Abstract
Background:
There is a large body of literature and scientific data regarding the efficacy of pharmacological and psychosocial interventions for schizophrenia, however, studies on Yoga therapy is scanty. Yoga is a means of balancing and harmonizing the body, mind and emotion, and for enlightening the mind and upliftment of the total personality.
Aims:
The present study was conducted to determine the efficacy of Yoga therapy as an adjunctive therapy and to see its effects on psychopathology on the patients suffering from chronic schizophrenia.
Settings and Design:
Pre- and post-test design with the control group.
Materials and Methods:
It is a study using purposive sampling technique by which 30 chronic schizophrenic patients were selected and 15 patients were randomly assigned to Yoga therapy along with pharmacotherapy (experimental group), and 15 were assigned pharmacotherapy alone (control group) after the baseline assessment using Positive and Negative Syndrome Scale (PANSS). The Yoga group attended Yoga therapy everyday for about 1½ h including motivational and feedback session.
Results:
At the end of 1 month postassessment was done, and schizophrenic patients, who received the yogic intervention showed better rating than those in pharmacotherapy alone on PANSS variables.
Conclusion:
Yoga could be a right choice for improving psychopathology resulting in better quality of life along with other pharmacological management and psychosocial interventions.
Keywords: Management, psychopathology, schizophrenia, Yoga therapy
INTRODUCTION
The contribution of Yoga on mental health practice has been acknowledged world-wide and is the oldest system of holistic health in the world with its roots originating in Indian philosophy and is used as an adjunct to psychotherapy in several countries. Yoga means union, as it harmonizes the body, breath, mind and spirit. It is a means of balancing and harmonizing the body, mind and emotion, and for enlightening the mind and upliftment of the total personality. The Yoga sessions involve the practice of floor, sitting, and standing postures, inversions (headstand, shoulder stand), breathing exercises (pranayama), and meditation. Specific asanas work on the various systems of the body, bringing alertness to mind, while soothing nervous system and glands, relaxing brain, and maintaining a physical, physiological, and emotional balance, and thus teach the brain, and body to work in harmony. Since, Yoga has a holistic approach encompassing body, mind and soul and therefore the Yoga is a combination of physiotherapy, psychotherapy, and spiritual therapy.
There is a large body of literature and scientific data regarding the pharmacological and psychosocial interventions and the rehabilitation of patients with schizophrenia. The efficacy of Yoga has not been much examined in schizophrenia. However, several features of Yoga make it an attractive option for improving psychopathology in schizophrenia. Yogic practices, though started to create discipline in an individual's holistic life, gradually experimented whether it could help to improve mental health of the patients suffering from various disorders starting from anxiety related disorders, to psychosomatic, to neurological disorders and presently reaching to major mental disorders like schizophrenia, and proved its efficacy.
Vahia[1] reported a study of patients comprising of anxiety neurotics, neurotic depression, conversion reaction, mixed neurosis and psychosomatic disorder and observed significant improvement, and further studies also well established its efficacy in various anxiety disorders like obsessive-compulsive disorder;[2] on anxiety, depression, and tension.[3,4] Yoga has proved its efficacy in treating patients suffering from mild to moderate level of depression,[5,6] and is associated with improved mood, and may be a useful way of reducing stress during inpatient psychiatric treatment.[7]
Yogic practice, including physical postures, Yoga breathing, and meditation and guided relaxation improved delayed recall of spatial information in children.[8] Sharma et al.[9] demonstrated that the yogic practice could improve executive functions such as manipulation of information in the verbal working memory, attention span and the visuo-motor speed of the depressives in patients suffering from major depression. The practice of Yoga regulates body physiology through control of posture, breathing, and meditation. Yoga could bring a significant reduction in scores on anxiety, depression and tension as well as an increase in well-being as found in Yoga group.[4]
Duraiswamy et al., and Mukherjee et al.[10,11] demonstrated that the yogic practice, in conjunction with conventional medical treatment, may improve schizophrenic symptoms, social and occupational functioning, quality of life, discipline, and adaptive functioning among schizophrenia patients. However, their assessment on psychopathology was restricted on limited parameters. Duraiswamy et al.[10] used total scores of Positive and Negative Syndrome Scale (PANSS) for analyzing the effects of interventions, and also their participants were not evaluated with General Psychopathology Scale of PANSS. Similarly, Mukherjee et al.[11] evaluated the efficacy of Yoga therapy by using Brief Psychiatric Rating Scale (BPRS).
