Abstract
There is high comorbidity between personality disorders and alcohol use disorders, which appears related to individual differences in underlying personality dimensions of behavioral undercontrol and affective dysregulation. Very little is known about how the DSM-5 Section III trait model of personality pathology relates to alcohol problems, however, or how the strength of the relationship between personality pathology and alcohol problems changes with age and across gender. The current study examined these questions in a sample of 877 participants using the General Assessment of Personality Disorder to assess general personality dysfunction, the Personality Inventory for DSM-5 to measure specific traits, and the Alcohol Use Disorder Identification Test to assess problematic alcohol use. Results demonstrated that general personality pathology (Criterion A) was significantly related to problematic alcohol use after controlling for age and gender effects. Further, two of the five higher-order personality trait domains (Criterion B), Antagonism and Disinhibition, remained significant predictors of problematic alcohol use after accounting for the influence of general personality pathology; however, general personality pathology no longer predicted hazardous alcohol use once Antagonism and Disinhibition were added into the model. Finally, these two specific traits interacted with age, such that Antagonism was a stronger predictor of AUDIT scores among older individuals and Disinhibition was a stronger predictor of alcohol problems among younger individuals. Findings support the general validity of this new personality disorder diagnostic system and suggest important age effects in the relationship between traits and problematic alcohol use.
Keywords: personality traits, alcohol use, DSM-5, personality pathology, five-factor model
Alcohol use disorders (AUDs) are highly comorbid with personality disorders (PDs) in both community and clinical samples (Morgenstern, Langenbucher, Labouvie, & Miller, 1997; Sher, Trull, Bartholow, & Vieth, 1999; Trull, Jahng, Tomko, Wood, & Sher, 2010), and this co-occurrence significantly exacerbates the deleterious social and health outcomes associated with either disorder alone (Hasin et al., 2011; Schuckit, 1985). The strongest and most consistent links reported in the literature have been found between externalizing-related personality pathology (i.e., antisocial personality disorder [ASPD] and borderline personality disorder [BPD]; Eaton et al., 2011) and AUDs (Grant et al., 2006; Jahng et al., 2011; Sher et al., 1999). This comorbidity is thought to relate to individual differences in underlying personality dimensions of behavioral undercontrol and affective dysregulation (Agrawal, Narayanan, & Oltmanns, 2013; Jahng et al., 2011; Kotov, Gamez, Schmidt, & Watson, 2010; Krueger et al., 2007; Lejuez et al., 2010; Littlefield & Sher, 2010; Ruiz et al., 2008), which serve as risk factors for both personality pathology and alcohol problems.
While prior studies have examined the relationship between alcohol problems and both categorical PD diagnoses and underlying dimensions of personality and its pathology (Sher et al., 1999), far less is known about the association between alcohol problems and the alternative model of PD diagnosis in DSM-5 Section III (American Psychiatric Association, 2013). This model was proposed in response to extensive criticism of the DSM’s longstanding categorical system of PDs for its failure to provide a structurally valid and clinically useful representation of personality pathology (e.g., Skodol et al., 2011; Widiger & Trull, 2007). In the DSM-5 Section III model, a distinction is drawn between general personality dysfunction and specific maladaptive personality traits, such that the presence of both are necessary for the diagnosis of a personality disorder. Specifically, for the diagnosis of a personality disorder, an individual must demonstrate at least moderate impairments in self and interpersonal functioning (Criterion A), which are intended to reflect the defining features shared across personality disorders (i.e., general personality pathology). Additionally, phenotypic variation in the expression of personality pathology is captured with relevant elevations from a system of 25 primary traits (i.e., facets) organized into five higher order domains (Criterion B). The aim of the new model is to provide increased validity by matching the empirical structure of PD, while also focusing attention on the trans-diagnostic features that likely align with the psychological and physiological mechanisms underpinning PD (Wright & Simms, in press). Distinct aspects of this model have rapidly been accruing support in the form of replicability of structure (Morey, Krueger, & Skodol, 2013; Wright, Thomas, et al., 2012), concurrent and criterion validity (Few et al., 2013; Fossati et al., 2013; Hopwood et al., 2012; Miller et al., 2013; Watson et al., 2013; Wright, Pincus, Hopwood, et al., 2012; Wright & Simms, 2014; Wright et al., 2013), longitudinal stability and prospective prediction (Wright et al., 2015), and ratings of clinical utility (Morey, Skodol, & Oldham, 2014) and usability (Zimmermann et al., 2014). However, despite the purported increased structural and predictive validity of the Section III model of personality pathology, there is a dearth of literature examining the relationship between specific personality traits and alcohol problems after accounting for general personality pathology.
We are aware of only one prior study examining the link between the DSM-5 trait model and alcohol problems (Few et al., 2013), but the researchers did not test whether specific personality traits demonstrated incremental validity when considered along with general personality dysfunction. Specifically, Few and colleagues (2013) examined the relationship between self-reported pathological traits as assessed by the Personality Inventory for DSM-5 (PID-5; Krueger, Derringer, Markon, Watson, & Skodol, 2012), clinician rated traits on the Personality Trait Rating Form (Bender et al., 2011), and alcohol problems as assessed by the Alcohol Use Disorder Identification Test (AUDIT; Saunders, Aasland, Babor, De La Fuente, & Grant, 1993) in 98 participants (aged 18–65 years) who were currently receiving mental health treatment. Results showed that PID-5 traits accounted for 15% of the variance in AUDIT scores with Antagonism being the strongest predictor (B = .30). In terms of clinician rated traits, these accounted for 21% of the variance, with Disinhibition being the strongest predictor (B = .31). Yet as noted above, this study did not examine whether these specific traits continued to predict alcohol misuse after accounting for the effect of general personality dysfunction. Knowledge about the incremental validity of specific personality traits in predicting alcohol problems above and beyond general personality dysfunction will inform both the assessment and treatment of these highly comorbid disorders.
