Abstract
Background
Altered biomechanics from repetitive microtrauma, such as long practice hours in en pointe (tip of the toes) or demi pointe (balls of the feet) predispose ballet dancers to a multitude of musculoskeletal pathologies particularly in the lower extremities. Both ultrasound and magnetic resonance imaging (MRI) are radiation-sparing modalities which can be used to confidently evaluate these injuries, with ultrasound (US) offering the added utility of therapeutic intervention at the same time in experienced hands.
Questions/Purposes
The purposes of this paper were: (1) to illustrate the US and MRI features of lower extremity injury patterns in ballet dancers, focusing on pathologies commonly encountered at a single orthopedic hospital; (2) to present complementary roles of both ultrasound and MRI in the evaluation of these injuries whenever possible; (3) to review and present our institutional approach towards therapeutic ultrasound-guided interventions by presenting explicit cases.
Methods
Online searches were performed using the search criteria of “ballet biomechanics” and “ballet injuries.” The results were then further narrowed down by limiting articles published in the past 15 years, modality (US and MRI), anatomical region (foot and ankle, hip and knee) and to major radiology, orthopedics, and sports medicine journals.
Results
Performing ballet poses major stress to lower extremities and predisposes dancer to several musculoskeletal injuries. These can be adequately evaluated by both US and MRI. US is useful for evaluating superficial structures such as soft tissues, tendons, and ligaments, particularly in the foot and ankle. MRI provides superior resolution of deeper structures such as joints, bone marrow, and cartilage. In addition, US can be used as a therapeutic tool for providing quick symptomatic improvement in these athletes for who “time is money”.
Conclusion
Performing ballet may cause major stress to the lower extremities, predominantly affecting the foot and ankle, followed by the knee and hip. US and MRI play complementary roles in evaluating various orthopedic conditions in ballet dancers, with US allowing for dynamic evaluation and guidance for interventions.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-015-9442-z) contains supplementary material, which is available to authorized users.
Keywords: ballet, ultrasound, MRI, foot and ankle, hip, tendon, ligament, osseous, labrum, corticosteroid and PRP
Introduction
Ballet is a physically challenging endeavor requiring long hours of rehearsals in en pointe and demi pointe positions, which lead to altered biomechanics and predispose the dancers to various lower extremity injuries. The female athlete triad, comprising of anorexia, amenorrhea, and osteoporosis due to the immense social stigma attached to the weight of the dancers, further predisposes them to injuries and delayed healing. In a 2008 study [30], 204 elite pre-professional ballet dancers were screened over a 5-year period to identify injury patterns specific to this group. The study found that 32 to 51% of the dancers were injured each year, with 53% occurring in the foot/ankle, 21.6% occurring in the hip, 16.1% occurring in the knee, and 9.4% occurring in the back. Although these cases and discussion target injuries encountered in ballet dancers, they can also be seen in non-ballet population as well. Radiographs are usually the initial screening modality to evaluate patients, including ballet dancers with lower extremity symptoms, nonetheless, cross-sectional imaging is often necessary when radiographs are non-diagnostic. Both US and magnetic resonance imaging (MRI) are radiation-sparing modalities with unique roles. MRI, although a static examination, provides a superb global evaluation of each joint, including deep structures such as the articular cartilage, which cannot be adequately evaluated using US due to poor acoustic penetration. On the other hand, US allows detailed assessment of the superficial soft tissue structures, as in the foot and ankle. US also allows dynamic evaluation to assess structures in motion, including tendons, ligaments, and joints. In addition, US allows targeted real-time imaging guided interventions.
The role of ultrasound as a therapeutic and prognostic tool is ever evolving. Currently, commonly performed therapeutic procedures include tendon sheath injections (flexor hallucis longus, posterior tibial tendon, and iliopsoas), Achilles paratenon injections, peritendinous hamstring injections, Morton’s neuromas, plantar fascia, and paralabral/ganglion cyst aspirations [83]. Tenography followed by anesthetic and steroid injection in the setting of peroneal, flexor hallucis longus (FHL), posterior and anterior tibial tendons has been shown to provide complete or near complete pain relief [43]. The exact mechanism of action of steroids is not clearly known, but they tend to exert anti-inflammatory effect and provide short and intermediate term pain relief [56]. A critical complication is the possibility of tendon necrosis with intra-tendinous injection. This can be avoided by dynamic sonographic technique with clear visualization of needle placement within the tendon sheath. However, there is a much smaller very rare risk of tendon damage with peritendinous injection [76]. The role of steroids in the setting of partial thickness tendon tear is controversial and may cause tendon weakness precipitating rupture. Currently, no definite guidelines have been established regarding steroid use in partial thickness tendon tears and further research is needed. At our institution, we continue to use anesthetic and steroid mixture for low grade intrasubstance tears, tendinosis, and tenosynovitis in conjunction with conservative and rehabilitative therapy. For Achilles, plantar fascia, ligamentous injuries and patellar tendon pathologies we have been successfully using platelet rich plasma (PRP) injections with good clinical outcomes [24].
Four main categories of injuries that are encountered in the foot and ankle of ballet dancers are tendinous, ligamentous, osseous, and several impingement syndromes. The commonly encountered hip injuries in ballet dancers due to repetitive microtrauma include chondrolabral instability, which may be associated with other complications such as paralabral ganglion cysts, which in turn may cause local compressive mass effect resulting in predominantly femoral and to a lesser extent sciatic neuropraxia. Other common hip pathologies include osseous as well as tendinous and capsular injuries resulting in impingement syndromes. In the knee, overuse injuries include sprains and strains, primarily jumper’s knee and to a lesser extent pathologies of the meniscocapsular and ligamentous complex.
Methods
Search Criteria
We performed online searches using Google Scholar with initial search criteria of “Ballet Injuries” and “Ballet biomechanics”. The search of “ballet injuries” identified 22,800 articles and the search of “ballet biomechanics” identified 4340 articles which were further narrowed down by adding “lower extremity” to both search phrases which yielded 17,500 and 3449 articles respectively. Priority was initially given to articles published in the past 10 years which decreased the search results to 15,600 and 2260. Ballet biomechanics articles were then sorted by relevance. Priority was given to articles published in radiology journals by including search criteria of several radiology journals. The search “lower extremity ballet injuries” was further narrowed down by “imaging features” in lower extremity injuries in ballet dancers which yielded 2270 results which was further subdivided as imaging features in “foot and ankle”, “knee”, and “hip” which were further subclassified by imaging modality of either MRI or US as described in detail in the flowchart. A separate search for imaging interventions in lower extremity injuries in ballet dancers yielded 2720 results which were further narrowed by ultrasound-guided interventions in foot and ankle (558 results), knee (510 results), and hip (463) results. Priority was then given to articles published in radiology- and orthopedic-based journals such as “Radiology”, “Radiographics”, “American journal of Roentgenology”, “Journal of Ultrasound”, “HSS Journal”, “American Journal of Sports Medicine”, “Orthopedics”, “International Orthopedics”, “Journal of Clinical Orthopaedics & Trauma”, “Journal of Bone Joint Surgery Am”, “Foot And Ankle International” and “Foot and Ankle Surgery”. Articles were then reviewed to determine if the content was applicable. Additional articles were incorporated into the manuscript as specific topics needed to be addressed.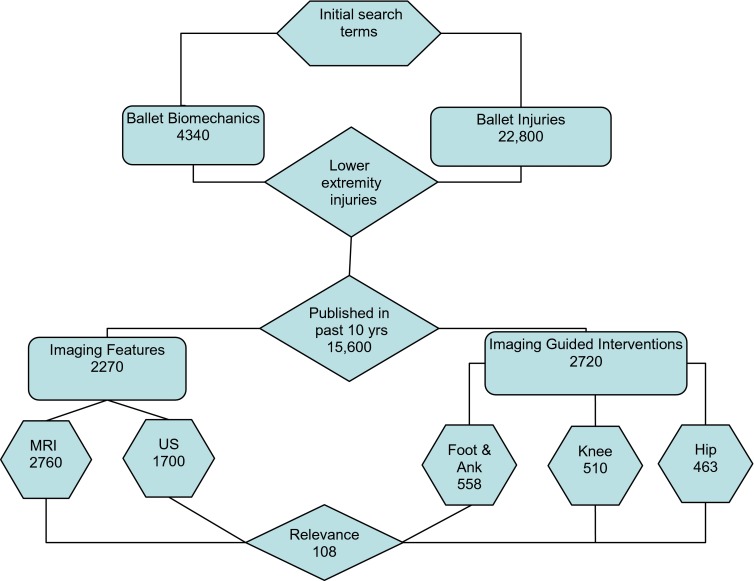
Foot and Ankle
The superficial anatomy of the ankle and foot can be well evaluated using US, which allows dynamic assessment to see structures in motion. Real-time visualization of echogenic needle tip under ultrasound allows accurate needle placement in the tendon sheath, bursa, joint, plantar fascia, neuromas (Morton’s Neuroma) as well as intratendinous calcification [1, 2, 55, 83]. US-guided targeted interventions include peritendinous injections particularly of the commonly injured FHL [65] and peroneal tendons [84] in ballet dancers. Perifascial injections are of benefit in tackling plantar fascial inflammation/tears. Steroid and anesthetic injections of painful Morton’s neuroma and intermetatarsal bursitis [85] are very successful. Intratendinous therapies with tenotomy followed by PRP injections have been shown to promote healing [53] which are commonly performed for Achilles tendons. At our institution, we commonly utilize a 1.5-in. 25 gauge needle under ultrasound guidance with low depth linear probes usually L12–15 Mhz.
Commonly encountered foot and ankle injuries in our patient population include overuse injuries, such as tendinous injuries mainly involving the peroneal and flexor hallucis longus tendons, ligamentous injuries particularly involving the anterior talofibular ligament (ATFL), a multitude of osseous injuries, impingement syndromes, Morton’s neuromas and plantar fasciitis [48].
Tendon Pathologies
Tendon abnormalities range from tendinosis, tenosynovitis, and tendon tear to tendon subluxation/dislocation.
Peroneal Tendons
Inversion injuries at the ankle with the foot held in plantar flexion can cause lateral ligamentous complex and peroneal tendon injuries, which can result in varus instability [75, 98]. Peroneal tenosynovitis is seen in ballet dancers due to long hours spent in demi pointe. The superior peroneal retinaculum (SPR) forms the posterolateral wall of the retromalleolar groove and serves to deepen this groove. It is a fibrous band that originates from the posterior ridge of the distal fibula and extends postero-inferiorly to insert on the lateral calcaneus. The SPR forms a proximal fibro-osseous tunnel through which the peroneal tendons pass, going from a medial to lateral relationship of the peroneus brevis and longus tendons, respectively, to an anterior and posterior relationship below the lateral malleolus. Distal to the peroneal tubercle, each tendon has its own fibro-osseous tunnel formed by the inferior peroneal retinaculum. Peroneal tendon dislocations and subluxations were originally described in ballet dancers [75]. Inversion injuries or forceful dorsiflexion and reflex peroneal contraction are responsible for subluxation events that may be associated with SPR injuries [98].
Imaging Features
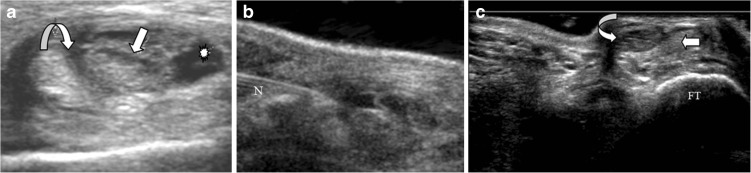
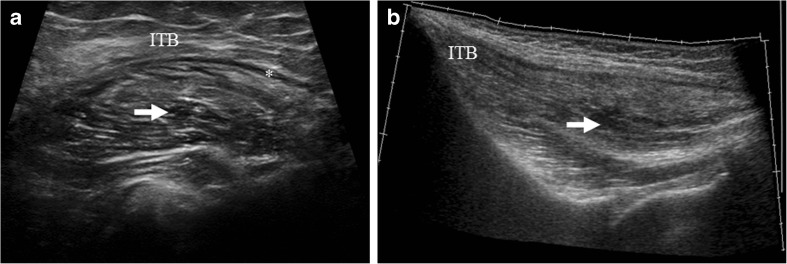
On MRI, tendinosis manifests as tendon thickening and increased intrasubstance T1 and T2 signal. Tenosynovitis appears as edema or fluid surrounding the tendon. Complete peroneus longus tear is associated with cuboid bone marrow edema with proximally retracted tendon [98]. MRI plays an important role in evaluating the integrity of the SPR and its attachment on the lateral malleolus as well as the status of the peroneal tendons. On ultrasound, tendinosis is seen as hypoechoic enlargement of the tendon without disruption, and tenosynovitis is seen as abnormal tendon with fluid within the tendon sheath. Tendon tear is seen as a discontinuity with a hypoechoic fluid-filled gap (Fig. 1a, b). Peroneal tendons can undergo episodic subluxations that can be demonstrated in real time by dynamic ultrasound (Fig. 1c, ESM 7), with provocative maneuvers such as active dorsiflexion and eversion of the ankle or circumduction of the foot [39, 57]. Palpable snapping or crepitus of the tendons may be evident during these maneuvers [68].
