evidence to support prevention of injury and violence is strong.8,42,43 Public health strategies for prevention such as education, behaviour change, policy, engineering, and environmental support are guided by the social-ecological model that informs how strategies should be implemented across individual, relationship, community, and society levels. Interventions that address the social and economic determinants of health and change the context to make individuals’ default decisions healthy can have a greater public health effect than can have interventions that require intensive, one-on-one, counselling.44 In 1996, the US Department of Health and Human Services established the Community Preventive Services Task Force (CPSTF), an independent, non-federal panel of public health and prevention experts. The CPSTF makes evidence-based recommendations about population health interventions that are scientifically proven to save lives, increase lifespans, and improve quality of life. The Guide to Community Preventive Services (a resource for dissemination of Task Force recommendations) highlights success in identification of effective interventions, including in the areas of injury and violence prevention. Findings are used to improve decision making about which approaches to use and which to avoid.45
The CPSTF recommends policy interventions that promote use of seat-belt and child safety-seat and prevention of drink driving to reduce motor-vehicle related injuries. Laws that require children riding in motor-vehicles to be restrained in federally approved infant or child safety-seats can decrease fatal injuries by 35%.46 Laws that mandate the use of safety belts by motor vehicle occupants can decrease fatal and non-fatal injuries combined by 8%, with greater effects noted in states with primary enforcement laws (in which a police officer is authorised to stop a motorist for not wearing a seat belt) than in those with secondary enforcement laws (in which a police officer can issue a citation only when a motorist is stopped for another reason).47 Implementation of laws for a legal limit of 0·08% blood alcohol content can reduce fatalities by 7%; all states in the USA having this law saves a potential 400–600 lives per year.48 The implementation of these effective interventions, in part, has led to the identification of prevention of motor vehicle injuries as one of the ten greatest public health achievements of the past century.13
The CPSTF recommends early childhood home visitation, school-based violence prevention, and therapeutic foster care to prevent violence. Programmes that use home visitation (eg, by nurses) during a child’s first 2 years of life and provide training (eg, about parenting skills and life skills) and assistance (eg, education and work opportunities, and community service linkage) can reduce child maltreatment in high risk families by 39%.49 School-based programmes that focus on building of social problem-solving skills and promotion of emotion regulation can result in a 15% relative reduction in violent behaviour in students across all school years receiving the programmes and a 29% reduction in violence among individuals in high school (aged about 14–18 years).50 Use of intensive therapeutic foster care as an alternative to incarceration or residential treatment for chronically delinquent adolescents can decrease violent crime. Investigators compared studies of young people who had a history of chronic delinquency given programme-intensive therapeutic foster care to those of young people given standard group residential treatment—the median reduction of violent crime was 72% greater in the group given intensive foster care.51
Emerging prevention strategies
The identification and testing of new innovative strategies to address pressing challenges is of equal importance as is the recommendation of effective and rigorously evaluated intervention strategies. For states to address the growing public health challenge of opioid overdose, but ensure that patients with pain are safely and effectively treated, the following practices have emerging evidence: to start or improve prescription drug monitoring programmes (electronic databases that track all prescriptions for painkillers in the state); to use these monitoring programmes, Medicaid, and workers’ compensation data to identify improper prescribing of painkillers; to implement and evaluate laws to limit pill mills and doctor shopping (to stop patients receiving drugs from several providers) and identify other laws to reduce prescription painkiller misuse; to encourage professional licensing boards to take action against inappropriate prescribing; and to increase access to treatment for substance misuse. With these programmes, health-care professionals and managed-care organisations can better follow prescription guidelines and incorporate data from prescription drug monitoring programmes into clinical decision making and workflow.24 Washington state has shown success in the development of interagency opioid-dosing guidelines in combination with support for legislation that repealed permissive prescribing rules and provided funding for the establishment and maintenance of a prescription drug monitoring programme.52
An emerging strategy in violence prevention focuses on changes to the community and policy. Results from an evaluation funded by the CDC suggested that business improvement districts effectively reduced rates of crime and violence in Los Angeles, CA. Business improvement districts are grassroots, self-organising, public–private organisations that collect monetary assessments from local merchants and property owners and use these funds to create economic opportunities and invest in local-area service provision and activities such as street cleaning and beautification and public safety. Business improvement districts were associated with a 12% drop in robbery rates and an 8% drop in violent crime compared with areas without these districts. Business improvement districts were also associated with 32% fewer police arrests, suggesting that decreases in crime were not due to increased police activity.53 A cost analysis showed that investments in business improvement districts resulted in cost savings due to reduced crime rates and arrests and lower prosecution-related expenditures.54
Return on investment for prevention strategies
Strategies for injury and violence prevention can be cost effective and even offer a positive return on investment. Road safety interventions such as child-occupant protection, helmet laws, graduated drivers licences, and strategies to prevent impaired driving save more resources than they cost to implement.55 Child safety-seat laws and sobriety checkpoints have net cost savings because the saved medical and other resource costs are more than are costs of implementation and maintenance— eg, estimated quality-adjusted life-year (QALY) savings of $1200 for safety-seat laws and $44 000 for sobriety checkpoints.55 Evidence-based community fall prevention programmes show a promising return—eg, Moving for Better Balance (160% return) and Stepping On (100%).56 Substantial savings could be achieved, particularly for third-party payers such as health maintenance organisations, if such prevention strategies were promoted more effectively through the public health and clinical medicine infrastructure.55
Evidence for the cost-effectiveness of violence prevention strategies is growing rapidly. Researchers have analysed several prevention strategies that are considered models of (or that show promise for) their cost-effectiveness on the basis of data for Washington state.57 Life Skills Training is a school-based programme that provides content for teachers and students on anger management and conflict resolution. Results indicate significant reductions in fighting and delinquency, and cost analyses estimate a return of $37·52 for each $1·00 invested. Nurse–Family Partnership provides information, training, and support to low-income women during their pregnancy and for the first 2 years of their child’s life. Nurse–Family Partnership results in long term reductions in child maltreatment and fewer problem behaviours when the child is an adolescent, including 56% fewer arrests. The programme is intensive and requires a significant investment, but the return of the investment is substantial, about $2·37 return for each $1·00 invested, resulting in about $13 181 in savings per child.