Furthermore, the study conducted by Few et al. (2013) was not sufficiently powered to examine potential moderating effects of gender and age on the relationship between personality traits and alcohol problems. Although several studies show that AUDs decrease substantially in prevalence across the lifespan (Grant et al., 2004; Wu & Blazer, 2011) and are far less common in women than in men (Grant et al., 2004), very few studies have examined whether the strength of the relationship between personality pathology and alcohol problems changes with age or across genders (Agrawal et al., 2013; Widiger & Seidlitz, 2002). Importantly, no prior study has examined the moderating effects of gender and age on the relationship between DSM-5 Section III personality traits and alcohol problems.
The present study aims to extend this work by investigating whether specific personality traits provide additional information, beyond general personality dysfunction, in the prediction of alcohol problems in a sample of 877 participants. Based on prior research (Kotov et al., 2010; Ruiz et al., 2008; Sher, Grekin, & Williams, 2005), we hypothesized that the domains of Negative Affectivity, Antagonism, and Disinhibition and their facets would be related to alcohol problems in this large community sample. However, given that both normal range and pathological personality traits demonstrate substantial shared variance, we additionally examined the unique associations between the trait domains and alcohol problems, controlling for all other traits and general personality pathology. Past work examining the unique associations among the DSM-5 Section III traits and alcohol problems suggest that the significant associations might be limited to Antagonism and Disinhibition when controlling for other traits (Few et al., 2013). Therefore, we predicted that Disinhibition and Antagonism, but not Negative Affectivity, would continue to relate to alcohol problems after controlling for all other trait domains. We further hypothesized that these traits would demonstrate specific effects that predict harmful drinking after accounting for the influence of general personality dysfunction. Finally, given the significant decrease in the prevalence of alcohol problems across the lifespan, as well as the lower prevalence of alcohol misuse among women compared to men, we sought to test whether gender and age interacted with measures of personality pathology in the prediction of alcohol problems.
Method
Participants
Participants were recruited via online postings on Craigslist (48.5%) and a variety of websites with mental health content to complete an anonymous survey on surveymonkey.com. The only requirement for participation was to be at least 18 years of age. Respondents could elect to be included in a random drawing for a $100 e-gift card to Target.com (chance of winning: 1 in 100) by submitting their email address. (Email addresses were not linked to questionnaire data.) As participation was entirely online, participants could elect to stop filling out the questionnaires (i.e., discontinue participation) at any time. This paper includes only those participants who completed all of the measures relevant to this study (i.e., 877 of the 1,722 individuals who started the survey). To ensure data integrity, the IP addresses of respondents were reviewed and duplicate entries were removed from the database throughout the data collection phase; IP addresses were not retained beyond the data collection phase.
The final sample (N = 877) was composed of 77.2% females with a mean age of 36.24 (SD = 13.01; age range: 18–76). The majority of the sample (81.8%) reported their ethnicity as Caucasian. The remainder of the sample’s ethnic breakdown was as follows: approximately 8% Asian, 6% Black or African American, 4% American Indian or Alaskan Native, and less than 1% Native Hawaiian or other Pacific Islander. Furthermore, 9 % of the sample additionally identified as Hispanic or Latino. Thirty-nine percent of the sample reported that they were currently in mental health treatment (i.e., participating in psychotherapy and/or taking psychiatric medications).
Measures
General personality dysfunction was assessed using the General Assessment of Personality Disorders (GAPD; Livesley, 2006), which is a self-report questionnaire measuring core components of personality pathology as specified by Livesley’s (2003) adaptive failure model (i.e., failure to establish stable and integrated representations of self and others; lack of capacity for intimacy and affiliative relationships; inability to function adaptively in a social group) which bears a close similarity to the DSM-5 Section III’s Criterion A. The GAPD consists of 83 items rated on a 5-point response scale (1, Very unlike me, to 5, Very like me). This study used the GAPD total score in analyses (Cronbach’s α = .97).
Maladaptive personality traits were measured using the Personality Inventory for DSM-5 (PID-5; Krueger et al., 2012). The PID-5 is a 220-item self-report questionnaire that measures the proposed 25 DSM-5 personality traits on a 4-point response scale (0, Very false or often false, to 3, Very true or often true). This measure has 25 primary scales that load onto five higher-order dimensions: Negative Affectivity, Detachment, Antagonism, Disinhibition, and Psychotocism (Krueger et al., 2012). Internal consistency of the scales ranged from .75 to .94. To examine whether the PID-5 factor structure replicated in this independent sample, we subjected the 25 primary scales to an exploratory factor analysis (EFA) using maximum likelihood estimation and oblique Equamax rotation in Mplus 7 (Muthen & Muthen, 2012) and computed congruences with the resulting factors. Supplementary Table 1 presents rotated factor loadings and factor correlations. Congruence coefficients ranged from .89 (Disinhibition) to .96 (Antagonism) with loadings from Krueger et al. (2012) and from .92 (Negative Affectivity) to .97 (Antagonism) with loadings from Wright, Thomas, et al. (2012) indicating strong convergence with results in other large samples. Factor determinacies were uniformly high (range = .91–.94), thus factor score estimates were saved and used in all analyses using the PID-5 domains.
The Alcohol Use Disorder Identification Test (AUDIT; Saunders et al., 1993) is a 10-item self-report measure that assesses problematic alcohol use and related behavior in the past year (Kokotailo et al., 2004). Items assess quantity and frequency of drinking, problems related to drinking behavior, and symptoms of alcohol dependence. A total score was obtained by summing items, with higher scores reflecting more severe alcohol-related problems (Babor, de la Fuente, Saunders, & Grant, 1989). Problematic alcohol use (i.e., hazardous drinking) was defined by a score of 8 or higher on the AUDIT (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). Cronbach’s α for the AUDIT was .88.
