Abstract
We previously demonstrated that cigarette smoke (CS) exposure decreases primordial follicle counts and induces autophagy in ovarian granulosa cells in preference to apoptosis. Therefore, the objective of this study was to investigate molecular targets underlying smoke-induced activation of the reparative autophagy pathway in the ovary. Briefly, ovarian homogenates were prepared from adult female mice exposed to mainstream CS twice daily for 8 wk, using a whole-body exposure system. A gene array revealed that CS exposure induced a greater than 2-fold significant increase in the expression of proautophagic genes Cdkn1b, Map1lc3a, Bad, and Sqstm1/p62. A significant increase in Prkaa2, Pik3c3, and Maplc31b expression, as well as a significant decrease in Akt1 and Mtor expression, was detected by quantitative PCR. The 5′-AMP-activated protein kinase catalytic subunit (AMPK) alpha1 + alpha2 and ATG7 protein expression was significantly increased, whereas AKT1, mTOR, CDKN1B/p27, and CXCR4 proteins were significantly decreased in CS exposed versus control ovaries. Up-regulation of AMPK alpha1 + alpha2, a known initiator of autophagic signaling, and ATG7 further suggests activation of the autophagy cascade. Two prosurvival factors, AKT and mTOR, were decreased in expression, an outcome that favors induction of the autophagy pathway, whereas decreased levels of CDKN1B is suggestive of cell cycle dysregulation. In summary, our data suggest that CS exposure induces ovarian follicle loss through induction of the autophagic cascade via the AMPK pathway together with inhibition of antiautophagic markers AKT and mTOR. We further postulate that toxicant-induced dysregulation of reparative autophagy is a novel pathway central to impaired follicle development and subfertility.
Keywords: autophagy, cell death, cigarette smoke, ovarian function
INTRODUCTION
Although the hazardous effects of cigarette smoke (CS) to the respiratory and cardiovascular systems have been well documented [1, 2], the effects on reproductive health and the reproductive tract specifically are less well defined. Shorter menstrual cycles, lower circulating concentrations of estradiol [3], decreased fertility rates, and early-onset menopause have been documented in women who smoke compared with nonsmokers [4]. Moreover, longer time to pregnancy, reduced success rates with assisted reproductive technology, altered ovarian steroidogenesis, depleted ovarian follicle reserve, impaired oocyte function and viability, and earlier mean age of menopause have all been documented in women who smoke versus nonsmokers [5–24], each of which has enormous emotional, financial, and health consequences. Although cigarette smoking is declining in men, the number of women and teenage girls who smoke is increasing. Globally, approximately 250 million women are daily smokers [25] and 30% of women of reproductive age in the United States are smokers [26, 27], whereas in Canada approximately 17% of Canadian women are current smokers, smoking an average of 14.0 cigarettes per day [28, 29]. Regrettably, most women remain unaware of the adverse effects of cigarette smoking on fertility and ovarian function [30].
Cigarette smoking in humans [19, 20, 24] and CS exposure in mice [31, 32] deplete the primordial follicle population. We previously demonstrated decreased primordial follicle counts coupled with oxidative stress and granulosa cell autophagy in mice exposed to CS at concentrations representative of those for women who smoke [24, 31, 33]. Contrary to our expectations, follicle loss was not associated with increased apoptosis, as shown by an absence of an effect on TUNEL staining, DNA laddering, and activated caspase-3, or caspase-8 and caspase-9 expression, compared with controls [31]. Rather, CS exposure induced oxidative stress in the ovary together with increased expression of Beclin-I and microtubule-associated protein-I light chain 3 (LC3), markers of autophagy. Increased numbers of autophagolysosomes in the granulosa cells of follicles from mice exposed to CS compared with control mice have also been demonstrated [33]. Taken together, we suggest that CS exposure causes follicle loss through induction of mitochondrial dysfunction, leading to oxidative stress and activation of autophagy (self-digestion), a novel alternative/accessory cell death pathway that is relatively unexplored in the ovary.
Autophagy is an intracellular mechanism whereby damaged organelles and proteins are degraded and recycled by the cell itself to ultimately protect the cell [34]. Autophagy can ensure cellular survival under conditions of stress, removing damaged subcellular constituents, including aggregated proteins, and may indirectly be a protective mechanism. Autophagy can be induced by either nutrient depletion (starvation) or energy exhaustion [34] and is implicated in a range of diseases, particularly cancer [35]. Under conditions of nutrient restriction or starvation, the mammalian target of rapamycin (mTOR) is inhibited, allowing autophagy to proceed via activation of 5′-AMP-activated protein kinase catalytic subunit (AMPK) and ULK1 (UNC-51-like kinase 1), sometimes in response to increased oxidative stress [36]. However, the mTORC1 (complex) is capable of negatively regulating the pathway through dephosphorylation of a macromolecular substrate complex that includes ULK1, ATG13, ATG101, and FIP200 (RB1CC10), which in turn inhibits autophagy [37]. Autophagy inhibitor complex mTORC1 integrates multiple signals, reflecting the availability of growth factors, nutrients, or energy to promote either cellular growth in favorable conditions or catabolic processes during stressful conditions. It is well known that autophagy is also regulated by Beclin1 (BECN1, the mammalian counterpart of the yeast ATG6 protein) [34] complex (death-associated autophagy), which is negatively regulated by the PI3K/AKT pathway (stimulated by growth factors) by interactions with the antiapoptotic Bcl-2 family of proteins. Our lab has shown that increased expression of both BECN1 and LC3 occurs in mice exposed to CS [33]. The mechanisms through which toxicants present in CS induce autophagy remain to be elucidated. In the present study we describe the CS exposure induced changes in gene and protein expression and propose a mechanism by which cigarettes activate smoke-induced autophagy.
MATERIALS AND METHODS
Ethics
All animal work was conducted using protocol AUP no. 14-07-24, approved by the McMaster University Animal Research Ethics Board, and was carried out in accordance with the Canadian Council for Animal Care guidelines for the use of animals in research.
CS Exposure
Female C57BL/6 mice (age 8 wk at the start of exposure) were obtained from Charles River Laboratories. Mice were maintained in polycarbonate cages at 22°C to 28°C and 50% ± 10% relative humidity on a 12L:12D photoperiod and were provided with food (LabDiet; PMI Nutrition International) and tap water ad libitum throughout the experiment. Mice were exposed to CS twice daily, 5 days a week, for a total of 8 wk using a whole-body, mainstream smoke exposure system (SIU48; Promech Lab AB). Cigarette smoke exposure resulted in carboxyhemoglobin and cotinine levels comparable to those in human smokers [38]. Details of the experimental design and exposure protocol have been described previously [33]. Briefly, one ovary was collected and fixed for routine histology and subsequent follicle counts, the results of which have been described previously and demonstrated a significant treatment-related decrease in primordial follicle numbers [6]. The remaining ovary was collected, immediately frozen, and stored at −80°C for gene and protein expression analyses. Demonstration of CS-induced decrease in primordial follicle counts and evidence of autophagy prompted us to expand our study to changes in gene and protein expression in the autophagy pathway.
