Abstract
Introduction
Ultra-fast track anaesthesia aims at immediate extubation of cardiac surgical patients at the end of the operation. This study compares the effect of ultrafast track anesthesia versus continued postoperative mechanical ventilation on the intensive care unit length of stay.
Methods
Fifty-two elective adult patients were randomly allocated into ultrafast track anaesthesia and conventional groups by computer-generated random numbers. Redo operations, pre-operative intubation, uncontrolled diabetes, shock/left ventricular ejection fraction < 45%, pulmonary artery systolic pressure >55mmHg, creatinine clearance -1, haemodynamic instability, or those with concerns of postoperative bleeding were excluded. Pre- and intra-operative management was similar and Logistic EuroSCORE II was calculated for all. Intra-operatively, haemodynamic parameters, urine output, oxygen saturation, arterial blood gas analysis, 5-lead electrocardiogram, operative bypass- and cross-clamp time, and opioid consumption were collected. Postoperatively, patients were compared during their intensive care unit stay. Data were analysed by χ²/Fischer exact, unpaired student’s t-test, univariate two-group repeated measures with post hoc Dunnett's test, and Mann-Whitney U tests as appropriate. p < 0.05 was considered significant.
Results
Patients were comparable regarding their peri-operative characteristics and EuroSCORE. The intensive care unit stay was shorter in the ultrafast track anaesthesia group [57.4 (18.6) vs. 95 (33.6) h. p < 0.001], without increasing postoperative renal, respiratory complications rate or reopening rate.
Conclusions
In this single center study, ultrafast track anaesthesia decreased intensive care unit stay without increasing the rate of post-operative complications.
Keywords: cardiac anaesthesia, ultra fast track anaesthesia, ICU stay
Introduction
The question of whether early extubation leads to shorter post-operative length of intensive care unit (ICU) stay has rapidly gained importance over the past few decades considering the correlation between length of hospital stay and costs. Although some investigations did not find a difference between post-operative length of stay in early and late extubated patients, most observational studies and small randomized clinical trials showed significant benefits for early extubation [1,2,3,4,5] and few contraindications exist to the adoption of early extubation protocols. The most commonly cited indications for mechanical ventilation after cardiac surgery are significant hemodynamic instability that would require control of respiration, anticipated respiratory failure, central nervous system abnormalities and depressed level of consciousness affecting ventilatory drive or airway maintenance, anticipated continuing blood loss which may require a return to the operating room, and known difficult airway rendering emergency re-intubation hazardous [6].
Ultra-fast track anesthesia (UFTA) aims at immediate extubation of cardiac surgical patients at the end of the operation as typically these patients, presenting for either elective or emergent surgery, have adequate ventilatory function. In addition, it is worth considering that if those patients were not intubated and ventilated preoperatively in the first place, they are not likely to require prolonged mechanical ventilation afterwards [7].
The primary goal of this study was to assess the impact of adopting UFTA on the length of ICU stay of patients undergoing elective cardiac surgery. The incidence of complications during their ICU stay was recorded as secondary outcome.
Methods
From February, 2011, through October, 2013, 52 consecutive patients underwent open heart surgeries and were managed by the same anesthesiologists. Adult patients (>18yrs) scheduled for primary elective cardiac operations were included in the study.
Patients undergoing emergency/redo operations, patients already intubated preoperatively, patients with preoperative uncontrolled diabetes (HbA1C >5.9 mg/dL), cardiogenic shock, poor left ventricular function (ejection fraction (EF) < 45%), severe pulmonary hypertension (pulmonary artery systolic pressure (PASP) > 55 mmHg), severe renal impairment (creatinine clearance (CC) < 50 mL*min-1) or on regular dialysis, and patients deliberately kept intubated for hemodynamic instability and/or concerns of postoperative bleeding were excluded from the study.
