Abstract
Objective
It is critical that pediatric residents learn to effectively screen families for active and addressable social needs (i.e., negative social determinants of health.) We sought to determine 1) whether a brief intervention teaching residents about IHELP, a social needs screening tool, could improve resident screening, and 2) how accurately IHELP could detect needs in the inpatient setting.
Methods
During an 18-month period, interns rotating on one of two otherwise identical inpatient general pediatrics teams were trained in IHELP. Interns on the other team served as the comparison group. Every admission history and physical (H&P) was reviewed for IHELP screening. Social work evaluations were used to establish the sensitivity and specificity of IHELP and document resources provided to families with active needs. During a 21-month post-intervention period, every third H&P was reviewed to determine median duration of continued IHELP use.
Results
619 admissions met inclusion criteria. Over 80% of intervention team H&Ps documented use of IHELP. The percentage of social work consults was nearly 3 times greater on the intervention team than on the comparison team (P<0.001). Among H&Ps with documented use of IHELP, specificity was 0.96 (95% CI 0.87–0.99) and sensitivity was 0.63 (95% CI 0.50–0.73). Social work provided resources for 78% of positively screened families. The median duration of screening use by residents after the intervention was 8.1 months (IQR 1–10 months)
Conclusions
A brief intervention increased resident screening and detection of social needs, leading to important referrals to address those needs.
Keywords: social determinants of health, socioeconomic factors, vulnerable populations, health status disparities, poverty
Socioeconomic status is one of the most important determinants of health in children.1–3 As many as 83% of pediatric patients in some primary care settings present with at least one major negative social determinant of health (such as unhealthy housing conditions or food insecurity.)4–6 Due to the impact of socioeconomic status on health, the Institute of Medicine recommends routine screening and data collection regarding social needs.7,8 In addition, the current pediatrics residency requirements of the Accreditation Council for Graduate Medical Education (ACGME) mandate advocacy training.9 Commentators have argued that this training should include screening for social needs and that the current pediatric social history does not adequately screen for social needs and must be improved. 10,11
Previously reported interventions have attempted to improve the ability of physicians to broadly screen for social needs. Screening instruments administered to parents prior to the physician encounter (such as in the waiting room) have been evaluated with respect to various social needs. 4,6,12–14 These instruments have been found to be effective in detecting social needs, were acceptable to parents, and resulted in increased social service referrals6,12 These instruments, however, may have requirements such as dedicated computers that limit their feasibility in certain medical contexts and are reliant on parental cooperation outside of the parent-provider interaction. In addition, most of the screening questions used in expanded social histories have not been previously validated.
Other studies have evaluated interventions teaching residents to improve their social histories15,16 or to identify and probe patient responses indicating possible unmet social needs.17 Those interventions often included multiple lectures over several weeks,16,17 did not demonstrate consistently increased referrals for unmet social needs,16 or did not evaluate whether the intervention’s effect faded over time.17 In order to address the ACGME’s requirement for competency in assessing and managing social needs, while remaining sensitive to work hour limits, a brief but intensive curriculum to train residents in screening patients for unmet social needs is needed.9,10
In this study, we sought to determine if a brief intervention, using multiple behavioral strategies to increase intervention intensity, could improve screening for social needs by pediatric residents. We also sought to determine the duration of resident screening for social needs over a prolonged study period, the validity of the screening in comparison to a full social work evaluation, and whether resources and referrals were made to correct the detected needs.
METHODS
Study Design, Population, Setting, and Period
We used a post-intervention only design with a usual-education comparison group. The intervention took place at Children’s Mercy Hospital, a 265-bed, freestanding children’s hospital with a pediatric residency program including a total of 106 pediatric and medicine-pediatric residents. All pediatric or medicine-pediatric interns were eligible for study participation. The intervention group consisted of interns rotating on one pre-selected inpatient general pediatrics team (“intervention team”). All interns on an otherwise identical inpatient general pediatrics team served as the comparison group (“comparison team”). Comparison team interns who had previously rotated on the intervention team during the study period were excluded from the comparison group analysis. However, if an intern had been on the comparison team and then later the intervention team, their data were treated as being on the comparison team during that month, and then as being on the intervention team when they started the intervention team rotation. Intervention and comparison team rotations were for 1 month in duration, and assignment to teams was not influenced by intern preferences. The intervention was conducted monthly for 18 months (July 1, 2011 – December 31, 2012). This study was approved by the Institutional Review Board at Children’s Mercy Hospital. Written informed consent was obtained.