A study conducted by Visceglia and Lewis,[12] investigated the effects of a Yoga therapy program on symptomatology and quality of life in adults with schizophrenia. After the 8-weeks Yoga therapy program significant improvement were found in positive and negative symptoms of schizophrenia, general psychopathology, activation, paranoia, depression, and in perceived quality of life in physical and psychological domains. Another study conducted by Behere et al.,[13] demonstrated that Yoga therapy could be a useful add-on treatment to improve facial emotion recognition deficits, psychopathology and socio-occupational functioning in antipsychotic-stabilized patients with schizophrenia. Recently Varambally et al.,[14] studied the efficacy of Yoga as an add-on treatment in outpatients with schizophrenia and their findings also suggested a significant improvement in PANSS and total PANSS scores as well as in the social functioning. The present study was conducted to determine the efficacy of Yoga therapy (package used by Mukherjee et al.[11]) on reduction of psychopathology of patients with schizophrenia.
Aims of the study
The objective of the present study is to determine the efficacy of Yoga therapy as an adjunctive therapy for the management of psychopathology of patients having chronic schizophrenia.
Hypothesis of the study
There will be no significant difference in the baseline assessment and follow-up assessment of psychopathology between schizophrenia patients getting Yoga therapy along with medications and those getting only medications.
MATERIALS AND METHODS
Design
Pre- and post-test control group design was used for the study.[15] Patients were assigned to Yoga therapy using block randomization, and same numbers of patients were also kept for the control group. The randomization list was generated by using a lottery method. One group was assigned for Yoga therapy along with pharmacotherapy (experimental group) and the other group for Pharmacotherapy alone (control group).
Setting and participants
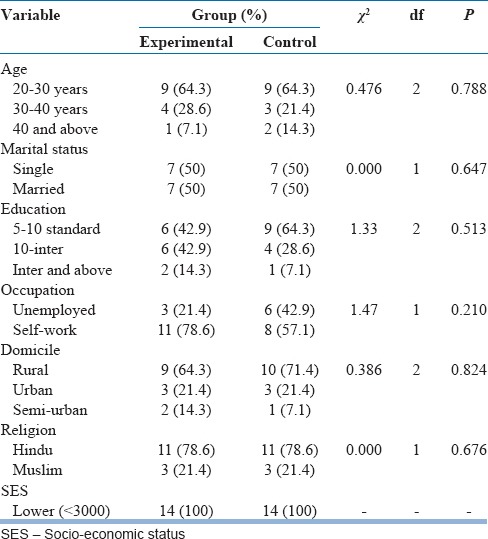
The study was conducted in Ranchi Institute of Neuro-Psychiatry and Allied Sciences, Ranchi (India). After 2 weeks of admission in the hospital, based on purposive sampling technique,[16] patients were screened from different wards of the institute and a total of 30 patients, who fulfilled inclusion and exclusion criteria were included in the study. All patients were having chronic schizophrenia and were not on regular medication before the admission in the hospital. The patients were on risperidone, and olanzapine, and the dozes were regulated according to the requirements of the patients. Only male schizophrenia patients in the age range of 20–50 years with minimum 2 years duration of illness, who had mild to moderate level of symptoms, were included in the study. Patients with a history of substance dependence, mental retardation, organic mental disorder, head injury and other neurological disorders were excluded. One patient from each group dropped out. Demographic statistics were summarized in Table 1. Both groups were comparable on age, sex, marital status, education, occupation, domicile, religion and family income variables. In clinical characteristics also the group were comparable in respect to age of onset, mode of onset, course of illness, family history of mental illness except duration of illness which was significantly different at 0.05 level (χ2 = 4.762, P < 0.05).
Table 1.
