Extracorporeal Membrane Oxygenation (ECMO) is used in both children and adults to provide sufficient gas exchange until pulmonary parenchymal complications of pneumonia can heal [1]. The natural history of severe pneumonia can result in formation of empyema and abscess, as well as lung necrosis and cystic disease that can compress the normal parenchyma. In severer cases, these complications will not improve without surgical intervention. Patients on ECMO, who experience these complications, face additional risks for surgical treatment due to the requirement of anticoagulation.
We present two patients on ECMO treated for pneumonia refractory to medical therapy. Both patients had anticoagulation held prior to surgery, and both were restarted on heparin drips 24 hours after their resection. Anticoagulation was managed solely based on the Anti Factor Xa Assay, as per protocol [2]. To our knowledge, this is the first report of pulmonary parenchyma resection secondary to pneumonia treated surgically for patients on ECMO.
Two patients (ages 13 and 17 years) were transferred to our institution with severe necrotizing pneumonia and clinical sepsis. Both developed respiratory failure refractory to medical therapy and both were being treated with escalating inotropes for sepsis when they were cannulated for ECMO. As they recovered end organ function on ECMO, their pulmonary processes matured. Pulmonary infarct, abscess formation and cystic degeneration are demonstrated on imaging studies (Figure 1).
Figure 1.
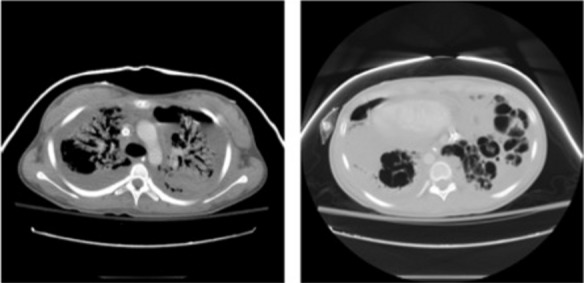
a) Axial image from a chest CT showing severe bilateral upper lobe consolidation with numerous air bronchograms, a loculated left hydropneumothorax and a loculated right pleural effusion. An ECMO cannula in the SVC is noted. b) A more caudal axial image demonstrates widespread cystic destruction of the lower lobe parenchyma representing necrosis. CT = computed tomography; ECMO = extracorporeal membrane oxygenation; SVC = superior vena cava.
Due to a prolonged failure to wean from ECMO support, bilateral thoracotomies were performed on each for abscess drainage, debridement of necrotic tissue, and resection of air/space cystic lung disease. One patient was extubated within 48 hours, and one within 10 days of their procedure. Each was eventually discharged home and was able to return to school. Follow-up chest radiograph showing near-complete resolution demonstrates the success of our endeavors (Figure 2).
Figure 2.

Posteroanterior chest X ray one year after discharge shows only minimal residual pleuroparenchymal scarring at the right lung base.
Footnotes
Source of Support Nil.
Disclosures None declared.
Cite as: Bressman M, Raad W, Levsky J, Weinstein S. Surgical therapy for complications of pneumonia on extracorporeal membrane oxygenation can improve the ability to wean patients from support. Heart, Lung and Vessels. 2015;7(4):330-331
References
- Zabrocki L A, Brogan T V, Statler K D, Poss W B, Rollins M D, Bratton S L. Extracorporeal membrane oxygenation for pediatric respiratory failure: Survival and predictors of mortality. Crit Care Med. 2011;39:364–370. doi: 10.1097/CCM.0b013e3181fb7b35. [DOI] [PubMed] [Google Scholar]
- Liveris A, Bello R A, Friedmann P, Duffy M A, Manwani D, Killinger J S. et al. Anti-factor Xa assay is a superior correlate of heparin dose than activated partial thromboplastin time or activated clotting time in pediatric extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2014;15:72–79. doi: 10.1097/PCC.0000000000000028. [DOI] [PubMed] [Google Scholar]