Bringing effective strategies into practice
Scientific evidence about injury and violence burden, risk factors, and effective prevention interventions does not automatically translate into more effective practices and policies. For maximum adoption, public health researchers must use implementation science to inform best practices for the translation and dissemination of interventions. Reductions in morbidity and mortality will be small until effective interventions are implemented and integrated into the broader health and wellness system. We outline potential methods to translate the science, disseminate effective interventions, and integrate injury prevention into health systems. In addition to these methods, strategic communication must be used for practitioners and decision makers to translate science into actionable knowledge at local, state, and national levels. Messages about injury can be enhanced through use of framing theory (to leverage societal values and enhance the prevention focus), social mathematics (to provide meaning and show statistics vividly), and success stories (to provide explicit action models for community mobilisation, needs assessments, strategy selection, and health effects). Further, communication with decision makers must occur when policy windows open and conditions align for evidence to inform action.
Translation and dissemination of effective interventions
Evidence-based interventions exist to prevent injuries and violence, but too often they are not available, not affordable, or simply not used by patients, providers, and consumers. The gap between research and practice, or discovery and delivery, is large and continues to impede progress in the USA.58 The Interactive Systems Framework highlights that key systems must be in place to synthesise evidence and translate information into user-friendly instruments and strategies; to build general and innovation-specific capacity for implementation through training and technical assistance; and to get strategies implemented at the organisational, community, or state level.59 Translation efforts should focus on interventions that can be scaled up and are anticipated to have the greatest public health effect.
Some important factors help the process of translation and dissemination and allow for the advancement of large-scale evidence-based practice. These factors include researchers actively communicating with practitioners to share information, targeted communication efforts by investigators to synthesise research and highlight particular areas of interest to users (eg, core components of effective strategies and key benefits), and audience engagement in translation of product development to enhance usefulness. Innovative approaches can identify and select the common elements of evidence-based interventions to allow this synthesis for practitioners, such as the Distillation and Matching Model.60 Partnerships and coalition building among stakeholders, such as health departments, clinical-care providers, educators, law enforcement, and community organisations, offer stimulation for planning and financing of prevention strategies. Training, technical assistance, and coaching for organisations and health systems to implement injury prevention activities would enhance adoption and implementation adherence. Finally, policies can help to build better injury-prevention capacity—eg, the American College of Surgeons’ requirement for trauma centre verified programmes to participate in injury prevention activities has led to injury prevention and community outreach coordinators being established within trauma centres. An example of translation of scientific information for practitioners is the CDC’s Heads Up initiative, which focuses on prevention, recognition, and response to concussion in youth sports. A suite of free materials and toolkits tailored to a varied audience including youth and high-school sports coaches, parents, athletes, and healthcare professionals are available. A key message contained in the various kits is the importance of removal of athletes from play after concussion and to delay return to play until they are cleared by an experienced health-care provider.61 These actions are important to reduce cumulative risk from repeated concussions and prevent serious long-term events. A large and varied audience hearing this information is essential to change cultural norms that encourage return to play before the brain has completely healed.
Similarly, the Blueprints for Healthy Youth Development project at the University of Colorado’s Center for the Study and Prevention of Violence translates information about effective youth prevention programmes for agencies, communities, schools, and foundations. Users can walk through a step-by-step menu to tailor their search of evidence-based programmes to local needs for their outcomes of interest (eg, behaviours such as violence or gang involvement), risks and protective factors that are most crucial for their community, and characteristics of the population served. Users are provided with rich descriptive information on relevant programmes, including the evidence rating, data for costs and potential funding strategies, a description of the target population, and effect sizes from rigorous assessments.62
Another example of a system that builds capacity for implementation is the CDC Tribal Motor Vehicle Injury Prevention Program. The CDC has supported four to eight Native American tribes each year to adapt, implement, and evaluate evidence-based interventions identified in the Community Guide to reduce motor vehicle-related injury and death in their communities. General capacity-building efforts have focused on surveillance and data use, whereas innovation-specific capacity has focused on best practices for implementation of interventions for motor-vehicle safety through education, awareness, and enforcement. Programmes increased seat-belt and child safety-seat use and decreased alcohol-impaired driving.63 A manual for best practice and lessons learned will be developed from these activities to support other tribes in adoption of this implementation model.
