Abstract
Objectives
Clinical and epidemiological evidence suggests that cocaine use is associated with an increased risk of premature atherosclerosis. The objectives of this study were to explore (1) whether cocaine abstinence is associated with a reduced marker of endothelial dysfunction, (2) whether cocaine abstinence is associated with a slower coronary plaque progression, and (3) whether reduction in cocaine use is associated with a reduced marker of endothelial dysfunction in African American chronic cocaine users with contrast-enhanced coronary CT angiography-confirmed less than 50% coronary stenosis.
Methods
Between March and June 2014, a total of 57 African American cocaine users with contrast-enhanced CT angiography-confirmed less than 50% coronary stenosis in Baltimore, Maryland, were enrolled in a 6-month follow-up study to investigate whether cocaine abstinence or reduction in cocaine use is associated with decreased endothelin-1 (ET-1) levels and coronary plaque progression at the 6-month follow-up. A voucher-based incentive approach was used to systematically reinforce cocaine abstinence, and urine benzoylecgonine test was implemented to confirm cocaine use.
Results
Among the 57 participants, 44 were HIV-infected. The median of duration of cocaine use was 18 (interquartile range, 7–30) years. According to generalized estimating equation analyses, both cocaine abstinence and reduction in cocaine use in the 6 months were independently associated with decreased ET-1. The incidence of coronary plaque progression was 7.4/100 person-years and 23.1/100 person-years in those who were totally abstinent from cocaine and those who continued to use cocaine, respectively. However, the difference in the incidence between these 2 groups was not significant (exact P = 0.30).
Conclusions
The findings of this study revealed a possible association of cocaine abstinence/reduction with lowered ET levels, which suggests that such changes in cocaine use might be beneficial for preventing endothelial damage. Further studies should be conducted to investigate whether ET-1 could be used as a marker for cocaine abstinence and reduction in cocaine use.
Keywords: African Americans, cocaine use, coronary plaque progression, endothelin-1, incidence
Cocaine use or cocaine use in combination with HIV infection has previously been implicated in the development and acceleration of coronary artery disease (CAD) (Kloner et al., 1992; Benzaquen et al., 2001; Sonne et al., 2005; Phillips et al., 2009). In our previous publications, we have demonstrated that cocaine use with and without HIV infection is associated with an increased risk of subclinical atherosclerosis in African Americans (AAs) (Lai et al., 2002,2005,2008). Despite the extensive research attempting to explain the increased incidence of CAD among persons with cocaine use, the mechanisms linking cocaine use with early atherosclerosis are not well described.
Endothelial dysfunction represents the first step in the pathogenesis of atherosclerosis (Ross, 1999), and increasing evidence suggests that endothelium-derived endothelin-1 (ET-1) is involved in the development of endothelial dysfunction, is increased in coronary and general circulation, and may be associated with the development of early atherosclerosis and endothelial dysfunction (Lerman et al., 1995; Ross, 1999; Pernow et al., 2012).
Cocaine, one of the most commonly abused illegal drugs in the United States, has been shown to increase ET-1, leading to cocaine-induced endothelial dysfunction (Hendricks-Munoz et al., 1996; Wilbert-Lampen et al., 1998; Pradhan et al., 2008). It has been reported that ET-1 in cocaine users was substantially higher than that in noncocaine users, and after cocaine withdrawal for 1 month, ET-1 was improved (Sáez et al., 2011). We have shown that ET-1 in chronic cocaine users is remarkably higher than noncocaine users, and duration of cocaine use is independently associated with ET-1 after controlling for HIV infection and other potential confounding factors (Tai et al., 2012).
Despite recognition that cocaine use promotes atherosclerosis, few studies have been conducted on the potential cardiovascular health benefits of abstinence from cocaine and reduction in cocaine consumption (Sáez et al., 2011). The objectives of this preliminary study were to explore (1) whether total abstinence from cocaine is associated with a reduced marker of endothelial dysfunction, (2) whether total abstinence from cocaine retards coronary plaque progression, and (3) whether reduction in cocaine use is associated with a reduced marker of endothelial dysfunction in AA chronic cocaine users with contrast-enhanced CT angiography (CTA)-confirmed less than 50% coronary stenosis.
METHODS
Study Participants
Between March and June 2014, 57 AA chronic cocaine users (16 women and 41 men) with and without HIV infection were consecutively enrolled in a preliminary study (1) to explore the effects of voucher-based incentives therapy on cocaine abstinence or reduction in cocaine use, (2) to explore whether changes in endothelial-1, a biomarker of endothelial function, are associated with changes in the levels of cocaine use, and (3) to explore whether cocaine abstinence or reduction in cocaine use is associated with coronary plaque progression in chronic cocaine users with contrast-enhanced CTA-confirmed less than 50% coronary stenosis at the Johns Hopkins Hospital, Baltimore, Maryland.
Inclusion criteria were (1) AA study participants aged 25 years or older of our ongoing studies (both HIV positive and HIV negative) with the presence of contrast-enhanced coronary CTA-confirmed less than 50% nonobstructive coronary plaque at enrollment, (2) chronic cocaine use, defined as use of cocaine by any route for at least 6 months, administered at least 4 times a month—infrequent users (fewer than 4 times a month, consecutive 6 months) were not included, and (3) self-reported recent cocaine use, confirmed by a positive urine test for cocaine or benzoylecgonine during the initial screening interview, and fulfilling diagnostic criteria for cocaine dependence on a computerized version of the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), Axis I Disorders. Exclusion criteria were (1) any evidence of clinical CAD, any symptoms believed to be related to cardiovascular disease, (2) history of serious physical disease or current physical disease, chronic obstructive pulmonary disease, seizure, head trauma or central nervous system tumors, or current or past histories of serious psychiatric disorder (ie, Axis I, DSM-IV), other than substance abuse or dependence, (3) pregnancy, or at risk of pregnancy—child-bearing potential and not using effective birth control measures or the intent to become pregnant during the follow-up period, (4) chronic kidney disease with an estimated glomerular filtration rate of less than 60 mL/min/1.73 m2, and (5) contraindication to CT scans, including a history of contrast allergy.
