Significance
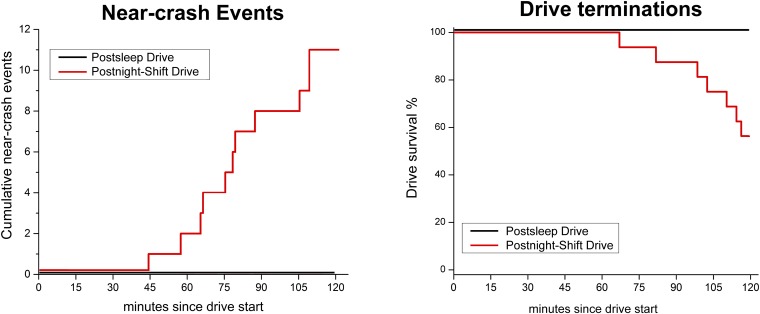
Drowsy driving is a major public health issue, particularly impacting the 9.5 million shift workers in America. Previous reports have assessed the impact of night work on driving in driving simulators. This real-vehicle driving study demonstrated increased objective and subjective drowsiness and degraded daytime driving performance in 16 night-shift workers while driving after a night of work, deteriorating with drive duration. No near-crashes occurred during driving after a night of sleep; 11 occurred during driving after night-work; all near-crashes occurred after at least 45 min of driving. Policy makers and night-workers should consider avoiding/minimizing driving or deploying effective countermeasures when driving after night-shift work to reduce drowsy driving and preventable crashes and injuries in this high-risk population.
Keywords: drowsy driving, sleep, EEG, infrared oculography, fatigue
Abstract
Night-shift workers are at high risk of drowsiness-related motor vehicle crashes as a result of circadian disruption and sleep restriction. However, the impact of actual night-shift work on measures of drowsiness and driving performance while operating a real motor vehicle remains unknown. Sixteen night-shift workers completed two 2-h daytime driving sessions on a closed driving track at the Liberty Mutual Research Institute for Safety: (i) a postsleep baseline driving session after an average of 7.6 ± 2.4 h sleep the previous night with no night-shift work, and (ii) a postnight-shift driving session following night-shift work. Physiological measures of drowsiness were collected, including infrared reflectance oculography, electroencephalography, and electrooculography. Driving performance measures included lane excursions, near-crash events, and drives terminated because of failure to maintain control of the vehicle. Eleven near-crashes occurred in 6 of 16 postnight-shift drives (37.5%), and 7 of 16 postnight-shift drives (43.8%) were terminated early for safety reasons, compared with zero near-crashes or early drive terminations during 16 postsleep drives (Fishers exact: P = 0.0088 and P = 0.0034, respectively). Participants had a significantly higher rate of lane excursions, average Johns Drowsiness Scale, blink duration, and number of slow eye movements during postnight-shift drives compared with postsleep drives (3.09/min vs. 1.49/min; 1.71 vs. 0.97; 125 ms vs. 100 ms; 35.8 vs. 19.1; respectively, P < 0.05 for all). Night-shift work increases driver drowsiness, degrading driving performance and increasing the risk of near-crash drive events. With more than 9.5 million Americans working overnight or rotating shifts and one-third of United States commutes exceeding 30 min, these results have implications for traffic and occupational safety.
Between 2009 and 2013 in the United States, a drowsy driver was involved in an estimated 21% of fatal crashes and 13% of crashes causing severe injury, consistent with earlier estimates that drowsy driving causes 20% of serious motor vehicle crash injuries resulting in hospitalization or death, and is associated with a four- to sixfold increase in crash/near-crash risk (1–4). These data indicate that drowsiness is likely one of the most prevalent causes of preventable road crashes worldwide (5). Most drivers admit to driving while drowsy, with 28% reporting falling asleep while driving within the past year (6). The nation’s 9.5 million shift workers, comprising 15% of the workforce (7), are at particular risk of drowsy driving (8). Night-shift work increases the risk for drowsy driving crashes, especially on the morning commute home from overnight work (9–11), when elevated homeostatic sleep pressure interacts with the peak of circadian sleep propensity to create a critical zone of performance vulnerability (10–12).
Despite the high prevalence of drowsy driving and sleep-related crashes, little is known about the characteristics of driver impairment preceding or during a drowsiness-related critical driving event. Increased weaving in the lane and episodes of lane crossing occur during prolonged nocturnal driving, similar to behaviors observed in drivers with elevated blood alcohol concentrations (13). Small steering corrections are reduced in drowsy drivers, who make infrequent large steering corrections (14). Physiological signs of drowsiness identified during night-time driving include brief sleep episodes and partial eyelid closure with slow eye movements (15). However, few studies have related these physiological changes to behavioral signs of impaired driving. After a night shift, increased out-of-lane events, subjective sleepiness, and blink duration are evident during simulated driving (16, 17).
Drowsiness and crash risk also increase with drive duration (13, 18–23). During simulated driving, sleep-deprived drivers show increased subjective sleepiness, reaction time, and improper lane crossings with increasing drive duration (18). Corrective steering wheel movements (22) and variation in car speed and lateral position (23) deteriorate over time, with severe driving impairment during nighttime highway driving after 2 h (13). Although few studies have evaluated the impact of drive duration on physiological indices of drowsiness, ocular measures of drowsiness appear to increase during the latter part of the commute home after the night shift (21). As such, the effects of circadian disruption and sleep restriction exhibited in night-shift workers are likely to be exacerbated as the homeward commute becomes prolonged.
