Abstract
Background
Current medical practice is grounded in a biomedical model that fails to effectively address multifaceted lifestyle and morbidogenic environmental components that are the root causes of contemporary chronic diseases. Utilizing the biopsychosocial (BPS) model in medical school training may produce competent healthcare providers to meet the challenge of rising chronic illnesses that are a result of these factors. This study explored the current trend of research on the utility of the BPS model in medical education and examined medical school curricula that have explicitly adopted the BPS model.
Methods
A systematic review of peer-reviewed literature was conducted on the BPS model and medical education since the 1970s using multiple databases. Descriptive analysis was used to illustrate findings regarding the trends of the BPS model in medical education and its utility in specific medical schools in the United States.
Results
Major findings illustrated a growing trend in research on the BPS model in medical education since the 1970s with literature in this area most visible since 2000. The same trend was established for the incorporation of psychosocial or behavioral and social science components in medical education. From our peer-reviewed literature search, only 5 medical schools featured utility of the BPS model in their curricula utilizing variable educational processes.
Conclusion
Although literature regarding the BPS model in medical education is growing, the explicit utility of the BPS model in medical school is limited. Our findings can stimulate educational processes and research endeavors to advance medical education and medical practice to ensure that future doctors can meet the challenge of rising lifestyle and environmental associated illnesses.
Keywords: Chronic disease, Lifestyle factors, Biopsychosocial model, Medical education, Curriculum
INTRODUCTION
In 2014, the World Health Organization (WHO) reported that non-communicable diseases make up for 88% of total deaths in the United States [1]. Non-communicable diseases include, but are not limited to obesity (35%), cardiovascular disease (31%), cancer (23%), and chronic respiratory diseases (8%) [1,2]. These diseases result from a multiplex of maladaptive health determinants including unhealthy dietary patterns, physical inactivity, tobacco use, and adverse psychosocial factors (e.g., chronic stress, lack of social support and community, and alienation). Most of the chronic diseases and disorders individuals experience are associated with multiple lifestyle and environmental factors that reinforce one another [3]. For example, metabolic syndrome among blue-collar workers is closely related to psychosocial factors, such as job stress, lack of social support, and risk perception, and if not managed properly, may lead to cardiovascular disease [4]. It is evident that a social factor like job loss can create perceived psychological as well as elevated physiological stress responses that lead to both chronic and acute health problems [5]. High levels of overall stress cause the release of the hormone cortisol, which can trigger increases in blood pressure, blood sugar, and even inflammation [6]. Job loss and its effects on the mind and body is just one of many cases explaining 21st century disease processes where one’s psychosocial factors are incorporated into his or her biological system.
It was reported that more than 50% of all primary health care visits in developed countries are due to these modern preventable and curable lifestyle-associated diseases [7]. This highlights the need for primary care physicians to be prepared to prevent or treat lifestyle-related multifactorial diseases that are mainly developed as a function of an adverse connection among biopsychosocial factors. In order to treat diseases that are affected by multiple lifestyle and morbidogenic environmental factors, it is important that physicians learn how to identify and address these factors. Multidisciplinary holistic medical training would allow physicians to accomplish this goal. However, the currently popular and widely used biomedical medical model embraces a more reductionist approach, which views health by its most basic components. The biomedical model treats health as the absence of disease or a physiological abnormality within the body. Furthermore, the model asserts that mental phenomena, such as emotional disturbance or delusions, are separate from and are unrelated to disturbances of bodily function [8]. In other words, the mainstream practice of medicine is highly focused on biological factors of illness and do not consider other lifestyle-related or psychosocial factors as significant as biomedical aspects.
In the late 1970s, psychologist George Engel pointed out various weaknesses in the biomedical approach to treating disease, of which three are highlighted here. First, a biochemical alteration does not translate directly into an illness. The appearance of illness results from the interaction of diverse causal factors, including those at the molecular, individual, and social levels. And the converse, psychological alterations may, under certain circumstances, manifest as illnesses or forms of suffering that constitute health problems, including, at times, biochemical correlates [9]. One study found that the risk for cardiovascular disease due to psychosocial stressors might be equal to previously established risk factors, such as hypertension and hypercholesterolemia, highlighting that psychosocial factors have an equal impact on health as do physiological disruptions [10]. Second, psychosocial variables are more important determinants of susceptibility, severity, and course of illness [9]. A study on irritable bowel syndrome found that alexithymia and the defectiveness schema appear to be directly related to both IBS and symptom severity [11]. Third, success of the most biological treatments is still influenced by psychosocial factors, for example, the so-called placebo effect [9]. The placebo effect is defined as “any improvement of symptoms or signs following a physically inert intervention,” and its effects are especially profound in relieving pain, anxiety, fatigue, and depression [12,13]. These critiques of the biomedical model stress the need for not only investigating pathology but also evaluating other external risk factors (psychological, sociological, or environmental) to provide the best level of care.