The Committee on Human Research at the Johns Hopkins School of Medicine approved the study protocol, and all study participants provided written informed consent. All procedures used in this study were in accordance with institutional guidelines.
Procedures
Interview, Medical Chart Review, Physical, and Laboratory Examination
All study participants underwent a baseline visit, including a detailed interview to obtain information about sociodemographic characteristics, medical history, behaviors, including alcohol consumption, drug use, and cigarette smoking, and medications. For HIV-positive participants, detailed information about HIV-related risk factors, duration of known HIV infection, and medications, including antiretroviral use, was also collected. A medical chart review was used to confirm the information on medical history and medications provided by the study participants. A physical examination was performed and vital signs were recorded. Routine clinical laboratory blood chemistry tests were conducted. The following laboratory tests were performed at baseline: total serum cholesterol, triglycerides, high-density lipoprotein, low-density lipoprotein, glucose, high-sensitivity C-reactive protein (CRP), and ET-I.
Collection of all the above-mentioned baseline data was repeated at the 6-month follow-up visit.
Anthropometry and Blood Pressure Measurement
Systolic and diastolic blood pressures were measured 3 times with a standard mercury sphygmomanometer. Measurements of height (to the nearest centimeter) and weight (to the nearest kilogram), and waist and hip circumferences, were recorded.
Phlebotomy
Participants were required to fast for at least 12 hours before phlebotomy. A blood sample of approximately 30 mL was drawn from an arm vein by the phlebotomist. The sample was centrifuged, the serum separated. Blood samples were transported to the laboratory at the Pathology Department at the Johns Hopkins Hospital within 4 hours of blood drawing.
ET-1 Assay
Extraction of plasma, assay, and calculation of results followed the specified procedures for EL1SA kit of ET-1 (R&D Systems, Inc, Minneapolis, MN). Standards of different concentration, control, and the samples extracted were assayed simultaneously in duplicate. The within-run precision correlation of variation was 5%.
Voucher-Based Incentive Interventions
The voucher-based incentive program utilized is a contingency management procedure that systematically reinforces cocaine abstinence, with features modeled after the escalating voucher incentive program developed by Higgins and colleagues (Higgins et al., 1993, 1994). Under a voucher earning procedure, points (each point = $1.00) were awarded for cocaine-negative urine test results, with the number of points to be earned increases for each consecutive negative urine test (Table 1). This escalation feature was designed to promote sustained periods of abstinence because a negative urine test was worth more and more money the longer abstinence was maintained. Furthermore, it was designed to promote sustained abstinence by a “reset penalty.” Specifically, should drug use be detected via submission of a cocaine-positive urine sample, the study participant must restart the incentive program at the week 1 level and then proceed again through the weekly steps. Not only did avoidance of the reset serve as a motivator for continued abstinence, but the return to more intensive monitoring was a clinically indicated response to evidence of drug relapse.
TABLE 1.
A 12-Month Abstinence Incentive Program
| Study Week | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 10 | 12 | 14 | 16 | 20 | 24 | 28 | 32 | 36 | 40 | 44 | 48 | 52 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of urine tests per week | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Award ($) for negative urine tests (weekly total) | 10 | 20 | 20 | 30 | 30 | 40 | 40 | 40 | 80 | 80 | 80 | 80 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
A final feature of the schedule was that the frequency of urine testing decreased over time once a stable period of abstinence had been established. Specifically, in the first 4 weeks, participants were asked to provide urine tests twice a week, and earned $ 10 if 2 urine tests were both negative. In weeks 2 and 3, the participant earned $20 for 2 negative urine tests, and earned $30 for 2 negative urine tests in week 4. In weeks 5 to 8, only one urine test per week was required and potential earnings increased from $30 to $40 per week. After week 8, when a stable period of abstinence had been established, frequency of urine collection continued to decline with biweekly testing in weeks 8 to 16, and then once monthly testing after week 16. To counteract the decreased frequency of reinforcement with longer time between testing, the value of the potential earnings increased to $80 with biweekly testing in weeks 10 to 16 and $ 100 with once monthly testing in weeks 20 to 52.
Earned money was distributed immediately after each negative urine test in the form of a check. Doing so provided immediate acknowledgment and reinforcement for the negative test. After money was earned, it belonged to the participant and was never taken back irrespective of subsequent drug use or other adverse behaviors. It was expected, on the basis of previous experience with these types of interventions, that exposure to this incentive program would produce reduced overall amounts of cocaine use in the majority of participants with long periods of sustained abstinence in some participants.
Urine Benzoylecgonine Test
Urine tests were scheduled in advance. Urine samples were collected under observation of a same-sex research assistant, and the temperature of the sample was examined to confirm its validity. Cocaine metabolite quantitation was conducted using Dip Card “DOA 1 Panel Dip Card–COC” (MP Biomedicals, Solon, OH), which was a one-step urinalysis immunochromatography drug rapid test (5 minutes). It provided for qualitative screening of cocaine metabolite in human urine specimens and provided a preliminary analytical test result for on-site testing. The urine samples were also stored for further quantitative urine analysis (Preston et al., 1997). Missing samples were considered positive.
Contrast-Enhanced Coronary CTA
Cardiac CT scans were performed at baseline and at the 6-month follow-up on a Siemens’ second-generation, 128-slice, dual-source CT (Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany).
