Abstract
Objective
To evaluate the longitudinal effects of cochlear implantation (CIs) on young, deaf children’s social competence over 5 years of implant use and compare their social skills to those of same-aged, hearing peers.
Study Design
Prospective, longitudinal between- and within-subjects design, with assessments completed 3 times over 5 years.
Setting
This study was conducted at 6 cochlear implant centers and 2 preschools that enrolled both CI and hearing children.
Patients
Parents of 132 children with CIs and 67 age-matched hearing controls completed the study measures. Children were between 5 and 9 years of age at the first time point.
Interventions
Cochlear implantation and speech-language therapy.
Main Outcome Measures
3 subscales were drawn from 2 standardized measures of behavioral and social functioning, the Behavioral Assessment Scale for Children (Adaptability, Social Skills) and the Social Skills Rating System (Social Skills). A latent social competence variable was created using multiple subscales, which was modeled over time.
Results
Parent data indicated that children with CIs were delayed in comparison to their hearing peers on the social competence latent variable across all time points. Further, there was minimal evidence of “catch-up” growth over this 5-year period.
Conclusion
Children with CIs continued to experience delays in social competence after several years of implant use. Despite documented gains in oral language, deficits in social competence remained. To date, no interventions for children with CIs have targeted these social and behavioral skills. Thus, interventions that address the functioning of the “whole child” following cochlear implantation are needed.
Keywords: cochlear implants, social skills, social competence, parent ratings
INTRODUCTION
Social competence is a broad construct that reflects a child’s ability to interact effectively with people in the environment, such as peers, family members and other adults.1 It is defined as the ability to spontaneously utilize social skills in a flexible and adaptive manner.2 These social skills include reciprocity, perspective taking, complying with directions and rules, problem-solving, and responding to the actions of others.1,3,4 It also encompasses the ability to express emotions appropriately and exhibit self-control.5,6 Thus, social competence is fundamental to the establishment and maintenance of positive relationships.
Social competence has a profound effect on child development and facilitates family and peer relationships, emotion regulation, and academic achievement.7,8 Deficits have been shown to predict developmental outcomes, such as social anxiety, antisocial behavior, and later psychopathology.9,10 Children with hearing loss, who have delays in language, may be at increased risk for delays in social competence and related sequelae.11-15 The purpose of this study was to compare social competence over time in children with cochlear implants (CIs) and their hearing peers over 5 years.
Using a dynamic systems approach, psychologists have demonstrated that there are interconnections among different areas of development, and that deficits in one area can lead to cascading effects in others.16-18 Children with CIs, who have substantial delays in language development, are likely to experience deficits in several aspects of social competence, such as social skills, emotional awareness, and interpersonal problem-solving.11,19,20
Although the typical development of social competence has been extensively studied, few studies have evaluated social competence in school-age children with CIs.7,10,21,22 Nicholas and Geers used parent ratings of social competence on a deaf-specific measure (Meadow-Kendall Social-Emotional Assessment Inventory)23 and found that children with CIs performed better than the normative data. However, these findings should be interpreted with caution because the SEAI is outdated (i.e. published in 1983).24 The study compared the social functioning of deaf children born in late 1970’s and early 80’s to children born in the 2000’s. This is problematic because it does not account for the positive advancements in the treatment of childhood deafness, such as universal newborn hearing screening and the advent of cochlear implants.
In a more recent study, Moog and colleagues used the Social Skills Rating Scale and found no significant differences between adolescents with CIs and the normative sample on the Assertion, Cooperation, and Empathy subscales.25 These results should also be interpreted with caution; participants were recruited from a previous study and those who re-enrolled had higher speech perception, speech intelligibility, and reading scores than those who did not. Thus, this sample may not be representative of the CI population. It should also be noted that both of these previous studies used normative data rather than a hearing, control group. A matched, hearing control group would provide more realistic comparisons.
Prior research on social competence in deaf children is limited in other important ways, including: 1) failure to reflect the implementation of universal newborn screening, which has facilitated earlier diagnosis and intervention, or advances in cochlear implant technology,26,27 and,2) use of cross-sectional methods, limiting our understanding of the development of social competence in deaf children over time. In contrast, this study utilized data from a large, national study at 6 implant centers.28,29 This comprehensive, multisite dataset provided an opportunity to test our hypotheses, while avoiding the limitations of previous research. We utilized parent, rather than child ratings, because the children were too young to provide reliable data on these measures.