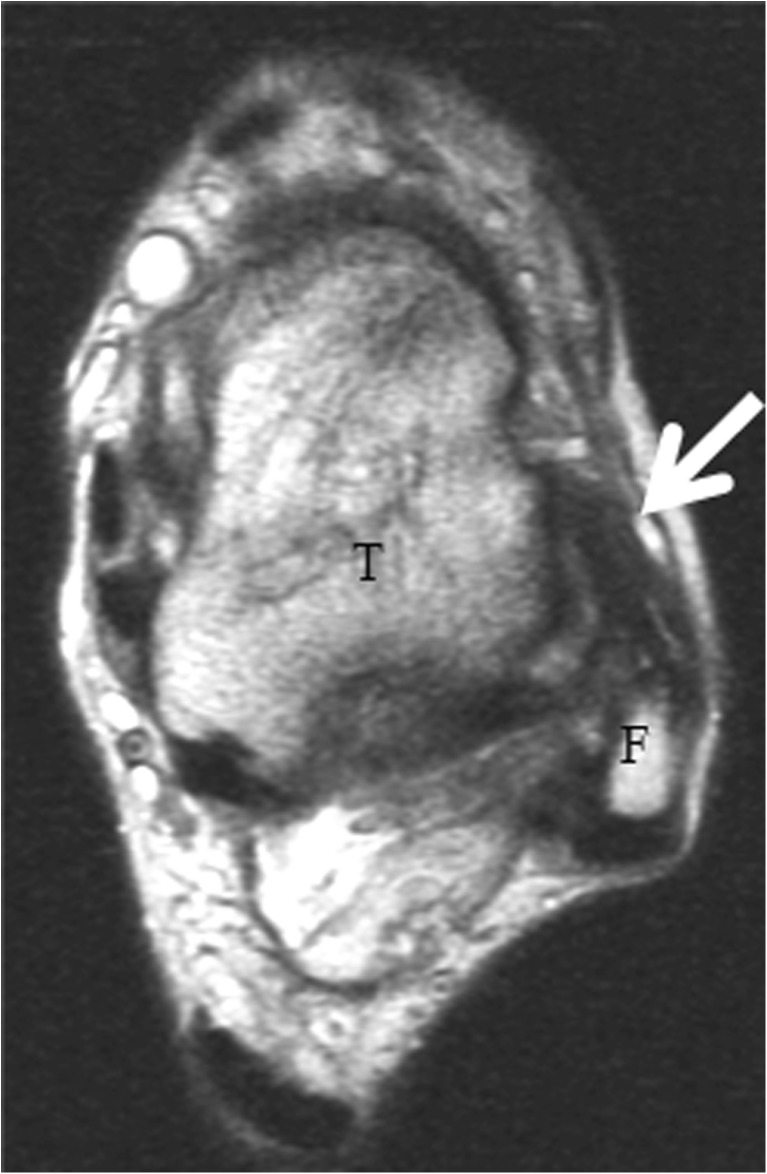
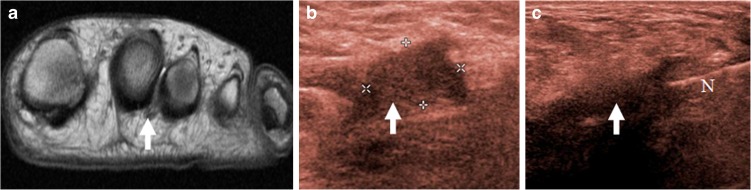
Fig. 1.
a, b A 27-year-old female professional ballet dancer with lateral ankle pain. a Ultrasound image obtained short axis to the peroneal tendons at the level of the calcaneus, demonstrates fluid and debris within the peroneal tendon sheath with an intrasubstance longitudinal split tear of the peroneus longus tendon (arrow peroneus longus, curved arrow peroneus brevis, asterisk tendon sheath fluid). b Ultrasound-guided steroid injection of the peroneal tendon sheath with linear echogenic needle tip (N) seen in long axis. c A 27-year-old ballet dancer with lateral ankle pain. Static short axis ultrasound image from a cine clip of the lateral ankle shows mild tendinosis of the peroneus longus (curved arrow) and brevis (straight arrow) tendons with a shallow fibular groove (FT) and PB subluxed beyond the fibular tip. d Dynamic cine clip imaged in short axis to the peroneal tendons with the patient actively circumducting at the level of the ankle shows intrasheath subluxation of the two tendons with respect to each other as well as subluxation onto and beyond the fibular tip with provocative maneuvers, reflecting laxity of the superior peroneal retinaculum (ESM 7).
Management
Conservative treatment includes anti-inflammatory medications, and immobilization, followed by rehabilitation. Cast placement, lateral ankle braces, and orthotic treatment can also be applied for stabilization. Indications for peritendinous peroneal tendon sheath steroid injection include tenosynovitis with tendon abnormality such as tendinosis [41, 84, 69]. The role of steroids with partial thickness tendon tear is controversial and institution dependent. Steroids provide short-term pain relief [76, 41]. Disruption of the SPR predisposes to early tendon degeneration and dislocation, predominantly affecting the peroneus brevis, and requires surgical intervention in active patients. Asymptomatic or static peroneal dislocation may not require treatment. However, chronic friction and motion of the tendon in and out of the retromalleolar groove can be painful and may progress to tear. Plaster cast immobilization is the initial management for acute SPR tears with variable results. Surgical repair with debridement, repair of the tear, tenosynovectomy, and groove deepening is reserved for severe cases or in athletes. Resection of os peroneum is also curative [84, 98].
Flexor Hallucis Longus/Dancer’s tendonitis
FHL is considered the “Achilles tendon of the foot” in ballet dancers and allows the push off maneuver from the forefoot in plantar-flexed position. In en pointe and demi pointe positions, the FHL may become stretched beyond its limits. There are three potential sites of entrapment of the FHL tendon: proximally within a fibro-osseous tunnel between the medial and lateral tubercles of the posterior talus, where it is lined by a synovial sheath (Fig. 2a, b); more inferiorly as it passes through a shallow groove on the posterior aspect of the sustentaculum tali; and lastly, more distally between the two sesamoids at the base of the proximal phalanx of the great toe. However, the most common site of FHL entrapment is within its fibro-osseous tunnel where it changes direction from a vertical course posterior to the talus to a more transverse course beneath the calcaneus [32, 54]. Most of the reported FHL abnormalities in ballet dancers have been attributed to an enlarged os trigonum resulting in posterior impingement syndrome. A Stieda process (prominent lateral tubercle of the talus) or an os trigonum (unfused lateral tubercle of the talus) can cause compression of the FHL tendon. Post-traumatic soft tissue scarring between the calcaneus and talus or around a calcaneus fracture can also predispose to soft tissue entrapment of the FHL tendon.
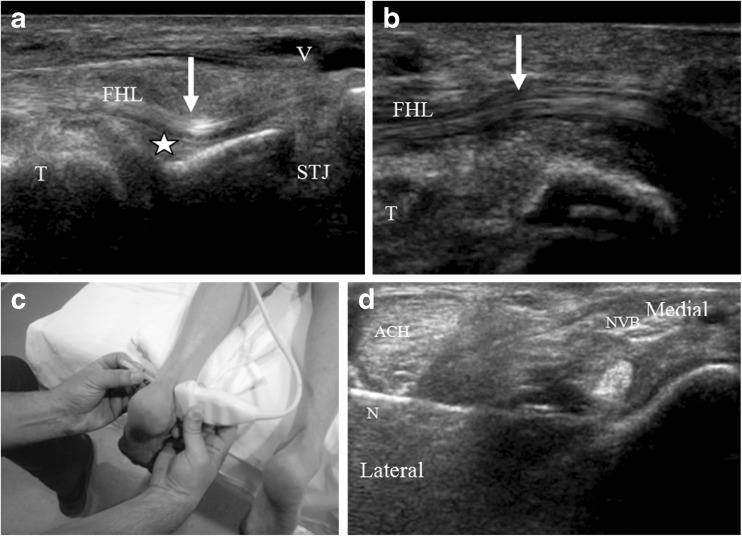
Fig. 2.
a and b Longitudinal images below the level of the medial malleolus demonstrates kinking (arrow in a) of the flexor hallucis longus (FHL) tendon proximal to the subtalar joint (STJ) from scarring of the posterior recess of the ankle joint (asterisk), reflecting posterior impingement. b Post FHL tendon sheath release surgery longitudinal imaging at the same level demonstrates mass effect on the FHL tendon to have resolved (arrow in b) (T talus). c, d Ultrasound showing FHL peritendinous injection using a lateral peri- Achilles (ACH Achilles tendon) approach in prone position with probe placed on medial skin side. This approach allows access to the FHL with the needle (N) while avoiding the posterior tibial neurovascular bundle (NVB). e, f Cine images before and after surgery similarly demonstrate smoother motion of the FHL tendon after surgical release with active plantar and dorsiflexion of the big toe (ESM 8, ESM 9).
Imaging Features
FHL tendon tear manifests as partial or complete discontinuity of the tendon with fluid signal within the gap. On ultrasound, tendinosis, tendon disruption and tenosynovitis can be easily demonstrated, as described above. Flexion motion of the great toe under real-time ultrasound allows identification and assessment of the normal FHL tendon excursion. This can be then be followed by ultrasound-guided peritendinous injection of the FHL tendon sheath with real-time visualization of the needle and distension of the tendon sheath. One should be aware of the possibility of inadvertent injury to the tibial neurovascular bundle, which lies in close proximity to the FHL tendon along the medial aspect of the hindfoot. Therefore, we describe a peri-Achilles approach with needle directed from the lateral to medial side targeting the FHL tendon sheath [65] directly and thus avoiding the tibial neurovascular bundle (Fig. 2a, b).
Management
Conservative non-operative treatment is the initial management for tendonitis and tenosynovitis with ice packs, anti-inflammatory medications, and arch support. The role of steroids with partial thickness tendon tear is controversial and institution dependent. Sonographically guided steroid injections provide short-term pain relief for tendinopathy and tenosynovitis [65]. FHL tenography followed by anesthetic and steroid injection has been shown to serve as both diagnostic and therapeutic tool for short-term pain relief suggesting tendon sheath as the possible pain generator [12, 65, 78, 23, 24]. Ultrasound-guided steroid injection using a lateral peri-Achilles approach from the lateral to medial side prevents inadvertent injury to the posterior tibial neurovascular bundle [65] as shown in Fig. 2c. However, one needs to be cognizant of the important anatomical landmark at the site where the sural nerve crosses the lateral border of the Achilles tendon approximately 8–10 cm from the superior border of the calcaneal tuberosity to prevent iatrogenic injury to the sural nerve [10]. Surgical release in cases of tendon entrapment is necessary (Fig. 2a, b, ESM 8, ESM 9). Resection of os trigonum or Stieda process is curative.
Achilles Tendon
Dancing “en pointe” introduces torsional stress causing weakening of the Achilles tendon at the critical zone in ballet dancers [57]. Achilles tendon injuries manifest as tendinosis, paratenonitis, and retrocalcaneal bursitis. Acute rupture, although uncommon, can also occur from inadequate warm up. The Achilles tendon has no synovial sheath but is almost completely enclosed within a paratenon that has both parietal and visceral layers [81]. Achilles tendon injuries can occur at the myotendinous junction and enthesis, but are most common at the critical zone, which is an area of relative hypovascularity, located 4–6 cm proximal to its calcaneal insertion [35]. Risk factors include diabetes, middle-aged intermittent/weekend athlete, and familial hypercholesterolemia. Tendinopathy is basically an “overuse” degenerative condition [92]. However, there is convincing evidence that the inflammatory response is a key component in chronic tendinopathy [79]. Both Achilles and patellar tendinopathy share common histopathology such as failed intratendinous healing response and neoangiogenesis [79, 92].
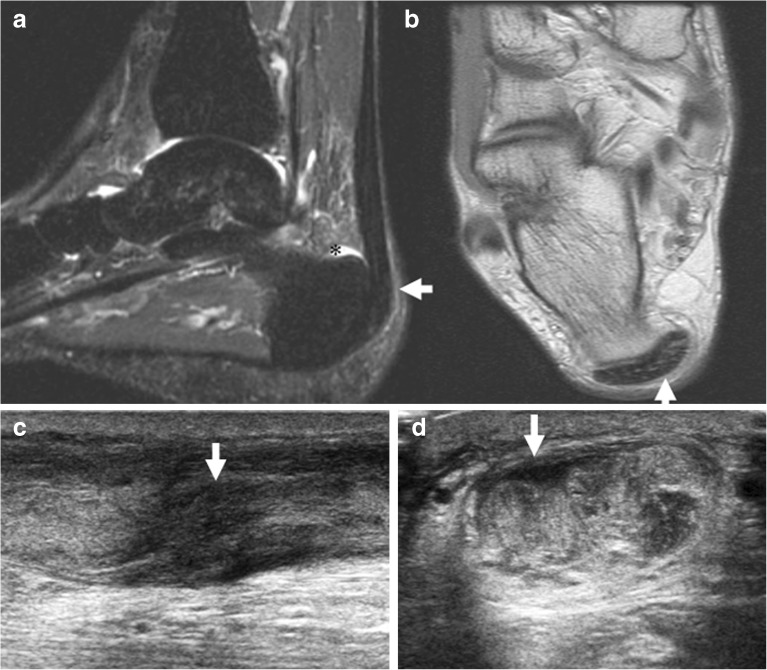
Imaging Features
On MRI, Achilles tendinosis is seen as central enlargement usually at the critical zone or at its calcaneal insertion (Fig. 3a, b). The normal average Achilles tendon thickness is 6 mm. The size of the Achilles tendon is proportional to the degree of an individual’s lean body mass and is known to be thicker in men, the elderly, and those who are tall [81]. A tear is seen as focal hyperintense signal with disrupted fibers, which may be associated with retrocalcaneal bursitis and bony prominence at the posterior aspect of the calcaneus (Haglund’s syndrome) [86]. Ultrasound demonstrates tendinosis as tendon thickening and intrasubstance hypoechogenicity as intrasubstance tears (Fig. 3c, d). Due to the superficial location of the Achilles tendon, it can be adequately assessed by ultrasound for tendinosis, tears, and retrocalcaneal bursitis. Dynamic ultrasound-directed flexion maneuvers allow assessment of the degree of tendon retraction in the setting of Achilles tendon ruptures, which is useful for surgical planning. Tendon retraction may be increased with dorsiflexion and decreased with plantar flexion. If the torn edges of the tendon approximate during plantar flexion, some physicians advocate casting in talipes equinus position rather than surgery. A normal Achilles tendon demonstrates no flow on power Doppler imaging. Increased flow on power Doppler imaging frequently accompanies symptomatic Achilles tendinosis and represents abnormal neovascularity (angiofibroblastic proliferation) [67, 74].
Fig. 3.
a and b A 44-year-old female ballet dancer with chronic hindfoot pain. a Sagittal inversion recovery sequence demonstrates insertional Achilles paratendinitis (arrow) with retrocalcaneal bursitis shown as fluid in the retrocalcaneal bursa (asterisk). b Axial proton density sequence at the level of Achilles insertion demonstrates thickened Achilles paratenon. c and d A 34-year-old male dancer with posterior ankle pain. Longitudinal (c) and transverse (d) sonographic images demonstrate marked Achilles tendon thickening at the critical zone and focal hypoechoic areas (arrow in c) reflecting partial thickness tears. Thickening of the paratenon is noted superficial to the tendon on the transverse image (arrow in d).