Autophagy Gene Array
The Mouse Autophagy RT2 Profiler PCR Array (SA Biosciences) was used in accordance with the manufacturer's recommendations, to study autophagy-specific gene expression profiles. Real-time PCR was performed with murine-specific primers using the Applied Biosystems 7900HT Fast Real-Time PCR System (Applied BioSystems). Analysis of gene expression changes were calculated according to the method of Livak et al. [39] using the 2-ΔΔCt method. Statistical analyses were performed using the ΔCt ± SD values.
Quantitative Real-Time PCR
Total RNA was isolated from ovaries using a total RNA purification kit (NORGEN; Biotek Corp.) per the manufacturer's instructions and was quantified by spectrophotometric analysis (Nanodrop). Complementary DNA was then reverse transcribed using an iScript kit (Bio-Rad). Primers were designed using the online tools Primer3, IDTDNA, and OligoAnalyzer3.0, and primer products between 50 and 130 bp were selected for analysis. Murine-specific primers were designed (Mobix Lab) and primer pairs (SA Biosciences) are displayed in Table 1. The PCR amplification was carried out in a 10-μl reaction volume (7 μl of master mix) containing 1 μg/100 ng cDNA (2.5 μl), either 1 μl of forward and 1 μl of reverse primers (Mobix Lab), or 10 μM forward and reverse primers (SA Biosciences) were added to 5 μl of SYBR Green Master Mix (Roche, Canada) and 2 μl of ddH2O. Real-time PCR reactions were carried out using the Roche LC480 instrument, and the program was set as follows: denaturation at 95°C for 10 min, followed by 40 amplification cycles of 95°C for 15 sec and 60°C for 1 min. Samples were run in duplicate and results were averaged. Relative quantification analysis was used to compare the levels of expression between treatments of either sham or smoke, and the housekeeper (reference) gene selected for analysis was constitutively expressed under all conditions. The reference gene (Actb) was used to normalize sample-to-sample differences. Results are presented as the mean normalized ratios of the internal reference gene.
TABLE 1.
List of forward and reverse primer sequences used for qPCR analysis.
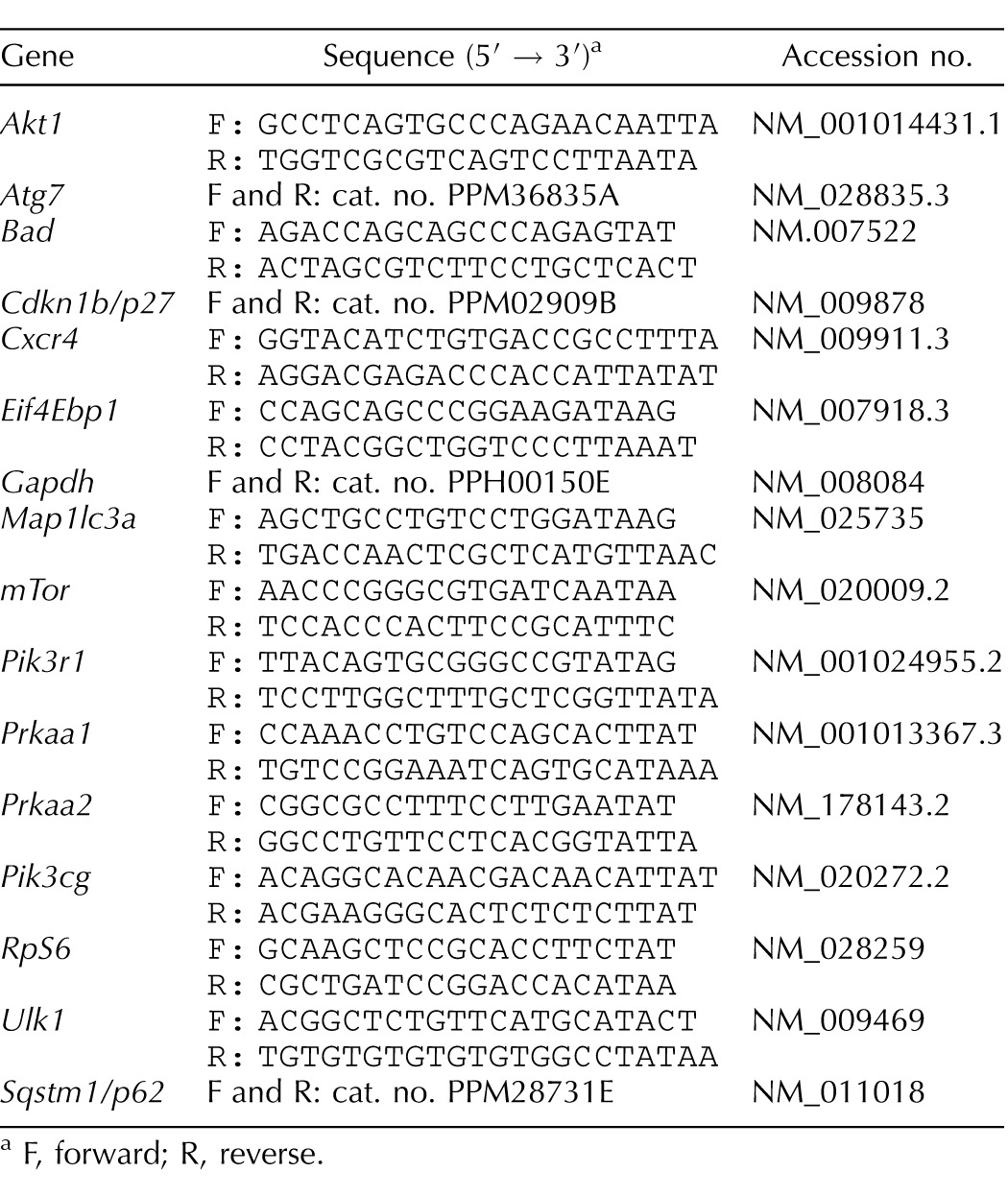
F, forward; R, reverse.
Western Blot Analysis
Protein expression was measured from the whole-ovarian homogenates from either sham- or smoke-exposed mice as described previously [31]. Following SDS-PAGE and transfer to polyvinylidene difluoride blotting membrane (Bio-Rad), membranes were blocked overnight with 5% (w/v) skim milk in Tris-buffered saline (TBS; 8 g/L [w/v] NaCl, 0.2 g/L [w/v] KCl, and 3 g/L [w/ v] Tris base; pH 7.4) with Tween-20 (TBS-T; 1 × TBS and 0.5% [v/v] Tween-20) or a blocking solution of 5% BSA:TBS-T (depending on the manufacturer's instructions), and incubated with primary antibody at 4°C overnight. The following antibodies were used for the present study: proto-oncogene AKT1 (also known as protein kinase B or PKB; 1:1000; Cell Signaling Technology), cellular homeostasis regulator AMP-k α1 and α2 (1:1000; Abcam), autophagy death-related protein 7 (ATG7; 1:30 000; Novus), cell cycle inhibitor protein CDKN1B/p27 (Novus), mTOR (1:1000; Cell Signaling Technology), phosphoinositide 3-kinase autophagy regulator (PIK3CG; 1:1000; Cell Signaling Technology), ubiquitin binding protein SQSTM1/p62 (1:1000; Novus), and downstream effector and negative regulator of mTOR ULK1 (1:1000; Cell Signaling Technology). Following washing with TBS-T, blots were incubated with horseradish peroxidase-conjugated secondary anti-rabbit immunoglobulin G (IgG; 1:4000; Amersham Biosciences) or anti-mouse IgG (1:4000; Amersham Biosciences) antibodies for 1 h at room temperature. Blots were thoroughly washed in TBS-T followed by TBS, whereupon reactive protein was detected using ECL Plus chemiluminescence substrate (Amersham Biosciences) and Bioflex x-ray film (Clonex Corp.). Densitometric analysis of immunoblots was performed using ImageJ 1.37v software (National Institutes of Health); all proteins were quantified relative to the loading control ACTB (Abnova no. 20272).
