Preface
After decades of discovery, inherited variation in approximately 20 genes affecting about 80 medications has been identified as actionable in the clinic. Additional somatically acquired genomic variants direct the choice of “targeted” anticancer drugs for individual patients. Current efforts that focus on the processes required to appropriately act on pharmacogenomic variability in the clinic are systematically moving pharmacogenomics from discovery to implementation as an evidenced-based strategy for improving the use of medications, thereby providing an important cornerstone for precision medicine.
Introduction
Pharmacogenomics focuses on the identification of genome variants that influence drug effects, typically via alterations in a drug’s pharmacokinetics (i.e., absorption, distribution, metabolism, elimination) or via modulation of a drug’s pharmacodynamics (e.g., modifying a drug’s target or perturbing biological pathways that alter sensitivity to the drug’s pharmacological effects). For diseases other than cancer and infectious diseases, the genome variations of interest are primarily in the germline DNA, either inherited from parents or de novo germline sequence changes that alter the function of gene products. In cancer, both inherited genome variations and somatically acquired genome variants can influence response to anticancer agents. For infectious diseases, genomic variation in the infectious agents themselves may alter their sensitivity to antimicrobials.1 Advances in genome interrogation technology and in analytical approaches have facilitated evolution of the discovery paradigm from candidate gene studies to more agnostic genomewide analyses of populations of patients who have been characterized for specific drug response phenotypes (e.g., toxicity or desired pharmacologic effects). In fact, current technologies for genome sequence interrogation are sufficiently robust that rigorously defining the drug response phenotype has become the more difficult component of pharmacogenomics research. Once pharmacogenomic relationships have been discovered and validated, there are many obstacles to their translation into clinical practice. Such translation requires that effective alternative therapy is available for those with “high risk” genotypes, and requires improvements in health care systems, structured approaches to guide prescribing (e.g., algorithms), and implementation of point-of-care electronic clinical decision support (CDS) to make it feasible to appropriately utilize genetics to guide drug prescribing.
A decade ago, we laid out a vision of how evolving genome technologies could be deployed to facilitate pharmacogenomic discoveries,2 and here we extend this to address how discoveries can best be translated into tools to optimize the use of medications in the clinic.
Review
Discovery research vs clinical implementation of pharmacogenomics---evolution to the clinic
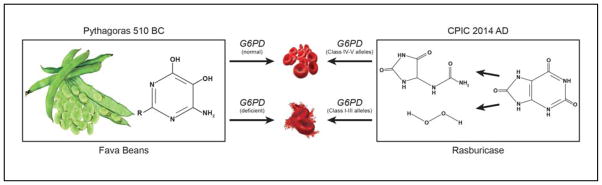
The earliest origins of pharmacogenomics are unclear; perhaps it was in 510 BC when Pythagoras reported that a subset of people ingesting fava beans experienced potentially fatal hemolytic anemia, whereas others did not (Figure 1). Centuries later this was shown to be due to an inherited deficiency of glucose-6-phosphate dehydrogenase (G6PD), which also predisposes to hemolysis from rasburicase and the antimalarial primaquine.3 In 1909, studying another bean (Phaseolus vulgaris), Danish pharmacist Wilhelm Johannsen coined the terms genotype and phenotype, linking genotype to the effects of volatile organics, a presage to pharmacogenetics. A clustering of drug metabolizing enzyme activities by racial groups strongly suggested a genetic component to population variation.4,5
Figure 1.
Pythagoras is thought to have banned the consumption of fava beans (vicia fava) after observing that their ingestion caused hemolytic anemia in a subset of people (left). This was subsequently shown to occur predominantly in persons with glucose-6-phosphate dehydrogenase (G6PD) deficiency, primarily persons who inherited the Class II “Mediterranean allele” of G6PD. The chemical moieties in fava beans thought to cause hemolysis in G6PD-deficient individuals are isouramil (R=OH) and divicine (R=NH2), pyrimidine aglycones of two glucosides found in fava beans. (vicine and convicine). Multiple medications also cause oxidative stress and erythrocytes of G6PD deficient individuals produce insufficient NADPH to protect from oxidative damage, and hemolysis and methemoglobinemia can ensue.39 Rasburicase is a recombinant form of urate oxidase that is used clinically to lower uric acid levels in the treatment of tumor lysis syndrome (right). The oxidative stress caused by hydrogen peroxide produced when rasburicase cleaves uric acid to allantoin and hydroperoxide is more likely to cause hemolytic anemia and methemoglobinemia in persons who have inherited G6PD deficiency; rasburicase is contraindicated in G6PD deficient individuals.109
In 1959, Friedrich Vogel first coined the term “pharmacogenetics,”6 a concept bolstered by landmark studies of Elliott Vesell and George Page showing that the pharmacokinetics of antipyrine were much more similar in monozygotic twins than in dizygotic twins.7 The clinical relevance of pharmacogenetics was reinforced when family studies indicated that racial differences in isoniazid metabolism and its side effect of peripheral neuritis were inherited as an autosomal recessive trait.8,9 Decades later the genetic polymorphism in isoniazid acetylation was shown to be caused by inherited variants in the gene encoding N-acetyltransferase 2 (NAT2).10,11
Additional family studies in the 1960s–1980s documented the pattern of inheritance for many drug effects, which eventually led to molecular genetic studies that revealed the inherited determinants for many of these traits, with CYP2D6 being the first polymorphic human drug metabolizing gene to be cloned and characterized in 1987.12 In the 1990s, the potential clinical utility of pharmacogenomics was clearly illustrated for several genes,13,14 including the inherited deficiency of thiopurine-methyltransferase and hematopoietic toxicity from mercaptopurine and azathioprine15 although implementation in the clinic progressed slowly at that time.16
Like most areas of genetics research, pharmacogenetic discoveries were accelerated by the human genome project and by advances in technologies for genome-wide interrogation of genetic variation. This shortened the timeline for discovery and enabled agnostic genome-wide studies of populations of patients who had been phenotyped for specific drug effects (treatment efficacy or toxicity), often leading to the identification of unanticipated genetic variants that were statistically associated with drug effects. These genomewide strategies helped introduce “pharmacogenomics” into the lexicon.17
Discoveries emerging from genome-wide or candidate gene strategies require independent validation before their translation into clinical diagnostics, and this can be facilitated by elucidation of the underlying mechanism(s) by which genome variation alters drug response. Because genetic variants often differ according to ancestry, this can confound the translation of pharmacogenetic traits from one population to another, as recently exemplified by genetic polymorphisms in CYP2C9 and VKORC1 and their population-specific influence on warfarin’s anticoagulant effects.18 Furthermore, it is becoming increasingly evident that many drug effects are influenced by multiple variants in the same gene (some of which are rare) and/or by variants in multiple genes within the same patient. The UK’s 100,000 Genomes Project and the US NIH’s Pharmacogenomics Research Network are two of many ongoing efforts to facilitate genome discoveries and their translation into new diagnostics that may eventually be used to optimize the selection and dosing of medications in individual patients. Discovery and translation of inherited determinants of drug response and somatically acquired genome variants in cancer are prominent pharmacogenomic components of these and other initiatives.
Criteria for implementing diagnostic tests in the clinic; clinical implementation of pharmacogenomics compared to other genomic tests
It is widely stated that in order for a test to be used in clinical care, it must meet criteria of analytic validity, clinical validity, and clinical utility.19 Several pharmacogenes are not trivial in terms of developing tests with analytic validity.20 Clinical utility involves assessing whether the use of the test leads to improved health outcomes for patients who are subject to testing, and an assessment of the risks that occur as a result of testing. However, there is substantial heterogeneity as to precisely what outcome measures constitute clinical utility.21,22 Some have broadened such assessments to go beyond the clinical utility for the tested individuals to include an assessment of the impact of broader use of testing on the entire health care system, including weighing the costs of genetic testing versus the costs of other health care interventions, and unintended consequences on behavior of clinicians. For example, the introduction of a pharmacogenetic screening policy in Hong Kong to test for the HLA-B*1502 allele prior to prescribing antiepileptic drugs (to avoid use of carbamazepine in those at high risk for severe skin reactions) had the unintended consequence of clinicians foregoing prescribing carbamazepine at all and instead prescribing phenytoin. Because phenytoin can also cause severe skin reactions, but the risk factors are not as well defined, the overall incidence of severe skin reactions remained unchanged after implementing the HLA-B-specific screening policy.23 For purposes of this review, we focus on the clinical utility of pharmacogenomic testing for individual patients, without consideration of possible untoward public health consequences based on unintended (and often unnecessary) changes in clinician prescribing behaviors.