The goals of this study were to test the hypotheses that night-shift work results in increased objective and subjective drowsiness and impaired driving performance, and that drive duration increases the risk of these events. To test these hypotheses, actual night-shift workers (Table 1) were recruited to undertake a 2-h drive in an instrumented vehicle on a closed test track following the night shift. The same drivers also completed a separate driving session following their usual nocturnal sleep episode.
Table 1.
Demographic and anthropometric summary (n = 16)
| Variable | Mean (SD) | Range |
| Age (y) | 48.7 (14.8) | 19–65 |
| Driving experience (y) | 27.4 (16.5) | 3–50 |
| Weight (lbs) | 184.3 (32.0) | 151–245 |
| Height (inches) | 62.9 (17.2) | 61–76 |
| Body mass index | 29.1 (6.0) | 19.2–40.7 |
| Chronotype | Morning type (n = 2) | |
| Intermediate type (n = 11) | ||
| Evening type (n = 2) | ||
| Risk of sleep apnea | 5 of 16 |
Results
Participants in the postsleep condition reported obtaining an average (±SD) of 7.6 ± 2.4 h of sleep during the previous night (range: 5–12 h). Participants in the postnight-shift condition reported obtaining an average (±SD) of 0.4 ± 1.1 h of sleep between the start of their overnight shift and the start of their postnight-shift drive (range: 0–4.3 h); in three cases this sleep occurred during the night shift, whereas in one case it occurred between the end of the night shift and the start of the postnight-shift drive. During the overnight shift before the postnight-shift drive, participants worked an average duration of 8.3 ± 4.1 h (range: 5–20.5 h), with at least 5 of those hours occurring between 10:00 PM and 8:00 AM. On average, the postsleep and the postnight-shift drives occurred at approximately the same time of day for each participant, with the average difference in the time of day at which each participant’s postsleep and postnight-shift drives started being 1.0 ± 1.2 h (range: 0.1–5 h). Before the start of the postsleep-drive session, participants had been awake for an average of 5.0 ± 1.7 h (range: 3.4–7.5 h) since their last sleep episode. Before the start of the postnight-shift drive, participants had been awake for an average of 12.8 ± 4.8 h (range: 3.3–18.9 h) since their last sleep episode. There was no significant effect of condition order as measured by lane crossings in either the postsleep condition (P = 0.58) or the postnight-shift condition (P = 0.68).
Driving Events.
Over one-third of postnight-shift drives (37.5%) required a safety observer to initiate emergency braking maneuvers in response to a near-crash event to ensure the safety of the participant and study staff, compared with none of the postsleep drives (Fisher’s exact test: P = 0.0088) (Table 2). A total of 11 emergency braking maneuvers were executed in response to a near-crash event during postnight-shift driving sessions compared with zero during postsleep driving sessions (Fig. 1, Left). Seven of the 16 postnight-shift drives (43.8%) were terminated prematurely because of failure to maintain adequate control of the vehicle (six identified by the investigator, one identified by the participant), compared with none of the postsleep drives (log-rank test: P = 0.00308) (Fig. 1, Right) (Fisher’s exact test: P = 0.0034) (Table 2). Among these 16 participants, all of the emergency brake maneuvers, near-crash events, and drive terminations occurred 45 min or more after the start of the postnight-shift drive (Fig. 1), although objective measures of driving performance impairment and drowsiness were evident during the first 15 min of driving (Fig. 2).
Table 2.
Comparison of driving performance, EEG and ocular measures on postnight-shift drives compared with postsleep drives
| Variable | Postnight-shift (n = 16) | Postsleep (n = 16) | P value |
| Driving performance | |||
| Drives with emergency brake maneuvers | 6 (37.5%)* | 0 (0%) | P = 0.0088 |
| Drive terminations | 7 (43.8%) | 0 (0%) | P = 0.0034 |
| Rate of lane excursions (overall) | 3.09/min | 1.49/min | P < 0.0001 rate ratio = 2.08 (95% CI:1.98, 2.19) |
| Rate of lane excursions (straight) | 0.59/min | 0.19/min | P < 0.0001 rate ratio = 3.11 (95% CI:2.72, 3.55) |
| EEG | |||
| Microsleep episodes | 1.00/h | 0.47/h | P = 0.0368 rate ratio = 2.09 (95% CI: 1.05, 4.18) |
| Ocular measures | |||
| Slow eye movements | 20.1/h | 10.6/hour | P < 0.0001 rate ratio = 1.89 (95% CI: 1.63, 2.19) |
| IED, mean (SD) (s) | 0.12 (0.04) | 0.10 (0.02) | P = 0.0192† |
| Time with eyes closed, mean (SD) (%) | 0.36 (0.13) | 0.32 (0.12) | P = 0.21‡ |
| Blink time duration, mean (SD) (s) | 0.18 (0.10) | 0.13 (0.07) | P = 0.18‡ |
| Positive AVR, mean (SD) | 0.50 (0.32) | 0.36 (21) | P = 0.0684† |
| JDS, mean (SD) | 1.71 (1.32) | 0.97 (0.90) | P = 0.0209† |
| Average maximum JDS, mean (SD) | 3.77 (1.77) | 2.80 (1.49) | P = 0.0658† |
Within these six sessions, there were a total of 11 braking maneuvers.
Student’s t-test.
Signed test.