This is the first study to examine the longitudinal development of social competence in children with CIs. There were 3 primary aims. Aim 1 was to create a latent variable of social competence by combining parent ratings from 3 subscales from validated measures. Next, we evaluated whether these scales loaded onto a single, unitary construct. Confirmatory factor analyses (CFA’s) were then conducted across 3 time points evaluating both groups’ scores (i.e., 48, 72, 96 months post-implantation). CFA’s whether the relationships across the combined, observed variables are consistent with the a priori conceptualization of the latent variable, at each time point. It was hypothesized that the observed variables would successfully combine to form a latent variable across all 3 time points. Aim 2 was to compare social competence in children with CIs and their hearing peers using the latent variable we identified across time. It was hypothesized that the CI group would be delayed compared to the hearing group across all assessment points. Aim 3 was to compare of the trajectories of social competence between the CI and hearing groups at 3 time points over 5 years. It was hypothesized that children with CIs would display worse social competence at 48 months, but exhibit greater improvement in social skills than their hearing peers over time.
MATERIALS AND METHODS
Participants
Data for this study were drawn from a longitudinal study of developmental outcomes following cochlear implantation (CDaCI; NIH #DC004797), using data from the 48, 72, and 96-month assessments. The parent study evaluated numerous outcomes in deaf children before and after cochlear implantation, including receptive and expressive language, joint attention, psychosocial skills, and parent-child interactions.29-31 Participants were between the ages of 5 months and 5 years at enrollment; however, we used social functioning measures at later time points because children were then entering school and interacting more frequently with peers.
Criteria for inclusion in the CI group were: 1) severe to profound sensorineural hearing loss, 2) presence of a caregiver at evaluations, and 3) commitment to educate the child in spoken English. Children who were CI candidates were enrolled at 6 implant centers across the US prior to implantation (mean age at enrollment = 2.2 years). Age-comparable hearing controls were recruited from 2 preschool programs (mean age at enrollment = 2.3 years). See Fink et al., 2007 for a detailed description of the sample.28 For this study, participants with missing data at all 3 time points were excluded (CI n = 25, hearing n = 18); in addition, children diagnosed with a significant developmental or behavioral disorder following enrollment were also excluded (e.g., attention deficit hyperactivity disorder, autism spectrum disorder; CI n=31; hearing n=12). The control group had significantly higher levels of maternal education and parent income, however there were no differences between the samples on gender, and racial minority status (see Table 1; all comparisons were made using independent samples t-tests). At Baseline, children in the CI vs. hearing groups had lower average expressive language scores on the Comprehensive Assessment of Spoken Language, however, we did not control for language ability because it would likely remove variance associated with social competence. In contrast, all analyses controlled for maternal education and family income. Post-hoc analyses examined the effects of school placement and mode of communication. Thus, a total of 86 children from both groups were excluded from the analyses, yielding a sample of 132 CI and 67 hearing children.
Table 1.
Demographics and clinical characteristics of the sample
| Characteristic | Deaf Group (n = 132) |
Hearing Group (n = 67) |
T-test pvalue |
|---|---|---|---|
| Age at 48 months post-implantation (months) (SD) | 73.68 (14.54) | 74.54 (12.48) | .40 |
| Age of onset (months) (SD) | 1.78 (4.79) | -- | |
| Age at diagnosis (months) (SD) | 9.31 (9.30) | -- | |
| Length of hearing aid use before implant(months) (SD) | 11.90 (9.27) | -- | |
| Onset of hearing loss % (n) | |||
| Sudden | 3.79% (5) | -- | |
| Progressive | 33.33% (44) | -- | |
| Congenital | 56.07% (74) | -- | |
| Missing/Unknown | 6.81% (9) | -- | |
| Pure tone average in better ear (SD) | 103.78 (18.24) | -- | |
| Age at activation (months) (SD) | 28.39 (14.44) | -- | |
| Communication mode at 72 months % (n) | |||
| Sign language | 4.54% (6) | -- | |
| Simultaneous/equal emphasis | 3.03% (4) | -- | |
| Oral Language | 74.24% (98) | -- | |
| Missing/Unknown | 18.19% (24) | -- | |
| Composite IQ at baseline (SD) | 96.54 (24.62) | 105.55 (19.94) | >.01** |
| Language Scaled Score at 48 months (SD) | 77.38 (22.30) | 117.02 (18.18) | >.01** |
| Gender % (n) | .43 | ||
| Male | 45.45% (60) | 40.30% (27) | |
| Female | 54.55% (72) | 59.70% (40) | |
| Race % (n) | .06 | ||
| White | 74.24% (98) | 85.07% (57) | |
| African American | 6.82% (9) | 7.46% (5) | |
| Asian | 5.30% (7) | 0.00% (0) | |
| Other | 6.82% (9) | 5.97% (4) | |