Sample size calculation. Based on two-tailed α error probability of 0.05 and β error probability of 0.2 (power of 80%), a total sample size of 52 patients equally allocated into two groups was required to detect a presumed minimum clinically significant effect size d of 0.8 in length of ICU stay. Statistical power calculations were performed using computer program G*Power 3 for Windows. (Franz Faul, Universität Kiel, Germany).
Randomization. After approval of the institutional ethical committee and obtaining written informed consent, participants who met inclusion criteria and not exclusion criteria preoperatively were randomly allocated to either the UFTA group or conventional group using computer generated random numbers. Opaque sealed envelopes were used for concealment. The trial is registered in clinicaltrial.gov as NCT02491749.
Preoperative evaluation. Patients underwent the same preoperative examination and preparation according to our institution protocol. Routine preoperative investigations included complete blood picture, bleeding profile, liver and kidney functions tests, fasting blood glucose level, chest X-ray, twelve-lead electrocardiogram (ECG), transthoracic echocardiography, and coronary angiography if indicated. Logistic EuroSCORE II (European System for Cardiac Operative Risk Evaluation) was calculated for all participants. Patients in both groups received their usual medications, excluding oral hypoglycemic and angiotensin-converting-enzyme inhibitor and angiotensin receptor blockers, up to the time of surgery. Premedication with intravenous midazolam (1-3 mg) was given to patients upon arrival to the anesthesia bay, 20-30 min before admission to the operating room.
Intraoperative monitoring was achieved using standard 5-lead ECG, invasive arterial blood pressure, pulse oximeter, and nasopharyngeal temperature probe, and transesophageal echocardiography.
Conduct of anesthesia. Induction of anesthesia was performed with midazolam [0.03-0.05 mg/kg], fentanyl [1-2 µg/kg], and propofol [1-2 mg/kg]. Orotracheal intubation was facilitated by atracurium [0.5 mg/kg]. Anesthesia was maintained with sevoflurane titrated to an expired minimum alveolar concentration (MAC) between 1-1.5, and a continuous infusion of morphine at 10 to 20 µg/kg/h. Additional doses of fentanyl and atracurium were given as needed.
Standard median sternotomy was performed for all but one patient, who had mitral valve replacement through lateral thoracotomy. One patient had off-pump coronary artery bypass grafting.
Post bypass fluid balance was maintained with warmed lactated/acetated Ringer’s to maintain patient’s nasopharyngeal temperature above 35.5°C. Hemodynamic instability (defined as systolic blood pressure less than 90 mmHg and/or mean arterial pressure less than 60 mmHg), if encountered, was corrected with intravenous bolus doses of ?uids, table positioning, and/or norepinephrine boluses [4-8 µg per dose]. While closing the subcutaneous tissue, patients received intravenous paracetamol [15 mg/kg].
For UFTA group, at the completion of surgery, the inhalational anesthetic concentration was reduced gradually to 0.4 expired MAC. If patients met the preset extubation criteria (SpO2 > 95% with FiO2 < 0.6, ETCO2 < 50 mmHg, spontaneous respiratory rate < 24/min), and train of four (TOF) > 90%, residual muscle relaxation was antagonized with neostigmine and atropine [0.05 mg/kg and 0.02 mg/kg respectively]. The trachea was then extubated and oxygen was delivered via an open face mask [10 L/min] during the transfer from the operating theatre to the ICU. Patients were questioned about recall of intraoperative events 12 and 24 hours after surgery.
For patients in the conventional group, patients were transferred to the ICU intubated and sedated with propofol infusion [50-70 µg/kg/min] and morphine [10-20 µg/kg/hr] while mechanical ventilation was continued.
According to the local ICU protocol and after discontinuation of sedation, patients were judged eligible for extubation if they were awake and able to respond comprehensively to simple verbal commands, provided that they were hemodynamically stable and had normal ventilatory mechanics, acid-base status, PaO2, and PaCO2 at an inspired FiO2 of 0.4.