Fig. 1.
Near-crash driving events and drive terminations occurred only in postnight-shift drives. (Left) Cumulative histogram of 11 near-crash driving events across time since drives began in each condition. (Right) Kaplan–Meier survival curve of the seven drive terminations since drives began in each condition (P = 0.00308). None of the drivers in the postsleep driving sessions had a near-crash driving event or drive termination, whereas 6 of the 16 participants had a near-crash driving event and 7 of the 16 participants had the drive terminated in the postnight-shift driving sessions (P = 0.0088 and P = 0.0034, respectively). Tick marks on both panels indicate driving breaks that occurred every 15 min to complete sleepiness assessment surveys.
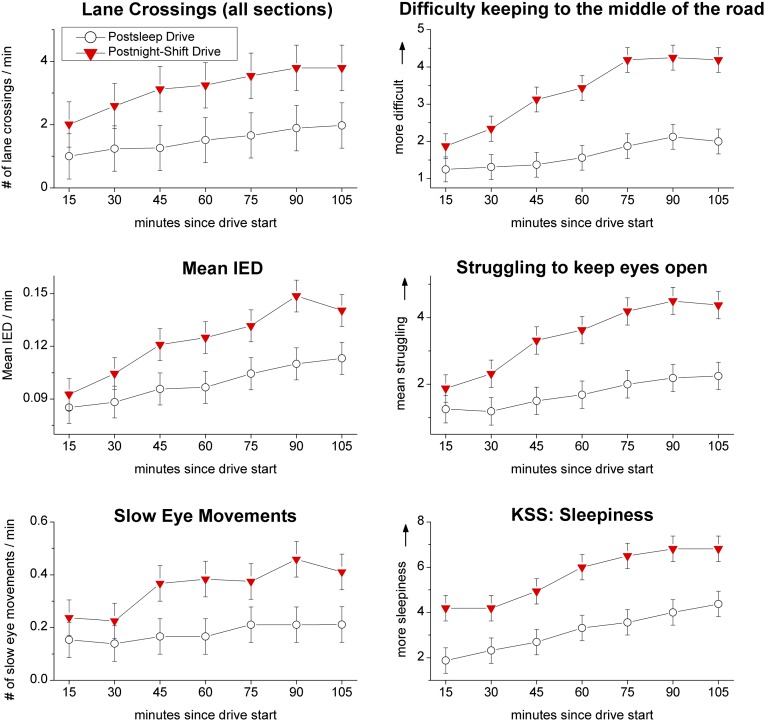
Fig. 2.
Drowsiness progressively increased across driving sessions. Driving performance, ocular, and survey measures of drowsiness are shown by drive condition and drive duration. Mean values with SE bars. For each of these variables except the KSS, there was a significant interaction effect of driving duration (driving block 1–7) by condition (P < 0.05). Condition alone had a significant effect on the KSS (P < 0.05). Tick marks indicate driving breaks, as in Fig. 1.
Lane excursions, slow eye movement intrusions, and microsleep episodes were significantly more frequent during the postnight-shift drives than during the postsleep drives (Table 2). Ocular measures of drowsiness [interevent duration (IED) and John’s Drowsiness Scale (JDS) (24)] were significantly higher on postnight-shift drives compared with postsleep drives. Percent of time with eyes closed and blink time duration did not show a significant difference, whereas the differences in condition for positive amplitude-velocity ratio (AVR) and average maximum JDS showed trends that were not quite statistically significant.
Time on Task.
Evidence of impairment of objective measures of driving performance and drowsiness during the postnight-shift drives compared with the postsleep drives was apparent within the first 15 min of driving (Fig. 2). The risk of microsleep episodes (>3 s of any stage of sleep) across all drives increased after driving for >30 min (Student’s t test, P = 0.04), increasing from 0.13 to 1.31 episodes of microsleep episodes per hour. Frequency of slow eye movements and lane-crossing events increased as a function of driving duration (z = 8.41, P < 0.001) and a condition by driving block (15-min segment) (see Materials and Methods) interaction was observed (z = 4.07, P < 0.001) (Fig. 2); however, driving condition did not have a significant effect with the interaction term included (z = −1.69, P = 0.091). Similar effects were evident for ocular measures of drowsiness: IED, JDS, blink time duration, and positive AVR all significantly increased across the driving block (z = 10.41, 9.91, 6.60, and 8.28, respectively; P < 0.001 for all) and condition by driving block interaction (z = −5.01, −4.26, −4.48, and −4.57, respectively; P < 0.001 for all), showing a time-on-task effect that impacts postnight-shift drives greater than postsleep drives. Subjective sleepiness (Karolinska Sleepiness Scale, KSS) increased in the postnight-shift drive (z = −3.34, P = 0.001) and by driving block (z = 5.45, P < 0.001), but there was no significant interaction effect. However, subjective indices of drowsiness increased with driving block and there was an interaction effect of condition and driving block (”struggling to keep eyes open”: z = 7.45 and −4.27, respectively; “difficulty keeping to the middle of the road”: z = 8.13 and −4.97, respectively; P < 0.001 for all) (Fig. 2).