In response to the weaknesses in the biomedical model, Engel created a multidisciplinary approach to treating illness known as the “Biopsychosocial Model.” The biopsychosocial (BPS) model proposes that, in addition to the biological factors in the biomedical model of illness, psychological (which entails thoughts, emotions, and behaviors) and social (socio-economical, socio-environmental, and cultural) factors also play a significant role in human functioning in the context of disease [14]. The primary difference between the BPS model and the biomedical model is the integration of “psychosocial” factors, the same health determinants that have a large role in causing many non-communicable diseases or namely lifestyle diseases. The biomedical model design fails to address these additional factors related to one’s lifestyle profile and living environmental context, which is why physicians who utilize the BPS model are more likely to have patients with better health outcomes [15]. One meta-analysis found that approaching changes in lifestyle factors such as diet and exercise, which may not be fully addressed in the biomedical model, showed significant benefit in reducing the development of cardiovascular disease in patients with type 2 diabetes [16]. Furthermore, using a BPS approach versus a biomedical approach to treating low back pain appears to positively influence pain, functional status, and work performance [17]. In the study, there were two groups: conventional biomedical treatment and biopsychosocial treatment. The only difference between the groups was that in addition to the biomedical treatment, the BPS treatment group also included psychotherapy sessions three times per week and relaxation therapy four times per week. The incorporation of psychotherapy and relaxation interventions modified psychosocial factors and improved prognosis.
Given that 21st century modern disease patterns are affected by multifaceted lifestyle and morbidogenic environmental factors, it is necessary for physicians to utilize an evidenced biopsychosocial framework in addressing not only each of the factors independently but also the connections between the factors. The biopsychosocial model is a theorized framework that is designed to deal with the interplay between biological, psychological, sociological, environmental, and occupational components [9,14]. The view of connecting body, mind, behavior, and environment in the BPS Model is particularly endorsed by the new science of epigenetics in the context of understanding how health happens and disease occurs. The principles and increasing body of data on epigenetics have revealed evidence-based linkage between gene expressions and environment where one’s multifaceted lifestyle and morbidogenic environmental factors (e.g. eating habits, exercise, stress, sleep pattern, attitudes, beliefs, emotion, social relationship, neighbor, pollution, toxicity) are subject to alter the propensities and markers of epigenomes [18–26]. Thus, it would be important to recognize that simply addressing psychosocial factors or behavioral and social health components based on a traditional biomedical framework would be different from executing the whole course of patient care services including diagnosis, treatment, and management from utility of the conceptual framework of the integrative BPS model. The distinction lies in the importance given to each domain of factors (biological, psychological, social) and in whether psychosocial or behavioral and social components are treated as independent factors or integrated factors. Social factors (e.g., chronic stress, unemployment, socioeconomic factors, lack of social support and community, and alienation) and behavioral components (e.g., unhealthy dietary patterns, physical inactivity, and recreational drug use) are sometimes addressed in biomedical practice as psychosocial factors that are a separate entity in addition to the biomedical or physiological component of health [8,14]. Furthermore, in a biomedical framework that may also address psychosocial components, these additional health determinants are treated inferiorly to biochemical or physiological factors since the model’s foundation remains in biological factors. However, it is unclear as to how lifestyle-related disease factors are handled in the biomedical model with an additional psychosocial focus, as it does not provide a structure in the current practice for evaluating psychosocial factors. The BPS model, which is designed to treat all health determinants equally and as interacting health factors in a more structured framework, is now available to fill in the gap of the biomedical model [14]. It is thereby important to adopt an evidence-based approach in preventing and treating contemporary lifestyle-related health problems with 21st-century idealistic and comprehensive healthcare solutions method such as the BPS model.
Despite supporting evidence for its efficacy in medical practice, utility of the BPS model is limited in current medical practice. Most physicians acknowledge the need to address psychosocial issues and believe that addressing such factors would lead to improvements in outcomes [27]. However, a majority of physicians report not receiving effective training regarding the role of biopsychosocial factors and thus have feelings of low self-efficacy in addressing and managing biopsychosocial issues [28]. Furthermore, physicians reported that a lack of knowledge, time, and adequate reimbursement in practicing the psychosocial domain prevents them from addressing these issues. Because psychosocial factors are very common and powerful health determinants [29], these results suggest the need for more comprehensive medical training with focus on the BPS model approach in various education avenues especially including medical education when student doctors are trained.
