Abstract
Background
The occurrence and severity of corneal oedema after phacoemulsification is dependent on the integrity of corneal endothelial cells. The function of these cells is affected by diabetes mellitus and consequently the behaviour of the cornea in diabetic patients is of special interest.
Aim
To compare the frequency of corneal oedema in two age-matched groups of diabetics and non diabetic patients that underwent cataract surgery in the Ophthalmology Department of Xanthi General Hospital in Greece.
Methods
A retrospective case control study was conducted in a retrospective fashion. Patients in the control and study groups were assessed regarding the severity of corneal oedema at three postoperative visits: days 1, 3–7, 10–14 after the operation. Ultrasound energy consumed during phacoemulsification was also a parameter of interest and possible correlations with the pre-existent cataract severity and the subsequent incidence of corneal oedema were investigated.
Results
The difference in the incidence of severe corneal oedema between the study and control group was statistically significant: (4.5% non diabetics vs 14.3% diabetics). The consumed ultrasound energy did not define final clinical outcome.
Conclusions
The existence of diabetes mellitus type 2 appears to be a significant risk factor for the development of persistent corneal oedema. The results of our study led to the modification of the algorithm for postoperative follow-up of patients of this remote area of Greece.
Keywords: Cornea, Phacoemulsification, Diabetes, Endothelium, Cataract
Highlights
-
•
Ultrasound energy is not the only defining factor for the development of corneal oedema.
-
•
Persistent corneal oedema is more frequent in diabetic patients 2 weeks postoperatively.
-
•
Modern Greek public health system requires modifications in clinical governance issues.
1. Introduction
Cataract surgery is a sophisticated procedure assisted by several imaging and diagnostic modalities that facilitate the surgeon and leads to a favourable result in the vast majority of cases. Despite technological innovations, there are many aspects of cataract surgery that remain to be investigated. One of these is the prediction of the behaviour of the corneal endothelium after the load of ultrasonic energy as well as the mechanical manipulations [1]. The incidence of persistent corneal oedema, implying dysfunction of the corneal endothelium, is estimated at 0.15% according to a recent large scale study [2]. Corneal decompensation after the removal of the crystalline lens through phacoemulsification even when performed by excellent and experienced surgeons can potentially lead to bullous keratopathy, permanent opacification of the cornea and eventually, penetrating or lamellar keratoplasty [3]. The main factor that determines the function of the cornea as a clear and transparent tissue is the corneal endothelium, a single layer of cells that serves as a continuous pump preserving the whole cornea in a dehydrated state [4].
There are numerous studies that have attempted to correlate the absolute number of endothelial cells with the development of corneal oedema after phacoemulsification. Nevertheless, there are also reports showing that corneas might be clear when supported by a small number of endothelial cells, while, on the other hand significant oedema might develop after the operation despite the presence of an adequate number of cells. Consequently, quantity is certainly an issue but the most important factor appears to be the quality of the endothelial cells, given of course that there is a minimum number of them [5]. The standard clinical practise in most small eye clinics does not include measuring endothelial cells during the preoperative stages and the condition of the cornea is assessed only through slit lamp examination in a similar pattern as lens opacities [6].
One of the most common co morbidities among people with cataract is diabetes mellitus [7], [8], [9]. We know that increased blood sugar levels affect ocular cells in many ways [10], [11] and in particular there are reports about the correlation of diabetes and corneal endothelial function [12], [13], [14].
The aim of our study was to compare the incidence of short term corneal oedema after phacoemulsification in diabetics (study group) and non diabetics (control group) and the rate of corneal clarity restoration in these two groups.