Demographic characteristics of experimental and control group
Assessment
The baseline and follow-up assessment of both the group was done using PANSS, which is used as a primary outcome measure. PANSS is a 30-item rating scale designed to assess presence and absence, and severity of positive, negative and general psychopathology of schizophrenia patients. The scale was developed from the content of BPRS and the Psychopathology Rating Scale. All 30 items are rated on a 7 point scale (1 = absent, 2 = minimal, 3 = mild, 4 = moderate, 5 = moderate-severe, 6 = severe, and 7 = extreme). Reliability coefficients for the Positive and Negative Scales are 0.73 and 0.83, respectively.[17] Both positive and negative scales is correlated strongly with the Composite Scale and coefficients of similar magnitude (r = 0.59 and −0.61).[17] The General Psychopathology Scale similarly has high internal consistency, producing a α coefficient of 0.79.[17]
Intervention
Participants in the intervention group practiced postures/asanas included: Standing postures (Tarasana, Trikonasana, Lolasana, Utkatasana, Santulanasan, Tadasan; Surya Namaskar – 2 chakra with mantra, Savasan); Lying posture – supine (Uttanpadasan, Uttanasan, Sarvangasan, Pastchimotasan, Pavan Muktasan, Naukasan, and Savasan); Lying posture – prone (Bhujangasan, Salabhasan, Dhanurasan, and Makrasan); Sitting posture (Vajrasan, Shasakasan, Gomukasan, Ardhmatsyendrasan, Yogmudrasan, and Padmasan); and Pranayam-breathing exercise (Bhastrika, Kapal-bhati, Anulom vilom, Bhramari, and Omkar). The patients attended Yoga therapy everyday, except holidays, for about one and half hours including motivational and feedback session, for about 1 month. All the sessions were conducted and monitored under the guidance of well-trained Yoga teacher of the institute. At the beginning of every Yoga session the patients were motivated by explaining the rationale and positive effects of particular postures/asanas.
Data analysis
Statistical analysis was carried out using the Statistical Package for Social Sciences (SPSS) version 17 (SPSS Inc., Chicago, IL, USA). Level of significance was set to P < 0.05. Since the sample size was small and, data were on category variable; nonparametric statistical techniques were used to interpret the data. Socio-demographic and clinical characteristics of experimental and control group were compared using χ2-test if all expected cell counts exceeded 5; otherwise Fisher exact tests were used. To know the therapeutic outcome of Yoga therapy (to compare the data obtained by the pre- and post-assessments score for the same group) the Wilcoxon signed ranks test was used. To know baseline and follow-up differences of both the group, the Wilcoxon Mann–Whitney test was used to compare between the pre- and post-assessment scores (PANSS) of experimental and control group.
RESULTS
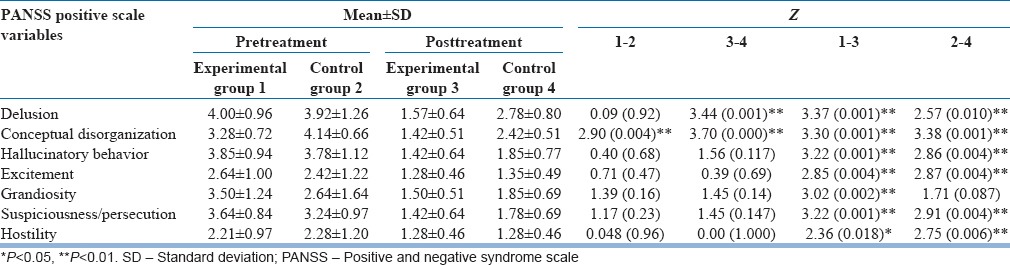
Baseline and follow-up assessment of positive symptoms for each group are given in Table 2. At baseline comparison between study and control group, there was no significant difference on positive symptoms of PANSS except on the conceptual disorganization (Z = 2.90, P < 0.01). At follow-up comparison between both groups, there was significant difference on domains of positive symptoms of PANSS, such as delusions (Z = 3.442, P < 0.001) and conceptual disorganization (Z = 3.70, P < 0.001). Because of the baseline difference on scores of conceptual disorganization, improvement score were calculated of both the group. After that, statistical analysis for differences of improvement scores were calculated, and we did not found any significant difference between both the group (Z = 83.00, P > 0.05). On other domains of positive symptoms of PANSS, no significant differences were found. On positive symptoms of PANSS, there was a significant difference between pre- and post-test comparison of the both experimental and control group.
Table 2.