Finally, the Maternal, Infant, and Early Childhood Home Visiting (MIECHV) programme is a prevention delivery system that supports implementation at federal, state, and community levels.64 It enhances coordination of evidence-based strategies for home visitation services within a comprehensive early childhood system to prevent child maltreatment, intimate partner violence, and emergency department visits due to injury in at-risk communities. Home visitors (including nurses, social workers, and other health professionals) work with families to assess their circumstances, help them gain the skills they need to ensure healthy development in their children, and connect them to other resources and support. The MIECHV programme allows for partnership among agencies at the state and community levels to support prevention service delivery that can lead to improvements in referrals for resources and supports.
Integration of public health with clinical medicine
Prevention of injuries and violence is a shared responsibility. People who work in public health must work in partnership with those in clinical medicine to ensure that health delivery systems are well integrated and are performing effectively, efficiently, and equitably to prevent injury and improve outcomes throughout the continuum of care. Goals for integration include to monitor and improve the quality and cost-effectiveness of injury prevention and treatment provided by the public health and health-care delivery system; to enhance health system capacity to adopt, implement, and diffuse evidence based injury-prevention practice such as through injury prevention education for health-care providers; to evaluate the effectiveness of public health and health system financing to improve injury prevention and outcomes for injured patients; and to strengthen the capacity of the health system workforce to deliver effective services for injury prevention and health.65
The Affordable Care Act provides an opportunity to integrate injury and violence prevention into health-care delivery systems.66 The law provides support to transform the US health system from one that emphasises care of the ill to one that better emphasises promotion of health and wellness through broad initiatives that support communities in the creation of safe environments. The law includes coverage of recommended preventive services that health insurance has traditionally not covered, and requires the meaningful use of electronic health records. Opportunity now exists to advance injury prevention through screening and referral for injury risk factors such as depression, domestic violence (for women of child-bearing age), alcohol misuse, and behavioural problems (for children). As new evidence emerges, opportunity might arise for coverage for other types of screening such as for fall risk among older adults. Innovations in health information technology such as support for computerised clinical decision within electronic health records could enhance health providers’ ability to provide injury preventive services. For example, electronic health records could trigger alerts for screening on the basis of risk factors for patients, provide real-time information about evidence-based treatment guidelines, generate reports that share information about injury prevention with patients, or automate referrals to community services. Codes embedded within technology can show provision of services by providers, and allow practices to efficiently record and report clinical quality measures associated with clinical practice (eg, approved quality measures for assessment of fall risk in older adults) and facilitate reimbursement.
The Stopping Elderly Accidents, Deaths, and Injuries (STEADI) toolkit is based on a simple algorithm for fall assessment and individualised interventions, adapted from the 2010 American and British Geriatric Societies’ Clinical Practice Guidelines.67 The toolkit includes information about falls, theory-informed case studies, conversation starters, and standardised gait and balance assessments.68 Through collaboration with state health departments and use of clinical engagement and education sessions that incorporate quality improvement, STEADI is being integrated into clinical workflow and information technology systems to enhance uptake and adherence to its guidelines. Health departments support continuing education sessions in clinical settings that focus on implementation in combination with systems changes for fall assessment (eg, claims data review and incorporation into the electronic health record). Feedback based on collection of evaluation data is provided by technical-assistance providers, and is used to improve implementation and change the standard of care.
Screening, Brief Intervention, and Referral to Treatment (SBIRT) aims to integrate public health with clinical medicine to reduce morbidity and mortality due to alcohol-associated violence and injuries. SBIRT is used in clinical settings, particularly in primary care, to decrease risk for alcohol-misuse disorders. The implementation of SBIRT can be done by a range of health-care personnel and trained laypersons and provides opportunities to intervene with people who are classified as risky drinkers. SBIRT has been used successfully in emergency departments to identify, intervene with, and refer patients who either misuse alcohol or are alcohol dependent.69 This strategy has the potential to decrease the public health burden of alcohol misuse, along with its health and social results. For example, the use of SBIRT in trauma patients admitted to hospital decreased readmissions for subsequent injuries.70,71 In emergency departments, the use of SBIRT with at-risk drinkers decreased total alcohol consumption and decreased adverse results.72 Panel 2 shows other examples that connect public health and clinical medicine.73–76
Supporting the science in injury and violence prevention
Although the USA has made great progress to reduce the burden of injuries over the past 20 years, more will need to be done for the science and practice of injury and violence prevention to grow.77 Enough evidence exists to support action, but gaps still exist in understanding of the burden for some forms of injuries and violence, specific injury causes, some effective prevention strategies, and mechanisms for translation of research into practice.78 Enhancement of injury and violence surveillance systems is needed to allow more timely and accurate data to monitor trends and evaluate the effects of prevention initiatives. Important gaps remain in the aetiological research that serves as the foundation for the development of novel prevention strategies. One important topic is the need to understand the modifiable factors that assist young people to overcome personal, relationship, and environmental challenges and to buffer against injury risks.79 This type of research can help understanding of why individuals are injured and the factors within communities, families, and schools that serve to protect individuals from injury.
