Abstract
Study Design
Retrospective analysis.
Objectives
To examine complications and rates of subsequent surgery following lumbar spinal fusion (LF) and lumbar total disc arthroplasty (TDA) at up to 5 years follow-up.
Summary of Background Data
LF is commonly used in the management of degenerative disc disease causing pain refractory to nonoperative management. Lumbar TDA was developed as an alternative to fusion with the theoretical advantage of reducing rates of adjacent segment pathology and reoperation. Most prior reports comparing these two interventions have come from industry-sponsored investigational device exemption trials and no large-scale administrative database comparisons exist.
Methods
The California Office of Statewide Health Planning and Development discharge database was queried for patients aged 18 to 65 years undergoing lumbar TDA and LF for degenerative disc disease from 2004 to 2010. Patient characteristics were collected, and rates of complications and readmission were identified. Rates of repeat lumbar surgery were calculated at 90-day and 1-, 3-, and 5-year follow-up intervals.
Results
A total of 52,877 patients met the inclusion criteria (LF = 50462, TDA = 2415). Wound infections were more common following LF than TDA (1.03% vs. 0.25%, p<0.001). Rates of subsequent lumbar surgery at 90-day and 1-year follow-up were lower with lumbar TDA than LF (90-day – TDA: 2.94% vs. LF: 4.01%, p=0.007; 1-year – TDA: 3.46% vs. LF: 4.78%, p=0.009). However, there were no differences in rates of subsequent lumbar surgery between the two groups at 3-year and 5-year follow-up.
Conclusions
Lumbar TDA was associated with fewer early reoperations, though beyond one year, rates of reoperation were similar. Lumbar TDA may be associated with fewer acute infections, though this may be approach-related and unrelated to the device itself.
Keywords: degenerative disc disease, lumbar spine, spinal fusion, total disc arthroplasty, artificial disc, reoperation, wound infection, surgical complications, outcomes, surgery
INTRODUCTION
Lumbar fusion (LF) is commonly performed for the treatment of severe degenerative disc disease (DDD) causing pain refractory to nonoperative management.1 The preferred method of fusion has been interbody fusion via a posterior or an anterior approach, or both combined for a circumferential fusion. Fusions performed for degenerative disc disease, and associated diagnoses, have become increasingly common over the past two decades, increasing 220% from 1990 to 2001 and increasing 2.4-fold from 2000 to 2009.2,3
Despite the relative frequency with which they are performed, lumbar fusions have several potential issues, such as pseudarthrosis and adjacent segment pathology (ASP).2 These complications can contribute to persistent low back pain and costly revision surgeries.4–8 ASP is thought to be related to loss of motion and altered biomechanics after spinal fusion and/or to the natural history of degenerative arthritis.9–12
Given the success of arthroplasty in other orthopaedic subspecialties, lumbar total disc arthroplasty (TDA) was proposed as an alternative to lumbar fusion for the treatment of DDD. The theoretical advantage of lumbar TDA is that it restores disc height and alleviates pain without eliminating motion at the diseased segment, which may minimize rates of reoperation due to ASP.13,14 Additionally, lumbar TDA may allow for earlier patient mobilization by negating the need for activity restrictions often required for fusion maturation.
The U.S. Food and Drug Administration (FDA) approved the CHARITÉ Artificial Disc (DePuy Spine Inc., Raynham, MA) in 2004 and the ProDisc-L Total Disc Replacement (Synthes Spine Inc., West Chester, PA) in 2006.15 Lumbar TDA is FDA-approved for skeletally mature patients with single-level DDD and no more than a grade 1 spondylolisthesis who have failed at least six months of nonoperative management. Several studies have reported that TDA is a safe and effective treatment for lumbar DDD.16–20 Lumbar TDA has been found to be equivalent, and in some studies superior, to fusion in improving patient-perceived outcomes such as disability, pain intensity, and quality of life.16–19,21 However, studies comparing the development of ASP and reoperation rates between lumbar TDA and fusion have produced mixed results.22
Given the paucity of data reported outside of industry-sponsored investigational device exemption (IDE) trials in the United States, there remains a need to report both acute and mid-term results following these procedures. The objectives of this study were: 1) to compare rates of complications and subsequent lumbar surgeries following lumbar TDA versus lumbar fusion at up to 5-year follow-up and 2) to identify factors associated with subsequent lumbar surgery following these procedures.
MATERIALS AND METHODS
Data Source
Data was obtained from California’s Office of Statewide Health Planning and Development (OSHPD) patient discharge database, which contains codes for up to 24 diagnoses and 20 inpatient procedures per hospitalization from all licensed nonfederal hospitals in California. The OSHPD database also includes several patient characteristics including age, gender, race/ethnicity, insurance type, and comorbidities. Patients were assigned unique identifiers to allow for longitudinal tracking across multiple hospitalizations. This data was also linked to the California State Death Statistical Master File (DSMF), which allowed for the tracking of patient mortality.