Discussion
We found a high risk of dangerous driving and near-crash events during actual driving by night-shift workers following overnight work, when physiological markers of drowsiness were significantly increased. Our data indicate that prolonged driving may be especially hazardous during the homeward commute following night-shift work. During daytime driving following the night shift, drivers were more likely to experience lane excursions. Importantly, all of the emergency near crashes (when safety observers intervened to stop the vehicle) and drive terminations that occurred in this study did so during the postnight-shift drive; none occurred during the postsleep drive. Nearly 40% of the postnight-shift daytime drives required the execution of emergency braking maneuvers for near-crash driving events (versus 0% in the postsleep condition), consistent with a prior study comparing day and night driving, in which 44% of night drives were terminated because of excessive sleepiness by an expert driving instructor compared with none of the day drives (25). These data are also consistent with laboratory simulation of driving performance, which is significantly worse after night work than after a night of sleep, with reduced time to first accident and increased lane excursions, eye closure duration, and subjective sleepiness (16). Our data reveal that actual daytime motor vehicle driving is profoundly degraded by drowsiness related to the sleep deprivation and circadian misalignment associated with night-shift work.
Workers driving home after night-shift report increased subjective sleepiness and more hazardous driving events, including crashes (11, 21). Increased objective measures of drowsiness, including blink duration and percent of time with eyes closed, have also been reported during the postnight-shift commute (21). Our results extend these previous findings, to our knowledge demonstrating for the first time a substantially increased risk of objectively measured drowsiness, impaired driving performance, and critical driving incidents when driving during the daytime following a night shift in actual night-shift workers. We found that drivers frequently exhibited indicators of drowsiness while driving following night shift that became worse as the drive progressed. Increases in blink duration, the frequency of slow eye movements/attentional failures that herald the transition from wakefulness to sleep (26–29), and the occurrence of microsleep episodes indicate that drivers were much more drowsy when driving after the night shift than when driving after a night of sleep, consistent with laboratory data (30). We found that postnight-shift drivers were much sleepier, and noticed increasing difficulty keeping their eyes open and maintaining lane position, particularly when driving for more than 15–30 min, which has been related to slowing on EEG (increased θ power), lane drifting and severe driving impairment during simulated driving, and increased crash risk (2, 31–33). Our findings on the controlled driving track were comparable to a study of nurses driving home after night shift, which showed that the maximum total blink duration was increased after the night shift and was associated with a greater incidence of subjective sleep-related events, such as “resting your eyes,” or “falling asleep at the stop light” (21). Although objective measures of drowsiness have been measured in simulated and real-world driving, the present study uniquely demonstrated an increase in objective EEG and ocular drowsiness measures in parallel with objectively impaired driving performance and safety critical driving events in a real-world vehicle. Driving duration interacts with other factors that cause drowsiness, with crash risk increasing with hours driven (34), although individual crash reports reveal that there is no safe driving duration for drivers with drowsiness-related impairment (35).
In the present study, drivers had increasing drowsiness over the course of the driving session. This time-on-task effect appeared to interact with night-shift work, given the rates of deterioration in driving performance; both ocular and subjective measures of drowsiness were significantly higher following a night of shift work. A time-on-task effect on subjective and objective measures has been reported during prolonged night driving in real-world and driving simulators (16, 18). In our study, both subjective reports and objective indices of drowsiness became prominent within the first 15–30 min of driving, with a marked increase in the rate of slow eye movements and ocular measures of drowsiness after 30 min. All of the critical driving events that we recorded in this group of 16 participants occurred after 45 min, suggesting that driving for more than 45 min after a night shift is likely to increase the risk of drowsiness-related impairment greatly. This accelerated deterioration after night shift was paralleled in most of the driver’s subjective measures of impairment.
The present study had several limitations. The driving sessions were conducted following a night of sleep or a night of shift work to recreate conditions commonly experienced by night-shift workers, including prolonged wakefulness. Although the study controlled for the time of the driving sessions to avoid confounding from time-of-day effects, the length of time awake differed between the two conditions. The driving session was interrupted approximately every 15 min for a short break to administer surveys, which may have a brief alerting effect (36). Drivers would not typically experience such frequent breaks in a real-world commute. Nevertheless, drivers had increasing drowsiness and impaired driving performance despite these breaks. Additionally, the driving session was carried out on a closed track with a relatively simple geometry, no navigation requirement and the absence of a rumble strip, vehicle traffic, or pedestrian traffic. It is possible that in a real-world commute, rumble strips, vehicle traffic, and pedestrian traffic would serve to increase driver attention and alertness. On the other hand, the presence of the study team in the vehicle and their continuous monitoring of alertness, performance, the electroencephalogram via EEG electrodes and infrared oculography through specially fitted glasses, and the breaks scheduled every 15 min to assess sleepiness may have increased driver attention, alertness, and awareness of sleepiness, compared with that of a worker driving home alone and without observation after the night shift. Nonetheless, our findings are consistent with field research demonstrating that drowsiness following night-shift work in real-world driving situations increases risk of vehicle crashes (8, 11). As previous studies have shown task-specific local changes in the EEG during prolonged wakefulness (37), future studies are needed to expand on these findings by monitoring electrical brain activity using high-density EEG to assess the impact of night-shift work on specific brain regions.