Data Analysis
In order to test associations between components of the DSM-5 Section III PD model and hazardous drinking, we adopted two approaches. First, we used Pearson correlations to estimate the strength of associations as these provide results in a metric that is highly familiar to readers. Second, due to concerns about severe non-normality in the AUDIT scores (i.e., large proportion of zeros with significant positive skew; See Supplemental Figure 1), we treated these as counts, and modeled them as negative-binomial distributed in generalized linear models. The negative-binomial distribution performs well in accommodating certain patterns of count distributions that deviate from the basic Poisson (Atkins & Gallop, 2007; Cameron & Trivedi, 1998; Long, 1997; Wright, Pincus, & Lenzenweger, 2012). Negative-binomial regression is part of the generalized linear model, and uses a log link to estimate regression coefficients that are linear, but are not interpretable in the metric of the count scale being predicted. By exponentiating the regression coefficients they are rendered interpretable. Specifically, the exponentiated intercept is the estimated count for the outcome for an individual when all predictors have a value of 0.0. The exponentiated values for the remaining regression coefficient are interpreted as rate ratios (RRs), reflecting the proportional increase in the count per unit increase in the predictor. For instance, a RR of 1.5 means that there is a 50% increase in the predicted count per unit increase in the predictor. Personality dysfunction and traits were standardized prior to running generalized linear models so that resulting RRs could be interpreted relative to a one standard deviation increase in the predictors. Finally, following the univariate models, we ran a series of generalized linear models predicting AUDIT scores from demographics (including age and gender), general personality dysfunction, trait domains, and trait domains interacting with age and gender.
Results
Table 1 shows participant characteristics and descriptive statistics for the GAPD, PID-5, and AUDIT across hazardous (n=185) and non-hazardous drinkers (n=692) as defined by the AUDIT cutoff of ≥ 8. As expected, hazardous drinkers were both significantly younger and less likely to be married/living with a partner as compared to individuals who did not report hazardous drinking. There were no differences in education level or race across the groups, but there was a trend (p=05) for a greater number of females to be in the non-hazardous drinking group. Hazardous drinkers scored higher on general personality pathology as assessed by the GAPD, as well as on four of the five PID-5 domains (i.e., Negative Affectivity, Antagonism, Psychoticism, and Disinhibition). Hazardous and non-hazardous drinkers did not differ on levels of Detachment.
Table 1.
Participant characteristics and descriptive statistics for the General Assessment of Personality Disorders (GAPD), the Personality Inventory for DSM-5 (PID-5), and the Alcohol Use Disorders Identification Test (AUDIT) across drinking groups
| Total Sample (N=877) |
Hazardous Drinkers (N=185) |
Non-Hazardous Drinkers (N=692) |
|||
|---|---|---|---|---|---|
| Variable | M (SD)/ % | F/ χ2 | p-value | ||
| Age | 36.2 (13.0) | 32.0 (11.2) | 37.4 (13.2) | 25.9 | <.001 |
| Female Gender | 77.2% | 71.9% | 78.6% | 3.8 | .05 |
| Education | 5.7 (1.1) | 5.5 (1.0) | 5.7 (1.1) | 3.04 | .08 |
| Married/Living with Partner | 38.1% | 28.6% | 40.6% | 8.9 | <.01 |
| Non-Caucasian Race | 18.2% | 22.2% | 17.2% | 2.4 | .12 |
| GAPD | |||||
| General Personality Pathology | 2.6 (.7) | 2.7 (0.8) | 2.5 (0.7) | 12.7 | <.001 |
| PID-5 Domains | |||||
| Negative Affectivity | 1.4 (0.7) | 1.6 (0.7) | 1.4 (0.7) | 13.7 | <.001 |
| Detachment | 1.2 (0.7) | 1.2 (0.6) | 1.2 (0.6) | 0.2 | .65 |
| Antagonism | 0.9 (0.6) | 1.1 (0.7) | 0.8 (0.6) | 50.6 | <.001 |
| Psychoticism | 1.0 (0.7) | 1.2 (0.7) | 0.9 (0.6) | 29.3 | <.001 |
| Disinhibition | 1.0 (0.6) | 1.2 (0.6) | 0.9 (0.6) | 25.4 | <.001 |
| PID-5 Facets | |||||
| Anxiousness | 1.8 (0.8) | 1.9 (0.8) | 1.7 (0.9) | 3.1 | .08 |
| Emotional Lability | 1.4 (0.8) | 1.6 (0.7) | 1.4 (0.8) | 10.8 | <.01 |
| Separation Insecurity | 1.1 (0.8) | 1.3 (0.8) | 1.0 (0.8) | 18.9 | <.001 |
| Perseveration | 1.4 (0.8) | 1.5 (0.8) | 1.4 (0.8) | 3.3 | .07 |
| Submissiveness | 1.4 (0.8) | 1.4 (0.7) | 1.4 (0.8) | 1.2 | .27 |
| Suspiciousness | 1.2 (0.7) | 1.4 (0.7) | 1.2 (0.7) | 22.4 | <.001 |
| Rigid Perfectionism | 1.4 (0.9) | 1.5 (0.9) | 1.4 (0.9) | 3.6 | .06 |
| Depressivity | 1.2 (0.8) | 1.3 (0.8) | 1.1 (0.8) | 6.0 | <.02 |
| Anhedonia | 1.4 (0.8) | 1.5 (0.7) | 1.4 (0.8) | 0.5 | .50 |
| Withdrawal | 1.3 (0.8) | 1.3 (0.8) | 1.3 (0.8) | 0.6 | .44 |
| Restricted Affectivity | 1.1 (0.7) | 1.1 (0.7) | 1.1 (0.7) | 1.7 | .19 |
| Intimacy Avoidance | 0.9 (0.8) | 0.8 (0.7) | 0.9 (0.8) | 0.9 | .76 |
| Manipulativeness | 1.0 (0.8) | 1.3 (0.8) | 0.9 (0.7) | 37.8 | <.001 |
| Callousness | 0.5 (0.5) | 0.7 (0.7) | 0.5 (0.5) | 38.7 | <.001 |
| Deceitfulness | 0.8 (0.7) | 1.1 (0.7) | 0.7 (0.6) | 54.8 | <.001 |
| Grandiosity | 0.9 (0.6) | 1.1 (0.7) | 0.9 (0.6) | 24.0 | <.001 |
| Attention Seeking | 1.0 (0.8) | 1.3 (0.8) | 0.9 (0.7) | 43.3 | <.001 |
| Hostility | 1.3 (0.7) | 1.5 (0.7) | 1.2 (0.7) | 14.6 | <.001 |
| Distractibility | 1.3 (0.8) | 1.5 (0.7) | 1.3 (0.8) | 6.4 | <.02 |
| Impulsivity | 0.9 (0.7) | 1.1 (0.7) | 0.9 (0.7) | 24.8 | <.001 |
| Irresponsibility | 0.7 (0.6) | 0.9 (0.7) | 0.7 (0.6) | 29.2 | <.001 |
| Risk Taking | 1.1 (0.6) | 1.3 (0.6) | 1.0 (0.6) | 42.9 | <.001 |
| Unusual Beliefs/Experiences | 0.8 (0.7) | 1.0 (0.8) | 0.7 (0.6) | 32.2 | <.001 |
| Perceptual Dysregulation | 0.8 (0.6) | 1.0 (0.7) | 0.7 (0.6) | 30.3 | <.001 |
| Eccentricity | 1.4 (0.9) | 1.6 (0.9) | 1.3 (0.9) | 13.1 | <.001 |
| AUDIT | |||||
| Total Score | 4.9 (6.0) | 14.4 (6.4) | 2.4 (2.1) | 1763.4 | <.001 |
Note. The 25 facet scores of the PID-5 were standardized. RR = Rate ratio.