Inclusion and Exclusion Criteria
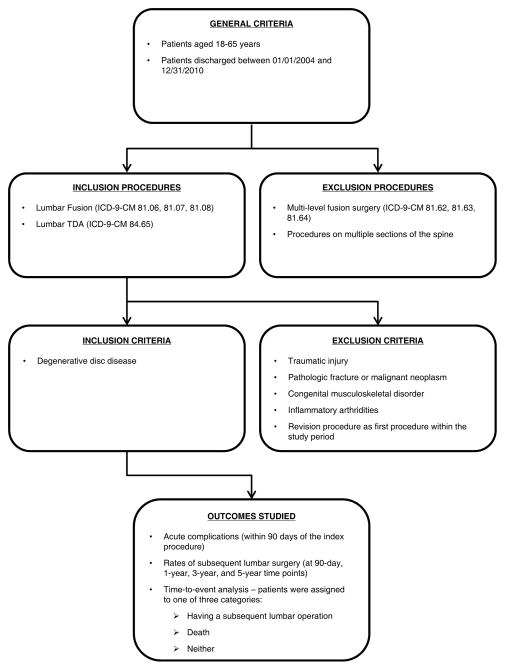
The OSHPD database was queried for patients aged 18 to 65 years from 01/01/2004 to 12/31/2010. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure and diagnosis codes were used to identify patients undergoing the procedures of interest (lumbar TDA – 84.65; lumbar fusion – 81.06, 81.07 or 81.08) and to eliminate patients meeting the exclusion criteria. Only patients with diagnoses of DDD were included. Patients with additional, potentially confounding diagnoses such as traumatic injuries, pathologic fractures, malignant neoplasms, congenital musculoskeletal disorders, inflammatory arthridities, and infections were excluded. All patients underwent single-level treatment. Patients who had multi-level fusion surgery (81.62, 81.63, 81.64) and patients who had procedures on multiple sections of the spine (e.g., both cervical fusion and lumbar fusion) were excluded. Finally, patients who underwent revision procedures as their first procedure within the study period were excluded (Figure 1).
Figure 1.
Patient selection flow chart
Outcomes Studied: Complications and Rates of Subsequent Lumbar Surgery
Following the index procedure, patients were identified as having complications using diagnosis and procedure codes, as previously described.23 Patients were identified for death within 30 days from the admission date of index hospitalization using the DSMF. Rates of subsequent lumbar surgery were calculated by examining the time periods at 90 days and 1, 3, and 5 years following each index procedure for additional lumbar surgery procedure codes.
Time-to-Event Analysis: Associations with Subsequent Lumbar Surgery
Time-to-event analysis was performed to assess the protective effect of lumbar TDA versus lumbar fusion on subsequent lumbar surgeries. Patients were assigned into one of three categories following the index procedure – a) having a subsequent lumbar operation, b) death, or c) neither by the end of the study period. Covariates analyzed included patient age, gender, race/ethnicity, comorbidities, and insurance type. Time-to-event analysis was performed by examining each of these covariates for potential associations with subsequent lumbar surgery.
Statistical Analysis
Student’s t-tests and chi-square tests were used to evaluate differences in patient demographics for continuous and categorical variables, respectively. Comparisons of rates of comorbidities, complications, and subsequent surgeries were performed using Fisher’s exact tests. Logistic regression was used to determine the effects of independent variables on various complications. Time-to-event analysis was conducted using a Cox proportional hazards model with subsequent lumbar surgery as the dependent variable. All statistical analyses were performed using STATA 13 (StataCorp LP, College Station, TX).
RESULTS
Trends
From 01/01/2004 to 12/31/2010, a total of 52,877 patients met the inclusion criteria. After TDA was FDA-approved in 2004, the procedure represented a small fraction of lumbar surgeries performed for DDD. 2005 marked the highest number and relative rate of lumbar TDAs performed in a single year. The number of lumbar TDA procedures performed compared to fusions steadily decreased from 2005 to 2010 (Table 1).
Table 1.
Trends in lumbar total disc arthroplasty and fusion in California from 2004 – 2010
| Year | TDA | Fusion | ||
|---|---|---|---|---|
|
| ||||
| # of Cases | Percentage (%) | # of Cases | Percentage (%) | |
|
| ||||
| 2004 | 53 | 0.80 | 6601 | 99.20 |
| 2005 | 484 | 7.22 | 6221 | 92.78 |
| 2006 | 439 | 6.24 | 6591 | 93.76 |
| 2007 | 444 | 5.88 | 7109 | 94.12 |
| 2008 | 351 | 4.52 | 7412 | 95.48 |
| 2009 | 327 | 3.84 | 8193 | 96.16 |
| 2010 | 317 | 3.66 | 8335 | 96.34 |
| Total | 2415 | 4.57 | 50462 | 95.43 |
Percentage reflects the frequency of that procedure compared to all lumbar surgeries (TDA and fusion combined) for that year.
Patient Characteristics
Of the 52,877 patients that met the inclusion criteria, 2,415 underwent lumbar TDA and 50,462 underwent lumbar fusion. The mean age of patients undergoing TDA was lower than that of LF patients (47.2 ± 8.8 vs. 51.8 ± 9.1). There was a higher proportion of males in the TDA group than the fusion group (56.9% (N=1375/2415) vs. 50.8% (N=25612/50462)). The mean number of total comorbidities per patient was higher in the fusion group than in the TDA group (0.8207 vs. 0.4605, p<0.0001) (Table 2). Specific patient comorbidities that were more frequent in the fusion group than the TDA group are listed in Table 3.
