Abstract
A local breast cancer recurrence or a new breast cancer in the previously treated breast is a staging challenge. Staging is important to tailor the local and the systemic treatment. Earlier treatment(s) can disrupt the primary lymphatic drainage. After the disruption, new lymphatic drainage pathways are often created. The identification of these new pathways together with their sentinel node(s) (SN) is important for retreatment. A fluorodeoxyglucose positron emission tomography-computerized tomography could be useful to identify the involved node(s), but, unfortunately, there is no evidence to support this. Ideally, in the case of a recurrence, an SN biopsy should be performed in order to identify the “new” draining lymph node(s). This new draining SN(s) can be located in unexpected places, and tumor invasion will lead to a change in the management.
Keywords: recurrence, sentinel node, treatment, radionuclide imaging, biopsy, breast cancer
The introduction of sentinel node biopsy (SNB) in breast cancer has led to a considerable reduction of axillary lymph node dissection (ALND) and related morbidity. It also created new options in the management of breast cancer recurrence. SNB has been regarded as a contraindication in the case of previous breast/axillary surgery, radiotherapy, or neoadjuvant chemotherapy.1,2 However, it is actually an indication to reveal new routes of dissemination.1,2
After conservative breast cancer surgery and radiotherapy, the local recurrence rate after 10 years is about 10%–20%.3,4 The knowledge of an involved lymph node after the local recurrence is important because it can alter the adjuvant systemic and local treatment.4–6 Therefore, it seems justified to perform SNB in all cases of local breast cancer recurrence. We recently found three different lymphatic pathways in a patient with a breast cancer recurrence. She has given her consent for publication of this case report.
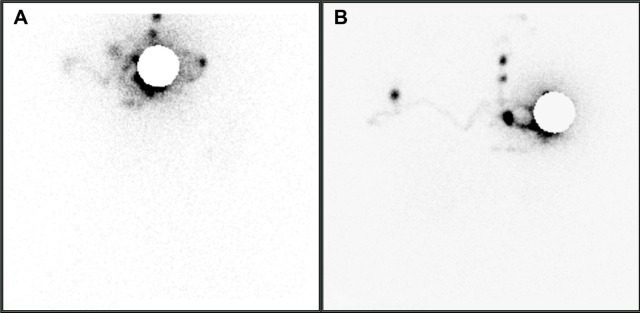
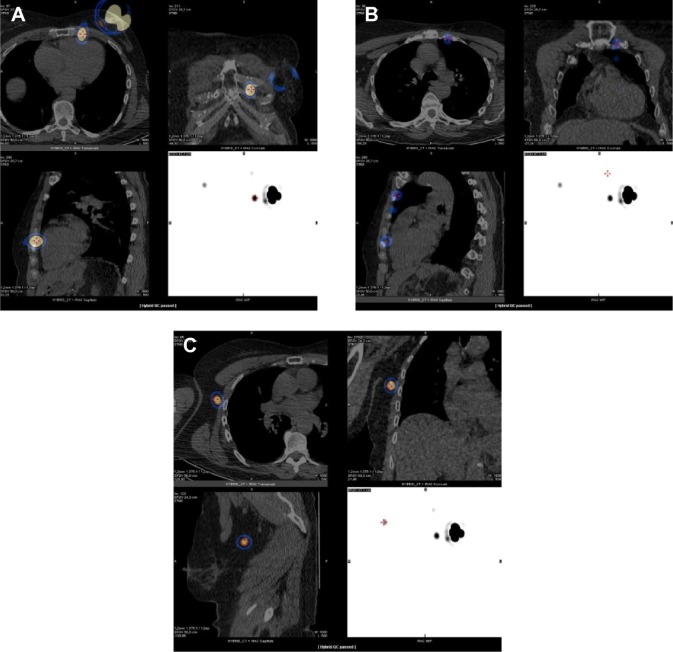
The patient had been diagnosed with breast cancer in her left breast at the age of 43 years. Her treatment at that time consisted of removal of the tumor, ALND, and adjuvant radiotherapy. The tumor was staged as pT2pN0M0. At the age of 72 years, she was again diagnosed with breast cancer in the same upper lateral quadrant of her left breast. Histology showed a high-grade invasive ductal-type carcinoma. There were no signs of metastatic disease. After multidisciplinary discussion, the management advice was a mastectomy and SNB with an intraoperative assessment (touch imprint cytology). In the case of lymph node involvement, an additional clearance would be performed. On the day of the operation, 2.5 mCi (93 MBq) of 99mtechnetium-labeled nanocolloids (Nanocoll, GE Healthcare) were injected intradermally into either side of the excision scar. Blue dye was not injected simultaneously. Thirty minutes after the injection, a planar left oblique anterior image of the left axilla, an anterior image (Fig. 1), and a single-photon emission computerized tomography-computed tomography of the thorax (Fig. 2) were acquired, which showed an SN at the right and left axilla and also the presence of SN at the site of the mammaria interna (Figs. 1 and 2). Histological examination showed that all the SNs were tumor free. Involvement of the lymph nodes would have altered the adjuvant