| Not reported | 6.82% (9) | 1.50% (1) | |
| Ethnicity% (n) | .22 | ||
| Hispanic | 19.70% (26) | 11.95% (8) | |
| Non-Hispanic | 80.30% (106) | 88.05% (59) | |
| Maternal Education % (n) | >.01** | ||
| < High school | 4.54% (6) | 1.50% (1) | |
| High school graduate | 13.64% (18) | 2.98% (2) | |
| College | 81.82% (108) | 95.52% (64) | |
| Parents’ Income% (n) | >.01** | ||
| < $15,000 | 6.07% (8) | 2.99% (2) | |
| $15 – 29,999 | 10.60% (14) | 1.49% (1) | |
| $30 – 49,999 | 19.70% (26) | 2.99% (2) | |
| $50 – 74,999 | 18.18% (24) | 17.92% (12) | |
| $75 – 100,000 | 13.63% (18) | 13.43% (9) | |
| $100,000 + | 15.91% (21) | 50.74% (34) | |
| Declined/don’t know | 15.91% (21) | 10.44% (7) |
p <.05,
p<.01;
Procedures
Study visits were conducted over 1 or 2 days, depending on family schedules and travel burden. Questionnaires were mailed to parents prior to the scheduled visit, and were completed before the visit or on site. Children were assessed using measures of language, cognitive/executive functioning, and an audiological exam. Data for these analyses were drawn from the 48, 72 and 96-month follow-up assessments.
Measures
Behavior Assessment System for Children, Second Edition (BASC-2)
Social competence was measured, in part, using parent report on the BASC-2, a questionnaire used to evaluate the behavior and skills of individuals ages 2 to 21. These forms consisted of up to 160 questions.32 The parent form consisted of short statements (e.g. “adjusts well to new teachers”) that describe how the child behaves. The respondent rates the child’s behavior over the last several months using the response options of “never,” “sometimes,” “often,” or “almost always.”
To measure social competence, the subscales of Adaptability and Social Skills were utilized. For the Adaptability subscale, lower T-scores (mean = 50; SD = 10) indicated more difficulty, with those below 40 considered “At-Risk” and those below 30 “Clinically Significant.” The Adaptability subscale measures a child’s ability to act in a flexible and adaptive manner, a key component of social competence.2 Sample items included: “Adjusts well to new teachers” and “Adjusts well to changes in routine.” The Social Skills subscale measures prosocial behaviors that are developmentally expected. Sample items included: “Congratulates others when good things happen to them,” and “Encourages others to do their best.” For this scale, higher T-scores (mean = 50; SD = 10) indicated more difficulty, with those above 60 considered “At-Risk” and those above 70 “Clinically Significant.” Previous estimates of reliability have been strong (Cronbach’s alpha = .79 to .88). Internal consistency for this sample could not be calculated because the data were not available at the item level. The BASC-2 is a well-established instrument that has been used in many clinical studies.33-35 However, no previous studies have validated the BASC-2 in a sample of CI children.
Social Skills Rating System (SSRS)
Social competence was also measured using the Social Skills Rating System, a questionnaire assessing social behaviors in the classroom and with peers.6 The parent version consists of up to 40 items rated on a 3-point frequency scale (from “never” to “very often”), with an additional 3-point scale evaluating how important that behavior is to their child’s development, ranging from “not important” to “critical.”
The SSRS consists of 3 composite scales: Social Skills, Problem Behaviors, and Academic Competence. Only the Social Skills composite was utilized, which has 4 subscales: Cooperation, Assertion, Self-Control, and Responsibility. Each composite and subscale represents a series of specific behaviors, and scores are classified by their frequency of occurrence; “Fewer,” “Average,” or “More.” For example, a child who is classified as “More” on the Social Skills Scale is rated as exhibiting more positive social skills than the normative population.
Standard scores were generated based on age-appropriate normative data,, with 85 to 115 falling within the “Average” range. Those below 85 were within the Fewer range and those above 115 were within the More range. Previous estimates of reliability in the standardization sample of the parent report have been adequate to strong (Cronbach’s alpha = .65 to .95). Cronbach’s alpha could not be calculated for the individual subscales because item level data were not available.
Statistical Analysis Plan
For Aim 1, a latent social competence variable utilizing scales from the BASC and SSRS was created. CFAs of the latent variable were evaluated for significant factor loadings at all 3 time points using Mplus statistical software (version 6.0). Goodness of fit was examined using the comparative fit index (CFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). Missing data was handled using full-information maximum likelihood (FIML), which estimates parameters using all available data.36,37 Missing data was as follows: 14.57% at 48 months, 25.63% 72 months, and 28.14% at 96 months. The assumption of missing completely at random was met using Little’s test: X2 (132) =121.45, p >.05).