Table 2.
Demographics of patient sample
| Characteristic | TDA | Fusion |
|---|---|---|
|
| ||
| Number of Patients
| ||
| Count | 2415 | 50462 |
|
| ||
| Age (p <0.0001)a
| ||
| Mean ± SD (years) | 47.2 ± 8.8 | 51.8 ± 9.1 |
| Min-Max (years) | 21.2 – 65.0 | 21.3 – 65.0 |
|
| ||
| Gender (p <0.0001)b
| ||
| Male | 56.94% | 50.76% |
| Female | 43.06% | 49.24% |
|
| ||
| Race (p <0.0001)c
| ||
| White | 84.55% | 80.88% |
| Black | 3.69% | 5.22% |
| Native American | 0.25% | 0.33% |
| Asian/Pacific Islander | 2.69% | 2.71% |
| Other | 6.92% | 9.61% |
| Unknown Race | 1.90% | 1.25% |
|
| ||
| Ethnicity (p <0.0001)c
| ||
| Hispanic | 17.81% | 20.37% |
| Nonhispanic | 79.17% | 77.99% |
| Unknown Ethnicity | 3.02% | 1.64% |
|
| ||
| Payer Category (p <0.0001)c
| ||
| Medicare | 3.52% | 7.19% |
| Medi-Cal | 1.20% | 5.96% |
| Private | 41.95% | 53.71% |
| Workers’ Compensation | 43.52% | 28.93% |
| Other Insurance | 9.81% | 4.21% |
|
| ||
| Mean Number of Comorbidities per Patient (p<0.0001)a
| ||
| Comorbidities | 0.4605 | 0.8207 |
Significant differences determined based on Satterthwaite t-tests (P<0.05).
Significant differences determined based on Fisher’s exact tests (P<0.05).
Significant differences determined based on chi-square tests (P<0.05).
Table 3.
Specific patient comorbidities
| Comorbidity | TDA | Fusion | P-value^ | ||
|---|---|---|---|---|---|
|
| |||||
| Counts | Percentage (%) | Counts | Percentage (%) | ||
|
| |||||
| Arrhythmias | 67 | 2.77 | 1543 | 3.06 | 0.4669 |
| Arthritis* | 10 | 0.41 | 863 | 1.71 | <0.0001 |
| Atherosclerosis* | 23 | 0.95 | 1306 | 2.59 | <0.0001 |
| Cancer* | 5 | 0.21 | 440 | 0.87 | <0.0001 |
| Cellulitis | 6 | 0.25 | 190 | 0.38 | 0.3917 |
| CHF* | 3 | 0.12 | 365 | 0.72 | <0.0001 |
| COPD* | 37 | 1.53 | 1716 | 3.40 | <0.0001 |
| Decubitus* | 0 | 0.00 | 162 | 0.32 | 0.001 |
| Dementia* | 9 | 0.37 | 464 | 0.92 | 0.0027 |
| Diabetes mellitus* | 92 | 3.81 | 4724 | 9.36 | <0.0001 |
| ESRD | 0 | 0.00 | 51 | 0.10 | 0.1745 |
| Hematological | 0 | 0.00 | 48 | 0.10 | 0.1729 |
| Hemiplegia* | 3 | 0.12 | 1363 | 2.70 | <0.0001 |
| Hypertension* | 383 | 15.86 | 14078 | 27.90 | <0.0001 |
| Infection* | 26 | 1.08 | 1151 | 2.28 | <0.0001 |
| Major symptoms | 132 | 5.47 | 3013 | 5.97 | 0.3325 |
| Metastatic* | 0 | 0.00 | 265 | 0.53 | <0.0001 |
| Neuropathy* | 12 | 0.50 | 608 | 1.20 | 0.0007 |
| Other injury | 90 | 3.73 | 1604 | 3.18 | 0.1389 |
| Pneumonia | 4 | 0.17 | 205 | 0.41 | 0.0668 |
| Protein | 5 | 0.21 | 168 | 0.33 | 0.3629 |
| Psychiatric* | 33 | 1.37 | 1395 | 2.76 | <0.0001 |
| Renal* | 6 | 0.25 | 585 | 1.16 | <0.0001 |
| Stroke | 0 | 0.00 | 29 | 0.06 | 0.6422 |
| Vascular* | 58 | 2.40 | 1918 | 3.80 | 0.0002 |
Percentage (%) reflects the frequency of that comorbidity in all patients undergoing that procedure.
Significant differences determined based on Fisher’s exact tests (P<0.05).
Comorbidities with significant differences between groups.
Postoperative Complications and Readmissions
The rate of all-cause readmissions following the index procedure was higher in the fusion group than the TDA group (6.04% vs. 4.76%, p=0.009). However, logistic regression analysis isolating the effect of individual variables on readmission demonstrated no difference in readmission rates between the two procedures (TDA OR 0.93, 95% CI 0.77–1.13, p=0.456). There were 72 deaths in the fusion group and no deaths in the TDA group, but this difference was not significant. Wound infections were more common following LF (LF: 1.03%; TDA: 0.25%, p<0.001) (Table 4). This difference was confirmed by logistic regression analysis, which demonstrated a lower risk of infection following TDA (TDA OR 0.29, 95% CI 0.13–0.66, p=0.003).