therapy considerably for this patient. Extra-axillary drainage would have an impact on the treatment if there is a lymph node invasion. For instance, an involved parasternal or contralateral axillary lymph node and a negative ipsilateral axillary lymph node could indicate parasternal radiotherapy and systemic therapy (eg, chemotherapy/targeted therapy) for the patient. There is growing evidence that a fluorodeoxyglucose positron emission tomography-CT (FDG PET-CT) is better than conventional modalities in detecting occult extra-axillary lesions, upstaging the disease with an impact on the systemic management.7 In locally advanced breast cancer, a positive FDG PET-CT is highly predictive. However, it needs to be validated if this is also true for early breast cancer. Moreover, there is limited knowledge regarding the significance of FDG PET-CT for locoregional nodal staging in breast cancer recurrence. It would be interesting to conduct a study in which FDG PET-CT and the histology of SNB in patients with recurrent breast cancer are compared in order to assess the sensitivity and specificity of FDG PET-CT in lymph node staging.
Figure 1.
A planar anterior left oblique image of the left axilla (A) and an anterior image of the thorax (B) showing an ipsi and contralateral SN in the axillae and the site of the mammaria interna.
Figure 2.
Hybrid SPECT-CT images of the SN at the site of the mammaria interna (A, B) and contralateral axillae (C).
The involvement of lymph nodes in a previous surgery or radiotherapy or neoadjuvant chemotherapy is regarded as a contraindication to SNB because the lymphatic drainage could be blocked or disrupted. Physiologically, in most cases, the human body will create a “new” or alternative lymphatic drainage. A SN identification procedure will lead to the draining lymph node of the tumor. Identification of this lymph node has to be regarded as the true sentinel, irrespective of its location. There are only a few published reports on SN in breast cancer recurrence. Kothari et al performed a literature review regarding SN in local relapse in women who had previously undergone limited axillary surgery (<9 nodes removed).4 In total, 199 patients were included and the success rate of SN localization at reoperation was 83% (range 68%–100%). During the follow-up period of 26–46 months, no axillary recurrences were noted.4
Intra et al8 analyzed 212 patients with operable local breast cancer recurrence treated previously with conservative surgery and a negative SNB. Preoperative lymphoscintigraphy demonstrated a new axillary SN in 207 cases (97.7%), and the success rate of SNB was 92.5%. They also visualized extra-axillary pathways in 17 patients (8%) and reported that the axillary recurrence rate after a median follow-up of 48 months was 0.8% and the cumulative incidence of axillary recurrence at 5 years was 3.9%. Tasevski et al9 performed a retrospective study to assess the feasibility, outcomes, and utility of SNB in local breast cancer recurrence. Eighteen patients with local breast cancer who had previously undergone axillary surgery and a reoperative SNB were included. SNB was successful in 12 of the 18 patients (with contralateral axillary localization in four patients). These studies demonstrated that the contraindications for performing a SNB in breast cancer might therefore be actually the best indications to perform a SNB.