Driving following night-shift work puts drivers as well as other road users at elevated risk of motor vehicle crashes. The results from the present study, using actual night-shift workers and carried out in an instrumented vehicle, demonstrate the contribution of sleep-related impairment of neurobehavioral function to the increased crash risk found in drivers commuting home after overnight work (11) and contribute new and compelling evidence of these risks. The abundance of emergency braking maneuvers required to avoid crashes for drivers in the postnight-shift condition highlights the safety hazards in this vulnerable group, with impairment becoming severe after 45 min. Importantly, deficits in driving performance outcomes (lane crossings) and physiological measures indicative of drowsiness were also evident from the outset of the drive, indicating that impairment among these night-shift workers occurred within the first 15 min of postnight-shift driving. These data therefore indicate that even night-shift workers with a relatively brief commute are vulnerable to fatigue-related driving incidents. Such measurements may provide the basis for real-time, in-vehicle technological countermeasures to reduce the risk of drowsy driving and near-crash events. These results have important implications for public policy and road safety (38). The average commute time in the United States is 25 min each way, with 15% of United States workers commuting more than 45 min each way (39). Because our results indicate that the risk of sleep-related near-crash incidents increases steeply with drive duration, night-shift workers should be advised to limit their drive duration or seek alternate forms of transportation after night-shift work. Given that drivers were aware of drowsiness and indicators of impaired performance, education about the hazards of driving after night-shift work and the need to heed the warning signs of increased drowsiness could help prompt drivers to minimize driving after night work and to stop driving when their performance is impaired by drowsiness.
Materials and Methods
Participant Screening and Recruitment.
Sixteen night-shift workers (nine women and seven men) between the ages of 18 and 65 y (Table 1), who worked regular night shifts [at least 5 continuous hours between 10:00 PM and 8:00 AM (mean = 3.1 nights per week)], held a valid United States or International driver’s license for a minimum of 2 y, and reported normal or corrected-to-normal visual acuity participated in a cross-over driving study that was approved by the Partners Human Research Committee and conducted between July and December of 2011. The study obtained ethics approval from the Brigham and Women’s Institutional Review Board #2011P000370. Participants provided written informed consent and were compensated. Participants completed the Horne-Östberg Morningness-Eveningness questionnaire to assess chronotype (40) and the Berlin questionnaire to assess risk of sleep apnea (41).
Protocol.
Participants completed two 2-h driving sessions in an instrumented vehicle on a closed driving track in each of two conditions: one following a night of at least 5 h of sleep, before which participants had not worked a night shift (5 h or more of work between the hours of 10:00 PM and 8:00 AM) for 30 continuous hours before the driving session and had at least two sleep episodes during that interval (postsleep drive), and one following night-shift work, before which participants had worked an overnight shift with at least 5 continuous hours of work occurring between 10:00 PM and 8:00 AM (postnight-shift drive). Participants in the postnight-shift driving condition were instructed not to sleep between the end of the prior night shift and the start of the drive. Driving order was determined by participant’s work schedule; 4 participants first completed the postsleep drive followed by postnight-shift drive, 12 participants first completed the postnight-shift drive followed by postsleep drive. Post hoc analysis did not reveal a significant effect of drive order on driving performance outcomes. Lane crossings for each driving condition were stratified by driving order and compared using Student’s t-test. Sleep and wake times, medication use, and caffeine intake were recorded via diary and wrist activity monitor for the week before each driving session (Actiwatch-L; Mini Mitter). Participants were provided transportation to and from the test facility and monitored en route to ensure they remained awake during transport and did not consume caffeine for at least 2 h before the drive. The drive sessions began between 9:30 AM and 2:30 PM. Each participant’s postsleep and postnight-shift drives were time-matched to control for potential time-of-day effects. Participants completed a brief self-reported sleepiness survey before starting the drive and during short 1- to 2-min breaks scheduled every 15 min.
Electroencephalography and electrooculography.
Continuous EEG and electrooculography (EOG) recordings were made using the Vitaport 4 system (Temec). EEG electrodes were fixed to the participant’s scalp in the frontal, parietal, central, and occipital positions (Fz, Cz, Pz, Oz, referenced to the contralateral mastoid process). EOG electrodes were placed 2 cm above and lateral to the right eye and 2 cm below and lateral to the left eye. EEG/EOG parameters for assessment are detailed in Table S1.
Infrared reflectance oculography.
Eye blink measures were quantified by monitoring eyelid movements via infrared reflectance oculography (Optalert) using a small infrared transducer mounted on an open-lens glasses frame that emits and detects infrared light (IR-A band: 760–1,400 nm) (Table S1).
Indices of driving performance.
Driving sessions were conducted on a 0.8-km closed-loop continuous-driving track with both curved and straight sections of road surrounded by a safety guard rail. A 2002 Ford Windstar minivan (Ford Motor Company) was equipped with a passenger brake and instrumented with multiple sensors and computers that collected driving performance data at 30 Hz. After a practice lap to orient participants with the instrumented vehicle, participants began a 2-h driving session. Drivers were instructed not to drive at excessive speeds and to keep the vehicle positioned in the center of the lane. A safety observer (W.J.H. or Y.L.) in the front passenger seat, blind to condition, monitored driving performance, recording lane crossings. The safety observer initiated emergency braking maneuvers if the participant entered a near-crash situation to ensure the safety of the participant and study staff. Driving parameters for assessment are detailed in Table S1.
Self-reported sleepiness.
Participants completed the Karolinska Sleepiness Scale (9) and sleepiness symptoms questionnaire (31, 42) before starting the drive and every 15 min thereafter.
Driving sessions were carried out under clear or overcast daytime weather conditions. One session was terminated 30 min early because of inclement weather.
Statistical Analysis.