The study parameters call for the lowest possible dose of radiation to obtain excellent quality studies. The participants arrived for CT in the Johns Hopkins Outpatient Center. An 18 g IV was started in the antecubital fossa and the participant was then brought to the scanner. No premedication was used in the study as the Flash Dual Source scanner can adjust for any heart rate. After a mini test bolus scan to optimize the acquisition timing for the participant (10-mL bolus of contrast and up to 10 low-dose CT slices), the study was performed. The scan parameters are 100 to 120 kVp (depending on the patient’s size), Care Dose reference mAs of 320 (using Care Dose 4D to minimize radiation dose), rotation time of 0.28 seconds, collimation of 128 × 0.6 mm, and average acquisition time of under 5 seconds (heart rate dependent). Scan data were reconstructed with 0.75-mm thickness at 0.5-mm reconstruction spacing using a B26ASA and B30f reconstruction algorithm. Multiphase images were generated across the electrocardiogram pulsing range every 5% to 10% of the R-R interval. Iterative reconstructions were also performed. The scan protocol uses between 80 and 100 mL of an iso-osmolar contrast agent (Vispaque-320, GE Medical Systems) injected at 5 to 6 mL/s with the test bolus data used to calculate the peak contrast enhancement to determine correct scan delay.
All image data were then transferred to a dedicated workstation where image analysis was performed using a combination of axial images, multiplanar reconstruction, and 3D mapping. Specific software programs that were used include lnSpace and Circulation on a Siemens MMW workstation and data analysis on an Rcadia cardiac analysis workstation. All images were interpreted by a radiologist with board certification in cardiac CT interpretation.
Coronary vessels were assessed for patency and stenoses using 3D visualization tools after the axial images were reviewed for determination of anatomy, quality of the study, and appearance of the vessels. One reviewer (E.K.F), blinded to the participants’ risk factor profiles, independently evaluated the contrast-enhanced CTA scans. The coronary artery tree was segmented according to the modified American Heart Association classification, and the segments were investigated for plaque and luminal narrowing. Calcified plaque was defined as a structure 1 mm2 or more in size with attenuation of more than 130 HU visualized separately from the intravascular lumen, identified in at least 2 independent planes. Noncalcified plaque was defined as a low-density area 1 mm2 or more in size and with a CT density 130 HU or less, located within the vessel wall. Partially calcified plaques were categorized into noncalcified plaques. Significant stenosis was defined as more than 50% diameter stenosis.
Statistical Analysis
Statistical analysis was performed with SAS 9.4 (SAS Institute, Cary, NC). All continuous parameters were summarized by medians and interquartile ranges (IQRs), and all categorical parameters were summarized as proportions. To compare between-group differences in demographic and clinical characteristics, laboratory parameters, and other factors, the nonparametric Wilcoxon 2-sample test was used for continuous variables and the Fisher exact test was employed for categorical variables. Incidence rate of coronary plaque progression was calculated by dividing the number of newly diagnosed cases with 50% or more coronary stenosis by the person-years (Pis) of follow-up. An exact method was used to construct the 95% confidence interval for the incidence rate and to compare the incidence rates (Martin & Austin, 1996).
Total cocaine abstinence was defined as all urine tests being negative for 6 months. In the first 8 weeks of the study, urine tests were performed weekly. One positive urine test in each week was counted as 7 days of cocaine use. From weeks 10 to 16, one positive urine test was counted as 14 days of cocaine use. From weeks 16 through 52, one positive urine test was counted as 28 days of cocaine use. Reduction in cocaine use was defined as number of days of no cocaine use, which equals to 182 days (6 months) minus the number of days of cocaine use. Because the distribution of ET-1 was considerably skewed, square-root-transformed ET-1 was used as the outcome variable in regression analyses.
Both bivariable generalized estimating equation (GEE) models (adjusted for baseline ET-1) and multivariable GEE models were used to examine whether cocaine-using days or total abstinence from cocaine was associated with ET-1. Because traditional cardiovascular risk factors may confound the relationships between ET-1 and cocaine use, and because these risk factors may be highly correlated with each other, a composite risk factor score, the 2013 American College of Cardiology (ACC)/American Heart Association (AHA)-defined cardiovascular risk (Goff et al., 2014) was controlled for in multivariable analyses. The 2013 ACC/AHA-defined cardiovascular risk is used to estimate 10-year primary risk of atherosclerotic cardiovascular disease (ASCVD) among individuals without preexisting cardiovascular disease who are between 40 and 79 years of age, on the basis of the Pooled Cohort Equations (Goff et al., 2014). The factors used to estimate ASCVD risk include age, sex, race, total cholesterol, high-density lipoprotein cholesterol, systolic blood pressure, blood pressure-lowering medication use, diabetes status, and smoking status. Estimates of the 10-year risk for ASCVD are based on data from multiple community-based populations and are applicable to African-American and non-Hispanic white men and women 40 through 79 years of age. Family history of heart attack, elevated CRP (>2.0 mg/dL), and baseline ET-1 were also controlled for in the multivariable models. To assess multicollinearity in the independent variables, variance inflation factors from the information matrix were calculated and evaluated. Because these variance inflation factors were small, no further multicollinearity analyses were performed for GEE models. The P values reported are 2-sided. A P value <0.05 indicated statistical significance.
RESULTS
General Characteristics
The demographic and clinical characteristics of these 57 study participants are presented in Table 2. The median age was 54 years and 28% were women. Among the 57 participants, 44 were HIV-infected. The median duration of cocaine use was 18 (1QR, 7–30) years. The median ET-1 was 1.66 (1.35–2.24) pg/mL. The median systolic blood pressure was 127 mm Hg (IQR, 113–137) and the median diastolic blood pressure was 73 mm Hg (IQR, 66–82). The median cardiovascular risk according to the 2013 ACC/AHA guidelines was 10.2 (IQR, 6.9–18.8). Thirty percent of participants had low cardiovascular risk according to the guidelines (Goff et al., 2014).