Management
Management outcome of treating Achilles tendinopathy is most favorable when treated within 6 months of onset. Non-operative conservative management include abstention of activities that caused the symptoms in acute phase and relative rest or modified activities. Complete rest of an injured tendon has been found to be counterproductive, since it has been shown that tendon loading during eccentric exercises stimulates collagen repair and remodeling. Eccentric training or other progressive loading exercises have also been shown to be particularly effective in managing midportion Achilles tendinopathy by disrupting neovascularity and therefore decreasing pain and improving outcome [92]. Gentle strength training should be started early after injury to prevent disuse atrophy and should not be painful [21].
Anti-inflammatory strategies such as NSAIDs and corticosteroids are often included to reduce tendon pain as there is now growing evidence of involvement of inflammatory mediators as part of ongoing tendinopathy. A Cochrane review of interventions for treating acute and chronic Achilles tendonitis found weak evidence of a moderate effect of NSAIDs, both oral and topical, on acute tendon pain [21]. A non-invasive soft tissue mobilization technique called augmented soft tissue mobilization (ASTM) has been successfully used in the treatment of chronic tendinopathy, probably through controlled application of microtrauma. Correction with orthotics can relieve heel pain by altering the biomechanics of the foot and ankle [21]. A heel lift of 12–15 mm is classically used as an adjunct to the management of Achilles tendon pain [21].
Achilles tendinosis treated with different injectable therapies has been shown to improve function and decrease pain when compared to control groups on short-term follow-up. No definite treatment recommendations can be made based on current evidence regarding the superiority of a particular therapy or on long-term efficacy. Peritendinous injections with corticosteroids are still controversial. Complications such as anterior talofibular (AT) tendon rupture have been described in literature [60]. However, a lot of these studies and risks were described with non-guided injections. There is substantial evidence that corticosteroids can be effective in chronic tendinopathy, reducing pain and improving function in short term. This has been shown to be effective in tendinopathy at multiple locations inclusive of patellar tendinopathy as per evidence-based research [31, 63]. To avoid these complications, steroids are injected around the AT in the paratenon [25, 31]. Fredberg et al. demonstrated benefit at 4 weeks using ultrasound-guided technique [25]. Hence, we can conclude that steroids offer short-term benefits and may cause intrinsic structural tendon weakening in the long term. Sometimes symptoms in patients with Achilles tendinopathy may result from pathological lesions between the AT and the paratenon, not within the tendon itself. This justifies an injection between the tendon and the paratenon [66, 102]. According to a cadaveric study, injections between the posterior paratenon and AT are superior to an anterior paratenon injection [26, 102] as it allows for injectate distribution into the AT, area between the paratenon and AT, as well as in the Kager’s fat pad. Runners with isolated midportion Achilles tendinopathy (nodular lesions <2.5 cm) without any sign of paratendinopathy have shown success with ultrasound-guided multiple percutaneous longitudinal tenotomies. This method is safe, cost-effective, and has been shown to be beneficial in the long term [59].
Blood and blood products such as PRP are rich sources of cells and growth factors, such as vascular endothelial growth factor (VEGF) and insulin like growth factor-1 (IGF-1) which allows tendon healing and growth [20, 36, 61, 101]. Although good-quality in vivo studies are lacking, PRP has been shown to be effective in small uncontrolled studies. However, large-scale scientific studies proving PRP to be better than placebo or no injection are lacking. This remains an area of further research interest.
Conservative treatment is beneficial only if started early. Chronic exposure to the offending activities after initial injury results in formation of adhesions which are less likely to respond to conservative treatment and may require surgical intervention. There are four main surgical techniques described in literature, all of which include open tenotomy with removal of abnormal tissue, which can be done without stripping of paratenon; with stripping of paratenon; with longitudinal tenotomy with or without paratenon stripping; and lastly percutaneous longitudinal tenotomy [7, 59]. The goal of the surgery is to detect and remove intratendinous lesions, restore vascularity by stimulating neoangiogenesis by multiple longitudinal tenotomies and perhaps stimulate a healing response in the remaining viable cells [7, 59, 93]. It is important to bear in mind that ultrasound-guided tenotomies are most useful for isolated midportion tendinopathy and not for diffuse disease. A formal surgical exploration with paratenon stripping and longitudinal tenotomies may be preferred for diffuse or multinodular tendinopathy or with pantendinopathy [59, 93]. Early mobilization is the mantra after intervention.
Several alternative pain management strategies besides NSAIDs and corticosteroids have been described. Denervation procedures can be used in chronic tendinopathy which aim to disrupt neural ingrowth which is accompanied by neovessel formation [5]. New emerging options in this area include sclerosant therapy (polidocanol and possibly dextrose) [4], high volume tendon stripping injections [15] and surgical techniques such as paratenon stripping. Extracorporeal shock wave therapy (ESWT) may influence pain processing due to direct effect on peripheral nerves [58] as they are toxic to the nerves.
Posterior Impingement Syndrome
Posterior ankle impingement refers to a group of clinical entities resulting from chronic repetitive or acute forced plantar flexion of the foot. Synonyms for this condition include os trigonum syndrome, talar compression syndrome, and posterior block of the ankle. This syndrome has been extensively described in ballet dancers [34]. There may be osseous or purely soft tissue impingement. Etiology includes repetitive plantar flexion in the setting of osseous risk factors such as an os trigonum, Stieda process, or prominent posterior process of the calcaneus. Soft tissue impingement may result from synovial hypertrophy of the FHL tendon sheath, the posterior recesses of the subtalar and tibiotalar joints, and the posterior intermalleolar ligament [14, 80]. The FHL tendon may become impinged and inflamed as it courses medial to the os trigonum with repetitive plantar flexion (en pointe) in ballet dancers [32].
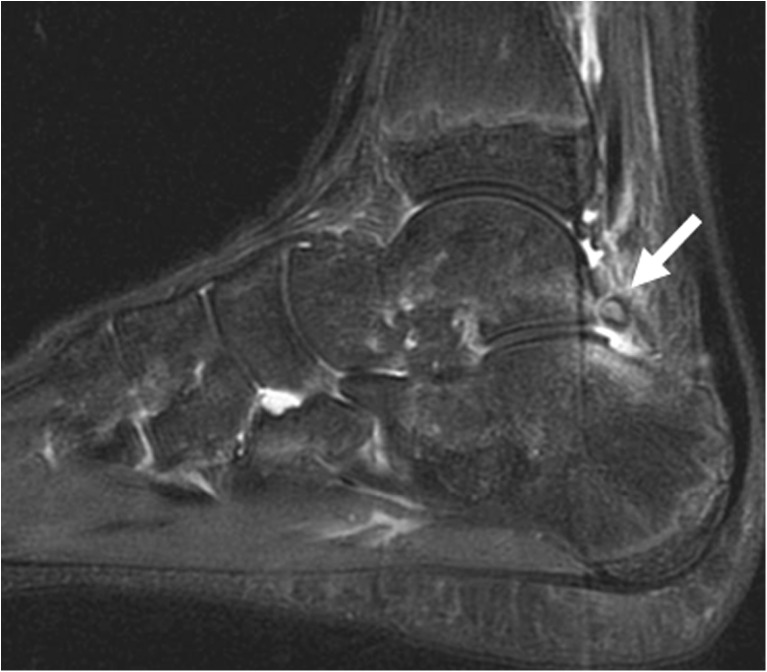
Imaging Features
MRI is useful in evaluating osseous causes of posterior impingement and can demonstrate bone marrow edema at the synchondrosis of an os trigonum (Fig. 4a). Soft tissue impingement may manifest as synovitis, scarring, and soft tissue edema. Dynamic ultrasound is useful in demonstrating motion at the os trigonum synchondrosis or an un-united fracture [48, 80], and poor excursion of the FHL tendon in cases of stenosing tenosynovitis. With plantar flexion, bony prominences may entrap adjacent posterior synovial recesses or the FHL tendon, causing soft tissue impingement (as described before under FHL tendon pathologies) (Fig. 2b, ESM 11).
Fig. 4.
A 14-year-old male dancer with posterior ankle pain. Sagittal inversion recovery MR image shows os trigonum with bone marrow edema both within the os (arrow in a) as well as the adjacent talus and calcaneus. This constellation of findings may be implicated in posterior impingement/os trigonum syndrome.
Management
Diagnostic steroid injections under ultrasound guidance can confirm the origin of pain and facilitate rehabilitative physiotherapy. We have also performed ultrasound-guided anesthetic injections without corticosteroid in cases where there is a diagnostic dilemma regarding the source of the patient’s symptoms. Structures involved in posterior impingement can be accessed by a needle via a lateral peri-Achilles approach placing the needle anterolateral to the Achilles tendon and advancing it anteromedially, thus avoiding the posterior tibial neurovascular bundle (Fig. 2a). However, one needs to remain cognizant to avoid inadvertent sural nerve injury lateral to the Achilles, as discussed earlier. Arthroscopic resection of an os trigonum or Stieda process is curative in dancers [80]. Operative release of the FHL tendon is effective in treating isolated stenosing tenosynovitis in ballet dancers.
Anterolateral Impingement
Chronic anterolateral foot pain can occur as a result of entrapment of abnormal soft tissues in the anterolateral gutter of the ankle. Predisposing factors include minor repetitive microtrauma from inversion injuries with forced plantar flexion and supination at the ankle, which results in hemorrhage and subsequent scar remodeling of the anterolateral capsule. Clinically, the patient presents with focal tenderness and limitation of movement in dorsiflexion. Additional contributing factors include hypertrophy of the accessory fascicle of the inferior anterior tibiofibular ligament, which may be worsened by adjacent osseous spurs [80].
Imaging Features
MR imaging is useful in assessing not only the bone marrow and cartilage status, but also synovitis and alternative intra-articular etiologies. Axial images may demonstrate scarring in the anterolateral gutter with intermediate to low signal intensity on T1 and fluid sensitive images (Fig. 5). Synovitis and scarring may show anterior displacement of normal fat anterior to the fibula best seen on sagittal T1 images. Enhancing vascularized synovial tissue in anterolateral gutter can be seen utilizing highly sensitive contrast enhanced fat suppressed 3D gradient recalled MR acquisition technique, although this finding is not very specific [22, 80]. Ultrasound finding of synovial mass or capsular nodularity in the anterolateral gutter has been shown to be validated well with arthroscopic technique [22, 62]. Using arthroscopy as a reference standard, it has been shown that the sensitivity and specificity of diagnostic sonography is 77% and 57% before joint injection and 85% and 71% after joint injection [18].
Fig. 5.
A 42-year-old female ballet dancer with lateral ankle pain and fullness. Axial intermediate weighted MR image at the level of the lateral gutter of the ankle joint demonstrates diffuse thickening and scar encasement of the anterior talofibular ligament (arrow in a) in a patient with symptoms of anterolateral impingement (T talus; F fibula). Ultrasound-guided diagnostic and therapeutic injections can be performed at this site to assess symptom relief.
Management
Targeted steroid injections under ultrasound guidance can confirm the origin of pain. Surgical debridement of synovitis and scarring has considerable proven success [14, 44].
Ligamentous Injuries of the Foot and Ankle
The most common injuries encountered in ballet dancers are no surprise ankle ligamentous injuries. Of these, lateral ligament injuries particularly the anterior talofibular ligament injuries are more common than medial deltoid ligament complex injuries in ballet dancers [29].
Lateral Ligament Complex Injuries
Plantar flexion and inversion mechanism is responsible for lateral ligament injuries. The anterior talofibular ligament which is the weakest of all, is injured first, followed by the calcaneofibular ligament. The posterior talofibular ligament is rarely injured.
Medial Ligament Complex Injuries
Medial ankle sprains due to deltoid ligament complex injuries are less common in ballet dancers. The superficial component that is comprised of the tibiocalcaneal, tibionavicular and tibiospring fibers, as well as the deep component made up of the anterior and posterior tibiotalar fibers, should be evaluated.
Imaging Features
On MRI, high signal fluid will be seen interposed between the disrupted fibers on T2-weighted or inversion recovery sequences. In the acute setting, bone marrow edema may be seen at the attachment sites of the torn ligament (Fig. 6a). On ultrasound, partial ligamentous tears appear hypoechoic with some of the fibers remaining in continuity, while complete tears are seen as focal discontinuity with hypoechoic fluid or heterogeneous granulation tissue in between the torn segments (Figs. 6b and 7a, b). Provocative maneuvers placing traction on the ligament may make the tear more conspicuous on ultrasound. In chronic tears, the ligament may appear thickened due to scar formation.
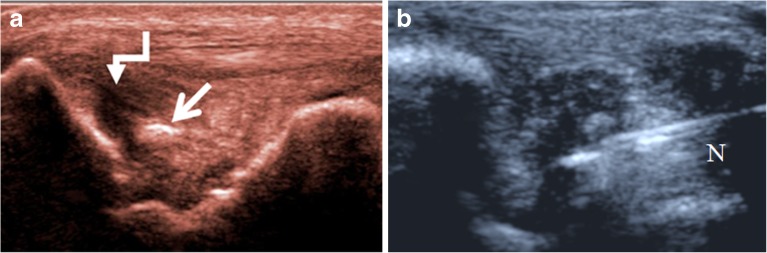
Fig. 6.
A 27-year-old female ballet dancer with acute on chronic lateral ankle pain. a Inversion recovery MRI axial image demonstrates absent anterior talofibular ligament fibers with fluid within the anterolateral gutter (arrow). Ultrasound image longitudinal to the anterior talofibular ligament (ATFL) anterior to the tip of the fibula, shows hypoechoic fluid (asterisk) in the lateral gutter indicative of ATFL tear without demonstrable intact overlying ATFL fibers with a suggestion of minimal hypoechoic discontinuity (arrow in a) at the fibular tip (F fibula).
Fig. 7.
a, b A 29-year-old female ballet dancer with medial ankle pain. a Coronal image distal to the medial malleolus shows a high-grade tear involving the proximal portion of the superficial fibers (curved white arrow) of the deltoid ligament. Small ossific fragment (straight arrow) represents a medial malleolar avulsion fracture. b Coronal image of a different patient undergoing PRP injection of the deltoid (N needle).