Main Exposure
The intervention consisted of seven components and reflected 5 behavioral change strategies. Table 1 displays the intervention components by behavioral change strategy. Components 1–5 occurred during 2 brief meetings with interns on the intervention team. During the first meeting lasting approximately 20 minutes, interns met with a member of the study team, who explained the relationship between social needs and child health, critiqued the current standard for social history questions (e.g., household members, daycare), and described an expanded social history for detecting social needs. The expanded social history (“IHELP”) was derived from Kenyon et al.,11 and explores 8 domains of social needs (Table 2). A reference card listing the IHELP questions was attached to the intern’s hospital identification badge, where they were always accessible, and negated the need for these questions to be memorized. The IHELP method was briefly demonstrated and practiced through role-playing. Participating interns were told that IHELP represents a higher standard of care and were strongly encouraged to use it when admitting patients. The participating interns were told that the study team member would briefly follow up with them in 7–10 days; although this subsequent meeting (lasting <5 minutes) simply addressed any barriers or questions faced by the intern in using IHELP, the intern’s knowledge of the follow-up meeting provided an incentive to begin using the method.
Table 1.
Intervention components and associated behavioral change strategies.
| Intervention Component | Behavioral Change Strategy |
|---|---|
| 1. Teaching IHELP | Education/Providing Information |
| 2. Providing IHELP cards so that memorization was not required | Reducing Barriers |
| 3. Critique of current social history standard of care | Social normalization |
| 4. IHELP role playing | Enhancing skills |
| 5. Follow up meeting with interns 7–10 days after initial teaching session | Reducing Barriers (and Changing the Consequences) |
| 6. Starting rounds with “Are there any IHELP issues?” | Social normalization |
| 7. Attending comments of use of IHELP in two H&Ps for each intern during the 1 month rotation | Changing the Consequences |
Table 2.
Screening questions for social needs by domain using the IHELP social history method.
| IHELP Social Domain | Screening Questions | |
|---|---|---|
| Framing Statement | “Let me ask you some questions I ask every family.” | |
| I | Income | Do you have any concerns about making ends meet? |
| Insurance | Do you have any concerns about your child’s health insurance? | |
| H | Hunger | Do you have any concerns about having enough food? Have you ever been worried whether your food would run out before you got money to buy more?a Within the past year has the food you bought ever not lasted and you didn’t have money to get more?a |
| Housing | Do you have any concerns about poor housing conditions like mice, mold, cockroaches? Do you have any concerns about being evicted or not being able to pay the rent? Do you have any concerns about not being able to pay your mortgage? |
|
| E | Education | Do you have any concerns about your child’s educational needs? |
| Ensuring Safety (Intimate Partner Violence) | From speaking to families, I have learned that violence in the home is common and now I ask all families about violence in the home. Do you have any concerns about violence in your home?b | |
| L | Legal Status (Immigration) | What hospital was your child born in? If not in U.S.: Are you aware that your child may be eligible for benefits even though they were not born in the U.S.? If you would like, I can have a social worker come talk to you about some possible benefits your child may be eligible for. Would you like me to do that? |
| P | Power of Attorney & Guardianship | Are you the biological or adoptive mother or father of this child? If not: “Can you show me the power of attorney or guardianship document you have? |
Hager ER, Quigg AM, Black MM, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–e32.
The screening question for intimate partner violence is not asked if other individuals are present in the room, including the patient if he or she is verbal. Thackeray JD, Hibard R, Dowd MD. Intimate partner violence: The role of the pediatrician. Pediatrics. 2010; 125(5):1094–1100.
In the sixth component of the intervention, the intervention team’s attending physicians agreed to start rounds each morning with the question, “Are there any IHELP issues on any of our patients?” This question, asked prior to the start of family-centered rounds, replaced the usual question, “Are there any social issues on any of our patients?” Doing so provided a daily explicit reminder of IHELP, creating a social norm and expectation for IHELP use, and elevating the role of “social issues” to health-related social needs. In the seventh component of the intervention, intervention team attending physicians would critique the presence or absence of IHELP in the social histories of the interns when conducting their usual in-person feedback of two admission history and physicals (H&P) each month. This provided additional incentives and reinforcement of the IHELP method.
