Abstract
Objective:
To present the clinical management of inguinal disruption in a professional hockey player and highlight the importance of a multidisciplinary approach to diagnosis and management.
Clinical Features:
A professional hockey player with recurrent groin pain presented to the clinic after an acute exacerbation of pain while playing hockey.
Intervention:
The patient received a clinical diagnosis of inguinal disruption. Imaging revealed a tear in the rectus abdominis. Management included two platelet-rich plasma (PRP) injections to the injured tissue, and subsequent manual therapy and exercise. The patient returned to his prior level of performance in 3.5 weeks.
Discussion:
This case demonstrated the importance of a multidisciplinary team and the need for advanced imaging in athletes with groin pain.
Summary:
Research quality concerning the non-surgical management of inguinal disruption remains low. This case adds evidence that PRP, with the addition of manual therapy and exercise may serve as a relatively quick and effective non-surgical management strategy.
Keywords: chiropractic, sports hernia, athletic pubalgia, inguinal disruption, PRP, platelet-rich plasma
Abstract
Objectif :
Présenter la prise en charge clinique d’une perturbation inguinale chez un joueur de hockey et mettre en évidence l’importance que revêt une approche multidisciplinaire pour le diagnostic et la prise en charge.
Caractéristiques cliniques :
Un joueur de hockey professionnel souffrant d’une douleur récurrente au niveau de l’aine s’est présenté à la clinique à la suite d’une exacerbation aiguë de la douleur survenue au cours de la pratique de son sport.
Intervention :
Le patient a reçu un diagnostic clinique d’une perturbation inguinale. L’imagerie médicale a révélé la présence d’une déchirure au niveau du grand droit de l’abdomen. La prise en charge comprenait deux injections de plasma riche en plaquettes (PRP) dans le tissu lésé, ainsi qu’une thérapeutique manuelle et des exercices ultérieurs. Le patient a retrouvé son niveau de performance antérieur en 3,5 semaines.
Discussion :
Ce cas prouve l’importance de recourir à une équipe pluridisciplinaire et la nécessité d’utiliser des technologies d’imagerie de pointe chez les athlètes souffrant de douleurs récurrentes au niveau de l’aine.
Résumé :
La qualité des recherches relatives à la prise en charge non-chirurgicale des perturbations inguinales demeure faible. Ce cas est une preuve supplémentaire que le PRP, associé à une thérapeutique manuelle et à des exercices, peut constituer une stratégie de prise en charge non-chirurgicale relativement rapide et efficace.
Keywords: chiropratique, hernie du sportif, pubalgie du sportif, perturbation inguinale, PRP, plasma riche en plaquettes
Introduction
Groin pain is a common complaint in athletes. It is estimated that approximately 5% to 18% of all sports injuries are groin-related.1 How many of these injuries are athletic pubalgia is unclear, due to the lack of consistent diagnostic criteria proposed in the literature. Unfortunately, the majority of research in this area are retrospective studies, non-randomised studies, case-controlled studies, and case reports.2,3 This may be due to the vast amount of disagreement in the literature regarding the diagnosis, pathophysiology, and treatment options.
The terminology for this injury is still controversial. Arguably, the most commonly used term is Sports Hernia (SH). This term is a misnomer and misleading. The condition does not involve a true hernia and it may also present in a non-athletic population. Other terms that have been used in the literature are: pubic inguinal pain syndrome, Gilmore’s groin, incipient hernia, conjoint tendon lesion, posterior abdominal wall deficiency, and sportsman’s groin.2–6
The term Athletic Pubalgia (AP) has also been used interchangeably with SH in the literature. AP can also be deemed a misnomer since it implies that the injury only takes place in athletes. However, there are some sources that describe AP as an injury to the many musculotendinous structures that cross the anterior pelvis, such as the rectus abdominis insertion onto the pubic symphysis, the adductors and conjoined tendon insertion.7–9
The British Hernia Society’s 2014 position statement based on the Manchester Consensus Conference proposed eliminating the various terms such as athletic pubalgia, sports hernia, sportsman’s groin, pubic inguinal pain syndrome, etc., and to replace them with the preferred term Inguinal Disruption (ID).6 The term ID is thought to describe the condition more accurately. The consensus statement reports that this injury includes posterior inguinal wall weakness (this area represents a combination of the transversalis fascia and the parietal peritoneum), external ring dilation, conjoint tendon damage and tears in the inguinal ligament. It was noted that not all of these features are present in every case, and that other pathologies involving the muscle, ligaments and joints may also be affected.6 To remain consistent with the updated terminology from the consensus statement, the remainder of this article shall only use the term ID.