Table 4.
Complication and subsequent lumbar surgery rates
| Outcome | TDA rate (%) | Fusion rate (%) | P-value^ |
|---|---|---|---|
|
| |||
| Death | 0 | 0.14 | 0.080 |
| Myocardial infarction | 0.04 | 0 | 0.131 |
| Pulmonary embolism | 0.21 | 0.20 | 0.819 |
| Pneumonia | 0.04 | 0.09 | 0.723 |
| Septicemia | 0.12 | 0.20 | 0.633 |
| Surgical site bleeding | 0.12 | 0.13 | 1 |
| Wound infection* | 0.25 | 1.03 | <0.001 |
| Periprosthetic joint infection | 0.04 | 0 | 0.131 |
| Mechanical complication | 0.87 | 0.69 | 0.315 |
| Readmission† | 4.76 | 6.04 | 0.009 |
| Subsequent surgery (within 90 days)* | 2.94 | 4.01 | 0.007 |
Significant differences determined based on Fisher’s exact tests (P<0.05).
Outcomes with significant differences between groups, confirmed by logistic regression analysis.
Outcomes with significant differences between groups using Fisher’s exact tests, but not supported by logistic regression analysis.
Subsequent Lumbar Surgeries and Time-To-Event Analysis
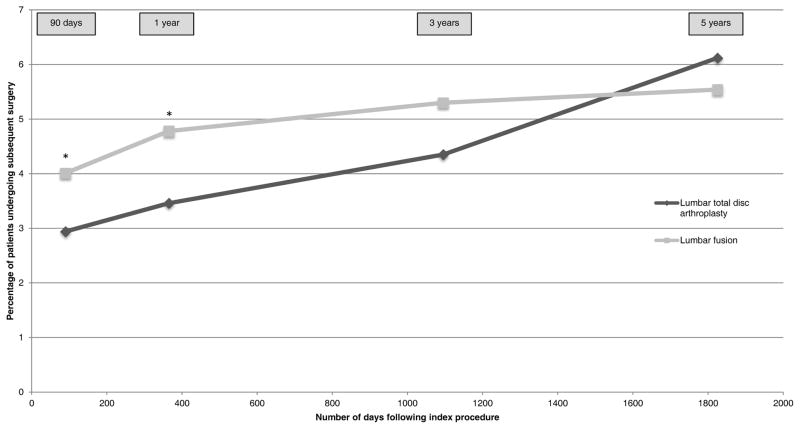
Subsequent lumbar surgeries within 90 days of the index procedure were performed more frequently in the LF group (LF: 4.01%; TDA: 2.94%, p=0.007) (Table 4). Again, this difference was supported by logistic regression analysis, which demonstrated a lower risk of subsequent surgery within 90 days following TDA (TDA OR 0.78, 95% CI 0.61–0.99, p=0.049). At 1-year follow-up, subsequent surgery rates were lower following TDA (TDA: 3.46%; LF: 4.78%, p=0.009). However, there were no significant differences in rates of subsequent lumbar surgeries between the two groups at 3-year and 5-year follow-up (3-year – TDA: 4.35% vs. LF: 5.3%, p=0.223; 5-year – TDA: 6.12% vs. LF: 5.54%, p=0.858) (Figure 2).
Figure 2. Rates of subsequent lumbar surgery over time.
* Significant differences between groups determined based on Fisher’s exact tests (P<0.05).
In the time-to-event analysis, Cox proportional hazard modeling revealed that older age (HR 1.011, 95% CI 1.006–1.017, p<0.0001), Medicare insurance (HR 1.407, 95% CI 1.201–1.650, p<0.0001), diabetes mellitus (HR 1.212, 95% CI 1.045–1.406, p=0.011) and psychiatric diagnoses (HR 1.358, 95% CI 1.059–1.742, p=0.0159) were associated with subsequent surgeries (Table 5). Finally, lumbar TDA was associated with a decreased need for subsequent lumbar surgery in the time-to-event analysis, but this did not reach statistical significance (HR 0.793, 95% CI 0.625–1.008, p=0.0577).
Table 5.
Parameters associated with subsequent lumbar surgery
| Parameter | Hazard Ratio | 95% Confidence Interval | P-value^ |
|---|---|---|---|
|
| |||
| Age | 1.011 | 1.006 – 1.017 | <0.0001 |
| Diabetes mellitus | 1.212 | 1.045 – 1.406 | 0.011 |
| Medicare | 1.407 | 1.201 – 1.650 | <0.0001 |
| Psychiatric Illness | 1.358 | 1.059 – 1.742 | 0.0159 |
Significant differences determined based on chi-square tests (P<0.05).