p< .05
p<.01
p<.001
Hazardous drinkers also scored significantly higher on most of the PID-5 facet scales related to Negative Affectivity, Disinhibition, Antagonism, and Psychoticism, compared to non-hazardous drinkers (i.e., attention seeking, callousness, deceitfulness, depressivity, distractibility, eccentricity, emotional lability, grandiosity, hostility, impulsivity, irresponsibility, manipulativeness, perceptual dysregulation, risk taking, separation insecurity, suspiciousness, and unusual beliefs). Scores were similar across hazardous and non-hazardous drinkers on Detachment related scales (i.e., anhedonia, anxiousness, intimacy avoidance, perseveration, restricted affectivity, rigid perfectionism, submissiveness, and withdrawal). Additionally, Table 2 displays bivariate correlations and rate ratios between personality variables and AUDIT total score. As can be seen, both the GAPD and most PID-5 scales were significantly related to AUDIT total score.
Table 2.
Correlations and Rate Ratios (RRs) of Personality Variables with AUDIT Total Score
| Variable | r | RR |
|---|---|---|
| General Pers Pathology | .18*** | 1.31*** |
| Trait Domains | ||
| Negative Affectivity | .16*** | 1.33** |
| Antagonism | .30*** | 1.70*** |
| Detachment | .07 | 1.13* |
| Psychoticism | .25*** | 1.53*** |
| Disinhibition | .25*** | 1.66*** |
| Primary Traits | ||
| Anxiousness | .09* | 1.12** |
| Emotional Lability | .16*** | 1.23*** |
| Separation Insecurity | .17*** | 1.21*** |
| Perseveration | .10** | 1.13** |
| Submissiveness | .08* | 1.11** |
| Suspiciousness | .19*** | 1.26*** |
| Rigid Perfectionism | .09** | 1.13** |
| Depressivity | .12*** | 1.15*** |
| Anhedonia | .06 | 1.09* |
| Withdrawal | .06 | 1.08* |
| Restricted Affectivity | .09** | 1.12** |
| Intimacy Avoidance | .04 | 1.05 |
| Manipulativeness | .25*** | 1.31*** |
| Callousness | .30*** | 1.34*** |
| Deceitfulness | .31*** | 1.40*** |
| Grandiosity | .23*** | 1.28*** |
| Attention Seeking | .26*** | 1.32*** |
| Hostility | .19*** | 1.26*** |
| Distractibility | .13*** | 1.20*** |
| Impulsivity | .23*** | 1.31*** |
| Irresponsibility | .28*** | 1.35*** |
| Risk Taking | .26*** | 1.38*** |
| Unusual Beliefs/Experiences | .25*** | 1.30*** |
| Perceptual Dysregulation | .27*** | 1.32*** |
| Eccentricity | .17*** | 1.23** |
Note. N = 877.
p< .05
p<.01
p<.001
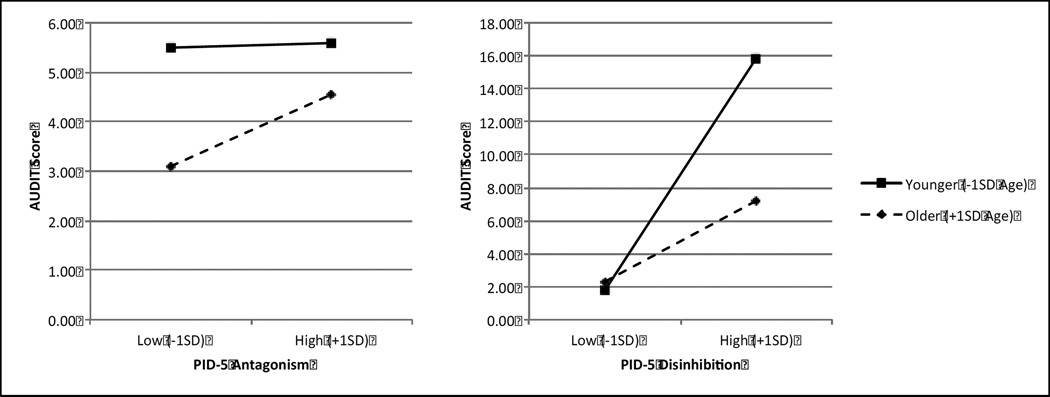
Table 3 shows results of generalized linear models predicting AUDIT scores from demographic and personality variables. In the first model, younger age and male gender were significantly related to higher AUDIT scores; however, current mental health treatment status (yes/no) was not. Increased general personality pathology predicted higher AUDIT scores in the second model, and age and gender remained significant in this model. Further, current mental treatment status predicted higher AUDIT scores with participants receiving treatment reporting higher AUDIT scores than participants not receiving treatment. In the third model, which also included the five specific domains of the PID-5, general personality pathology no longer significantly predicted AUDIT, but the specific traits of Antagonism and Disinhibition were predictive. In addition, gender dropped from being significant (age remained so). Further, although Negative Affectivity and Psychoticism were associated with AUDIT scores at the zero-order level, these associations were no longer significant in the multivariate regression models. In the fourth and final model, which included interaction terms between personality and age and personality and gender, we found significant interactions between Antagonism and age as well as Disinhibition and age. Specifically, Antagonism was a significant predictor of increased AUDIT scores among older individuals rather than younger individuals; although neither group reported hazardous drinking on the AUDIT. Disinhibition retained a main effect regardless of age but was a stronger predictor of hazardous alcohol use among youth, with a diminishing effect as individuals aged (See Figure 1). There were no interaction effects between personality and gender in the prediction of AUDIT scores.