Postoperative pain control. Postoperative pain management was multimodal. Each patient received a combination of the following treatments: continuous intravenous morphine [10-20 µg/kg/hr], intravenous morphine on demand [0.05 mg/kg (if pain scored 4 or more on a 0 to 10 pain scale with lockout time of 10 min)], and intravenous paracetamol [15 mg/kg every 6 hours]. Pain was assessed with Visual Analogue Scale (VAS) every 6 hours for the first 24 hours of their ICU stay by the intensivist in charge.
Data collection. Preoperative data included 1) demographic data 2) preoperative diagnosis and comorbidities 3) preoperative investigations and 4) logistic Euro SCORE II.
Intraoperative hemodynamic parameters, urine output, arterial oxygen saturation (SpO2), arterial blood gas analysis (ABG), standard 5-lead ECG analysis with ST segment analysis, total operative time, cardiopulmonary bypass time, aortic cross clamp time, and total opioid consumption (fentanyl and morphine) were continuously recorded.
Postoperative data collected included: time to extubation (in hours); total length of ICU stay (in hours); pain score (assessed every 6 hours); total opioid requirements; incidence of complications, including reintubation, excessive mediastinal bleeding (defined as 400 mL in the 1st hour, 200 mL/hr for the first 6 hours, or a total drainage of 1000 mL at any time), need for reopening, and postoperative nausea and vomiting; incidence of postoperative ischemia, detected by ECG changes (ST segment elevation or depression), creatinine kinase (CK), creatinine kinase - myocardial band (CK-MB) and Troponin I; incidence of postoperative renal impairment, detected by a diminished urine output < 0.5 mL/kg/hr and/or rising creatinine level; incidence of respiratory dysfunction detected by ABG changes and decreased SpO2.
Statistical Analysis. Obtained data was presented as mean (SD), median (interquartile ranges), or numbers and percentages. Nominal variables were analyzed using Chi-squared (χ²) test or Fischer exact test as deemed appropriate. Continuous variables were analyzed using unpaired Student’s t-test or univariate two-group repeated measures analysis of variance (ANOVA) with post hoc Dunnett's test. Nominal and non-normally distributed variables were analyzed using Mann-Whitney U test. Statistical calculations were performed using Microsoft® Office Excel 2010 and SPSS 16.0 for windows. P value < 0.05 was considered statistically significant.
Results
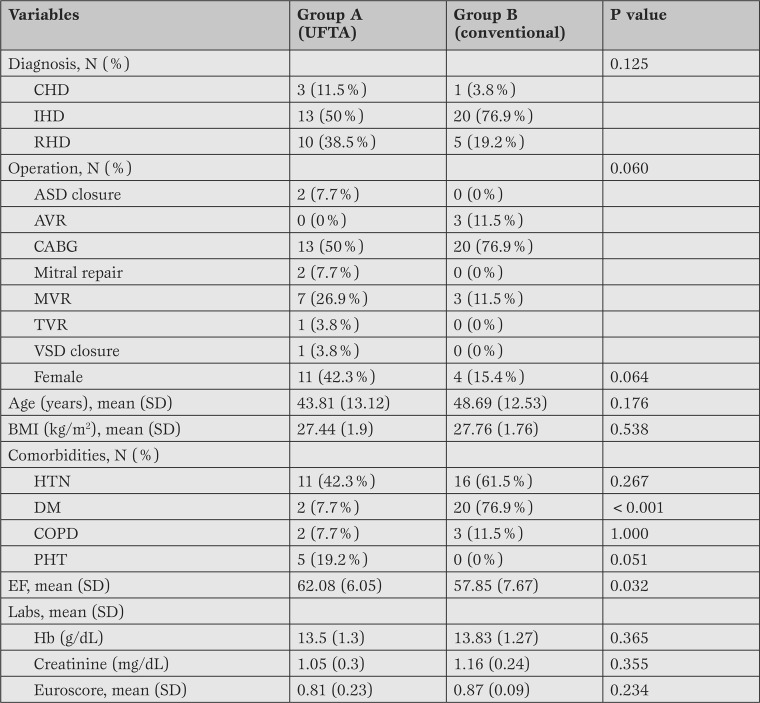
Fifty-two adult patients underwent cardiac operations, and were divided into 2 equal groups; UFTA group and conventional group. Baseline (Table 1) and surgical data (Table 2) were not well balanced.
