Abstract
OBJECTIVE
Current endoscopic transection devices are not optimized to meet the unique challenges posed by the task of vessel transection in difficult-to-access locations within the pleural cavity. The ECHELON FLEX™ powered vascular stapler (PVS) has been designed with four rows of staples instead of six, to decrease its size and enable more precise placement on fragile pulmonary vessels, using a narrower anvil than other commercially available transecting devices. This study was performed to determine whether the reduced number of staple rows affects haemostasis, and to assess surgeons' initial impression of the smaller stapler during in vivo usage.
METHODS
The new four-row stapler was compared with commercially available six-row articulating staplers via expert graders using a validated scale of haemostasis in vivo after application on porcine gastroepiploic pedicles and other thin- and thick-walled vessels. The new stapler was then compared with current products by practising thoracic surgeons (n = 27) during in vivo usage of simulated pulmonary procedures in a porcine model. The surgeons were also surveyed on the key attributes of the four-row stapler in relation to the six-row predicates.
RESULTS
Haemostasis evaluated on an ordered scale was clinically equivalent between the test and predicate staplers, and was deemed acceptable for all thin- and thick-vascular tissue applications. Surgeons found no difference in haemostasis between the four- and six-row staplers (P = 0.486), and judged the four-row stapler superior in terms of access, reduced need for dissection, reduced stress of surgeon and precise control (P < 0.001 for all).
CONCLUSIONS
The new ECHELON FLEX™ PVS provides haemostasis equivalent to six-row staplers. With a smaller anvil, narrower shaft and wider angle of articulation, the PVS demonstrated improved access capability for pulmonary vessel procedures.
Keywords: Stapler, Endocutter, Thoracic, Access, Haemostasis, Vascular
INTRODUCTION
In thoracoscopic surgery, endoscopic transection devices such as endostaplers are routinely used for applications on the pulmonary artery and vein, bronchus and lung parenchyma. Pulmonary vessels in particular are delicate, thin walled and easily damaged. Access to these vessels is challenging since they are immobile and located deep in the chest at the hilum. Manoeuvrability of a thoracoscopic device is limited by the fixed ribs and the narrow rib space, especially in cases of a thick chest wall or ‘low ceiling’, where the distance from the mediastinum to the lateral chest wall is less.
Current endoscopic devices are not optimized to meet the unique challenges posed by the task of pulmonary vessel division in difficult-to-access locations within the pleural cavity, for example, during major lung resection procedure. Decreasing the size of the transection device would make access to critical vascular structures in thoracic surgery easier by limiting the amount of vascular dissection required and potentially allowing for minimally invasive approaches in the management of more central tumours where only a limited dissection of the vessels is possible.
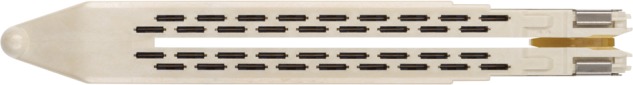
The ECHELON FLEX™ powered vascular stapler (PVS) (Fig. 1) has been designed to enable more precise placement on fragile pulmonary vessels using a narrower anvil than standard six-row staplers. The new PVS is a 35-mm articulating endocutter that allows for a broader range of approach angles due to its thinner shaft and wider angle of articulation when working within the limits of the intercostal space. The decrease in size has been accomplished by changing from six rows of staples to four rows of staples in a staggered pattern with a modified staple form. This new design makes the PVS well suited for vascular applications at the pulmonary hilum deep in the pleural space.
Figure 1:
ECHELON FLEX™ powered vascular stapler with advanced placement tip.
With a decrease in the number of rows of staples to secure the vessel following division, a potential concern would be a corresponding decrease in the haemostatic capability of the device. This study was performed in order to determine whether the novel design of the four-row PVS provides haemostasis similar to that of commercially available six-row staplers. Comparison of haemostasis for four- and six-row staplers was performed in two separate experiments: (i) in preclinical studies using a validated Likert scale of haemostasis administered by internal experts and (ii) in preclinical evaluations by practising thoracic surgeons at multiple sites within and outside the USA. After the evaluation of haemostasis, surgeons were also surveyed on the use of the devices, especially as to whether the new, smaller device did indeed provide easier placement, potentially reducing the amount of dissection required, facilitating the procedure and enabling more precise control of the stapler.
MATERIALS AND METHODS
All in vivo procedures were approved by an Institutional Animal Care and Usage Committee. Devices and cartridges used in the study are illustrated in Table 1.