Statistical Analysis
Statistical differences were measured using GraphPad Prism software. Data were initially checked for normality by applying a D'Agostino and Pearson omnibus normality test, followed by either a t-test (normally distributed data) or a Mann-Whitney (nonnormally distributed data) test. The quantitative PCR (qPCR) results are presented as normalized mean ratios ± SEM of the target:reference genes. Representative Western blot results are shown and ACTB was used as the loading control. A P value of 0.05 was considered statistically significant.
RESULTS
CS Exposure and General Health of Animals
Animals were assessed during the course of the experiment and at necropsy for changes in general health. No adverse changes in body condition, dehydration, lethargy, and atypical behaviors were noted as a result of CS exposure.
CS Exposure Induces Autophagic Gene Expression Changes with Gene Array
The complete list of autophagic genes analyzed with the gene array is presented in the Supplemental Table S1 (available online at www.biolreprod.org). A summary of the autophagy genes whose expression was significantly changed by CS exposure is listed in Table 2, including a description of their role in autophagy. The genes that were significantly increased in the gene array were as follows: Arsa was changed 1.82-fold (P = 0.012), Atg7 changed 1.58-fold (P = 0.050), Bad changed 2.7-fold (P = 0.022), Bak1 changed 1.78-fold (P = 0.037), Cdkn1b changed 4.32-fold (P = 0.011), Cxcr4 changed 1.93-fold (P = 0.028), Map1lc3a changed 3.94-fold (P = 0.006), Pik3c3 changed 1.38-fold (P = 0.041), Rab24 changed 1.95-fold (P = 0.044), Sqstm1/p62 changed 2.44-fold (P = 0.035), and Gapdh changed 1.94-fold (P = 0.030). Next, the genes that were significantly decreased in the gene array were as follows: Atg4b changed −1.24-fold (P = 0.014), Ctsb changed −1.63-fold (P = 0.004), Ctss changed −1.81-fold (P = 0.022), Pik3r4 changed −1.42-fold (P = 0.018), Tgm2 changed −1.73-fold (P = 0.0002), Hprt changed −1.35-fold (P = 0.022), and Hsp90ab1 changed −1.24-fold (P = 0.034).
TABLE 2.
Gene array analyses; autophagy genes significantly altered by cigarette smoke exposure.
CS Exposure Induces the Autophagic Cascade Through AMPK Activation
The qPCR analysis revealed a significant increase in expression of Prkaa2 (P = 0.0457), Pik3c3 (P = 0.0122), and Map1lc3b (P = 0.0321), and a significant decrease in expression of Akt1 (P = 0.0064) and Mtor (P = 0.0237; Figs. 1–3 and 4). Treatment had no effect on the expression of Pik3r1, Eif4ebp1, Ulk, Map1lc3a, Pik3cg, Prkaa1, Rps6, Cdkn1b, Gapdh, Bad, Cxcr4, Sqstm1/p62, and Atg7. Although mRNA changes are not always complemented with comparable protein expression changes and it is ultimately the posttranslational changes that are the most notable indicators of cell signaling, we followed with an investigation for changes in protein expression.
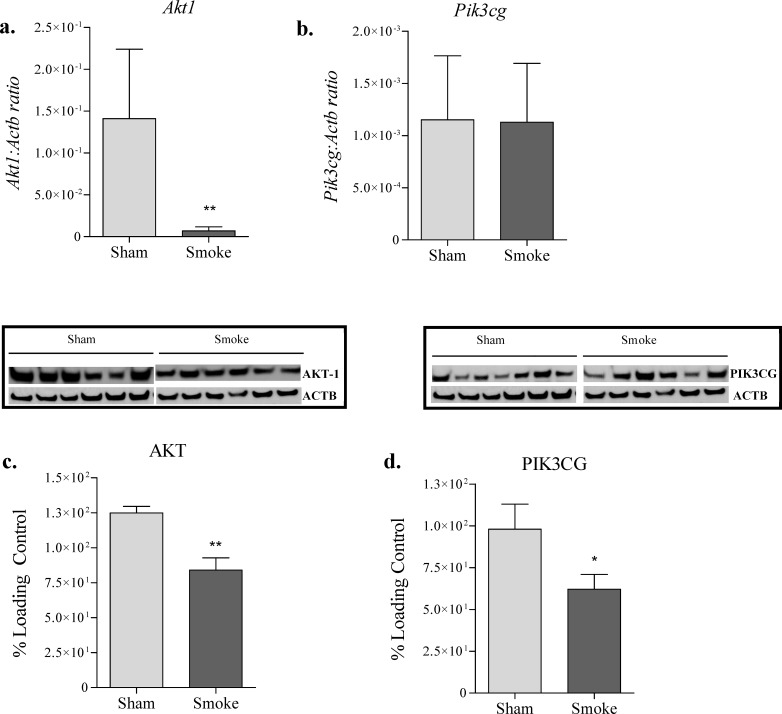
FIG. 1.
Changes in Akt1 gene (a), Pik3cg gene (b), AKT protein (c), and PIK3CG protein (d) expression following 8 wk of exposure to CS. Analysis of Akt1and Pik3cg gene and AKT1 and PIK3CG protein expression was performed on whole-ovarian homogenates from sham and smoke-exposed mice. a and b) qPCR gene expression changes relative to the Actb control (n = 6 per group). c and d) Representative immunoblots demonstrating protein expression changes relative to the ACTB loading control (n = 7 sham and 6 smoke). Data were checked for normality and equal variance, and treatment effects were tested using t-test. Values are expressed as mean ± SEM. *P < 0.05 and ** P < 0.01.
FIG. 2.
Changes in Prkaa1 (a) and Prkaa2 (b) gene and AMPK-α1 and AMPK-α2 protein (c) expression following 8 wk of exposure to cigarette smoke. Analysis of Prkaa1 and Prkaa2 gene and AMPK protein expression was performed on whole-ovarian homogenates from sham and smoke-exposed mice. a and b) qPCR gene expression changes relative to Actb used as a loading control (n = 6 per group). c) Representative immunoblot showing protein expression changes relative to the ACTB loading control (n = 7 sham and 6 smoke). Data were checked for normality and equal variance, and treatment effects were tested using t-test. Values are expressed as mean ± SEM. *P < 0.05.