Comparison of positive symptoms and its resolution for both experimental and control groups
Baseline and follow-up assessment of negative symptoms for each group is given in Table 3. At baseline, there was no significant difference between both experimental and control group. At follow-up assessment, schizophrenia patients who were on Yoga Therapy showed better improvement in comparison to control group on domains of negative symptoms such as blunted affect (Z = 4.06, P < 0.001), emotional withdrawal (Z = 2.95, P < 0.01), passive social withdrawal (Z = 2.59, P < 0.01) and difficulty in abstract thinking (Z = 2.60, P < 0.01). On other domains of negative symptoms such as poor rapport and lack of spontaneity, the experimental group shown better improvement in comparison to the control group; however, improvement differences were not statistically significant. On negative symptoms of PANSS, a significant difference was found between pre- and post-test comparison of the both experimental and control group.
Table 3.
Comparison of negative symptoms scores and its resolution for both experimental and control groups
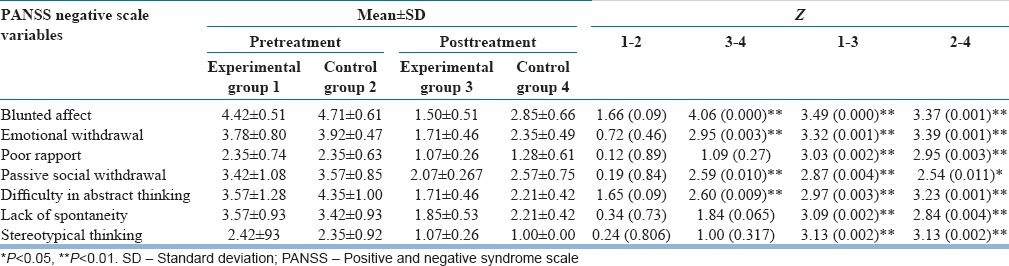
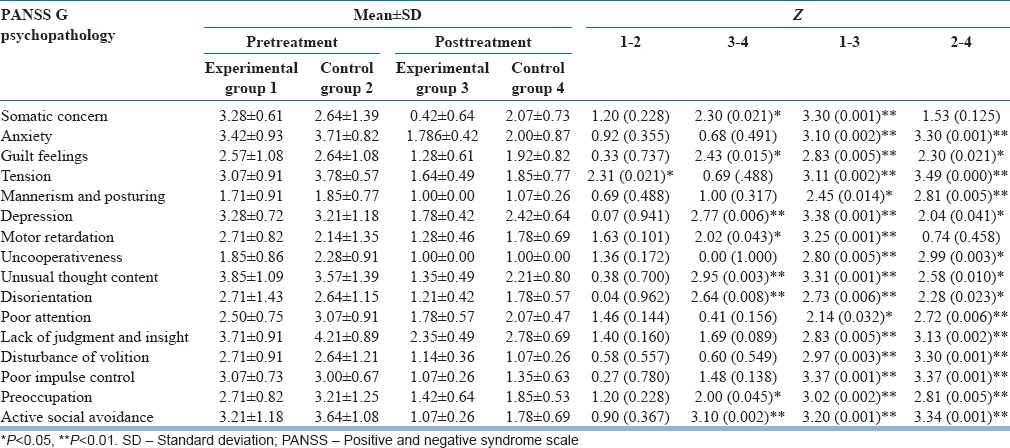
Table 4 shows baseline and follow-up assessment of general psychopathology for both experimental and control group. At baseline scores of general psychopathology, there was statistically no significant difference between both experimental and control group except scores on tension (Z = 2.31, P < 0.05). At follow-up assessment, schizophrenia patients who were on Yoga therapy showed better improvement in comparison to control group on domains of general psychopathology such as somatic concern (Z = 2.30, P < 0.05), guilt feelings (Z = 2.43, P < 0.05), motor retardation (Z = 2.02, P < 0.05), depression (Z = 2.77, P < 0.01), unusual thought content (Z = 2.95, P < 0.01), disorientation (Z = 2.64, P < 0.01), preoccupation (Z = 2.00, P < 0.05) and active social avoidance (Z = 3.10, P < 0.001). There was a significant difference between pre- and post-test comparison of the both experimental and control groups except motor retardation for the control group. Patients of the control group did not show significant improvement in the area of motor retardation; however, patients who were on Yoga Therapy showed significant improvement in this domain.
Table 4.