Table 1:
Devices and cartridges used in this study
| ID | Endocutter | Cartridge reload | Anvil dimensionsa | Manufacturer |
|---|---|---|---|---|
| PVS | ECHELON FLEX™ powered vascular stapler with advanced placement tip (PVE35A) | ENDOPATH® ECHELON™ vascular white reload for advanced placement tip, four-row (VASECR35) | Width: 7.0 mm Perimeter: 19.1 mm |
Ethicon, Cincinnati, OH |
| ETS-6 | ENDOPATH® ETS 35-mm articulating linear cutter (ATW35) | ENDOPATH® ETS 35-mm reloads, white, six-row, vascular (TR35W) | Width: 8.3 mm Perimeter: 20.4 mm |
Ethicon |
| FLEX-6 | ECHELON FLEX™ powered articulating ENDOPATH® Stapler (PSE45A) | ENDOPATH® ECHELON™ White Reload, six-row (ECR45W) | Width: 9.4 mm Perimeter: 22.2 mm |
Ethicon |
| GIA-6 | Endo GIA™ ultra universal stapler (EGIAUSTND) | Tan Endo GIA™ articulating vascular/medium reload with Tri-Staple™ technology, six-row, (EGIA30CTAVM) Grey Endo GIA™ articulating vascular reload, six-row (EGIA30CTAV) |
Width: 9.5 mm Perimeter: 22.1 |
Covidien, Mansfield, MA |
aThe anvil perimeter is the perimeter of the cross-sectional area of the anvil.
PVS: powered vascular stapler.
Internal expert assessment
Haemostasis was evaluated after stapling applications in a porcine model via a visual 5-point Likert scale [1]. Briefly, the anchor points of the haemostasis scale can be described as follows: 1: no bleeding, 2: minimal bleeding, 3: mild bleeding, 4: moderate bleeding and 5: substantial bleeding. Blinding was not practical because of the differences in physical appearance of the devices and the resulting staple lines.
Paired firings were performed per the manufacturers' instruction for use for the test device (PVS) and predicate device (ETS-6) in gastroepiploic pedicle (n = 94 applications each). The gastroepiploic pedicle was selected based on an established ability to detect ‘relative’ differences in haemostasis between surgical staplers [1]. Statistical analysis used a modified ordered rank test, a non-parametric test in which the difference between devices was demonstrated to be less than an a priori clinically relevant difference (0.5 Likert units) with statistical confidence. The sample size was calculated based on historical values for similar haemostasis testing to provide sufficient power to show that the difference between devices was less than this predetermined value of 0.5 Likert units. Proportions were also calculated for the number of firings rated ‘1–3’ (no intervention needed) and the number of firings rated ‘4–5’ (intervention required) for each device. Fisher's exact test for two proportions was performed to compare the devices. The test device was also applied to uterine artery (n = 30), pulmonary artery and vein (n = 30) and renal artery (n = 17). These different vessels were examined to test haemostatic performance in variable vessel sizes and thicknesses which may be encountered during vessel transections for lung resection.
The gastroepiploic pedicle included vein, artery and associated fat. The uterine arteries were taken as a pedicle, with artery, vein and broad ligament, or as an isolated vessel. The pulmonary arteries and veins were taken as isolated vessels. The renal applications involved the artery, vein or pedicle. Uterine and renal artery/pedicles were considered thick-walled vascular applications, whereas pulmonary vessels and renal vein were considered thin-walled applications.
For gastroepiploic applications, a window was created at the perfusion midpoint and transected with an energy device. Dissection continued along the pedicle to free it from the stomach either towards the spleen or towards the pylorus for the first firing. A tissue thickness measurement was performed on the pedicle after the dissection from the stomach in preparation for the endocutter applications. Applications targeted vessels ≤2 mm thick.
For pulmonary applications, a 10-mm Bivona tube was inserted through a tracheotomy to selectively intubate the right lung. The left caudal lobe was used for application. In addition to the peripheral vessels in the caudal lung lobe, the pulmonary artery and the pulmonary vein at the base (hilum) of the lobes were used. Vessels at least 5 mm wide were targeted.
For uterine applications, the uterine artery pedicle was placed in the distal portion of the device jaws. Tissue thickness was measured and applications targeted vessels ≤2 mm thick. Because of the difficulty in dissecting and isolating an artery from the surrounding tissue, these isolated vessels were usually <5 mm wide, so uterine firings were generally performed as a pedicle. This has the potential to create a staple line with extraneous tissues; as a result, only the bleeding from the primary artery was rated.