2. Methods
2.1. Setting
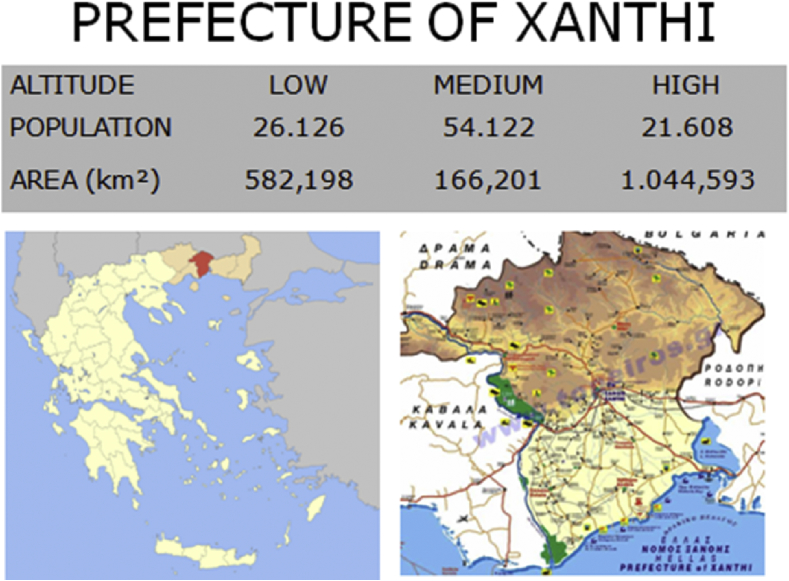
This retrospective case-control study took place in the cataract service of the ophthalmology department of the Xanthi General Hospital. The above district hospital serves a population of near 120,000 habitants and control of postoperative inflammation is quite challenging given that access to the hospital is limited for most of the nearby rural areas (Fig. 1). The study protocol adhered to the tenets of the Declaration of Helsinki and anonymity and confidentiality were guaranteed.
Fig. 1.
Map of the area that study conducted showing that there is a substantial number of patients with a considerable difficulty to reach the hospital facilities coming from the northern mountainous provinces. These patients needed an optimized algorithm to secure the most favourable outcome and the minimum number of postoperative visits.
2.2. Participants
For the purposes of the study, records for cases of phacoemulsification performed in Xanthi's Ophthalmology Department from January 2014 to October 2014 were examined. In bilateral cases, one eye was arbitrarily chosen: the eye with the smaller amount of energy consumed during the operation or in equal cases the dominant eye.
Inclusion criteria were: a) operations to be performed uneventfully by experienced surgeons (KTT and DS); b) senile cataract (all other forms were excluded) and existence of type 2 diabetes mellitus adequately controlled for at least 3 months before the time of the operation (regular strategy for diabetic patients); c) to complete the first (day 1) and final postoperative check (day 10–14).
Exclusion criteria were: a) prior history of uveitis, dense cataract, corneal disease or degeneration (mainly Fuchs' corneal dystrophy) and significant diabetic macular oedema were not included; b) The endothelial pump is reliant on oxygen, glucose and carbohydrate metabolism so special care was given to the recognition of factors that could independently affect the endothelium pump such as severe pulmonary diseases [15]; c) Another factor of significance is the ATPase complex activity [15]. Medications such as dactinomycin, ouabain, and oligomycin are potent inhibitors of this activity and patients taking these drugs were also excluded. Patients with senile cataracts and without diabetes or any of the defined entities were enrolled the study and served as the non-diabetic “control” group.
Data were retrieved by thorough review of patients' medical records and the incidence of corneal oedema was recorded and analysed with a primary focus on the incidence related to nuclear density, and intraoperative parameters, such as the ultrasonic energy and diabetes and also the time needed for this oedema to be resolved during the early postoperative period (2 weeks). All records were examined by two researchers independently and only in cases of agreement, patients included in the study.
2.3. Pre/intra operative assessment
Preoperative assessment included a thorough slit-lamp and retinal examination, measurements of best-corrected visual acuity, intraocular pressure (IOP) and classification of nuclear cataract; i.e., grades NC1 to NC5 (or NO1 to NO5) according to LOCS III classification system while NC6 cases allocated for extracapsular extraction. Biometry was performed on all patients through A-scan ultrasound for the calculation of intraocular lens power. All patients were advised to install tobramycin/dexamethasone eye drops four times/day 2 days before surgery. Given that many of the cataract patients were of advanced age and also a portion of the local population does not speak Greek, special attention was paid to the cooperation of relatives and carers to secure an adequate compliance regarding the pre- and postoperative eye drops administration. Uncomplicated phacoemulsification was performed in all cases using topical anaesthesia, and a 2.4 mm clear corneal incision. The surgical procedure followed a standardized method: injection of a viscoelastic agent, capsulorrhexis, hydrodissection, phacoemulsification (Infiniti® Vision System Alcon, Laboratories Inc, Fort Worth, TX, USA), irrigation and aspiration, viscoelastic in the bag, and implantation of a foldable acrylic lens (Tecnis IOL; Abbott Medical Optics, Santa Ana, CA, USA). The ultrasound energy as expressed by the Cumulative Dissipated Energy (CDE) metric that was consumed during the phacoemulsification cataract operation was recorded as a parameter of interest.