During the study period, the social history section of admission history and physicals (H&P) were written using free text. There were no prompts for either writing a social history or any specific elements within a social history. Interns had the ability, however, to create templates for writing H&Ps.
Main Outcomes
Use of the IHELP Social History Method (“Adoption”)
Every admission H&P to the intervention and comparison teams during the study period was reviewed. An H&P was included in the analysis if it was written by a participating intervention team intern after the first IHELP teaching session or was written by a comparison team intern. An H&P was excluded if the patient had been previously admitted to the intervention team during the study period or if the patient was initially admitted to a different inpatient team during the same hospitalization (e.g., intensive care unit), then transferred to the intervention or comparison team. Each H&P was reviewed for the presence or absence of each of the IHELP domains listed in Table 2, the number of IHELP social needs documented, and whether the H&P’s assessment and plan indicated that a social work (SW) consult would be placed.
Continued Use of IHELP after Leaving the Intervention Team (“Maintenance”)
In order to determine if intervention interns continued to use IHELP after leaving the intervention team, the H&P’s for every third admission to the study site during a 21-month maintenance period (July 2011 – March 2013) were reviewed. Maintenance of IHELP was defined as the use of IHELP in an H&P (dichotomous). The maximum possible duration of IHELP maintenance ranged from 3 months (for December 2012 intervention team interns) to 20 months (for July 2011 intervention team interns.)
Validity of IHELP & Resources Provided
For every intervention team H&P where the intervention intern screened for unmet social needs, the screen was compared against a full social work evaluation performed during the hospital stay. All inpatient social work evaluations were completed by inpatient, master’s degree-level social workers. Due to staffing, logistical (e.g., early patient discharge), and other limitations, social work evaluations could be completed for only about half of intervention team admissions. Two members of the study team who are also master’s degree-level inpatient social workers (BN and SD) independently scored the first 20 admissions with social work evaluations, demonstrating perfect inter-rater agreement (kappa=1.0). Thereafter, any social work evaluation with possible detection of an unmet need or provision of assistance for a social need were reviewed by one social work study team member. They recorded whether the inpatient social work evaluation detected one of the social needs listed in Table 2. In addition, actions taken by the consulting social worker to address that need were categorized as (1) resource or referral given, (2) family already appropriately addressing the need, (3) no resources/referrals available for this need, or (4) family refused help for this need. Sensitivity, specificity, and positive and negative predictive values were calculated for admissions using the social work evaluation as the gold standard. A social work evaluation and intern IHELP screen were considered positive and in agreement if any domain was positive. The percentage of social work evaluations and IHELP screens matching for the specific domain was also determined.
Other Covariates
Data on intern demographics, education, and career plans were collected from a survey of all residents administered as a part of a separate research project. Patient characteristics were collected from the Pediatric Health Information System database, which is an administrative database of 43 free-standing children’s hospitals. For each inpatient discharge, the database contains data on patient demographics, length of stay, and up to 41 International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnoses and 41 ICD-9-CM procedures. Quality of data is ensured though a collaboration of Children’s Mercy Hospital, the Children’s Hospital Association (Overland Park, KS), and Truven Health Analytics (Ann Arbor, MI) and has been described elsewhere.18,19 Patient demographics included age, gender, race, ethnicity, and primary insurance. ICD-9-CM codes were used to identify patients with a complex chronic condition using a previously described classification method.20
Statistical Analysis
Univariate statistics were used to describe the demographic and clinical characteristics of intervention and comparison team patients and interns. Univariate statistics were also used to describe the percentage of H&Ps using IHELP, the mean number of IHELP domains used per H&P, the number of social works consults, the percentage of social work consults confirming the resident-identified social need, and the percentage of patients receiving resources by the consulting social worker. The chi-square test was used to compare categorical demographic and clinical characteristics of intervention and comparison patients and interns as well as intervention and comparison teams’ use of IHELP and social work consults. The Mann-Whitney U test was used to compare intervention and comparison team continuous demographic and clinical characteristics and the number of IHELP domains used per H&P. Median duration of IHELP use after leaving the intervention team was determined using life tables.