Platelet-rich plasma (PRP) injections have recently gained attention in the treatment of sports injuries. The rationale behind PRP is that there would be enhancement of the natural healing process if additional growth factors were introduced into the damaged tissue.10,11 There is evidence that these growth factors are needed in muscle repair and regeneration process.11
Our case describes the non-surgical management of ID due to a tear of the rectus abdominis and conjoint tendon. This case demonstrates the importance of a multidisciplinary approach to diagnosis and co-management.
Case Presentation
A 31–year-old male professional hockey player presented to a sports chiropractor after an acute exacerbation of lower abdominal pain. Two weeks prior to presentation, he was experiencing a feeling that he described as a tight groin and hip flexor, which responded well to stretching and warm-up but would tighten up quickly with skating. He described receiving soft tissue therapy from the team athletic trainer on the lower abdominal region, which seemed to temporarily ease the tension. During a practice session just prior to presentation to the clinic, he executed a slap shot and immediately felt a sharp pain above the pubic symphysis and along the left inguinal ligament. The pain forced him to discontinue skating and practice. He stated he had pain with walking, straining and coughing with a general ache at rest. He received an MRI that night which revealed a tear in the left rectus abdominis, rectus sheath and a portion of the conjoint tendon. The team physician recommended surgery based on the MRI findings. The player decided to get a second opinion from a sports chiropractor.
Upon presentation to the sports chiropractor, the patient indicated a general feeling of tightness through the left lower abdominal region and left anterior/medial thigh, and a sharp pain just superior to the pubic symphysis slightly left of midline.
Physical examination revealed sharp local pain on palpation over the left medial inguinal ligament, pubic symphysis, conjoint tendon and rectus abdominis insertion. Passive hip range of motion was unremarkable. Lumbar spine range of motion was within normal range. Patellar, hamstring and Achilles tendon reflexes were 2+ bilaterally. Sensory examination was unremarkable. Straight leg raise was normal. Resisted hip adduction was graded 3/5 with inguinal pain. Resisted sit-up was positive for weakness and inguinal pain. Valsalva’s maneuver produced inguinal pain. The patient received a working diagnosis of ID, as per the criteria in Table 1.
Table 1.
Diagnostic criteria of Inguinal Disruption6
| Clinical diagnosis of Inguinal Disruption (ID) can be made if 3 of the following 5 signs are present: | |
| 1 | Pinpoint tenderness over the pubic tubercle at the point of insertion of the conjoint tendon |
| 2 | Palpable tenderness over the deep inguinal ring |
| 3 | Pain and/or dilation of the external ring with no obvious hernia evident |
| 4 | Pain at the origin of the adductor longus tendon |
| 5 | Dull, diffused pain in the groin, often radiating to the perineum and inner thigh or across the midline |
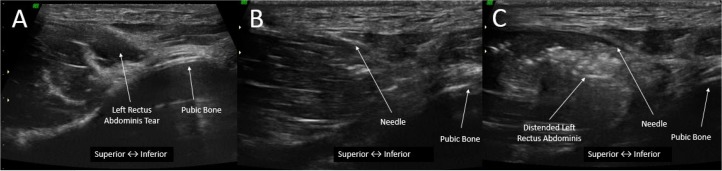
The patient was subsequently referred to a sports physician. Diagnostic ultrasound imaging revealed a left rectus abdominis tear at the insertion on the pubic tubercle and a tear of a portion of the left conjoint tendon. The tear measured 12.6mm × 4.4mm. The patient was treated with an ultrasound-guided PRP injection (Figure 1). One week later, the tear measured 4.6mm × 2.6mm. A second PRP injection was administered (Figure 2). At this point, he was referred back to the sports chiropractor and a strength and conditioning coach to commence rehabilitation.
Figure 1.
First ultrasound-guided PRP injection of left rectus abdominis (week 1). A) 12.6mm × 4.4mm tear of the left rectus abdominis. B) Insertion of needle into the tear (pre-injection). C) Distended left rectus abdominis (post-injection).
Figure 2.
Second ultrasound-guided PRP injection of left rectus abdominis (week 2). A) 4.6mm × 2.6mm tear of the left rectus abdominis. B) Insertion of needle into the tear (pre-injection). C) Distended left rectus abdominis (post-injection).