Promising strategies (such as policy and community level change initiatives with the potential to enhance population-level safety) need to be rigorously assessed for their effectiveness and return on investment. A crucial need also exists to assess programmes that are used widely, but for which effectiveness has not yet been shown. Research evidence that indicates effectiveness for these strategies can enhance their momentum, whereas evidence that indicates little, no, or harmful effects can prevent waste of resources. Researchers should develop interventions with dissemination in mind so that they can be efficiently scaled-up to the population to have the greatest health effect.80 Research efforts might focus on interventions that target risk factors for multiple forms of injury and violence, such as excessive alcohol consumption, and determine their corresponding effect on injury outcomes. For example, the Community Preventive Services Task Force has recommended actions such as dram-shop liability (holding owners or servers at retail alcohol establishments responsible for alcohol related harms), increases in alcohol taxes, regulation of alcohol-outlet density for the general population, and enhanced enforcement of laws prohibiting sales to underage individuals; these strategies might serve as leverage points for policy change that affects whole communities.81 For prevention strategies that are known to be effective and can be efficiently scaled up, dissemination and implementation research is needed to understand how to increase adoption and compliance, overcome the barriers to implementation, and build capacity for sustainability.82
Conclusion
Greater success in the USA is possible through public health and medical practice working together to frame injuries and violence as preventable, identify cost-effective and evidence-based interventions, provide evidence to decision makers, and strengthen the capacity of the health-care system.83 Clinical medicine and public health partnerships can help to ensure that life is not stopped by a preventable injury and that thousands are spared the debilitating effects of a car crash, non-fatal drowning, severe burn, fall, or assault. Effective interventions to prevent injuries and violence are available; effort to make them more salient and implementable will widen their adoption and effect.
Key messages.
In the first three decades of life, more people in the USA die from injuries and violence than from any other cause
Injuries and violence take an enormous economic toll on the USA, including the cost of medical care and lost productivity; they are preventable and have been linked to a wide range of physical, mental health, and reproductive health problems, and chronic diseases
For all ages, the five largest causes of injury deaths are motor-vehicle crashes, poisoning, falls, firearm suicides, and firearm homicides
Injury and violence-prevention strategies include education, behavioural changes, policy, engineering, and environmental supports; they have a positive return on investment and can be supported through use of communication framing theory, sharing of success stories, and provision of data to decision makers
Systems must be in place to allow the widespread adoption of effective strategies for injury and violence prevention and to bridge the gap between research and practice
Professionals in public health must work in partnership with those in clinical medicine to ensure that health delivery systems are well integrated and perform effectively, efficiently, and equitably to prevent injuries and violence and to improve outcomes
Continuing investments for research and innovation are needed to achieve further reductions in injury and violence
Panel 1. Key statistics about the burden of injuries and violence in the USA.
The most frequent causes of unintentional injury death in 2010 were motor-vehicle crashes (33 687 people), poisoning (33 041), falls (26 009), suffocation (6165), drowning (3782), and fire (2845). 1
Among non-fatal injuries, falling was the largest cause seen in emergency departments, causing more than 9 million visits in 2010. 1
Although the number of miles travelled by vehicles on roads in the USA increased by 8.5% between 2000 and 2009, the death rate related to that travel fell from 14·9 deaths per 100 000 to 11.0 deaths, and the injury rate decreased from 1130 to 722; among children, the number of pedestrian deaths decreased by 49% and the number of bicyclist deaths reduced by 58%. 13
Unintentional injury death is the largest cause of potential life-years lost before age 65 years. 1
The US Centers for Disease Control and Prevention1 estimated that the medical costs of unintentional injuries in 2010 were US$81.6 billion;1 by comparison, the medical costs associated with HIV infection in 2010 were about $12.6 billion. 14
Findings from the National Survey of Drug Use and Health indicate that 1 million adults in the USA attempt suicide every year. 15
In a national survey, nearly 12 million men and women reported being a victim of rape, physical violence, or stalking by an intimate partner in the previous 12 months. 12
Over their lifetime, one in five women in the USA has been raped, one in six has been stalked, and one in four has experienced severe physical violence from an intimate partner (eg, hit with a fist or an hard object, kicked, beaten, burned, or had a knife or gun used against them). 12
US state and local child protective services receive about 3·4 million reports of child maltreatment every year;16 studies not by child protective services estimate that one in five children in the USA have experienced some form of child maltreatment in their lifetime. 17–19
The economic cost of child maltreatment is substantial; the total lifetime costs of child maltreatment (including health care, child welfare, criminal justice, and the value of lost future productivity and earnings) are $124 billion a year. 20
Panel 2. Examples that connect public health with clinical medicine.
Child unintentional injury: provision of public health safety information in clinical settings
The Johns Hopkins Center for Injury Research and Policy has established child safety centres next to children’s hospitals and medical clinics. The centres are open to all community members; however, physicians can also refer families directly. These centres provide safety information and personalised injury-prevention services such as car safety-seat checks and installations. Educational information is provided, and safety products are offered at a discounted price, such as carbon monoxide alarms, smoke alarms, cabinet latches, and stair gates. Visiting families showed higher rates of safety practices than did other families.73 Child safety centres serve as a model for other children’s hospitals and health clinics in the US.
Traumatic brain injury: use of surveillance data to develop and evaluate clinical prevention plans
As part of the core injury programme from the Centers for Disease Control and Prevention, state public health departments collect data from hospitals and use vital statistics to examine trends and identify the most common causes of traumatic brain injury. States are using these clinical data to develop a prevention action plan on the basis of burden and evidence-based strategies. Surveillance measures can then be used to track trends and determine the effectiveness of identified strategies. For example, in Oregon surveillance for traumatic brain injury has shown that self-inflicted gunshot wounds to the head (by suicide) is the most common cause of traumatic brain injury death, and that falling is the largest cause visits to emergency departments and hospital admissions with traumatic brain injury. To reduce suicide among young people, the Oregon Injury and Violence Prevention Program (OIVPP) encourages health professionals to counsel parents of adolescents at risk of suicide to ensure their adolescents do not have unsupervised access to firearms. In addition, OIVPP works with health-care partners to use the Stopping Elderly Accidents, Deaths, and Injuries (STEADI) toolkit to assess fall risk in older adults and refer those at risk to evidence-based exercise programmes.