Table 3.
Summary of Generalized Linear Models for Variables Predicting AUDIT (N = 877)
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | B | SE | RR | B | SE | RR | B | SE | RR | B | SE | RR |
| Intercept | 2.15*** | 0.12 | 8.58 | 1.50*** | 0.20 | 4.48 | 2.03*** | .31 | 7.61 | 1.87*** | .32 | 6.49 |
| Age | −0.02*** | 0.00 | 0.98 | −0.02*** | 0.00 | 0.98 | −0.01*** | 0.00 | 0.99 | −0.01** | 0.00 | 0.99 |
| Gender | 0.48*** | 0.09 | 0.63 | 0.35*** | 0.10 | 0.69 | 0.18 | 0.10 | 1.20 | 0.05 | 0.11 | 1.05 |
| Treatment Status (yes/no) | 0.13 | 0.08 | 1.14 | 0.21** | 0.08 | 1.24 | 0.19* | 0.08 | 1.21 | 0.19* | 0.09 | 1.21 |
| General Pers Pathology | 0.22*** | 0.05 | 1.25 | −0.08 | 0.12 | 0.92 | −0.05 | 0.12 | 0.95 | |||
| Negative Affect FS | 0.06 | 0.07 | 1.06 | 0.03 | 0.15 | 1.03 | ||||||
| Antagonism FS | 0.19*** | 0.05 | 1.21 | −0.22 | 0.16 | 0.80 | ||||||
| Detachment FS | −0.04 | 0.06 | 0.96 | −0.14 | 0.16 | 0.87 | ||||||
| Psychoticism FS | 0.09 | 0.05 | 1.09 | −0.16 | 0.16 | 0.85 | ||||||
| Disinhibition FS | 0.24*** | 0.05 | 1.27 | 0.77*** | 0.16 | 2.16 | ||||||
| Age × Negative Affect | 0.00 | 0.00 | 1.00 | |||||||||
| Age × Antagonism | 0.01* | 0.00 | 1.01 | |||||||||
| Age × Detachment | 0.00 | 0.00 | 1.00 | |||||||||
| Age × Psychoticism | 0.01 | 0.00 | 1.01 | |||||||||
| Age × Disinhibition | −0.02** | 0.01 | 0.98 | |||||||||
| Gender × Negative Affect | −0.05 | 0.12 | 0.95 | |||||||||
| Gender × Antagonism | 0.12 | 0.14 | 1.13 | |||||||||
| Gender × Detachment | 0.09 | 0.12 | 1.09 | |||||||||
| Gender × Psychoticism | 0.09 | 0.14 | 1.09 | |||||||||
| Gender × Disinhibition | 0.06 | 0.12 | 1.06 | |||||||||
Note: Age was centered at its mean.
p<.05
p<.01
p<.001
Figure 1.
Plot of Antagonism and Disinhibition interactions with age.
Discussion
There is high comorbidity between PDs and AUDs (e.g., Trull et al., 2010), which appears related to a common liability distribution unifying personality dimensions of behavioral undercontrol and affective dysregulation with alcohol problems (e.g., Jahng et al., 2011). Very little is known about how the DSM-5 Section III trait model of personality pathology relates to alcohol problems, however, or how the strength of the relationship between personality pathology and alcohol problems changes with age and across gender. To our knowledge, the current study is the first with adequate power to examine these questions. In a large sample, we showed that general personality pathology, operationalized similarly to Criterion A of the DSM-5 Section III model of personality dysfunction, was significantly related to problematic alcohol use after controlling for age and gender effects. Further, we demonstrated that two of the five higher-order domains (Criterion B), Antagonism and Disinhibition, remained significant predictors of problematic alcohol use after accounting for the influence of general personality pathology and all other trait domains.
The current results support the validity of the Criterion B trait model, in so far as they replicate prior work underscoring the importance of trait Disinhibition and Antagonism in the prediction of hazardous alcohol use (e.g., Creswell et al., in press; Few et al., 2013; Kotov et al., 2010; Read, Merrill, Griffin, Bachrach, & Khan, 2014; Ruiz et al., 2008). Notably, these same dimensions are also implicated in various PD diagnoses, including ASPD and BPD (Few et al., 2013; Hopwood et al., 2012; Samuel & Widiger, 2008). Indeed, growing research suggests that the comorbidity between AUDs and these PDs is attributable to common etiological processes with early expression of impaired impulse control (Sher & Trull, 2002).
However, although a large body of prior work (Kotov et al., 2010; Ruiz et al., 2008; Sher et al., 2005) supports a strong relationship between negative emotionality and problematic alcohol use, we did not find unique effects of Negative Affectivity in the multivariate regression models. Although our findings may seem discrepant with prior work, it is important to recognize that in much of the published literature the relationship between alcohol and trait domains is investigated univariately as opposed to controlling for shared variance among traits. This approach is often defended theoretically based on assumptions of trait orthagonality, despite the fact that in practice trait domains share considerable variance, especially those targeting the domains of affective, interpersonal, and behavioral regulation (DeYoung, 2006; Digman, 1997). Thus, it is understandable that Negative Affectivity is related to AUDIT scores in isolation, whereas in the context of multivariate models alongside Disinhibition and Antagonism, Negative Affectivity is no longer a significant predictor (see also Creswell et al., in press). An alternative perspective on this issue comes from the latent structure of psychopathology, which suggests that problematic alcohol use is related to Internalizing disorders, but primarily (if not exclusively) through the shared variance with other Externalizing pathology (e.g., Krueger & Markon, 2006; Wright & Simms, in press).