TABLE 2.
Baseline Characteristics of 57 African American Study Participants in Baltimore, Maryland
| Characteristic | Total* (N = 57) |
|---|---|
| Age, yr | 54 (52–58) |
| Male sex, % | 71.9 |
| Family history of heart attack, % | 26.3 |
| Cigarette smoking, % | 84.2 |
| Cigarette smoking, yr | 30 (20–40) |
| Alcohol use, % | 96.5 |
| Cocaine use, yr | 18 (7–30) |
| BMI, kg/m2 | 27.2 (22.6–31.6) |
| hsCRP, mg/dL | 2.6 (0.8–5.2) |
| hsCRP >2.0, mg/dL | 56.1 |
| Systolic BP, mm Hg | 127 (113–137) |
| Diastolic BP, mm Hg | 73 (66–82) |
| Glucose, mg/dL | 90 (80–97) |
| Total cholesterol, mg/dL | 172 (149–200) |
| LDL-C, mg/dL | 87 (64–107) |
| HDL-C, mg/dL | 57 (47–66) |
| Triglycerides, mg/dL | 120 (88–181) |
| Endothelin-1, pg/mL | 1.66 (1.35–2.24) |
| HIV infection | 77.2 |
| 2013 ACC/AHA risk, % | 10.2 (6.9–18.8) |
| Low 2013 ACC/AHA risk, % | 29.8 |
Median (interquartile range) for continuous variables, proportion (%) for categorical variables.
BMI. body mass index; BP, blood pressure; BSA, body surface area; HDL-C, high-density lipoprotein cholesterol; hsCRP, high-sensitivity C-reactive protein; glucose, fasting glucose; LDL-C, low-density lipoprotein cholesterol; 2013 ACC/AHA risk, cardiovascular risk defined by the 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk (Goff et al, 2014); Low 2013 ACC/AHA risk, cardiovascular risk defined by the 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk ≤7.5%.
Table 3 shows the ET-1 values at baseline and follow-up, and the association between ACC/AHA cardiovascular risk and ET-1 at follow-up. The differences in ET-1 levels at baseline and follow-up were not significant between those who were at low ACC/AHA cardiovascular risk and those who were not. Although the differences in ET-1 levels at baseline and follow-up were not significant between those who were abstinent from cocaine in the 6 months and those who were not, the differences in ET-1 levels between baseline and 6-month follow-up were statistically significant.
TABLE 3.
ET-1 Levels at Baseline and 6-Month follow-up and in Relation to the 2013 ACC/AHA Cardiovascular Risk*
| All | Cocaine Abstinence for 6 mos (+)(N = 28) |
Cocaine Abstinence for 6 mos (−)(N = 29) |
P† | 2013 ACC/AHA- Defined Low Cardiovascular Risk (+)(N = 20) |
2013 ACC/AHA- Defined Low Cardiovascular Risk (−)(N = 37) |
P‡ | |
|---|---|---|---|---|---|---|---|
| Baseline | 1.66 (1.35–2.24) | 1.65 (1.24–2.14) | 1.74 (1.52–2.40) | 0.20 | 1.59 (1.07–1.92) | 1.75 (1.40–2.24) | 0.28 |
| 6-mo follow-up | 1.10 (0.91–1.33) | 1.05 (0.93–1.28) | 1.13 (0.91–1.54) | 0.27 | 1.06 (0.90–1.36) | 1.12 (0.95–1.33) | 0.73 |
| P§ | < 0.0001 | 0.004 | 0.005 | 0.01 | <0.0001 |
Medians (interquartile range) of ET-1 levels (ng/mL) are presented.
Comparisons between those who were totally abstinent from cocaine during the 6 months and those who were not.
Comparisons between those who were at low 2013 ACC/AHA cardiovascular risk and those who were not.
Paired comparisons between baseline and 6-month follow-up.
2013 ACC/AHA risk, cardiovascular risk defined by the 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk; Low 2013 ACC/AHA risk, cardiovascular risk defined by the 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk ≤7.5%.