Prescription drug overdose: data sharing to improve prescribing and health
The Consistent Care Program in Washington State aims to reduce prescription drug overdoses through assuring the uniform application of evidence-based guidelines for opioid prescribing and managing drug-seeking patients and others that overuse emergency departments. Making use of an electronic medical records system called the Washington Emergency Department Information Exchange, the Consistent Care Program connects emergency departments with real-time records of a patient’s previous visits to state emergency departments, helping clinicians to understand use patterns of patients and avoid overprescribing opioids. Further, it enables care coordination by sharing care plans for patients, which helps to connect their emergency department clinicians with primary care providers. The programme can monitor drug-seeking patterns of patients and inform other population-level intervention strategies. Coupled with other state-level public health activities such as the Washington state programme for monitoring prescription drugs, it is another clinical decision-support method to help best practice across health-care settings.
Community violence: use of clinical data to inform public health strategies for prevention
In the UK’s Cardiff Violence Prevention Programme, health services, law enforcement, and local government partnered to regularly share aggregated, anonymous information about assault-related injuries treated in emergency departments. These clinical data, not traditionally brought to the attention of law enforcement, informed targeted policing and guided other violence-prevention policies and strategies that could improve population health. This model resulted in large and sustained reductions in assault-related injuries recorded by police or hospitals relative to comparison cities and provided about £82 in benefit for each £1 spent.74,75
Child maltreatment: clinical risk factors and prevention strategies
Safe Environment for Every Kid (SEEK) aimed to enhance paediatric primary care and address major risk factors for child maltreatment. This model includes training of residents (junior doctors) to address targeted risk factors; a brief parent-screening questionnaire that asks about safety in the home, exposure to second-hand smoke, depression, stress, substance misuse, partner violence, and child physical and sexual abuse; and a resident social worker team to address concerns. Findings from a randomised control trial 76 to compare SEEK with standard paediatric care showed that SEEK resulted in significantly fewer reports to child protective services, fewer instances of possible medical neglect, fewer children with delayed immunisations, and less harsh punishment reported by parents. The SEEK model is a potentially promising strategy to prevent child maltreatment.76
Acknowledgments
The conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention. We thank Rosemary Bretthauer-Mueller, Norm Alexander, and Margaret deNeergaard of the CDC for assistance in developing figure 1, and thank J Lee Annest and Erin Sullivan of the CDC for providing statistical data for cost of injury.
Footnotes
Contributors
All authors participated in the search of published work and wrote sections of the report. All authors revised subsequent drafts of the Series paper and approved its final version.
Declaration of interests
We declare no competing interests.
References
- 1.Centers for Disease Control and Prevention. [accessed Feb 19, 2013];Web-based Injury Statistics Query and Reporting System (WISQARS) http://www.cdc.gov/ncipc/wisqars.
- 2.Girasek DC. Public beliefs about the preventability of unintentional injury deaths. Accid Anal Prev. 2001;33:455–65. doi: 10.1016/s0001-4575(00)00059-2. [DOI] [PubMed] [Google Scholar]
- 3.Torell U, Bremberg S. Unintentional injuries: attribution, perceived preventability, and social norms. J Safety Res. 1995;26:63–73. [Google Scholar]
- 4.Ikeda R. Injury prevention and lifestyle medicine. Am J Lifestyle Med. 2010;4:5. [Google Scholar]
- 5.Dellinger AM, Chen J, Vance A, Breiding MJ, Simon T, Ballesteros MF. Injury prevention counseling for adults: have we made progress? Fam Community Health. 2009;32:115–22. doi: 10.1097/FCH.0b013e31819946e7. [DOI] [PubMed] [Google Scholar]
- 6.Yarnall KS, Pollak KI, Østbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93:635–41. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adams WG, Mann AM, Bauchner H. Use of an electronic medical record improves the quality of urban pediatric primary care. Pediatrics. 2003;111:626–32. doi: 10.1542/peds.111.3.626. [DOI] [PubMed] [Google Scholar]
- 8.Sleet DA, Dahlberg LL, Basavaraju SV, Mercy JA, McGuire LC, Greenspan A. Injury prevention, violence prevention, and trauma care: building the scientific base. MMWR Surveill Summ. 2011;60(suppl):78–85. [PubMed] [Google Scholar]
- 9.Scheier M, Carver C. Effects of optimism on psychological and physical well-being: Theoretical overview and empirical update. Cognit Ther Res. 1992;16:201–28. [Google Scholar]
- 10.Shakur H, Roberts I, Piot P, Horton R, Krug E, Mersch J. A promise to save 100 000 trauma patients. Lancet. 2012;380:2062–63. doi: 10.1016/S0140-6736(12)62037-6. [DOI] [PubMed] [Google Scholar]
- 11.Shiffman J, Smith S. Generation of political priority for global health initiatives: a framework and case study of maternal mortality. Lancet. 2007;370:1370–79. doi: 10.1016/S0140-6736(07)61579-7. [DOI] [PubMed] [Google Scholar]