Treatment by the sports chiropractor was performed daily and included myofascial release to the quadriceps, adductors, psoas, medial hamstring group and tensor fascia lata (TFL) in order to normalise the abnormal muscle tension crossing the anterior pelvis. Care was taken not to treat directly over the torn site. Due to the fact that the tear was still maturing, manual therapy over the injection site may have disrupted the regenerative process of PRP, potentially negating its effectiveness.
Exercises were supervised by a strength and conditioning coach. The exercises were performed daily and included 2 sets of 15 repetitions of: transversus abdominis setting, monster walks with a blue theraband, high hurdle steps, walking lunges with overhead reach, hip airplanes, one leg squat with opposite leg towel slide and bowler squats (Figures 3–9). The goal of the exercises was to strengthen the muscles crossing the anterior pelvis.
Figure 3.
Transversus abdominis setting
Figure 4.
Monster walks with blue theraband
Figure 5.

Walking lunge with overhead reach
Figure 6.

Hip airplane
Figure 7.

Bowler squat
Figure 8.
High hurdle steps
Figure 9.
One leg squat with opposite leg towel slide
As his pain decreased, the player gradually transitioned back to hockey. At the end of week two, the player began skating lightly. A few days later, he began shooting drills. At the start of week three, he participated in full practice with the team and resumed training with his hockey team’s strength and conditioning coach. Full return to play occurred in the middle of week three. The player was asymptomatic at return to play and remains asymptomatic at six months follow-up.
Discussion
This case describes the non-surgical management of ID due to a rectus abdominis and conjoint tendon tear. The injury occurred in the player’s pre-season training and therefore a timely recovery and return-to-play was of utmost importance to him. High quality evidence regarding athletic pubalgia is lacking. Only a few case reports and case series demonstrate successful treatment of ID by purely non-surgical means.4,9,12,13 The majority of the literature concur that treatment by surgery more often leads to favorable outcomes compared to non-surgical management alone. 2,3,14 Currently, there is only one case report that has shown successful treatment of ID with PRP.8
Etiology
The exact etiology of ID is under debate. Meyers has described the relationship between the rectus abdominis and the adductor longus and how they play a crucial role in the stability of the anterior pelvis.15–17 The rectus abdominis provides a supero-posterior tension, while the adductors provide an infero-anterior tension to the anterior pelvis.16 Motions such as repetitive hip hyperabduction and lumbar hyperextension, a movement commonly seen in sports, can induce sheering at the pubic symphysis and may lead to a tear or series of microtears of the rectus abdominis muscle or tendon as it inserts onto the pubis.4,17 Cadaveric dissections have shown that when the rectus abdominis is cut, the pelvis tilts anteriorly.15 This finding may suggest that muscle balance is altered in these athletes and this may be the start of a cascade of events that lead to ID.15,17 Meyers performed surgery to strengthen the anterior pelvic floor and reported a 95% success rate via his surgical method.15
Typical presentation of a patient with ID will be a young athletic male who plays a sport that involves running while changing directions, twisting, skating and kicking.2,3,18 The most common sports are soccer, rugby, football and hockey.2,4 They will describe an insidious onset of deep lower abdominal and/or groin pain that is exacerbated with sporting activity, coughing or straining.2
Diagnosis
Groin pain is common among athletes. Anatomically speaking, the groin represents a complex confluence of structures. There are multiple anatomical structures that, when injured, may present as groin pain.2,3,9,15,18 Between 27% and 90% of athletes who present with symptoms of ID may have multiple pathologies, thus examination may require a multidisciplinary approach.2,3 Considering the vast differential diagnosis for groin pain, ID is considered a diagnosis of exclusion 2,3,13,18,19 and can only be confirmed by endoscopic examination. 4,20 Differentials of groin pain include: femeroacetabular impingement, labral tears, muscle contusion, sacroiliac or iliolumbar ligament injury, sprain nerve entrapment/neuropathy, stress fracture, osteoarthritis and referred pain from viscera.2,3,6,18
It has been proposed that diagnostic imaging is mainly used to rule out other causes of groin pain.2,18,21,22 MRI typically reveals non-specific findings in patients with ID.19 The main findings are bone marrow edema and increased signal of the rectus abdominis/adductor aponeurosis. 6,23 A dynamic ultrasound may also be used to assess the integrity of the posterior inguinal wall while having the patient strain.2,6 If weakened, the posterior inguinal wall will displace anteriorly rather than remain taut.2 The sensitivity for this test is 100%, however the specificity is 0%.24,25 It should be noted that this particular phenomenon is often present in asymptomatic athletes, and thus these findings should be clinically correlated.6,26 The gold standard to detect posterior inguinal wall deficiencies is surgical exploration.24
A recent consensus statement on ID proposed a set of criteria to aid in the diagnosis of ID (see Table 1).6 The validity and reliability of these criteria are unknown at this time. Further studies should be conducted to evaluate these criteria. It was also noted that all other causes of groin pain must be excluded.6 In our presented case, 3 of the 5 criteria were met (numbers 1, 4, and 5).