With the continuing decline in cost of sequencing, many have predicted that in the not-too-distant future, every individual will have their entire inherited genome sequenced early in life, with the results available for clinical use throughout a lifetime of health care. Assuming that this will be true (at least to some extent), we have called for a shift away from debating whether specific pharmacogenes should be tested prior to using specific drugs, and toward a model in which clinicians are provided with guidelines on how genomic variants should be interpreted and deployed to improve prescribing. This assumption underlies the efforts of the Clinical Pharmacogenetics Implementation Consortium (CPIC),24,25 an open international group that creates standardized, evidence-based, peer-reviewed, publicly available, nonprofit gene/drug guidelines for how to use genomic data to inform prescribing.
The decision as to whether each set of pharmacogenomic results has the necessary evidence to support analytic validity, clinical validity, and clinical utility to warrant use in prescribing depends on many factors.21 Analytic validity will depend on the quality of the data from genetic tests, and on performance characteristics such as positive and negative predictive value. Many types of data can be used to evaluate clinical validity and utility, including the penetrance of genetic variation on drug effects based on retrospective studies, the mechanism(s) by which genetic variation influences drug effects or a relevant endophenotype (such as drug metabolizing enzyme activity), in vivo pharmacokinetic or other functional studies, in vitro functional studies, pre-clinical and clinical studies linking pharmacologic effects or drug concentrations to genomic variation, case reports, family studies, and randomized clinical trials comparing outcomes of genetically-based prescribing versus “standard of care.” Other factors that are considered in deciding on the actionability of pharmacogenomic variation include the therapeutic index of a drug, the severity of drug toxicity, the severity of the underlying disease, and the consequences of suboptimal prescribing.
A key consideration for actionability of a gene/drug relationship is based on the availability of and evidence for alternative therapy, and may partly depend upon the mechanism of the gene/drug association. If the gene is affecting the drug by virtue of affecting active drug pharmacokinetics (e.g. CYP3A5 catabolism of tacrolimus), there may be substantial literature supporting a dose adjustment based on extrapolation of pharmacokinetic effects, analogous to decisions often made in the clinic based on altered renal function, liver function, or age. Such dose adjustment decisions are particularly defensible if the drug is one for which therapeutic drug monitoring (based on measures of drug concentration in blood) is readily available. If genetic tests indicate that a particular drug is not effective in those with the high-risk genotype (e.g. those homozygous for inactive CYP2D6 alleles cannot anabolize codeine to its active metabolite, morphine), then the recommendation for alternative therapy will be dependent upon weighing the evidence for both the efficacy and possible toxicity of an alternative medication; for codeine, there are generally several alternative opiate analgesics available with reasonable data on doses likely to achieve comparable analgesia.26 If genetic tests indicate an extremely high risk for a serious adverse event (e.g. carriers of the HLA-B*57:01 allele have a high risk of hypersensitivity to abacavir),27,28 the alternative therapy would ideally be equally effective with an acceptable risk of adverse effects (which may or may not be influenced by other genetic variants).
Some treatment efficacy decisions are not all-or-none, but rather are based on a range of probabilities: for example, there are substantial data that efficacy against breast cancer recurrence is reduced in patients who have inherited two defective CYP2D6 alleles, as they have much lower levels of the active metabolite endoxifen than the majority of the population,29–34 but whether the best alternative therapy is a different drug (e.g. a different selective estrogen receptor modulator) or an altered dose of tamoxifen is not clear, particularly in premenopausal women for whom there are a dearth of data supporting alternatives. These cases are the most difficult: it is clear from pharmacogenomics that the drug or drug dose is not optimal in a patient with the high-risk genotype compared to the majority of the population, but a lack of clinical data for alternative therapies makes it difficult or impossible to recommend alternative medications.
CPIC considers all such evidence in prioritizing which gene/drug pairs are clinically actionable. Given the high bar required for clinical actionability, the number of actionable inherited genes (those that have at least one actionable “high risk” diplotype) and the list of medications for which clinical actions can be recommended (pharmacogenetically “high risk” drugs) is relatively short (Table 1). We acknowledge that there are additional medications for which regulatory agencies include pharmacogenomic information in their labels;35–37 however, not all such mentions are actionable. Information on genetic variation is sometimes included even when the effects are modest (and therefore don’t translate into changes in the prescribing sections of the drug label), and have been included for some drugs when the evidence is weak or conflicting.
Table 1.
Actionable germline genetic variation and associated medications
| Genetic Variation | Medication |
|---|---|
| TPMT | mercaptopurine, thioguanine, azathioprine |
| CYP2D6 | codeine, tramadol, tricyclic antidepressants |
| CYP2C19 | tricyclic antidepressants, clopidogrel, voriconazole |
| VKORC1 | Warfarin |
| CYP2C9 | warfarin, phenytoin |
| HLA-B | allopurinol, carbamazepine, abacavir, phenytoin |
| CFTR | Ivacaftor |
| DPYD | fluorouracil, capecitabine, tegafur |
| G6PD | rasburicase |
| UGT1A1 | irinotecan, atazanavir |
| SLCO1B1 | simvastatin |
| IFNL3 (IL28B) | interferon |
| CYP3A5 | tacrolimus |
From https://www.pharmgkb.org/cpic/pairs (accessed May 7, 2015)
One item to note: there are currently very few examples of actionable pharmacogenes that also carry a disease risk. The only examples thus far are UGTIA1 and Gilbert’s disease,38 and G6PD and hemolytic anemia.39 Thus, many of the ethical concerns affecting clinical implementation of “disease risk” genomics have less relevance for pharmacogenomics.40
Critical issues for clinical implementation of pharmacogenomics
Drugs and genes
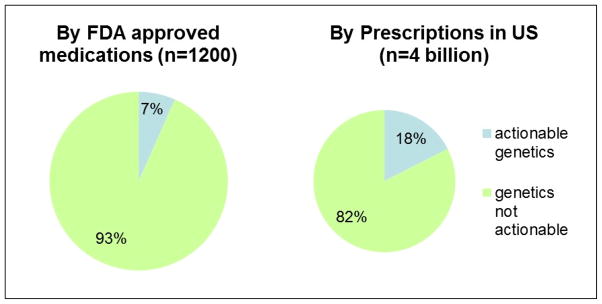
There are more than 1200 individual molecular entities approved as drugs by regulatory agencies in the US, Europe and Asia (i.e., FDA41, -EU-EMA35 and PMDA.37 Although about 15% of EU-EMA and US-FDA approved medications contain pharmacogenomic information in their label35 http://www.fda.gov/drugs/scienceresearch/researchareas/pharmacogenetics/ucm083378.htm), only a subset of these are deemed actionable. As summarized in Figure 2, the use of only about7% of medications have actionable germline pharmacogenetics (https://www.pharmgkb.org/cpic/pairs, corresponding to CPIC level A and level B genes/drugs---corresponding to actionable prescribing recommendations). Interestingly, in the US, these medications constitute ~18% of all prescriptions, indicating that there is a slight overrepresentation of pharmacogenomically high-risk medications among highly-prescribed medications (Figure 2).42 Thus far, only 17 of ~ 18,000 human genes are considered clinically actionable for germline pharmacogenomics (https://www.pharmgkb.org/cpic/pairs). Not only is most human germline genetic variation unlikely to be actionable for medication prescribing, pharmacogenomics is unlikely to be useful for improving prescribing for the majority of drugs. However, for that relatively small set of medications for which genomics is actionable, prescribing could be improved and outcomes optimized if genetic testing were more widely and appropriately deployed clinically. And the number of such actionable gene drug pairs continues to grow, albeit at a relatively slow pace.
Figure 2.
Approximately 7% percentage of medications (FDA approved) are affected by actionable inherited pharmacogenes (right), whereas approximately 18% of outpatient prescriptions in the US are affected by actionable germline pharmacogenomics (left),42 illustrating that several pharmacogenetically high-risk drugs are commonly prescribed.