- 12.Black M, Basile KC, Breiding MJ, et al. The National Intimate Partner and Sexual Violence Survey: 2010 summary report. National Center for Injury Prevention and Control; Atlanta: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 13.Centers for Disease Control and Prevention. Ten great public health achievements–United States, 2001–2010. MMWR Morb Mortal Wkly Rep. 2011;60:619–23. [PubMed] [Google Scholar]
- 14.Owusu-Edusei K, Jr, Chesson HW, Gift TL, et al. The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sex Transm Dis. 2013;40:197–201. doi: 10.1097/OLQ.0b013e318285c6d2. [DOI] [PubMed] [Google Scholar]
- 15.Crosby AE, Han B, Ortega LA, Parks SE, Gfroerer J. Suicidal thoughts and behaviors among adults aged ≥18 years—United States, 2008–2009. MMWR Surveill Summ. 2011;60:1–22. [PubMed] [Google Scholar]
- 16.US Department of Health and Human Services, Administration on Children and Families, Administration on Children Youth and Families, Children’s Bureau. Child maltreatment 2011. Washington, DC: US Department of Health and Human Services; 2012. [Google Scholar]
- 17.Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: a comprehensive, national survey. Child Maltreat. 2005;10:5–25. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- 18.Finkelhor D, Turner H, Ormrod R, Hamby SL. Violence, abuse, and crime exposure in a national sample of children and youth. Pediatrics. 2009;124:1411–23. doi: 10.1542/peds.2009-0467. [DOI] [PubMed] [Google Scholar]
- 19.Theodore AD, Chang JJ, Runyan DK, Hunter WM, Bangdiwala SI, Agans R. Epidemiologic features of the physical and sexual maltreatment of children in the Carolinas. Pediatrics. 2005;115:e331–37. doi: 10.1542/peds.2004-1033. [DOI] [PubMed] [Google Scholar]
- 20.Fang X, Brown DS, Florence CS, Mercy JA. The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse Negl. 2012;36:156–65. doi: 10.1016/j.chiabu.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haegerich T, Dahlberg L. Violence as a public health risk. Am J Lifestyle Med. 2011;5:392–406. [Google Scholar]
- 22.Lyons RA, Finch CF, McClure R, van Beeck E, Macey S. The injury list of all deficits (load) framework--conceptualizing the full range of deficits and adverse outcomes following injury and violence. Int J Inj Contr Saf Promot. 2010;17:145–59. doi: 10.1080/17457300903453104. [DOI] [PubMed] [Google Scholar]
- 23.Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013;309:657–59. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (CDC) Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morb Mortal Wkly Rep. 2011;60:1487–92. [PubMed] [Google Scholar]
- 25.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–56. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 26.Teno J, Kiel DP, Mor V. Multiple stumbles: a risk factor for falls in community-dwelling elderly. A prospective study. J Am Geriatr Soc. 1990;38:1321–25. doi: 10.1111/j.1532-5415.1990.tb03455.x. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention (CDC) Fatalities and injuries from falls among older adults–United States, 1993–2003 and 2001–2005. MMWR Morb Mortal Wkly Rep. 2006;55:1221–24. [PubMed] [Google Scholar]
- 28.Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18:141–58. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 29.Menon DK, Schwab K, Wright DW, Maas AI for the Demographics and Clinical Assessment Working Group of the International and Interagency Initiative toward Common Data Elements for Research on Traumatic Brain Injury and Psychological Health. Position statement: definition of traumatic brain injury. Arch Phys Med Rehabil. 2010;91:1637–40. [Google Scholar]
- 30.Faul M, Xu L, Wald MH, Coronado VG. Traumatic brain injury in the United States: emergency department visits, hospitalizations, and deaths. National Center for Injury Prevention and Control; Atlanta: Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 31.Coronado VG, McGuire LC, Sarmiento K, et al. Trends in traumatic brain injury in the U.S. and the public health response: 1995–2009. J Safety Res. 2012;43:299–307. doi: 10.1016/j.jsr.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 32.McKee AC, Stern RA, Nowinski CJ, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. 2013;136:43–64. doi: 10.1093/brain/aws307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention (CDC) Vital signs: Unintentional injury deaths among persons aged 0–19 years–United States, 2000–2009. MMWR Morb Mortal Wkly Rep. 2012;61:270–76. [PubMed] [Google Scholar]
- 34.Danese A, Moffitt TE, Harrington H, et al. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. 2009;163:1135–43. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 36.Sachs-Ericsson N, Cromer K, Hernandez A, Kendall-Tackett K. A review of childhood abuse, health, and pain-related problems: the role of psychiatric disorders and current life stress. J Trauma Dissociation. 2009;10:170–88. doi: 10.1080/15299730802624585. [DOI] [PubMed] [Google Scholar]
- 37.Shonkoff JP, Garner AS for the Committee on Psychosocial Aspects of Child and Family Health, the Committee on Early Childhood, Adoption, and Dependent Care, and the Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 38.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and injury mortality: individual and neighbourhood determinants. J Epidemiol Community Health. 2000;54:517–24. doi: 10.1136/jech.54.7.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dahlberg L, Simon TR. Predicting and preventing violence: developmental pathways and risk. In: Lutzker JR, editor. Preventing volence: research and evidence-based intervention strategies. Washington, DC: American Psychiological Association; 2006. pp. 97–124. [Google Scholar]