Total Abstinence From Cocaine and Reduction in Cocaine Use
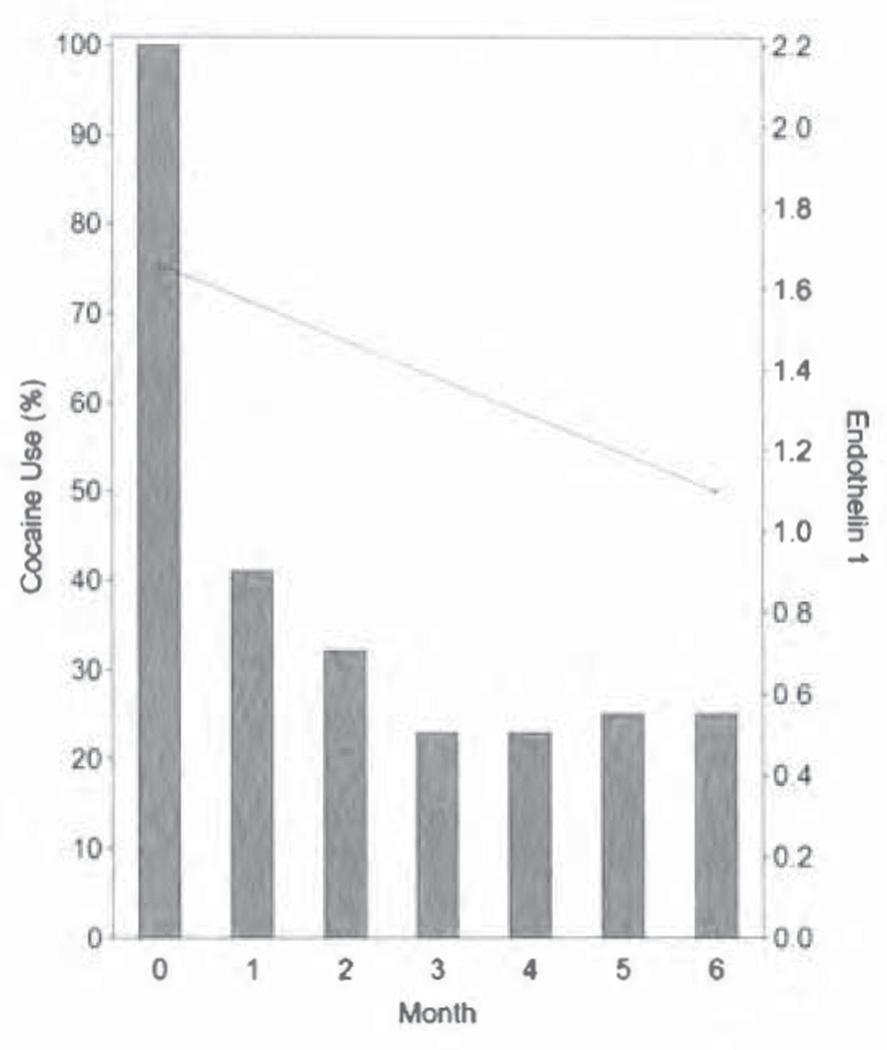
Among these 57 participants, 28 were abstinent from cocaine, whereas 29 continued to use cocaine. Among those who continued to use cocaine, 2 participants used every day on the basis of urine tests. The distribution of cocaine use during the 6 months is presented in Figure 1.
FIGURE 1.
Proportions of study participants using cocaine in the 6-month period and the median ET-1 levels (pg/mL) at baseline and 6-month follow-up. Both the proportions of study participants who were using cocaine in the 6-month period and the median ET-1 levels at baseline and 6-month follow-up are presented in this figure. The proportions of study participants using cocaine are plotted using the y axis on the left side of the figure, whereas the median ET-1 levels at baseline and 6-month follow-up are presented using the y axis on the right side of the figure. The ET-1 at baseline was significantly higher than that at 6-month follow-up (P < 0.0001). ET-1 indicates endothelin-1.
Total Abstinence From Cocaine and Reduction in ET-1
By bivariable GEE analysis (adjusted for baseline ET-1), cocaine abstinence for 6 months was significantly associated with lower ET-1 (P = 0. 039). After controlling for family history of heart attack, baseline ET-1, elevated CRP, and 2013 ACC/AHA cardiovascular risk, total abstinence from cocaine remained significantly associated with decreased ET-1 (P = 0.041) (Table 4).
TABLE 4.
Effects of Total Abstinence From Cocaine and Other Factors on Endothelin-1 Levels (Square-Root Transformed): Generalized Estimating Equation Analysis (N = 57)
| Bivariate Model* | Multivariate Model | |||||
|---|---|---|---|---|---|---|
| Factor | Regression Coefficient |
SE | P | Regression Coefficient |
SE | P |
| Family history of heart attack | 0.0283 | 0.0572 | 0.62 | 0.0060 | 0.0557 | 0.91 |
| hsCRP >2.0, mg/dL | − 0.0866 | 0.0431 | 0.045 | −0.0838 | 0.0511 | 0.10 |
| Baseline ET-1 <1.0, pg/mL | −0.2741 | 0.0290 | <0.0001 | −0.2780 | 0.0396 | <0.0001 |
| Low 2013 ACC/AHA risk | −0.0148 | 0.0543 | 0.78 | −0.0578 | 0.0633 | 0.36 |
| Cocaine abstinence in the 6 mos | −0.0846 | 0.0409 | 0.039 | −0.0829 | 0.0407 | 0.041 |
Adjusted for baseline ET-1 < 1.0 pg/mL.
ET-1 endothelin-1; hsCRP, high-sensitivity C-reactive protein; Low 2013 ACC/AHA risk, cardiovascular risk denned by the 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk≤7.5% (Goff et al, 2014); SE, standard error.
Reduction in Cocaine Use and Reduction in ET-1
By bivariable GEE analysis (adjusted for baseline ET-1), reduction in cocaine use was marginally significantly associated with decreased ET-1 (P = 0.07). However, after controlling for family history of heart attack, baseline ET-1, elevated CRP, and 2013 ACC/AHA risk, reduction in cocaine use was independently associated with decreased ET-1 (P = 0.021) (Table 5).
TABLE 5.
Effects of Days of Cocaine Use and Other Factors on Endothelin-1 Levels (Square-Root Transformed): Generalized Estimating Equation Analysis (N = 57)
| Bivariate Model* | Multivariate Model | |||||
|---|---|---|---|---|---|---|
| Factor | Regression Coefficient |
SE | P | Regression Coefficient |
SE | P |
| Family history of heart attack | 0.0283 | 0.0572 | 0.62 | 0.0251 | 0.0567 | 0.66 |
| hsCRP >2.0, mg/dL | −0.0866 | 0.0431 | 0.045 | −0.0977 | 0.0492 | 0.047 |
| Baseline ET-1 <1.0, pg/mL | −0.2741 | 0.0290 | <0.0001 | −0.2931 | 0.0391 | <0.0001 |
| Low 2013 ACC/AHA risk | −0.0148 | 0.0543 | 0.79 | −0.0419 | 0.0645 | 0.52 |
| Reduction in cocaine use in the 6 mos | −0.0006 | 0.0003 | 0.07 | −0.0007 | 0.0003 | 0.021 |
Adjusted Tor baseline ET-1 <l.0pg/mL.
