Abstract
A 64-year-old woman presented with contralateral right adrenal metastasis with adrenal vein thrombus, which was diagnosed many years after left nephrectomy with adrenalectomy due to renal cell cancer. The patient underwent right adrenalectomy with adrenal vein tumor thrombectomy for treatment. The pathologic examination confirmed metastatic clear cell carcinoma. The remote but existing risk of developing contralateral adrenal metastasis (CAM) after primary radical nephrectomy supports the idea of sparing the adrenal gland in suitable patients who undergo radical nephrectomy. Contralateral adrenal metastasis from RCC is a rare finding with the potential benefit of cure after resection. Care must be taken in preoperative diagnostics, as this metastasis is capable of causing inferior vena cava tumor thrombus via the suprarenal venous route. According to our knowledge, our case is the second similar entity described in literature so far.
Keywords: adrenal metastasis, contralateral, renal cell carcinoma, tumor thrombus, adrenal vein
Abstract
U 64-letniej chorej stwierdzono przerzut do przeciwległego nadnercza wraz z obecnością czopu nowotworowego w żyle nadnerczowej, który został rozpoznany wiele lat po lewostronnej nefrektomii wraz z adrenalektomią, wykonanej z powodu raka nerkowokomórkowego. Pacjentka została poddana prawostronnej adrenalektomii z usunięciem czopa nowotworowego z żyły nadnerczowej. W badaniu histopatologicznym potwierdzono przerzut raka jasnokomórkowego. Ryzyko wystąpienia przerzutu do przeciwległego nadnercza po pierwotnej radykalnej nefrektomii istnieje, choć jest niewielkie, dlatego zasadne wydaje się zachowanie nadnercza w wybranej grupie chorych poddawanych radykalnej nefrektomii. Występowanie zmian wtórnych raka nerkowokomórkowego w przeciwległym nadnerczu jest rzadko spotykane, natomiast resekcja guza wiąże się z możliwością wyleczenia. Konieczna jest staranna diagnostyka przedoperacyjna w związku ze zdolnością przerzutu raka nerkowokomórkowego do tworzenia czopa nowotworowego w żyle głównej dolnej drogą żył nadnerczowych. Wedle wiedzy autorów niniejszy przypadek jest drugim tego rodzaju opisywanym dotąd w literaturze przedmiotu.
Introduction
Although renal cell cancer (RCC) may reach almost every organ to form metastases, the most common metastatic sites include the lungs, abdomen, bones and brain(1). Whereas metastases of RCC to different sites are not uncommon, contralateral adrenal gland is rarely involved. In one autopsy study of more than 400 patients who had undergone nephrectomy for RCC(2), the contralateral adrenal gland was the sole site of metastatic infiltration in only 2.5%. Among those with widespread RCC metastases identified in autopsy, the contralateral adrenal gland was involved in 12.7% of patients. In addition to being able to metastasize to numerous different organs, RCC can recur or metastasize many years after the removal of the primary tumor(3).
One of the unique forms of RCC growth is the ability to infiltrate the renal vein or even the vena cava, and propagate within the vessels to reach the right atrium in selected cases. It has been estimated that among those diagnosed with RCC, tumor thrombus is located in the renal vein or vena cava inferior (VCI) in approximately 10% of patients, including 1% of those with right atrium involvement(4).
We present the case of a metachronous contralateral adrenal metastasis of RCC with tumor thrombus located in the adrenal vein. According to our knowledge, our case is the second similar entity described in the literature of the subject so far(5).
Case report
A 47-year- old woman presented with a left-side renal mass detected incidentally in an ultrasound scan (USS). This lesion was further evaluated in computer tomography (CT) imaging of the abdomen, which revealed a solid 3-cm-in-diameter lesion in the upper pole of the left kidney without lymphadenopathy. Chest X-Ray (CXR) was normal and the creatinine level was 1.4 mg%. On the 6th of October 1994, she was subjected to left-side radical nephrectomy with adrenalectomy, performed without complications. The pathologic examination confirmed clear cell carcinoma G2 without metastases to the lymph nodes and the left adrenal gland. The lesion was classified as cRCC pT1aN0M0.