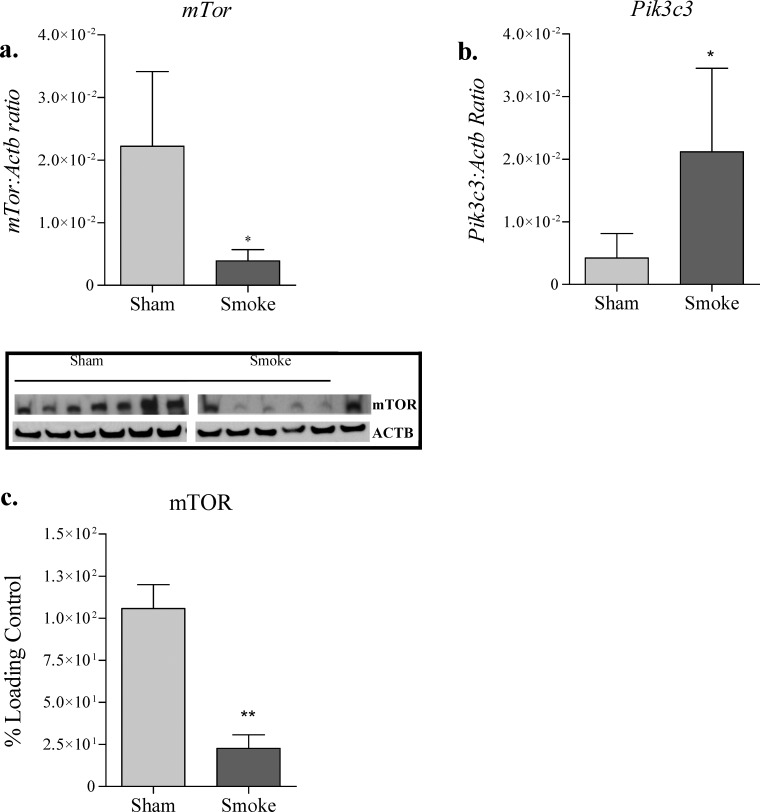
FIG. 3.
Changes in mTor gene (a), Pik3c3 gene (b), and mTOR protein (c) expression following 8 wk of exposure to cigarette smoke. Analysis of mTor and Pik3c3 gene and mTOR protein expression was performed on whole-ovarian homogenates from sham and smoke-exposed mice. a and b) qPCR gene expression changes relative to the Actb control (n = 6 per group). c) Representative immunoblot showing protein expression changes relative to the ACTB loading control (n = 7 sham and 6 smoke). Data were checked for normality and equal variance, and treatment effects were tested using t-test. Values are expressed as mean ± SEM. *P < 0.05 and ** P < 0.01.
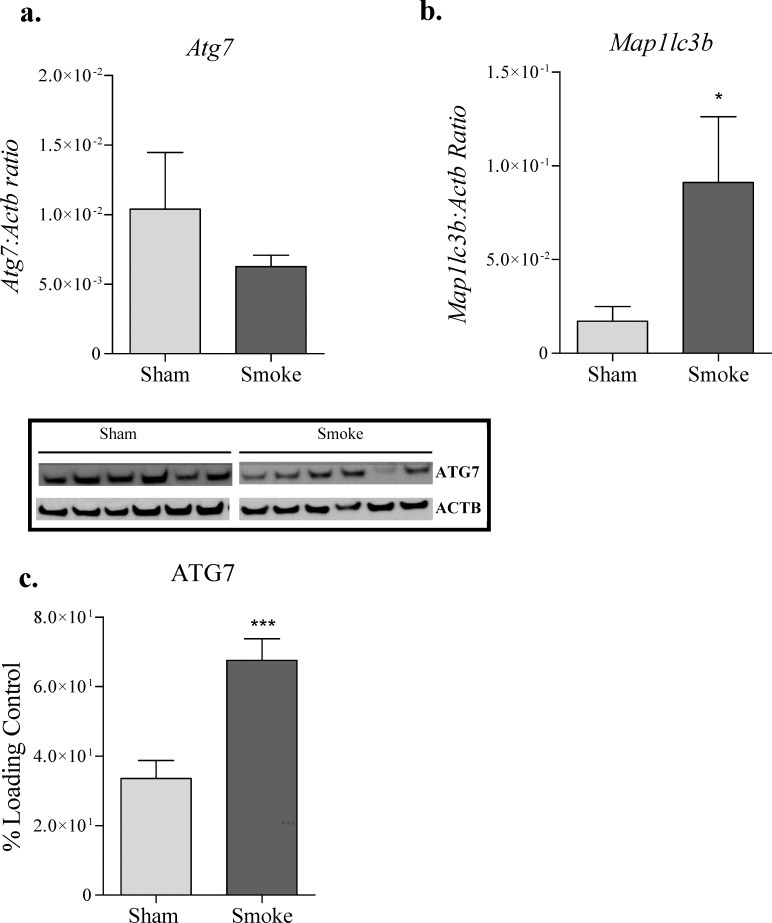
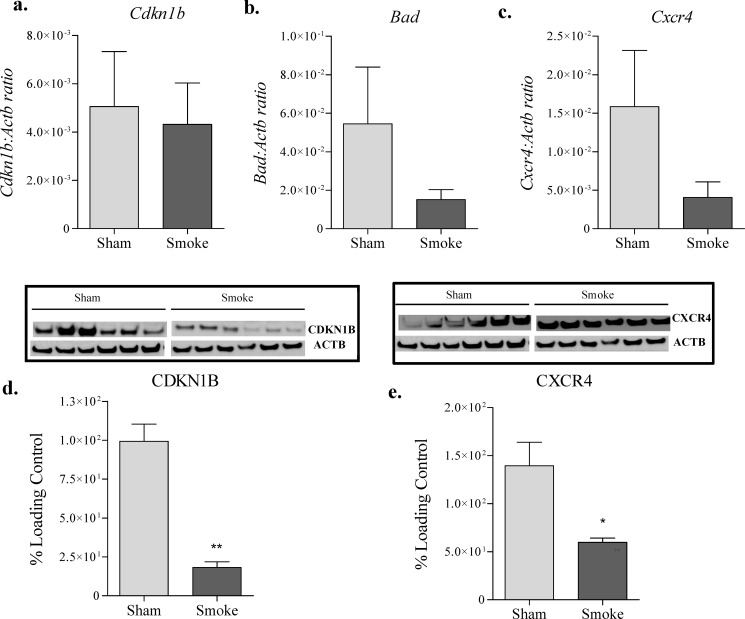
Western blot analysis revealed a significant CS-induced 1.82-fold increase in AMP-k α1 + α2 (P = 0.0119; Fig. 2) and a significant 2-fold increase in ATG7 expression (P = 0.0006; Fig. 4). Furthermore, CS exposure induced significant decreases of −1.49-fold in AKT1 (P = 0.0022; Fig. 1), −1.6 fold in PIK3CG (P = 0.0325; Fig. 1), −4.66-fold in mTOR (P = 0.0043; Fig. 3), −5.46-fold in CDKN1B/p27 (P = 0.0022; Fig. 5), and −2.33-fold in CXCR4 (P = 0.0109; Fig. 5). Exposure to CS had no effect on the expression of p62/SQSTM1 (data not shown).
FIG. 4.
Changes in Atg7 gene (a) and Map1lc3b gene (b) and ATG7 protein (c) expression following 8 wk of exposure to cigarette smoke. Analysis of Atg7 and Map1lc3b gene and ATG7 protein expression was performed on whole-ovarian homogenates from sham and smoke-exposed mice. a and b) qPCR gene expression changes relative to the Actb control (n = 6 per group). c) Representative immunoblots demonstrating protein expression changes relative to the ACTB loading control (n = 7 sham and 6 smoke). Data were checked for normality and equal variance, and treatment effects were tested using t-test. Values are expressed as mean ± SEM. *P < 0.05 and ** P < 0.01.