Once the diagnosis of ID is made, a trial of conservative care lasting six to eight weeks should commence.2,4,6,12,27
Non-surgical Management
There are several case reports/series that describe a proposed rehabilitation protocol for ID. Woodward et al12 described a 3-phase rehabilitation protocol of a professional hockey player with the signs and symptoms of ID. Phase 1 (4 days) focused on pain management. Phase 2 (14 days) focused on strength and stability. Phase 3 (31 days) focused on functional progression and return to sport. Treatment lasted a total of 49 days. The athlete was able to return to play without recurrence of these symptoms for the following 8 seasons.
Yuill et al4 reported the non-surgical management (a combination of manual therapy and rehabilitation exercises) of two high-level and one recreational soccer player with ID. Manual therapy for all three patients occurred one to two times per week for six to eight weeks in total, and included soft tissue therapy, laser, microcurrent, electro-acupuncture, and wobenzyme. Rehabilitation exercises were performed three times per week for eight weeks and progressed from strengthening, to functional, to sport specific. All three athletes were able to return to play after eight weeks of treatment without recurrence of symptoms at two years follow-up.
There were similarities between the exercises used in our presented case and the previous cases. All programs included exercises that strengthened and stabilized the muscles that cross the anterior pelvis. However, in our case, the player returned to play in much less time. This can be due to any combination of the PRP injection, manual therapy and exercises.
Surgery
A recent systematic review by Serner et al concluded that there is moderate evidence (evidence provided by one high-quality study and/or two or more low-quality studies and by generally consistent findings in all studies) suggesting that surgery results in better treatment success than non-surgical treatment.1 Surgery should be considered if a trial of conservative care has failed.2,6
The two surgical approaches to treat ID are the open (anterior) approach and the laprascopic (posterior) approach, and there are various methods within each.2,6,22 Favourable outcomes are reported in 63% to 97% of cases for both relief of symptoms and return to previous levels of sport activity.2,6
It should be noted that there are currently no studies that directly compare the various surgical methods.6 There is no clear recommendation as to which method is most appropriate and it is largely determined by the level of the surgeon’s experience and expertise of a particular technique.6 The goal of surgery, independent of the type of surgery used, is to normalize any abnormal tension surrounding the injured tissue (often including an adductor tenotomy).2,6
Platelet-Rich Plasma
Platelet-rich plasma (PRP) has gained interest in the treatment of sport injuries.10 PRP is prepared by collecting a blood sample from the subject. The sample is then put in a centrifuge to separate the platelets from the rest of the sample; this platelet portion is then injected into the injured tissue.10,28,29 Platelets can release several growth factors which may promote tissue healing.10,28,29
In our case, the sports physician decided to inject PRP into the rectus abdominis tear. The patient was informed of the treatment plan and gave consent to treatment. The PRP was prepared using the Angel Hematocrit Setting. A sample of 10mL of blood was drawn in preparation for each injection. A 7% hematocrit setting was used. This method yields a 5.4-fold increase in platelet concentration. There is currently a lack of standardization regarding PRP preparation.28 As a result, it is difficult to conclude efficacy of PRP across the literature due to the heterogeneity of the PRP preparation.10,29 In the author’s (AMG) experience, the Angel Hematocrit Setting has resulted in good results and was used in this particular case.
A recent case report by Scholten et al reported the treatment of a lacrosse player with ID due to a distal rectus abdominis tendinopathy.8 This patient was treated with one injection of PRP into the left distal rectus abdominis muscle. At four weeks post injection, the patient had no pain or tenderness at the pubic symphysis on palpation. At week six, the player was cleared for sport-specific training and modified practice. At eight weeks, the player returned to his normal level of performance prior to injury.