ET-1 endothelin-1; hsCRP, high-sensitivity C-reactive protein; Low 2013 ACC/AHA risk, cardiovascular risk defined by the 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk ≤7.5% (Goff et al, 2014); SE, standard error.
Incidence of Coronary Plaque Progression
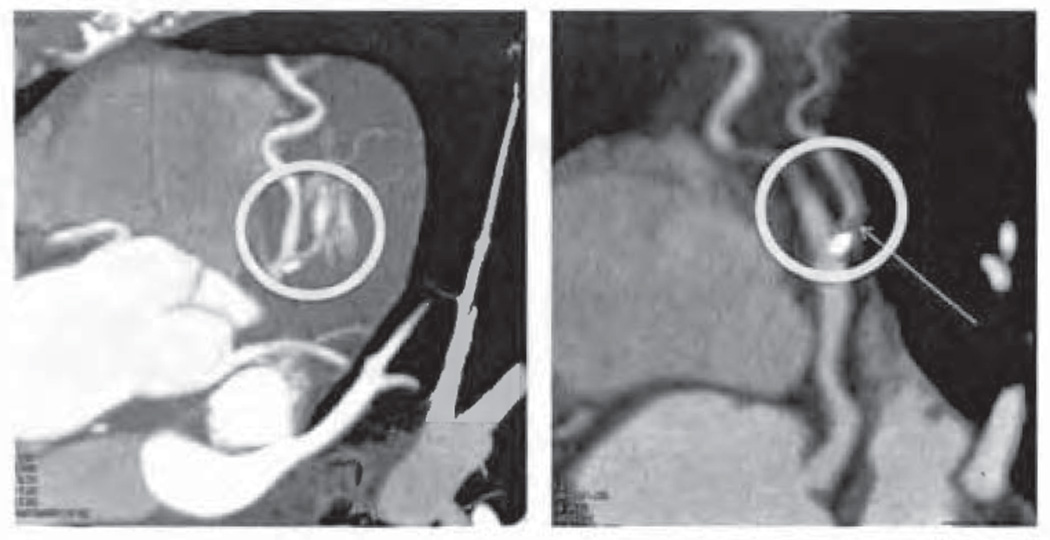
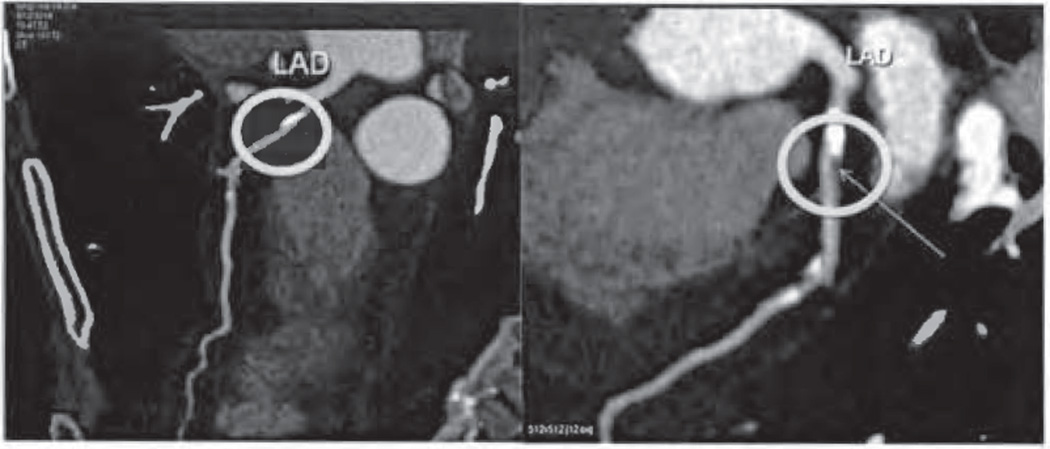
The incidence of coronary plaque progression in these 57 participants was 15.1/100 PYs. The incidence of coronary plaque progression was 7.4/100 PYs and 23.1/100 PYs in those who were totally abstinent from cocaine, and those who continued to use cocaine, respectively. However, the difference in the incidence between these 2 groups was not significant (exact P = 0.30; Table 6). Coronary CTA images to demonstrate plaque progression from baseline to 6-month follow-up are shown in Figures 2 and 3.
TABLE 6.
Incidence of Coronary Plaque Progression by Cocaine Use in 57 Chronic Cocaine Users
| Coronary Plaque Progression | ||||
|---|---|---|---|---|
| Factor | No. Cases | PY | Incidence per 100 PYs (95%CI) |
P* |
| Abstinence from cocaine | 1 | 13.5 | 7.41 (0.10–41.21) | 0.30 |
| Not abstinence from cocaine | 3 | 13.0 | 23.08 (4.64–67.42) | |
| All | 4 | 26.5 | 15.09 (4.06–38.64) | |
On the basis of exact test.
CI, confidence interval; PY, person-year.
FIGURE 2.
Coronary plaque progression detected by consecutive coronary CTA in the 61-year-old male cocaine user. The participant underwent contrast-enhanced coronary CTA on March 27, 2014 (baseline), and October 2, 2014 (6-month follow-up). In the left image from baseline CTA, calcified plaque in the proximal left anterior descending coronary artery (LAD) near the first diagonal is eccentric and no any narrowing is seen. In the right image from 6-month follow-up, plaque is seen in the proximal LAD near the first diagonal, causing at least 50% diameter stenosis. During the 6-month study, he used cocaine for 70 days. CTA indicates CT angiography.
FIGURE 3.