It has been traditionally established that medical training remains grounded in the biomedical model [30]. US medical education is predominantly biomedical in focus, with most medical schools dedicating only a handful of hours to training in the BPS model [31]. According to a survey spanning from 1997 to 1999, study of behavioral and social science was estimated to comprise only about 10% of medical school curricula in US medical schools [32]. Another survey assessed residents’ perception of their readiness after completing medical school. Over 50% felt well prepared to be a resident, especially in taking a history and presenting a physical exam; however, they did not feel prepared for applied medical and psychosocial practices [33]. Although a majority of students and residents recognize the need to address psychosocial factors, 30%–40% believe that addressing such factors leads to minimal or no improvement in outcomes [34]. The majority of students and residents report that their training in these areas was ineffective and few indicate interest in receiving further training. It was reported that students are not much exposed to an opportunity to learn that lifestyle is the greatest determinant of health where multiple biopsychosocial factors are the core cause. Student doctors perceive that the psychosocial domain is outside the realm of physicians’ work, which may be due to a medical education that is grounded in the biomedical framework [35]. All this information raises questions as to whether or not medical schools are training future doctors to become competent health care providers to address and implement multifaceted lifestyle interventions based on the BPS model to meet the essential needs of health promotion, disease prevention, and therapeutic effect through variable education processes [36].
Clearly, in the traditional medical education approach, medical students are not being taught the efficacy of addressing biopsychosocial factors that are associated with developing chronic diseases or disorders, and they are not receiving training in this multifactorial holistic domain. It appears that ineffective medical school training without the BPS framework creates physicians who are unprepared to optimally treat multifactorial lifestyle diseases that are rising as a modern disease pattern in this 21st century. To address this ineffective training, a new model of medical school training needs to be implemented that addresses the interplay between the biological, psychological, and sociological determinants of health. The biopsychosocial approach to illness could further help students understand how a variety of factors can lead to the presentation of psychosomatic diseases that occur as a function of mind-body imbalance caused by integration of various psychosocial lifestyle practices and environmental circumstances [37]. The incorporation of the BPS model, which is designed to address such factors, should be utilized in medical school training so that medical students can be well prepared in addressing biopsychosocial issues when they encounter their patients who live with a multidimensional lifestyle including environmental factors.
Fifteen years ago, only 8% of the 62 U.S. medical schools that responded to a survey about their curricula reported that they had integrated programs of behavioral medicine using a BPS model [38]. However, there is no current information regarding the present status of implementing the BPS model in medical school curricula since 2000. The objectives of this review are to (1) investigate the current trends in the interest of adopting the BPS model in medical education in the United States and (2) examine which medical schools have specifically adopted the BPS model in their curricula.
MATERIALS AND METHODS
We conducted a systematic review of the peer-reviewed literature on medical education in the United States, the biopsychosocial model, psychosocial components, and the behavioral and social sciences. Corresponding to the first objective, we conducted two sets of data searches to determine the trends of implementing the BPS model in medical education. Our first search criteria used the following search terms: “biopsychosocial” “medical education,” and “United States.” This allowed us to find articles that discussed BPS model in medical education. Our second search criteria included “psychosocial,” “behavioral science,” and “social science” to find articles discussing incorporation of psychological and sociological components in medical school curricula, which include other methods besides the biopsychosocial model to teach medical students about additional external health determinants. Once we received our search results, we pooled them together and removed duplicates. PubMed and Scopus were the databases used for the first objective. Our search goes as far back as the 1970s, when George Engel first introduced the BPS model as a theoretical framework for medical practice.
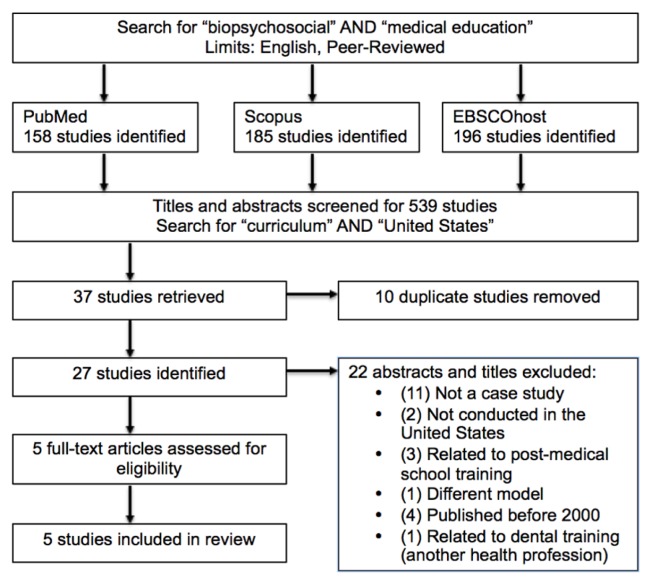
To address our second objective, we conducted a separate search using PubMed, Scopus, and EBSCOhost (which includes Academic Search Complete, ERIC, PsycINFO, PsycArticles, and MEDLINE) database sources to find peer-reviewed literature on medical schools featuring utility of the BPS model. The articles that were included in our study discussed how a specific medical school featured the BPS model in its curriculum in the manner of a case study. We used the following search terms: “biopsychosocial,” medical education,” “curriculum,” and “United States.” Because Objective 2 focused more on specific curricula as opposed to Objective 1, we used “curriculum” as a search term in addressing Objective 2 but not in addressing Objective 1. Once we received our search results, we pooled them together and removed any duplicates. Then, we selected articles based off inclusion and exclusion criteria, which are shown in Table 1. The process of article selection for the second objective is seen in Fig. 1.