Table 1.
Perioperative diagnosis, operation, demographic data, co-morbidities, and lab findings. Data are presented as number (percentages), mean (SD) as appropriate.
UFTA = ultra-fast track anesthesia; CHD = congenital heart disease; IHD = ischemic heart disease; RHD = rheumatic heart disease; ASD = atrial septal defect; AVR = aortic valve replacement; CABG = coronary artery bypass graft; MVR = mitral valve replacement; TVR = tricuspid valve replacement; VSD = ventricular septal defect; BMI = body mass index; SD = standard deviation; HTN = hypertension; DM = diabetes mellitus; COPD = chronic obstructive pulmonary disease; PHT = pulmonary hypertension; EF = ejection fraction; Hb = hemoglobin; Euroscore = European System for Cardiac Operative Risk Evaluation.
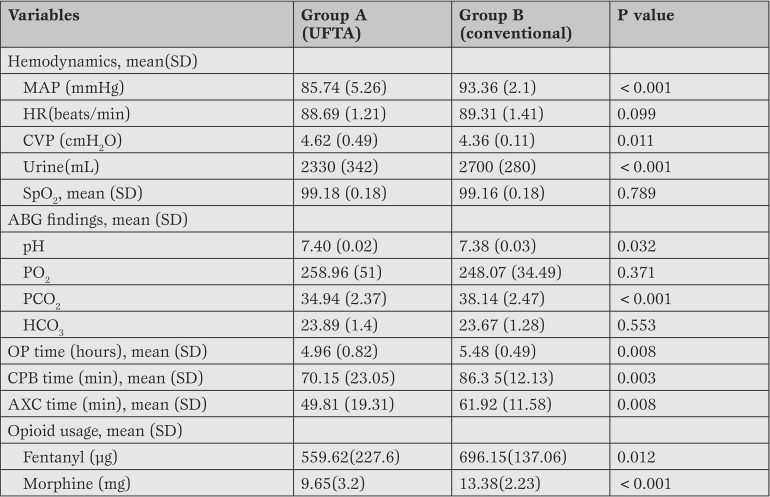
Table 2.
Intraoperative hemodynamics, ABG findings, intraoperative findings, and opioid usage. Data are presented as mean (standard deviation).
UFTA = ultra-fast track anesthesia; SD = standard deviation; MAP = mean arterial pressure; HR = heart rate; CVP = central venous pressure; SpO2 = arterial oxygen saturation; ABG = arterial blood gas; pH = power of hydrogen; PO2 = arterial oxygen tension; PCO2 = arterial carbon dioxide tension; HCO3 = bicarbonate; OP = operative; CPB = cardiopulmonary bypass; AXC = aortic cross clamp.
Patients of the conventional group received more morphine than patients of the UFTA group did [13.38 (2.23) vs. 9.65 (3.2) mg, respectively, p < 0.001] and more fentanyl [696.15 (137.06) vs. 559.62 (227.6) µg, respectively, p = 0.012] (Table 2).
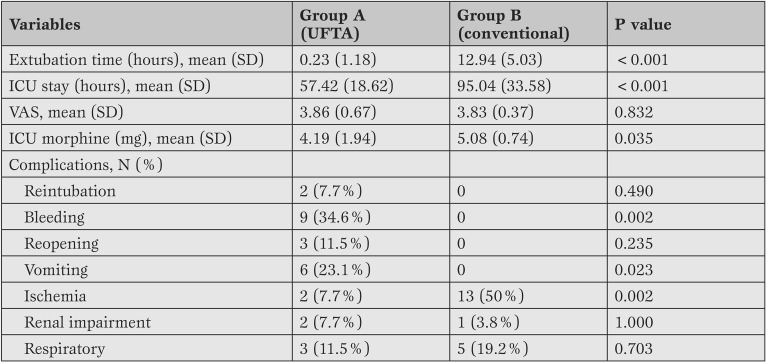
Postoperatively, there was a significant reduction in mean length of ICU stay between the UFTA and the conventional groups [57.42 (18.62) vs. 95.04 (33.58) h, p value < 0.001].