RESULTS
Intern and Patient Characteristics
During the 18-month intervention period, 100% of eligible interns were enrolled (N = 43 on the intervention team, N = 44 on the comparison team). Demographics, medical education, and career plans of intervention and comparison team interns were similar (Table 3). A total of 619 admission H&Ps met the inclusion criteria (Table 3). There were no differences in the demographic and clinical characteristics of patients admitted to either team (Table 3). The majority of patients were male, non-Hispanic, white, and on government insurance (58.0%). One-quarter of patients had a complex chronic condition.
Table 3.
Characteristics of Intervention and Comparison Team Interns and Patients.a
| Total n (%) | Intervention Team, n (%) | Comparison Team, n (%) | ||
|---|---|---|---|---|
| Intern Characteristics | ||||
| Number of Interns | 87 (100.0) | 43 | 44 | |
| Median Age, years, (IQR) | 27 (26, 28) | 27 (27, 28) | 27 (26, 28) | |
| Gender, female | 59 (67.8) | 30 (69.8) | 29 (65.9) | |
| Fellowship planned, yes | 41 (49.4) | 22 (52.4) | 19 (46.3) | |
| Attended medical school in Kansas City | 32 | 14 (32.6) | 18 (46.2) | |
| Patient Characteristics | ||||
| Number of Patients | 619 (100.0) | 347 (56.1) | 272 (43.9) | |
| Median Age, years, (IQR) | 3 (0, 8) | 2 (0, 8) | 3 (1, 9) | |
| Gender, female | 288 (46.5) | 160 (46.1) | 128 (47.1) | |
| Ethnicity, Hispanic | 91 (14.7) | 55 (15.9) | 36 (13.2) | |
| Race | Non-Hispanic white | 337 (54.4) | 191 (55.0) | 146 (53.7) |
| Non-Hispanic black | 138 (22.3) | 75 (21.6) | 63 (23.2) | |
| Asian, Pacific Islander, Native American | 9 (1.5) | 5 (1.5) | 4 (1.5) | |
| Other | 135 (21.8) | 76 (21.9) | 59 (21.7) | |
| Insurance | Government | 359 (58.0) | 208 (59.9) | 151 (55.5) |
| Private/commercial | 229 (37.0%) | 123 (35.4) | 106 (39.0) | |
| Other | 18 (2.9) | 10 (2.9) | 8 (2.9) | |
| Unknown | 13 (2.1) | 6 (1.7) | 7 (2.6) | |
| Complex Chronic Condition, yes | 140 (22.6) | 81 (23.3) | 59 (21.7) | |
| Length of Stay, days, median (IQR) | 2 (1, 3) | 2 (1, 3) | 2 (1, 3) | |
All comparisons P>0.05
Use of IHELP
Significant differences between teams were found in the use of IHELP, the number of IHELP domains documented per H&P, and the number of social work consults (Table 4). More than 80% of the intervention team’s H&Ps documented use of IHELP. Due to informal dissemination of IHELP among residents and hospitalists, about one-sixth of the comparison team’s H&Ps also documented use of IHELP. Nevertheless, the percentage of intervention team admissions with social work consult requests was still nearly 3 times that of the comparison team. Of the intervention team H&Ps documenting IHELP use, the most commonly screened domains were housing (78.1%), income (77.4%) and health insurance (77.0%). Intimate partner violence was the least commonly asked domain (20.1%). An unmet need was detected by an intern for 27.4% of intervention team admissions. The most commonly detected unmet needs were income (13.5%) and health insurance (6.6%). The most common domains in the 16.5% of comparison team H&Ps using IHELP were housing (22.0%), insurance (18.6%), and intimate partner violence (16.9%).
Table 4.