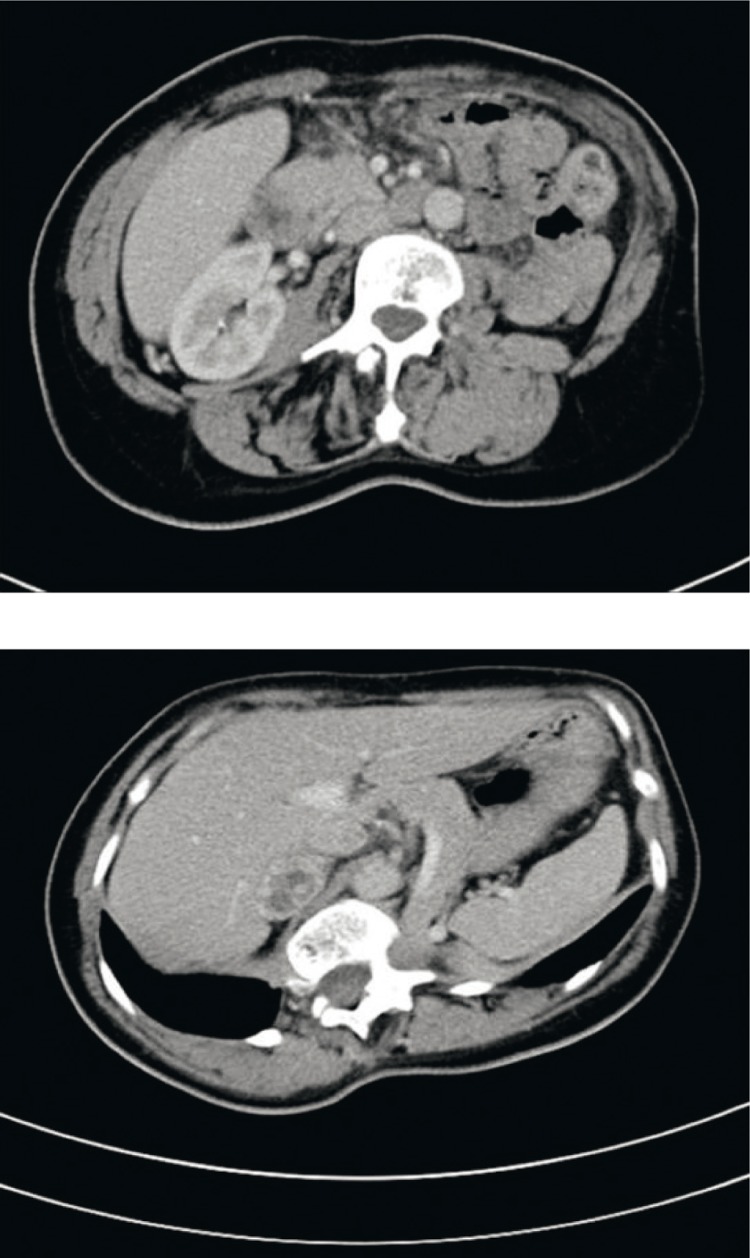
The patient was then followed up very strictly. One of the recent USS, conducted in January 2011, did not show any abnormalities, but the next one, performed in January 2012, revealed a solid 6x3cm lesion in the right adrenal gland (Fig. 1). A CT scan of the chest and abdomen was carried out on the 10th of January 2012, and revealed a metastasis in the lung, and confirmed a solid 41x21x30 mm lesion in the right adrenal gland, with adhesion to VCI (Fig. 2).
Fig. 1.
Ultrasound image of the right adrenal gland lesion
Fig. 2.
Selected CT images of the adrenal lesions
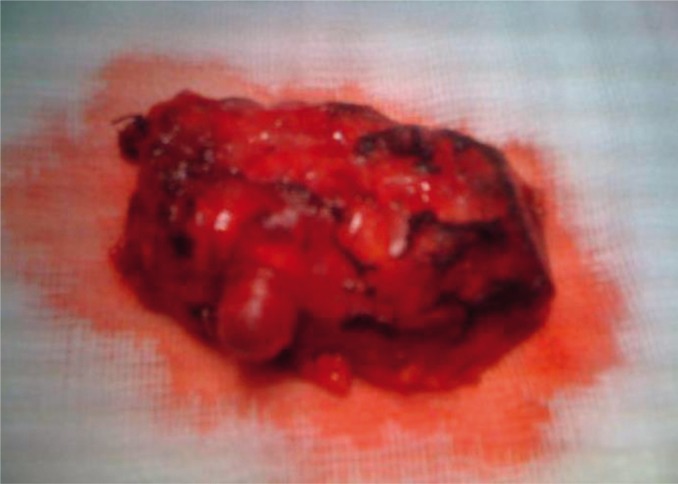
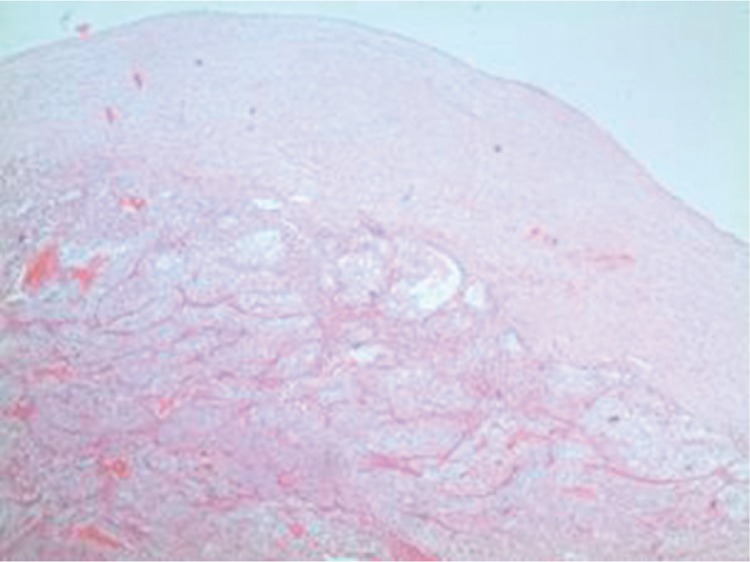
Since the lung lesions were deemed resectable, right adrenalectomy was proposed and consented to. Prior to the procedure, the patient was seen by an endocrinologist, and steroid supplementation was prescribed. Plasma levels of cortisol, aldosterone, 17-OH-progesterone, dehydroepiandrosterone sulfate and δ4-androstenedione were all normal. The patient was operated on at the age of 64, on the 19th of January 2012,– when right adrenalectomy was performed with adrenal vein tumor thrombectomy (Fig. 3). There were no complications after the procedure, and the patient was discharged on the 5th post-op day. The pathologic examination confirmed metastatic clear cell carcinoma (Fig. 4). She was referred to a thoracic surgeon for further treatment of the metastasis in the lungs.
Fig. 3.
Postoperative picture of the removed metastasis
Fig. 4.
Histological confirmation of clear cell type of RCC adrenal metastasis
Discussion
The behaviour of RCC is unpredictable, metastases may be found synchronously with the primary tumour, or in various organs many years after the treatment of the primary lesion(6, 7). Metastasis of RCC to the contralateral adrenal gland can be diagnosed as late as 23 years after nephrectomy(7).
There are two possible explanations for the delayed diagnosis of metastases. First, some metastases can be very slowgrowing, especially if they are low grade. Second, failure to use routine imaging studies might explain the delayed detection in some cases. Adrenal metastases are usually anatomically and functionally silent, and patients rarely have symptoms or signs of adrenal insufficiency. The underlying biological pathway for secondary involvement of the contralateral adrenal gland by RCC is unknown(8).