DISCUSSION
Substantial debate persists regarding the role of TDA in the treatment of lumbar DDD.24 LF is performed in select cases of DDD, although there is concern regarding the long-term consequences of lumbar arthrodesis. The discs adjacent to the fusion may degenerate and, in some cases, become a cause for reoperation. Additionally, LF is not always successful, with non-union rates reported as high as 36%.25,26 Lumbar TDA was developed as an alternative to LF, with the theoretical benefit of decreasing adjacent segment stresses by maintaining motion at the operated level. Studies comparing clinical outcomes and reoperation rates following fusion and TDA have produced mixed results and most reports in the United States come from IDE studies, limiting the generalizability of the results.27–31 Our study utilizes a statewide database to provide results that should be generalizable to the broader population of the United States, and the large sample size allows for the examination of rare adverse outcomes that might not otherwise be observed.
Our findings suggest that rates of complications following both LF and TDA are low. However, rates of wound infection and subsequent lumbar surgery at 90-day and 1-year follow-up were higher in patients undergoing LF than TDA. Rates of subsequent lumbar surgery did not differ significantly at 3- and 5-year follow-up between the groups. Finally, older age, Medicare insurance, diabetes mellitus, and psychiatric diagnoses were covariates associated with subsequent lumbar surgery in the time-dependent analysis.
Lumbar TDA has constituted only a small fraction of lumbar surgeries in the United States, and since its approval, there has been no significant increase in the utilization of TDA for lumbar DDD.3,32 Our findings reflected a steady decrease in the utilization of lumbar TDA in California from 2005 to 2010, as well as an increase in the number of lumbar fusion procedures performed, mirroring the trends previously observed on a national level and supporting that our cohort is representative of the country.
Complication rates and the types of complications studied following lumbar TDA have varied in the literature. Tropiano et al. reported complications including vertebral body fractures, retrograde ejaculation, and incisional hernias following lumbar TDA.33,34 A recent meta-analysis examined complication rates in 5 different studies and found a higher rate of overall complications – including implant removal, major vessel injury, nerve damage, and death – associated with LF than with TDA (LF: 10.8%; TDA: 5.8%).20 On the other hand, several prior reports have found no differences in complications between LF and TDA.16,35 While we were unable to investigate all of the aforementioned complications using the OSHPD database, we found that rates of wound infection and overall readmission were higher in the fusion group. Regression analysis reaffirmed the difference in wound infection following these procedures irrespective of the differences in patient demographics; however, there was no difference in the logistic regression with regards to readmission.
Reoperation for persistent low back pain following lumbar surgery can be clinically challenging. Pseudarthrosis, implant bursitis, and ASP have all been implicated as possible contributors. However, studies examining the development of ASP after spinal fusion and TDA have been inconclusive. Some studies have cited a lower incidence of ASP in lumbar TDA patients compared to LF patients,6,36 while others have cited no clear decrease in ASP following lumbar TDA.10,19,37–39 Additionally, rates of subsequent lumbar surgery have varied in the literature, ranging from 6% to 11%.34,39 Of the few studies that have directly compared reoperation between lumbar TDA and fusion, none has cited significant differences in reoperation rates.16,20,35 The rates of subsequent lumbar surgery found in this study were higher in the fusion group than the TDA group at 90-day and 1-year follow-up though, overall, the rates in both groups were low (<5%). The fact that rates of subsequent lumbar surgery at 3- and 5- year follow-up did not differ between patients undergoing lumbar TDA or fusion in this study further supports the notion that ASP may occur as part of the degenerative process of the lumbar spine and not as a complication specific to fusion surgery, as early reoperation is unlikely to be due to adjacent segment pathologies, while surgeries further out are more likely due to ASP.
Several patient-specific variables – older age, Medicare insurance, diabetes mellitus, and psychiatric diagnoses – were found to have associations with subsequent lumbar surgery following TDA and fusion in the time-to-event analysis. Older patients are at a known increased risk for complications and reoperation following LF due to multiple comorbidities, poor bone quality, and reduced fusion potential.40,41 Multiple studies have also demonstrated similar adverse outcomes among diabetic patients undergoing lumbar spine surgery.42,43 The presence of psychiatric illness or poor emotional health has been demonstrated to adversely affect pain and function after spine surgery and may lead to more frequent reoperation.44,45
The OSHPD database has been successfully utilized to evaluate other orthopaedic procedures, though there are some limitations inherent in using this administrative database. Complications may be underreported, as we rely on ICD-9-CM coding for identification. Some complications of interest may be treated in outpatient settings and, therefore, would not be recorded in this database, which only contains discharge abstracts for inpatient admissions. Thus, our reported rates of these complications may be lower than the true values. Additionally, some potential complicating factors, such as disease severity, concomitant presence of lumbar stenosis, and, most importantly, the physician’s rationale behind choosing which procedure to perform, are not recorded in the database. Furthermore, the demographics of the two patient groups studied were found to differ in several categories. Surgeons may have been more hesitant to perform TDA on older patients or those with osteoporosis due to fear of complications such as component subsidence. This is likely an inherent problem when comparing these two procedures retrospectively, as other studies have similarly shown differences in their respective patient populations.32 Our regression analyses did, however, control for patient-specific demographic variables, including age. Lumbar TDA is performed exclusively through an anterior approach, while LF may be performed from a number of approaches. It may be that a posterior approach is associated with higher rates of wound infection, making our conclusion inevitable. We were unable to control for approach with our design and approach may be the risk factor for any particular complication, rather than the device used. Finally, there is a possibility that some early reoperations may have been planned, staged fusion procedures, which may have falsely elevated the rates of subsequent lumbar surgeries in our study.46
Data comparing outcomes following lumbar TDA and fusion is necessary, as the utility of TDA continues to be a subject of debate. As many as 14.9% of patients who have undergone lumbar fusion are also candidates for TDA as they do not meet the IDE exclusion criteria for TDA, such as multiple level DDD, adjacent prior fusion, known fracture or trauma, severe spondylolisthesis or severe medical comorbidities.47 In a survey conducted at the 2007 “Contemporary Update on Disorders of the Spine” conference, 64% of respondents reported that they were less likely to perform lumbar TDA compared to one year earlier, citing concerns about long-term outcomes and revision procedures.48 Our study demonstrates that the overall rates of complications following lumbar TDA and fusion are low. The rates of wound infection and subsequent lumbar surgery at 90-day and 1-year follow-up were higher in the fusion group than the TDA group; however, subsequent lumbar surgery rates did not differ between the two groups at 3- and 5-year follow-up. While the low rates of adverse outcomes following lumbar TDA may seem promising, the fact that there were no differences in the rates of lumbar surgery at 3 and 5 years following the index procedure suggest that TDA may not help to prevent subsequent lumbar surgeries at mid-term follow-up. Further clinical studies are necessary to better characterize the long-term outcomes following lumbar TDA given the short time period over which the procedure has been available in the United States.