There was insignificant difference in the postoperative pain perception detected by VAS score between the 2 groups, albeit there was a significant difference in the ICU morphine consumption between the conventional and the UFTA groups [5.08 (0.74) vs. 4.19 (1.94) mg respectively, p = 0.035].
Postoperatively, nine patients in the UFTA group experienced increased chest tube drainage compared to none in the conventional group (p=0.002) with 3 of these patients requiring surgical re-exploration in the first postoperative day. Similarly, 6 patients in the UFTA group experienced postoperative vomiting while no patient in the conventional group did (p=0.23). Notably, there was a significant decrease in the incidence of postoperative ischemia in the UFTA group compared to the conventional group [2 vs. 13 patients respectively, p= 0.002].
In the UFTA group, only one patient failed to meet the extubation criteria and was maintained intubated because of lack of spontaneous ventilation at the end of surgery. He was extubated safely six hours postoperatively. Two patients in the UFTA group were reintubated and continued being sedated because of agitation and restlessness on arrival to the ICU. They received additional bolus doses of propofol [0.5 mg/kg] and concerns of their capability to maintain their airway patent was the cause for the decision of reintubation. These patients were extubated few hours later with no evidence of chest infection during their ICU stay. In comparison, no patients in the conventional group required reintubation (Table 3).
Table 3.
Postoperative ICU course, pain score, and postoperative complications. Data are presented as mean (standard deviation), frequency (percentage) as appropriate.
UFTA = ultra-fast track anesthesia; SD = standard deviation; ICU = intensive care unit; VAS = visual analogue score.
Discussion
In our study, UFTA with early tracheal extubation showed significant reduction in the length of ICU stay compared to conventional postoperative ventilation.
Several studies reported shorter ICU stay with UFTA with different designs and different population. Chamchad et al. [8] showed that immediate extubation was associated with a shorter ICU stay by an average of 23 hours. Similarly, Amirghofran et al. [9] retrospectively studied 2126 patients who had undergone cardiac operations among which 1833 patients underwent either immediate or early extubation. In a study of 2376 consecutive patients undergoing isolated off-pump coronary artery bypass grafting Edgerton et al. [10] observed that immediately extubated patients had shorter length of stay, a reduced incidence of atrial fibrillation, and reduced mortality independent of comorbidities.
In the context of our exclusion criteria, Borracci et al. [11] suggested that immediate extubation after on-pump and off-pump cardiac surgery should be avoided in patients with heart failure, left ventricular dysfunction, long cross-clamping time, pacemaker usage, hemodynamic compromise and difficult cardiopulmonary bypass weaning. The chances of requiring reintubation are increased if the patients are hemodynamically unstable, cold, hypovolemic or had considerable opioid medication.
In our study the conventional patient population suffered from postoperative ischemia more than patients in the UFTA group did. This finding differs from what Cheng et al. [12] reported. They reported insignificant difference regarding the incidence of myocardial ischemia, or CK-MB levels following 120 coronary artery bypass grafting surgeries albeit four patients in the conventional group, but not in the early group, had postoperative myocardial infarction. This difference could be attributed to the fact that 20 out of the 26 patients in the conventional group in our study were ischemic.
In the current study, three patients did not meet UFTA criteria whether at the end of surgery or early in the ICU and 2 patients were reintubated in the ICU. Similarly, a study by Rodriguez Blanco et al. [13] reported the incidence of unanticipated subsequent tracheal intubation in the ICU to be comparable to noncardiac high-risk procedures. In their study, two patients (2.5%) were subsequently re-intubated in the ICU out of the 78 patients extubated in the operating room. Safety concerns, psychological reluctance, and uncertainty about economic benefit stand as the factors to blame for abandoning early extubation strategy.