2.4. Post operative follow up
There is no universally accepted pattern for follow-up visits after a cataract operation. In the UK, as per the guidelines of the Royal College of Ophthalmologists, even a patient visit on the first-day postoperative review is not considered mandatory [16], [17]. In our study, given that there is no easy access to advice and assessment for patients other than the visit in the ophthalmology clinic, a modified protocol was selected to secure that post-operative complications were identified and managed properly.
Most of the patients during the first postoperative week visited the clinic on the following days: 1, 3–7 (interim visit) and 10–14 (final check). During the follow up appointment, patients were examined unaided and with a pinhole for the determination of their distance visual acuity, intraocular pressure was measured by Goldmann applanation tonometry, and corneal oedema grading according to the Oxford Cataract Treatment and Evaluation Team (OCTET) was noted. Corneal oedema was defined as an increase in central corneal thickness with or without descemet folds. The OCTET grades corneal oedema as transient corneal oedema(+), transient corneal oedema with descemet membrane folds of <10 (++), and transient corneal oedema with descemet membrane folds of >10 (+++) [18], [19]. Although postoperative oedema, as expected, affects the overall quality of a patients' vision causing blurred sight and a reduction in visual acuity, quantified visual acuity data are not presented since they do not directly correlated with oedema severity. Anterior chamber activity and lens location were documented as well. The algorithm for postoperative pharmaceutical treatment includes standard use of steroid drops every 4 h for the first week and four times per day until week 4. Antibiotic drops are recommended for four times/day for the first 2 weeks. Some cataract centres include the use of hypertonic saline agents, such as sodium chloride 5% solution or ointment. We tend to use these agents in persistent cases and not apply directly postoperatively (first 2 weeks); therefore, this medication was not included in the present study.
2.5. Measured outcomes
The primary outcome of the present study was the comparison of severe postoperative corneal oedema between a diabetic and a non diabetic population according to a standardised method of clinical evaluation. A secondary outcome was the detection of a significant correlation between the ultrasound energy that is required during phacoemulsification and the development of severe (+++) oedema in the study populations. Ultrasound energy was measured intraoperatively and expressed as the CDE parameter (numerical).
2.6. Statistics
Data were collected retrospectively, and the completed data forms were analysed with Microsoft Excel 2007 for Windows (Microsoft Corporation, Redmond, WA, USA) and SPSS version 16.0 for Windows (SPSS Inc., Chicago, IL, USA).
The chi-square test for proportions was used to detect any statistically significant difference concerning corneal oedema frequencies between group 1 and group 2 while t-test performed in order to test continuous data. Power calculation, performed post-hoc using the G*Power version 3.1.3 (Franz Paul, University of Kiel, Germany) [20], for 1-way ANOVA (2 groups), a-error probability of 0.05, and an effect size of 0.5 rendered a power (1-β error probability) of 0.91.
3. Results
Potentially eligible for the study were 398 patients who underwent a phacoemulsification in our centre during the examined period. In total, 242 eyes of 242 patients fulfilled the inclusion criteria and were enrolled in the study. The non-diabetic group had 200 participants (108 women, mean age 73.4 ± 5.13 years) and the diabetics group had 42 participants (25 women, mean age 74.5 ± 4.22 years). The two groups had similar percentages of female/male patients (Chi-square test, P = 0.63) and were also age-matched (two-tailed P value = 0.1949). Demographic data of all subjects are summarized in Table 1.
Table 1.
Demographic baseline data summary of the participants.
| Group | Sex |
Age |
|
|---|---|---|---|
| Males (n) | Females (n) | Mean (years) | |
| Non diabetics (control) | 92 | 108 | 73.4 ± 5.1 |
| Diabetics (study) | 17 | 25 | 74.5 ± 4.2 |
During the follow up, all patients had improvement in their distance visual acuity while a transient increase in intraocular pressure was adequately controlled with monotherapy in nine cases (two in the study group and seven in the control group). There were 19 cases in the control group (9.5%) and 5 cases in the study group (diabetics, 11.5%) where patients skipped the interim visit. These missing data, implemented in the study and we considered that these patients had the same grade of corneal oedema in the missing visit (last observation carried forward). We did not ignore the missing data since this could induce a potentially significant bias [21].