IHELP Use and Social Work Consults.a
| Intervention Team, n (%) | Comparison Team, n (%) | |
|---|---|---|
| IHELP Use | 283 (81.6) | 45 (16.5) |
| Mean (SD) Number of IHELP Domains per History and Physical | 3.3 (2.5) | 0.4 (1.2) |
| Social Work Consults | 74 (21.3) | 22 (8.1) |
All comparisons P <0.001
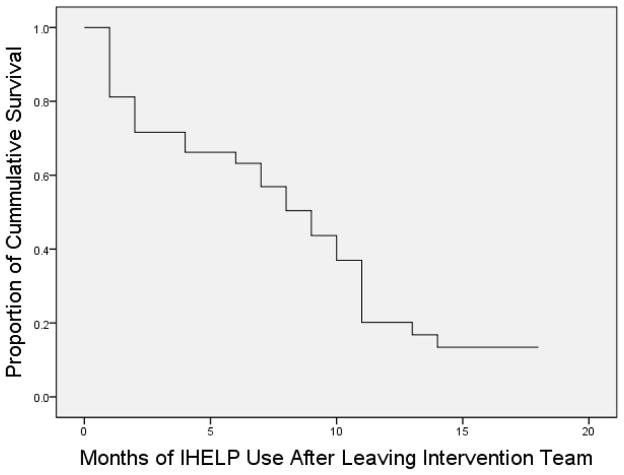
Every third H&P at the study site during the 21-month maintenance period was reviewed in order to determine continued use of IHELP by former intervention team interns. The available maintenance periods ranged from 3 months (December 2012 intervention interns) to 20 months (July 2011 intervention interns). Of the 43 intervention interns, 30 (69.8%) stopped using IHELP at some point during the maintenance period, while 13 (30.2%) maintained usage to the end of the period. The median survival time was 8.1 months (IQR 1–10 months) (Figure 1).
Figure 1.
Maintenance of IHELP Use After Leaving the Intervention Team
Social Work Confirmation of IHELP Need and Resources Provided
Of the 283 intervention team admissions with documented IHELP use, 143 (50.5%) also received complete social work evaluations. Both the intern and the social work evaluation detected an unmet social need for 45 admissions (specificity 0.96, 95% CI 0.87–0.99; positive predictive value 0.94, 95% CI 0.82–0.98). For 6 (12.5%) of these patients, the social worker detected a different need than the intern. The intern did not identify an unmet need in 27 admissions where an additional social need was detected by social work (sensitivity 0.63, 95% CI 0.50–0.73; negative predictive value 0.72, 95% CI 0.61–0.80). For social work-confirmed needs, social work was able to provide resources or referrals to 77.8%, while finding that 13.3% of the families were already appropriately addressing the unmet need. Less than 10% had active needs but were unable to be connected with resources or referrals.
DISCUSSION
The present study used a multiple behavioral change strategy intervention to improve the social histories of pediatric interns on an inpatient rotation so they could better detect social needs of hospitalized patients. Interns on the intervention team used the improved social history (IHELP) in over 80% of admissions, resulting in social work consults in nearly 25% of the admissions. Interns’ use of IHELP had a positive predictive value over 90% (using social work evaluation as the gold standard), and resources or referrals were made by social work for the great majority of all detected social needs.
The intervention was unique in using multiple behavioral change strategies, including reducing barriers, social normalization, and changing the consequences. This contrasts with most clinical training that primarily relies on classroom didactics or bedside teaching (i.e., providing information, which is considered a relatively weaker behavioral change strategy.) 21,22 The detection of active social needs by interns in 25% of admissions is similar to other interventions designed to increase resident screening for social needs, where active social needs were detected in <5.0% to 52% of study participants..5,6,12,16 The advantage of the current intervention lies in its brevity, with only 30 minutes or less of total faculty time needed. While other studies suggest that computer-based screening methods may produce higher detection rates,4,14,23 the use of dedicated computers may not always be practical in all settings, may exclude physicians of his or her role in addressing social needs, and may not follow trainees once they graduate and move to a different institution.
The initial success of the current intervention has implications not only for the Accreditation Council for Graduate Medical Education’s new child advocacy training requirements, but for all residency training where more impactful education is needed in light of reduced resident work hours.9 By supplementing teaching (providing information) with stronger behavioral change strategies (such as modifying barriers and changing the consequences), residency program faculty may be able to integrate this type of educational strategy easily into bedside teaching while complying with work hour limits.
However, we also found that the median duration of IHELP use after leaving the intervention team was 8 months. This suggests that although the intervention succeeded in initially altering intern behavior, a “booster shot” to reinforce the behavior is likely needed. In addition, not all domains were asked equally by intervention group interns. While it may be inappropriate to ask certain domains (e.g., intimate partner violence when other individuals are present), the use of all IHELP may be improved by the inclusion of IHELP in the electronic health record and by attending emphasis on intern use of all domains. The duration of behavior change in other interventions to improve resident detection of social needs is unclear. It is possible that the sustained use of IHELP could be also improved by integrating IHELP into the electronic health record to facilitate, which would prompt the use of IHELP. Sustained use of IHELP may also be promoted by encouraging IHELP on other rotations in both the inpatient and outpatient settings.