Postoperative pain perception, in our study, was comparable by VAS score between both groups although morphine usage significantly differed. Patients in the UFTA group required a mean (SD) morphine dose of 4.19 (1.94) mg, while the patients in the conventional group required a mean (SD) morphine dose of 5.08 (0.74) mg (p value = 0.035). It can postulated that patients in the conventional group required much higher analgesic dose to tolerate the stress of endotracheal intubation and mechanical ventilation. In agreement with our results, Amirghofran et al. [9], showed a significant difference in the dose of postoperative analgesics between those who had immediate or early extubation compared to those who did not.
Intraoperatively, there was a significant difference in the mean (SD) operative time between the UFTA and conventional groups, 4.96 (0.82) hours and 5.48 (0.49) hours respectively. There was a significant difference in the mean (SD) bypass time between the UFTA and conventional groups, 70.15 (23.05) min and 86.35 (12.13) min respectively. Also, there was a significant difference in the mean (SD) aortic cross clamp time between the UFTA and conventional groups, 49.81 (19.31) min and 61.92 (11.58) min respectively. This significant difference in intraoperative timings may be due to the more lengthy nature of CABG cases which was more prevalent in the conventional group.
A significant difference in the mean (SD) arterial blood pressure between the UFTA and conventional groups was also observed [85.74 (5.26) mmHg vs. 93.36 (2.1) mmHg, respectively]. This may be attributed to prevalence of hypertension among patients in the conventional group. Also, there was a significant difference in the mean (SD) volume of total urine output between the UFTA and conventional groups, [2330 ( 342 ) mL and 2700 ( 280 ) mL respectively] which may be a result of the increased time patients spent intraoperatively in the conventional group.
Regarding intraoperative opioid consumption, a significant difference in the mean (SD) amount of fentanyl used between the UFTA and conventional groups, [559.62 (227.6) µg and 696.15 (137.06) µg respectively]. Also, there was a significant difference in the mean (SD) amount of morphine used between the UFTA and conventional groups, [9.65 (3.2) mg and 13.38 (2.23) mg respectively]. This difference can be explained again by the prevalence of hypertension in the conventional group as well as the lengthy nature of their operations.
Based on the controversy regarding the benefits of epidural anesthesia [14], epidural anesthesia in the present study was discarded as a prerequisite to adopt UFTA technique in favor of the use of a balanced mixture of narcotics and non-opioid analgesics. This is in concert with the suggestion by Dorsa et al. [15] that epidural anesthesia is not essential in order to obtain optimal postoperative results with UFTA. Aiming at the same decent levels of pain relief and hemodynamic stability, the analgesic management in the current study was tailored with the combined effects of fentanyl, morphine and paracetamol. Technical and timing issues were much easier to manipulate compared to the use of TEA, and hemodynamic stability was not breeched.
Several studies reported predictors of UFTA feasibility. A study by Constantinides et al. [16], found 3 preoperative predictors for immediate extubation failure: previous renal failure, cardiac reoperation, and preoperative IABP (intra-aortic balloon pump) placement. Another study by Chamchad et al. [8] showed that postoperative renal failure, atrial fibrillation, and tracheal reintubation consistently predicted longer ICU duration and/or hospital length of stay.
In concert with the present results, Brucek et al. [17] reported the impact of total surgical time on UFTA feasibility. In their study, the authors included 547 patients who underwent coronary and/or valvular surgical procedure either with OPCAB or conventional CABG surgery. Intraoperative conversion to conventional CABG surgery was usually a marker of severe hemodynamic instability and was clearly associated with a worse clinical outcome. As expected, intraoperative conversion had been a strong predictor of immediate extubation failure [18].