Management
Ankle sprains are managed conservatively with a view to early mobilization to avoid joint stiffness, muscle atrophy, and loss of proprioception [29]. Sonographically guided steroid injections allow symptomatic pain relief for partial thickness ligament tear. Instillation of autologous blood products such as PRP directly at the injury site has gained interest lately and is believed to potentially promote healing [24]. Recent review article discussed the clinical applications of PRP in orthopedics [24]. However, no randomized controlled trials with validated outcomes have been done yet and it remains an area of growing research. Injury involving both the anterior talofibular and calcaneofibular ligaments is unstable and may require primary surgical repair in professional dancers [90].
Lisfranc Ligament Injuries
Although Lisfranc (tarsometatarsal joint) ligament injuries classically occur in the setting of high-velocity impact, they can be seen in ballet dancers due to forced plantar flexion at the ankle and the metatarsophalangeal joint from long hours in en pointe. Full body weight transmitted along what is functionally an elongated lever arm results in failure of the joints dorsally [38, 46].
Imaging Features
Radiographically, widening between the medial cuneiform and base of the second metatarsal by more than 2 mm is diagnostic. CT may disclose unsuspected fractures. MRI allows detailed evaluation of the plantar and dorsal components of the Lisfranc ligament fibers [38]. Ultrasound has limited utility but can evaluate for avulsion fractures.
Management
Non-operative treatment is limited to stable Lisfranc complex injuries and include nondisplaced, with no fracture and stable under radiographic stress examination [6, 46]. Treatment includes controlled ankle motion (CAM) walking boot, with frequent follow-up radiographs to ensure no change in alignment. In unstable Lisfranc injuries, open reduction with internal fixation (ORIF) is necessary. Known complications include non-union as well as early post-traumatic arthritis.
Plantar Fascia
The plantar fascia is a fibrous aponeurosis that takes its origin from the medial calcaneal tuberosity and helps to maintain the longitudinal arch of the foot. Heel pain is not as common in dancers as might be expected [47]. Plantar fasciitis has been shown to be the most common cause of heel pain [47]. Plantar fasciitis is a low-grade inflammatory process manifested by abnormal thickening of the proximal calcaneal origin of the plantar aponeurosis (PA), with or without plantar fascial tears. The etiology of plantar fasciitis is variable, but can be grouped into three major categories: mechanical, degenerative, and systemic [64]. Forcible plantar flexion can cause acute (complete or partial) rupture of the PA, whereas chronic repetitive stress or minor trauma may also result in rupture. Plantar fasciitis, especially the ones treated with local steroid injections can predispose to spontaneous rupture of the PA [64].
Imaging Features
On MRI, plantar fasciitis manifests as proximal plantar fascial thickening (>5 mm) [64], often with substantial adjacent calcaneal bone marrow edema (Fig. 8). Plantar fascial tears are seen as hyperintense foci on T2-weighted or inversion recovery sequences. On ultrasound, plantar fasciitis manifests as thickening of the plantar fascia at its calcaneal origin with intrinsic increased vascularity, while plantar fascial tears demonstrate hypoechoic fluid replacing the fascial tissue (Fig. 8).
Fig. 8.
A 45-year-old female ballet dance instructor with heel pain (a, b). a Ultrasound of the heel in long axis to the plantar fascial origin shows hypoechoic thickening of the plantar fascia, measuring 7 mm (normal 4 mm), with a deep surface partial tear at the medial plantar fascial origin (arrow in a). b Ultrasound image shows subsequent needle insertion (N) as part of a PRP injection for the treatment of plantar fasciitis. c Sagittal inversion recovery image in a different patient, shows a partial thickness tear of the medial band of the plantar fascia (arrow in c) in the setting of plantar fasciitis eliciting slight stress reaction within the calcaneus (arrowhead) and soft tissue edema in the heel pad.
Management
Pre-rehearsal stretching of the fascia can reduce incidence of injury [47]. Initial and ongoing conservative measures provide benefit and include weight loss, orthoses, activity modification as well as physical therapy including stretching and taping measures. Ultrasound-guided perifascial corticosteroid injections offer symptomatic relief due to their anti-inflammatory properties during the acute and subacute stages [1, 19, 64]. Alternative interventional methods focussed at triggering a healing response by controlled injury include dry needling, PRP injections and extracorporeal shock wave therapy (ECSW) [40]. At our institution, perifascial ultrasound-guided steroid injections are performed with the needle placed immediately superficial to the site of pathology and advanced either longitudinally or transversely relative to the plantar fascia. Alternatively, ultrasound-guided needle fenestration of the fascia and platelet-rich plasma (PRP) injection is routinely performed successfully at our institution and has shown improved clinical outcome, especially in more chronic cases where steroids are of little benefit. A study comparing ultrasound-guided fenestration and tenotomy for PRP and steroid injections in patients with plantar fasciitis showed good results with PRP in comparison to steroid [95]. Additional studies have shown that PRP is a safe therapeutic option with the ability to decrease heel pain in patients with chronic PF refractory to appropriate conservative management, without any serious side effects [95, 103]. PRP works by reigniting the inflammatory cascade and thereby promoting healing [95]. Extracorporeal shockwave therapy is a safe and effective treatment for pain relief from recalcitrant plantar fasciopathy and additionally has been shown to improve gait parameters [40].
Morton’s Neuroma
Morton’s neuroma is a non-neoplastic encasement of a common plantar digital nerve by perineural fibrosis due to repetitive microtrauma, producing a pseudotumor which may or may not be painful. Morton’s neuroma is most common in the third web space because the third digital nerve is the largest and receives branches from both the medial and lateral plantar nerves [11]. The exact etiology of Morton’s neuroma remains unknown and several theories have been proposed, including ischemia and mechanical compression of the plantar nerve against the transverse intermetatarsal ligament [11]. Morton’s neuroma is common in joggers, and can occasionally be seen in dancers [94]. Clinical assessment can be accurate for the diagnosis of Morton’s neuroma; both MRI and US are very useful in its localisation. MR imaging allows determination of site and size of Morton’s neuroma and therefore plays a crucial role in the diagnosis and therapeutic decisions by orthopedic surgeons as shown by Zanetti et al. US and MRI both demonstrate high sensitivities for the diagnosis of Morton’s neuroma ranging from 87–98% [8, 107]
Imaging Features
MR imaging at the level of the metatarsal heads, obtained in short axis (Fig. 9a) and coronal planes, is most useful. These are typically seen as “tear drop”-shaped hypointense masses [23, 108] with variable gadolinium contrast enhancement. Ultrasound imaging performed just proximal to the metatarsal heads, demonstrates well circumscribed, ovoid, hypoechoic, nodular masses (Fig. 9b, c), at the level of the intermetatarsal spaces, which become more prominent with ankle plantar flexion [99]. Manual palpation and compression of the web space by the ultrasound probe often reproduces the symptoms.
Fig. 9.
a, b, c A 23-year-old dancer with forefoot pain. a Transverse intermediate weighted MR image at the level of the metatarsal heads demonstrates a teardrop-shaped hypointense lesion in the second web space (arrow), reflecting a Morton’s neuroma. b Ultrasound image in the sagittal plane at the level of the second web space shows a non-compressible hypoechoic neuroma (arrow). c Ultrasound-guided therapeutic steroid and anesthetic injection into the Morton’s neuroma (N needle).
Management
Ultrasound-guided steroid injection into and around the neuroma gives considerable initial pain relief, with one study demonstrating 62% of symptomatic pain relief at 7 days [37]. The ultrasound probe is placed along the plantar or dorsal surface of the web space depending on the side that allows better visualization, and a 1.5″ hypodermic needle is advanced into and around the neuroma into the intermetatarsal bursa, with direct visualization of fluid spreading within the lesion on sonography without leaks. The patients are instructed not to engage in strenuous activity immediately after injection to avoid dispersal of injectate. Return to full activity 1 day after injection is permissible. Preoperative workup with clinical examination, diagnostic 1% lidocaine only injections followed by surgical excision, does not always result in good clinical outcome [9]. Surgical excision of neuromas has yielded variable results. Overall, 20% of patients experience less than 50% pain relief after surgical excision. According to one series, it has been shown that almost 24% of primary excision and 43% of re-excision of stump neuromas are clinical failures with residual pain, persistent need for shoe modification and cosmetic issues with scar formation [85]. Postsurgical stump neuroma formation is generally symptomatic only when they recur close to the skin, joint capsule, or under the metatarsal heads [85]. To avoid this complication, the transected nerve edge is placed into the muscle which results in smaller recurrent stump neuroma and moves their location of recurrence away from the symptomatic area. Activity modification and proper shoe wear are often needed even after surgical resection [85]. A few percutaneously treated neuromas have demonstrated a change in morphology from typical hypoechoic to more echogenic appearance on follow-up examination. However, further randomized controlled research is needed to document post-treatment change in morphology and correlation between the number and size of neuromas and clinical outcome after percutaneous steroid treatment.
Osseous Injuries in the Foot and Ankle
Repetitive plantar and dorsiflexion in dancers can result in chronic overuse subchondral stress osseous injuries. The second metatarsal is the longest of all the metatarsals and is weight-bearing when the foot is in the demi pointe position [33] and is therefore the most common site of stress fracture in the foot and ankle (Fig. 10a, b). Calcaneal stress fractures from overuse are not uncommon (Fig. 10c, d). The Stieda process of the talus can be a source of pain and may fracture in the setting of posterior impingement. Sesamoids are small bones which articulate with the plantar aspect of the metatarsal heads and are embedded in the flexor hallucis brevis (FHB) tendons. Since ballet predisposes the sesamoids to significant force during demi pointe and en pointe as well as in jump landings, it is not uncommon for dancers to present with MTP pain, which may be due to sesamoiditis (Fig. 10e, f, g), sesamoid fractures, premature osteoarthritis, or even sesamoid osteonecrosis (Fig. 10h, i) [33, 44]. Repeated subchondral stress from prolonged plantar flexion predisposes the ballet dancers to osteochondral injury of the talar dome [44]. Avulsion fractures can be a complication of ligamentous sprain in the foot and ankle. Posteromedial impingement lesion can occur after severe ankle inversion and excessive plantar flexion [47].
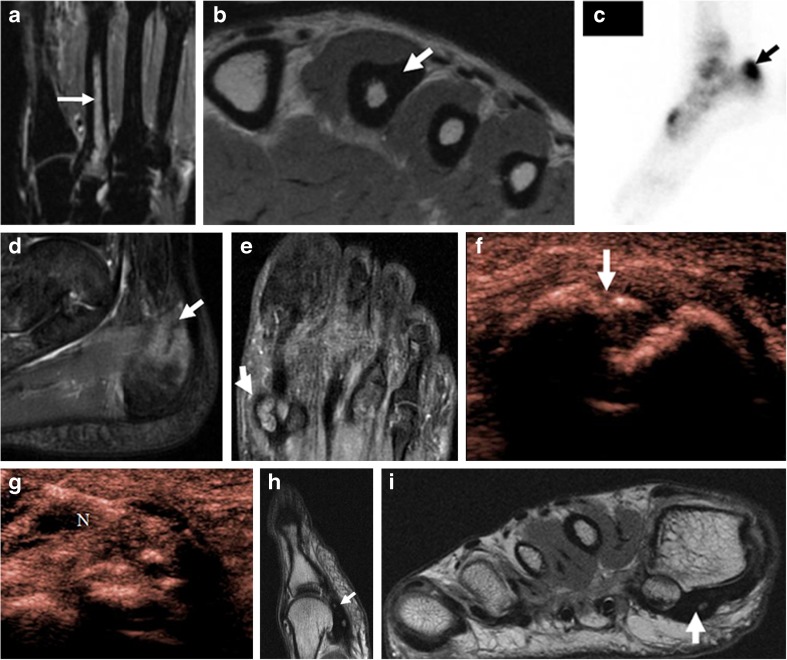
Fig. 10.
a, b A 27-year-old female ballet dancer with pain and soreness of foot. a Coronal inversion recovery MR image shows bone marrow edema within the second metatarsal (arrow) reflecting an acute stress reaction. b Axial intermediate weighted MR image of the same patient shows prominent cortical thickening (arrow) of the metatarsal shaft secondary to chronic stress remodeling. c, d A 24-year-old female ballet dancer with heel pain. c Delayed phase of three phase bone scan in a patient with posterior ankle pain demonstrates focal increased radiotracer uptake within the posterior calcaneus (arrow). d Sagittal inversion recovery MR image demonstrates a well-defined stress fracture (arrow) within the posterior calcaneus with surrounding bone marrow edema. e, f, g A 22-year-old female ballet dancer with pain and tenderness over the ball of her foot. e Coronal inversion recovery MR image demonstrates a bipartite medial sesamoid with a small fracture at the distal pole with bone marrow edema (arrow e). f Ultrasound over the plantar surface of the great toe, long axis to the sesamoid, shows a small fracture at the distal pole of a bipartite medial sesamoid (arrow). g Ultrasound-guided therapeutic steroid injection was performed around the sesamoid (N needle). h, i A 23-year-old female dancer with chronic pain and tenderness under the great toe for several months. Sagittal (h) and axial (i) intermediate weighted MR images show chronic osteonecrosis (arrow) of the medial sesamoid with collapse.
Imaging Features
Stress reaction on MRI is seen as bone marrow edema on fat saturated T2-weighted or inversion recovery sequences and is commonly seen in the second metatarsal, calcaneus, and talus. Variable increased bone marrow signal is seen in the acute or subacute phase of avascular necrosis of the sesamoid, while predominantly hypointense signal with eventual fragmentation and collapse may be seen during the chronic phase. In contrast, stress fractures demonstrate a clearly defined hypointense fracture line within the area of bone marrow edema. On ultrasound, stress fractures can be detected as cortical disruption and hyperemia when there is involvement of the cortex. Focal pain at the site upon pressure with the transducer is a helpful secondary sign.
Management
Ultrasound-guided diagnostic and therapeutic injections allow symptomatic management and earlier return to practice (Fig. 10e), [33, 83]. Stress reaction and nondisplaced fractures are routinely managed conservatively with non-weight-bearing and immobilization. ORIF may be needed for displaced fractures or with non-union.
Hip
MRI serves as the primary imaging modality in the hip and allows for assessment of intra-articular pathologies. Although the deeper structures of the hip make ultrasound less useful, ultrasound can be valuable for dynamic assessment, such as in cases of snapping hip syndrome or impingement syndromes, and for administering specific intervention. Apophyseal avulsion fractures and apophysitis from overuse are common in young dancers and are well evaluated on MRI.