We examined the impact of condition and drive duration on driving performance, subjective sleepiness, and physiological measures of drowsiness in a two-drive condition (postsleep; postnight-shift) by duration [seven-driving blocks (15-min segments), ordered 1 through 7] analysis. Table S2 contains all of the de-identified data from individual participants during the postsleep and postnight-shift drives that were used to construct the tables and figures in this manuscript.
Missing data.
Some sessions were terminated prematurely, resulting in missing data that were not random, as early termination was usually because of poor vehicle control, yielding a potential survivor effect. Missing data were thus accounted for by using the last value carried forward technique (i.e., data for an absent 15-min driving block was replaced using data from the preceding 15-min driving block for that participant). Using this technique resulted in the conservation of 11 driving blocks, ∼4% of the total 256 driving blocks.
Condition analysis.
A contingency table analysis using a Fisher’s exact test was used to examine the effect of night-shift work on emergency brake maneuvers and drive terminations. In addition, drive terminations were analyzed using a log-rank test to compare Kaplan–Meier survival probability for each driving condition. Log-linked Poisson model rate ratios and 95% confidence intervals (CI) were calculated to examine the effect of condition on rates of lane excursions, microsleep episodes, and SEM intrusions.
Time on task analysis.
Linear mixed models were used to examine the fixed effects of condition (postsleep and postnight shift), time on task (driving block), and their interaction on driving performance, subjective sleepiness, and physiological measures of drowsiness, with the participant as a random intercept assumed to be constant, fitted using restricted maximum-likelihood, and using an autoregressive covariance structure to adjust for serial correlation across time (xtmixed; STATA software, v11; StataCorp).
Supplementary Material
Acknowledgments
We thank the participants for taking part in the study. The authors acknowledge the contributions of Joseph Ronda for his technical expertise, Brandon Lockyer for scoring of the EEG and EOG data, Ms. Lorna Preston for editorial assistance, and Dr. Murray Johns for his advice concerning use of the Optalert. The authors also acknowledge Marvin Dainoff, Mary Lesch, and Vincent Ciriello for their comments and review of the project proposal and/or this manuscript. This study was supported by a grant from the Institute of Breathing and Sleep Research (to M.E.H.); by Liberty Mutual Insurance; National Institutes of Health Award 5T32HL7901-14 (to M.L.L.); National Space Biomedical Research Institute Award PF03002 (to M.L.L.); Department of Homeland Security Federal Emergency Management Agency Assistance to Firefighter Grant EMW-2010-FP-00521 (to C.A.C.); National Heart, Lung and Blood Institute Cooperative Agreement U01-HL111478 (to C.A.C.); National Institute of Occupational Safety and Health Grant R01-OH0103001 (to C.A.C.); National Institute on Aging Grant R01-AG044416 (to C.A.C.); and an endowed professorship provided to Harvard Medical School by Cephalon, Inc. (to C.A.C.). The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the Federal Emergency Management Agency, Assistance to Firefighters Grant Program, National Institutes of Health, National Space Biomedical Research Institute, Institute of Breathing and Sleep, or Liberty Mutual Insurance Company. The federal sponsors did not have a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Conflict of interest statement: C.A.C. has received consulting fees from or served as a paid member of scientific advisory boards for: Amazon.com, Inc.; A2Z Development Center, Inc.; Bose Corporation; Boston Red Sox; Cleveland Browns; Institute of Digital Media and Child Development; Jazz Pharmaceuticals, Inc.; Merck Sharpe and Dohme; Purdue Pharma; Quest Diagnostics; Samsung Electronics; Teva Pharmaceutical Industries Ltd.; Koninklijke Philips Electronics, N.V.; Novartis; and Vanda Pharmaceuticals, Inc. C.A.C. owns an equity interest in Somnus Therapeutics, Inc. and Vanda Pharmaceuticals, Inc., and has received research/education support from Mary Ann and Stanley Snider through Combined Jewish Philanthropies, National Football League Charities, Optum, ResMed, Philips Respironics, the San Francisco Bar Pilots, Simmons, Schneider, Inc., and Sysco. C.A.C. has received royalties from McGraw Hill, Penguin Press/Houghton Mifflin Harcourt, and from Philips Respironics, Inc., for the Actiwatch 2 and Actiwatch Spectrum devices; C.A.C.’s interests were reviewed and are managed by Brigham & Women’s Hospital and Partners HealthCare in accordance with their conflict of interest policies. The Harvard Medical School Division of Sleep Medicine and the Brigham and Women's Hospital Division of Sleep and Circadian Disorders, which C.A.C. directs, have received unrestricted research and educational gifts and endowment funds from: Boehringer Ingelheim Pharmaceuticals, Inc.; Cephalon, Inc.; GlaxoSmithKline; Jazz Pharmaceuticals; Merck & Co., Inc.; Pfizer; ResMed; Philips Respironics, Inc.; Sanofi-Aventis, Inc.; Sealy, Inc.; Sepracor, Inc.; Simmons, Spring Aire; Takeda Pharmaceuticals; Tempur-Pedic; Walmart; Proctor and Gamble; Optum; Bose; Vanda Pharmaceuticals, Inc.; and have received Educational Grant funding from Apria Healthcare; Cephalon, Inc.; Jazz Pharmaceuticals; Philips Respironics; Takeda Pharmaceuticals; ResMed Foundation; Sanofi-Aventis, Inc.; Sepracor, Inc.; Teva Pharmaceutical Industries, Ltd.; and Wake Up Narcolepsy. C.A.C. holds a number of process patents in the field of sleep/circadian rhythms (e.g., photic resetting of the human circadian pacemaker). Since 1985, C.A.C. has also served as an expert witness on various legal cases related to sleep and circadian rhythms, including matters related to Bombardier, Citgo, HG Energy, Michael Jackson’s mother and children, Purdue Pharma, Stric Lan LLC, Valero, and matters related to commercial drivers employed by Celadon, Crete Carrier Corporation, FedEx, United Parcel Service, and other commercial carriers. M.E.H. reports grants from the Institute for Breathing and Sleep, during the conduct of the study; and grants from Resmed Foundation, grants from Edansafe, grants from Prevention Express, and nonfinancial support from Sleep Diagnostics, outside the submitted work. C.A. reports personal fees from Rail, Tram and Bus Union (Australia); grants from VicRoads; personal fees from AusMed; personal fees from Providence Sleep Research Interest Group, Brown University; personal fees from the National Transport Commission; and personal fees from VicPolice, outside the submitted work.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1510383112/-/DCSupplemental.