FIG. 5.
Changes in Cdkn1b gene (a), Bad gene (b), Cxcr4 gene (c), CDKN1B protein (d), and CXCR4 protein (e) expression following 8 wk of exposure to cigarette smoke. Analysis of Cdkn1b Bad and Cxcr4 gene and CDKN1B and CXCR4 protein expression was performed on whole-ovarian homogenates from sham and smoke-exposed mice. a–c) qPCR gene expression changes relative to actb control (n = 6 per group). d and e) Representative immunoblots showing protein expression changes relative to the ACTB loading control (n = 7 sham and 6 smoke). Data were checked for normality and equal variance, and treatment effects were tested using t-test. Values are expressed as mean ± SEM. *P < 0.05 and ** P < 0.01.
DISCUSSION
We previously demonstrated that CS exposure induces oxidative stress, ovarian follicle loss, and autophagy in the mouse ovary [24, 31, 33]. Using ovarian homogenates from our prior study [33], we demonstrated that CS exposure-induced autophagy arises from activation of the AMPK pathway together with inhibition of the antiautophagic factors AKT and mTOR. Although gene array results revealed significant changes in the expression of genes involved in the autophagy pathway, these results could not be confirmed by real-time PCR. Although the gene array used was composed of multiple genes reported to be involved in the autophagy pathway, it was not enriched with genes central to the regulation of autophagy, and therefore targeted real-time PCR was used to extend our investigation of CS exposure-induced changes in autophagy. Our results revealed that CS exposure induced significant changes in the expression of genes and proteins involved in: 1) induction of the autophagy pathway (AMPK-α1, AMPK-α2); 2) inhibition of antiautophagic proteins (AKT and mTOR); changes that were coupled with cell cycle dysregulation (CDKN1B) and cell survival (CXCR4 and BAD); and 3) autophagosome and lysosome fusion (ATG7). These results expand on our prior observations [24, 31, 33] and, taken together, suggest that CS exposure induces ovarian stress, resulting in ovarian follicle loss through diminished inhibition coupled with activation of the autophagic cascade.
Results of the current study demonstrated that CS exposure-induced ovarian cell autophagy [5] follows from activation of AMPK-α1and AMPK-α2 in the ovary of CS-exposed mice compared with the control group. Unfortunately, we did not have enough sample to examine for treatment-related changes in AMPK phosphorylation, but this will be examined in our ongoing studies. Autophagy is an integral part of the mammalian stress response, and emerging evidence has linked CS exposure and CS extract treatment with autophagy in the lung, intestine, pancreatic ductal cells, and fibroblasts [40–44]. Moreover, autophagy has been induced in cultures of blastocysts [45], human cord blood hematopoietic stem cells [46] treated with polychlorinated biphenyls, and heavy metals, suggesting that autophagy is a common response to toxicant exposure. Consistent with our findings, oxidative stressors produced by CS have been shown to increase AMPK expression in the lung and diaphragm muscle of mice [47]. AMPK plays a key role in regulating cellular energy metabolism in response to depleted energy levels. AMPK is activated in response to a reduction of intracellular ATP levels and consequently inhibits cell growth and proliferation [48]. AMPK is responsive to exercise, nutrient levels, and cytokines, thus controlling appetite and energy expenditure [49]. Although AMPK is recognized for its role as an energy sensor and regulator, there is emerging evidence advocating a role for AMPK as an oxidative stress sensor and redox regulator, in addition to its traditional functions. Oxidant-mediated activation of AMPK has also been shown to occur in cultured vascular smooth muscle cells exposed to nicotine, a component of CS [50]. It is believed that AMPK is activated in response to the intracellular reactive oxygen species generated from toxic exposure of CS and is capable of inhibiting oxidative stress, therefore maintaining intracellular redox status. We previously demonstrated that autophagy was also coupled with mitochondrial dysfunction, as demonstrated by increased expression of parkin protein and decreased expression of its target profusion proteins, mitofusin 1 and mitofusin 2, indicative of mitophagy [33]. Taken together, we suggest that CS exposure induces mitochondrial dysfunction and oxidative stress, leading to the inability of the granulosa cell to meet its energy needs and culminating in activation of the reparative autophagy cascade.
In addition to activation of the autophagy cascade, results of the present study revealed CS exposure-induced inhibition of cell survival and expression of inhibitory markers of autophagy. Akt1 gene, AKT1 protein, and PI3K Class 3 protein expression were decreased in CS-exposed mice compared with controls. The PI3K Class 1/AKT signaling pathway is responsible for promoting both growth and cell survival [51] and is a negative regulator of autophagy. The PI3K/Akt pathway is also responsible for activation of the mTOR pathway, in turn regulating cell growth [52]. Although in the current study Mtor gene expression was nonsignificantly changed, the MTOR protein was significantly down-regulated, possibly inhibited by upstream activation of AMPK protein. The mTOR responds to changes in growth factors, nutrients, and an induction of stress signals, regulating cellular metabolism [36], and is a negative regulator of autophagy [53]. Harmonious with decreased mTOR expression, we found no change in the expression of downstream mTOR-regulated genes: eukaryotic translation repressor gene (Eif4ebp1) and ribosomal protein S6 kinase (RpS6; data not shown). Consistent with results of the present study, the mTOR signaling pathway was down-regulated in CS-exposed aortic endothelial cells together with up-regulated AMPK, indicative of a CS-induced, AMPK driven-autophagic response [54]. Further downstream of mTOR signaling, we investigated treatment-induced changes in Unc51-like kinase (ULK1) expression because both AMPK and mTOR are responsible for regulation of autophagy via coordinated phosphorylation of ULK1 [36, 55]. ULK1 is a serine/threonine kinase that responds to decreased energy levels and starvation, regulating the formation of autophagophores [56], precursors to autophagosomes. In the current study, Ulk1 gene and ULK1 protein expression were unchanged by CS exposure (data not shown).
We next reasoned that CS exposure-induced chronic oxidative stress in the ovary [5] would be associated with dysregulation of cell cycle gene expression. We therefore investigated expression of cyclin-dependent kinase inhibitor 1B (CDKN1B/p27) and Gapdh. Although Gapdh had no significant change in expression by CS exposure in the current study, cell cycle dysregulation was shown by the significant down-regulation of cyclin-dependent kinase inhibitor 1B (CDKN1B/p27) protein, an important regulator of cell cycle progression. These findings are consistent with our observations that CS extract exposure attenuated ovarian follicle development in culture [9]. Because these effects could equally arise from augmented cell death, we also evaluated treatment-induced changes in cell survival by measurement of proapoptotic Cxcr4 and Bad expression. C-X-C chemokine receptor type 4 (Cxcr4) acts as a receptor for the C-X-C chemokine CXCL12/SDF-1, which transduces a signal by increasing intracellular calcium ion levels and enhancing MAPK1/MAPK3 activation, and it acts as a receptor for extracellular ubiquitin, leading to enhanced intracellular calcium ions and reduced cellular cAMP levels, thus engaging in either prosurvival or prodeath signals [57]. Our results revealed that CXCR4 protein was significantly down-regulated following 8 wk of exposure to CS. Expression of Bad gene was nonsignificantly changed in response to CS. Proapoptotic Bad is a BCL-2-associated death promoter via activation of Bax and inhibition of antiapoptotic Bcl-2 [57]. Bcl-2 acts as a link between growth factor receptor signaling and the apoptotic pathway, findings that are harmonious with our prior studies [24, 31, 33]. Although CS exposure had no effect on Bax expression and Bcl2 expression was decreased, apoptosis was absent, as shown by no change in either activated caspase-3 concentrations or TUNEL staining of ovarian sections. Our results therefore suggest an absence of apoptosis and a role for an alternative cell death response mechanism, such as autophagy.