Severity of cataract as expressed by the LOCS III classification and its correlation with CDE are shown in Table 2.
Table 2.
Patients of both groups and the ultrasound energy (CDE) related to the severity of their pre existent nuclear cataract. As expected, harder nucleus demanded increased amount of energy during phacoemulsification.
| Cataract Classification (NC) | 1 | 2 | 3 | 4 | 5 | Total number of patients | |
|---|---|---|---|---|---|---|---|
| Control group (non diabetics) | Patients | 8 (4%) | 5 (2.5%) | 114 (57%) | 66 (33%) | 7 (3.5%) | 200 |
| CDE (mean) | 7.63 | 2.46 | 7.40 | 14.10 | 22.98 | ||
| Study group (diabetics) | Patients | 0 | 2 (4.8%) | 25 (59.5%) | 14 (33.3%) | 1 (2.4%) | 42 |
| CDE (mean) | – | 3.18 | 8.5 | 13.98 | 30.32 | ||
With respect to the incidence of corneal oedema and comparing between groups: 38.1% of patients in the study group presented with severe (+++) corneal oedema, which reduced to 19% during the interim visit and 14.3% of the patients had persistent severe oedema after the third check-up. The respective percentages in the control group were 32.5%, 7.5% and 4.5%. This difference was statistically significant (Chi-square test, P = 0.0414). For the study group, comparing CDE values between patient with severe (+++) oedema on the first postoperative day and patients with milder oedema (+,++) did not revealed statistical significance (P > 0.05). In the non diabetics group, CDE was increased for patients with severe oedema compared to patients with mild oedema (+) but not significantly elevated than the moderate oedema subgroup (++). Detailed results for both groups are summarised in Table 3.
Table 3.
Incidence of corneal oedema for both groups and corresponding CDE value for each subgroup. 4.5% of patients in the control group had severe corneal oedema in contrast to the study group where 14.3% of the patients had significant corneal oedema demanding further close follow up. Subgroups of patients with mild and moderate corneal oedema were merged for the 3rd visit, since these patients did not need any further follow-up.
| Oedema | Control group (non diabetics) |
Study group (diabetics) |
|||||
|---|---|---|---|---|---|---|---|
| + | ++ | +++ | + | ++ | +++ | ||
| 1st visit | Patients | 118 (59%) | 18 (9%) | 64 (32%) | 23 (54.8%) | 3 (7.1%) | 16 (38.1%) |
| CDE | 8.1 | 11.64 | 13.39 | 7.87 | 23.3 | 12.34 | |
| 2nd visit | Patients | 136 (68%) | 49 (24.5%) | 15 (7.5%) | 27 (64.3%) | 7(16.7%) | 8 (19%) |
| 3rd visit | Patients | 191 (95.5%) (not required further f/u) | 9 (4.5%) | 36 (85.7%) (not required further f/u) | 6 (14.3%) | ||
The odds ratio (OR) for developing severe oedema (+++) in diabetics compared to non-diabetics was 3.54 (95% confidence interval: 1.18–10.5, P = 0.023), meaning that patients with diabetes were 3.5 times more likely to develop severe corneal oedema after phacoemulsification compared to non-diabetics.
4. Discussion
As expected, the study results showed that the required ultrasound energy is strongly dependent on the severity of the cataract (nuclear density), despite that fact the consumed energy is not the determining factor for the corresponding severity of corneal oedema, especially in the study group in which patients with mild oedema demanded more ultrasonic energy than those who eventually developed severe oedema (23.3 vs. 12.34 were the CDE values in the two subgroups (mild and severe oedema) of the diabetic group, respectively). This observation might be explained by the hypothesis that the most significant factor is the preceding condition of the endothelial cells which makes some of them able to ‘tolerate’ increased amounts of CDE.
Another field of interest is the time required for corneas to restore clarity after the operation. In the control group, 64 patients had severe oedema in the first postoperative day and only 15 of them had persistent severe oedema after the interim visit (3–7 days). On the other hand, in the study group 38% of patients had severe oedema and this number reduced to 19% after the second visit. This finding corroborates analogous results from previous studies about the slower recovery of corneal endothelial cells in diabetics [22], [23].