Post-PRP injection, it is recommended to introduce a rehabilitation programme as a synergist to repair and remodel the injured tissue.11 Loading of the tissue (via manual therapy and exercise) leads to upregulation of mechanogrowth factor, leading to activation of satellite cells, which in turn improves the alignment of the regenerating myotubes.11,30 In our case, the patient was referred by the sports physician to the sports chiropractor and the strength and conditioning specialist. The goal of the manual therapy performed by the sports chiropractor included normalizing the abnormal muscular tension across the anterior pelvis. The goal of the strength and conditioning specialist was to strengthen the musculature of the anterior pelvis. Both manual therapy and exercise contributed to loading of the tissue and subsequent cellular processes as described above.
Summary
The scientific literature regarding the conservative management of ID are currently limited to retrospective studies, non-randomised studies, case-controlled studies and case reports.2,3 There is still disagreement in the literature regarding the pathophysiology of ID.2 It includes any combination of injuries to the posterior inguinal wall, conjoint tendon, inguinal ligament, rectus abdominis, hip adductors, external oblique musculature, etc.2–4,6,19,27 There is a need for higher quality studies regarding non-surgical intervention for ID.
ID is common in sports involving running, kicking and twisting motions. We reported a case of a professional hockey player who was non-surgically treated with PRP, chiropractic, and rehabilitation exercises with a relatively quick recovery in 3.5 weeks. This case highlights the importance of a multidisciplinary approach to the diagnosis and management of ID.
Footnotes
Disclaimers: None
Sources of funding: None
Patient written consent was obtained for the use of clinical information and imaging with respect to this case report.
References
- 1.Serner A, van Eijck CH, Beumer BR, Holmich P, Weir A, de Vos R-J. Study quality on groin injury management remains low: a systematic review on treatment of groin pain in athletes. Br J Sports Med. 2015;50:1–11. doi: 10.1136/bjsports-2014-094256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caudill P, Nyland J, Smith C, Yerasimides J, Lach J. Sports hernias: a systematic literature review. Br J Sports Med. 2008;42(12):954–964. doi: 10.1136/bjsm.2008.047373. [DOI] [PubMed] [Google Scholar]
- 3.Swan KG, Wolcott M. The athletic hernia: a systematic review. Clin Orthop Relat Res. 2007;455:78–87. doi: 10.1097/BLO.0b013e31802eb3ea. [DOI] [PubMed] [Google Scholar]
- 4.Yuill EA, Pajaczkowski JA, Howitt SD. Conservative care of sports hernias within soccer players: a case series. J Bodyw Mov Ther. 2012;16(4):540–548. doi: 10.1016/j.jbmt.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Campanelli G. Pubic inguinal pain syndrome: the so-called sports hernia. Hernia. 2010;14(1):1–4. doi: 10.1007/s10029-009-0610-2. [DOI] [PubMed] [Google Scholar]
- 6.Sheen AJ, Stephenson BM, Lloyd DM, et al. “Treatment of the Sportsman’s groin”: British Hernia Society’s 2014 position statement based on the Manchester Consensus Conference. Br J Sports Med. 2013:1–9. doi: 10.1136/bjsports-2013-092872. [DOI] [PubMed] [Google Scholar]
- 7.Tyler TF, Silvers HJ, Gerhardt MB, Nicholas SJ. Groin Injuries in Sports Medicine. Sport Health: A Multidiscip Approach. 2010;2(3):231–236. doi: 10.1177/1941738110366820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scholten PM, Massimi S, Dahmen N, Diamond J, Wyss J. Successful Treatment of Athletic Pubalgia in a Lacrosse Player with Ultrasound-Guided Needle Tenotomy and Platelet-Rich Plasma Injection: A Case Report. PM&R. 2015;7(1):79–83. doi: 10.1016/j.pmrj.2014.08.943. [DOI] [PubMed] [Google Scholar]
- 9.Ellsworth AA, Zoland MP, Tyler TF. Athletic Pubalgia and Associated Rehabilitation. Int J Sports Phys Ther. 2014;9(6):774–784. [PMC free article] [PubMed] [Google Scholar]
- 10.Hamid MSA, Yusof A, Mohamed Ali MR. Platelet-rich plasma (PRP) for acute muscle injury: A systematic review. PLoS ONE. 2014;9(2):e90538. doi: 10.1371/journal.pone.0090538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sánchez M, Anitua E, Delgado D, Sánchez P, Orive G, Padilla S. Muscle repair: platelet-rich plasma derivates as a bridge from spontaneity to intervention. Injury. 2014;45:S7–S14. doi: 10.1016/S0020-1383(14)70004-X. [DOI] [PubMed] [Google Scholar]