Somatically acquired genomic variation
A special case of pharmacogenomics applies to somatically acquired genomic variants that are specific to cancer tissue. In some cancer types, somatic genomic variations can guide the choice of anticancer agents, by virtue of identifying which malignancies are more or less likely to respond to specific anticancer agents.43,44 The recognition that cancer tissue can be distinguished from normal host tissue by the presence of specific genomic abnormalities predates the human genome project, with early examples of genomic abnormalities such as unfavorable ploidy in neuroblastoma,45 and cytogenetic abnormalities in acute lymphoblastic leukemia,46 being used to determine the composition and aggressiveness of cytotoxic chemotherapy. In more recent years, the genetic testing of malignancies has become more specific, as several anticancer agents have been developed that are directed against or proven to be much more effective for tumors that harbor specific acquired genetic variants (Table 2). The US FDA has generally approved companion diagnostics concomitantly with new targeted anticancer agents, whereas the EU EMA requirements have been somewhat less stringent47, but proposed changes in the EU framework would lead to greater harmonization.48
Table 2.
Actionable somatic genome variants in cancer cells and associated medications1
| Genetic Abnormality2 | HGVS Nomenclature3 | Target4 | Medications | Disease5 |
|---|---|---|---|---|
| AKT Mut (Act) | p.Glu17Lys | mTOR | sirolimus, everolimus | RCC |
| BCR-ABL (SV) | t(9;22) (q34.1;q11.21) | ABL | imatinib, dasatinib | CML, Ph+ ALL |
| BCR-ABL (SV + Mut) | p.Val299Leu | ABL | bosutinib, nilotinib | imatinib resistant CML |
| BCR-ABL (T135I) | p.Thr135Ile | ABL | ponatinib | CML, Ph+ ALL |
| BCR-ABL (SV) | t(9;22) (q34.1;q11.21) | SRC | dasatinib | CML, Ph+ ALL |
| BRCA1/2 variants | too numerous to list | PARP | olaparib | ovarian |
| BRAF SNVs (V600E/K) | p.Val600Glu, p.Val600Lys, p.Val600Asp | BRAF | dabrafenib, vemurafenib | melanoma |
| BRAF SNVs (V600) | p.Val600Glu, p.Val600Lys, p.Val600Asp | MEK | trametinib | melanoma |
| EGFR (Ex 19 del., SNV L858R) | p.Glu746_Ala750del, p.Leu858Arg | EGFR | afatinib, erlotinib | NSCLC (EGRF+) |
| EGFR Mut (Act, Amp) | p.Glu746_Ala750del, p.Leu858Arg | EGFR | gefitinib | NSCLC (EGRF+) |
| EGFR+ & WT KRAS | NA | EGFR | cetuximab, panitumumab | EGRF+ colon (WT KRAS) |
| EML-ALK (SV) | inv(2)(p21p23) | ALK | crizotinib | NSCLC |
| FLT3 CNV (Amp) | p.D600_L601insFREYEYD, p.Asp835Tyr | FTL3 | sunitinib, sorafenib | AML |
| HER2 (Amp) | NA | ERBB2 | lapatinib, trastuzumab | HER2+ breast |
| KIT (Act Mut) | p.Trp557_Lys558del, p.Asp579del, p.Val559Asp | KIT | imatinib, sunitinib | RCC, GIST |
| PDGFR (Mut, SV) | p.Asp842Val | PDGFR | sunitinib, imatinib | RCC, GIST, pancreas |
| PI3K (Mut, Amp) | PIK3CA p.Glu542Lys, p.Glu545Lys; p.His1047Arg, p.His1047Leu | PI3K | idelalisib | CLL, NHL |
| RARA (SV, gene fusion) | t(15;17)(q24;q21) | RARA | tretinoin, alitretinoin | APL CTCL, Kaposi |
| RARA (SV, gene fusion) | t(15;17)(q24;q21) | RARA | arsenic trioxide | APL |
| SMO (Mut, Act) | p.Trp535Leu, p.Arg199Trp, p.Arg562Gln | Smoothen | vismodegib | basal cell |
| VHL (Mut) | too numerous to list | VEGFR | sorafenib | RCC, hepatic, thyroid |
| VEGF (Mut) | NA | VEGF | ziv-aflibercept | colon |
Medications targeting normal cell surface proteins that are expressed on some tumor cells (e.g., ER, PR, CD20, CD30, CD52) are not included in this summary of drugs targeting proteins with aberrant expression or function due to somatic genome variants.
Act= activating; Amp= amplification, typically by CNV; CNV=copy number variant; Epigen= epigenetic; Mut=mutation; NA = not applicable; SNV= single nucleotide variant; SV= structural variant.
Only representative examples of known mutations are shown.
Targets are generally protein products encoded by the gene listed.
ALCL= anaplastic large cell lymphoma; ALL= acute lymphoblastic leukemia; AML= acute myeloid leukemia; CLL=chronic myeloid leukemia, CML= chronic myeloid leukemia; CTCL= cutaneous T-cell lymphoma; Ex= exon; GIST= gastrointestinal stromal tumor; NHL= non-Hodgkins lymphoma; NSCLC= non-small cell lung cancer; RCC= renal cell carcinoma.
Single gene vs multi-gene panels; reactive vs pre-emptive genomic testing
Strong “monogenic” gene/drug associations, coupled with limitations in genotyping technology, led to the initial clinical practice of using single-gene pharmacogenetic tests,49 as has been true for all of genetic testing. In this model, genetic tests are ordered one at a time on an “as needed” or reactive basis: the patient is likely to need a pharmacogenetically high-risk drug, and so the clinician orders the applicable genetic test. However, with improvements in technology, it is possible to interrogate multiple genes in a single assay, for far less expense than was formerly the case for single gene tests.
Most human diseases, including cancer, are influenced by multiple genes and genetic variants. Likewise, the pharmacokinetics and pharmacological effects of most medications are determined by multiple gene products (e.g., genes encoding drug metabolizing enzymes, transporters, targets, and disease modifying genes). Many of the pharmacogenes that have been identified to date are genes that have a strong effect on a drug’s pharmacokinetics and/or pharmacodynamics (i.e., they represent the “low hanging fruit”). The genetic polymorphism in thiopurine methyltransferase (TPMT) and its strong effects on the risk of hematopoietic toxicity from thiopurine medications (e.g., mercaptopurine, azathioprine) nicely illustrates how such “low hanging fruit” are often merely the first step down a polygenic path. For example, it was found that after one adjusts the dosage of mercaptopurine based on TPMT genetic test results, then genetic polymorphisms in other genes surface as important (e.g., ITPA).50 Furthermore, genetic polymorphisms in others genes along the same pharmacological pathway can emerge as important in populations of a different ancestry, as illustrated by the strong influence of an inherited variant in NUDT15 on thiopurine toxicity. NUDT15 variants are extremely uncommon in persons of European and African ancestry, but are relatively common among people of Asian ancestry,51 explaining the relatively high frequency of thiopurine intolerance in Asians despite a relatively low frequency of TPMT variants. When a GWAS of thiopurine intolerance was eventually performed in a diverse population comprising people of European, Asian, African and Native American ancestry, both TPMT and NUDT15 reached genomewide significance,52 revealing that TPMT variants were the major determinant of tolerated dose in patients of European and African ancestry, whereas NUDT15 was the major genetic determinant in patients of Asian and Native American ancestry. Because the metabolism and effects of anticancer agents, including thiopurines, can be affected by both germline and somatic genome variation53, this can further increase the complexity of cancer pharmacogenomics.
There are several other examples for which more than one gene is clinically actionable for a given medication, such as the anticoagulant warfarin (affected by both CYP2C9 and VKORC1)18 and tricyclic antidepressants (affected by both CYP2C19 and CYP2D6). Given that one gene can affect multiple medications (Table 1), there are potential benefits of genotyping a panel of pharmacogenomic variants that may be applicable for multiple drugs that could be given throughout a patient’s lifetime. For pharmacogenetic testing as for all of genetic testing, there is increasing evidence that genotyping multiple genes in a single test is more cost effective, makes better use of DNA, and allows for pre-emptive availability of genetic test information. Such multigene panels can change practice from a “reactive” approach (order a new genetic test every time in the patient’s life that the results are deemed to be of interest) to a pre-emptive approach (test for likely-to-be actionable genes in a single sample, thereby providing a lifetime’s worth of test results). Several groups have begun implementing such pre-emptive multigene panels for pharmacogenomics,54–58 but the practice is by no means widespread at the present time.