Kandasamy et al. [19] also concluded that shorter AXC (aortic cross clamp) and CPB (cardiopulmonary bypass) times, uncontrolled arrhythmias, and absence of severe PHT were the factors found to be associated with early extubation. A recent study by Dorsa et al. [15] found, among other factors, three preoperative predictors for immediate extubation failure, standing as the main obstacle against it: previous renal failure, cardiac reoperation, and preoperative IABP placement. Additionally, diabetic patients had a higher risk for extubation failure, which is in agreement with the results reported by Constantinides et al. [16].
A recent study by Rodriguez Blanco et al. [13] stated that some preoperative variables (presence of EF ≥30% and hypertension) and intraoperative variables (off-pump, shorter surgical times) appeared to be associated with increased likelihood of extubation in the operating room. Even though the patients who were extubated in the operating room had statistically significant shorter CPB and AXC times, these factors were not found to be independent predictors of safe extubation in the operating room. Wong et al. [14] reported two preoperative variables (increased age and female gender) and four postoperative variables (usage of intra-aortic balloon pump, inotropes, excessive bleeding, and atrial arrhythmia) to be associated with delayed extubation.
Limitations
The small number of participants included in this single center trial is the main limitation of this study together with the unbalance in pre-randomization data. A large multicenter trial would offer more strength to build up a consensus about the feasibility of the concept of UFTA.
Conclusion
The implementation of UFTA protocol appeared to be feasible and safe in our single center study. It led to a significant reduction in the length of ICU stay of adult patients undergoing elective cardiac surgical operations, without significantly increasing postoperative complications.
Footnotes
Source of Support Nil.
Disclosures None declared.
Cite as: Salah M, Hosny H, Salah M, Saad H. Impact of immediate versus delayed tracheal extubation on length of ICU stay of cardiac surgical patients, a randomized trial. Heart, Lung and Vessels. 2015;7(4):311-319
References
- Montes F R, Sanchez S I, Giraldo J C, Rincón J D, RincÓn I E, Vanegas M V. et al. The lack of benefit of tracheal extubation in the operating room after coronary artery bypass surgery. Anesth Analg. 2000;91:776–780. doi: 10.1097/00000539-200010000-00003. [DOI] [PubMed] [Google Scholar]
- Berry P, Thomas S, Mahon S, Jackson M, Fox M, Fabri B. et al. Myocardial ischaemia after coronary artery bypass grafting: early vs late extubation. Br J Anaesth. 1998;80:20–20. doi: 10.1093/bja/80.1.20. [DOI] [PubMed] [Google Scholar]
- Bainbridge D, Cheng D. Initial Perioperative Care of the Cardiac Surgical Patient. Semin Cardiothorac Vasc Anesth. 2002;6:229–236. [Google Scholar]
- Cheng DC, Karski J, Peniston C, Raveendran G, Asokumar B, Carroll J. et al. Early tracheal extubation after coronary artery bypass graft surgery reduces costs and improves resource use. A prospective, randomized, controlled trial. Anesthesiology. 1996;85:1300–1310. doi: 10.1097/00000542-199612000-00011. [DOI] [PubMed] [Google Scholar]
- Lazar HL, Fitzgerald CA, Ahmad T, Bao Y, Colton T, Shapira OM. et al. Early discharge after coronary artery bypass graft surgery: are patients really going home earlier? J Thorac Cardiovasc Surg. 2001;121:943–950. doi: 10.1067/mtc.2001.113751. [DOI] [PubMed] [Google Scholar]
- Le TW, Jacobsoh E. Pro: tracheal extubation should occur routinely in the operating room after cardiac surgery. J Cardiothorac Vasc Anesth. 2000;14:603–610. doi: 10.1053/jcan.2000.9498. [DOI] [PubMed] [Google Scholar]