References
- 1.Institute of Medicine . Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Institute of Medicine of the National Academies; The National Academies Press; Washington, DC: 2006. [PubMed] [Google Scholar]
- 2.Connor J, et al. Driver sleepiness and risk of serious injury to car occupants: Population based case control study. BMJ. 2002;324(7346):1125. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tefft BC. Prevalence of Motor Vehicle Crashes Involving Drowsy Drivers, United States, 2009–2013. AAA Foundation for Traffic Safety; Washington, DC: 2014. [DOI] [PubMed] [Google Scholar]
- 4.Dingus TA, et al. The 100-Car Naturalistic Driving Study; Phase II-Results of the 100-Car Field Experiment. National Highway Traffic Safety Administration; Washington, DC: 2006. pp. 1–352. [Google Scholar]
- 5.MacLean AW, Davies DR, Thiele K. The hazards and prevention of driving while sleepy. Sleep Med Rev. 2003;7(6):507–521. doi: 10.1016/s1087-0792(03)90004-9. [DOI] [PubMed] [Google Scholar]
- 6.National Sleep Foundation 2009 2009 Sleep in America Poll: Summary of Findings. Available at https://sleepfoundation.org/sleep-polls-data/sleep-in-america-poll/2009-health-and-safety. Accessed November 16, 2015.
- 7.McMenamin T. A time to work: Recent trends in shift work and flexible schedules. Mon Labor Rev. 2007;130(12):3–15. [Google Scholar]
- 8.Gold DR, et al. Rotating shift work, sleep, and accidents related to sleepiness in hospital nurses. Am J Public Health. 1992;82(7):1011–1014. doi: 10.2105/ajph.82.7.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Åkerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosci. 1990;52(1-2):29–37. doi: 10.3109/00207459008994241. [DOI] [PubMed] [Google Scholar]
- 10.Crummy F, Cameron PA, Swann P, Kossmann T, Naughton MT. Prevalence of sleepiness in surviving drivers of motor vehicle collisions. Intern Med J. 2008;38(10):769–775. doi: 10.1111/j.1445-5994.2008.01629.x. [DOI] [PubMed] [Google Scholar]
- 11.Barger LK, et al. Harvard Work Hours, Health, and Safety Group Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352(2):125–134. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 12.Czeisler CA, Gooley JJ. Sleep and circadian rhythms in humans. Cold Spring Harb Symp Quant Biol. 2007;72:579–597. doi: 10.1101/sqb.2007.72.064. [DOI] [PubMed] [Google Scholar]
- 13.Verster JC, Taillard J, Sagaspe P, Olivier B, Philip P. Prolonged nocturnal driving can be as dangerous as severe alcohol-impaired driving. J Sleep Res. 2011;20(4):585–588. doi: 10.1111/j.1365-2869.2010.00901.x. [DOI] [PubMed] [Google Scholar]
- 14.O’Hanlon JF, Beatty J. Concurrence of electroencephalographic and performance changes during a simulated radar watch and some implications for the arousal theory of vigilance. In: Mackie RR, editor. Vigilance Theory, Operational Performance, and Physiological Correlates. Plenum Press; New York: 1977. pp. 189–201. [Google Scholar]
- 15.Mitler MM, Miller JC, Lipsitz JJ, Walsh JK, Wylie CD. The sleep of long-haul truck drivers. N Engl J Med. 1997;337(11):755–761. doi: 10.1056/NEJM199709113371106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akerstedt T, Peters B, Anund A, Kecklund G. Impaired alertness and performance driving home from the night shift: A driving simulator study. J Sleep Res. 2005;14(1):17–20. doi: 10.1111/j.1365-2869.2004.00437.x. [DOI] [PubMed] [Google Scholar]
- 17.Howard ME, Radford L, Jackson ML, Swann P, Kennedy GA. The effects of a 30-minute napping opportunity during and actual night shift on performance and sleepiness in shift workers. Biol Rhythm Res. 2009;41(2):137–148. [Google Scholar]
- 18.Collision Analysis Working Group . 65 Main-Track Train Collisions, 1997 through 2002: Review, Analysis, Findings, and Recommendations. 2006. Available at www.fra.dot.gov/Elib/Document/1575. Accessed November 16, 2015. [Google Scholar]
- 19.National Transportation Safety Board . Railroad Accident Report. Collision Between Two Washington Metropolitan Area Transit Authority Trains at the Woodley Park-Zoo/Adams Morgan Station in Washington, D.C. November 3, 2004. National Transportation Safety Board; Washington, DC: 2006. [Google Scholar]
- 20.Philip P, et al. Fatigue, sleep restriction and driving performance. Accid Anal Prev. 2005;37(3):473–478. doi: 10.1016/j.aap.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Ftouni S, et al. Objective and subjective measures of sleepiness, and their associations with on-road driving events in shift workers. J Sleep Res. 2013;22(1):58–69. doi: 10.1111/j.1365-2869.2012.01038.x. [DOI] [PubMed] [Google Scholar]