Having shown that CS exposure induces activation of autophagy, we next examined treatment-induced changes in microtubule-associated protein 1 light chain 3 alpha and beta (Map1lc3a and Map1lc3b), which are associated with the formation of autophagosomes [58]. Treatments had no effect on Map1lc3a expression (data not shown), whereas Map1lc3b expression was significantly increased. Similarly, we could not demonstrate treatment-induced changes in Sqstm1/p62 gene and SQSTM1/p62 expression. We postulate that differences in gene and protein expression were not detected because of a large variability in both the control and CS groups. We note that in our prior study, CS induced an overexpression of the autophagic proteins, BECN1 and LC3, indicative of autophagy, with clear morphological evidence of autophagy [33]. Although MAP1LC3a is involved in the formation of the autophagosome, LC3 is responsible for elongation of the phagophore membranes [59]. We speculate that CS exposure triggers autophagy with autophagosome formation supported by basal MAP1LC3a expression, whereas elongation of the autophagosome is supported by increased LC3 expression, as shown in our previous work [33]. These events occur upstream of Pik3c3, which was similarly not significantly changed in expression. Even though Pik3c3 is known to play a role in the initiation and maturation of autophagosomes, LC3 is the major regulator of this process. Next, the expression of Atg7 gene was measured and found to be unchanged, whereas ATG7 protein was significantly increased in response to CS. ATG7 is known for its involvement in vesicle elongation and is an E1-like protein, required for the formation of autophagosomes and involved in the conjugation of ubiquitin-like systems of ATG5-ATG12 and the addition of phosphatidylethanolamine to LC3/GABARAPL2 (microtubule-associated protein light chain 3) [60], which permits elongation of the autophagosome membrane. Our findings are supported by evidence of autophagy in lung tissue of patients with early-stage chronic obstructive pulmonary disease, demonstrated by increases in ATG7 and LC3 activity [61]. The same group also demonstrated that cigarette smoke extract in vitro increased autophagy. Collectively, our results suggest that autophagy is a potential therapeutic target for CS-related disease.
In summary, results of the present study reveal that CS exposure triggers activation of the reparative autophagy cascade through up-regulation of the AMPK pathway together with inhibition of the antiautophagic factors AKT and mTOR in the mouse ovary. We conclude that autophagy is activated by CS in addition to toxicants from different chemical classes [45, 46]. Moreover, our results further indicate that autophagy is an integral part of the mammalian stress response in multiple target tissues [40–44] that includes the ovary. Therefore, we suggest that further investigation of the autophagy pathway could elucidate potential targets for novel therapeutic interventions for fertility preservation and CS-related illness.
ACKNOWLEDGMENT
The authors would like to thank Joanna Kasinska for her technical support with the full-body smoke-exposure system. The authors declare that they do not have any conflict of interest to report.
Footnotes
Supported by a scholarship from the Canadian Institutes of Health Research Training Program in Reproduction, Early Development, and the Impact on Health (H.C.F.).
REFERENCES
- Chen Z, Lam HC, Jin Y, Kim H, Cao J, Lee S, Ifedigbo E. Autophagy protein microtubule-associated protein 1 light chain-3B (LC3B) activates extrinsic apoptosis during cigarette smoke-induced emphysema. Proc Natl Acad Sci U S A. 2010;107:18880–18885. doi: 10.1073/pnas.1005574107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakahira K, Choi AMK. Autophagy: a potential therapeutic target in lung diseases. Am J Physiol Lung Cell Mol Physiol. 2013;305:L93–L107. doi: 10.1152/ajplung.00072.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windham GC, Elkin EP, Swan SH, Waller KO, Fenster L. Cigarette smoking and effects on menstrual function. Obstet Gynecol. 1999;93:59–65. doi: 10.1016/s0029-7844(98)00317-2. [DOI] [PubMed] [Google Scholar]
- Soares SR, Simon C, Remohí J, Pellicer A. Cigarette smoking affects uterine receptiveness. Hum Reprod. 2007;22:543–547. doi: 10.1093/humrep/del394. [DOI] [PubMed] [Google Scholar]
- Swauger JE, Steichen TJ, Murphy PA, Kinsler S. An analysis of the mainstream smoke chemistry of samples of the U.S. cigarette market acquired between 1995 and 2000. Regul Toxicol Pharmacol. 2002;35:142–156. doi: 10.1006/rtph.2001.1521. [DOI] [PubMed] [Google Scholar]
- Fuentes A, Muñoz A, Barnhart K, Argüello B, Díaz M, Pommer R. Recent cigarette smoking and assisted reproductive technologies outcome. Fertil Steril. 2010;93:89–95. doi: 10.1016/j.fertnstert.2008.09.073. [DOI] [PubMed] [Google Scholar]
- Neal MS, Hughes EG, Holloway AC, Foster WG. Sidestream smoking is equally as damaging as mainstream smoking on IVF outcomes. Hum Reprod. 2005;20:2531–2535. doi: 10.1093/humrep/dei080. [DOI] [PubMed] [Google Scholar]
- Waylen AL, Metwally M, Jones GL, Wilkinson AJ, Ledger WL. Effects of cigarette smoking upon clinical outcomes of assisted reproduction: a meta-analysis. Hum Reprod Update. 15:31–44. doi: 10.1093/humupd/dmn046. [DOI] [PubMed] [Google Scholar]
- Weigert M, Hofstetter G, Kaipl D, Gottlich H, Krischker U, Bichler K, Poehl M, Feichtinger W. The effect of smoking on oocyte quality and hormonal parameters of patients undergoing in vitro fertilization-embryo transfer. J Assist Reprod Genet. 1999;16:287–293. doi: 10.1023/A:1020496330424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crha I, Hrubá D, Fiala J, Ventruba P, Záková J, Petrenko M. The outcome of infertility treatment by in-vitro fertilisation in smoking and non-smoking women. Cent Eur J Public Health. 2001;9:64–68. [PubMed] [Google Scholar]
- Sterzik K, Strehler E, De Santo M, Trumpp N, Abt M, Rosenbusch B, Schneider A. Influence of smoking on fertility in women attending an in vitro fertilization program. Fertil Steril. 1996;65:810–814. doi: 10.1016/s0015-0282(16)58219-3. [DOI] [PubMed] [Google Scholar]