- Horswel JL, Herber MA, Princ SL, Mac MJ. Routine immediate extubation after off-pump coronary artery bypass surgery: 514 consecutive patients. J Cardiothorac Vasc Anesth. 2005;19:282–287. doi: 10.1053/j.jvca.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Chamcha D, Horro JC, Nachamchi L, Sutte FP, Samuel LE, Trac CL. et al. The impact of immediate extubation in the operating room after cardiac surgery on intensive care and hospital lengths of stay. J Cardiothorac Vasc Anesth. 2010;24:780–784. doi: 10.1053/j.jvca.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Amirghofra A, Rayatpishe M, Rayatpishe S, Kavian M. A comparative study of immediate and late extubation after open heart surgery. Int Cardiovascular Res J. Safranek. 2007;1:42–49. [Google Scholar]
- Edgerto JR, Herber MA, Princ SL, Horswel JL, Michelso L, Mage MJ. Reduced atrial fibrillation in patients immediately extubated after off-pump coronary artery bypass grafting. Ann Thorac Surg. 2006;81:2121–2127. doi: 10.1016/j.athoracsur.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Borracc RA, Dayá R, Rubi M, Axelru G, Ocho G, Rodrígue LD. [Operating room extubation (ultra fast-track anesthesia) in patients undergoing on-pump and off-pump cardiac surgery]. Arch Cardiol Mex. 2006;76:383–389. [PubMed] [Google Scholar]
- Chen DCH, Karsk J, Penisto C, Asokuma B, Raveendra G, Carrol J, e al.. Morbidity outcome in early versus conventional tracheal extubation after coronary artery bypass grafting: a prospective randomized controlled trial. J Thorac Cardiovasc Surg. 1996;112:755–764. doi: 10.1016/S0022-5223(96)70062-4. [DOI] [PubMed] [Google Scholar]
- Rodriguez Blanc YF, Candiott K, Gologorsk A, Tan F, Gique J, Barro ME. et al. Factors which predict safe extubation in the operating room following cardiac surgery. J Card Surg. 2012;27:275–280. doi: 10.1111/j.1540-8191.2012.01434.x. [DOI] [PubMed] [Google Scholar]
- Won DT, Chen DCH, Kustr R, Tibshiran R, Karsk J, Carroll-Munr J. et al. Risk factors of delayed extubation, prolonged length of stay in the intensive care unit, and mortality in patients undergoing coronary artery bypass graft with fast-track cardiac anesthesia: a new cardiac risk score. Anesthesiology. 1999;91:936–936. doi: 10.1097/00000542-199910000-00012. [DOI] [PubMed] [Google Scholar]
- Dors AG, Ross AI, Thiere J, Lupiañe B, Vranci JM, Vaccarin GN. et al. Consecutive Patients’: Feasibility, Safety and Predictors of When Not To Attempt It. J Cardiothorac Vasc Anesth. 2011;25:431–436. doi: 10.1053/j.jvca.2010.08.013. [DOI] [PubMed] [Google Scholar]
- Constantinide VA, Tekki PP, Fazi A, Kau K, Leonar R, Plat M. et al. Fast-track failure after cardiac surgery: Development of a prediction model. Crit Care Med. 2006;34:2875–2885. doi: 10.1097/01.CCM.0000248724.02907.1B. [DOI] [PubMed] [Google Scholar]
- Bruce PJ, Strak Z, Vane T, Jare M. Less Invasive Cardiac Anesthesia: An Ultra-Fast-Track Procedure Avoiding Thoracic Epidural Analgesia. Heart Surg Forum. 2003;E:107–110. [PubMed] [Google Scholar]
- Landon G, Pappalard F, Crescenz G, Alett G, Marchett C, Pol D. et al. The outcome of patients requiring emergency conversion from off-pump to on-pump coronary artery bypass grafting. Eur J Anaesthesiol. 2007;24:317–322. doi: 10.1017/S0265021506001578. [DOI] [PubMed] [Google Scholar]
- Kandasam A, Ramalinga SK, Simo HA, Arumugha S, Redd BD, Krupanand H. Ultra fast-tracking versus a conventional strategy in valve replacement surgery. Indian J Anaesth. 2013;57:298–300. doi: 10.4103/0019-5049.115567. [DOI] [PMC free article] [PubMed] [Google Scholar]