Hip Instability
In a dancer, the hip joint is one of the most important joints, as it controls both the trunk and extremity motion. The ability to externally rotate (turn out) the hip is one of the fundamental aesthetic poses of ballet. Incorrect “turnout” is the most common cause of stress and soft tissue injury around the hip [33]. Upon ossification of the femoral head, “turnout” can only be achieved by stretching adjacent soft tissues. Chronic increased capsular tension can lead to injury of the static hip stabilizers, resulting in painful acetabular labral tears, iliofemoral ligament injury, capsular redundancy, and subsequent microinstability [70].
Acetabular Labrum
The acetabular labrum consists of fibrocartilage that attaches to the bony acetabular rim and deepens it, thereby preventing dislocation of the femoral head. Extreme external rotation can cause the head of the femur to sit too far forward in the acetabulum, which eventually gives way. The dancers will experience stiffness in the affected hip and may have difficulty with arabesque position (dancer stands on one leg, while the other leg is extended behind the body) or any extension over 90°. Atraumatic instability is an overuse injury from repetitive hip rotation with axial loading, leading to microinstability and generalized ligamentous laxity [33].
Imaging Features
On MRI, a linear high intensity cleft suggestive of tear can be seen through the normally low signal intensity labrum (Fig. 11a) [87]. Evaluation for labral tears is much more difficult on US. However, a hypoechoic cleft representing the tear can occasionally be visualized through the normally hyperechoic labrum on targeted sonogram (Fig. 11b). According to an institutional study of 21 hips, 13 hips shown to have anterior labral tears seen as hypoechoic clefts during sonographically guided intra-articular hip injections were shown to be concordant with the MR findings. However, this study is limited since only 14 patients underwent MRI [87]. The tear can sometimes become apparent after US-guided intra-articular injection, in which the injectate can provide a “sonoarthrographic effect” (Fig. 11c). Although intra-articular injection during sonographic examination could improve diagnosis of labral tears, sonographic examination as a diagnostic technique is still of limited use. However, CT arthrogram (CTA) shows reliable validity in the diagnosis of acetabular labral tears. The sensitivity, specificity, and accuracy for sonographic detection of labral tear before injection/after injection were 58%/79%, 67%/58%, and 61%/72%, respectively, for observer 1 and 75%/92%, 25%/42%, and 58%/75%, respectively, for observer 2. The sensitivity, specificity, and accuracy for CTA detection of labral tears were 96%, 92%, and 94%, respectively, for observer 1 and 88%, 92%, and 89%, respectively, for observer 2. When the sonographic classification was compared with the arthroscopic findings of observer 1 and observer 2, the accuracy before injection/after injection was only 53%/67% and 58%/75%, respectively. The accuracy of morphologic classification of CTA and arthroscopic findings of observer 1 and observer 2 was 83% and 75%, respectively [83]. According to a 2007 study, the ability to diagnose acetabular labral tears upon US examination was calculated: sensitivity 44%, specificity 75%, positive predictive value 88%, and negative predictive value 25% [45]. However, according to a 2012 study, the sensitivity, specificity, and accuracy for the diagnosis of tears by sonography and MR arthrography were 82%, 60%, and 75% and 91%, 80%, and 88%, respectively using arthroscopic results as the reference standard [106]. However, it is crucial to bear in mind that the quality of MR imaging can demonstrate considerable institutional variation and can tremendously influence the outcome.
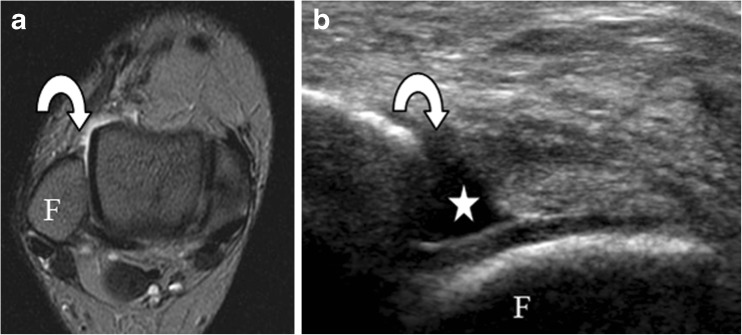
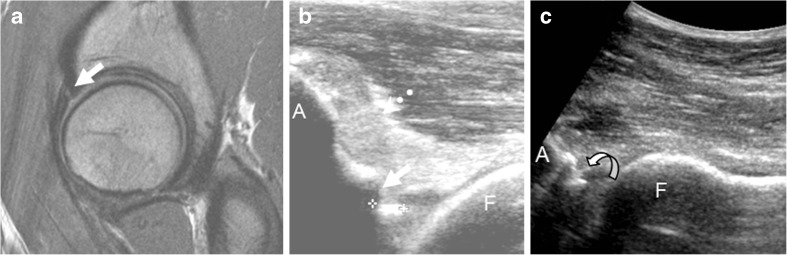
Fig. 11.
a, b, c A 39-year-old female dancer with chronic anterolateral hip pain. a Sagittal intermediate weighted fast spin echo magnetic resonance image shows anterior labral tear extending to the articular surface (arrow). b Corresponding longitudinal ultrasound image demonstrates complex anechoic cleft in the anterior labrum which extends to the articular surface (likely representing labral tear) with associated intralabral ossification (straight arrow in b) and capsular thickening (dotted arrow in b). c Following injection, there is fluid imbibition into the labral tear (arrow in c).
It has been suggested that the increased intra-articular pressure secondary to the loss of congruency between the femoral head and the acetabulum can force synovial fluid through the area of labral degeneration or through the tear in the acetabulum, resulting in a paralabral cyst. It is reasonable to assume that pain in this condition is caused by the cyst stretching the hip joint capsule and by the labral tear. These paralabral cysts, when large, can cause mass effect on the surrounding structures including regional nerves. On MRI, paralabral cysts appear as T2 hyperintense and T1 hypointense foci adjacent to a labral tear. Sometimes paralabral cysts are seen in absence of identifiable labral tears and may represent ganglion cyst (Fig. 12a, b). Cyst decompression combined with labral debridement is generally accepted as the optimal treatment. This can be performed through an open or arthroscopic surgical approach, with minimally invasive arthroscopic surgery considered the preferred treatment method for those conditions to avoid the morbidity of an open surgical procedure [51]. At our institution, US guidance is utilized for aspiration of paralabral or ganglion cysts, which are easily seen as anechoic or hypoechoic fluid collections (Fig. 12c, d). Treatment of these cysts in the hip under sonographic guidance is limited in the literature and restricted to radiographic findings.
Fig. 12.
a, b Axial T2 fat-saturated and T1 fast spin echo MRI series in a 15-year-old female dancer without a definitely identifiable acetabular labral tear but only a well-demarcated posterior paralabral cyst presumably a ganglion cyst (arrow in a and b) compressing sciatic nerve (arrowhead in a and b). c, d Longitudinal hip sonogram in a 15-year-old female dancer with painful left posterior ganglion cyst in close proximity to the sciatic nerve (arrowhead in a and b). Pre (arrow in c) and post (arrow in d) ultrasound-guided paralabral ganglion cyst aspiration.
Management
Ultrasound-guided intra-articular steroid injections can provide short-term symptomatic pain relief for labral tears [33]. Ultimately, surgical debridement and repair of complex or displaced tears may be necessary.
Snapping Hip Syndromes/Coxa Saltans
The snapping hip syndrome refers to a sudden snapping sensation during hip motion. The snapping hip syndrome is a common problem in ballet dancers (43.8% of hip problems), with about one third associated with pain [16, 77]. Three types of snapping hip syndromes have been described in the literature, namely external/lateral, internal/medial, and intra-articular [77]. External snapping hip commonly affects the stationary or non-active supporting leg, wherein the thickened posterior iliotibial band or leading anterior edge of the gluteus maximus tendon snaps over the greater trochanter upon forward flexion [77, 105]. Internal or medial snapping, which is the most common, usually affects the active leg of a dancer and is believed to be due to the iliopsoas tendon snapping over the adjacent iliopsoas muscle fibers. The third type, which is due to intra-articular causes such as labral tears, chondral lesions, synovial chondromatosis or loose bodies, is no longer referred to as a snapping hip because the diagnosis of intra-articular pathology is more accurate. Femoroacetabular impingement (FAI) syndromes are an important cause of hip pain in ballet dancers. They can be divided into cam, pincer, or mixed types and can contribute to hip pain in athletes including ballet dancers. A detailed discussion of FAI is beyond the scope of this manuscript and additional references are suggested [71, 73, 91]. Stress fractures of the hip can often be easily overlooked and may progress to complete fracture with continued weight-bearing.
Imaging Features
Self-reported snapping is likely to be palpable/audible click elicited clinically and exaggerated by certain dance maneuvers. Iliotibial band snapping is easier to identify than iliopsoas snapping due to ease of clinical examination during provocative maneuvers. US demonstrates a high sensitivity for iliopsoas snapping, and therefore serves as a useful tool for diagnosis confirmation. However, in one third of the cases, ultrasound is not useful in identifying the cause of snapping [3]. On static imaging, the offending tendon often appears normal, although peritendinous fluid, tendinosis, and adjacent bursitis may be seen (Fig. 13). Dynamic sonography allows documentation of the tendon jerk/snap with hip motion. For lateral/external snapping, a snap would be palpated over the greater trochanter during ronde de jambe (hip circumduction) and grand plié (deep knee bends) while the dancer is bearing weight. An internal/medial click can be palpated with passive hip flexion, hip abduction, and hip external rotation [3].
Fig. 13.
a, b A 39-year-old female dancer with acute lateral hip pain during rehearsal. Longitudinal extended field of view (a) and transverse (b) images of the tensor fascia lata shows muscle edema (white arrow) and subfascial fluid (asterisk) deep to iliotibial band (ITB).
Management
Ultrasound-guided therapeutic iliopsoas peritendinous steroid injections provide symptomatic pain relief in those with a snapping iliopsoas regardless of demonstrable imaging findings in symptomatic patients [88, 97]. Surgical release of the snapping tendon is curative [42]. Arthroscopic debridement of intra-articular loose bodies may also be curative.
Greater Trochanteric Pain Syndrome
Greater trochanteric pain syndrome (GTPS) is a clinical entity that was originally defined as “tenderness to palpation over the greater trochanter [89].” This terminology has now expanded to include several disorders of the lateral, peritrochanteric space of the hip, including trochanteric bursitis, tears of the gluteus medius and minimus, and external coxa saltans (snapping hip). This is a common entity often responsible for chronic pain in dancers that may be mistaken for a hip fracture [82]. Gluteus medius tendinopathy is believed to be the initiating disorder followed by greater trochanteric bursopathy.
Imaging Features
Ultrasound imaging of gluteus medius tendinopathy may demonstrate increased tendon thickness, increased hypoechogenicity, loss of fibrillary pattern, intrinsic tendon tears and presence of insertional calcifications or enthesophytes. Calcifications appear as echogenic intratendinous foci which demonstrate posterior acoustic shadowing, whereas enthesophytes are seen as small echogenic bony projections emanating from the greater trochanteric surface within the tendon. Tendon tears appear as loss of continuity of the hypointense tendon fibers by anechoic foci with or without retraction. On US, trochanteric bursal thickening manifests as hypoechoic foci that may demonstrate hyperemia on power Doppler. GTPS associated with gluteus medius tendinopathy has been shown to benefit from US-guided steroid injection [50]. On MRI, bursal thickening manifests as high T2 signal in the greater trochanteric bursa often in the setting of tendinopathy of the gluteus medius and minimus tendons.
Management
Conservative treatment is the primary therapy with physical therapy and judicious use of US-guided steroid. Although uncommon, if there is a visible distended bursal sac, that site itself can be targeted for sonographic guided steroid injection. In the absence of a distended greater trochanteric bursa, peritendinous injection superficial to the gluteus medius tendon insertion provides symptomatic relief [50]. Surgery is also an option, as there is a growing interest in using primary abductor repair and endoscopic trochanteric bursectomy.
Osseous Injuries
Stress fractures of the femoral neck and acetabulum can occur uncommonly with overuse. Adolescent athletes can sustain physeal and bony stress injuries. Ballet dancers and gymnasts often show delayed skeletal maturity and thus may experience these injuries at a much later chronological age. The ischial apophysis, the attachment site of the hamstring tendons and adductor magnus, begins to ossify at 13–15 years of age and fuses to the pelvis by 16–25 years. Ischial tuberosity avulsion fractures are common in dancers, runners, and soccer players due to forceful hip flexion and knee extension [27]. The hamstring muscle group is susceptible to injury for several reasons: one component, the biceps femoris, has two heads of origin, it crosses two joints, and it is made up of type 2 muscle fibers that produce a more powerful contraction [67]. Apophyseal avulsion may be cartilaginous or osseous and occur due to vigorous hamstring contraction with the hip flexed or knee extended. Apophysitis is a chronic traction injury without bony avulsion. Alternatively, the injury can occur not at the apophysis but primarily within the muscle or tendon.
Imaging Features
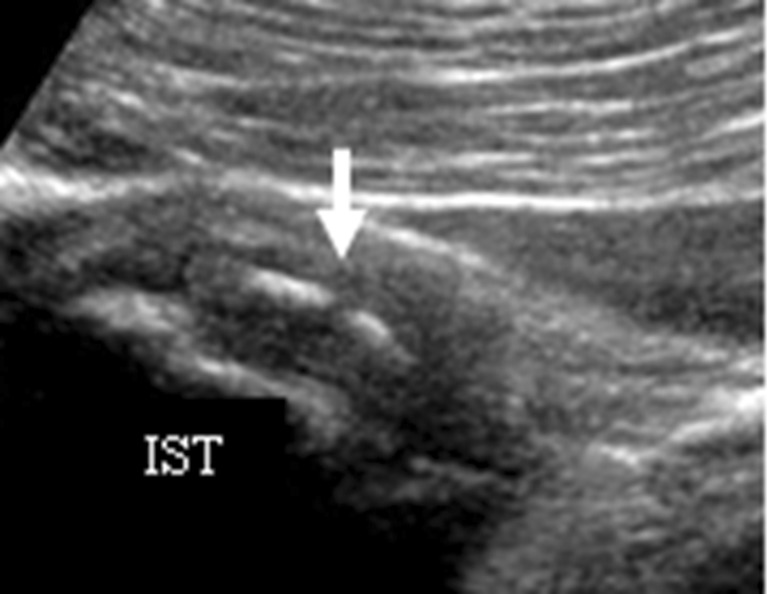
Avulsion fracture of the ischial tuberosity is seen as a sharply defined bone fragment, displaced inferior to the ischial tuberosity (Fig. 14). In skeletally immature dancers, forceful hip flexion can cause Salter I injury at the apophysis. On US, longitudinal scanning over the ischial tuberosity may demonstrate the displaced thin echogenic surface of the ischial tuberosity (Fig. 14) and US may reveal an associated hematoma at the site of the avulsion. However, sonography is less accurate than MRI for diagnosing proximal hamstring avulsion [96], because of deeper location of the ischial tuberosity, especially in obese or muscular patients. In addition, the presence of mixed echogenicity hematoma can make detection of the avulsed tendon difficult on sonography [96]. Chronic fractures demonstrate irregularity and bony remodeling at the site of avulsion. MRI is also more sensitive than sonography for detecting mild muscle strain due to its greater soft tissue contrast.