Aim 2 compared social competence between the CI and hearing groups at each time point. These differences were evaluated using analysis of variance (ANOVA), controlling for maternal education and income. Group means of the latent variable were compared at 3 time points. Cohen’s d analyses were used to evaluate the magnitude of differences between groups. This provided another method for ensuring that observed differences between groups were not due to type I error. Post-hoc ANOVAs were conducted to examine the effects of school placement and communication mode on social competence using the 72 month data. After removing those who were home schooled (n = 4), the remaining categories for school placement (i.e. mainstreamed, mainstreamed with pull-out classes, self-contained classroom in school for Deaf, self-contained classroom in mainstream school) were collapsed into 2 categories: mainstreamed (n = 15) vs. self-contained classroom (n = 117). Post-hoc analyses also examined the effects of mode of communication on social competence. Children with CIs were divided into 3 categories: sign language (n= 6), a combination of sign language/spoken language (n = 4), or spoken language (n = 98).
To evaluate the growth of social competence in CI and hearing children over a 5-year period, longitudinal modeling was used to plot the trajectory of social competence in both groups using data over time. Multiple Group Analysis was used to examine the fit of the models, with hearing status as a moderator (see Figure 1). All analyses controlled for income and maternal education.
Figure 1.
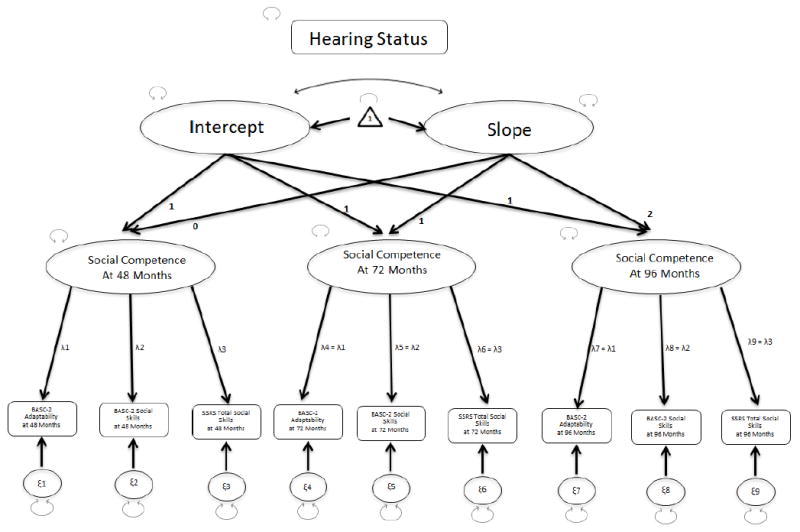
Theoretical longitudinal model of social competence using parent report
Note: This figure depicts the theoretical longitudinal model input into Mplus to generate the comparison of the latent social competence scores over time.
RESULTS
Confirmatory Factor Analyses
For Aim 1, it was hypothesized that all indicators of the latent social competence variable (the hypothesized, underlying factor that combines 3 observed variables) would load significantly onto a unitary construct across all time points. This hypothesis was fully supported at each time point. In other words, the observed variables were able to be statistically combined to form 1 underlying, latent variable at each time point. Given that all potential pathways between the variables for the latent construct were displayed in the model, the goodness-of-fit test was not required. Goodness-of-fit is a test that assesses whether the hypothesized relationships between the variables is similar to the relationships inferred from the data. In this study, all of the potential relationships between variables were hypothesized, thus goodness-of-fit did not need to be evaluated. See Table 2 for individual standardized factor loadings and correlations of each latent variable. All indicators had significant standardized factor loadings ranging from .67 to .87. By squaring the standardized coefficients, the amount of variance in the latent variable accounted for by each indicator was calculated, and ranged from 45% to 76%.
Table 2.