Acknowledgments
The device(s)/drug(s) is/are FDA-approved or approved by corresponding national agency for this indication. No funds were received in support of this work. Relevant financial activities outside the submitted work: grants.
Footnotes
Level of Evidence: 3
Contributor Information
Claire D. Eliasberg, Email: celiasberg@mednet.ucla.edu, Department of Orthopaedic Surgery, University of California at Los Angeles, 615 Charles E Young Drive, South, Room 44607-A, Los Angeles, CA 90095, Telephone number: 858-775-2882.
Michael P. Kelly, Email: kellymi@wudosis.wustl.edu, Department of Orthopaedic Surgery, Washington University School of Medicine, 660 South Euclid Avenue, Campus Box 8233, St. Louis, MO 63110, Telephone number: 314-514-3500.
Remi M. Ajiboye, Email: rajiboye@mednet.ucla.edu, Department of Orthopaedic Surgery, University of California at Los Angeles, 10833 Le Conte Avenue, 76-143 CHS, Los Angeles, CA 90095, Telephone number: 510-828-7906.
Nelson F. SooHoo, Email: nsoohoo@mednet.ucla.edu, Department of Orthopaedic Surgery, University of California at Los Angeles, 1250 16th Street, Suite 3142, Santa Monica, CA 90404, Telephone number: 424-259-9813.
References
- 1.German JW, Foley KT. Disc arthroplasty in the management of the painful lumbar motion segment. Spine (Phila Pa 1976) 2005;30(16 Suppl):S60–67. doi: 10.1097/01.brs.0000174511.66830.e9. [DOI] [PubMed] [Google Scholar]
- 2.Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005;30(12):1441–1445. doi: 10.1097/01.brs.0000166503.37969.8a. discussion 1446–1447. [DOI] [PubMed] [Google Scholar]
- 3.Yoshihara H, Yoneoka D. National trends in the surgical treatment for lumbar degenerative disc disease: United States, 2000 to 2009. Spine J. 2015;15(2):265–271. doi: 10.1016/j.spinee.2014.09.026. [DOI] [PubMed] [Google Scholar]
- 4.Dimitriou R, Mataliotakis GI, Angoules AG, Kanakaris NK, Giannoudis PV. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: a systematic review. Injury. 2011;42(Suppl 2):S3–15. doi: 10.1016/j.injury.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Fritzell P, Hagg O, Wessberg P, Nordwall A. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine (Phila Pa 1976) 2002;27(11):1131–1141. doi: 10.1097/00007632-200206010-00002. [DOI] [PubMed] [Google Scholar]
- 6.Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976) 2008;33(15):1701–1707. doi: 10.1097/BRS.0b013e31817bb956. [DOI] [PubMed] [Google Scholar]
- 7.Malter AD, McNeney B, Loeser JD, Deyo RA. 5-year reoperation rates after different types of lumbar spine surgery. Spine (Phila Pa 1976) 1998;23(7):814–820. doi: 10.1097/00007632-199804010-00015. [DOI] [PubMed] [Google Scholar]
- 8.Turner JA, Ersek M, Herron L, et al. Patient outcomes after lumbar spinal fusions. JAMA. 1992;268(7):907–911. [PubMed] [Google Scholar]
- 9.Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004;86-A(7):1497–1503. doi: 10.2106/00004623-200407000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Helgeson MD, Bevevino AJ, Hilibrand AS. Update on the evidence for adjacent segment degeneration and disease. Spine J. 2013;13(3):342–351. doi: 10.1016/j.spinee.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 2004;29(17):1938–1944. doi: 10.1097/01.brs.0000137069.88904.03. [DOI] [PubMed] [Google Scholar]
- 12.Xia XP, Chen HL, Cheng HB. Prevalence of adjacent segment degeneration after spine surgery: a systematic review and meta-analysis. Spine (Phila Pa 1976) 2013;38(7):597–608. doi: 10.1097/BRS.0b013e318273a2ea. [DOI] [PubMed] [Google Scholar]
- 13.David T. Lumbar disc prosthesis. Surgical technique, indications and clinical results in 22 patients with a minimum of 12 months follow-up. Eur Spine J. 1993;1(4):254–259. doi: 10.1007/BF00298370. [DOI] [PubMed] [Google Scholar]
- 14.Kostuik JP. Intervertebral disc replacement. Experimental study. Clin Orthop Relat Res. 1997;(337):27–41. doi: 10.1097/00003086-199704000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Administration USFaD. Medical Devices: Recently-Approved Devices. 2012 http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/DeviceApprovalsandClearances/Recently-ApprovedDevices/default.htm.