Table 1.
Inclusion and exclusion criteria for systematic review of the literature on utility of a BPS model in medical school curricula
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Population |
|
|
| Study design and features |
|
|
| Descriptive data |
|
|
Fig. 1.
Flowchart of systematic review of study selection procedures.
The article search limits were that studies were conducted in the United States and were written in English. The search was conducted on September 10th, 2015.
RESULTS
1. Current trends regarding the BPS model and united states medical education
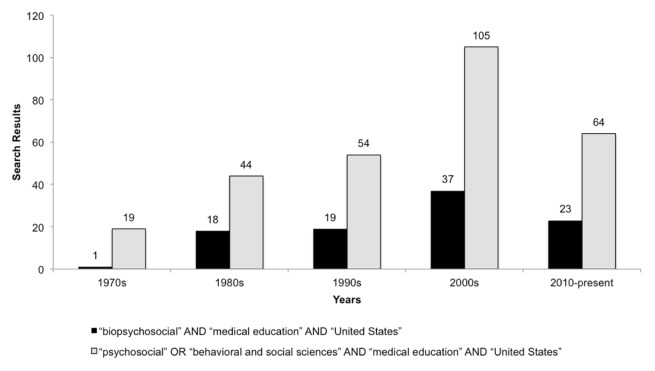
The findings from study analysis of Objective 1 reveal that there is a growing trend in peer-reviewed articles over time for the BPS model in medical education. Since the 1970s, the amount of peer-reviewed literature on the BPS model in medical education has increased with each decade. Since 2000, more research addressed the BPS model in medical education. Between January 2010 and September 2015, the amount of search results is nearly half of the previous decade. Furthermore, we found that there was almost a doubling in research articles between the 1990s and the 2000s. The same trends were found to be consistent regarding psychosocial, behavioral science, and social science components in medical education. Fig. 2 illustrates the amount of research available regarding the BPS model and psychosocial, behavioral science, and social science components in medical education. The articles that have been accounted for contain the search terms displayed in the legend of Fig. 2.
Fig. 2.
Search results for BPS model and psychosocial, behavioral and social components in medical education.
2. The medical school curricula featuring utility of the BPS model
From our literature search, the BPS model is utilized in the curricula of only five medical schools: Florida State University College of Medicine (FSU), University of California San Francisco School of Medicine (UCSF), University of California Davis School of Medicine (UC Davis), University of Rochester School of Medicine and Dentistry (URSMD), and University of Washington School of Medicine (UWSOM). Information regarding the way the schools organize their curricula is seen in Table 2. The mission, BPS competencies, teaching methods, and student assessment were all presented in the articles utilized from our search.
Table 2.
The medical school curricula featuring utility of the BPS model
| School | Mission | BPS competencies, themes, objectives | Teaching methods | Student assessment and evaluation |
|---|---|---|---|---|
| FSU Clinical Skills Curriculum [29] | This clinical skills curriculum is a continuum throughout the first three years, beginning with training in basic clinical skills, communication, history taking, and physical examination and progressing through training in diagnosis and management of complex medical problems in the third year. |
|
|
Written evaluations by staff and patients |
| UCSF General Curriculum [30] | The curriculum is organized into three stages spanning four years: the Essential Core, the Clinical Core, and Advanced Studies. “The interaction of biology and the environment in determining health” serves as the foundational theme for the new curriculum. |
|
|
|
| UC Davis Doctoring Curriculum [31] | The Doctoring Curriculum, which are longitudinal courses, takes place in the first three years of medical school. The skills and competencies required are increasingly more challenging throughout the curriculum. |
|
|
Standardized patient interviews |
| URSMD Palliative Care Curriculum [32] | In 1996, the University of Rochester School of Medicine formulated the Double Helix Curriculum, which integrated the basic sciences and clinical trainings over the four years of medical school. This curricular reform provided an opportunity to address the topic of palliative care in a fully integrated and comprehensive BPS curriculum. |
|
|
|
| UWSOM Pain Curriculum [33] | The current pain curriculum at UWSOM focuses on patient narrative, co-occurring BPS conditions and risks, common office-based primary care chronic pain conditions, and opioid, nonopioid, and nondrug treatments, with less attention to pain pathways, research design, and surgical and neuromodulatory interventions. 25 hours are spent on pain education at the UWSOM. |
|
|
|
The five medicals schools identified from this present study analysis feature the BPS model in various ways. Florida State University College of Medicine utilizes a four-year curriculum that is clinically focused from the beginning of medical school [39]. Psychosocial training is included in the form of clinical experiences, traditional lectures, and small group discussions. The University of California San Francisco School of Medicine organizes their four years into three phases and is not as clinically focused as FSU [40]. Instead, UCSF requires their students to conduct projects and “BPS discharge plans” in addition to attending lectures, and small group discussions. It also appears as though UCSF has a much more explicit utility of the BPS model as opposed to FSU.