Results of confirmatory factor analyses at 48, 72, and 96 months post-implantation
| Children with CIs | Est. | SE | Sig. | % Var. Exp. |
|---|---|---|---|---|
| BASC Adaptability at 48 months | .67 | .05 | <0.01* | 49 |
| BASC Social Skills at 48 months | .78 | .04 | <0.01* | 61 |
| SSRS Social Skills at 48 months | .82 | .05 | <0.01* | 67 |
| BASC Adaptability at 72 months | .67 | .05 | <0.01* | 45 |
| BASC Social Skills at 72 months | .76 | .05 | <0.01* | 58 |
| SSRS Social Skills at 72 months | .80 | .05 | <0.01* | 64 |
| BASC Adaptability at 96 months | .67 | .05 | <0.01* | 49 |
| BASC Social Skills at 96 months | .78 | .05 | <0.01* | 61 |
| SSRS Social Skills at 96 months | .81 | .05 | <0.01* | 66 |
|
| ||||
| Hearing Children | Est | SE | Sig. | % Var. Exp. |
|
| ||||
| BASC Adaptability at 48 months | .72 | .07 | <0.01* | 52 |
| BASC Social Skills at 48 months | .87 | .06 | <0.01* | 76 |
| SSRS Social Skills at 48 months | .73 | .07 | <0.01* | 53 |
| BASC Adaptability at 72 months | .69 | .07 | <0.01* | 48 |
| BASC Social Skills at 72 months | .85 | .06 | <0.01* | 72 |
| SSRS Social Skills at 72 months | .70 | .07 | <0.01* | 49 |
| BASC Adaptability at 96 months | .70 | .07 | <0.01* | 49 |
| BASC Social Skills at 96 months | .86 | .05 | <0.01* | 73 |
| SSRS Social Skills at 96 months | .72 | .07 | <0.01* | 51 |
Statistically Significant Value
Comparisons of Social Competence at Each Time Point
Our hypothesis that CI children vs. hearing children would display significant delays on the latent social competence variable was fully supported. Controlling for maternal education and income, parents rated CI children as having significant delays in social competence at all time points (48 months: F(1, 190) = 6.82, p<.05, d = .46; 72 months: F(1, 190) = 7.89, p<.05, d = .48; 96 months: F(1, 190) = 7.58, p<.05, d = .47). Post-hoc analyses evaluated the effects of school placement and mode of communication on social competence. No differences were found on ratings of social competence between children in mainstreamed and self-contained classrooms at any point (48 months: F(1, 80) = 2.26, p >.05; 72 months: F(1, 80) = 2.00, p >.05; 96 months: F(1, 80) = 1.80, p >.05). Similarly, no differences were found on ratings of social competence between children who used sign language, a combination of sign/oral language, or oral language at any time point (48 months: F(2, 85) = 0.26, p >.05; 72 months: F(2, 85) = 0.25, p >.05; 96 months: F(2, 85) = 0.49, p >.05). However, note that this sample is quite small (n = 10).
Latent Growth Modeling
The hypothesis that children with CIs would display lower initial levels of social competence but would evidence greater improvement over time was partially supported. The default latent growth model demonstrated metric and scalar invariances across groups, with factor loadings across indicators constrained over time and across groups. The residual error variances and latent variances were free to vary. This model resulted in extremely poor model fit. Therefore, an adjusted default model was run in which the residual and latent variances within groups were constrained to be equal over time. Furthermore, the residual variances of the same observed variables were constrained to be equal over time (e.g. Adaptability at 48, 72, and 96 months).
Adding these constraints to the model created consistent measurement models across time in the latent variables. This model still yielded poor fit (X2 (58) =90.93, p <.05). To improve model fit, 2 residual covariances were added as suggested by the modification indices (See Figures 1 and 2 for path diagram). This model yielded significant improvement in model fit (X2 difference test (2) = 22.54, p <.05) and fit the data well, (X2 (58) = 70.67, p >.05; RMSEA = .047; CFI = .98). However, the SRMR value of .12 was above the suggested maximum of .08. This may be due to small sample size given that the SRMR value improves with larger samples.
Figure 2.
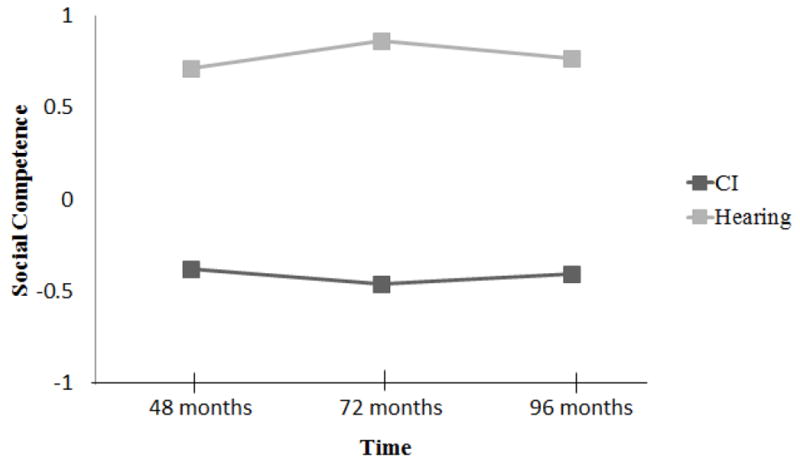
Results of longitudinal modeling of social competence
Note: This figure compares the mean scores of the latent social competence variable over time for children with CIs vs. hearing peers. Children with CIs, according to parent report, had social competence deficits compared to hearing peers at each time point (months after implantation) and demonstrated minimal evidence of “catch-up” growth.