Barriers to and resources for clinical implementation of pharmacogenomics
What is preventing the widespread use of pre-emptive multi-gene panels to guide drug prescribing? One barrier is the lack of incentives for health care systems to conduct tests or implement procedures to prevent adverse events in the future. There are relatively few studies proving the cost-effectiveness of pharmacogenetic testing,59 and although a multi-gene panel approach is of course less expensive than ordering tests for one pharmacogene at a time, there are no data assessing the cost-effectiveness of a panel approach implemented early in life and usable for a patient’s lifetime. Many health care systems do not provide financial reimbursement for preventive medicine services or for pre-emptive screening services, and thereby create a barrier to pharmacogenetic testing in the clinic.60,61
Layered onto the costs of the laboratory test of genome interrogation itself are the costs and complexity of computational approaches to identify, catalog, prioritize, and interpret genome variants that influence prescribing decisions. Even with a growing number of publicly availability computational tools to analyze genome variation, this process continues to evolve and generally requires a substantial level of expertise and manual interpretation to use successfully in the clinic. Computational tools for clinical decision support (CDS) will be required to prompt and guide clinicians to use genetic information when prescribing affected drugs, triggered by patient-specific alerts.42,62,63 The costs associated with pharmacogenomics in clinical practice is quickly shifting from the cost of the laboratory test to the costs associated with linking genetic test results with evidence-based decisions that will robustly guide prescribing, and will be routinely updated as new evidence emerges. Again, with many healthcare systems, it is not clear who will take responsibility for ongoing updates of interpretations, and who will pay for such interpretations.
Another barrier to clinical uptake of pharmacogenomic testing is that there has been a lack of clear clinical guidelines for translating genomic variation into actionable recommendations, and there is sometimes disagreement among professional societies or other guideline generating groups on whether and how to proceed with pharmacogenetic testing. Examples for which there has been disagreement include testing for warfarin64 and for clopidogrel65, with a common reason for lack of support for genetic testing being the paucity of randomized prospective controlled trials comparing genetically guided testing vs conventional therapy, Also, many professional societies and guideline-generating groups have approached evaluations of pharmacogenomic tests from the standpoint of whether the clinician is obligated to order the genetic test.49,64–66 However, with inexpensive multi-gene tests becoming increasingly available, the question is shifting from whether to order a genetic test, to how the genetic test results “already” generated can and should be used for prescribing decisions. For inherited genomic variation, CPIC has taken on the task of creating such guidelines that focus on how genetic test results should be translated into specific prescribing actions. A similar approach was taken by the Royal Dutch Association for the Advancement of Pharmacy.67,68 Multiple resources exist to help guide cancer drug selection based on somatically acquired genomic variation (Table 2), although these are constantly changing based on new evidence.69–72
With more widespread deep sequencing, additional variants will be discovered in pharmacogenes.73 As for other areas of clinical genetics, it will be challenging to catalog and annotate the additional novel variants. Given the importance of novel rare variants to both inherited 23 and cancer-related pharmacogenes, publicly available and easily updatable resources such as PharmGKB, ClinGen and ClinVar will be critical to feed into computational CDS in health care record systems to provide up-to-date recommendations based on genomic test results.74–76 Currently, heterogeneity among genomic variation databases and among health care record systems, coupled with lack of common ontology for genomic test results and interpretations, limit interoperability and are hindering the use of pharmacogenetic test results longitudinally as well as across all of the health care systems each patient must navigate. Several groups are working to standardize pharmacogenetic test terminologies,77–82 with an eye toward creating terminology that can drive CDS across health care record systems. Initiatives such as the Institute of Medicine Roundtable on Translating Genomic-Based Research for Health and CPIC are working to create terms and language that can be directly uploaded into electronic health care records’ CDS, but heterogeneity across systems will at least initially slow creation and uptake of CDS to facilitate use of pharmacogenetic information.81
Additional barriers include the insatiable desire for more evidence, the lack of education amongst clinicians, the paucity of evidence-based implementation systems, and concerns about incidental or secondary findings from genetic testing, not to mention inertia for change in health care systems.66,83–86 These barriers are not unique to pharmacogenomics, and the energy to overcome them will likely come from multiple sources, ranging from the “push” of patient advocates to the “pull” of courtrooms. For example, an advocate for pediatric patients expressed a disquieting lay perspective; “I am mystified by the resistance to a simple blood test that might save children’s lives,”16 As the general public becomes more aware of the potential of genetic tests to improve medication use, including direct-to-consumer testing,87,88 it is possible that their advocacy will grow even stronger. Meanwhile, the attorney general in Hawaii brought a lawsuit against the manufacturer of the anti-platelet drug clopidogrel because they marketed their drug in Hawaii without warning that a high percentage of the Hawaiian population has inherited low-function alleles of CYP2C19, which encodes the enzyme required to convert clopidogrel to its active metabolite.89 This legal case asserts that it was known a priori that CYP2C19 variant allele frequencies are higher in East Asians and Pacific Islanders, which comprise about 40% and 10% of the Hawaiian population, respectively, and there was abundant evidence that the antithrombotic effects of clopidogrel are diminished in patients with low CYP2C19 activity (predisposing to an increased incidence of cardiovascular events such as stent thrombosis).90,91 From an educational perspective, there are multiple accrediting agencies that are calling for pharmacogenomics to be part of curricula for health care students, trainees, and advanced practitioners,92 and the availability of educational tools continues to grow.93–95 Although the early adopters of clinical pharmacogenomics are establishing methods to advance treatment, broad clinical implementation remains elusive.
Organized efforts to facilitate clinical use of pharmacogenomics
Many groups are working worldwide to share resources to facilitate clinical implementation of germline pharmacogenetic tests.96 The European Pharmacogenetics Implementation Consortium (http://www.eu-pic.net/) is an international consortium whose goal is to improve therapy by integrating pharmacogenetic information into clinical care.97 Efforts to facilitate implementation have also been undertaken by the Royal Dutch Association for the Advancement of Pharmacy.67,68 In the US, members of NIH’s Pharmacogenomics Research Network organized a Translational Pharmacogenetics Project,54–58,98–100 which is dedicated to sharing best practices for clinical implementation of CPIC pharmacogenomics guidelines, and the eMERGE and IGNITE networks are testing pharmacogenetic implementation strategies.85,101,102 In Thailand and Singapore, where the HLA-B*15:02 variant is common and strongly predisposes to severe skin toxicity after specific drugs, pharmacogenetic testing is common.103–105 The Genomic Medicine Alliance (http://www.genomicmedicinealliance.org/)106 facilitates the clinical use of pharmacogenomics and has created a database linking drugs with genes.107 Population admixture in diverse populations must also be considered in global efforts for clinical implementation. 108
Future directions
Clinicians are accustomed to making prescribing decisions based on patient characteristics such as age, renal function, liver function, drug/drug interactions, and patient preferences. Much of this prescribing, however, is taking place without optimal clinical decision support to assist in compiling those characteristics and matching them with evidenced-based choices on medications and their doses. As CDS improves and becomes more widespread, and as the evidenced supporting pharmacogenomic testing continues to grow, the momentum for clinical implementation of pharmacogenomics should accelerate. Going forward, there is a growing body of evidence that pharmacogenomics will be an expanding component of evidence-based precision medicine.
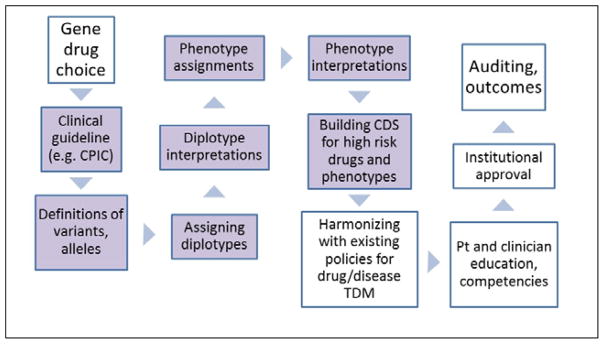
Figure 3.