UC Davis differs from both schools by incorporating the BPS model in a longitudinal course that runs throughout the entire four years that covers various topics, such as “Population Medicine and Prevention” and “Cultural Competency” [41]. In addition to lectures, large-group discussion panels, and small group case discussions, UC Davis also incorporates apprenticeships at a prison HIV ward, a local county juvenile hall, an in-home geriatric program, a psychiatric inpatient service, a pregnancy consultation center, the emergency room, and the inpatient nursing service. This allows medical students to observe the interactions between various disciplines in tending to the multiple factors of health and disease.
URSMD and UWSOM utilizes the BPS model in more specialized curricula as opposed to their general curricula. URSMD incorporates the BPS model in their specialized palliative care curriculum by having students attend BPS morbidity and mortality conferences and write structured BPS essays in a home-visit program in addition to lectures and small-group learning sessions [42]. UWSOM features a BPS model in their pain education curriculum by teaching students about co-occurring BPS conditions and risks in the form case presentations in the telemedicine format and the addition of more clinical scenarios throughout lectures [43].
DISCUSSION
The first objective of our study was to investigate the current trend of adopting the BPS model in medical education in the United States. From our search, we found that since its conception in the late 1970s, the BPS model has become more increasingly visible and discussed in research as it can be applied to medical education. The types of articles found during our search include empirical research, reviews, and conceptual discussions regarding the BPS model. The amount of literature has increased with each decade, with the most noted in the 21st century. Between January 2010 and September 2015, the amount of search results is nearly half of that of the previous ten years. Fig. 1 shows the number of search results from 2010-present. It is important that the current decade has not yet completed but much research has already been conducted these past five years. In fact, Fig. 1 shows that over half as many articles were published since 2010 in comparison to the previous decade. Furthermore, we found that there was almost a doubling in research articles between the 1990s and the 2000s. We predict that from these two latter findings that will be a doubling in research articles in this current decade as compared to the previous decade. In addition, we conducted a search on the incorporation of psychosocial or behavioral and social science components in curricula. We found that the same trend can be seen as that with the BPS model. The increasing trends in literature for both the BPS model and psychosocial factors suggests that psychosocial factors or behavioral and social factors such as inactivity, dietary patterns, stress, sleep, socioeconomic status, relationships, etc. are of interest to being taught during a student doctor’s medical education. Moreover, the increasing research trend on the BPS model in medical education indicates a possibility for its implementation at all levels of medical education. We foresee that research in medical education will continue to grow in relation to the BPS model and then will reflect increased education of and practice of the BPS model in healthcare services.
The second objective of our study was to examine schools that have adopted the BPS model in their curricula. Our literature search for medical school case studies retrieved five articles on five medical school curricula that feature a BPS model, with the most recent article published in 2013. Each school features and teaches the BPS model in a different way. FSU presents psychosocial information in traditional lectures, small-group discussions, and clinical experiences [39], while UC Davis utilizes apprenticeships to not only teach BPS but also inter-professional education [41]. Similarly, UWSOM features a telemedicine case presentation to teach students about co-occurring BPS conditions and risks [43]. Both URSMD and UCSF evaluate their students based on BPS structured essays and “discharge plans” [40,42]. This small sample of medical schools that utilize the BPS model utilize various teaching methods and evaluations of student performance. More information, such as student outcomes or student self-perceptions of addressing biopsychosocial illnesses after graduation, will be necessary to determine which schools optimally utilized a BPS model and to assess student doctors’ direct learning benefits. However, the articles selected for this study did not present this information.
The primary limitation in our study is that we only searched for medical school curricula in peer-reviewed literature. There may be many more medical schools that utilize the BPS model; however, there is no peer-reviewed literature to support that claim. This publication bias may be due to some medical schools that did not publish on their utility of the BPS model and are instead focused on its implementation.