For renal applications, the base of the kidney was exposed and the ureter was separated from the renal artery and vein. Depending on the vessel size, renal vessels were taken as isolated artery and isolated vein, or as a combined artery and vein pedicle. If isolating the vessels was not feasible, or if the isolated renal artery was less than 5 mm in diameter, the firing was performed on a pedicle.
Practising surgeon evaluation
The test system was PVS with white reload. The comparator control systems were GIA-6 with either Tan or Grey reloads, and FLEX-6 with white reloads.
Assessment of haemostasis was made by thoracic surgeons (n = 27) at four sites within the USA and one in Japan; the Center for the Future of Surgery at the UC San Diego School of Medicine; the Miller School of Medicine at the University of Miami; Translational Testing and Training Laboratories, Atlanta, GA; Houston Methodist Hospital; Kobe Medical Device Development Center (MEDDEC), Japan. All surgeons were required to have been in active practice for 2–25 years. Thoracic or cardiothoracic surgeons were required to normally conduct at least five surgical procedures per month, including lobectomy and pneumonectomy. More than 40% of procedures must have been performed via mini-thoracic surgery, video-assisted thoracic surgery (VATS) or robotic access.
Surgeons, blinded to the sponsor of the study, evaluated the endocutters during access, and after stapling and cutting vessels in a pulmonary lobectomy in an in vivo porcine model. This model was chosen because the anatomy of the pulmonary vessels is similar to that of humans, and the pig is a common model used for training in these procedures. However, the porcine thoracic cavity is smaller than a human thoracic cavity, so there would be less working space during VATS. To simulate the working space in a human VATS procedure, a simulated human rib cage (Fig. 2) was used in conjunction with the porcine model during the lobectomies.
Figure 2:

Rib cage model used for thoracic evaluation of stapler approach.
For VATS simulation of pulmonary lobectomy, the anaesthetized pig was placed in the right oblique recumbency, and skin, muscle and ribs were removed to provide unrestricted access to the thoracic cavity. The cranial–caudal access extended from midscapula to the diaphragm. The medial–lateral access extended from the longissimus muscle to short of the costal cartilage. The pig was selectively intubated to deflate the left lung and ventilate the right lung with a double-lumen tube. The apical pulmonary artery and superior vein and the inferior pulmonary vein were dissected to facilitate vessel identification. The simulated rib cage was placed over the pig's thoracic cavity and positioned to ∼6 inches above the heart. The model had a simulated scapula as a landmark for the surgeon and a replaceable simulated skin. Landmarks identified were the scapula, costal margin and the 4th–5th intercostal space. Access ports were created and the surgeon could add ports as necessary. Test and control articles were advanced through a constrained access port and visualized with an endoscope. Stapler firings were conducted on the identified pulmonary arteries and veins, or pedicle, i.e. a combination of vessels.
For all procedures, surgeons rated haemostasis for each firing as acceptable, acceptable with comments or unacceptable. If bleeding was present, the location (cut line or staple leg) was recorded. Surgeons evaluated access via Likert ratings on a 5-point scale (disagree strongly, disagree slightly, neutral, agree slightly, agree strongly) of the following four statements:
The four-row test device has easier placement on vessels compared with the six-row control devices.
The four-row test device has the potential to reduce the amount of dissection required around the vessel to place the stapler compared with the six-row control devices.
The four-row test device has the potential to reduce stress of surgeons during the most challenging step of the procedure, i.e. pulmonary artery/vein transection, compared with the six-row control devices.
The four-row test device enables precise control of end effector placement compared with the six-row control devices.
Statistical analysis of the haemostasis evaluation was performed by Fisher's exact test of the proportion of surgeons rating haemostasis as acceptable or acceptable with comments. The sample size was sufficient to detect a difference of 0.2 in the proportion of total acceptable haemostasis ratings with an 80% power. Likert ratings were evaluated by the Wilcoxon signed-rank test with the midpoint of the scale (neutral) centred as zero.
RESULTS
Internal expert assessment
In the gastroepiploic pedicle model, the median haemostasis scores were a ‘3 Mild’ for both the four-row PVS and the six-row predicate ETS-6 (Table 2). These medians were determined to be statistically equivalent by the modified ordered rank test at a P-value of less than 0.05. PVS had non-significantly fewer applications with a score of 4 or 5 (bleeding needing intervention) than the predicate ETS-6 applications.