- 40.ACIP. The Social Determinants of Injury. Nova Scotia: Atlantic Collaborative on Injury Prevention; 2012. [Google Scholar]
- 41.Cubbin C, Smith GS. Socioeconomic inequalities in injury: critical issues in design and analysis. Annu Rev Public Health. 2002;23:349–75. doi: 10.1146/annurev.publhealth.23.100901.140548. [DOI] [PubMed] [Google Scholar]
- 42.McClure R, Stevenson M, McEvoy S, editors. The scientific basis of injury prevention and control. Melbourne: IP Communications; 2004. [Google Scholar]
- 43.Doll LS, Bonzo SE, Mercy JA, Sleet D. Handbook of injury and violence prevention. New York: Springer; 2007. [Google Scholar]
- 44.Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–95. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zaza S, Briss P, Harris K. The Guide to community preventive services: what works to promote health? New York: Oxford University Press; 2005. [Google Scholar]
- 46.Zaza S, Sleet DA, Thompson RS, Sosin DM, Bolen JC for the Task Force on Community Preventive Services. Reviews of evidence regarding interventions to increase use of child safety seats. Am J Prev Med. 2001;21(suppl):31–47. doi: 10.1016/s0749-3797(01)00377-4. [DOI] [PubMed] [Google Scholar]
- 47.Dinh-Zarr TB, Sleet DA, Shults RA, et al. for the Task Force on Community Preventive Services. Reviews of evidence regarding interventions to increase the use of safety belts. Am J Prev Med. 2001;21(suppl):48–65. doi: 10.1016/s0749-3797(01)00378-6. [DOI] [PubMed] [Google Scholar]
- 48.Shults RA, Elder RW, Sleet DA, et al. for the Task Force on Community Preventive Services. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. Am J Prev Med. 2001;21(suppl):66–88. doi: 10.1016/s0749-3797(01)00381-6. [DOI] [PubMed] [Google Scholar]
- 49.Bilukha O, Hahn RA, Crosby A, et al. for the Task Force on Community Preventive Services. The effectiveness of early childhood home visitation in preventing violence: a systematic review. Am J Prev Med. 2005;28(suppl 1):11–39. doi: 10.1016/j.amepre.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 50.Hahn R, Fuqua-Whitley D, Wethington H, et al. for the Task Force on Community Preventive Services. Effectiveness of universal school-based programs to prevent violent and aggressive behavior: a systematic review. Am J Prev Med. 2007;33(suppl 1):S114–29. doi: 10.1016/j.amepre.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 51.Hahn RA, Bilukha O, Lowy J, et al. for the Task Force on Community Preventive Services. The effectiveness of therapeutic foster care for the prevention of violence: a systematic review. Am J Prev Med. 2005;28(suppl 1):72–90. doi: 10.1016/j.amepre.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 52.Centers for Disease Control and Prevention (CDC) CDC grand rounds: prescription drug overdoses—a U.S. epidemic. MMWR Morb Mortal Wkly Rep. 2012;61:10–13. [PubMed] [Google Scholar]
- 53.MacDonald J, Golinelli D, Stokes RJ, Bluthenthal R. The effect of business improvement districts on the incidence of violent crimes. Inj Prev. 2010;16:327–32. doi: 10.1136/ip.2009.024943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cook P, MacDonald J. Public safety through private action: an economic assessment of BIDs. Econ J (London) 2011;121:445–62. [Google Scholar]
- 55.Miller TR, Finkelstein AE, Zaloshnja E, Hendrie D. American Public Health Association. The cost of child and adolescent injuries and the savings from prevention. In: Liller KD, editor. Injury prevention for children and adolescents: research, practice, and advocacy. Washington, DC: American Public Health Association; 2006. [Google Scholar]
- 56.Carande-Kulis VG, Stevens J, Beattie BL, Arias I. The business case for interventions to prevent fall injuries in older adults. Inj Prev. 2010;16(suppl 1):A249. [Google Scholar]
- 57.Lee S, Aos S, Drake E, Pennucci A, Miller M, Anderson L. Return on investment: evidence-based options to improve statewide outcomes. Olympia: Washington State Institute for Public Policy; Apr, 2012. document no 12-04-1201. [Google Scholar]
- 58.Sogolow E, Sleet D, Saul J. Dissemination, implementation, and widespread use of injury prevention interventions. In: Doll LS, Bonzo SE, Mercy JA, Sleet D, editors. Handbook of injury and violence prevention. New York: Springer; 2007. pp. 493–510. [Google Scholar]
- 59.Wandersman A, Duffy J, Flaspohler P, et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41:171–81. doi: 10.1007/s10464-008-9174-z. [DOI] [PubMed] [Google Scholar]
- 60.Chorpita BF, Daleiden EL, Weisz JR. Identifying and selecting the common elements of evidence based interventions: a distillation and matching model. Ment Health Serv Res. 2005;7:5–20. doi: 10.1007/s11020-005-1962-6. [DOI] [PubMed] [Google Scholar]
- 61.Centers for Disease Control and Prevention. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤19 years—United States, 2001–2009. MMWR Morb Mortal Wkly Rep. 2011;60:1337–42. [PubMed] [Google Scholar]
- 62. [accessed March 18, 2013];Blueprints for Healthy Youth Development. http://www.colorado.edu/cspv/blueprints/
- 63.Pollack KM, Frattaroli S, Young JL, Dana-Sacco G, Gielen AC. Motor vehicle deaths among American Indian and Alaska Native populations. Epidemiol Rev. 2012;34:73–88. doi: 10.1093/epirev/mxr019. [DOI] [PubMed] [Google Scholar]
- 64.Health Resources and Services Administration. [accessed Feb 17, 2014];Maternal, Infant, and Early Childhood Home Visiting programme. http://mchb.hrsa.gov/programs/homevisiting.