From our study analysis, it appears that there is a limited utility of the BPS model in United States medical school education. There are currently 136 allopathic medical schools in the United States; however, we found only five medical school curricula featuring utility of the BPS model. The limited utility of the BPS approach in medical school parallels the limited amount of research available on the topic. According to our study, research in the area is still growing, as illustrated within the past 15 years, and needs to be continued. The limited research available on the BPS model in medical education could be due to it being younger concept, only having originated in the late 1970s, as compared to the biomedical model.
Our investigation has found that the trend of literature addressing the BPS model in medical education is growing; however, this trend has not actually been translated or applied to medical education. Perhaps, more time will be needed for widespread integration of the BPS model in medical schools across the United States as research continues to become more available on the efficacy and implementation of the BPS model. There is greater evidence of psychosocial components or behavioral and social sciences being addressed in medical education, which indicates that student doctors are learning about the role of these additional health factors. Many medical schools, however, may not specifically utilize a BPS model when presenting these additional factors in their curricula. Since there is limited research available regarding how these additional factors are presented in medical schools that do not feature a BPS model, we are not sure if students are learning about psychosocial factors as being separate from biological factors or if all of the factors are integrated in a BPS approach.
In reviewing curricular content across medical schools, it becomes evident that there is great variability in time spent covering psychosocial components or the behavioral and social sciences, teaching methods, timing of courses during a student’s medical education, and selected psychosocial topics to be discussed [23,44]. Currently, no national survey or database compiles information on the incorporation of psychosocial topics in medical school [44]. Having a database that shows schools’ educational processes including learning modalities, course topics, teaching methods, and evaluations can help provide a better view for improvements in incorporating the BPS model into medical education. This highlights the need for further research on how multifaceted lifestyle health determinants are being taught in medical school, what the barriers are to incorporating the BPS model, what are the resources of opportunities to facilitate implementation of the BPS model, and what are the outcomes for medical school graduates with a BPS medical education. Moreover, it is critical to examine holistic models, other than the BPS model, that can potentially produce doctors who make a significantly better impact regarding health outcomes and preventable diseases. Future investigation may also include conducting a questionnaire that is submitted to all of the allopathic and non-allopathic medical schools in the United States and asking how the schools incorporate a BPS model perspective or other holistic model that addresses lifestyle and environmental health factors.
Therefore, it is important to encourage further investigation and research in the area of medical education and training that can then be applied to provide future doctors with tools and approaches, such as the BPS model, to meet the challenge of rising chronic illnesses. The endeavors of our present study may contribute to medical practice that requires addressing and solving 21st century illnesses that result from multifaceted lifestyle and morbidogenic environmental factors.
REFERENCES
- 1.Noncommunicable diseases country profiles 2014. Geneva: World Health Organization; 2014. [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of Childhood and Adult Obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mcgue M, Skytthe A, Christensen K. The Nature of Behavioural Correlates of Healthy Ageing: A Twin Study of Lifestyle in mid to Late Life. International Journal of Epidemiology. 2014;43:775–82. doi: 10.1093/ije/dyt210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hwang WJ, Lee CY. Effect of Psychosocial Factors on Metabolic Syndrome in Male and Female Blue-collar Workers. Japan Journal of Nursing Science. 2012;11:23–34. doi: 10.1111/j.1742-7924.2012.00226.x. [DOI] [PubMed] [Google Scholar]
- 5.Huijts T, Reeves A, Mckee M, Stuckler D. The Impacts of Job Loss and Job Recovery on Self-rated Health: Testing the Mediating Role of Financial Strain and Income. The European Journal of Public Health. 2015 doi: 10.1093/eurpub/ckv108. [DOI] [PubMed] [Google Scholar]