Table 2:
Results of internal preclinical assessment of haemostasis via Likert scale
| Test location | PVS (four-row) | ETS-6 (six-row) | P-value |
|---|---|---|---|
| Gastroepiploic (n = 94) | |||
| Median | 3.0 | 3.0 | <0.001a |
| Mean ± SD | 2.6 ± 1.1 | 2.8 ± 1.0 | – |
| Score >3 | 17/94 (18%) | 20/94 (21%) | 0.714 |
| Uterine (n = 30) | |||
| Median | 1.0 | 1.0 | <0.001a |
| Mean ± SD | 1.1 ± 0.4 | 1.1 ± 0.4 | – |
| Pulmonary (n = 30) | |||
| Median | 1.0 | – | <0.001b |
| Mean ± SD | 1.3 ± 0.6 | – | |
| Renal veins (n = 16) | |||
| Median | 1.0 | – | <0.001b |
| Mean ± SD | 1.7 ± 1.1 | – | |
| Renal arteries (n = 17) | |||
| Median | 1.0 | – | <0.001b |
| Mean ± SD | 1.2 ± 0.5 | – | |
aA significant P-value implies that the difference between devices was less than 0.5 units.
bA significant P-value implies that the haemostasis was less than 3.0 units.
PVS: powered vascular stapler.
The median haemostasis score for the PVS applications in thin-walled vascular applications (pulmonary vessels and renal veins) was ‘1 None’, less than the median on the gastroepiploic tissue of ‘3 Mild’. The median haemostasis score for the PVS applications in thick-walled vascular applications (uterine vessels and renal arteries) was ‘1 None’, again less than the median on the gastroepiploic tissue of ‘3 Mild’.
Practising surgeons
The procedures were performed on 32 pigs weighing 34–75 kg. All surgeons were comfortable working through a constrained access port, except for one who converted to a thoracotomy with Finochietto retractor to complete the evaluation. Three surgeons either extended existing ports or created new ones. For the pulmonary lobectomy section of the study, a total of 30 firings were conducted on pulmonary artery, 52 on pulmonary vein and 24 on pulmonary pedicle, i.e. a combination of vessels.
There was no significant difference between the PVS test stapler and the GIA-6 control stapler with either the Tan (P = 0.341), Grey (P = 1.000) or combined (P = 0.486) cartridges for percentage of total acceptable haemostasis ratings (Table 3).
Table 3:
Ratings of acceptability of haemostasis by thoracic surgeons after stapler application
| Response | PVS (four-row) | GIA-6 Tan (six-row) | P-value vs PVS | GIA-6 Grey (six-row) | P-value vs PVS |
|---|---|---|---|---|---|
| Acceptable | 53/56 (94.6%) | 25/29 (86.2%) | 22/24 (91.7%) | ||
| Acceptable with comments | 3/56 (5.4%) | 3/29 (10.3%) | 2/24 (8.3%) | ||
| Total acceptable | 56/56 (100%) | 28/29 (96.6%) | 24/24 (100%) | ||
| Unacceptable | 0/56 (0%) | 1/29 (3.4%) | 0.341 | 0/24 (0%) | 1.000 |
PVS: powered vascular stapler.
All 43 surgeons had the opportunity to compare access with the PVS to the GIA-6 and Flex-6 staplers in a variety of vessels and approaches. For all four statements concerning access, surgeons significantly favoured the PVS stapler over the other two staplers (Table 4). The margin of difference was slightly greater for PVS versus Flex-6 than versus GIA-6.
Table 4:
Comparisons of access between the PVS and six-row GIA-6 and Flex-6 staplers by thoracic surgeons
| Comparative statement | Median PVS vs GIA-6 | P-value | Median PVS vs Flex-6 | P-value |
|---|---|---|---|---|
| Easier placement on vessels | +1.0 | 0.001 | +2.0 | <0.001 |
| Can reduce the amount of dissection required | +1.0 | 0.008 | +1.5 | <0.001 |
| Can reduce stress of surgeon during PA/PV transection | +1.0 | <0.001 | +2.0 | <0.001 |
| Enables precise control of end effector placement | +1.0 | <0.001 | +2.0 | <0.001 |
Positive values for the medians indicate that PVS was favoured over the six-row stapler for the associated statement, and a negative value would have indicated that the six-row stapler was favoured over PVS.
PVS: powered vascular stapler.