The routine follow-up ultrasound evaluation may therefore miss adrenal lesions with diameters <3 cm. If CT were to be performed on every routine follow-up evaluation in patients after radical nephrectomy for RCC, these metastases could probably be identified only slightly earlier, at a size of 1.5–2 cm(9). On the other hand, it is difficult to imagine routine annual CT scans conducted for many years after radical nephrectomy performed due to low risk RCC. European Urological Association does not recommend imaging in these circumstances after 5 years of follow-up. We may therefore emphasize the role of widely spread and easily accessible USS that revealed the lesion in our case.
The remote but existing risk of developing contralateral adrenal metastasis (CAM) after primary radical nephrectomy supports the idea of sparing the adrenal gland in suitable patients who undergo radical nephrectomy(8). In a prospective study, ipsilateral adrenal involvement during radical nephrectomy was reported in 2% of cases. Thus, the need for routine adrenalectomy during radical nephrectomy has been questioned, especially since the risk of an ipsilateral tumour developing after adrenal-sparing nephrectomy is low(10). Sparing the ipsilateral adrenal gland in radical nephrectomy would prevent the risk of adrenal insufficiency if the development of a tumour necessitates removing the contralateral adrenal gland, either at the time of nephrectomy or later(8).
Adrenalectomy is not indicated in the following situations:
Pre-operative tumour staging (USS, CT, MRI) shows a normal adrenal gland;
Intra-operative findings do not give any indication of a nodule within the adrenal gland suspicious of metastatic disease;
There is no evidence of direct invasion of the adrenal gland by a large upper pole tumour(11).
The survival rate of patients with untreated widely metastatic RCC is low, and may differ from that of patients with solitary or limited metastases, in many of whom the removal of the RCC metastasis is associated with prolonged survival. Of patients who undergo nephrectomy and resection of a solitary or limited metastasis, 30% have prolonged survival, many for >5 years after removing the metastasis. Therefore, aggressive treatment of such lesions is indicated(3). The longest disease-free interval after removing a CAM was 12.1 years(12), and the longest crude survival 14.3 years(13).