- 6.Price RH, Choi JN, Vinokur AD. Links In The Chain Of Adversity Following Job Loss: How Financial Strain And Loss Of Personal Control Lead To Depression, Impaired Functioning, And Poor Health. Journal of Occupational Health Psychology. 2002;7:302–12. doi: 10.1037/1076-8998.7.4.302. [DOI] [PubMed] [Google Scholar]
- 7.Petterson SM, Liaw WR, Phillips RL, Rabin DL, Meyers DS, Bazemore AW. Projecting US Primary Care Physician Workforce Needs: 2010–2025. The Annals of Family Medicine. 2012;10:503–09. doi: 10.1370/afm.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wade DT, Halligan PW. Do Biomedical Models Of Illness Make For Good Healthcare Systems? BMJ. 2004;329:1398–401. doi: 10.1136/bmj.329.7479.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Borrell-Carrio F, Suchman AL, Epstein RM. The Biopsychosocial Model 25 Years Later: Principles, Practice, And Scientific Inquiry. The Annals of Family Medicine. 2004;2:576–82. doi: 10.1370/afm.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rozanski A, Blumenthal JA, Kaplan J. Impact of Psychological Factors on the Pathogenesis of Cardiovascular Disease and Implications for Therapy. Circulation. 1999;99:2192–217. doi: 10.1161/01.CIR.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 11.Phillips K, Wright BJ, Kent S. Psychosocial Predictors of Irritable Bowel Syndrome Diagnosis and Symptom Severity. Journal of Psychosomatic Research. 2013;75:467–74. doi: 10.1016/j.jpsychores.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Tavel ME. The Placebo Effect: The Good, the Bad, and the Ugly. The American Journal of Medicine. 2014;127:484–88. doi: 10.1016/j.amjmed.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 13.Colagiuri B, Schenk LA, Kessler MD, Dorsey SG, Colloca L. The Placebo Effect: From Concepts to Genes. Neuroscience. 2015;307:171–90. doi: 10.1016/j.neuroscience.2015.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Engel GL. The Biopsychosocial Model and the Education of Health Professionals. General Hospital Psychiatry. 1979;1:156–65. doi: 10.1016/0163-8343(79)90062-8. [DOI] [PubMed] [Google Scholar]
- 15.Margalit APA, Glick SM, Benbassat J, Cohen A. Effect of a Biopsychosocial Approach on Patient Satisfaction and Patterns of Care. Journal of General Internal Medicine. 2004;19:485–91. doi: 10.1111/j.1525-1497.2004.30059.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen L, Pei JH, Kuang J, Chen HM, Chen Z, Li ZW, Yang HZ. Effect of Lifestyle Intervention in Patients with Type 2 Diabetes: A Meta-analysis. Metabolism. 2015;64:338–47. doi: 10.1016/j.metabol.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 17.Schiltenwolf M, Buchner M, Heindl B, Reumont JV, Müller A, Eich W. Comparison of a Biopsychosocial Therapy (BT) with a Conventional Biomedical Therapy (MT) of Subacute Low Back Pain in the First Episode of Sick Leave: A Randomized Controlled Trial. European Spine Journal Eur Spine J. 2006;15:1083–092. doi: 10.1007/s00586-005-0008-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vickers MH. Early life nutrition, epigenetics and programming of later life disease. Nutrients. 2014;6:2165–2178. doi: 10.3390/nu6062165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim U, Song MA. Cancer Epigenetics. Humana Press; 2012. Dietary and lifestyle factors of DNA methylation; pp. 359–76. [DOI] [PubMed] [Google Scholar]
- 20.Sanchis-Gomar F, Garcia-Gimenez JL, Perez-Quilis C, Gomez-Cabrera MC, Pallardo FV, Lippi G. Physical exercise as an epigenetic modulator: Eustress, the “positive stress” as an effector of gene expression. The Journal of Strength & Conditioning Research. 2012;26:3469–72. doi: 10.1519/JSC.0b013e31825bb594. [DOI] [PubMed] [Google Scholar]
- 21.Collins A, Gutièrrez-Mecinas M, Trollope AF, Reul JM. Epigenetics of stress. Experimental Neurology. 2012:70–89. doi: 10.1016/j.expneurol.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 22.Amarasekera M, Prescott SL, Palmer DJ. Nutrition in early life, immune-programming and allergies: the role of epigenetics. Asian Pacific Journal of Allergy and Immunology. 2013;31:175–82. [PubMed] [Google Scholar]