According to the model, CI children had significantly lower levels of social competence at all time points compared to hearing children (differences between groups at 48 months = .47 points, p<.05; 72 months: .43 points, p<.05; 96 months: .73 points, p<.05). Although CI children had a steeper slope over time (.46 point increase per year compared to .42 unit increase per year in the hearing group), these slopes were not significantly different (p = .23) (See Figure 2).
DISCUSSION
This study evaluated the largest cohort of school-age children with CIs in the US and examined their trajectory of social competence over 5 years. Our study was the first to utilize a longitudinal design to examine social competence in children with CIs.25,38 The results strongly supported the dynamic systems model, which posits that deficits in one area of development have cascading effects on other areas.15,17,18 In particular, children with hearing loss, who have delays in language, may be at increased risk for delays in social competence and related developmental domains. Our results showed that children with CIs had significant delays in social competence across time compared to their hearing peers, even 8 years after implantation. These findings contradict previous studies of children with CIs, which found high ratings of social competence in relation to normative data.24,25 However, our study was the first to use multiple measures of social competence and a typically hearing control group.
This study had several limitations. First, children diagnosed with a developmental or behavioral disorder following enrollment were excluded to avoid confounds between the effects of the implant and comorbidities (e.g., autism). Thus, this sample was not representative of the entire CI population. Second, the hearing group had significantly higher levels of mean income and maternal education than the CI group. Although our analyses controlled for these differences, social competence may have been affected by other variables associated with economic advantage and this may have inflated the differences we found. However, there is previous literature supporting the deficits in social competence we found among the CI group.24-25 Third, parents of children with versus without hearing loss may have different perspectives, expectations, and biases that influence their ratings of their children’s social competence. However, it was not possible to measure these potential biases or control for them.
In contrast, this study had several strengths. First, it used data from a large, multisite sample that recruited families from varied races and ethnicities, increasing the generalizability of our results. Second, this study was the first to model social competence longitudinally, while all previous studies have used cross-sectional designs.25 Third, this study used a consensus definition of social competence as suggested by Cook and Oliver, allowing comparison of our results to similar studies, which used the same definition.3 Fourth, we utilized parent data because it was the most complete, was comparable to previous studies, and provided consistency in the rater across time (e.g., teachers changed each year).
The findings from this study have major clinical implications. Results suggested auditory remediation via CI does not generalize to other areas of development. Children who receive CIs require rehabilitation beyond surgery to achieve full recovery of developmental systems. Implant surgery only restores audition and does not foster catch-up growth in other developmental areas, including social competence. Children with CIs also experience delays in related domains, such as social problem-solving. Interventions that focus on the complex, multi-systemic development of the “whole child” are needed to address these deficits. Providing interventions for social competence may increase language skills in children with CIs given the emphasis on social interactions.39 Despite this need and the benefits of social skills interventions, none have been developed or tested in this population. Interventions that target the “whole child” across multiple areas of development are paramount to improving the quality of life for children with CIs.
Future directions include conducting in-depth studies evaluating social competence in children with CIs and identifying relevant intervention targets. For example an observational study that measures social exchanges between children with CIs and their hearing peers would provide a deeper understanding of the challenges these children are experiencing. In addition to their limited oral language skills, children with CIs have difficulty interpreting social cues, inhibiting impulsive responding, and expressing empathy.11
Another area for future research is identifying predictors of social competence. One variable that is likely to be strongly related to social competence is maternal sensitivity.30 Interactions with parents lay the foundation for the development of social skills, including turn-taking, sharing, compromising, and behavioral regulation. Given that hearing parents of deaf children have a “mismatch” in terms of their communication 31, it may be more challenging to model these early social behaviors. Lower maternal sensitivity has been found in this population in comparison to "matched" dyads (i.e., hearing-hearing) and this may partly explain the deficits in social competence observed in this study. Thus, training in sensitive parenting may also serve as an important target for research and early intervention.
Acknowledgments
The Childhood Development after Cochlear Implantation (CDaCI) Investigative Team was supported by Grant R0l DC004797 from the National Institute on Deafness and Other Communication Disorders. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Deafness and Other Communication Disorders or the National Institutes of Health.