The present study has certain limitations. First, we did not quantify the number of endothelial cells in each eye. However, special care was taken to include patients with similar demographic characteristics (age matched) without significant cornea pathologies and consequently we assumed homogeneity among participants regarding endothelial cell reserves. Another limitation is that the corneal oedema was not determined objectively due to lack of resources (human and financial) [24] in a modern Greek district hospital, but thorough slit lamp examination according to a standardized protocol guaranteed a satisfactory evaluation of corneal oedema.
The presented study was initially designed as a clinical audit project in order to determine the optimal scheme for postoperative follow up given that many of the patients had limited access to the hospital (2–3 h drive). According to the results of the study, only 15 patients (out of 242) needed follow up after the 2 week period. Our findings led our department to minimise (1) the appointments for patients without intraoperative complications or diabetes while for most diabetic patients their condition was assessed on the first postoperative day and after 2 weeks since after that time we can assess better the ability of the “diabetic” endothelium to restore cornea clarity.
In conclusion, the results of our study confirmed that the behaviour of corneal endothelium after cataract surgery is different in patients with diabetes mellitus. Thus, the follow-up of diabetic patients should be customized and particular care should be given during the surgery to minimize the damage of the endothelial cells either due to ultrasound load or mechanical manoeuvers. Evidently, a cataract service centre should modify preoperative and postoperative patterns of care according to specific needs. In any case, diabetic patients are a population at increased risk either for intraoperative or/and postoperative complications and consequently special attention should be paid.
Ethical approval
N/A.
Sources of funding
None.
Author contribution
KTT: study design, data analysis, writing.
DZP: data collection, data analysis.
EK: data collection, data analysis.
VV: data collection.
DS: data analysis, revision.
Conflicts of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Guarantor
KT Tsaousis.
Acknowledgements
The study has been partially presented at the 29th annual congress of the Hellenic Society of Intraocular Implant and Refractive Surgery (HSIOIRS), February 2015, Athens, Greece. Drs Panagiotou, Kostopoulou and Vlatsios were residents of Ophthalmology in the General Hospital of Xanthi at the time the study conducted.
Dr. Tsaousis received the “Spyros Georgaras” annual scholarship (2015) from the Hellenic Society of Intraocular Implants and Refractive Surgery for postgraduate training.
References
- 1.Rosado-Adames N., Afshari N.A. The changing fate of the corneal endothelium in cataract surgery. Curr. Opin. Ophthalmol. 2012;23:3–6. doi: 10.1097/ICU.0b013e32834e4b5f. [DOI] [PubMed] [Google Scholar]
- 2.Lundström M., Barry P., Henry Y., Rosen P., Stenevi U. Evidence-based guidelines for cataract surgery: guidelines based on data in the European registry of quality outcomes for cataract and refractive surgery database. J. Cataract. Refract Surg. 2012;38:1086–1093. doi: 10.1016/j.jcrs.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Siu G.D., Young A.L., Jhanji V. Alternatives to corneal transplantation for the management of bullous keratopathy. Curr. Opin. Ophthalmol. 2014;25:347–352. doi: 10.1097/ICU.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 4.DelMonte D.W., Kim T. Anatomy and physiology of the cornea. J. Cataract. Refract. Surg. 2011;37:588–598. doi: 10.1016/j.jcrs.2010.12.037. [DOI] [PubMed] [Google Scholar]
- 5.Hillenaar T., van Cleynenbreugel H., Remeijer L. How normal is the transparent cornea? effects of aging on corneal morphology. Ophthalmology. 2012;119:241–248. doi: 10.1016/j.ophtha.2011.07.041. [DOI] [PubMed] [Google Scholar]
- 6.Wong W.L., Li X., Li J. Cataract conversion assessment using lens opacity classification system III and Wisconsin cataract grading system. Invest. Ophthalmol. Vis. Sci. 2013;9(54):280–287. doi: 10.1167/iovs.12-10657. [DOI] [PubMed] [Google Scholar]