As noted above, despite a significant zero-order association between general personality pathology and AUDIT scores, general personality pathology no longer predicted hazardous alcohol use once Antagonism and Disinhibition were added into the models. This is consistent with previous findings, in which early models of Criterion A failed to increment the Criterion B traits in the prediction of Section II PD symptom counts (Hopwood et al., 2012; Few et al., 2013). However, the DSM-5 traits, as pathological or maladaptive variants of basic trait domains, are by design inherently psychometrically redundant with Criterion A (Wright, 2011). The lack of relationship between general personality pathology and alcohol problems after controlling for Disinhibition and Antagonism attests to the specific, and incremental, relevance of these two trait domains for understanding problematic alcohol use.
Results also showed that the strength of the relationships between traits and problematic alcohol use varied with age. Specifically, findings indicated that Antagonism was a stronger predictor of alcohol use among older relative to younger individuals, but this finding is not clinically significant, as the effect is not in the range of hazardous drinking levels. Furthermore, we are unaware of prior work that has observed a similar finding, suggesting caution in interpretation. More importantly, results showed that Disinhibition was a stronger predictor of alcohol problems among younger relative to older individuals. Indeed, younger individuals with elevated trait Disinhibition reported very high AUDIT scores (~16.0) compared to older individuals with similarly high Disinhibition (~2.0). These results are consistent with longitudinal studies suggesting that increased Disinhibition often precedes problem drinking (e.g., Caspi, Begg, Dickson, Harrison, Langley, Moffit, & Silva, 1997; Schuckit, 1998; Sher, Bartholow, & Wood, 2000) and highlight the importance of assessing Disinhibition in young adult drinkers to identify those at particular risk for AUDs.
Our findings are also consistent with a small number of prior studies that have found null results when studying the association between impulsivity/lack of constraint and alcohol problems in older samples (e.g., Cloninger et al., 1995; LoCastro et al., 2000). Taken together, these results raise interesting questions about the mechanisms underlying this attenuation in association between Disinhibition and alcohol problems with increasing age. One possibility is that older people may not be as impulsive in general, as there are normative declines in impulsivity across the life course with concurrent increases in traits antithetic to impulsivity (i.e., conscientiousness and constraint; Blonigen, 2010; Roberts, Walton, & Viechtbauer, 2006). Indeed, in our sample, individuals older than the median age of 33 reported significantly lower Disinhibition scores than those younger than the median age. Another possibility is that with shifting social roles as individuals age, even the more disinhibited participants are constrained by their responsibilities, surroundings, and relationships, such that they cannot engage in problematic alcohol use at nearly the levels seen in younger participants (Roberts & Wood, 2006). Alternatively, it may be that our sampling method missed individuals whose disinhibition at younger ages has now led to more severe AUDs. Regardless of the precise mechanisms, these findings point to the need for future studies to examine personality pathology and alcohol misuse within a developmental framework in order to understand patterns of stability and change in the association between alcohol misuse and personality dysfunction (Agrawal et al., 2013; Vergés, Jackson, Bucholz, Grant, Trull, Wood, & Sher, 2012).
Although this study is the first with sufficient power to examine the relationship between a trait model of personality pathology and problematic alcohol use and the influence of age and gender on these associations, there are limitations. First, this is a cross-sectional study, and therefore we cannot draw definitive conclusions regarding the directionality of effects between personality pathology and alcohol misuse. Future studies using longitudinal designs will help to tease apart the temporal ordering of effects. Second, we rely on survey data collected online, and we do not have corroborating reports from informants or clinicians to validate respondents’ personality and alcohol use data. Third, the sample includes relatively young drinkers who were recruited anonymously through Craigslist, which may limit the generalizability of the findings. Indeed, when interpreting age effects using a cross-sectional sample, one must be mindful of cohort effects. Fourth, the sample contained a higher percentage of females than males, which could be problematic given known gender differences in the rates of externalizing disorders (Eaton et al., 2012). Studies that recruit equal numbers of males and females are warranted and may be better able to detect moderation effects of gender in the relationship between personality traits and problematic alcohol use. Finally, due to concerns about response burden, the AUDIT was the only alcohol-related measure included in this study. Studies that include other alcohol measures (e.g., quantity and frequency of alcohol use) and assessments of other substance use disorders are needed.
In sum, this study demonstrates that specific facets of personality pathology continue to be strong predictors of problematic alcohol use even after accounting for the influence of general personality pathology. Moreover, the current study highlights the notion that this relationship is fluid and developmentally contextualized, as the strength between personality traits and hazardous drinking differed according to age. Findings underscore the need for future studies to prospectively examine how the association between personality and alcohol misuse changes over time.
Supplementary Material
Acknowledgments
This study was supported by grants K23 MH080221 (Pinto), K08DA029641 (Ansell), and F31AA022272 (Bachrach).