- 12.Woodward JS, Parker A, Macdonald RM. Non-surgical treatment of a professional hockey player with the signs and symptoms of sports hernia: a case report. Int J Sports Phys Ther. 2012;7(1):85–100. [PMC free article] [PubMed] [Google Scholar]
- 13.Kachingwe AF, Grech S. Proposed algorithm for the management of athletes with athletic pubalgia (sports hernia): a case series. J Orthop Sports Phys Ther. 2008;38(12):768–781. doi: 10.2519/jospt.2008.2846. [DOI] [PubMed] [Google Scholar]
- 14.Paajanen H, Brinck T, Hermunen H, Airo I. Laparoscopic surgery for chronic groin pain in athletes is more effective than nonoperative treatment: A randomized clinical trial with magnetic resonance imaging of 60 patients with sportsman’s hernia (athletic pubalgia) Surgery. 2011;150(1):99–107. doi: 10.1016/j.surg.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 15.Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BB. Management of severe lower abdominal or inguinal pain in high-performance athletes. Am J Sports Med. 2000;28(1):1–7. doi: 10.1177/03635465000280011501. [DOI] [PubMed] [Google Scholar]
- 16.Meyers WC, Greenleaf R, Saad A. Anatomic basis for evaluation of abdominal and groin pain in athletes. Oper Tech Sports Med. 2005;13:55–61. [Google Scholar]
- 17.Meyers WC, Yoo E, Devon ON, et al. Understanding “Sports Hernia” (Athletic Pubalgia): The Anatomic and Pathophysiologic Basis for Abdominal and Groin Pain in Athletes. Oper Tech Sports Med. 2012;20:33–45. [Google Scholar]
- 18.Hegedus EJ, Stern B, Reiman MP, Tarara D, Wright AA. A suggested model for physical examination and conservative treatment of athletic pubalgia. Phys Ther Sport. 2013;14(1):3–16. doi: 10.1016/j.ptsp.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 19.Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15(8):507–514. doi: 10.5435/00124635-200708000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Kachingwe AF, Grech S. Proposed algorithm for the management of athletes with athletic pubalgia (sports hernia): a case series. J Orthop Sports Phys Ther. 2008;38(12):768–781. doi: 10.2519/jospt.2008.2846. [DOI] [PubMed] [Google Scholar]
- 21.Rabe SB, Oliver GD. Athletic Pubalgia: Recognition, Treatment, and Prevention. Athl Train Sport Heal Care. 2010;2(1):25–30. [Google Scholar]
- 22.Garvey JFW, Read JW, Turner A. Sportsman hernia: What can we do? Hernia. 2010;14:17–25. doi: 10.1007/s10029-009-0611-1. [DOI] [PubMed] [Google Scholar]
- 23.Omar IM, Zoga AC, Kavanagh EC, et al. Athletic pubalgia and “sports hernia”: optimal MR imaging technique and findings. Radiographics. 2008;28:1415–1438. doi: 10.1148/rg.285075217. [DOI] [PubMed] [Google Scholar]
- 24.Orchard JW, Read JW, Neophyton J, Garlick D. Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian Rules footballers. Br J Sports Med. 1998;32(2):134–139. doi: 10.1136/bjsm.32.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drew MK, Osmotherly PG, Chiarelli PE. Imaging and clinical tests for the diagnosis of long-standing groin pain in athletes. A systematic review. Phys Ther Sport. 2014;15(2):124–129. doi: 10.1016/j.ptsp.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 26.Serner A, Tol JL, Jomaah N, et al. Diagnosis of Acute Groin Injuries: A Prospective Study of 110 Athletes. Am J Sports Med. 2015 doi: 10.1177/0363546515585123. [DOI] [PubMed] [Google Scholar]
- 27.Larson CM. Sports hernia/athletic pubalgia: evaluation and management. Sports Health. 2014;6(2):139–144. doi: 10.1177/1941738114523557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moraes VY, Lenza M, Tamaoki MJ, et al. Platelet-rich therapies for musculoskeletal soft tissue injuries (Review) Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev. 2014;(4):CD010071. doi: 10.1002/14651858.CD010071.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grambart ST. Sports Medicine and Platelet-Rich Plasma: Nonsurgical Therapy. Clin Pod Med Surg. 2015;32(1):99–107. doi: 10.1016/j.cpm.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 30.Khan KM, Scott A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. Br J Sports Med. 2009;43(4):247–252. doi: 10.1136/bjsm.2008.054239. [DOI] [PMC free article] [PubMed] [Google Scholar]