Disclosures: This project was funded by the National Institute of Deafness and Other Communication Disorders
References
- 1.Waters E, Sroufe LA. Social competence as a developmental construct. Dev Rev. 1983;3(1):79–97. [Google Scholar]
- 2.Lillvist A, Sandberg A, Björck-Äkesson E, Granlund M. The construct of social competence-how preschool teachers define social competence in young children. Int J Early Child. 2009;41(1):51–68. [Google Scholar]
- 3.Cook F, Oliver C. A review of defining and measuring sociability in children with intellectual disabilities. Res Dev Disabil. 2011;32(1):11–24. doi: 10.1016/j.ridd.2010.09.021. [DOI] [PubMed] [Google Scholar]
- 4.Spence SH. Social skills training with children and young people: Theory, evidence and practice. J Child Adolesc Ment Health. 2003;8(2):84–96. doi: 10.1111/1475-3588.00051. [DOI] [PubMed] [Google Scholar]
- 5.Hogan AE, Scott KG, Bauer CR. The Adaptive Social Behavior Inventory (ASBI): A new assessment of social competence in high-risk three-year-olds. J Psychoeduc Assess. 1992;10(3):230–239. [Google Scholar]
- 6.Gresham FM, Elliot SN. Social Skills Rating System: Preschool, Elementary Level. Coral Pines, MN: American Guidance Service; 1990. [Google Scholar]
- 7.Semrud-Clikeman M. Social Competence in Children. New York, NY: Springer; 2007. [Google Scholar]
- 8.Spinrad TL, Eisenberg N, Cumberland A, et al. Relation of emotion-related regulation to children’s social competence: A longitudinal study. Emotion. 2006;6(3):498–510. doi: 10.1037/1528-3542.6.3.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hymel S, Rubin KH, Rowden L, LeMare L. Children’s peer relationships: longitudinal prediction of internalizing and externaliziing problems from middle to late childhood. Child Dev. 1990;61(6):2004–2021. [Google Scholar]
- 10.Ladd GW, Troop-Gordon W. The role of chronic peer difficulties in the development of children’s psychological adjustment problems. Child Dev. 2003;74(5):1344–1367. doi: 10.1111/1467-8624.00611. [DOI] [PubMed] [Google Scholar]
- 11.Barker DH, Quittner AL, Fink NE, et al. Predicting behavior problems in deaf and hearing children: the influences of language, attention, and parent-child communication. Dev Psychopathol. 2009;21(2):373–392. doi: 10.1017/S0954579409000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quittner AL, Smith LB, Osberger MJ, Mitchell TV, Katz DB. The impact of audition on the development of visual-attention. Psychol Sci. 1994;5(6):347–353. [Google Scholar]
- 13.Mitchell TV, Quittner AL. Multimethod study of attention and behavior problems in hearing-impaired children. J Clin Child Psychol. 1996;25(1):83–96. [Google Scholar]
- 14.Smith LB, Quittner AL, Osberger MJ, Miyamoto R. Audition and visual attention: The developmental trajectory in deaf and hearing populations. Dev Psychol. 1998;34(5):840–850. doi: 10.1037//0012-1649.34.5.840. [DOI] [PubMed] [Google Scholar]
- 15.Hoffman MF, Quittner AL, Cejas I. Comparisons of social competence in young children with and without hearing loss: A dynamic systems framework. J Deaf Stud Deaf Educ. 2015:115–124. doi: 10.1093/deafed/enu040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rubin KH, Burgess KB, Kennedy AE, Stewart S. Social withdrawal in childhood. In: Barkley EMR, editor. Child Psychopathology. New York, NY: Guilford Press; 2003. pp. 372–406. [Google Scholar]
- 17.Smith LB, Thelen E. A Dynamic Systems Approach to Development: Applications. Cambridge, MA: MIT Press; 1993. [Google Scholar]
- 18.Thelen E, Smith LB. A Dynamic Systems Approach to the Development of Perception and Action. Cambridge, MA: MIT Press; 1994. [Google Scholar]
- 19.Arnold D, Tremblay A. Interaction of deaf and hearing preschool children. J Commun Disord. 1979;12(3):245–251. doi: 10.1016/0021-9924(79)90045-5. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy CR, McCann DC, Campbell MJ, et al. Language ability after early detection of permanent childhood hearing impairment. New Engl J Med. 2006;354(20):2131–2141. doi: 10.1056/NEJMoa054915. [DOI] [PubMed] [Google Scholar]
- 21.Bar-On R, Parker JDA. The Handbook of Emotional Intelligence : Theory, Development, Assessment, and Application at Home, School, and in the Workplace. San Francisco, CA: Jossey-Bass; 2000. [Google Scholar]