Multiple steps in bringing pharmacogenomic tests to the clinic. These include prioritizing the choice of gene(s)/drug(s) for actionability; CPIC guidelines exist or are being developed for all actionable inherited pharmacogenes,24 and the guidelines provide guidance for the steps shaded in lavender. Genotypes must be assigned to alleles, and diplotypes assigned to patients. The diplotypes must be translated into phenotypes (gene function) and interpreted with respect to drug therapy. Appropriate clinical decision support (CDS) should be built and deployed to provide prescribers with recommendations, and pharmacogenetic considerations must be harmonized with other policies for the affected medications, using therapeutic drug monitoring (TDM) where applicable. Education of clinicians and of patients should take place, and institutional oversight committees may approve prescribing recommendations and policies. Many groups are auditing clinical and prescribing outcomes to evaluate the impact of clinical implementation of pharmacogenomics.
Footnotes
Additional updated information from regulatory agencies can be found at:
http://www.fda.gov/drugs/scienceresearch/researchareas/pharmacogenetics/ucm083378.htm
References
- 1.Hughes D, Andersson DI. Evolutionary consequences of drug resistance: shared principles across diverse targets and organisms. Nat Rev Genet. 2015;16(8):459–471. doi: 10.1038/nrg3922. [DOI] [PubMed] [Google Scholar]
- 2.Evans WE, Relling MV. Moving towards individualized medicine with pharmacogenomics. Nature. 2004;429(6990):464–468. doi: 10.1038/nature02626. Review of pharmacogenomics from discovery to the clinic. [DOI] [PubMed] [Google Scholar]
- 3.Alving AS, Carson PE, Flanagan CL, Ickes CE. Enzymatic deficiency in primaquine-sensitive erythrocytes. Science. 1956;124(3220):484–485. doi: 10.1126/science.124.3220.484-a. [DOI] [PubMed] [Google Scholar]
- 4.Motulsky AG. Drug reactions enzymes, and biochemical genetics. J Am Med Assoc. 1957;165(7):835–837. doi: 10.1001/jama.1957.72980250010016. [DOI] [PubMed] [Google Scholar]
- 5.Kalow W, Genest K. A method for the detection of atypical forms of human serum cholinesterase; determination of dibucaine numbers. Can J Biochem Physiol. 1957;35(6):339–346. doi: 10.1139/y57-041. [DOI] [PubMed] [Google Scholar]
- 6.Vogel F. Moderne problem der humangenetik. Ergeb Inn Med U Kinderheik. 1959;(12):52–125. [Google Scholar]
- 7.Vesell ES, Page JG. Genetic control of drug levels in man: antipyrine. Science. 1968;161(3836):72–73. doi: 10.1126/science.161.3836.72. [DOI] [PubMed] [Google Scholar]
- 8.Hughes HB, Biehl JP, Jones AP, Schmidt LH. Metabolism of isoniazid in man as related to the occurrence of peripheral neuritis. Am Rev Tuberc. 1954;70(2):266–273. doi: 10.1164/art.1954.70.2.266. [DOI] [PubMed] [Google Scholar]
- 9.Evans DA, Manley KA, Mc KV. Genetic control of isoniazid metabolism in man. Br Med J. 1960;2(5197):485–491. doi: 10.1136/bmj.2.5197.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blum M, Demierre A, Grant DM, Heim M, Meyer UA. Molecular mechanism of slow acetylation of drugs and carcinogens in humans. Proc Natl Acad Sci U S A. 1991;88(12):5237–5241. doi: 10.1073/pnas.88.12.5237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vatsis KP, Martell KJ, Weber WW. Diverse point mutations in the human gene for polymorphic N-acetyltransferase. Proc Natl Acad Sci U S A. 1991;88(14):6333–6337. doi: 10.1073/pnas.88.14.6333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gonzalez FJ, Skoda RC, Kimura S, Umeno M, Zanger UM, Nebert DW, et al. Characterization of the common genetic defect in humans deficient in debrisoquine metabolism. Nature. 1988;331(6155):442–446. doi: 10.1038/331442a0. [DOI] [PubMed] [Google Scholar]
- 13.Ingelman-Sundberg M. Pharmacogenomic biomarkers for prediction of severe adverse drug reactions. N Engl J Med. 2008;358(6):637–639. doi: 10.1056/NEJMe0708842. [DOI] [PubMed] [Google Scholar]
- 14.Wang L, McLeod HL, Weinshilboum RM. Genomics and drug response. N Engl J Med. 2011;364(12):1144–1153. doi: 10.1056/NEJMra1010600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yates CR, Krynetski EY, Loennechen T, Fessing MY, Tai HL, Pui CH, et al. Molecular diagnosis of thiopurine S-methyltransferase deficiency: genetic basis for azathioprine and mercaptopurine intolerance. Ann Intern Med. 1997;126(8):608–614. doi: 10.7326/0003-4819-126-8-199704150-00003. [DOI] [PubMed] [Google Scholar]
- 16.Marshall E. Preventing toxicity with a gene test. Science. 2003;302(5645):588–590. doi: 10.1126/science.302.5645.588. [DOI] [PubMed] [Google Scholar]
- 17.Carr DF, Alfirevic A, Pirmohamed M. Pharmacogenomics: Current State-of-the-Art. Genes (Basel) 2014;5(2):430–443. doi: 10.3390/genes5020430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pirmohamed M, Kamali F, Daly AK, Wadelius M. Oral anticoagulation: a critique of recent advances and controversies. Trends Pharmacol Sci. 2015;36(3):153–163. doi: 10.1016/j.tips.2015.01.003. Discussion of complexities of evaluating the benefit of individualizing therapy based on genetic tests, and how race/ethnicity may complicate this, for one of the most important clinically actionable gene/drug pairs. [DOI] [PubMed] [Google Scholar]
- 19.Burke W. Clinical validity and clinical utility of genetic tests. Curr Protoc Hum Genet. 2009;Chapter 9(Unit 9):15. doi: 10.1002/0471142905.hg0915s60. [DOI] [PubMed] [Google Scholar]
- 20.Gaedigk A. Complexities of CYP2D6 gene analysis and interpretation. Int Rev Psychiatry. 2013;25(5):534–553. doi: 10.3109/09540261.2013.825581. [DOI] [PubMed] [Google Scholar]
- 21.Grosse SD, Khoury MJ. What is the clinical utility of genetic testing? Genet Med. 2006;8(7):448–450. doi: 10.1097/01.gim.0000227935.26763.c6. [DOI] [PubMed] [Google Scholar]
- 22.Scott SA. Personalizing medicine with clinical pharmacogenetics. Genet Med. 2011;13(12):987–995. doi: 10.1097/GIM.0b013e318238b38c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Z, Liew D, Kwan P. Effects of a HLA-B*15:02 screening policy on antiepileptic drug use and severe skin reactions. Neurology. 2014;83(22):2077–2084. doi: 10.1212/WNL.0000000000001034. [DOI] [PubMed] [Google Scholar]
- 24.Relling MV, Klein TE. CPIC: Clinical Pharmacogenetics Implementation Consortium of the Pharmacogenomics Research Network. Clin Pharmacol Ther. 2011;89(3):464–467. doi: 10.1038/clpt.2010.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caudle KE, Klein TE, Hoffman JM, Muller DJ, Whirl-Carrillo M, Gong L, et al. Incorporation of pharmacogenomics into routine clinical practice: the Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline development process. Curr Drug Metab. 2014;15(2):209–217. doi: 10.2174/1389200215666140130124910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crews KR, Gaedigk A, Dunnenberger HM, Leeder JS, Klein TE, Caudle KE, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for cytochrome P450 2D6 genotype and codeine therapy: 2014 update. Clin Pharmacol Ther. 2014;95(4):376–382. doi: 10.1038/clpt.2013.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mallal S, Phillips E, Carosi G, Molina JM, Workman C, Tomazic J, et al. HLA-B*5701 screening for hypersensitivity to abacavir. N Engl J Med. 2008;358(6):568–579. doi: 10.1056/NEJMoa0706135. [DOI] [PubMed] [Google Scholar]