A contralateral adrenal metastasis from RCC is a rare finding with the potential benefit of cure after resection. Care must be taken in preoperative diagnostics, as thismetastasis is capable of causing inferior vena cava tumour thrombus via the suprarenal venous route(5). Interestingly, the ability of venous involvement shown by primary RCC is preserved by the metastatic lesions, though not uniformly. Caution is needed when the preoperative surgical template is planned in such cases.
Conclusions
To the best of our knowledge, we present the second similar entity described in literature so far. Although rarely encountered, late metastases may occur in patients managed due to renal cancer even in low risk disease. Nonetheless, CT repeated on a regular basis in this cohort would hardly be substantiated over the period of 5 years. The role of USS that revealed the lesion in our case should be emphasized. The remote but existing risk of developing contralateral adrenal metastasis after primary radical nephrectomy supports the idea of sparing the ipsilateral adrenal gland in suitable patients who undergo radical nephrectomy. Patients may benefit from the surgical removal of CAMs from RCC.
Conflict of interest
The authors do not report any conflict of interest.
References
- 1.Kozlowski JM. Management of distant solitary recurrence in the patient with renal cancer: contralateral kidney and other sites. Urol Clin North Am. 1994;21:601–624. [PubMed] [Google Scholar]
- 2.Saitoh H, Nakayama M, Nakamura K, Satoh T. Distant metastasis of renal adenocarcinoma in nephrectomized cases. J Urol. 1982;127:1092–1095. doi: 10.1016/s0022-5347(17)54243-3. [DOI] [PubMed] [Google Scholar]
- 3.O'dea MJ, Zincke H, Utz DC, Bernatz PE. The treatment of renal cell carcinoma with solitary metastasis. J Urol. 1978;120:540–542. doi: 10.1016/s0022-5347(17)57264-x. [DOI] [PubMed] [Google Scholar]
- 4.Marshall VF, Middleton RG, Holswade GR, Goldsmith EI. Surgery for renal cell carcinoma in the vena cava. J Urol. 1970;103:414–420. doi: 10.1016/s0022-5347(17)61970-0. [DOI] [PubMed] [Google Scholar]
- 5.von Knobloch R, Hegele A, Kälble T, Hofmann R. Management of contralateral adrenal metastasis from renal cell carcinoma: possibility of inferior vena cava tumour thrombus. Scand J Urol Nephrol. 2000;34:109–113. doi: 10.1080/003655900750016715. [DOI] [PubMed] [Google Scholar]
- 6.O'dea MJ, Zincke H, Utz DC, Bernatz PE. The treatment of renal cell carcinoma with solitary metastasis. J Urol. 1978;120:540–542. doi: 10.1016/s0022-5347(17)57264-x. [DOI] [PubMed] [Google Scholar]
- 7.Mesurolle B, Mignon F, Travagli JP, Meingan P, Vanel D. Late presentation of solitary contralateral adrenal metastasis of renal cell carcinoma. Eur Radiol. 1997;7:557–558. doi: 10.1007/s003300050204. [DOI] [PubMed] [Google Scholar]
- 8.Lau WK, Zincke H, Lohse CM, Cheville JC, Weaver AL, Blute ML. Contralateral adrenal metastasis of renal cell carcinoma: treatment, outcome and a review. BJU Int. 2003;91:775–779. doi: 10.1046/j.1464-410x.2003.04237.x. [DOI] [PubMed] [Google Scholar]
- 9.von Knobloch R, Seseke F, Riedmiller H, Gröne HJ, Walthers EM, Kälble T. Radical nephrectomy for renal cell carcinoma: is adrenalectomy necessary? Eur Urol. 1999;36:303–308. doi: 10.1159/000020009. [DOI] [PubMed] [Google Scholar]
- 10.Kletscher BA, Qian J, Bostwick DG, Blute ML, Zincke H. Prospective analysis of the incidence of ipsilateral adrenal metastasis in localized renal cell carcinoma. J Urol. 1996;155:1844–1846. [PubMed] [Google Scholar]
- 11. EAU Guidelines. [Google Scholar]
- 12.Sapienza P, Stipa F, Lucandri G, Baratti L, Delfino M, Mingazzini PL. Renal carcinoma with a solitary synchronous contralateral adrenal metastasis: a case report. Anticancer Res. 1997;17:743–747. [PubMed] [Google Scholar]
- 13.Elashry OM, Clayman RV, Soble JJ, McDougall EM. Laparoscopic adrenalectomy for solitary metachronous contralateral adrenal metastasis from renal cell carcinoma. J Urol. 1997;157:1217–1222. [PubMed] [Google Scholar]