Comparison of general psychopathology scores and its resolution for both experimental and control group
DISCUSSION
To our knowledge, this is the first study demonstrating the efficacy of Yoga therapy with inpatient schizophrenia group and assessing broad domains of positive and negative symptoms as well as general psychopathology. Findings of present research study reveal that along with pharmacotherapy Yoga therapy is helpful in managing positive symptom such as delusions, and negative symptoms such as blunted affect, emotional withdrawal, passive social withdrawal and difficulty in abstract thinking. Present research findings are similar to that of Duraiswamy et al.[10] and they have also documented the effectiveness of Yoga therapy in schizophrenia patients. They compared Yoga therapy group with physical training group, and found that schizophrenia patients who were on Yoga therapy improved more than those with physical training group. They have reported that along with pharmacotherapy Yoga therapy is helpful in the management of negative symptoms of schizophrenia patients, but it is found less effective in the management of positive symptoms. Similarly, the recent study reported by Varambally et al.[14] reported a significant improvement in PANSS and total PANSS scores as well as in the social functioning of patients having schizophrenia after Yoga therapy.
On general psychopathology domains such as somatic concern, guilt feelings, motor retardation, depression, unusual thought content, disorientation, preoccupation and active social avoidance Yoga therapy group showed better improvement in comparison to the control group. Findings of the present study are consistent with the findings of Mukherjee et al.,[11] who have reported that the practice of Yoga increases positive moods decreases negative moods. Shapiro and Cline[18] also reported that Yoga practice increases energy level regardless of the âsana practiced. Visceglia and Lewis,[12] found significant improvement in positive and negative symptoms of schizophrenia, general psychopathology, activation, paranoia, depression, and in perceived quality of life in physical and psychological domains of adults with schizophrenia after the 8-week Yoga therapy program. Behere et al.,[13] also suggested that Yoga therapy could be a useful add-on treatment as they improved facial emotion recognition deficits, psychopathology and socio-occupational functioning in antipsychotic-stabilized patients with schizophrenia.
Since the schizophrenic disorder is associated with mood changes particularly depression, anxiety, fatigue, etc., above studies validate present findings. Improvements were observed in their positive emotional state with subjective reporting of decreased levels of negative mood and fatigue and a better mental function after yogic practices. Present research findings are similar to that of Duraiswamy et al.,[10] Mukherjee et al.,[11] Butler et al.,[6] and Shapiro et al.[5] they have also reported that Yoga can work well with the moderate level of depression and associated quality of life. The above findings suggest how well Yoga could be utilized to improve psychopathology of the patients. There are studies that proved Yoga could help positive mental health.[19] Stress is associated with the worsening of schizophrenic symptoms[20] and Yoga could help to handle stress more effectively,[21] and that may be resulted in better rating in the experimental group.
Before concluding, we would like to share to the future researchers on this topic in the beginning of our study we were frustrated because getting cooperation of the schizophrenic patients was found little hard. However, the things began to change after 1 week and could see that patients were waiting in the ward with properly dressed and encouraging others to participate in Yoga. Hence, it is very important to establish very good rapport with the patients and to impart motivation in them as we could. The current findings should be interpreted in light of the limitations in the study like small sample size, only male inpatients were included, groups could be controlled on limited parameters and Yoga interventions were given only for a limited period of time.