- 28.Martin MA, Hoffman JM, Freimuth RR, Klein TE, Dong BJ, Pirmohamed M, et al. Clinical Pharmacogenetics Implementation Consortium Guidelines for HLA-B Genotype and Abacavir Dosing: 2014 update. Clin Pharmacol Ther. 2014;95(5):499–500. doi: 10.1038/clpt.2014.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Province MA, Altman RB, Klein TE. Interpreting the CYP2D6 results from the International Tamoxifen Pharmacogenetics Consortium. Clin Pharmacol Ther. 2014;96(2):144–146. doi: 10.1038/clpt.2014.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ratain MJ, Nakamura Y, Cox NJ. CYP2D6 genotype and tamoxifen activity: understanding interstudy variability in methodological quality. Clin Pharmacol Ther. 2013;94(2):185–187. doi: 10.1038/clpt.2013.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brauch H, Schroth W, Goetz MP, Murdter TE, Winter S, Ingle JN, et al. Tamoxifen use in postmenopausal breast cancer: CYP2D6 matters. J Clin Oncol. 2013;31(2):176–180. doi: 10.1200/JCO.2012.44.6625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Irvin WJ, Jr, Walko CM, Weck KE, Ibrahim JG, Chiu WK, Dees EC, et al. Genotype-guided tamoxifen dosing increases active metabolite exposure in women with reduced CYP2D6 metabolism: a multicenter study. J Clin Oncol. 2011;29(24):3232–3239. doi: 10.1200/JCO.2010.31.4427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brauch H, Schwab M. Prediction of tamoxifen outcome by genetic variation of CYP2D6 in post-menopausal women with early breast cancer. Br J Clin Pharmacol. 2014;77(4):695–703. doi: 10.1111/bcp.12229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Province MA, Goetz MP, Brauch H, Flockhart DA, Hebert JM, Whaley R, et al. CYP2D6 genotype and adjuvant tamoxifen: meta-analysis of heterogeneous study populations. Clin Pharmacol Ther. 2014;95(2):216–227. doi: 10.1038/clpt.2013.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ehmann F, Caneva L, Prasad K, Paulmichl M, Maliepaard M, Llerena A, et al. Pharmacogenomic information in drug labels: European Medicines Agency perspective. Pharmacogenomics J. 2015;15(3):201–210. doi: 10.1038/tpj.2014.86. [DOI] [PubMed] [Google Scholar]
- 36.Tutton R. Pharmacogenomic biomarkers in drug labels: what do they tell us? Pharmacogenomics. 2014;15(3):297–304. doi: 10.2217/pgs.13.198. [DOI] [PubMed] [Google Scholar]
- 37.Ishiguro A, Yagi S, Uyama Y. Characteristics of pharmacogenomics/biomarker-guided clinical trials for regulatory approval of anti-cancer drugs in Japan. J Hum Genet. 2013;58(6):313–316. doi: 10.1038/jhg.2013.36. [DOI] [PubMed] [Google Scholar]
- 38.Bosma PJ, Chowdhury JR, Bakker C, Gantla S, de Boer A, Oostra BA, et al. The genetic basis of the reduced expression of bilirubin UDP-glucuronosyltransferase 1 in Gilbert’s syndrome. N Engl J Med. 1995;333(18):1171–1175. doi: 10.1056/NEJM199511023331802. [DOI] [PubMed] [Google Scholar]
- 39.Beutler E. G6PD deficiency. Blood. 1994;84(11):3613–3636. [PubMed] [Google Scholar]
- 40.McCarthy JJ, McLeod HL, Ginsburg GS. Genomic medicine: a decade of successes, challenges, and opportunities. Sci Transl Med. 2013;5(189):189sr184. doi: 10.1126/scitranslmed.3005785. [DOI] [PubMed] [Google Scholar]
- 41.Kinch MS, Haynesworth A, Kinch SL, Hoyer D. An overview of FDA-approved new molecular entities: 1827–2013. Drug Discov Today. 2014;19(8):1033–1039. doi: 10.1016/j.drudis.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 42.Dunnenberger HM, Crews KR, Hoffman JM, Caudle KE, Broeckel U, Howard SC, et al. Preemptive clinical pharmacogenetics implementation: current programs in five US medical centers. Annu Rev Pharmacol Toxicol. 2015;55:89–106. doi: 10.1146/annurev-pharmtox-010814-124835. Detailed discussion of a pre-emptive approach to clinical implementation of pharmacogenetics, with quantitative information on use of medications subject to genetic actionability. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wheeler HE, Maitland ML, Dolan ME, Cox NJ, Ratain MJ. Cancer pharmacogenomics: strategies and challenges. Nat Rev Genet. 2013;14(1):23–34. doi: 10.1038/nrg3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McLeod HL. Cancer pharmacogenomics: early promise, but concerted effort needed. Science. 2013;339(6127):1563–1566. doi: 10.1126/science.1234139. Analysis of considerations for using both somatic and inherited germline genetic lesions for presribing anticancer drugs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Look AT, Hayes FA, Nitschke R, McWilliams NB, Green AA. Cellular DNA content as a predictor of response to chemotherapy in infants with unresectable neuroblastoma. N Engl J Med. 1984;311(4):231–235. doi: 10.1056/NEJM198407263110405. [DOI] [PubMed] [Google Scholar]
- 46.Pui CH, Crist WM, Look AT. Biology and clinical significance of cytogenetic abnormalities in childhood acute lymphoblastic leukemia. Blood. 1990;76(8):1449–1463. [PubMed] [Google Scholar]
- 47.Senderowicz AM, Pfaff O. Similarities and differences in the oncology drug approval process between FDA and European Union with emphasis on in vitro companion diagnostics. Clin Cancer Res. 2014;20(6):1445–1452. doi: 10.1158/1078-0432.CCR-13-1761. [DOI] [PubMed] [Google Scholar]
- 48.Pignatti F, Ehmann F, Hemmings R, Jonsson B, Nuebling M, Papaluca-Amati M, et al. Cancer drug development and the evolving regulatory framework for companion diagnostics in the European union. Clin Cancer Res. 2014;20(6):1458–1468. doi: 10.1158/1078-0432.CCR-13-1571. [DOI] [PubMed] [Google Scholar]
- 49.Flockhart DA, Skaar T, Berlin DS, Klein TE, Nguyen AT. Clinically available pharmacogenomics tests. Clin Pharmacol Ther. 2009;86(1):109–113. doi: 10.1038/clpt.2009.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stocco G, Cheok MH, Crews KR, Dervieux T, French D, Pei D, et al. Genetic polymorphism of inosine triphosphate pyrophosphatase is a determinant of mercaptopurine metabolism and toxicity during treatment for acute lymphoblastic leukemia. Clin Pharmacol Ther. 2009;85(2):164–172. doi: 10.1038/clpt.2008.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yang SK, Hong M, Baek J, Choi H, Zhao W, Jung Y, et al. A common missense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat Genet. 2014;46(9):1017–1020. doi: 10.1038/ng.3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang JJ, Landier W, Yang W, Liu C, Hageman L, Cheng C, et al. Inherited NUDT15 Variant Is a Genetic Determinant of Mercaptopurine Intolerance in Children With Acute Lymphoblastic Leukemia. J Clin Oncol. 2015;33(11):1235–1242. doi: 10.1200/JCO.2014.59.4671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cheng Q, Yang W, Raimondi SC, Pui CH, Relling MV, Evans WE. Karyotypic abnormalities create discordance of germline genotype and cancer cell phenotypes. Nat Genet. 2005;37(8):878–882. doi: 10.1038/ng1612. [DOI] [PubMed] [Google Scholar]