- 7.Prokofyeva E., Wegener A., Zrenner E. Cataract prevalence and prevention in Europe: a literature review. Acta Ophthalmol. 2013;91:395–405. doi: 10.1111/j.1755-3768.2012.02444.x. [DOI] [PubMed] [Google Scholar]
- 8.Olafsdottir E., Andersson D.K., Stefánsson E. The prevalence of cataract in a population with and without type 2 diabetes mellitus. Acta Ophthalmol. 2012;90:334–340. doi: 10.1111/j.1755-3768.2011.02326.x. [DOI] [PubMed] [Google Scholar]
- 9.Richter G.M., Torres M., Choudhury F., Azen S.P., Varma R., Los Angeles Latino Eye Study Group Risk factors for cortical, nuclear, posterior subcapsular, and mixed lens opacities: the Los Angeles Latino Eye Study. Ophthalmology. 2012;119:547–554. doi: 10.1016/j.ophtha.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lutty G.A. Effects of diabetes on the eye. Invest. Ophthalmol. Vis. Sci. 2013;13:54. doi: 10.1167/iovs.13-12979. ORSF81-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Clerck E.E., Schouten J.S., Berendschot T.T. New ophthalmologic imaging techniques for detection and monitoring of neurodegenerative changes in diabetes: a systematic review. Lancet Diabetes Endocrinol. 2015;3:653–663. doi: 10.1016/S2213-8587(15)00136-9. [DOI] [PubMed] [Google Scholar]
- 12.Misra S.L., Goh Y.W., Patel D.V., Riley A.F., McGhee C.N. Corneal microstructural changes in nerve fiber, endothelial and epithelial density after cataract surgery in patients with diabetes mellitus. Cornea. 2015;34:177–181. doi: 10.1097/ICO.0000000000000320. [DOI] [PubMed] [Google Scholar]
- 13.Storr-Paulsen A., Singh A., Jeppesen H., Norregaard J.C., Thulesen J. Corneal endothelial morphology and central thickness in patients with type II diabetes mellitus. Acta Ophthalmol. 2014;92:158–160. doi: 10.1111/aos.12064. [DOI] [PubMed] [Google Scholar]
- 14.Urban B., Raczyńska D., Bakunowicz-Łazarczyk A., Raczyńska K., Krętowska M. Evaluation of corneal endothelium in children and adolescents with type 1 diabetes mellitus. Mediat. Inflamm. 2013;2013:913754. doi: 10.1155/2013/913754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waring G.O., 3rd, Bourne W.M., Edelhauser H.F., Kenyon K.R. The corneal endothelium. Normal and pathologic structure and function. Ophthalmology. 1982;89:531–590. [PubMed] [Google Scholar]
- 16.Tinley C.G., Frost A., Hakin K.N., McDermott W., Ewings P. Is visual outcome compromised when next day review is omitted after phacoemulsification surgery? a randomised control trial. Br. J. Ophthalmol. 2003;87:1350–1355. doi: 10.1136/bjo.87.11.1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tan J.H., Newman D.K., Klunker C., Watts S.E., Burton R.L. Phacoemulsification cataract surgery: is routine review necessary on the first post-operative day? Eye. 2000;14(Pt 1):53–55. doi: 10.1038/eye.2000.11. [DOI] [PubMed] [Google Scholar]
- 18.Long-term corneal endothelial cell loss after cataract surgery. Results of a randomized controlled trial. Oxford Cataract Treatment and Evaluation Team (OCTET) Arch. Ophthalmol. 1986;104:1170–1175. [PubMed] [Google Scholar]
- 19.Use of a grading system in the evaluation of complications in a randomised controlled trial on cataract surgery. Oxford Cataract Treatment and Evaluation Team (OCTET) Br. J. Ophthalmol. 1986;70:411–414. doi: 10.1136/bjo.70.6.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Faul F., Erdfelder E., Buchner A., Lang A.G. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 21.Horton N.J., Kleinman K.P. Much ado about nothing: a comparison of missing data methods and software to fit incomplete data regression models. Am. Stat. 2007;61:79–90. doi: 10.1198/000313007X172556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morikubo S., Takamura Y., Kubo E., Tsuzuki S., Akagi Y. Corneal changes after small incision cataract surgery in patients with diabetes mellitus. Arch. Ophthalmol. 2004;122:966–969. doi: 10.1001/archopht.122.7.966. [DOI] [PubMed] [Google Scholar]
- 23.Dhasmana R., Singh I.P., Nagpal R.C. Corneal changes in diabetic patients after manual small incision cataract surgery. J. Clin. Diagn Res. 2014;8:VC03–VC06. doi: 10.7860/JCDR/2014/7955.4288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsaousis K.T. Ophthalmology training in Greece during its financial crisis: a need for change. Educ. Health (Abingdon) 2013;26:192–193. doi: 10.4103/1357-6283.126005. [DOI] [PubMed] [Google Scholar]