Fig. 14.
A 13-year-old ballet dancer with chronic hip pain. a Longitudinal sonographic image in the region of the ischial tuberosity (IST) with patient positioned in prone position, demonstrates thickened origin of the hamstring with multiple linear echogenic intratendinous areas of ossification/calcification (arrow), sequela of remote ischial tuberosity (IST) avulsion injury without tendon retraction.
Management
Conservative US-guided targeted therapeutic steroid injections may be useful in dancers with chronic refractory pain at the hamstring origin. Retrospective independent studies have shown that PRP is superior to traditional conservative treatment [100]. Ultrasound-guided PRP injections have been shown to provide moderate pain relief in majority of patients with tendinopathy [100]. A recent prospective study concluded that biologic therapies such as autologous blood (AB) and PRP injection were moderately effective for treatment of recalcitrant tendinopathy which failed to respond to conservative treatment, and PRP was more effective than AB [101]. Reliable independent randomized controlled trials regarding PRP injections for hamstring tendons are lacking, however, our institutional experience regarding PRP hamstring injections in ballet dancers has been promising. Non-operative treatment with only protected weight bearing is initially utilized. Surgery may be required for displaced avulsion fractures.
Knee
The most common knee injury in ballet dancers is proximal patellar tendon overuse injury, known as jumper’s knee [72]. Ballet dancers commonly face knee hyperextension injuries due to extreme laxity of the knee ligaments (loose ligaments). Hence, dancers often place excessive stress on the knee joint itself, instead of using muscle strength for movement. Injuries occur due to improper positioning when the dancer “locks” back into the knees. Medial collateral ligament (MCL) injury is the most common ligamentous injury around the knee in dancers [72, 104]. Anterior cruciate ligament injuries are less common in dancers than in athletes participating in team ball sports due to better lower extremity balancing skills, and they are usually related to fatigue [52]. Patellar tracking disorders can occur due to general ligamentous laxity or poor quadriceps muscle tone. Medial tibial stress syndrome affects the posteromedial tibial shaft and manifests as periosteal reaction without a defined fracture. High amounts of stress on the lower extremity can result in “shin splints” or tibial stress fractures in severe cases. Stress fracture of the anterior tibia is seen with the “bravura” style of ballet choreography, which emphasizes dramatic leaps producing large deceleration forces on the tibia. This style is commonly utilized by the American Ballet Theatre [33]. Aging dancers commonly experience anterior knee pain from chondromalacia due to wear of the patellar articular cartilage.
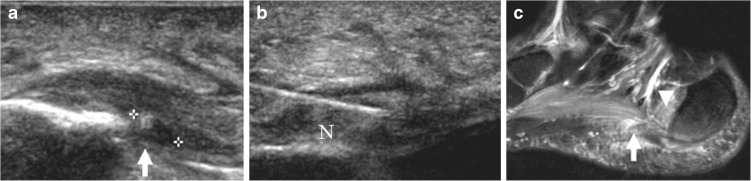
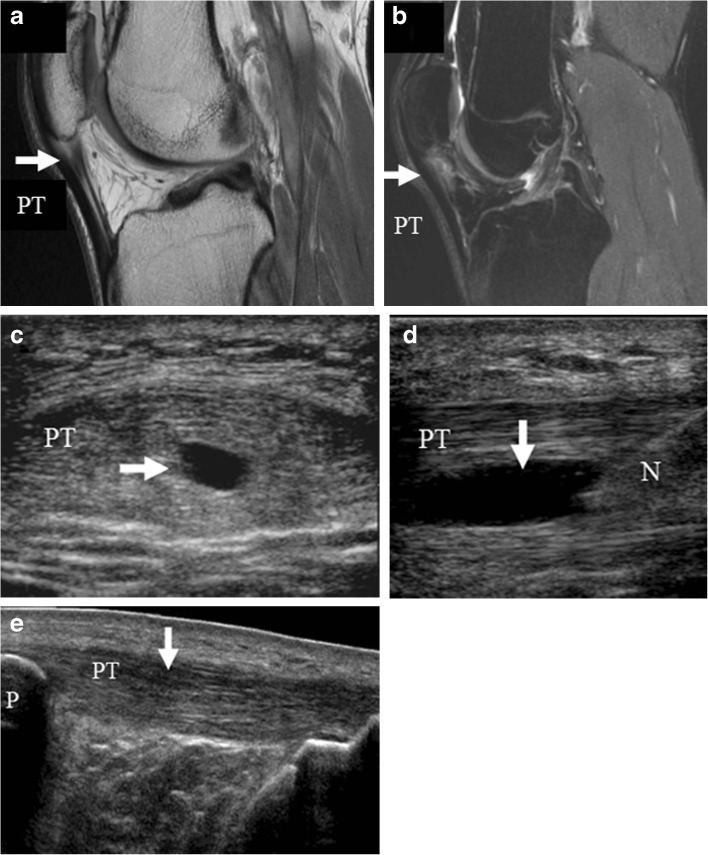
Imaging Features
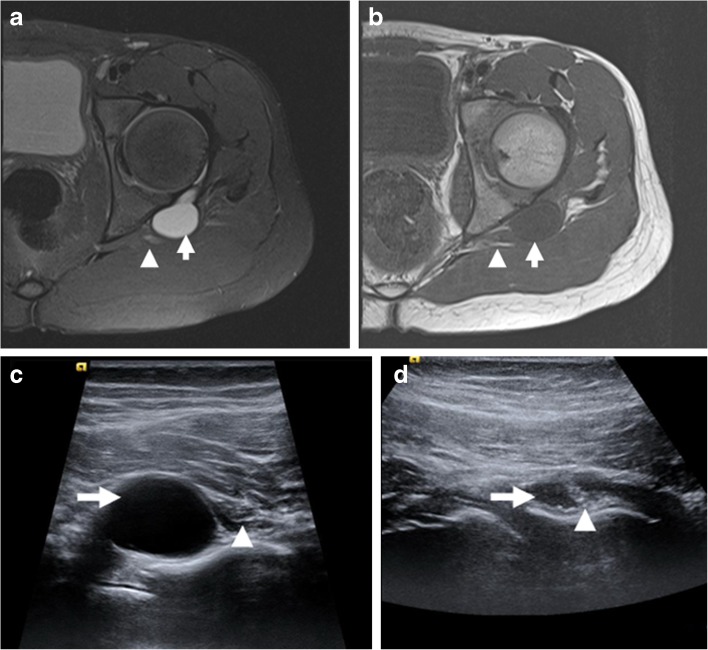
MRI provides detailed evaluation of deeper structures such as menisci and cruciate ligaments in the knee, which cannot be evaluated with US. MRI features of jumper’s knee include tendinosis manifested by thickening of the proximal patellar tendon and T2 hyperintensity with or without tear (Fig. 15a, b). Diagnostic US and targeted US-guided procedures can be easily utilized for more superficial structures such as the patellar tendon and the collateral ligaments. On ultrasound, patellar tendinosis alone manifests as hypoechoic thickening (Fig. 15c, d), often demonstrating concomitant hypervascularity on power Doppler imaging, while superimposed tears may be seen as partial or full thickness clefts within the substance of the tendon (Fig. 15c, d) [13]. Enthesophytic change and/or intratendinous ossification are not uncommon. Stress reactions and stress fractures would be easily visible on MRI but difficult to detect on US unless there is cortical disruption or exuberant periosteal reaction.
Fig. 15.
a, b, c, d, e A 24-year-old professional male ballet dancer with progressively worsening infrapatellar pain for several months. a, b Sagittal proton density and inversion recovery MR images demonstrate intrasubstance tear of the proximal patellar tendon in the setting of underlying tendinosis (arrows in a and b). Ultrasound images in short axis (c) and long axis (d) to the patellar tendon show longitudinal tear of the patellar tendon yielding intrasubstance fluid (arrows in c and d), with needle (N in d) directed to the tear as part of a PRP injection. d Follow-up panoramic ultrasound image of the patellar tendon 6 months later shows progressive healing of the tear (arrow in e) PT patellar tendon, TT tibial tubercle, P patella).
Management
Conservative management with physiotherapy is initially indicated for jumper’s knee. There is now evidence that chronic tendinopathy is related to inflammatory cascade as discussed in detail under Achilles tendinopathy management. Corticosteroid injections for short-term pain relief have been shown to be beneficial as shown by evidence-based research [17, 49]. Occasionally, focal debridement of areas of painful myxoid degeneration at the site of patellar tendinosis may be necessary. Ultrasound-guided needle tenotomy and PRP injection have shown clinically significant response with chronic refractory tendinopathy [28]. However, there is currently minimal scientific evidence in the form of a in vivo randomized controlled trial establishing that either PRP or autologous blood is effective when compared to placebo or no injection and further studies are going on. Alternative approach is to control pain by denervation procedures which aim to disrupt neural ingrowth which is accompanied by neovessel formation in chronic tendinopathy [5]. Emerging techniques in this area include sclerosant therapy (polidocanol and possibly dextrose) [4], high-volume tendon stripping injections [15] and surgical techniques such as paratenon stripping. As shock waves are toxic to nerves, it is possible that ESWT may influence pain processing due to direct effect on peripheral nerves [58].
Discussion
Behind a perfect evening of beautiful ballet performance lays the pain of endless hours of rehearsals. Behind beauty lies pain! Ballet is a physically challenging sport requiring immense dedication and long hours of rehearsals in demi pointe and en pointe position, making dancers prone to various orthopedic injuries. The most common site of injury is seen at foot and ankle, followed by hip and then knee. This review article has a twofold purpose, i.e., to outline the interesting imaging findings of commonly seen lower extremity injuries in ballet dancers and secondly to create some awareness about the available ultrasound-guided therapeutic interventions by giving a brief overview of our institutional experience. Successful management of these injuries involves a multidisciplinary approach with orthopedic surgeons, foot and ankle specialists, podiatrists, rehabilitation team as well as radiologists. Radiologists are the meeting point between various disciplines and have a key role to play. Radiologists can create added value by facilitating in quick diagnosis and recovery of these athletes for who time is life, with focus on shortening the recovery period whenever possible.
Ultrasound and MRI are two great radiation free modalities available to us today. MRI is immensely useful in assessing the deep structures, such as bone, cartilage, joints, synovium, neurovascular structures, labrum, and deep musculature. However, at this time, MRI is a static exam. Ultrasound on the other hand is a readily available, quick dynamic modality, which is also cost-effective. In the right hands, this modality allows real-time visualization of structures in motion while exposed to offending stimulus, for example episodic peroneal tendon subluxation is often times seen only during circumduction of the foot under dynamic sonography and may be missed on MRI. Secondly, the utility of ultrasound as a diagnostic as well as therapeutic modality is ever expanding. Since ultrasound offers excellent resolution for superficial structures, it is of great value in assessing pathologies of foot and ankle. Real-time ultrasound-guided injections are routinely used for both diagnostic (1% lidocaine injections for confirming the site of pain) and therapeutic (steroid/PRP injections) purposes at our institution. The drawback of ultrasound lies in the fact that it is operator dependent and cannot evaluate deeper structures such as bone marrow, cartilage, deep joints, and may be suboptimal in patients with large body habitus.
Our study has several limitations. Since ours is a review article based on our institutional experience, it is out of scope of this article to make recommendations regarding specific therapeutic interventional techniques, which would require a large-sample-sized double-blinded randomized observational study. Utilization of ultrasound as a diagnostic and therapeutic tool has tremendous inter-institutional and inter-user variability and its optimal utilization requires certain degree of hands on skill.
Of all the various dance forms, ballet places the most stringent physical demands on its performer. Ballet is an arduous activity requiring long hours of practice and balancing of the foot in en pointe or demi pointe position, which alters the normal biomechanics and predisposes the performer to a variety of lower extremity injuries. US and MRI play complementary roles in the diagnosis of lower extremity injuries in ballet dancers, with dynamic imaging and US-guided targeted interventions playing a crucial role in both the diagnosis and management of these injuries.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
ESM 7. A 27-year-old ballet dancer with lateral ankle pain. Dynamic cine clip imaged in short axis to the peroneal tendons with the patient actively circumducting at the level of the ankle shows intrasheath subluxation of the two tendons with respect to each other as well as subluxation onto and beyond the fibular tip with provocative maneuvers, reflecting laxity of the Q3 superior peroneal retinaculum. (AVI 50409 kb)
ESM 8. Cine images before and after surgery similarly demonstrate smoother motion of the FHL tendon after surgical release with active plantar and dorsiflexion of the big toe. (AVI 22014 kb)
ESM 9. Cine images before and after surgery similarly demonstrate smoother motion of the FHL tendon after surgical release with active plantar and dorsiflexion of the big toe. (AVI 24623 kb)
Disclosures
Conflict of Interest
Razia Rehmani, MD, Yoshimi Endo, MD, Phillip Bauman, MD, William Hamilton, MD, Hollis Potter, MD and Ronald Adler, MD, PhD have declared that they have no conflict of interest.