DISCUSSION
Lobectomy evolved from open thoracotomy to three-port VATS in 1994 and then to single-port VATS in 2012 [2]. Instrument crowding is a special concern for single-port procedures [3], leading to the development over the years of smaller, more manoeuvrable instruments [4, 5]. In the design of endocutters with improved vessel accessibility, what has been needed is a narrower anvil and shaft, a wider range of articulation and consistent firing power while maintaining equivalent haemostasis to current devices.
The PVS has a decreased shaft diameter of 9 mm, compared with a conventional endocutter with a 12 mm diameter, potentially allowing for easier insertion through the ribcage. This thinner shaft also permits a wider pivot between ribs and increased tip manoeuvrability which can minimize chest wall trauma that may be induced by a larger endocutter [6]. In addition, the end of the stapler can be articulated at settings of 17°, 34° and 50° for extended flexibility.
By changing the design from a conventional six rows to four rows, the anvil perimeter of the PVS is smaller by up to 14% than the other comparison staplers (Table 1). To compensate for the reduced number of rows, the space between rows has been laterally decreased, and longitudinally decreased between staples (Fig. 3). In addition, refinements in the design of the staple itself with wider staple crown, bent tips and tapered pockets all contribute to improved handling of thin tissue and haemostasis. As the current study shows, the new modifications allow reduction in rows without compromising haemostasis.
Figure 3:
Cartridge of the PVS showing decreased lateral spacing between rows and decreased longitudinal spacing between staples. PVS: powered vascular stapler.
Whether six rows of staples provide superior haemostasis to four rows of staples has been a matter of debate over several decades. For many studies, confounding factors, such as staple form, row layout and compression time have muddied the waters, making conclusions about the effect of the number of rows unclear. To combat bleeding and staple line failure, an early effort aimed at double application of four-row staplers [7]. This technique had a staple line failure rate of less than 1%, which was claimed to be lower than the historical rate for single application. However, no direct comparison to a single four-row application was made within this study.
In a study that included both four- and six-row staplers [8], prolonging the compression time prior to firing the stapler reduced the number of staple bleeding points. Use of a wait time of 1 min decreased the dry-to-wet weight ratio of the compressed tissue, resulting in less mucosal cutting. Six-row devices tended to have ‘more’ bleeding than four-row devices, perhaps, as suggested, because more mucosal cutting was occurring. However, there were also subtle design differences between the two staplers beyond the obvious difference in the number of rows. Another comparison of four- and six-row staplers in gastric bypass showed no difference in bleeding or leaks, but there was a lower rate of strictures with the six-row stapler [9]. This was not a randomized study; the use of the four-row stapler occurred earlier than that of the six-row stapler, so there is the chance that there were differences in design of the device or its application.
A comparison between a four-row stapler (Endopath TSB45) and a six-row stapler (Echelon 60) showed no significant difference in anastomotic bleeding rates, although haemostasis trended better for the six-row stapler (P = 0.074) [10]. This was not a pure comparison of differing number of rows, however, because there were also other differences in the design of the two staplers. Likewise, a new six-row 3D stapler provided less bleeding at the staple line than a four-row device of standard design [11], but again both the design and the number of rows had been altered between the two staplers.
In this study, we tested whether haemostasis of a four-row stapler with a novel staggered design was equivalent to six-row staplers. For the in vivo testing, the control of haemostasis could have been measured either by objective methods, e.g. gravimetrically, or via subjective assessment, as was done here. Although objective methods can provide quantitative results, we chose to use the surgeon's evaluation as it has previously been demonstrated that this method more closely models what occurs during actual clinical practice [1]. A limitation of the present study, and of most medical device studies, is that the evaluators could not be completely blinded to the particular brand of device that was used. Given their level of experience, many of the surgeons may have recognized the devices. However, the surgeons were blinded to the sponsor by the use of an independent study agency, and so were not susceptible to the direct influence of a particular manufacturer.
There was no clinically significant difference in haemostasis between the PVS and the other tested devices, either by expert grading assessment or grading by practising surgeons. In addition, the surgeons rated the smaller PVS as having easier device placement on vessels, the potential to reduce the amount of dissection required around the vessel to place the stapler, the potential to reduce stress of surgeon during the most challenging step of the procedure, i.e. pulmonary artery/vein transection, and superiority in terms of precisely controlling the placement of the end effector.