CONCLUSION
Considering the various positive effects of Yoga as revealed in this study, along with pharmacological management and psychosocial interventions the patients with schizophrenia could be exposed to Yoga therapy as a daily routine for improving psychopathology and overall functioning. In Indian cultural environment patients suffering from schizophrenia can possibly be more easily motivated to undergo Yoga therapy and internalize its beneficial effects.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Vahia NS. A therapy based upon some concepts prevalent in India. Indian J Psychiatry. 1973;2:7–14. [Google Scholar]
- 2.Shannahoff-Khalsa DS, Beckett LR. Clinical case report: Efficacy of yogic techniques in the treatment of obsessive compulsive disorders. Int J Neurosci. 1996;85:1–17. doi: 10.3109/00207459608986347. [DOI] [PubMed] [Google Scholar]
- 3.Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K. Yoga for anxiety: A systematic review of the research evidence. Br J Sports Med. 2005;39:884–91. doi: 10.1136/bjsm.2005.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kozasa EH, Santos RF, Rueda AD, Benedito-Silva AA, De Ornellas FL, Leite JR. Evaluation of siddha samadhi yoga for anxiety and depression symptoms: A preliminary study. Psychol Rep. 2008;103:271–4. doi: 10.2466/pr0.103.1.271-274. [DOI] [PubMed] [Google Scholar]
- 5.Shapiro D, Cook IA, Davydov DM, Ottaviani C, Leuchter AF, Abrams M. Yoga as a complementary treatment of depression: Effects of traits and moods on treatment outcome. Evid Based Complement Alternat Med. 2007;4:493–502. doi: 10.1093/ecam/nel114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butler LD, Waelde LC, Hastings TA, Chen XH, Symons B, Marshall J, et al. Meditation with yoga, group therapy with hypnosis, and psychoeducation for long-term depressed mood: A randomized pilot trial. J Clin Psychol. 2008;64:806–20. doi: 10.1002/jclp.20496. [DOI] [PubMed] [Google Scholar]
- 7.Lavey R, Sherman T, Mueser KT, Osborne DD, Currier M, Wolfe R. The effects of yoga on mood in psychiatric inpatients. Psychiatr Rehabil J. 2005;28:399–402. doi: 10.2975/28.2005.399.402. [DOI] [PubMed] [Google Scholar]
- 8.Manjunath NK, Telles S. Spatial and verbal memory test scores following yoga and fine arts camps for school children. Indian J Physiol Pharmacol. 2004;48:353–6. [PubMed] [Google Scholar]
- 9.Sharma VK, Das S, Mondal S, Goswami U, Gandhi A. Effect of sahaj yoga on neuro-cognitive functions in patients suffering from major depression. Indian J Physiol Pharmacol. 2006;50:375–83. [PubMed] [Google Scholar]
- 10.Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia – A randomized controlled trial. Acta Psychiatr Scand. 2007;116:226–32. doi: 10.1111/j.1600-0447.2007.01032.x. [DOI] [PubMed] [Google Scholar]
- 11.Mukherjee P, Kumar D, Singh PK, Singh AR. Effect of yoga on social-adaptive functioning of psychiatric patients. Indian J Clin Psychol. 2008;35:74–81. [Google Scholar]
- 12.Visceglia E, Lewis S. Yoga therapy as an adjunctive treatment for schizophrenia: A randomized, controlled pilot study. J Altern Complement Med. 2011;17:601–7. doi: 10.1089/acm.2010.0075. [DOI] [PubMed] [Google Scholar]
- 13.Behere RV, Arasappa R, Jagannathan A, Varambally S, Venkatasubramanian G, Thirthalli J, et al. Effect of yoga therapy on facial emotion recognition deficits, symptoms and functioning in patients with schizophrenia. Acta Psychiatr Scand. 2011;123:147–53. doi: 10.1111/j.1600-0447.2010.01605.x. [DOI] [PubMed] [Google Scholar]
- 14.Varambally S, Gangadhar BN, Thirthalli J, Jagannathan A, Kumar S, Venkatasubramanian G, et al. Therapeutic efficacy of add-on yogasana intervention in stabilized outpatient schizophrenia: Randomized controlled comparison with exercise and waitlist. Indian J Psychiatry. 2012;54:227–32. doi: 10.4103/0019-5545.102414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campbell DT, Stanley JC. Experimental and quasi – Experimental designs. In: Gage NL, editor. Handbook of Research on Teaching. Chicago: Rand McNally; 1963. [Google Scholar]
- 16.Cochran WG. New York: John Willey and Sons; 1963. Sampling Techniques. [Google Scholar]
- 17.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 18.Shapiro D, Cline K. Mood changes associated with Iyengar yoga practices: A pilot study. Int J Yoga Therap. 2004;14:35–44. [Google Scholar]
- 19.Brown RP, Gerbarg PL. Sudarshan Kriya Yogic breathing in the treatment of stress, anxiety, and depression. Part II – Clinical applications and guidelines. J Altern Complement Med. 2005;11:711–7. doi: 10.1089/acm.2005.11.711. [DOI] [PubMed] [Google Scholar]
- 20.Yeap S, Thakore JH. Stress axis dysfunction in schizophrenia. Eur Psychiatry. 2005;20(Suppl 3):S307–12. doi: 10.1016/s0924-9338(05)80181-6. [DOI] [PubMed] [Google Scholar]
- 21.Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: A randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255–9. doi: 10.1016/s0165-0327(99)00079-8. [DOI] [PubMed] [Google Scholar]