- Zenzes MT. Smoking and reproduction: gene damage to human gametes and embryos. Hum Reprod Update. 6:122–131. doi: 10.1093/humupd/6.2.122. [DOI] [PubMed] [Google Scholar]
- Zenzes MT, Wang P, Casper RF. Cigarette smoking may affect meiotic maturation of human oocytes. Hum Reprod. 1995;10:3213–3217. doi: 10.1093/oxfordjournals.humrep.a135891. [DOI] [PubMed] [Google Scholar]
- Zenzes MT, Reed TE, Casper RF. Effects of cigarette smoking and age on the maturation of human oocytes. Hum Reprod. 1997;12:1736–1741. doi: 10.1093/humrep/12.8.1736. [DOI] [PubMed] [Google Scholar]
- Van Voorhis BJ, Dawson JD, Stovall DW, Sparks AE, Syrop CH. The effects of smoking on ovarian function and fertility during assisted reproduction cycles. Obstet Gynecol. 1996;88:785–791. doi: 10.1016/0029-7844(96)00286-4. [DOI] [PubMed] [Google Scholar]
- Rowlands DJ, McDermott A, Hull MG. Smoking and decreased fertilisation rates in vitro. Lancet. 1992;340:1409–1410. doi: 10.1016/0140-6736(92)92595-7. [DOI] [PubMed] [Google Scholar]
- Rosevear SK, Holt DW, Lee TD, Ford WC, Wardle PG, Hull MG. Smoking and decreased fertilisation rates in vitro. Lancet. 1992;340:1195–1196. doi: 10.1016/0140-6736(92)92895-m. [DOI] [PubMed] [Google Scholar]
- Jick H, Porter J. Relation between smoking and age of natural menopause: report from the Boston Collaborative Drug Surveillance Program, Boston University Medical Center. Lancet. 1977;1:1354–1355. doi: 10.1016/s0140-6736(77)92562-4. [DOI] [PubMed] [Google Scholar]
- Freour T, Masson D, Mirallie S, Jean M, Bach K, Dejoie T, Barriere P. Active smoking compromises IVF outcome and affects ovarian reserve. Reprod Biomed Online. 2008;16:96–102. doi: 10.1016/s1472-6483(10)60561-5. [DOI] [PubMed] [Google Scholar]
- El-Nemr A, Al-Shawaf T, Sabatini L, Wilson C, Lower AM, Grudzinskas JG. Effect of smoking on ovarian reserve and ovarian stimulation in in-vitro fertilization and embryo transfer. Hum Reprod. 1998;13:2192–2198. doi: 10.1093/humrep/13.8.2192. [DOI] [PubMed] [Google Scholar]
- Curtis KM, Savitz DA, Arbuckle TE. Effects of cigarette smoking, caffeine consumption, and alcohol intake on fecundability. Am J Epidemiol. 1997;146:32–41. doi: 10.1093/oxfordjournals.aje.a009189. [DOI] [PubMed] [Google Scholar]
- Hughes EG, Yeo J, Claman P, YoungLai EV, Sagle MA, Daya S, Collins JA. Cigarette smoking and the outcomes of in vitro fertilization: measurement of effect size and levels of action. Fertil Steril. 1994;62:807–814. doi: 10.1016/s0015-0282(16)57009-5. [DOI] [PubMed] [Google Scholar]
- Hughes EG, Brennan BG. Does cigarette smoking impair natural or assisted fecundity? Fertil Steril. 1996;66:679–689. doi: 10.1016/s0015-0282(16)58618-x. [DOI] [PubMed] [Google Scholar]
- Tuttle AM, Stämpfli M, Foster WG. Cigarette smoke causes follicle loss in mice ovaries at concentrations representative of human exposure. Hum Reprod. 2009;24:1452–1459. doi: 10.1093/humrep/dep023. [DOI] [PubMed] [Google Scholar]
- Macaluso M, Wright-Schnapp TJ, Chandra A, Johnson R, Satterwhite CL, Pulver A, Berman SM, Wang RY, Farr SL, Pollack LA. A public health focus on infertility prevention, detection, and management. Fertil Steril. 2010 doi: 10.1016/j.fertnstert.2008.09.046. 93:16:e1–e10. [DOI] [PubMed] [Google Scholar]
- Canadian Tobacco Use Monitoring Survey (CTUMS) 2011 Statistics Ottawa, ON: Health Canada; 2011 http://www.hc-sc.gc.ca/hc-ps/tobac-tabac/research-recherche/stat/ctums-esutc_2011-eng.php. Accessed 17 February 2015. [Google Scholar]
- Woodruff TJ, Zota AR, Schwartz JM. Environmental chemicals in pregnant women in the United States: NHANES 2003-2004. Environ Health Perspect. 2011;119:878–885. doi: 10.1289/ehp.1002727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Tobacco Use Monitoring Survey (CTUMS) 2012 Statistics Ottawa, ON: Health Canada; 2012 http://www.hc-sc.gc.ca/hc-ps/tobac-tabac/research-recherche/stat/ctums-esutc_2012-eng.php. Accessed 30 May 2015. [Google Scholar]
- Cohen B, Evers S, Manske S, Bercovitz K, Edward HG. Smoking, physical activity and breakfast consumption among secondary school students in a southwestern Ontario community. Can J Public Health. 2003;94:41–44. doi: 10.1007/BF03405051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baird DD, Wilcox AJ. Cigarette smoking associated with delayed conception. JAMA. 253:2979–2983. [PubMed] [Google Scholar]
- Gannon AM, Stämpfli MR, Foster WG. Cigarette smoke exposure leads to follicle loss via an alternative ovarian cell death pathway in a mouse model. Toxicol Sci. 2012;125:274–284. doi: 10.1093/toxsci/kfr279. [DOI] [PubMed] [Google Scholar]
- Sadeu JC, Foster WG. Effect of in vitro exposure to benzo[a]pyrene, a component of cigarette smoke, on folliculogenesis, steroidogenesis and oocyte nuclear maturation. Reprod Toxicol. 2011;31:402–408. doi: 10.1016/j.reprotox.2010.12.006. [DOI] [PubMed] [Google Scholar]
- Gannon AM, Stämpfli MR, Foster WG. Cigarette smoke exposure elicits increased autophagy and dysregulation of mitochondrial dynamics in murine granulosa cells. Biol Reprod. 2013;88:63. doi: 10.1095/biolreprod.112.106617. [DOI] [PubMed] [Google Scholar]
- Vazquez-Nin GH, Escobar ML, De Felici M, Echeverria OM, Kilinger FG. Cell Death in Mammalian Ovary Dordrecht, the Netherlands: Springer Netherlands; 2011. [Google Scholar]
- Inguscio V, Panzarini E, Dini L. Autophagy contributes to the death/survival balance in cancer photodynamic therapy. Cells. 2012;1:464–491. doi: 10.3390/cells1030464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Kundu M, Viollet B, Guan KL. AMPK. and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat Cell Biol. 2011;13:132–141. doi: 10.1038/ncb2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryter SW, Mizumura K, Choi AM. The impact of autophagy on cell death modalities. Int J Cell Biol. 2014;2014:502676. doi: 10.1155/2014/502676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botelho FM, Gaschler GJ, Kianpour S, Zavitz CCJ, Trimble NJ, Nikota JK, Bauer CMT, Stämpfli MR. Innate immune processes are sufficient for driving cigarette smoke-induced inflammation in mice. Am J Respir Cell Mol Biol. 2010;42:394–403. doi: 10.1165/rcmb.2008-0301OC. [DOI] [PubMed] [Google Scholar]
- Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- Ito S, Araya J, Kurita Y, Kobayashi K, Takasaka N, Yoshida M, Hara H, Minagawa S, Wakui H, Fujii S, Kojima J, Shimizu K, et al. PARK2-mediated mitophagy is involved in regulation of HBEC senescence in COPD pathogenesis. Autophagy. 2015;11:547–559. doi: 10.1080/15548627.2015.1017190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran I, Ji C, Ni I, Min T, Tang D, Vij N. Role of cigarette smoke-induced aggresome-formation in COPD-emphysema pathogenesis. Am J Respir Cell Mol Biol. 2015;53:159–173. doi: 10.1165/rcmb.2014-0107OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verschuere S, Allais L, Bracke KR, Lippens S, De Smet R, Vandenabeele P, Brusselle GGG, Cuvelier CA. Cigarette smoke and the terminal ileum: increased autophagy in murine follicle-associated epithelium and Peyer's patches. Histochem Cell Biol. 2012;137:293–301. doi: 10.1007/s00418-011-0902-3. [DOI] [PubMed] [Google Scholar]
- Park CH, Lee IS, Grippo P, Pandol SJ, Gukovskaya AS, Edderkaoui M. Akt kinase mediates the prosurvival effect of smoking compounds in pancreatic ductal cells. Pancreas. 2013;42:655–662. doi: 10.1097/MPA.0b013e3182762928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salem AF, Al-Zoubi MS, Whitaker-Menezes D, Martinez-Outschoorn UE, Lamb R, Hulit J, Howell A, Gandara R, Sartini M, Galbiati F, Bevilacqua G, Sotgia F, et al. Cigarette smoke metabolically promotes cancer, via autophagy and premature aging in the host stromal microenvironment. Cell Cycle. 2013;12:818–825. doi: 10.4161/cc.23722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ptak G, Zacchini F, Czernik M, Fidanza A, Palmieri C, Della Salda L, Scapolo PA, Loi P. A short exposure to polychlorinated biphenyls deregulates cellular autophagy in mammalian blastocyst in vitro. Hum Reprod. 2012;27:1034–1042. doi: 10.1093/humrep/der454. [DOI] [PubMed] [Google Scholar]
- Di Gioacchino M, Petrarca C, Perrone A, Farina M, Sabbioni E, Hartung T, Martino S, Esposito DL, Lotti LV, Mariani-Costantini R. Autophagy as an ultrastructural marker of heavy metal toxicity in human cord blood hematopoietic stem cells. Sci Total Environ. 2008;392:50–58. doi: 10.1016/j.scitotenv.2007.11.009. [DOI] [PubMed] [Google Scholar]
- Carlos SP De, Dias AS, Alberto L, Júnior F, Patricio PD, Graciano T, Nesi RT, Valença S, Meira A, Chiappa G, SouzaJr GC, De CT et al. Oxidative damage induced by cigarette smoke exposure in mice: impact on lung tissue and diaphragm muscle. J Bras Pneumol. 2014;40:411–420. doi: 10.1590/S1806-37132014000400009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardie DG. AMP-activated protein kinase-an energy sensor that regulates all aspects of cell function. Genes Dev. 2011;25:1895–1908. doi: 10.1101/gad.17420111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg GR, Kemp BE. AMPK in health and disease. Physiol Rev. 2009;89:1025–1078. doi: 10.1152/physrev.00011.2008. [DOI] [PubMed] [Google Scholar]
- Wang S, Zhang C, Zhang M, Liang B, Zhu H, Lee J, Viollet B, Xia L, Zhang Y, Zou MH. Activation of AMP-activated protein kinase α2 by nicotine instigates formation of abdominal aortic aneurysms in mice in vivo. Nat Med. 2012;18:902–910. doi: 10.1038/nm.2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley JK, Carayannopoulos MO, Wyman AH, Chi M, Ratajczak CK, Moley KH. The PI3K/Akt pathway is present and functional in the preimplantation mouse embryo. Dev Biol. 2005;284:377–386. doi: 10.1016/j.ydbio.2005.05.033. [DOI] [PubMed] [Google Scholar]
- Vivanco I, Sawyers CL. The phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat Rev Cancer. 2002;2:489–501. doi: 10.1038/nrc839. [DOI] [PubMed] [Google Scholar]
- Alers S, Löffler AS, Wesselborg S, Stork B. Role of AMPK-mTOR-Ulk1/2 in the regulation of autophagy: cross talk, shortcuts, and feedbacks. Mol Cell Biol. 2012;32:2–11. doi: 10.1128/MCB.06159-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemaître V, Dabo AJ, D'Armiento J. Cigarette smoke components induce matrix metalloproteinase-1 in aortic endothelial cells through inhibition of mTOR signaling. Toxicol Sci. 2011;123:542–549. doi: 10.1093/toxsci/kfr181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roach PJ. AMPK -> ULK1 -> autophagy. Mol Cell Biol. 2011;31:3082–3084. doi: 10.1128/MCB.05565-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripathi DN, Chowdhury R, Trudel LJ, Tee AR, Slack RS, Walker CL, Wogan GN. Reactive nitrogen species regulate autophagy through ATM-AMPK-TSC2-mediated suppression of mTORC1. Proc Natl Acad Sci U S A. 2013;110:E2950–E2957. doi: 10.1073/pnas.1307736110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galluzzi L, Vitale I, Abrams JM, Alnemri ES, Baehrecke EH, Blagosklonny MV, Dawson TM, Dawson VL, El-Deiry WS, Fulda S, Gottlieb E, Green DR, et al. Molecular definitions of cell death subroutines: recommendations of the Nomenclature Committee on Cell Death 2012. Cell Death Differ. 2012;19:107–120. doi: 10.1038/cdd.2011.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He H, Dang Y, Dai F, Guo Z, Wu J, She X, Pei Y, Chen Y, Ling W, Wu C, Zhao S, Liu JO, et al. Post-translational modifications of three members of the human MAP1LC3 family and detection of a novel type of modification for MAP1LC3B. J Biol Chem. 2003;278:29278–29287. doi: 10.1074/jbc.M303800200. [DOI] [PubMed] [Google Scholar]
- Cherra SJ, Kulich SM, Uechi G, Balasubramani M, Mountzouris J, Day BW, Chu CT. Regulation of the autophagy protein LC3 by phosphorylation. J Cell Biol. 2010;190:533–539. doi: 10.1083/jcb.201002108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawriluk TR, Hale AN, Flaws J, Dillon CP, Green DR, Rucker EB. Autophagy is a cell survival program for female germ cells in the murine ovary. Reproduction. 2011;141:759–765. doi: 10.1530/REP-10-0489. [DOI] [PubMed] [Google Scholar]
- Chen ZH, Kim HP, Sciurba FC, Lee SJ, Feghali-Bostwick C, Stolz DB, Dhir R, Landreneau RJ, Schuchert MJ, Yousem SA, Nakahira K, Pilewski JM, et al. Egr-1 regulates autophagy in cigarette smoke-induced chronic obstructive pulmonary disease. PLoS One. 2008;3:e3316. doi: 10.1371/journal.pone.0003316. [DOI] [PMC free article] [PubMed] [Google Scholar]