In this study, we sought to determine the validity of screening for social needs. Our finding of a high positive predictive value of IHELP use by residents suggests that screening for social needs does not result in unnecessary social work consults and leads to appropriate resources and referrals to address social factors with important health implications. Our study is unable to conclude, however, whether the family actually received the community resource or referral and, if so, whether the unmet need was corrected and positive health incurred. We found that the negative predictive value was lower (75%), with sensitivity upper limit confidence intervals just exceeding 70%. It is unclear if the relatively low sensitivity is due to inherent limitations in the IHELP screening questions, resident physician inexperience (either as a physician or with IHELP specifically), inefficiencies in documentation of social needs, ineffectiveness of the IHELP curriculum in this setting, situational factors such as time of day (e.g., admissions occurring at night when parents and physicians may be tired), higher acuity early in the admission when resident physician screening was conducted, or even the manner and degree of empathy in which the screening questions were asked. In addition, our findings of IHELP specificity and sensitivity in this study have two important limitations. First, only half of the admissions had full social work evaluations. Although many of the missed social work evaluations were related to short length of stay rather than intentional selection, it is unknown whether the patients receiving social work evaluations differed systematically from those not receiving them. If the patients receiving social work evaluations were more likely to have a social need, it might falsely inflate our sensitivity and specificity calculations. Second, the great majority of intern screening did not use all IHELP domains. The average H&P used approximately half of the eight IHELP domains. The incomplete use of IHELP means that our sensitivity and specificity calculations should be interpreted with caution. Nevertheless, despite both incomplete use of IHELP by the intervention team and IHELP contamination of the control team, the intervention team still requested three times as many social work consults as the control team, clearly demonstrating that the effect on clinical practice was substantial.
The current findings should be interpreted in light of other important limitations. It should be noted that the success of the current intervention depended on the fact that social workers were available to respond to positive screens and that many resources were available due to the study’s location in a large metropolitan area. Other institutions may not have these resources for physicians. Although other referral sources are available when social needs are detected (e.g., the nationwide network of 2-1-1 call centers supported by the Alliance of Information and Referral Systems and the United Way), a master’s degree-level social worker is likely the preferred resource in most health care settings. Not only did the availability of social work contribute to the great majority of positively screened patients receiving resources but it also allowed interns to screen families confident that referrals could be made when unmet needs were detected. The success of the intervention also depended on the cooperation and training of the inpatient attending physicians. Furthermore, it may be difficult to translate some aspects of this intervention (e.g., starting rounds with “Are there any IHELP issues?”) to the outpatient setting, where the vast majority of pediatric patients are seen. Our findings are also limited by the need to use a social work evaluation as the gold standard for detecting all unmet social needs. Currently, there are few validated screening questions for social needs, and few prior studies of screening for social needs have examined sensitivity and specificity. Determining the most accurate and sensitive method for detecting social needs and for training residents in addressing those needs should become more possible as more screening instruments are validated. Finally, further research is needed on whether families receive the needed resource and the effect on patient health.24
CONCLUSIONS
The current brief intervention, which used multiple behavioral change strategies, effectively increased resident screening and detection for social needs in inpatient settings. Nearly all detected needs were confirmed by social work and the great majority of families with detected needs were given resources or referrals to mitigate those needs, potentially leading to improvements in patient and family health.
WHAT’S NEW.
A brief intervention using multiple behavioral change strategies effectively increased resident screening and detection for social needs. Due to the strong impact on child health, it is imperative that physicians are adequately trained in the detection of social needs.
Acknowledgments
Funding for this project was provided by the Katherine B. Richardson Award from Children’s Mercy Hospitals and Clinics. Research reported in this publication was also supported by the National Institute on Drug Abuse of the National Institutes of Health under award number DA07272. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The sponsors had no role in study design, data collection, analysis or interpretation, the writing of the manuscript, or the decision to submit the manuscript for publication.