- 65.Scutchfield FD, Pérez DJ, Monroe JA, Howard AF. New public health services and systems research agenda: directions for the next decade. Am J Prev Med. 2012;42(suppl 1):S1–S5. doi: 10.1016/j.amepre.2012.01.027. [DOI] [PubMed] [Google Scholar]
- 66.The Patient Protection and Affordable Care Act of 2010 (PL 111–48), as amended by the Health Care and Education Reconciliation Act of 2010 (PL 111–52), together referred to as the Affordable Care Act. USA, 2010.
- 67.The American Geriatrics Society and British Geriatric Society. AGS, ABS clinical practice guidelines: prevention of falls in older persons. New York: American Geriatrics Society; 2010. [Google Scholar]
- 68.Stevens JA, Phelan EA. Development of STEADI: a fall prevention resource for health care providers. Health Promot Pract. 2013;14:706–14. doi: 10.1177/1524839912463576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.D’Onofrio G, Degutis LC. Integrating project ASSERT: a screening, intervention, and referral to treatment program for unhealthy alcohol and drug use into an urban emergency department. Acad Emerg Med. 2010;17:903–11. doi: 10.1111/j.1553-2712.2010.00824.x. [DOI] [PubMed] [Google Scholar]
- 70.Gentilello LM, Rivara FP, Donovan DM, et al. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Ann Surg. 1999;230:473–80. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Neumann T, Neuner B, Weiss-Gerlach E, et al. The effect of computerized tailored brief advice on at-risk drinking in subcritically injured trauma patients. J Trauma. 2006;61:805–14. doi: 10.1097/01.ta.0000196399.29893.52. [DOI] [PubMed] [Google Scholar]
- 72.D’Onofrio G, Pantalon MV, Degutis LC, et al. Brief intervention for hazardous and harmful drinkers in the emergency department. Ann Emerg Med. 2008;51:742–50. e2. doi: 10.1016/j.annemergmed.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gielen AC, McDonald EM, Wilson ME, et al. Effects of improved access to safety counseling, products, and home visits on parents’ safety practices: results of a randomized trial. Arch Pediatr Adolesc Med. 2002;156:33–40. doi: 10.1001/archpedi.156.1.33. [DOI] [PubMed] [Google Scholar]
- 74.Florence C, Shepherd J, Brennan I, Simon T. Effectiveness of anonymised information sharing and use in health service, police, and local government partnership for preventing violence related injury: experimental study and time series analysis. BMJ. 2011;342:d3313. doi: 10.1136/bmj.d3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Florence C, Shepherd J, Brennan I, Simon TR. An economic evaluation of anonymised information sharing in a partnership between health services, police and local government for preventing violence-related injury. Injury Prev. 2013 doi: 10.1136/injuryprev-2012-040622. published online Sept 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dubowitz H, Feigelman S, Lane W, Kim J. Pediatric primary care to help prevent child maltreatment: the Safe Environment for Every Kid (SEEK) Model. Pediatrics. 2009;123:858–64. doi: 10.1542/peds.2008-1376. [DOI] [PubMed] [Google Scholar]
- 77.Sleet DA, Baldwin G, Marr A, et al. History of injury and violence as public health problems and emergence of the National Center for Injury Prevention and Control at CDC. J Safety Res. 2012;43:233–47. doi: 10.1016/j.jsr.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 78.National Center for Injury Prevention and Control. CDC Injury Research Agenda, 2009–2018. Atlanta: Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 79.Hall JE, Simon TR, Lee RD, Mercy JA. Implications of direct protective factors for public health research and prevention strategies to reduce youth violence. Am J Prev Med. 2012;43(suppl 1):S76–83. doi: 10.1016/j.amepre.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 80.Owen N, Goode A, Fjeldsoe B, Sugiyama T, Eakin E. Designing for dissemination of environmental and policy initiatives and programs for high-risk groups. In: Brownson R, Colditz G, Proctor E, editors. Dissemination and implementation research in health: translating science to practice. New York: Oxford University Press; 2012. pp. 114–27. [Google Scholar]
- 81.Sleet DA, Howat P, Elder R, Maycock B, Baldwin G, Shults R. Interventions to reduce impaired driving and traffic injury. In: Verster JC, Pandi-Perumal SR, Ramaekers JG, Gier JJ, editors. Drugs, driving and traffic safety. Basel: Birkhäuser Verlag AG; 2009. pp. 439–56. [Google Scholar]
- 82.Brownson RC, Colditz GA, Proctor EK. Dissemination and implementation research in health: translating science to practice. New York: Oxford University Press; 2012. [Google Scholar]
- 83.Sleet DA, Moffett DB. Framing the problem: injuries and public health. Fam Community Health. 2009;32:88–97. doi: 10.1097/01.FCH.0000347985.67681.9d. [DOI] [PubMed] [Google Scholar]