References
- Agrawal A, Narayanan G, Oltmanns TF. Personality pathology and alcohol dependence at midlife in a community sample. Personality Disorders: Theory, Research, and Treatment. 2013;4(1):55–61. doi: 10.1037/a0030224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: Author; 2013. [Google Scholar]
- Atkins DC, Gallop RJ. Rethinking how family researchers model infrequent outcomes: A tutorial on count regression and zero- inflated models. Journal of Family Psychology. 2007;21:726–735. doi: 10.1037/0893-3200.21.4.726. [DOI] [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. Geneva: WHO/MNH/DAT 89.4, World Health Organization; 1989. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. Geneva: WHO/MSD/MSB 01.6a, World Health Organization; 2001. [Google Scholar]
- Bender DS, Morey LC, Skodol AE. Toward a model for assessing level of personality functioning in DSM-5, Part I: A review of theory and methods. Journal of Personality Assessment. 2011;93:332–346. doi: 10.1080/00223891.2011.583808. [DOI] [PubMed] [Google Scholar]
- Blonigen DM. Explaining the relationship between age and crime: contributions from the developmental literature on personality. Clinical Psychology Review. 2010;31:89–100. doi: 10.1016/j.cpr.2009.10.001. [DOI] [PubMed] [Google Scholar]
- Cameron AC, Trivedi PK. Regression analysis of count data. Cambridge, United Kingdom: Cambridge University Press; 1998. [Google Scholar]
- Caspi A, Begg D, Dickson N, Harrington H, Langley J, Moffitt TE, et al. Personality differences predict health-risk behaviors in young adulthood: Evidence from a longitudinal study. J Pers Soc Psychol. 1997;73(5):1052–63. doi: 10.1037//0022-3514.73.5.1052. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Sigvardsson S, Przybeck TR, Svrakic DM. Personality antecedents of alcoholism in a national area probability sample. European archives of psychiatry and clinical neuroscience. 1995;245(4–5):239–244. doi: 10.1007/BF02191803. [DOI] [PubMed] [Google Scholar]
- Creswell KG, Chung T, Wright AGC, Black JJ, Clark DB, Martin CS. Personality, negative affect coping, and drinking alone: A structural equation modeling approach to examine correlates of adolescent solitary drinking. Addiction. in press doi: 10.1111/add.12881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeYoung CG. Higher-order factors of the Big Five in a multi-informant sample. Journal of personality and social psychology. 2006;91(6):1138. doi: 10.1037/0022-3514.91.6.1138. [DOI] [PubMed] [Google Scholar]
- Digman JM. Higher-order factors of the Big Five. Journal of personality and social psychology. 1997;73(6):1246. doi: 10.1037//0022-3514.73.6.1246. [DOI] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, Hasin DS. An invariant dimensional liability model of gender differences in mental disorder prevalence: evidence from a national sample. Journal of Abnormal Psychology. 2012;121(1):282–288. doi: 10.1037/a0024780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, Hasin DS. Borderline personality disorder co-morbidity: relationship to the internalizing-externalizing structure of common mental disorders. Psychological Medicine. 2011;41(05):1041–1050. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Few LR, Miller JD, Rothbaum AO, Meller S, Maples J, Terry DP, MacKillop J. Examination of the Section III DSM-5 diagnostic system for personality disorders in an outpatient clinical sample. Journal of Abnormal Psychology. 2013;122(4):1057–1069. doi: 10.1037/a0034878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossati A, Krueger RF, Markon KE, Borroni S, Maffei C. Reliability and Validity of the Personality Inventory for DSM-5 (PID-5) Predicting DSM-IV Personality Disorders and Psychopathy in Community-Dwelling Italian Adults. Assessment. 2013;20(6):689–708. doi: 10.1177/1073191113504984. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant B, Stinson F, Dawson D, Chou S, Ruan W, Pickering R. Co-Occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Alcohol Research & Health. 2006;29(2):121–130. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Hasin D, Fenton M, Skodol A, Krueger R, Keyes K, Geier T, Grant B. Personality disorders and the 3-year course of alcohol, drug, and nicotine use disorders. Archives of General Psychiatry. 2011;68(11):1158–1167. doi: 10.1001/archgenpsychiatry.2011.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Thomas KM, Markon KE, Wright AGC, Krueger RF. DSM-5 personality traits and DSM-IV personality disorders. Journal of Abnormal Psychology. 2012;121(2):424–432. doi: 10.1037/a0026656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahng S, Trull TJ, Wood PK, Tragesser SL, Tomko R, Grant JD, Sher KJ. Distinguishing general and specific personality disorder features and implications for substance dependence comorbidity. Journal of Abnormal Psychology. 2011;120(3):656–669. doi: 10.1037/a0023539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokotailo PK, Egan J, Gangnon R, Brown D, Mundt M, Fleming M. Validity of the Alcohol Use Disorders Identification Test in College Students. Alcoholism: Clinical and Experimental Research. 2004;28(6):914–920. doi: 10.1097/01.alc.0000128239.87611.f5. [DOI] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological Bulletin. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Derringer J, Markon KE, Watson D, Skodol AE. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychological Medicine. 2012;42(09):1879–1890. doi: 10.1017/S0033291711002674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual review of clinical psychology. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, Kramer MD. Linking antisocial behavior, substance use, and personality: An integrative model of the adult externalizing spectrum. Journal of Abnormal Psychology. 2007;116:645–666. doi: 10.1037/0021-843X.116.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Magidson JF, Mitchell SH, Sinha R, Stevens MC, de Wit H. Behavioral and biological indicators of impulsivity in the development of alcohol use, problems, and disorders. Alcoholism: Clinical and Experimental Research. 2010;34:1334–1345. doi: 10.1111/j.1530-0277.2010.01217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlefield AK, Sher KJ. The multiple distinct ways that personality contributes to alcohol use disorders. Social and Personality Compass. 2010;4:767–782. doi: 10.1111/j.1751-9004.2010.00296.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livesley WJ. Practical management of personality disorders. New York: Guilford Press; 2003. [Google Scholar]
- Livesley WJ. Differentiating normal and abnormal personality. 2nd ed. New York, NY, US: Springer Publishing Co; 2006. The Dimensional Assessment of Personality Pathology (DAPP) Approach to Personality Disorder; pp. 401–429. [Google Scholar]
- LoCastro J, Spiro A, Monnelly E, Ciraulo D. Personality, family history, and alcohol use among older men: The VA Normative Aging Study. Alcoholism: Clinical and Experimental Research. 2000;24(4):501–511. [PubMed] [Google Scholar]
- Long JS. Regression models for categorical and limited dependent variables. Thousand Oaks, CA: Sage Publications; 1997. [Google Scholar]
- Miller JD, Gentile B, Wilson L, Campbell WK. Grandiose and vulnerable narcissism and the DSM-5 pathological personality trait model. Journal of personality assessment. 2013;95(3):284–290. doi: 10.1080/00223891.2012.685907. [DOI] [PubMed] [Google Scholar]