Coronary plaque progression detected by consecutive coronary CTA in the 51-year-old female cocaine user. The participant underwent contrast-enhanced coronary CTA on March 12, 2014 (baseline), and September 25, 2014 (6-month follow-up). In the left image from baseline CTA, calcified plaque in the proximal LAD is present; causing less than 20% diameter stenosis and no noncalcified plaque is seen. In the right image from 6-month follow-up, in addition to calcified plaque, noncalcified plaque is present, causing roughly 50% diameter stenosis. During the 6-month study, she used cocaine for 98 days. CTA indicates CT angiography; LAD, left anterior descending coronary artery.
DISCUSSION
The findings of this preliminary study suggest that both total abstinence from cocaine and reduction in cocaine use are associated with reductions in ET-1, a marker of endothelial dysfunction, suggesting that such changes in cocaine use might lead to reduced endothelial damage and thus better cardiovascular health outcomes in chronic cocaine users with less than 50% coronary stenosis. In this study we may have overestimated cocaine use by assuming that subjects used cocaine all days between the last test and a positive test. Despite this, our intervention was successful, with half our patients achieving total abstinence and only 2 patients with positive screens through the entire duration of the study. This suggests that even in those with incomplete abstinence there probably was reduction in use, in keeping with the findings in previous studies.
This study found that total abstinence from cocaine for 6 consecutive months was significantly associated with a lower ET-1 after adjusting for age, sex, and the 2013 ACC/AHA-defined cardiovascular risk. It was previously reported that after 1 month of cocaine abstinence, ET-1 levels in cocaine users in a drug rehabilitation setting (N = 20) were significantly lower, compared with ET levels before cocaine abstinence (Sáez et al., 2011). However, demographic factors and cardiovascular risks in these participants were not adjusted for in the data analysis. The current study was conducted in a community-based setting. We used a voucher-based incentive approach to encourage cocaine users to quit and urine test to confirm continuing cocaine use or cocaine abstinence. Because elevated ET-1 is a marker for endothelial dysfunction and damage (Chong et al., 2003), our study provides preliminary evidence that cocaine abstinence is independently associated with less endothelial dysfunction and damage.
This study also found that the number of days of cocaine use was positively associated with ET-1 levels, suggesting that reduction in cocaine use is independently associated with less endothelial dysfunction and damage. This finding has not been reported previously.
The incidence of coronary plaque progression in these 57 chronic cocaine users with less than 50% coronary stenosis is alarmingly high (15/100 PYs). The incidence implies that if we followed up 100 AA chronic cocaine users with less than 50% coronary stenosis for 1 year (who are similar to our sample, eg, large sample, high prevalence of cigarette smoking, and HIV infection), 18 would develop significant (≥50%) coronary stenosis. In our ongoing study, among 85 AA noncocaine users with less than 50% coronary stenosis at the first CTA, 11 developed 50% or more coronary stenosis at the second CTA, yielding an incidence of coronary plaque progression of 4.58 (95% confidence interval, 2.29–8.19)/100 PYs. Previous work has shown that participants using cocaine have increased plaque deposition and increased coronary artery stenosis and risk for premature cardiovascular morbidity and mortality (Lai et al., 2002, 2005, 2008). We found that 2 of our participants using cocaine progressed to more than 50% stenosis during the brief 6-month duration of this study (whereas one of the participants who were abstinent progressed). Nevertheless, it must be clearly understood that the difference between these 2 groups in coronary plaque progression was not statistically significant with a P value of 0.30. Thus, these findings should be regarded merely suggestive. Further studies should be conducted to confirm these results.
This study was designed to explore whether cocaine abstinence and reduced use are associated with improved cardiovascular health outcomes with the use of the voucher program. Although the association between cocaine abstinence and reduced use and lowered ET-1 levels were observed, this study failed to provide evidence indicating cocaine abstinence and reduced use lower the risk of subclinical or clinical cardiovascular hard endpoints, such as myocardial infarction and mortality.
Several potential limitations of this study merit discussion. First, this is a preliminary study with a small sample size and short follow-up time. Although there was sufficient statistical power to yield precise ET-1 measurements, the incidence of coronary plaque progression estimated from this study had wide 95% confidence intervals, indicating the point estimate of incidence is not as precise. Second, the study participants were not a random sample of the people in the community. Thus, the findings from this study should be generalized to other settings with caution. Third, because the urine testing was scheduled in advance, and because urine testing was not randomly performed, some participants could “prepare” for their urine tests by not using cocaine, or could have timed their use to avoid detection. Fourth, this study may have missed cocaine use episodes given the short half-life of cocaine (approximately 0.8 ± 0.2 hours) and benzoylecgonine (approximately 6 hours) and the fact you are only testing urine at most 2 times per week (eg, negative on Monday, used Tuesday, negative on Thursday, used Friday/Saturday, and negative on Monday). Also, if the urine testing was not random, it is even more likely that people could have timed their use to avoid detection. Lastly, because 41 of the 57 participants were HIV-infected, the impact of HIV infection on ET-1 could not be investigated. Fifth, although elevated ET-1 levels may be associated with early atherosclerosis and endothelial dysfunction, it is not known what the observed magnitude of difference in ET-1 levels means for a clinically important effect on endothelial damage or cardiovascular disease of clinical significance (eg, unknown meaning of a −0.0829 in effect of abstinence on the square root of ET-1 levels, Table 4). Sixth, although it has been reported that cocaine increases the ET-1 release in vitro and in vivo, and cocaine seems to be an exogenous stimulator at endothelial sigma-receptors (Wilbert-Lampen et al., 1998), the exact mechanisms by which cocaine exposure influences ET-1 levels are not fully understood. Lastly, this study is not a randomized clinical trial, and therefore no causal inference (eg, cocaine abstinence causes decreased ET-1) can be drawn from this data.