Multiple injection techniques exist, including peritumoral, subdermal, periareolar, intradermal, and subareolar; however, the applied method of injection does not significantly affect the detection of the SN when the injection is performed superficially.10 De Cicco et al11 demonstrated that there was no overall difference between peritumoral and intradermal injection in terms of detection of the SN, although the intradermal injection appears to be superior, because it is simple to perform, relatively inexpensive, well accepted by patients, showed a better intranodal uptake, and has a faster visualization of the SN. Usually, a subdermal injection of 0.5 mL over the tumor site is performed or, if the lump is not palpable, ultrasound guidance can be used. Periareolar injection is used when the tumor is in the upper quadrant (to minimize the crosstalk between the injection site and SN at the site of the axilla) or when the practitioner has less experience.10 When a SNB is performed in the case of breast cancer recurrence, the site of injection is important because of the blockage or disrupted lymphatic drainage. Studies demonstrated a better identification rate when the injection was made peritumorally (in case of no prior excision) or on both sides of the scar.4 The alternative SN can be located in unexpected places, and tumor invasion will lead to a change in the management.
Footnotes
ACADEMIC EDITOR: Goberdhan P. Dimri, Editor in Chief
PEER REVIEW: Three peer reviewers contributed to the peer review report. Reviewers’ reports totaled 799 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Author Contributions
Provided clinical care and conceived the concepts: AA, WT. Analyzed the data: AA, IH, SS, WT. Wrote the first draft of the manuscript: AA. Contributed to the writing of the manuscript: IH, SS, WT. Agree with manuscript results and conclusions: AA, IH, SS, WT. Jointly developed the structure and arguments for the paper: AA, IH, SS, WT. Made critical revisions and approved final version: AA, IH, SS, WT. All authors reviewed and approved of the final manuscript.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
REFERENCES
- 1.Tjalma WAA. The contraindications for a sentinel node biopsy in breast cancer are actually indications. Surgeon. 2015;13:59–60. doi: 10.1016/j.surge.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 2.Wellner R, Dave J, Kim U, Menes TS. Altered lymphatic drainage after breast-conserving surgery and axillary node dissection: local recurrence with contralateral intramammary nodal metastases. Clin Breast Cancer. 2007;7(6):486–488. doi: 10.3816/CBC.2007.n.006. [DOI] [PubMed] [Google Scholar]
- 3.Palit G, Jacquemyn Y, Tjalma W. Sentinel node biopsy for ipsilateral breast cancer recurrence: a review. Eur J Gynaecol Oncol. 2008;29(6):565–567. [PubMed] [Google Scholar]
- 4.Kothari MS, Rusby JE, Agusti AA, MacNeill FA. Sentinel lymph node biopsy after previous axillary surgery: a review. Eur J Surg Oncol. 2012;38(1):8–15. doi: 10.1016/j.ejso.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Tjalma WA. The importance of performing a sentinel node biopsy in case of recurrent vulval cancer. Int J Gynecol Cancer. 2014;24(4):622. doi: 10.1097/IGC.0000000000000119. [DOI] [PubMed] [Google Scholar]
- 6.Cordoba O, Perez-Ceresuela F, Espinosa-Bravo M, et al. Detection of sentinel lymph node in breast cancer recurrence may change adjuvant treatment decision in patients with breast cancer recurrence and previous axillary surgery. Breast. 2014;23(4):460–465. doi: 10.1016/j.breast.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Liu Y. Role of FDG PET-CT in evaluation of locoregional nodal disease for initial staging of breast cancer. World J Clin Oncol. 2014;5(5):982–989. doi: 10.5306/wjco.v5.i5.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Intra M, Viale G, Vila J, et al. Second axillary sentinel lymph node biopsy for breast tumor recurrence: experience of the European Institute of Oncology. Ann Surg Oncol. 2015;22(7):2372–2377. doi: 10.1245/s10434-014-4282-5. [DOI] [PubMed] [Google Scholar]
- 9.Tasevski R, Gogos AJ, Mann GB. Reoperative sentinel lymph node biopsy in ipsilateral breast cancer relapse. Breast. 2009;18(5):322–326. doi: 10.1016/j.breast.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Giammarile F, Alazraki N, Aarsvold JN, et al. The EANM and SNMMI practice guideline for lymphoscintigraphy and sentinel node localization in breast cancer. Eur J Nucl Med Mol Imaging. 2013;40(12):1932–1947. doi: 10.1007/s00259-013-2544-2. [DOI] [PubMed] [Google Scholar]
- 11.De Cicco C, Cremonesi M, Luini A, et al. Lymphoscintigraphy and radioguided biopsy of the sentinel axillary node in breast cancer. J Nucl Med. 1998;39(12):2080–2084. [PubMed] [Google Scholar]