- 22.Thiffault P, Bergeron J. Monotony of road environment and driver fatigue: A simulator study. Accid Anal Prev. 2003;35(3):381–391. doi: 10.1016/s0001-4575(02)00014-3. [DOI] [PubMed] [Google Scholar]
- 23.Ting PH, Hwang JR, Doong JL, Jeng MC. Driver fatigue and highway driving: A simulator study. Physiol Behav. 2008;94(3):448–453. doi: 10.1016/j.physbeh.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 24.Johns MW, et al. A new scale of drowsiness based on multiple characteristics of eye and eyelid movements: The Johns Drowsiness Scale. Sleep Biol Rhythms. 2006;4(Suppl 1):A37. [Google Scholar]
- 25.Akerstedt T, et al. Having to stop driving at night because of dangerous sleepiness—Awareness, physiology and behaviour. J Sleep Res. 2013;22(4):380–388. doi: 10.1111/jsr.12042. [DOI] [PubMed] [Google Scholar]
- 26.Office or Motor Carrier Research Standards . PERCLOS: A Valid Psychophsiological Measure of Altertness as Assessed by Psychomotor Vigilance. US Department of Transportation Federal Highway Administration; Washington, DC: 1998. pp. 1–4. [Google Scholar]
- 27.Wilkinson VE, et al. The accuracy of eyelid movement parameters for drowsiness detection. J Clin Sleep Med. 2013;9(12):1315–1324. doi: 10.5664/jcsm.3278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson C, Chang AM, Sullivan JP, Ronda JM, Czeisler CA. Assessment of drowsiness based on ocular parameters detected by infrared reflectance oculography. J Clin Sleep Med. 2013;9(9):907–920, 920A–920B. doi: 10.5664/jcsm.2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lockley SW, et al. Harvard Work Hours, Health and Safety Group Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351(18):1829–1837. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 30.Cajochen C, Khalsa SBS, Wyatt JK, Czeisler CA, Dijk DJ. EEG and ocular correlates of circadian melatonin phase and human performance decrements during sleep loss. Am J Physiol. 1999;277(3 Pt 2):R640–R649. doi: 10.1152/ajpregu.1999.277.3.r640. [DOI] [PubMed] [Google Scholar]
- 31.Howard ME, et al. Specific sleepiness symptoms are indicators of performance impairment during sleep deprivation. Accid Anal Prev. 2014;62:1–8. doi: 10.1016/j.aap.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 32.Horne JA, Baulk SD. Awareness of sleepiness when driving. Psychophysiology. 2004;41(1):161–165. doi: 10.1046/j.1469-8986.2003.00130.x. [DOI] [PubMed] [Google Scholar]
- 33.Reyner LA, Horne JA. Falling asleep whilst driving: Are drivers aware of prior sleepiness? Int J Legal Med. 1998;111(3):120–123. doi: 10.1007/s004140050131. [DOI] [PubMed] [Google Scholar]
- 34.Folkard S. Black times: Temporal determinants of transport safety. Accid Anal Prev. 1997;29(4):417–430. doi: 10.1016/s0001-4575(97)00021-3. [DOI] [PubMed] [Google Scholar]
- 35. Massachusetts v. Salvaggio, North Berkshire County, Massachusetts District Court 1994, No. 9428CR000504. (1994). Available at www.cnn.com/HEALTH/9703/17/nfm/sleep.deprivation/. Accessed November 16, 2015.
- 36.Philip P, Taillard J, Quera-Salva MA, Bioulac B, Akerstedt T. Simple reaction time, duration of driving and sleep deprivation in young versus old automobile drivers. J Sleep Res. 1999;8(1):9–14. doi: 10.1046/j.1365-2869.1999.00127.x. [DOI] [PubMed] [Google Scholar]
- 37.Hung CS, et al. Local experience-dependent changes in the wake EEG after prolonged wakefulness. Sleep. 2013;36(1):59–72. doi: 10.5665/sleep.2302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moore RT, Kaprielian R, Auerbach J. 2009. Asleep at the Wheel. Report of the Massachusetts Commission on Drowsy Driving. Available at https://sleep.med.harvard.edu/file_download/103. Accessed November 16, 2015.
- 39.McKenzie B, Rapino M. 2011. Commuting in the United States: 2009. American Community Survey Reports ACS-15 (US Census Bureau, Washington, DC). Available at https://www.census.gov/prod/2011pubs/acs-15.pdf. Accessed November 17, 2015. [Google Scholar]
- 40.Horne JA, Östberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4(2):97–110. [PubMed] [Google Scholar]
- 41.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131(7):485–491. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 42.Howard ME, Gora J, Swann P, Pierce RJ. Evidence for poor perception of sleepiness in professional drivers. Sleep. 2002;25(Suppl):A146. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.