- 16.Berg S, Tullberg T, Branth B, Olerud C, Tropp H. Total disc replacement compared to lumbar fusion: a randomised controlled trial with 2-year follow-up. Eur Spine J. 2009;18(10):1512–1519. doi: 10.1007/s00586-009-1047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park CK, Ryu KS, Lee KY, Lee HJ. Clinical outcome of lumbar total disc replacement using ProDisc-L in degenerative disc disease: minimum 5-year follow-up results at a single institute. Spine (Phila Pa 1976) 2012;37(8):672–677. doi: 10.1097/BRS.0b013e31822ecd85. [DOI] [PubMed] [Google Scholar]
- 18.Scott-Young MN, Lee MJ, Nielsen DE, Magno CL, Kimlin KR, Mitchell EO. Clinical and Radiological Mid-Term Outcomes of Lumbar Single-Level Total Disc Replacement. Spine (Phila Pa 1976) 2011 doi: 10.1097/BRS.0b013e3182345aa2. [DOI] [PubMed] [Google Scholar]
- 19.Van de Kelft E, Verguts L. Clinical outcome of mono segmental total disc replacement for lumbar disc disease with ball in socket prosthesis (Maverick(R)): Prospective study with 4 year follow-up. World neurosurgery. 2011 doi: 10.1016/j.wneu.2011.10.043. [DOI] [PubMed] [Google Scholar]
- 20.Wei J, Song Y, Sun L, Lv C. Comparison of artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. International orthopaedics. 2013;37(7):1315–1325. doi: 10.1007/s00264-013-1883-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lemaire JP, Skalli W, Lavaste F, et al. Intervertebral disc prosthesis. Results and prospects for the year 2000. Clin Orthop Relat Res. 1997;(337):64–76. doi: 10.1097/00003086-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Wang JC, Arnold PM, Hermsmeyer JT, Norvell DC. Do lumbar motion preserving devices reduce the risk of adjacent segment pathology compared with fusion surgery? A systematic review. Spine (Phila Pa 1976) 2012;37(22 Suppl):S133–143. doi: 10.1097/BRS.0b013e31826cadf2. [DOI] [PubMed] [Google Scholar]
- 23.Mehrotra A, Sloss EM, Hussey PS, Adams JL, Lovejoy S, SooHoo NF. Evaluation of a center of excellence program for spine surgery. Medical care. 2013;51(8):748–757. doi: 10.1097/MLR.0b013e31829b091d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hanley EN, Jr, Herkowitz HN, Kirkpatrick JS, Wang JC, Chen MN, Kang JD. Debating the value of spine surgery. J Bone Joint Surg Am. 2010;92(5):1293–1304. doi: 10.2106/JBJS.I.01439. [DOI] [PubMed] [Google Scholar]
- 25.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73(6):802–808. [PubMed] [Google Scholar]
- 26.Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H. Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17(8):1107–1112. doi: 10.1007/s00586-008-0695-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blumenthal S, McAfee PC, Guyer RD, et al. A prospective, randomized, multicenter Food and Drug Administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine (Phila Pa 1976) 2005;30(14):1565–1575. doi: 10.1097/01.brs.0000170587.32676.0e. discussion E1387–1591. [DOI] [PubMed] [Google Scholar]
- 28.Delamarter R, Zigler JE, Balderston RA, Cammisa FP, Goldstein JA, Spivak JM. Prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement compared with circumferential arthrodesis for the treatment of two-level lumbar degenerative disc disease: results at twenty-four months. J Bone Joint Surg Am. 2011;93(8):705–715. doi: 10.2106/JBJS.I.00680. [DOI] [PubMed] [Google Scholar]
- 29.Delamarter RB, Bae HW, Pradhan BB. Clinical results of ProDisc-II lumbar total disc replacement: report from the United States clinical trial. The Orthopedic clinics of North America. 2005;36(3):301–313. doi: 10.1016/j.ocl.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Gornet MF, Burkus JK, Dryer RF, Peloza JH. Lumbar disc arthroplasty with Maverick disc versus stand-alone interbody fusion: a prospective, randomized, controlled, multicenter investigational device exemption trial. Spine (Phila Pa 1976) 2011;36(25):E1600–1611. doi: 10.1097/BRS.0b013e318217668f. [DOI] [PubMed] [Google Scholar]
- 31.Zigler J, Delamarter R, Spivak JM, et al. Results of the prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine (Phila Pa 1976) 2007;32(11):1155–1162. doi: 10.1097/BRS.0b013e318054e377. discussion 1163. [DOI] [PubMed] [Google Scholar]