Abbreviations
- CI
Confidence Interval
- H&P
History and Physical
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- IQR
Inter-Quartile Range
- SES
Socioeconomic Status
- SW
Social Work
Footnotes
Financial Disclosure: All of the authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: All of the authors declare no conflicts of interest.
Author Contributions
Jeffrey D. Colvin - Has participated in the study design, analysis and interpretation of the data, and was the primary author of the manuscript. He has approved the final version of the manuscript being submitted.
Jessica L Bettenhausen - Has participated in the study design and interpretation of the data and has provided critical intellectual content in the revision of the manuscript. She has approved the final version of the manuscript being submitted.
Kaston D. Anderson-Carpenter - Has participated in the study design and interpretation of the data and has provided critical intellectual content in the revision of the manuscript. He has approved the final version of the manuscript being submitted.
Vicki Collie-Akers - Has participated in the study design and interpretation of the data and has provided critical intellectual content in the revision of the manuscript. She has approved the final version of the manuscript being submitted.
Laura Plencner - Has participated in the study design and interpretation of the data and has provided critical intellectual content in the revision of the manuscript. She has approved the final version of the manuscript being submitted.
Molly Krager - Has participated in the study design and interpretation of the data and has provided critical intellectual content in the revision of the manuscript. He has approved the final version of the manuscript being submitted.
Brooke Nelson - Has participated in the study design and interpretation of the data and has provided critical intellectual content in the revision of the manuscript. She has approved the final version of the manuscript being submitted.
Sara Donnelly - Has participated in the study design and interpretation of the data and has provided critical intellectual content in the revision of the manuscript. He has approved the final version of the manuscript being submitted.
Julia Simmons - Has participated in the study design and interpretation of the data and has provided critical intellectual content in the revision of the manuscript. She has approved the final version of the manuscript being submitted.
Valeria Higinio - Has participated in the study design and interpretation of the data and has provided critical intellectual content in the revision of the manuscript. She has approved the final version of the manuscript being submitted.
Paul J. Chung - Has participated in the study design, analysis and interpretation of the data, and has provided critical intellectual content in the revision of the manuscript. He has approved the final version of the manuscript being submitted.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jeffrey D. Colvin, Email: jdcolvin@cmh.edu.
Jessica L. Bettenhausen, Email: jlbettenhausen@cmh.edu.
Kaston D. Anderson-Carpenter, Email: kacarpenter@ucla.edu.
Vicki Collie-Akers, Email: vcollie@ku.edu.
Laura Plencner, Email: lmplencner@cmh.edu.
Molly Krager, Email: mkkrager@cmh.edu.
Brooke Nelson, Email: banelson@cmh.edu.
Sara Donnelly, Email: smdonnelly@cmh.edu.
Julia Simmons, Email: jsimmons@cmpcn.org.
Valeria Higinio, Email: vhiginio@thcckc.org.
Paul J. Chung, Email: paulchung@mednet.ucla.edu.
References
- 1.Singh GK, Yu SM. US childhood mortality, 1950 through 1993: Trends and socioeconomic diffferentials. American Journal of Public Health. 1996;86(4):505–512. doi: 10.2105/ajph.86.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Newacheck PW, Hung YY, Park MJ, Brindis CD, Irwin CE. Disparities in adolescent health and health care: does socioeconomic status matter? Health Serv Res. 2003;38(5):1235–1252. doi: 10.1111/1475-6773.00174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Victorino CC, Gauthier AH. The social determinants of child health: variations across health outcomes – a population-based cross-sectional analysis. BMC Pediatr. 2009;9(1):53. doi: 10.1186/1471-2431-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff S. Families’ Health-Related Social Problems and Missed Referral Opportunities. Pediatrics. 2007;119(6):e1332–e1341. doi: 10.1542/peds.2006-1505. [DOI] [PubMed] [Google Scholar]
- 5.Garg A, Butz AM, Dworkin PH, Lewis RA, Serwint JR. Screening for Basic Social Needs at a Medical Home for Low-Income Children. Clinical Pediatrics. 2008;48(1):32–36. doi: 10.1177/0009922808320602. [DOI] [PubMed] [Google Scholar]