- 54.Bielinski SJ, Olson JE, Pathak J, Weinshilboum RM, Wang L, Lyke KJ, et al. Preemptive genotyping for personalized medicine: design of the right drug, right dose, right time-using genomic data to individualize treatment protocol. Mayo Clin Proc. 2014;89(1):25–33. doi: 10.1016/j.mayocp.2013.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gottesman O, Scott SA, Ellis SB, Overby CL, Ludtke A, Hulot JS, et al. The CLIPMERGE PGx Program: clinical implementation of personalized medicine through electronic health records and genomics-pharmacogenomics. Clin Pharmacol Ther. 2013;94(2):214–217. doi: 10.1038/clpt.2013.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fernandez CA, Smith C, Yang W, Lorier R, Crews KR, Kornegay N, et al. Concordance of DMET plus genotyping results with those of orthogonal genotyping methods. Clin Pharmacol Ther. 2012;92(3):360–365. doi: 10.1038/clpt.2012.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Johnson JA, Burkley BM, Langaee TY, Clare-Salzler MJ, Klein TE, Altman RB. Implementing personalized medicine: development of a cost-effective customized pharmacogenetics genotyping array. Clin Pharmacol Ther. 2012;92(4):437–439. doi: 10.1038/clpt.2012.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Oetjens MT, Denny JC, Ritchie MD, Gillani NB, Richardson DM, Restrepo NA, et al. Assessment of a pharmacogenomic marker panel in a polypharmacy population identified from electronic medical records. Pharmacogenomics. 2013;14(7):735–744. doi: 10.2217/pgs.13.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Buchanan J, Wordsworth S, Schuh A. Issues surrounding the health economic evaluation of genomic technologies. Pharmacogenomics. 2013;14(15):1833–1847. doi: 10.2217/pgs.13.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schroeder SA, Frist W National Commission on Physician Payment R. Phasing out fee-for-service payment. N Engl J Med. 2013;368(21):2029–2032. doi: 10.1056/NEJMsb1302322. [DOI] [PubMed] [Google Scholar]
- 61.Levy KD, Decker BS, Carpenter JS, Flockhart DA, Dexter PR, Desta Z, et al. Prerequisites to implementing a pharmacogenomics program in a large health-care system. Clin Pharmacol Ther. 2014;96(3):307–309. doi: 10.1038/clpt.2014.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Overby CL, Erwin AL, Abul-Husn NS, Ellis SB, Scott SA, Obeng AO, et al. Physician Attitudes toward Adopting Genome-Guided Prescribing through Clinical Decision Support. J Pers Med. 2014;4(1):35–49. doi: 10.3390/jpm4010035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Crawford DC, Crosslin DR, Tromp G, Kullo IJ, Kuivaniemi H, Hayes MG, et al. eMERGEing progress in genomics-the first seven years. Front Genet. 2014;5:184. doi: 10.3389/fgene.2014.00184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cavallari LH, Nutescu EA. Warfarin pharmacogenetics: to genotype or not to genotype, that is the question. Clin Pharmacol Ther. 2014;96(1):22–24. doi: 10.1038/clpt.2014.78. [DOI] [PubMed] [Google Scholar]
- 65.Chan NC, Eikelboom JW, Ginsberg JS, Lauw MN, Vanassche T, Weitz JI, et al. Role of phenotypic and genetic testing in managing clopidogrel therapy. Blood. 2014;124(5):689–699. doi: 10.1182/blood-2014-01-512723. [DOI] [PubMed] [Google Scholar]
- 66.Stanek EJ, Sanders CL, Taber KA, Khalid M, Patel A, Verbrugge RR, et al. Adoption of pharmacogenomic testing by US physicians: results of a nationwide survey. Clin Pharmacol Ther. 2012;91(3):450–458. doi: 10.1038/clpt.2011.306. [DOI] [PubMed] [Google Scholar]
- 67.Swen JJ, Wilting I, de Goede AL, Grandia L, Mulder H, Touw DJ, et al. Pharmacogenetics: from bench to byte. Clin Pharmacol Ther. 2008;83(5):781–787. doi: 10.1038/sj.clpt.6100507. [DOI] [PubMed] [Google Scholar]
- 68.Swen JJ, Nijenhuis M, de Boer A, Grandia L, Maitland-van der Zee AH, Mulder H, et al. Pharmacogenetics: from bench to byte--an update of guidelines. Clin Pharmacol Ther. 2011;89(5):662–673. doi: 10.1038/clpt.2011.34. Survey of clinically actionable germline genetic variants and affected medications, with basic prescribing advice. [DOI] [PubMed] [Google Scholar]
- 69.Yeh P, Chen H, Andrews J, Naser R, Pao W, Horn L. DNA-Mutation Inventory to Refine and Enhance Cancer Treatment (DIRECT): a catalog of clinically relevant cancer mutations to enable genome-directed anticancer therapy. Clin Cancer Res. 2013;19(7):1894–1901. doi: 10.1158/1078-0432.CCR-12-1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Van Allen EM, Wagle N, Levy MA. Clinical analysis and interpretation of cancer genome data. J Clin Oncol. 2013;31(15):1825–1833. doi: 10.1200/JCO.2013.48.7215. Overview of databases to match somatic cancer-specific genetic variants with targeted anticancer drugs. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Abrams J, Conley B, Mooney M, Zwiebel J, Chen A, Welch JJ, et al. National Cancer Institute’s Precision Medicine Initiatives for the new National Clinical Trials Network. Am Soc Clin Oncol Educ Book. 2014:71–76. doi: 10.14694/EdBook_AM.2014.34.71. [DOI] [PubMed] [Google Scholar]
- 72.Agundez JA, Esguevillas G, Amo G, Garcia-Martin E. Clinical practice guidelines for translating pharmacogenomic knowledge to bedside. Focus on anticancer drugs. Front Pharmacol. 2014;5:188. doi: 10.3389/fphar.2014.00188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gordon AS, Tabor HK, Johnson AD, Snively BM, Assimes TL, Auer PL, et al. Quantifying rare, deleterious variation in 12 human cytochrome P450 drug-metabolism genes in a large-scale exome dataset. Hum Mol Genet. 2014;23(8):1957–1963. doi: 10.1093/hmg/ddt588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Landrum MJ, Lee JM, Riley GR, Jang W, Rubinstein WS, Church DM, et al. ClinVar: public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res. 2014;42(Database issue):D980–985. doi: 10.1093/nar/gkt1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rehm HLBJ, Brooks LD, Bustamante CD, Evans JP, Landrum MJ, Ledbetter DH, Maglott DR, Martin CL, Nussbaum RL, Plon SE, Ramos EM, Sherry ST, Watson MS. ClinGen. ClinGen--the Clinical Genome Resource. N Engl J Med. 2015;372(23):2235–2242. doi: 10.1056/NEJMsr1406261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Whirl-Carrillo M, McDonagh EM, Hebert JM, Gong L, Sangkuhl K, Thorn CF, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92(4):414–417. doi: 10.1038/clpt.2012.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Percha B, Altman RB. Inferring the semantic relationships of words within an ontology using random indexing: applications to pharmacogenomics. AMIA Annu Symp Proc. 2013;2013:1123–1132. [PMC free article] [PubMed] [Google Scholar]
- 78.Samwald M, Freimuth RR. Making data on essential pharmacogenes available for every patient everywhere: the Medicine Safety Code initiative. Pharmacogenomics. 2013;14(13):1529–1531. doi: 10.2217/pgs.13.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bell GC, Crews KR, Wilkinson MR, Haidar CE, Hicks JK, Baker DK, et al. Development and use of active clinical decision support for preemptive pharmacogenomics. J Am Med Inform Assoc. 2014;21(e1):e93–99. doi: 10.1136/amiajnl-2013-001993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhu Q, Freimuth RR, Lian Z, Bauer S, Pathak J, Tao C, et al. Harmonization and semantic annotation of data dictionaries from the Pharmacogenomics Research Network: a case study. J Biomed Inform. 2013;46(2):286–293. doi: 10.1016/j.jbi.2012.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Overby CL, Kohane I, Kannry JL, Williams MS, Starren J, Bottinger E, et al. Opportunities for genomic clinical decision support interventions. Genet Med. 2013;15(10):817–823. doi: 10.1038/gim.2013.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Minarro-Gimenez JA, Blagec K, Boyce RD, Adlassnig KP, Samwald M. An ontology-based, mobile-optimized system for pharmacogenomic decision support at the point-of-care. PLoS One. 2014;9(5):e93769. doi: 10.1371/journal.pone.0093769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Haga SB, O’Daniel JM, Tindall GM, Mills R, Lipkus IM, Agans R. Survey of genetic counselors and clinical geneticists’ use and attitudes toward pharmacogenetic testing. Clin Genet. 2012;82(2):115–120. doi: 10.1111/j.1399-0004.2012.01848.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Haga SB, Burke W, Ginsburg GS, Mills R, Agans R. Primary care physicians’ knowledge of and experience with pharmacogenetic testing. Clin Genet. 2012;82(4):388–394. doi: 10.1111/j.1399-0004.2012.01908.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Weber GM, Mandl KD, Kohane IS. Finding the missing link for big biomedical data. JAMA. 2014;311(24):2479–2480. doi: 10.1001/jama.2014.4228. [DOI] [PubMed] [Google Scholar]