The PVS provides several other benefits to the minimally invasive surgeon by potentially allowing for the removal of one port, depending on technique, during a VATS lobectomy, due to thinner shaft and higher degree of articulation. With one reload designed to cover a tissue range from 0.75 to 1.5 mm, the number of products required and concomitant logistical demands may be reduced. When the compressed vessel is behind the indicated cut line, there may be a reduction in incomplete transections. In addition to the smaller overall size, the use of a powered handle substantially reduces the movement of the distal tip during transection of the carotid arteries compared with manual devices, reducing device-tissue interaction [12].
In conclusion, the four-row PVS provides equivalent haemostasis to predicate six-row staplers, while its more compact design provides easy, more precise access for vascular tissue stapling during minimally invasive procedures such as VATS lobectomy.
Funding
This work was supported by Ethicon, Inc., manufacturer of the Echelon Flex powered vascular stapler. Funding to pay the Open Access publication charges for this article was provided by Ethicon, Inc.
Conflict of interest: Calvin S. H. Ng and Allan Pickens are compensated consultants for Ethicon, Inc. Julianne M. Siegel, John F. Cummings and Jeffrey W. Clymer are employees of Ethicon, Inc.
REFERENCES
- 1.Siegel JM, Cummings JF, Clymer JW. Reproducible, repeatable and clinically-relevant hemostasis scoring. J Adv Med Pharm Sci 2014;1:30–9. [Google Scholar]
- 2.Ng CS, Lau KK, Gonzalez-Rivas D, Rocco G. Evolution in surgical approach and techniques for lung cancer. Thorax 2013;68:681. [DOI] [PubMed] [Google Scholar]
- 3.Ng CS, Kim HK, Wong RH, Yim AP, Mok TS, Choi YH. Single-port video-assisted thoracoscopic major lung resections: experience with 150 consecutive cases. Thorac Cardiovasc Surg 2015; doi:10.1055/s-0034-1396789. [DOI] [PubMed] [Google Scholar]
- 4.Ng CS, Rocco G, Wong RH, Lau RW, Yu SC, Yim AP. Uniportal and single-incision video-assisted thoracic surgery: the state of the art. Interact CardioVasc Thorac Surg 2014;19:661–6. [DOI] [PubMed] [Google Scholar]
- 5.Ng CS, Wong RH, Lau RW, Yim AP. Single port video-assisted thoracic surgery: advancing scope technology. Eur J Cardiothorac Surg 2015;47:751. [DOI] [PubMed] [Google Scholar]
- 6.Ng CS, Wong RH, Lau RW, Yim AP. Minimizing chest wall trauma in single-port video-assisted thoracic surgery. J Thorac Cardiovasc Surg 2014;147:1095–6. [DOI] [PubMed] [Google Scholar]
- 7.Jones KB, Homza W, Peavy PW, Williams LH, Leopard PB, Mastrodomineco L et al. Double application of TA-90 four-row AutoSuture(c) stapling instrument: a safe, effective method of staple-line production indicated by follow-up GI series. Obes Surg 1996;6:494–9. [DOI] [PubMed] [Google Scholar]
- 8.Morita K, Maeda N, Kawaoka T, Hiraki S, Kudo A, Fukuda S et al. Effects of the time interval between clamping and linear stapling for resection of porcine small intestine. Surg Endosc 2008;22:750–6. [DOI] [PubMed] [Google Scholar]
- 9.Szomstein S, Whipple OC, Zundel N, Cal P, Rosenthal R. Laparoscopic Roux-en-Y gastric bypass with linear cutter technique: comparison of four-row versus six-row cartridge in creation of anastomosis. Surg Obes Relat Dis 2006;2:431–4. [DOI] [PubMed] [Google Scholar]
- 10.Czymek R, Keller R, Hildebrand P, Bouchard R, Bader FG, Jungbluth T et al. Does the third staple line of a new endostapler offer an advantage? Zentralbl Chir 2009;134:254–9. [DOI] [PubMed] [Google Scholar]
- 11.Sozutek A, Colak T, Dag A, Olmez T. Comparison of standard 4-row versus 6-row 3-D linear cutter stapler in creation of gastrointestinal system anastomoses: a prospective randomized trial. Clinics (Sao Paulo) 2012;67:1035–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chekan E, Whelan RL. Surgical stapling device–tissue interactions: what surgeons need to know to improve patient outcomes. Med Devices (Auckl) 2014;7:305–18. [DOI] [PMC free article] [PubMed] [Google Scholar]