Human/Animal Rights
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed Consent
N/A
References
- 1.Adler RS, Sofka CM. Percutaneous ultrasound guided injections in the musculoskeletal system. Ultrasound Quarterly. 2003;19(1):3–12. doi: 10.1097/00013644-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Adler RS, Finzel KC. The Complementary Roles of MR Imaging and Ultrasound of Tendons. Radiol Clinic N Am. 2005;43(4):771–807. doi: 10.1016/j.rcl.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 3.Adler RS, Buly R, Ambrose R, et al. Diagnostic and therapeutic use of ultrasound guided Iliopsoas peritendinous injections. AJR. 2005;185(4):940–943. doi: 10.2214/AJR.04.1207. [DOI] [PubMed] [Google Scholar]
- 4.Alfredson H, Öhberg L. Sclerosing injections to areas of neo-vascularisation reduce pain in chronic Achilles tendinopathy: a double-blind randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. 2005;13:338–44. doi: 10.1007/s00167-004-0585-6. [DOI] [PubMed] [Google Scholar]
- 5.Alfredson H, Ohberg L, Forsgren S. Is vasculo-neural ingrowth the cause of pain in chronic Achilles tendinosis? An investigation using ultrasonography and colour Doppler, immunohistochemistry, and diagnostic injections. Knee Surg Sports Traumatol Arthrosc. 2003;11:334–8. doi: 10.1007/s00167-003-0391-6. [DOI] [PubMed] [Google Scholar]
- 6.Andrew Rosenbaum MD, Samuel Dellenbaugh MD, John DiPreta MD, et al. Subtle Injuries to the Lisfranc Joint. Orthopedics. 2011;34(11):882–887. doi: 10.3928/01477447-20110922-23. [DOI] [PubMed] [Google Scholar]
- 7.Benazzo F, Maffulli N. An operative approach to Achilles tendinopathy. Sports Med Arthroscopy Rev. 2000;8:96–101. doi: 10.1097/00132585-200008010-00009. [DOI] [Google Scholar]
- 8.Bencardino J, Rosenberg ZS, Beltran J, et al. Morton’s neuroma: is it always symptomatic? AJR Am J Roentgenol. 2000;175:649–653. doi: 10.2214/ajr.175.3.1750649. [DOI] [PubMed] [Google Scholar]
- 9.Biasca N, Zanetti M, Zollinger H. Outcomes after partial neurectomy of Morton’s neuroma related to preoperative case histories, clinical findings, and findings on magnetic resonance imaging scans. Foot Ankle Int. 1999;20(9):568–575. doi: 10.1177/107110079902000906. [DOI] [PubMed] [Google Scholar]
- 10.Blackmon JA, Atsas S, Clarkson MJ, et al. Locating the sural nerve during calcaneal (Achilles) tendon repair with confidence: a cadaveric study with clinical applications. J Foot Ankle Surg. 2013;52(1):42–7. doi: 10.1053/j.jfas.2012.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blitch LE, Chaney M, Dinucci AK, et al. Diagnosis and Treatment of Forefoot Disorders. Section 3. Morton’s Intermetatarsal Neuroma. J of Foot Ankle Surg. 2009;48(2):1067–2516. doi: 10.1053/j.jfas.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Na B, Bergman G, Oloff L, et al. The Flexor Hallucis Longus: Tenographic Techniques and Correlation of Imaging Findings with Surgery in 39 Ankles. Radiology. 2005;236:974–982. doi: 10.1148/radiol.2362040835. [DOI] [PubMed] [Google Scholar]
- 13.Bryson P, Lesniak, Dustin L, et al. Use of Ultrasonography as a Diagnostic and Therapeutic Tool in Sports Medicine. Arthroscopy. J Arthroscopy Related Med. 2014;30(2):151–280. doi: 10.1016/j.arthro.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 14.Cerezal L, Abascal F, Canga A. MR imaging of Ankle Impingement Syndromes. AJR. 2003;181(2):551–559. doi: 10.2214/ajr.181.2.1810551. [DOI] [PubMed] [Google Scholar]
- 15.Chan O, O’Dowd D, Padhiar N, et al. High volume image guided injections in chronic Achilles tendinopathy. Disabil Rehabil. 2008;30:1697–708. doi: 10.1080/09638280701788225. [DOI] [PubMed] [Google Scholar]
- 16.Choi YS, Lee SM, Song BY, et al. Dynamic sonography of external snapping hip syndrome. J Ultrasound Med. 2002;21(7):753–8. doi: 10.7863/jum.2002.21.7.753. [DOI] [PubMed] [Google Scholar]
- 17.Christian C, Skjong MD. Tendinopathy Treatment: Where is the Evidence? Clin Sports Med. 2012;31(2):329–350. doi: 10.1016/j.csm.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Cochet H, Pele E, Amoretti N, et al. Anterolateral Ankle Impingement: Diagnostic Performance of MDCT Arthrography and Sonography. AJR. 2010;194:6. doi: 10.2214/AJR.09.3650. [DOI] [PubMed] [Google Scholar]
- 19.Crawford F, Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev. 2003;3 doi: 10.1002/14651858.CD000416. [DOI] [PubMed] [Google Scholar]
- 20.De Vos RJ, Weir A, van Schie HTM, et al. Platelet-rich plasma injection for chronic Achilles tendinopathy. JAMA. 2010;303:144–9. doi: 10.1001/jama.2009.1986. [DOI] [PubMed] [Google Scholar]
- 21.Kader D, Saxena A, Movin T, et al. Achilles tendinopathy: some aspects of basic science and clinical management. Br J Sports Med. 2002;36:239–249. doi: 10.1136/bjsm.36.4.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Donovan A, Zehava SR. MRI of ankle and lateral hindfoot Impingement Syndromes. AJR. 2010;195(3):595–604. doi: 10.2214/AJR.09.4199. [DOI] [PubMed] [Google Scholar]
- 23.Fazal MA, Khan I, Thomas C. Ultrasonography and magnetic resonance imaging in the diagnosis of Morton’s neuroma. J Am Podiatr Med Assoc. 2012;102(3):184–6. doi: 10.7547/1020184. [DOI] [PubMed] [Google Scholar]
- 24.Foster T, Puskas B, Mandelbaum B, et al. Platelet-Rich Plasma from Basic Science to Clinical Applications. Am J Sports Med. 2009;37(11):2259–2272. doi: 10.1177/0363546509349921. [DOI] [PubMed] [Google Scholar]
- 25.Fredberg U, Ostgaard R. Effect of ultrasound-guided, peritendinous injections of adalimumab and anikinra in chronic Achilles tendinopathy. Scan J Med Sci Sports. 2009;19:338–44. doi: 10.1111/j.1600-0838.2008.00813.x. [DOI] [PubMed] [Google Scholar]
- 26.Fredberg U, Bolvig L, Pfeiffer-Jensen M, et al. Ultrasonography as a tool for diagnosis, guidance of local steroid injection and, together with pressure algometry, monitoring of the treatment of athletes with chronic jumper’s knee and Achilles tendinitis: a randomized, double-blind, placebo controlled study. Scand J Rheumatol. 2004;33:94–101. doi: 10.1080/03009740310004126. [DOI] [PubMed] [Google Scholar]
- 27.Frush T, Lindenfeld T. Peri-epiphyseal and Overuse Injuries in Adolescent Athletes. Sports Health: A Multidisciplinary Approach. 2009;1(3):201–11. doi: 10.1177/1941738109334214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Filardo G, Kon E, Villa S, et al. Use of Platelet Rich Plasma for the treatment of Refractory Jumper’s Knee. Int Orthopaedics (SICOT) 2010;34(6):909–915. doi: 10.1007/s00264-009-0845-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fong DT, et al. Understanding acute ankle ligamentous sprain injury in sports. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:14. doi: 10.1186/1758-2555-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gamboa JM, Roberts LA, Maring J, et al. Injury patterns in elite preprofessional ballet dancers and the utility of screening programs to identify risks characteristics. A J Orthop Sports Phys Ther. 2008;38(3):126–36. doi: 10.2519/jospt.2008.2390. [DOI] [PubMed] [Google Scholar]
- 31.Gross CE, Hsu AR, Chahal J, et al. Injectable Treatments for Noninsertional Achilles Tendinosis: A systematic Review. Foot Ankle Int. 2013; 32: 619. [DOI] [PubMed]
- 32.Hamilton WG. Stenosing tenosynovitis of the flexor hallucis longus tendon and posterior impingement upon the os trigonum in ballet dancers. Foot Ankle. 1982;3(2):74–80. doi: 10.1177/107110078200300204. [DOI] [PubMed] [Google Scholar]
- 33.Hamilton WG. Foot and ankle injuries in dancers. Clin Sports Med. 1998;7(1):143–173. [PubMed] [Google Scholar]
- 34.Hamilton WG, Geppert MJ, Thompson FM. Pain in the posterior aspect of the ankle in dancers. Differential diagnosis and operative treatment. J Bone Joint Surg Am. 1996;78(10):1491–500. doi: 10.2106/00004623-199610000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Hartgerink, Fessell, Jacobson Full versus Partial-thickness Achilles tendon tears: Sonographic Accuracy and Characterization in 26 patients with Surgical Correlation. Radiology. 2001;220(2):406–412. doi: 10.1148/radiology.220.2.r01au41406. [DOI] [PubMed] [Google Scholar]
- 36.Harmon K, Drezner J, Rao A. Platelet Rich Plasma for Chronic Tendinopathy. Br J Sports Med. 2013;47:9. doi: 10.1136/bjsports-2012-091941. [DOI] [PubMed] [Google Scholar]
- 37.Hassouna H, Singh D, Taylor H, et al. Ultrasound guided steroid injection in the treatment in the treatment of interdigital neuralgia. Acta Orthop Belg. 2007;73(2):224–9. [PubMed] [Google Scholar]
- 38.Hatem SF. Imaging of Lisfranc injury and midfoot sprain. Radiol Clin North Am. 2008;46(6):1045–60. doi: 10.1016/j.rcl.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 39.Heckman D, Gluck G, Parekh S. Tendon Disorders of the Foot and Ankle. Am J Sports Med. 2009;37(3):614–25. doi: 10.1177/0363546508331206. [DOI] [PubMed] [Google Scholar]
- 40.Hsu W-H, Lai L-J, Chang H-Y, et al. Effect of shockwave therapy on plantar fasciopathy A biomechanical Prospective. Bone Joint J Aug. 2012;95-B(8):1088–1093. doi: 10.1302/0301-620X.95B8.31497. [DOI] [PubMed] [Google Scholar]
- 41.Hurtwitz S, Philip EL. Image guided anesthetic injection into the painful foot or ankle as a guide to orthopedic treatment. App Radiology 2000; 29 (8).
- 42.IIizakiturri V, Chaidez C, Villegas P, et al. Prospective Randomized Study of 2 Different Techniques for Endoscopic Iliopsoas Tendon Release in the treatment of Internal Snapping Hip Syndrome. Arthroscopy: J Arthroscopic Related Surg. 2009;25(2):159–163. doi: 10.1016/j.arthro.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 43.Jaffee N, Gilula L, Wissman R, et al. Diagnostic and Therapeutic Ankle Tenography Outcomes and Complications. AJR. 2001;176:2. doi: 10.2214/ajr.176.2.1760365. [DOI] [PubMed] [Google Scholar]
- 44.Hillier JC, Peace K, Hulme A, et al. MRI features of foot and ankle injuries in ballet dancers. Br J Radiol. 2004;77(918):532–537. doi: 10.1259/bjr/60447506. [DOI] [PubMed] [Google Scholar]
- 45.Jung YJ, Kim G-U, Jee H-J, et al. Diagnostic Value of Ultrasound and Computed Tomographic Arthrography in Diagnosing Anterosuperior Acetabular Labral Tears. J Arthroscopic Related Surg. 2013;29(11):1769–1776. doi: 10.1016/j.arthro.2013.07.274. [DOI] [PubMed] [Google Scholar]
- 46.Kadel N, Boensish M, Teitz C, et al. Stability of Lisfranc joints in ballet pointe position. Foot Ankle Int. 2005;26(5):394–400. doi: 10.1177/107110070502600510. [DOI] [PubMed] [Google Scholar]
- 47.Kennedy J, Hodgkins C, Colombier J, et al. Foot and Ankle Injuries n Dancers. Int Sport Med J. 2007;8(3):141–165. [Google Scholar]
- 48.Valencia KM. Dance Related Injury. Phy Med Rehabil Clin N Am. 2006;17(3):697–723. doi: 10.1016/j.pmr.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 49.Kongsgaard M, Kovanen V, Aagaard P, et al. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scan J Med Sci Sports. 2009;19:790–802. doi: 10.1111/j.1600-0838.2009.00949.x. [DOI] [PubMed] [Google Scholar]
- 50.Labrosse J, Cardubak E, Leduc B, et al. Effectiveness of Ultrasound guided Corticosteroid Injection for the treatment of Gluteus Medius Tendinopathy. Am J Roent. 2010;194:202–206. doi: 10.2214/AJR.08.1215. [DOI] [PubMed] [Google Scholar]
- 51.Keun-Ho L, Youn-Soo, Lim SJ. Arthroscopic Treatment of Symptomatic Paralabral Cysts in the Hip. Orthopedics. 2013;36(3):e373–e376. doi: 10.3928/01477447-20130222-29. [DOI] [PubMed] [Google Scholar]
- 52.Liederbach M, Dilgen F, Rose D. Incidence of Anterior Cruciate Ligament Injuries among Elite Ballet and Modern Dancers. A 5 year Prospective Study. Am J Sports Med. 2008;36(9):1779–1788. doi: 10.1177/0363546508323644. [DOI] [PubMed] [Google Scholar]
- 53.Loftus ML, Endo Y, Adler RS. “Retrospective Analysis of Post-injection Ultrasound Imaging following Platelet Rich Plasma or Autologous Blood, Observational Review of Anatomic Distribution of Injected Material”. AJR. 2012;199(4):W501–5. doi: 10.2214/AJR.11.8075. [DOI] [PubMed] [Google Scholar]
- 54.Lo LD, Schweitzer ME, Fan JF, et al. MR imaging findings of entrapment of the flexor hallucis longus tendon. AJR Am J Roentgenol. 2001;176(5):1145–8. doi: 10.2214/ajr.176.5.1761145. [DOI] [PubMed] [Google Scholar]
- 55.Luchs JS, Sofka CM, Adler RS. Contrast effect of combined steroid and anesthetic injections: In vitro analysis. Ultrasound Med. 2007;26(2):227–31. doi: 10.7863/jum.2007.26.2.227. [DOI] [PubMed] [Google Scholar]
- 56.Macmohan PJ, Eustace SJ, Kavanagh E. Injectable Corticosteroid and Local Anesthetic Preparations: A review for Radiologists. Radiology. 2009;252:647–661. doi: 10.1148/radiol.2523081929. [DOI] [PubMed] [Google Scholar]
- 57.Macintyre J, Joy E. Foot and Ankle Injuries in Dance. Clin Sports Med. 2000;19(2):351–68. doi: 10.1016/S0278-5919(05)70208-8. [DOI] [PubMed] [Google Scholar]
- 58.Maffulli N, Longo UG, Denaro V. Novel approaches for the management of tendinopathy. J Bone Joint Surg Am. 2010;92:2604–13. doi: 10.2106/JBJS.I.01744. [DOI] [PubMed] [Google Scholar]
- 59.Nicola M, Francesco O, Vittorino T, et al. Multiple Percutaneous Longitudinal Tenotomies for Chronic Achilles Tendinopathy in Runners. A Long-Term Study. Am J Sports Med Sep. 2013;41(9):2151–2157. doi: 10.1177/0363546513494356. [DOI] [PubMed] [Google Scholar]
- 60.Mahler F, Fritschy D. Partial and complete ruptures of the Achilles tendon and local corticosteroid injections. Br J Sports Med. 1992;26:7–14. doi: 10.1136/bjsm.26.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mautner K, Colberg R, Malanga G, et al. Outcomes After Ultrasound Guided Platelet Rich Plasma Injections for Chronic Tendinopathy: A Multicenter, Retrospective Review. PM R. 2013;5(3):169–175. doi: 10.1016/j.pmrj.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 62.McCarthy CL, Wilson DJ, Coltman TP. Anterolateral ankle impingement: findings and diagnostic accuracy with ultrasound imaging. Skeletal Radiol. 2008;37(3):209–216. doi: 10.1007/s00256-007-0411-6. [DOI] [PubMed] [Google Scholar]
- 63.McLauchlan G, Handoll HHG. Interventions for treating acute and chronic Achilles tendinitis. Editorial Group: Cochrane Bone, Joint and Muscle Trauma Group. Published Online: 21 Jan 2009 Assessed as up-to-date: 29 Dec 2000.