- 6.Keller D, Jones N, Savageau J, Cashman S. Development of a Brief Questionnaire to Identify Families in Need of Legal Advocacy to Improve Child Health. Ambulatory Pediatrics. 2008;8(4):266–269. doi: 10.1016/j.ambp.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Fiscella K, Burstin HR, Nerenz DR. Quality measures and sociodemographic risk factors: to adjust or not to adjust. JAMA. 2014;312(24):2615–2616. doi: 10.1001/jama.2014.15372. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington, DC: National Academies Press; 2014. pp. 1–375. [PubMed] [Google Scholar]
- 9.Accreditation Council for Graduate Medical Education, American Board of Pediatrics. The Pediatrics Milestone Project. 2013:1–124. [Google Scholar]
- 10.Klein MD, Schumacher DJ, Sandel M. Assessing and managing the social determinants of health: defining an entrustable professional activity to assess residents’ ability to meet societal needs. Academic Pediatrics. 2014;14(1):10–13. doi: 10.1016/j.acap.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Kenyon C, Sandel M, Silverstein M, Shakir A, Zuckerman B. Revisiting the Social History for Child Health. Pediatrics. 2007;120(3):e734–e738. doi: 10.1542/peds.2006-2495. [DOI] [PubMed] [Google Scholar]
- 12.Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the Management of Family Psychosocial Problems at Low-Income Children’s Well-Child Care Visits: The WE CARE Project. Pediatrics. 2007;120(3):547–558. doi: 10.1542/peds.2007-0398. [DOI] [PubMed] [Google Scholar]
- 13.Garg A, Marino M, Vikani AR, Solomon BS. Addressing families’ unmet social needs within pediatric primary care: the health leads model. Clinical Pediatrics. 2012;51(12):1191–1193. doi: 10.1177/0009922812437930. [DOI] [PubMed] [Google Scholar]
- 14.Gottlieb L, Hessler D, Long D, Amaya A, Adler N. A Randomized Trial on Screening for Social Determinants of Health: the iScreen Study. Pediatrics. 2014;134(6):e1611–e1618. doi: 10.1542/peds.2014-1439. [DOI] [PubMed] [Google Scholar]
- 15.Klein MD, Alcamo AM, Beck AF, et al. Can a video curriculum on the social determinants of health affect residents“ practice and families” perceptions of care? Academic Pediatrics. 2014;14(2):159–166. doi: 10.1016/j.acap.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Klein MD, Kahn RS, Baker RC, Fink EE, Parrish DS, White DC. Training in social determinants of health in primary care: does it change resident behavior? Academic Pediatrics. 2011;11(5):387–393. doi: 10.1016/j.acap.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz A, Weiner SJ, Harris IB, Binns-Calvey A. An educational intervention for contextualizing patient care and medical students’ abilities to probe for contextual issues in simulated patients. JAMA. 2010;304(11):1191–1197. doi: 10.1001/jama.2010.1297. [DOI] [PubMed] [Google Scholar]
- 18.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA. 2011;305(7):682–690. doi: 10.1001/jama.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morse RB, Hall M, Fieldston ES, et al. Hospital-level compliance with asthma care quality measures at children’s hospitals and subsequent asthma-related outcomes. JAMA. 2011;306(13):1454–1460. doi: 10.1001/jama.2011.1385. [DOI] [PubMed] [Google Scholar]
- 20.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths Attributed to Pediatric Complex Chronic Conditions: National Trends and Implications for Supportive Care Services. Pediatrics. 2001;107(6):e99–e99. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 21.Frieden TR. A framework for public health action: the health impact pyramid. American Journal of Public Health. 2010;100(4):590–595. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collie-Akers V, Schultz JA, Carson V, Fawcett SB, Ronan M. REACH 2010: Kansas City, Missouri: Evaluating Mobilization Strategies With Neighborhood and Faith Organizations to Reduce Risk for Health Disparities. Health Promotion Practice. 2009;10(2 Suppl):118S–127S. doi: 10.1177/1524839908331271. [DOI] [PubMed] [Google Scholar]
- 23.Hassan A, Blood EA, Pikcilingis A, et al. Youths’ Health-Related Social Problems: Concerns Often Overlooked During the Medical Visit. Journal of Adolescent Health. 2013;53(2):265–271. doi: 10.1016/j.jadohealth.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 24.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing Social Determinants of Health at Well Child Care Visits: A Cluster RCT. Pediatrics. 2015;135(2):e296–e304. doi: 10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]