Despite its limitations, the findings of this study revealed a possible association of cocaine abstinence/reduction with lowered ET levels, which suggests that such changes in cocaine use might be beneficial for preventing endothelial damage. Further studies should be conducted to investigate whether ET-1 could be used as a marker for cocaine abstinence and reduction in cocaine use.
Acknowledgments
We thank the study participants for their contributions.
Funded by the National Institute on Drug Abuse, National Institutes of Health (NIH R01-DA 12777, DA035632, DA25524, and DAI5020). There are no relationships with industry.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Benzaquen BS, Cohen V, Eisenberg MJ. Effects of cocaine on the coronary arteries. Am Heart J. 2001;142(3):402–410. doi: 10.1067/mhj.2001.117607. [DOI] [PubMed] [Google Scholar]
- 2.Chong AY, Blann AD, Lip GY. Assessment of endothelia damage and dysfunction: observations in relation to heart failure. QJM. 2003;96:253–267. doi: 10.1093/qjmed/hcg037. [DOI] [PubMed] [Google Scholar]
- 3.Goff DC, Jr, Lloyd-Jones DM, Bennett G, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2935–2959. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hendricks-Munoz KD, Gerrets RP, Higgins RD, et al. Cocaine-stimulated endothelin-1 release is decreased by angiotensin-converting enzyme inhibitors in cultured endothelial cells. Cardiovasc Res. 1996;31(1):117–123. doi: 10.1016/s0008-6363(95)00168-9. [DOI] [PubMed] [Google Scholar]
- 5.Higgins ST, Budney AJ, Bickel WK, et al. Achieving cocaine abstinence with a behavioural approach. Am J Psychiatry. 1993;150:763–769. doi: 10.1176/ajp.150.5.763. [DOI] [PubMed] [Google Scholar]
- 6.Higgins ST, Budney AJ, Bickel WK, et al. Incentives improve outcome in out-patient behavioural treatment of cocaine dependence. Arch Gen Psychiatry. 1994;51:568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- 7.Kloner RA, Hale S, Alker K, et al. The effects of acute and chronic cocaine use on the heart. Circulation. 1992;85(2):407–419. doi: 10.1161/01.cir.85.2.407. [DOI] [PubMed] [Google Scholar]
- 8.Lai S, Fishman EK, Lai H, et al. Long-term cocaine use and antiretroviral therapy are associated with silent coronary artery disease in cardiovascularly asymptomatic African Americans with HIV infection. Clin Infect Dis. 2008;46:600–610. doi: 10.1086/526782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lai S, Lai H, Meng Q, et al. Effect of cocaine use on coronary calcification among black adults in Baltimore. Am J Cardiol. 2002;90:326–328. doi: 10.1016/s0002-9149(02)02475-x. [DOI] [PubMed] [Google Scholar]
- 10.Lai S, Lima JA, Lai H, et al. HIV-1 infection, cocaine, and coronary calcification. Arch Intern Med. 2005;165:690–695. doi: 10.1001/archinte.165.6.690. [DOI] [PubMed] [Google Scholar]
- 11.Lerman A, Holmes DR, Bell MR, et al. Endothelin in coronary endothelial dysfunction and early atherosclerosis in humans. Circulation. 1995;92:2426–2431. doi: 10.1161/01.cir.92.9.2426. [DOI] [PubMed] [Google Scholar]
- 12.Martin DO, Austin H. Exact estimates for a rate ratio. Epidemiology. 1996;7(1):29–33. doi: 10.1097/00001648-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Pernow J, Shemyakin A, Böhm F. New perspectives on endothelin-1 in atherosclerosis and diabetes mellitus. Life Sci. 2012;91(13–14):507–516. doi: 10.1016/j.lfs.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 14.Phillips K, Luk A, Soor GS, et al. Cocaine cardiotoxicity: a review of the pathophysiology, pathology, and treatment options. Am J Cardiovasc Drugs. 2009;9(3):177–196. doi: 10.2165/00129784-200909030-00005. [DOI] [PubMed] [Google Scholar]
- 15.Pradhan L, Mondal D, Chandra S, et al. Molecular analysis of cocaine-induced endothelial dysfunction: role of endothelin-1 and nitric oxide. Cardiovasc Toxicol. 2008;8(4):161–171. doi: 10.1007/s12012-008-9025-z. [DOI] [PubMed] [Google Scholar]
- 16.Preston KL, Silverman K, Schuster CR, et al. Assessment of cocaine use with quantitative urinalysis and estimation of new uses. Addiction. 1997;92(6):717–727. [PubMed] [Google Scholar]
- 17.Ross R. Atherosclerosis—an inflammatory disease. New Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 18.Sáez CG, Olivares P, Pallavicini J, et al. Increased number of circulating endothelial cells and plasma markers of endothelial damage in chronic cocaine users. Thromb Res. 2011;128(4):e18–e23. doi: 10.1016/j.thromres.2011.04.019. [DOI] [PubMed] [Google Scholar]
- 19.Sonne C, Stempfle HU, Klauss V, et al. Intravascular ultrasound-guided percutaneous coronary intervention in a human immunodeficiency virus-positive patient with cocaine-associated acute myocardial infarction: case report and review. Heart Lung Circ. 2005;14(3):197–200. doi: 10.1016/j.hlc.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 20.Tai H, Lai H, Jani J, et al. HIV infection and cocaine use induce endothelial damage and dysfunction in African Americans. Int J Cardiol. 2012;161(2):83–87. doi: 10.1016/j.ijcard.2011.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilbert-Lampen U, Seliger C, Zilker T, et al. Cocaine increases the endothelial release of immunoreactive endothelin and its concentrations in human plasma and urine: reversal by coincubation with sigma-receptor antagonists. Circulation. 1998;98(5):385–390. doi: 10.1161/01.cir.98.5.385. [DOI] [PubMed] [Google Scholar]