- 64.Nally M, Shilpa S. Plantar Fascia: Imaging Diagnosis and Guided Treatment. Semin Musculoskelet Radiol. 2010;14:334–343. doi: 10.1055/s-0030-1254522. [DOI] [PubMed] [Google Scholar]
- 65.Mehdizade A, Adler RS. Sonographically Guided Flexor Hallucis Longus Tendon Sheath Injection. J Ultrasound Med. 2007;26(2):233–7. doi: 10.7863/jum.2007.26.2.233. [DOI] [PubMed] [Google Scholar]
- 66.Metcalfe D, Achten J, Costa ML. Glucocorticoid injections in lesions of the Achilles tendon. Foot Ankle Int. 2009;30:661–665. doi: 10.3113/FAI.2009.0661. [DOI] [PubMed] [Google Scholar]
- 67.Miller T. Common Tendon and Muscle Injuries: Lower Extremity. Ultrasound Clin. 2007;2(4):595–615. doi: 10.1016/j.cult.2007.11.005. [DOI] [Google Scholar]
- 68.Muirr JJ, Curtiss HM, Hollman J, et al. The accuracy of ultrasound guided and palpation guided peroneal tendon sheath injections. Am J Phys Med Rehab. 2011;90(7):564–71. doi: 10.1097/PHM.0b013e31821f6e63. [DOI] [PubMed] [Google Scholar]
- 69.Muirr JJ, Curtiss HM, Hollman J, et al. The accuracy of ultrasound guided and palpation guided peroneal tendon sheath injections. Am J Phys Med Rehab. 2011;90(7):564–71. doi: 10.1097/PHM.0b013e31821f6e63. [DOI] [PubMed] [Google Scholar]
- 70.Nepple JJ, Matava JM. Soft Tissue Injections in the Athlete. Sports Health: Multidisciplinary Approach. 2009;1(5):396–404. doi: 10.1177/1941738109343159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nepple JJ, Zebala LP, Clohisy JC. Labral disease associated with cam-type femoroacetabular impingement. Radiology. 2005;236(20):588–92. [Google Scholar]
- 72.Nilsson C, Leanderson J, Wykman A, et al. The Injury Panorama in a Swedish Professional Ballet Company. Knee Surg Sports Traumatol Arthrosc. 2001;9(4):242–246. doi: 10.1007/s001670100195. [DOI] [PubMed] [Google Scholar]
- 73.Notzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg (Br) 2002;84(4):556–60. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 74.Ohberg L, Lorentzon R, Alfredson H. Neovascularization in Achilles tendons with painful tendinosis but not in normal tendon: An Ultrasonographic Investigation. Knee Surg Sports Traumatol Arthrosc. 2001;9(4):233–238. doi: 10.1007/s001670000189. [DOI] [PubMed] [Google Scholar]
- 75.Padhraig D, Hodgkins C, Kennedy J. Ankle Sprains and Instability in Dancers. Clin Sports Med. 2008;27(2):247–262. doi: 10.1016/j.csm.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 76.Fadale PD, Wiggins ME. Corticosteroid Injections: Their Use and Abuse. J Am Acad Orthop Surg. 1994;2(3):133–140. doi: 10.5435/00124635-199405000-00001. [DOI] [PubMed] [Google Scholar]
- 77.Pelsser V, Cardinal E, Hobden R, et al. Extraarticular snapping hip: sonographic findings. AJR Am J Roentgenol. 2001;176(1):67–73. doi: 10.2214/ajr.176.1.1760067. [DOI] [PubMed] [Google Scholar]
- 78.Reach JS, Easley ME, Chuckpaiwong B, et al. Accuracy of ultrasound guided injections in the foot and ankle. Foot Ankle Int. 2009;30(3):239–42. doi: 10.3113/FAI.2009.0239. [DOI] [PubMed] [Google Scholar]
- 79.Rees D. Jonathan, Stride Mathew, Scott Alex. Tendons-time to revisit inflammation. Br. J Sports Med. 2013;0:1–7. doi: 10.1136/bjsports-2012-091957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Robinson P, White LM. Soft-tissue and osseous impingement syndromes of the ankle: role of imaging in diagnosis and management. Radio-Graphics. 2002;22(6):1457–1469. doi: 10.1148/rg.226025034. [DOI] [PubMed] [Google Scholar]
- 81.Schweitzer M, Karasick D. MR Imaging of Disorders of the Achilles tendon. AJR. 2000;175(3):613–625. doi: 10.2214/ajr.175.3.1750613. [DOI] [PubMed] [Google Scholar]
- 82.Silva F, Adams T, Feinstein J, et al. Trochanteric bursitis: Refuting the myth of inflammation. JCR J Clin Rheumatol. 2008;14(2):82–86. doi: 10.1097/RHU.0b013e31816b4471. [DOI] [PubMed] [Google Scholar]
- 83.Sofka CM, Collins AJ, Adler RS. Use of ultrasonographic guidance in interventional musculoskeletal procedures: a review from a single institution. J Ultrasound Med. 2001;20(1):21–6. doi: 10.7863/jum.2001.20.1.21. [DOI] [PubMed] [Google Scholar]
- 84.Sofka C, Adler RS, Saboeiro G, et al. Sonographic Evaluation and sonographic-guided therapeutic options of lateral ankle pain: peroneal tendon pathology associated with the presence of an Os Peroneum. HSS J. 2010;6(2):177–181. doi: 10.1007/s11420-010-9154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sofka CM, Adler RS, Ciavarra G, et al. Ultrasound-guided Interdigital Neuroma Injections: short-term Clinical Outcomes after a Single Percutaneous Injection-Preliminary Results. HSS J. 2007;3(1):44–49. doi: 10.1007/s11420-006-9029-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sofka CM, Adler RS, Positano R, et al. Haglund’s syndrome: Diagnosis and treatment using sonography. HSS J. 2006;2(1):27–29. doi: 10.1007/s11420-005-0129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Sofka C, Adler R, Danon M. Sonography of the Acetabular Labrum. J Ultrasound. 2006;25(10):1321–1326. doi: 10.7863/jum.2006.25.10.1321. [DOI] [PubMed] [Google Scholar]
- 88.Sofka C, Saboeiro G, Adler RS. Ultrasound-guided adult hip injections. J Vasc Interventional Radiol. 2005;16(8):1121–1123. doi: 10.1097/01.RVI.0000167855.43900.74. [DOI] [PubMed] [Google Scholar]
- 89.Strauss E, Nho S, Kelly B. Greater trochanteric pain syndrome. Sports Med Arthrosc. 2010;18:2. doi: 10.1097/JSA.0b013e3181cdd195. [DOI] [PubMed] [Google Scholar]
- 90.Stretanski MF. Classical ballet: the full contact sport. Am J Phys Med Rehabil. 2002;81(5):392–393. doi: 10.1097/00002060-200205000-00014. [DOI] [PubMed] [Google Scholar]
- 91.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement radiographic diagnosis- what the radiologists should know. AJR Am J Roentgenol. 2007;188(6):1540–52. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 92.Tan Suan C, Otto C. Achilles and patellar tendinopathy: Current understanding of pathophysiology and management. Disability Rehab. 2008;30(20–22):1608–1615. doi: 10.1080/09638280701792268. [DOI] [PubMed] [Google Scholar]
- 93.Testa V, Maffulli N, Capasso G, et al. Management of Achilles tendinopathy by ultrasound guided percutaneous longitudinal tenotomy. Med Sci Sports Exerc. 2002;34(4):573–580. doi: 10.1097/00005768-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 94.Toth C. Peripheral Nerve Injuries Attributable to Sport and Recreation. Neurol Clin. 2008;26(1):89–113. doi: 10.1016/j.ncl.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 95.Tuwaru M, Bhargava R. Platelet rich Plasma therapy: A comparative effective therapy with promising results in plantar fasciitis. J Clin Orth Trauma. 2013;4(1):31–35. doi: 10.1016/j.jcot.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Verrall GM, Connell D. Evaluation of hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32(10):582–589. doi: 10.1007/s00256-003-0674-5. [DOI] [PubMed] [Google Scholar]
- 97.Wahl CJ, Warren RF, Adler RS, et al. Internal coxa saltans (snapping hip) as a result of overtraining: a report of 3 cases in professional athletes with a review of causes and the role of ultrasound in early diagnosis and management. Am J Sports Med. 2004;32(5):1302–9. doi: 10.1177/03363546503258777. [DOI] [PubMed] [Google Scholar]
- 98.Wang X, Rosenberg Z, Mechlin M, et al. Normal Variants and Diseases of the Peroneal Tendons and Superior Peroneal Retinaculum: MR Imaging Features. Radiographics. 2005;25(3):587–602. doi: 10.1148/rg.253045123. [DOI] [PubMed] [Google Scholar]
- 99.Weishpaut D, Treiber K, Kundert H, et al. Morton Neuroma: MR Imaging in Prone, Supine, and Upright Weight-bearing Body Positions. Radiology. 2003;226:849–856. doi: 10.1148/radiol.2263011925. [DOI] [PubMed] [Google Scholar]
- 100.Wetzel R, Ronak P, Terry M. Platelet-Rich Plasma as an Effective Treatment for Proximal Hamstring Injuries. Orthopedics. 2013;36(1):e64–e70. doi: 10.3928/01477447-20121217-20. [DOI] [PubMed] [Google Scholar]
- 101.Wiegerinck J, Reilingh M, Milko J, et al. Injection Techniques of Platelet Rich Plasma Into and Around the Achilles Tendon A Cadaveric Study. Am J Sports. 2011;39:1681. doi: 10.1177/0363546511401577. [DOI] [PubMed] [Google Scholar]
- 102.Wijesekera NT, Chew NS, Lee JC, et al. Ultrasound-guided treatments for chronic Achilles tendinopathy: an update and current status. Skeletal Radiol. 2010;39:425–434. doi: 10.1007/s00256-009-0873-9. [DOI] [PubMed] [Google Scholar]
- 103.Timothy WC, William SH, Darren JL. Medial Collateral Ligament “Tibial” Injuries: Indication for Acute Repair. Sports Med Update. 2004;27(4):389–393. doi: 10.3928/0147-7447-20040401-15. [DOI] [PubMed] [Google Scholar]
- 104.Wilson J, Lee K, Wang S .Platelet Rich Plasma for the Treatment of Chronic Plantar Fasciopathy in Adults A Case Series. Foot Ankle Spec Nov 2013. [DOI] [PubMed]
- 105.Winston P, Awan R, Cassidy D, et al. Clinical Examination and Ultrasound of Self Reported Snapping Hip Syndrome in Elite Ballet Dancers. Am J Sports Med. 2007;35(1):118–126. doi: 10.1177/0363546506293703. [DOI] [PubMed] [Google Scholar]
- 106.Jin W, Kim KI, Rhyu KH, et al. Sonographic Evaluation of Anterosuperior Hip Labral Tears With Magnetic Resonance Arthrographic And Surgical Correlation. JUM. 2012; 31(3): 439-447. [DOI] [PubMed]
- 107.Zanetti M, Strehle JK, Kundert HP, et al. Morton neuroma: effect of MR imaging findings on diagnostic thinking and therapeutic decisions. Radiology. 1999;213(2):583–588. doi: 10.1148/radiology.213.2.r99nv06583. [DOI] [PubMed] [Google Scholar]
- 108.Zanetti M, Dominik W. MR Imaging of the Forefoot: Morton Neuroma and Differential Diagnosis. Semin Musculoskelet Radiol. 2005;9(3):175–186. doi: 10.1055/s-2005-921938. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
ESM 7. A 27-year-old ballet dancer with lateral ankle pain. Dynamic cine clip imaged in short axis to the peroneal tendons with the patient actively circumducting at the level of the ankle shows intrasheath subluxation of the two tendons with respect to each other as well as subluxation onto and beyond the fibular tip with provocative maneuvers, reflecting laxity of the Q3 superior peroneal retinaculum. (AVI 50409 kb)
ESM 8. Cine images before and after surgery similarly demonstrate smoother motion of the FHL tendon after surgical release with active plantar and dorsiflexion of the big toe. (AVI 22014 kb)
ESM 9. Cine images before and after surgery similarly demonstrate smoother motion of the FHL tendon after surgical release with active plantar and dorsiflexion of the big toe. (AVI 24623 kb)