- 32.Awe OO, Maltenfort MG, Prasad S, Harrop JS, Ratliff JK. Impact of total disc arthroplasty on the surgical management of lumbar degenerative disc disease: Analysis of the Nationwide Inpatient Sample from 2000 to 2008. Surgical neurology international. 2011;2:139. doi: 10.4103/2152-7806.85980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tropiano P, Huang RC, Girardi FP, Cammisa FP, Jr, Marnay T. Lumbar total disc replacement. Seven to eleven-year follow-up. J Bone Joint Surg Am. 2005;87(3):490–496. doi: 10.2106/JBJS.C.01345. [DOI] [PubMed] [Google Scholar]
- 34.Tropiano P, Huang RC, Girardi FP, Marnay T. Lumbar disc replacement: preliminary results with ProDisc II after a minimum follow-up period of 1 year. J Spinal Disord Tech. 2003;16(4):362–368. doi: 10.1097/00024720-200308000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Skold C, Tropp H, Berg S. Five-year follow-up of total disc replacement compared to fusion: a randomized controlled trial. Eur Spine J. 2013;22(10):2288–2295. doi: 10.1007/s00586-013-2926-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang MC, Shivakoti M, Sparapani RA, Guo C, Laud PW, Nattinger AB. Thirty-day readmissions after elective spine surgery for degenerative conditions among US Medicare beneficiaries. Spine J. 2012;12(10):902–911. doi: 10.1016/j.spinee.2012.09.051. [DOI] [PubMed] [Google Scholar]
- 37.Berg S, Tropp HT, Leivseth G. Disc height and motion patterns in the lumbar spine in patients operated with total disc replacement or fusion for discogenic back pain. Results from a randomized controlled trial. Spine J. 2011;11(11):991–998. doi: 10.1016/j.spinee.2011.08.434. [DOI] [PubMed] [Google Scholar]
- 38.Huang RC, Tropiano P, Marnay T, Girardi FP, Lim MR, Cammisa FP., Jr Range of motion and adjacent level degeneration after lumbar total disc replacement. Spine J. 2006;6(3):242–247. doi: 10.1016/j.spinee.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 39.Putzier M, Funk JF, Schneider SV, et al. Charite total disc replacement--clinical and radiographical results after an average follow-up of 17 years. Eur Spine J. 2006;15(2):183–195. doi: 10.1007/s00586-005-1022-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85-A(11):2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Okuda S, Oda T, Miyauchi A, Haku T, Yamamoto T, Iwasaki M. Surgical outcomes of posterior lumbar interbody fusion in elderly patients. J Bone Joint Surg Am. 2006;88(12):2714–2720. doi: 10.2106/JBJS.F.00186. [DOI] [PubMed] [Google Scholar]
- 42.Golinvaux NS, Varthi AG, Bohl DD, Basques BA, Grauer JN. Complication rates following elective lumbar fusion in patients with diabetes: insulin dependence makes the difference. Spine (Phila Pa 1976) 2014;39(21):1809–1816. doi: 10.1097/BRS.0000000000000506. [DOI] [PubMed] [Google Scholar]
- 43.Guzman JZ, Iatridis JC, Skovrlj B, et al. Outcomes and complications of diabetes mellitus on patients undergoing degenerative lumbar spine surgery. Spine (Phila Pa 1976) 2014;39(19):1596–1604. doi: 10.1097/BRS.0000000000000482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Trief PM, Grant W, Fredrickson B. A prospective study of psychological predictors of lumbar surgery outcome. Spine (Phila Pa 1976) 2000;25(20):2616–2621. doi: 10.1097/00007632-200010150-00012. [DOI] [PubMed] [Google Scholar]
- 45.Trief PM, Ploutz-Snyder R, Fredrickson BE. Emotional health predicts pain and function after fusion: a prospective multicenter study. Spine (Phila Pa 1976) 2006;31(7):823–830. doi: 10.1097/01.brs.0000206362.03950.5b. [DOI] [PubMed] [Google Scholar]
- 46.Amin BY, Tu TH, Schairer WW, et al. Pitfalls of calculating hospital readmission rates based on nonvalidated administrative data sets: : presented at the 2012 Joint Spine Section Meeting: clinical article. J Neurosurg Spine. 2013;18(2):134–138. doi: 10.3171/2012.10.SPINE12559. [DOI] [PubMed] [Google Scholar]
- 47.Quirno M, Goldstein JA, Bendo JA, Kim Y, Spivak JM. The Incidence of Potential Candidates for Total Disc Replacement among Lumbar and Cervical Fusion Patient Populations. Asian spine journal. 2011;5(4):213–219. doi: 10.4184/asj.2011.5.4.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Whang PG, Simpson AK, Rechtine G, Grauer JN. Current trends in spinal arthroplasty: an assessment of surgeon practices and attitudes regarding cervical and lumbar disk replacement. J Spinal Disord Tech. 2009;22(1):26–33. doi: 10.1097/BSD.0b013e3181659804. [DOI] [PubMed] [Google Scholar]