- Morey LC, Krueger RF, Skodol AE. The hierarchical structure of clinician ratings of proposed DSM-5 pathological personality traits. Journal of Abnormal Psychology. 2013;122(3):836–841. doi: 10.1037/a0034003. [DOI] [PubMed] [Google Scholar]
- Morey LC, Skodol AE, Oldham JM. Clinician judgments of clinical utility: A comparison of DSM-IV-TR personality disorders and the alternative model for DSM-5 personality disorders. Journal of abnormal psychology. 2014;123(2):398. doi: 10.1037/a0036481. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Langenbucher J, Labouvie E, Miller KJ. The comorbidity of alcoholism and personality disorders in a clinical population: Prevalence and relation to alcohol typology variables. Journal of Abnormal Psychology. 1997;106(1):74–84. doi: 10.1037//0021-843x.106.1.74. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7th ed. Los Angeles, CA: Muthén and Muthén; 2012. [Google Scholar]
- Read JP, Merrill JE, Griffin MJ, Bachrach RL, Khan S. Posttraumatic stress and alcohol problems: Self-medication or trait vulnerability? The American Journal on Addictions. 2014;23:108–116. doi: 10.1111/j.1521-0391.2013.12075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Wood D. Personality development in the context of the Neo-Socioanalytic Model of personality. In: Mroczek D, Little T, editors. Handbook of Personality Development. Mahwah, NJ: Lawrance Erlbaum Associates; 2006. pp. 11–39. Chapter 2. [Google Scholar]
- Ruiz MA, Pincus AL, Schinka JA. Externalizing pathology and the five-factor model: A meta-analysis of personality traits associated with antisocial personality disorder, substance use disorder, and their co-occurrence. Journal of Personality Disorders. 2008;22(4):365–388. doi: 10.1521/pedi.2008.22.4.365. [DOI] [PubMed] [Google Scholar]
- Samuel DB, Widiger TA. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: A facet level analysis. Clinical Psychology Review. 2008;28:1326. doi: 10.1016/j.cpr.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. The clinical implications of primary diagnostic groups among alcoholics. Archives of General Psychiatry. 1985;42(11):1043–1049. doi: 10.1001/archpsyc.1985.01790340021003. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. Biological, psychological and environmental predictors of the alcoholism risk: A longitudinal study. Journal of Studies on Alcohol. 1998;59:485–494. doi: 10.15288/jsa.1998.59.485. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Bartholow BD, Wood MD. Personality and substance use disorders: A prospective study. Journal of Consulting and Clinical Psychology. 2000;68:818–829. [PubMed] [Google Scholar]
- Sher KJ, Grekin ER, Williams NA. The development of alcohol use disorders. Annual Review of Clinical Psychology. 2005;1:493–523. doi: 10.1146/annurev.clinpsy.1.102803.144107. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Trull TJ. Substance use disorder and personality disorder. Current Psychiatry Reports. 2002;4:25–29. doi: 10.1007/s11920-002-0008-7. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Trull TJ, Bartholow B, Vieth A. Psychological theories of drinking and alcholism. 2nd ed. New York: Plenum; 1999. Personality and alcoholism: issues, methods, and etiological processes; pp. 55–105. [Google Scholar]
- Skodol AE, Clark LA, Bender DS, Krueger RF, Morey LC, Verheul R, Oldham JM. Proposed changes in personality and personality disorder assessment and diagnosis for DSM-5 Part I: Description and rationale. Personality Disorders: Theory, Research, and Treatment. 2011;2(1):4–22. doi: 10.1037/a0021891. [DOI] [PubMed] [Google Scholar]
- Trull T, Jahng S, Tomko R, Wood P, Sher K. Revised NESARC personality disorder diagnoses: Gender, prevalence, and comorbidity with substance dependence disorders. Journal of Personality Disorders. 2010;24(4):412–426. doi: 10.1521/pedi.2010.24.4.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vergés A, Jackson KM, Bucholz KK, Grant JD, Trull TJ, Wood PK, Sher KJ. Deconstructing the age-prevalence curve of alcohol dependence: Why “maturing out” is only a small piece of the puzzle. Journal of Abnormal Psychology. 2012;121:511–523. doi: 10.1037/a0026027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Stasik SM, Ro E, Clark LA. Integrating normal and pathological personality: Relating the DSM-5 trait-dimensional model to general traits of personality. Assessment. 2013;20:312–326. doi: 10.1177/1073191113485810. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Seidlitz L. Personality, psychopathology, and aging. Journal of Research in Personality. 2002;36(4):335–362. [Google Scholar]
- Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: Shifting to a dimensional model. American Psychologist. 2007;62(2):71–83. doi: 10.1037/0003-066X.62.2.71. [DOI] [PubMed] [Google Scholar]
- Wright AGC. Quantitative and qualitative distinctions in personality disorder. Journal of Personality Assessment. 2011;93(4):370–379. doi: 10.1080/00223891.2011.577477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Calabrese WR, Rudick MM, Yam WH, Zelazny K, Rotterman J, Simms LJ. Stability of the DSM-5 Section III pathological personality traits and their longitudinal associations with functioning in personality disordered individuals. Journal of Abnormal Psychology. 2015;124(1):199–207. doi: 10.1037/abn0000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Hopwood CJ, Thomas KM, Markon KE, Krueger RF. An interpersonal analysis of pathological personality traits in DSM-5. Assessment. 2012;19(3):263–275. doi: 10.1177/1073191112446657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Lenzenweger MF. An empirical examination of distributional assumptions underlying the relationship between personality disorder symptoms and personality traits. Journal of Abnormal Psychology. 2012;121(3):699–706. doi: 10.1037/a0029042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Pincus AL, Thomas KM, Hopwood CJ, Markon KE, Krueger RF. Conceptions of Narcissism and the DSM-5 Pathological Personality Traits. Assessment. 2013;20(3):339–352. doi: 10.1177/1073191113486692. [DOI] [PubMed] [Google Scholar]
- Wright AGC, Simms LJ. On the structure of personality disorder traits: Conjoint analyses of the CAT-PD, PID-5, and NEO-PI-3 trait models. Personality Disorders: Theory, Research, and Treatment. 2014;5(1):43–54. doi: 10.1037/per0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Simms LJ. A metastructural model of mental disorders and pathological personality traits. Psychological Medicine. in press doi: 10.1017/S0033291715000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, Krueger RF. The hierarchical structure of DSM-5 pathological personality traits. Journal of Abnormal Psychology. 2012;121(4):951–957. doi: 10.1037/a0027669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG. Illicit and Nonmedical Drug Use Among Older Adults: A Review. Journal of Aging and Health. 2011;23(3):481–504. doi: 10.1177/0898264310386224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann J, Benecke C, Bender DS, Skodol AE, Schauenburg H, Cierpka M, Leising D. Assessing DSM-5 Level of Personality Functioning From Videotaped Clinical Interviews: A Pilot Study With Untrained and Clinically Inexperienced Students. Journal of personality assessment. 2014;96(4):397–409. doi: 10.1080/00223891.2013.852563. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.