- 86.Hayden EC. Geneticists push for global data-sharing. Nature. 2013;498(7452):16–17. doi: 10.1038/498017a. [DOI] [PubMed] [Google Scholar]
- 87.Prainsack B, Vayena E. Beyond the clinic: ‘direct-to-consumer’ genomic profiling services and pharmacogenomics. Pharmacogenomics. 2013;14(4):403–412. doi: 10.2217/pgs.13.10. [DOI] [PubMed] [Google Scholar]
- 88.Caulfield T. DTC genetic testing: pendulum swings and policy paradoxes. Clin Genet. 2012;81(1):4–6. doi: 10.1111/j.1399-0004.2011.01799.x. [DOI] [PubMed] [Google Scholar]
- 89.http://ag.hawaii.gov/wp-content/uploads/2014/01/News-Release-2014-09.pdf. HI Plavix Lawsuit news-release
- 90.Shuldiner AR, O’Connell JR, Bliden KP, Gandhi A, Ryan K, Horenstein RB, et al. Association of cytochrome P450 2C19 genotype with the antiplatelet effect and clinical efficacy of clopidogrel therapy. JAMA. 2009;302(8):849–857. doi: 10.1001/jama.2009.1232. Primary findings showing that CYP2C19 genetic affects effectiveness and bleeding risk from clopidogrel; led to FDA black box warning for the drug label. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mega JL, Simon T, Collet JP, Anderson JL, Antman EM, Bliden K, et al. Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis. JAMA. 2010;304(16):1821–1830. doi: 10.1001/jama.2010.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Manolio TA, Green ED. Leading the way to genomic medicine. Am J Med Genet C Semin Med Genet. 2014;166C(1):1–7. doi: 10.1002/ajmg.c.31384. [DOI] [PubMed] [Google Scholar]
- 93.Manolio TA, Murray MF Inter-Society Coordinating Committee for Practitioner Education in G. The growing role of professional societies in educating clinicians in genomics. Genet Med. 2014;16(8):571–572. doi: 10.1038/gim.2014.6. [DOI] [PubMed] [Google Scholar]
- 94.Korf BR, Berry AB, Limson M, Marian AJ, Murray MF, O’Rourke PP, et al. Framework for development of physician competencies in genomic medicine: report of the Competencies Working Group of the Inter-Society Coordinating Committee for Physician Education in Genomics. Genet Med. 2014;16(11):804–809. doi: 10.1038/gim.2014.35. [DOI] [PubMed] [Google Scholar]
- 95.Wiener CM, Thomas PA, Goodspeed E, Valle D, Nichols DG. “Genes to society”--the logic and process of the new curriculum for the Johns Hopkins University School of Medicine. Acad Med. 2010;85(3):498–506. doi: 10.1097/ACM.0b013e3181ccbebf. [DOI] [PubMed] [Google Scholar]
- 96.Manolio TA, Abramowicz M, Al-Mulla F, Anderson W, Balling R, Berger AC, et al. Global implementation of genomic medicine: We are not alone. Sci Transl Med. 2015;7(290):290ps213. doi: 10.1126/scitranslmed.aab0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Becquemont L, Alfirevic A, Amstutz U, Brauch H, Jacqz-Aigrain E, Laurent-Puig P, et al. Practical recommendations for pharmacogenomics-based prescription: 2010 ESF-UB Conference on Pharmacogenetics and Pharmacogenomics. Pharmacogenomics. 2011;12(1):113–124. doi: 10.2217/pgs.10.147. [DOI] [PubMed] [Google Scholar]
- 98.Shuldiner AR, Relling MV, Peterson JF, Hicks JK, Freimuth RR, Sadee W, et al. The Pharmacogenomics Research Network Translational Pharmacogenetics Program: overcoming challenges of real-world implementation. Clin Pharmacol Ther. 2013;94(2):207–210. doi: 10.1038/clpt.2013.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Pulley JM, Denny JC, Peterson JF, Bernard GR, Vnencak-Jones CL, Ramirez AH, et al. Operational implementation of prospective genotyping for personalized medicine: the design of the Vanderbilt PREDICT project. Clin Pharmacol Ther. 2012;92(1):87–95. doi: 10.1038/clpt.2011.371. Description of the benefits and efficiency of implementing a large and innovative multi-gene preemptive pharmacogenetics program at a major medical center. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.O’Donnell PH, Danahey K, Jacobs M, Wadhwa NR, Yuen S, Bush A, et al. Adoption of a clinical pharmacogenomics implementation program during outpatient care--initial results of the University of Chicago “1,200 Patients Project”. Am J Med Genet C Semin Med Genet. 2014;166C(1):68–75. doi: 10.1002/ajmg.c.31385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gottesman O, Kuivaniemi H, Tromp G, Faucett WA, Li R, Manolio TA, et al. The Electronic Medical Records and Genomics (eMERGE) Network: past, present, and future. Genet Med. 2013;15(10):761–771. doi: 10.1038/gim.2013.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Rasmussen-Torvik LJ, Stallings SC, Gordon AS, Almoguera B, Basford MA, Bielinski SJ, et al. Design and anticipated outcomes of the eMERGE-PGx project: a multicenter pilot for preemptive pharmacogenomics in electronic health record systems. Clin Pharmacol Ther. 2014;96(4):482–489. doi: 10.1038/clpt.2014.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rattanavipapong W, Koopitakkajorn T, Praditsitthikorn N, Mahasirimongkol S, Teerawattananon Y. Economic evaluation of HLA-B*15:02 screening for carbamazepine-induced severe adverse drug reactions in Thailand. Epilepsia. 2013;54(9):1628–1638. doi: 10.1111/epi.12325. [DOI] [PubMed] [Google Scholar]
- 104.Toh DS, Tan LL, Aw DC, Pang SM, Lim SH, Thirumoorthy T, et al. Building pharmacogenetics into a pharmacovigilance program in Singapore: using serious skin rash as a pilot study. Pharmacogenomics J. 2014;14(4):316–321. doi: 10.1038/tpj.2013.46. [DOI] [PubMed] [Google Scholar]
- 105.Sukasem C, Puangpetch A, Medhasi S, Tassaneeyakul W. Pharmacogenomics of drug-induced hypersensitivity reactions: challenges, opportunities and clinical implementation. Asian Pac J Allergy Immunol. 2014;32(2):111–123. [PubMed] [Google Scholar]
- 106.Cooper DNBA, Dolzan V, Fortina P, Innocenti F, Lee MT, Macek M, Al-Mulla F, Prainsack B, Squassina A, Vayena E, Vozikis A, Williams MS, Patrinos GP. Bridging genomics research between developed and developing countries. The Genomic Medicine Alliance. 2014 doi: 10.2217/pme.14.59. In Press. [DOI] [PubMed] [Google Scholar]
- 107.Dalabira E, Viennas E, Daki E, Komianou A, Bartsakoulia M, Poulas K, et al. DruGeVar: an online resource triangulating drugs with genes and genomic biomarkers for clinical pharmacogenomics. Public Health Genomics. 2014;17(5–6):265–271. doi: 10.1159/000365895. [DOI] [PubMed] [Google Scholar]
- 108.Bonifaz-Pena V, Contreras AV, Struchiner CJ, Roela RA, Furuya-Mazzotti TK, Chammas R, et al. Exploring the distribution of genetic markers of pharmacogenomics relevance in Brazilian and Mexican populations. PLoS One. 2014;9(11):e112640. doi: 10.1371/journal.pone.0112640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Relling MV, McDonagh EM, Chang T, Caudle KE, McLeod HL, Haidar CE, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines for rasburicase therapy in the context of G6PD deficiency genotype. Clin Pharmacol Ther. 2014;96(2):169–174. doi: 10.1038/clpt.2014.97. [DOI] [PMC free article] [PubMed] [Google Scholar]