- 23.Ho SM, Johnson A, Tarapore P, Janakiram V, Zhang X, Leung YK. Environmental Epigenetics and Its Implication on Disease Risk and Health Outcomes. ILAR Journal. 2012;53:289–305. doi: 10.1093/ilar.53.3-4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Migliore L, Coppedè F. Genetics, environmental factors and the emerging role of epigenetics in neurodegenerative diseases. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis. 2009;667:82–97. doi: 10.1016/j.mrfmmm.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 25.Gluckman PD, Hanson MA, Spencer HG, Bateson P. Environmental influences during development and their later consequences for health and disease: implications for the interpretation of empirical studies. Proceedings of the Royal Society of London B: Biological Sciences. 2005;272:671–7. doi: 10.1098/rspb.2004.3001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hou L, Zhang X, Wang D, Baccarelli A. Environmental chemical exposures and human epigenetics. International journal of epidemiology. 2011 doi: 10.1093/ije/dyr154. dyr154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Astin JA, Soeken K, Sierpina VS, Clarridge BR. Barriers to the Integration of Psychosocial Factors in Medicine: Results of a National Survey of Physicians. The Journal of the American Board of Family Medicine. 2006;19:557–65. doi: 10.3122/jabfm.19.6.557. [DOI] [PubMed] [Google Scholar]
- 28.Moser EM, Stagnaro-Green A. Teaching Behavior Change Concepts and Skills During the Third-Year Medicine Clerkship. Academic Medicine. 2009;84:851–58. doi: 10.1097/ACM.0b013e3181a856f8. [DOI] [PubMed] [Google Scholar]
- 29.Holmes SM. Fresh Fruit, Broken Bodies Migrant Farmworkers in the United States. 2008. [DOI] [PubMed] [Google Scholar]
- 30.McLean M, Gibbs TJ. Learner-centred Medical Education: Improved Learning or Increased Stress? Educ Health (Abingdon) 2009;23:287. [PubMed] [Google Scholar]
- 31.Novack DH. Realizing Engel’s vision: psychosomatic medicine and the education of physician-healers. Psychosom Med. 2003;65:925. doi: 10.1097/01.PSY.0000099944.98748.FC. [DOI] [PubMed] [Google Scholar]
- 32.Waldstein SR, Neumann SA, Drossman DA, Novack DH. Teaching Psychosomatic (Biopsychosocial) Medicine in United States Medical Schools: Survey Findings. Psychosomatic Medicine. 2001;63:335–43. doi: 10.1097/00006842-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 33.Chen C, Kotliar D, Drolet BC. Medical Education in the United States: Do Residents Feel Prepared? Perspect Med Educ. 2015;4:181–85. doi: 10.1007/s40037-015-0194-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Astin JA, Sierpina VS, Forys K, Clarridge B. Integration of the Biopsychosocial Model: Perspectives of Medical Students and Residents. Academic Medicine. 2008;83:20–27. doi: 10.1097/ACM.0b013e31815c61b0. [DOI] [PubMed] [Google Scholar]
- 35.Astin JA, Goddard TG, Forys K. Barriers to the Integration of Mind-Body Medicine: Perceptions of Physicians, Residents, and Medical Students. EXPLORE: The Journal of Science and Healing. 2005;1:278–83. doi: 10.1016/j.explore.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 36.Chisholm A, Hart J, Mann KV, Harkness E, Peters S. Preparing Medical Students to Facilitate Lifestyle Changes With Obese Patients. Academic Medicine. 2012;87:912–23. doi: 10.1097/ACM.0b013e3182580648. [DOI] [PubMed] [Google Scholar]
- 37.Novack DH, Epstein RM, Paulsen RH. Toward Creating Physician-healers: Fostering Medical Students’ Self-awareness, Personal Growth, and Well-being. Academic Medicine. 1999;74:516–20. doi: 10.1097/00001888-199905000-00017. [DOI] [PubMed] [Google Scholar]
- 38.Brook DW, Gordon C, Meadow H, Cohen MC. Behavioral medicine in medical education: report of a survey. Social Work in Health Care. 2000;31:15–29. doi: 10.1300/J010v31n02_03. [DOI] [PubMed] [Google Scholar]
- 39.Hurt MM, Harris JO. Founding a New College of Medicine at Florida State University. Academic Medicine. 2005;80:973–79. doi: 10.1097/00001888-200511000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Satterfield JM, Mitteness LS, Tervalon M, Adler N. Integrating the Social and Behavioral Sciences in an Undergraduate Medical Curriculum: The UCSF Essential Core. Academic Medicine. 2004;79:6–15. doi: 10.1097/00001888-200401000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Bourgeois JA, Ton H, Onate J, Mccarthy T, Stevenson FT, Servis ME, Wilkes MS. The Doctoring Curriculum at the University of California, Davis School of Medicine: Leadership and Participant Roles for Psychiatry Faculty. Academic Psychiatry. 2008;32:249–54. doi: 10.1176/appi.ap.32.3.249. [DOI] [PubMed] [Google Scholar]
- 42.Quill TE, Dannefer E, Markakis K, Epstein R, Greenlaw J, Mcgrail K, Milella M. An Integrated Biopsychosocial Approach to Palliative Care Training of Medical Students. Journal of Palliative Medicine. 2003;6:365–80. doi: 10.1089/109662103322144682. [DOI] [PubMed] [Google Scholar]
- 43.Tauben DJ, Loeser JD. Pain Education at the University of Washington School of Medicine. The Journal of Pain. 2013;14:431–37. doi: 10.1016/j.jpain.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cuff PA, Vanselow NA. Institute of Medicine (US) Committee on Behavioral and Social Sciences in Medical School Curricula. Washington (DC): National Academies Press (US); 2004. [PubMed] [Google Scholar]