- 22.Brown WH, Odom SL, McConnell SR. Social Competence of Young Children : Risk, Disability, & Intervention. Baltimore: Paul H Brookes Publishing Company; 2008. [Google Scholar]
- 23.Meadow-Orlans KP. Meadow/Kendall Social-Emotional Assessment Inventories for Deaf and Hearing-Impaired Students: Manual. Washington D.C: Gallaudet University; 1983. [Google Scholar]
- 24.Nicholas JG, Geers AE. Personal, social, and family adjustment in school-aged children with a cochlear implant. Ear Hear. 2003;24(1):69S–81S. doi: 10.1097/01.AUD.0000051750.31186.7A. [DOI] [PubMed] [Google Scholar]
- 25.Moog JS, Geers AE, Gustus C, Brenner C. Psychosocial adjustment in adolescents who have used cochlear implants since preschool. Ear Hear. 2011;32(1 Suppl):75S. doi: 10.1097/AUD.0b013e3182014c76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Antia SD, Kreimeyer KH. Social interaction and acceptance of deaf or hard-of-hearing children and their peers: A comparison of social-skills and familiarity-fased Interventions. Volta Rev. 1996;98(4):157–180. [Google Scholar]
- 27.Andersson G, Olsson E, Rydell AM, Larser HC. Social competence and behavioural problems in children with hearing impairment. Int J Audiol. 2000;39(2):88–92. doi: 10.3109/00206090009073058. [DOI] [PubMed] [Google Scholar]
- 28.Fink NE, Wang NY, Visaya J, et al. Childhood development after cochlear implantation (CDaCI) study: Design and baseline characteristics. Cochear Implants Int. 2007;8(2):92–116. doi: 10.1179/cim.2007.8.2.92. [DOI] [PubMed] [Google Scholar]
- 29.Niparko JK, Tobey EA, Thal DJ, et al. Spoken language development in children following cochlear implantation. Jama-J Am Med Assoc. 2010;303(15):1498–1506. doi: 10.1001/jama.2010.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quittner AL, Cruz I, Barker DH, et al. Effects of maternal sensitivity and cognitive and linguistic stimulation on cochlear implant users’ language development over four years. J Pediatr-Us. 2013;162(2) doi: 10.1016/j.jpeds.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quittner AL, Leibach P, Marciel K. The impact of cochlear implants on young deaf children - New methods to assess cognitive and behavioral development. Arch Otolaryngol. 2004;130(5):547–554. doi: 10.1001/archotol.130.5.547. [DOI] [PubMed] [Google Scholar]
- 32.Kamphaus RW, Reynolds CR. Behavior Assessment System for Children Second Edition: Behavioral and Emotional Screening System. Bloomington, MN: Pearson; 2007. [Google Scholar]
- 33.Mahan S, Matson JL. Convergent and discriminant validity of the Autism Spectrum Disorder-Problem Behavior for Children against the Behavioral Assessment System for Children, Second Edition. Res Autism Spect Dis. 2011;5(1):222–229. [Google Scholar]
- 34.Papazoglou A, Jacobson LA, Zabel TA. Sensitivity of the BASC-2 adaptive skills composite in detecting adaptive impairment in a clinically referred sample of children and adolescents. Clin Neuropsychol. 2013;27(3):386–395. doi: 10.1080/13854046.2012.760651. [DOI] [PubMed] [Google Scholar]
- 35.Kreisman NV, John AB, Kreisman BM, Hall JW, Crandell CC. Psychosocial status of children with auditory processing disorder. J Am Acad Audiol. 2012;23(3):222–233. doi: 10.3766/jaaa.23.3.8. [DOI] [PubMed] [Google Scholar]
- 36.Kline RB. Structural Equation Modeling. New York, NY: The Guilford Press; 2006. [Google Scholar]
- 37.Hancock GR, Mueller RO. Structural Equation Modeling: A Second Course. New York, NY: Lambert Academic Publishing; 2013. [Google Scholar]
- 38.Wiefferink CH, Rieffe C, Ketelaar L, Frijns JHM. Predicting social functioning in children with a cochlear implant and in normal-hearing children: The role of emotion regulation. Int J Pediatr Otorhinolaryngol. 2012;76(6):883–889. doi: 10.1016/j.ijporl.2012.02.065. [DOI] [PubMed] [Google Scholar]
- 39.Barnett MA, Gustafsson H, Deng M, Mills-Koonce WR, Cox M. Bidirectional associations among sensitive parenting, language development, and social competence. Infant Child Dev. 2012;21(4):374–393. doi: 10.1002/icd.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]


